- 1Department of Comprehensive Chemotherapy/Head and Neck Cancer, Hunan Cancer Hospital, The Affiliated Cancer Hospital of Xiangya School of Medicine, Central South University, Changsha, Hunan, China
- 2Department of Pain Management and Anesthesiology, The Second Xiangya Hospital, Central South University, Changsha, Hunan, China
Some special therapeutic responses may appear during immunotherapy, such as hyperprogression, pseudoprogression and so on. Dissociated response of immunotherapy has been clinically reported in recent years mainly in lung cancer and kidney cancer. Since there were poor prognosis and simple treatment of advanced head and neck cancer, the application of immunotherapy in head and neck cancer has risen in recent years. But the dissociated response of immunotherapy in head and neck cancer is rarely reported. We reported two series of cases of advanced head and neck cancer that showed dissociated response after immunotherapy, tumor progression was assessed by imaging methods such as PET-CT, enhanced CT and enhanced MR, and reviewed the literature related to dissociated response in immunotherapy. We propose that the dissociated response of immunotherapy may affect the treatment strategy of advanced head and neck cancer, but more clinical analyses and researches are needed to confirm it.
Introduction
Squamous cell carcinoma of the head and neck (HNSCC) is the seventh most common malignancy worldwide, with approximately 64% of patients already locally advanced at the time of initial diagnosis (1, 2). With the increased use of immunotherapy in Patients with advanced head and neck cancer (3, 4), some special therapeutic responses of immunotherapy, such as hyperprogression (5), pseudoprogression (6), dissociated response(DR) and so on, deserve our attention. The dissociated response of immunotherapy in head and neck cancer has been rarely reported. We present two cases of recurrent and metastatic head and neck tumors with immunotherapeutic dissociated response in order to provide new insights for clinical decision-making.
Cases reports
