- 1Department of Geriatric Rehabilitation, Rehabilitation Hospital affiliated to Fujian University of Traditional Chinese Medicine, Fuzhou, Fujian, China
- 2Fujian Key Laboratory of Rehabilitation Technology, Fuzhou, Fujian, China
Objective: This study aims to assess the associations of complete blood cell count (CBC)-derived inflammatory biomarkers with the prevalence of asthma and mortality.
Methods: Data was collected from the 1999-2018 National Health and Nutrition Examination Survey (NHANES). Mortality was identified using the National Death Index until December 31, 2019. The study analyzed the relationship between CBC-derived inflammatory biomarkers, including neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), monocyte-to-lymphocyte ratio (MLR), systemic inflammatory response index (SIRI), and systemic immune-inflammation index (SII), and the prevalence of asthma using multiple logistic regressions. To assess the significance of CBC-derived inflammatory biomarkers in predicting all-cause and respiratory disease mortality in asthma patients, Cox proportional regressions and the random survival forest (RSF) analysis were utilized.
Results: A total of 48,305 participants were included, with a mean age of 47.27 ± 0.18 years and 49.44% male. Among them, 6,403 participants had asthma, with a prevalence of 13.28%. The all-cause and respiratory disease deaths at a median follow-up of 8.2 (4.5, 12.8) years were 929 and 137 respectively. After adjusting for confounders, the prevalence of asthma was found to be positively associated with NLR, PLR, MLR, SIRI and SII. Compared to the lowest quartile, the highest quartile of NLR (HR=1.765 [1.378-2.262]), MLR (HR=1.717 [1.316-2.241]), SIRI (HR=1.796 [1.353-2.383]) and SII (HR=1.432 [1.141-1.797]) were associated with an increased risk of all-cause mortality. These associations were more pronounced in respiratory disease mortality of asthma patients. RSF analysis showed that MLR had the highest predictive value for all-cause and respiratory disease mortality in adults with asthma. The sensitivity analysis demonstrated the stability of our results.
Conclusion: The findings suggest that CBC-derived inflammatory biomarkers are associated with a higher risk of all-cause and respiratory disease mortality in adults with asthma.
1 Background
//Asthma has become a severe public health problem, affecting people from childhood to old age (1). Approximately 300 million people in the world have asthma, with at least 250,000 deaths attributed to the disease each year (2). Inflammation plays a pivotal role in the process of developing asthma (3). Both local and systemic inflammation are involved in the development of asthma (4, 5). Neutrophils, in the early stages of asthma exacerbations, play a crucial role by releasing various pro-inflammatory mediators, thereby contributing to airway inflammation (6). Monocytes differentiate into macrophages, which are central to the chronic inflammation observed in asthma (7). Macrophages release inflammatory molecules like cytokines and chemokines, which attract and activate other immune cells, perpetuating the inflammatory response. Lymphocytes, particularly T-helper 2 (Th2) lymphocytes, also play a significant role in asthma (8). Th2 lymphocytes release cytokines that promote airway inflammation, mucus production, and bronchoconstriction (8). Consequently, inflammatory indicators appear to be effective biomarkers for assessing severity and potential therapeutic targets in patients with asthma (9). Current studies have reported that a variety of inflammation-related indicators might be related to outcomes in asthma patients (10, 11), but the optimal biomarker for asthma is unclear.
Recently, CBC-derived inflammatory biomarkers such as the neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), monocyte-to-lymphocyte ratio (MLR), systemic inflammatory response index (SIRI), and systemic immune-inflammation index (SII) were used as prognostic factors in various diseases (12, 13). These biomarkers are based on two or three parameters related to neutrophils, lymphocytes, platelets, and monocytes. The NLR, SII, and SIRI have a predictive power of severe COVID-19 and invasive mechanical ventilation (IMV) support during hospitalization in Mexican COVID-19 patients (14). In addition, the WBC count, neutrophil count, dNLR, and SII were significantly associated with survival in COVID-19 patients (15). Similarly, in individuals diagnosed with community-acquired pneumonia, neutrophil-lymphocyte ratio has been associated with increased mortality risk (16). Furthermore, in chronic obstructive pulmonary disease (COPD) patients, elevated neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR) values have been linked to higher mortality rates (17, 18). Additionally, the SII, another CBC-derived biomarker, has demonstrated its potential in predicting mortality among middle-aged and elderly individuals with COPD and asthma (19).