Female patient in their 60s presented with a thyroid mass and lung metastases on imaging at the initial diagnosis (Figures 1A, D). The pathological report of the mass in left lobe of thyroid gland showed that it has been squamous cell carcinoma, and the immunohistochemical results demonstrated that malignant cells were positive for CK7 (regional positive), P40, CKpan, CK5/6, EMA, P16, PD-L1 (22C3) (CPS: > 50), EGFR, and negative for Calcitonin, CD117, CD5, CD56, CgA, CK20, Pax-8, SYN, Tg, NapsinA and TTF-1 immunohistochemical markers (Figure 1G). The patient was diagnosed with thyroid carcinoma (squamous cell carcinoma of the left lobe, cT2N1M1, stage IV lung metastases).
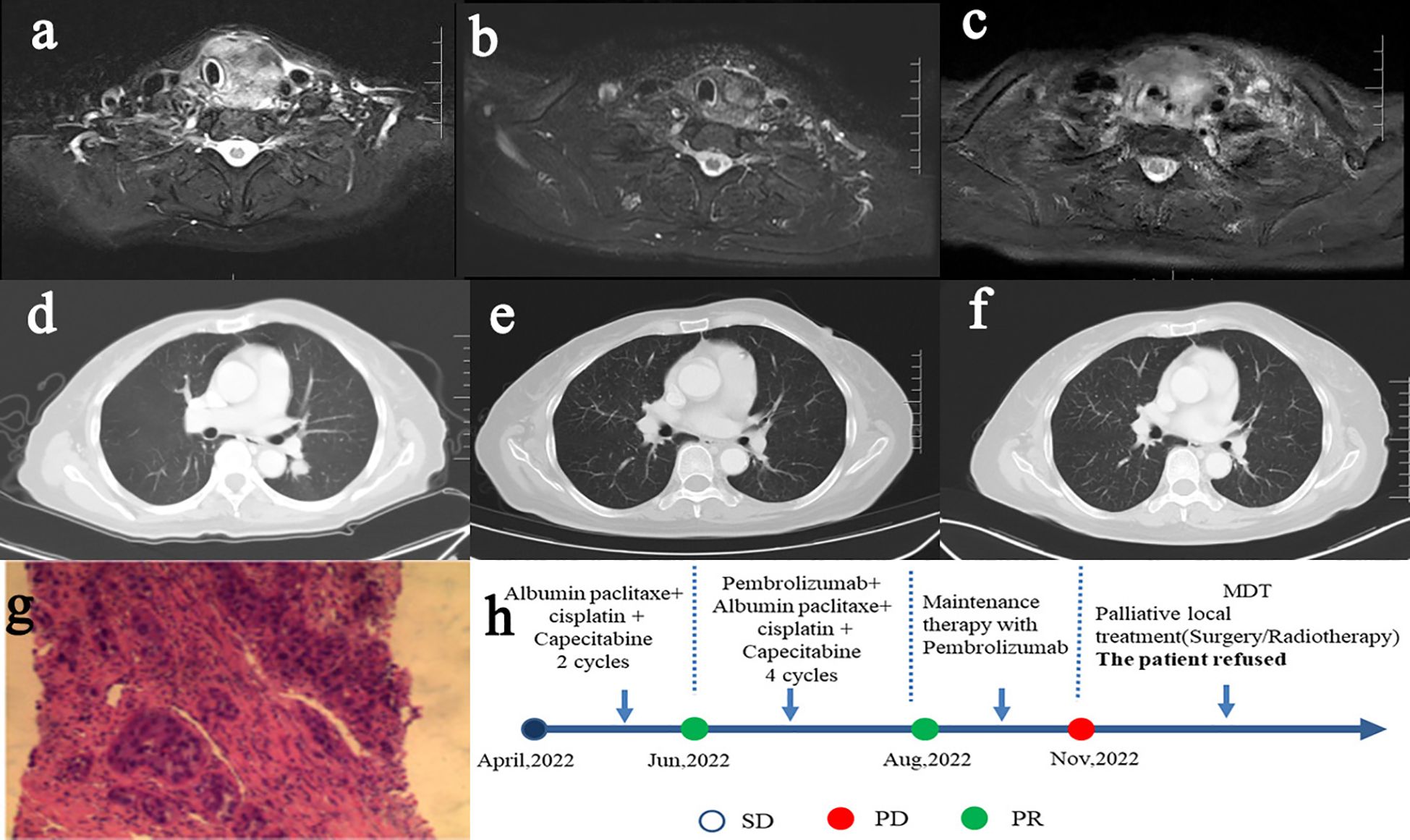
Figure 1. Contrast MR imaging of thyroid lesions (A, April 2022) (B, Aug 2022) (C, Nov 2022), contrast CT imaging of pulmonary metastases (D, April 2022) (E, Aug 2022) (F, Nov 2022), pathological HE staining (G), treatment procedure and curative effect evaluation (H).
After completing 6 cycles of chemotherapy and 4 cycles of immunotherapy, the pulmonary metastases were evaluated as complete response (CR) (Figures 1B, E). In the immune maintenance stage, the primary lesions progressed but the metastatic lung lesions were still in CR after 3 cycles of immunotherapy (Figures 1C, F). After consultation of multi-disciplinary team (MDT), it was recommended to have local treatment of surgery or radiotherapy for thyroid lesions progress. However, the patient and her family refused further treatment of surgery or radiotherapy after consideration, and still asked for conservative treatment. Considering the persistent CR of pulmonary metastases and the willingness of the patient, we retained immunotherapeutic drugs, changed the chemotherapy regimen, and added targeted therapy. The treatment of the patient was shown as follows in Figure 1H.
Male patient in their 40s presented with postoperative recurrence of gingival carcinoma. Both PET-CT and contrast CT/MR of the patient suggested pulmonary metastases (Figures 2A–C, F). The pathology of the mass showed that it has been highly-moderately differentiated squamous cell carcinoma, and the immunohistochemistry demonstrated that malignant cells were positive for CK-pan, CK5/6, EGFR, Ki67 (35%), P16 (small focus positive), P40, p53, PD-L1 (22C3) (CPS:5) immunohistochemical markers (Figure 2J). The patient was diagnosed with postoperative recurrence of gingival carcinoma (moderately-well differentiated squamous cell carcinoma, rT2N2M1, stage IVc lung metastasis).
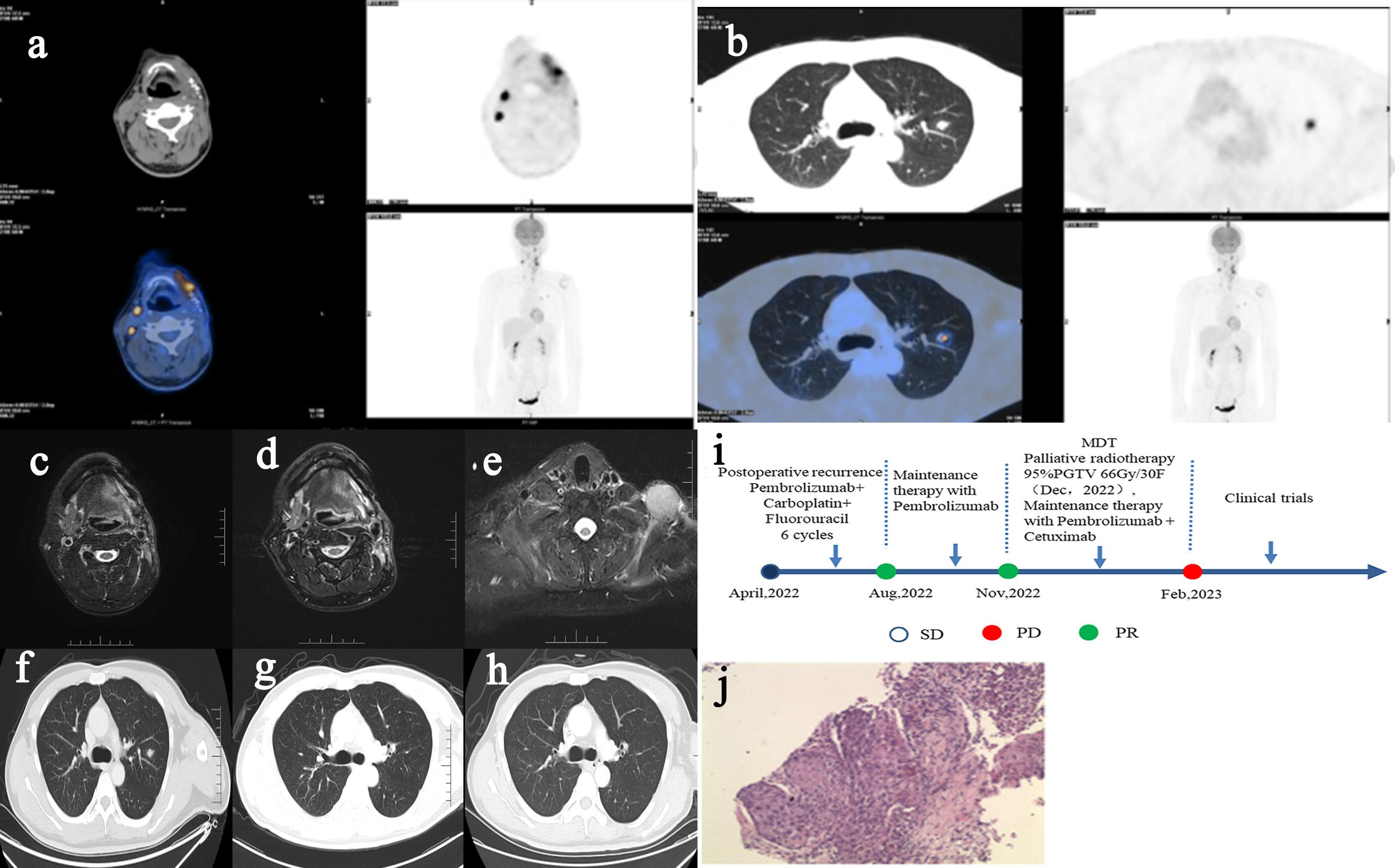
Figure 2. PET-CT imaging of recurrent lesions of head and neck (A, April 2022), PET-CT imaging of metastatic lesions of lung (B, April 2022), contrast MR imaging of recurrent lesions of head and neck (C, April 2022) (D, Nov2022), contrast MR imaging of new supraclavicular lesions that progressed after radiotherapy (E, Feb 2023), contrast CT imaging of metastatic lesions of lung (F, April 2022) (G, Nov2022) (H, Feb 2023), treatment procedure and curative effect evaluation (I), pathological HE staining (J).