Asthma is a chronic inflammatory disorder primarily affecting the airways. The underlying immune and inflammatory mechanisms in asthma may differ from those in other diseases, such as infectious diseases or systemic inflammatory conditions. Thus, the inflammatory profiles and immune responses can vary among different subgroups of asthma patients. Furthermore, the relationship between CBC-derived inflammatory biomarkers and survival has not been comprehensively evaluated in patients with asthma. Therefore, using data from the 1999-2018 National Health and Nutrition Examination Survey (NHANES), this study examined the association between CBC-derived inflammatory biomarkers and the prevalence of asthma, as well as the mortality in participants with asthma. Our study aimed to provide a valuable prognostic indicator and guide the individual treatment of asthma.
2 Materials and methods
2.1 Study population
Data were obtained from the NHANES, which is a national survey that collected nutritional and health status of children and adults (20). This project is conducted by the National Center for Health Statistics (NCHS) at the Centers for Disease Control and Prevention (CDC) and focuses on collecting basic physical and biochemical examinations and other medically relevant information. The National Center for Health Statistics (NCHS) Research Ethics Review Board approved the research protocols, and all participants gave informed consent.
In this study, we analyzed data from the 1999-2018 NHANES. We excluded participants under the age of 20 and those with missing asthma assessment data. Participants who were pregnant, lacking data on CBC parameters, and had no follow-up information were also excluded.
2.2 Assessment of CBC-derived inflammatory biomarkers
The complete blood count (CBC) is measured using automated hematology analyzers, which count the number of different blood cells (red blood cells, white blood cells, and platelets) in given volume of blood. We calculated the SIRI, SII, NLR, PLR, and MLR as follows: SIRI = neutrophil counts × monocyte counts/lymphocyte counts, SII = platelet counts × neutrophil counts/lymphocyte counts, NLR = neutrophil counts/lymphocyte counts, PLR = platelet counts/lymphocyte counts, MLR = monocyte counts/lymphocyte counts (12, 13).
2.3 Assessment of asthma
By using a self-administered questionnaire, NHANES collected information on asthma and associated symptoms (21). Patients who answered affirmatively to the following two questions were defined as having current asthma: “Has a doctor or other health professional ever told you that you have asthma?” and “Do you still have asthma?”. Patients who gave negative answers to these two questions were used as the control group.
2.4 Assessment of mortality
Study participants who had died were identified by linkage to the National Death Index (NDI). As of December 31st, 2019, we obtained all-cause and respiratory disease mortality records for participants via the 2019 Linked Mortality File (LMF), which reports the latest associations made between selected NCHS surveys and the NDI.
2.5 Covariates
Information regarding participants’ baseline data was collected through questionnaires and laboratory tests, including age (years), sex (male or female), race/ethnicity (Mexican American, other Hispanic, non-Hispanic white, non-Hispanic black, or other race), educational attainment (below high school, high school, or above high school), and body mass index (<25.0, 25.0-29.9, or >29.9 kg/m2). Income was measured using the poverty-income ratio (PIR; the ratio of family income divided by a poverty threshold specific for family size using guidelines from the US Department of Health and Human Services) and categorized as ≤1.0, 1.1-3.0, and >3.0 (22). Never smokers were identified as those who reported smoking <100 cigarettes over the course of their lifetime. Those who smoked >100 cigarettes in their lifetime were classified as current smokers, and those who smoked >100 cigarettes and had quit smoking were labeled as former smokers (23). Drinking status was classified as nondrinker, low-to-moderate drinker (<2 drinks/day in men and <1 drink/day in women), or heavy drinker (≥2 drinks/day in men and ≥1 drinks/day in women) (23). Physical activity was divided into three groups: inactive (no leisure-time physical activity), insufficiently active (moderate activity 1–5 times per week with metabolic equivalent of task [MET] 3–6 or vigorous activity 1–3 times per week with MET >6), and active (those who had more moderate or vigorous activity than the previously mentioned) (23–25). The energy intake (kcal/day) was calculated by averaging two values from two 24-hour recall interviews. Information on the prevalence of hypertension and diabetes was retrieved using self-reported questionnaires.