After 6 cycles of chemotherapy and immunotherapy, the primary lesions of head and neck was partial response (PR) and the metastatic lesions of lung was CR (Figures 2D, G). After consultation of MDT, the patient was advised to receive local radiotherapy. The patient developed new lesions at the time more than 1 month after radiotherapy, and progressive disease (PD) was considered, but the pulmonary metastases were still in the state of CR (Figures 2E, H). Then the patient was suggested to enter a clinical trial and he agreed. The treatment of the patient was shown as follows in Figure 2I. The above two patients had no special past history and no family history of malignancy.
Discussion
At present, the dissociated response of immunotherapy is not well defined in radiological criteria guidelines. Generally speaking, it means that multiple target lesions have different degrees of therapeutic responses in the process of immunotherapy. According to the combination of different target lesions in clinic, Vaflard et al. have defined three types of DR (7): (1) one target lesion with CR/PR and one target lesion with PD (DR1); (2) one target lesion with stable disease (SD) and one target lesion with PD (DR2); (3) one target lesion with CR/PR and one target lesion with SD (DR3). According to the immune Response Evaluation Criteria in Solid Tumours (iRECIST), the overall response assessment of DR patients can be iPR, iSD, iUPD or iCPD. Then DR may be mistakenly classified as true progression by RECIST and iRECIST. Therefore, the occurrence of dissociated response may affect the decision of immunotherapy application. In addition, most current studies tend to believe that dissociated response in immunotherapy is an indicator with good prognosis (8–10), and prefer to retain immunotherapy after dissociated response occurs, which is different from the fact that dissociated response in chemotherapy and targeted therapy is an indicator of poor prognosis (11). The follow-up diagnosis and treatment program of the female patient we reported above referred to these studies and then retained immunotherapy. However, most of the cases in these published studies were lung cancer and other cancer types of solid tumors. When dissociated response appeared in head and neck cancer, the choice of immunotherapy was worthy of further discussion.
In the cases we provide, the distant metastases have achieved continuous CR during the treatment process, so whether the treatment of the primary lesion is still treated with systemic therapy or local treatment intervention (radiotherapy, surgery, etc.) can be considered is the focus of our next treatment strategy selection. It is noteworthy that Chinese researchers proposed localized nasopharyngeal radiotherapy for nasopharyngeal carcinoma patients with distant metastasis (non-liver metastasis) still had survival benefit (12). Therefore, based on the cases we provided, whether further refinement and stratification is needed to explore the differences of metastatic lesions with dissociated response may affect the decision of immunotherapy application, and then affect the prognosis and survival of patients.
The conversion therapy for colorectal cancer with liver metastasis has become a standard clinical practice. With the addition of immunotherapy, patients who had locally advanced head and neck cancer could achieve the goal of downstaging and benefit to reach the condition for focal treatment. At present, this clinical practice has been further confirmed by large-scale clinical trials (13).However, the studies on the conversion therapy for advanced head and neck cancer with distant metastasis were not sufficient. The cases reports we provided suggested that the dissociated response of immunotherapy in clinic had a significant impact on therapeutic strategies. Furthermore, because of the trailing effect of immunotherapy, some metastatic lesions continue subsided in the subsequent stage of treatment. Therefore, in the case of CR of distant metastatic lesions, whether there is survival benefit in continuing local treatment (surgery or radiotherapy) in head and neck lesions, further clinical studies are needed to confirm these results.
In the report of Bernard-Tessier A (9), a total of 360 patients with solid tumors were included, of which 24 cases of head and neck cancer had no dissociated response. But the researcher did not report the metastasis of the 24 cases of head and neck cancer in detail. The two cases we reported were both patients with lung metastases in head and neck cancer. According to the study of Vaflard P (7), if only focus on the organ where the target lesion is located and paying no attention to the type of primary tumor, the target lesion response rates and the probability of CR and PR were all higher in the lung and lymph node lesions. This is similar to CR of pulmonary lesions in the two patients of head and neck cancer with lung metastases we reported above. We speculate that the mechanism may be as follows: tumor heterogeneity, differences in the PD-L1 expression (14), and differences in the immune microenvironment in different organs (15).
In addition, PET/CT was used in the diagnosis of distant metastases in one of the HNSCC cases we offered. PET/CT is involved in the diagnosis and treatment and management of HNSCC, and plays an important role in the comprehensive evaluation before treatment, the determination of the target area of surgery and radiotherapy, the identification of in situ recurrence and inflammation, the identification of distant metastatic lesions, the evaluation of treatment efficacy, and prognostic follow-up (16, 17). PET/CT has been shown to improve the accuracy of lymph node staging on MRI of the neck in untreated laryngeal cancer and to increase the prognosis of survival outcomes through the use of multiple PET measures (18). With the comprehensive application of immunotherapy in tumor treatment, the development of immunotherapy imaging for cancer provides an important reference for clinical decision-making, especially for the identification of hyperprogression, pseudoprogression, and dissociative response (19).
In conclusion, we provide two cases reports of head and neck cancer with dissociated response of immunotherapy, which puts forward new ideas and challenges for the conversion therapy of immunotherapy in advanced head and neck cancer.
Data availability statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving humans were approved by Ethics Committee of Hunan Provincial Cancer Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
Author contributions
SJ: Writing – original draft. XL: Writing – review & editing. JL: Software, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Hunan Cancer Hospital Qihang Youth Fund Project (QH2021007).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Vos JL, Elbers J, Krijgsman O, Traets J, Qiao X, van der Leun AM, et al. Neoadjuvant immunotherapy with nivolumab and ipilimumab induces major pathological responses in patients with head and neck squamous cell carcinoma. Nat Commun. (2021) 12:7348. doi: 10.1038/s41467-021-26472-9
2. Qiu H, Cao S, Xu R. Cancer incidence, mortality, and burden in China: a time-trend analysis and comparison with the United States and United Kingdom based on the global epidemiological data released in 2020. Cancer Commun (Lond). (2021) 41:1037–48. doi: 10.1002/cac2.12197
3. Harrington KJ, Ferris RL, Blumenschein GJ, Colevas AD, Fayette J, Licitra L, et al. Nivolumab versus standard, single-agent therapy of investigator’s choice in recurrent or metastatic squamous cell carcinoma of the head and neck (CheckMate 141): health-related quality-of-life results from a randomised, phase 3 trial. Lancet Oncol. (2017) 18:1104–15. doi: 10.1016/S1470-2045(17)30421-7
4. Burtness B, Harrington KJ, Greil R, Soulieres D, Tahara M, de Castro GJ, et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet. (2019) 394:1915–28. doi: 10.1016/S0140-6736(19)32591-7
5. Champiat S, Dercle L, Ammari S, Massard C, Hollebecque A, Postel-Vinay S, et al. Hyperprogressive disease is a new pattern of progression in cancer patients treated by anti-PD-1/PD-L1. Clin Cancer Res. (2017) 23:1920–8. doi: 10.1158/1078-0432.CCR-16-1741
6. Seiwert TY, Burtness B, Mehra R, Weiss J, Berger R, Eder JP, et al. Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. Lancet Oncol. (2016) 17:956–65. doi: 10.1016/S1470-2045(16)30066-3
7. Vaflard P, Paoletti X, Servois V, Tresca P, Pons-Tostivint E, Sablin MP, et al. Dissociated responses in patients with metastatic solid tumors treated with immunotherapy. Drugs R D. (2021) 21:399–406. doi: 10.1007/s40268-021-00362-3