2.6 Statistical analysis
Normally distributed continuous variables were described as means ± standard errors (SEs), and continuous variables without a normal distribution were presented as medians (interquartile range [IQR]). Categorical variables were presented as numbers (percentages). Continuous variables are compared using Student’s t-test (normal distribution) or the Mann-Whitney U test (non-normal distribution). Categorical variables are compared using the chi-square test. Missing values for covariates were filled using the imputation approach, which was based on a “mice” package of the Random Forest algorithm. We performed all statistical analyses using R software (version 4.2.0).
A multiple logistic regression model was employed to ascertain the adjusted odds ratios (ORs) and 95% confidence intervals (CIs) of the association between CBC-derived inflammatory biomarkers and the prevalence of asthma. A multiple COX regression was implemented to calculate adjusted hazard ratios (HRs) and 95% CIs in relation to all-cause and respiratory disease mortality of participants with asthma. To explore the dose–response curves between CBC-derived inflammatory biomarkers and mortality in asthma patients, restricted cubic spline regression analysis was performed. The knots were placed at each exposure variable’s 10th, 50th and 90th percentiles.
Spearman’s correlation analysis was used to calculate the correlation coefficients among CBC-derived inflammatory biomarkers and CBC. A random survival forest method was used to compare the value of CBC-derived inflammatory biomarkers in predicting all-cause and respiratory disease mortality in asthma patients. Stratified analysis was conducted to assess the associations between quartiles of CBC-derived inflammatory biomarkers levels and all-cause and respiratory disease mortality by smoking among adults with asthma in NHANES 1999–2018.
Multiple sensitivity analyses were performed to evaluate the robustness of the results. Firstly, we further adjusted for anti-asthmatic medications such as bronchodilators, inhaled corticosteroids, or other anti-asthmatic drugs, as well as lung function parameters including forced vital capacity (FVC) and forced expiratory volume 1st second (FEV1). Secondly, to minimize the potential for reverse causation bias, participants who died within the first two years of follow-up were excluded from the study. Additionally, participants with a history of cancer, HIV infection, or respiratory infections at baseline were also excluded from the study. Cox regression analysis was then performed to assess the relationship between CBC-derived inflammatory biomarkers and mortality in asthma participants. Lastly, participants with self-reported chronic obstructive pulmonary disease (COPD) at baseline were excluded from the study, and the relationship was analyzed once again.
3 Results
3.1 Characteristics of study participants
Between 1999 and 2018, 48,305 adults participated in the NHANES. We removed participants younger than 20 and missing data on asthma assessment (n=46,235). Subsequently, we excluded participants who were pregnant (n=1,317), and those who lacked data on CBC parameters (n=5,459). In addition, the eleven participants with asthma whom we failed to interview were excluded, resulting in a total of 6,403 participants with asthma for survival analysis (Figure S1).
Table 1 displays the baseline characteristics of adults with CBC-derived inflammatory biomarkers in the 1999–2018 NHANES. The study population had a mean age of 47.27 ± 0.18 years, was 49.44% male, and was mainly non-Hispanic white (44.57%). The medians of NLR, PLR, MLR, SIRI and SII were 2.00 [IQR 1.51, 2.62], 121.43 [IQR 96.45, 153.13], 0.26 [IQR 0.21, 0.33], 1.06 [IQR 0.73, 1.53] and 487.18 [IQR 353.69, 680.77], respectively. There were 6,414 (13.28%) participants have asthma. Compared to non-asthmatic participants, they were more likely to be younger non-Hispanic White females, to have higher education and lower income levels, to be current smokers, low-to-moderate drinkers, physically inactive, to have a higher BMI, and to have higher prevalence of hypertension (P<0.05). The counts of white blood cell (WBC), neutrophils, monocyte, lymphocyte, and platelet were significantly higher in asthma patients (P<0.05). Among all CBC-derived indicators, only SIRI and SII showed significant differences between participants with and without asthma.