8. Tozuka T, Kitazono S, Sakamoto H, Yoshida H, Amino Y, Uematsu S, et al. Dissociated responses at initial computed tomography evaluation is a good prognostic factor in non-small cell lung cancer patients treated with anti-programmed cell death-1/ligand 1 inhibitors. BMC Cancer. (2020) 20:207. doi: 10.1186/s12885-020-6704-z
9. Bernard-Tessier A, Baldini C, Castanon E, Martin P, Champiat S, Hollebecque A, et al. Patterns of progression in patients treated for immuno-oncology antibodies combination. Cancer Immunol Immunother. (2021) 70:221–32. doi: 10.1007/s00262-020-02647-z
10. Sato Y, Morimoto T, Hara S, Nagata K, Hosoya K, Nakagawa A, et al. Dissociated response and clinical benefit in patients treated with nivolumab monotherapy. Invest New Drugs. (2021) 39:1170–8. doi: 10.1007/s10637-021-01077-7
11. Dong ZY, Zhai HR, Hou QY, Su J, Liu SY, Yan HH, et al. Mixed responses to systemic therapy revealed potential genetic heterogeneity and poor survival in patients with non-small cell lung cancer. Oncologist. (2017) 22:61–9. doi: 10.1634/theoncologist.2016-0150
12. You R, Liu YP, Huang PY, Zou X, Sun R, He YX, et al. Efficacy and safety of locoregional radiotherapy with chemotherapy vs chemotherapy alone in de novo metastatic nasopharyngeal carcinoma: A multicenter phase 3 randomized clinical trial. JAMA Oncol. (2020) 6:1345–52. doi: 10.1001/jamaoncol.2020.1808
13. Ferris RL, Spanos WC, Leidner R, Goncalves A, Martens UM, Kyi C, et al. Neoadjuvant nivolumab for patients with resectable HPV-positive and HPV-negative squamous cell carcinomas of the head and neck in the CheckMate 358 trial. J Immunother Cancer. (2021) 9(6). doi: 10.1136/jitc-2021-002568
14. Moutafi MK, Tao W, Huang R, Haberberger J, Alexander B, Ramkissoon S, et al. Comparison of programmed death-ligand 1 protein expression between primary and metastatic lesions in patients with lung cancer. J Immunother Cancer. (2021) 9(4). doi: 10.1136/jitc-2020-002230
15. Oliver AJ, Lau P, Unsworth AS, Loi S, Darcy PK, Kershaw MH, et al. Tissue-dependent tumor microenvironments and their impact on immunotherapy responses. Front Immunol. (2018) 9:70. doi: 10.3389/fimmu.2018.00070
16. Cammaroto G, Quartuccio N, Sindoni A, Di Mauro F, Caobelli F. The role of PET/CT in the management of patients affected by head and neck tumors: a review of the literature. Eur Arch Otorhinolaryngol. (2016) 273:1961–73. doi: 10.1007/s00405-015-3651-4
17. Caldarella C, De Risi M, Massaccesi M, Micciche F, Bussu F, Galli J, et al. Role of (18)F-FDG PET/CT in head and neck squamous cell carcinoma: current evidence and innovative applications. Cancers (Basel). (2024) 16(10). doi: 10.3390/cancers16101905
18. Al-Ibraheem A, Abdlkadir AS, Al-Adhami D, Hejleh TA, Mansour A, Mohamad I, et al. The prognostic and diagnostic value of [(18)F]FDG PET/CT in untreated laryngeal carcinoma. J Clin Med. (2023) 12(10). doi: 10.3390/jcm12103514
Keywords: dissociated response, immunotherapy, advanced head and neck cancer, treatment strategy, conversion therapy
Citation: Jiang S, Li X and Li J (2024) Case report: The impact of dissociated response of immunotherapy on the treatment strategy of advanced head and neck cancer. Front. Immunol. 15:1460480. doi: 10.3389/fimmu.2024.1460480
Received: 06 July 2024; Accepted: 17 September 2024;
Published: 15 October 2024.
Edited by:
Lei Tao, Fudan University, ChinaReviewed by:
Firas Hamdan, University of Helsinki, FinlandAkram Al-Ibraheem, King Hussein Cancer Center, Jordan
Copyright © 2024 Jiang, Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jin Li, bGlqaW5AaG5jYS5vcmcuY24=
 Siqing Jiang
Siqing Jiang Xin Li
Xin Li Jin Li
Jin Li