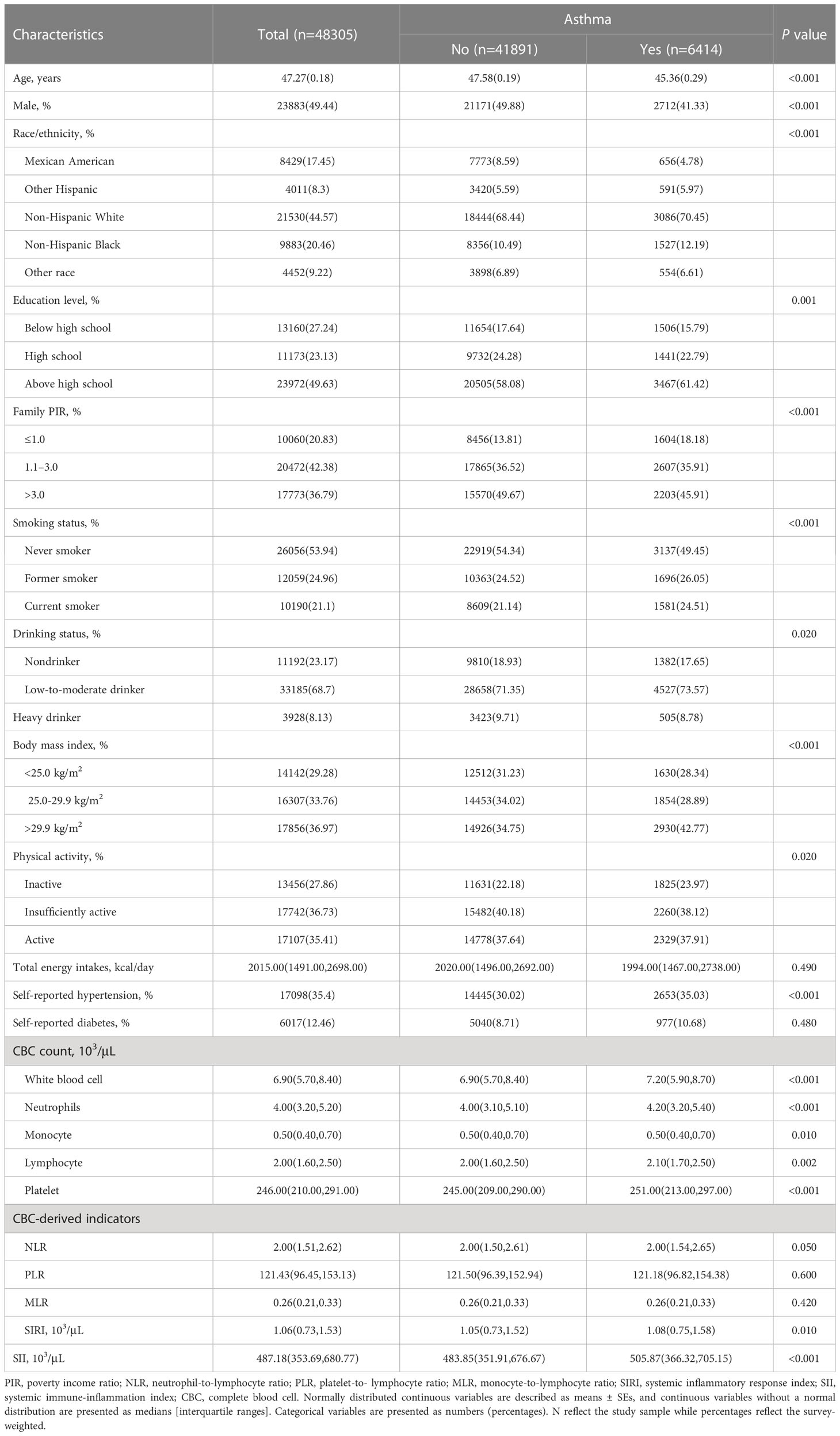
Table 1 Baseline characteristics of adults with CBC-derived inflammatory biomarkers in NHANES 1999–2018.
Over a median follow-up of 8.2 (4.5, 12.8) years, there were 929 (4.5%) all-cause deaths among 6,403 adults with asthma (Table S2). Compared to survivors, those who died of all causes were more likely to be older non-Hispanic White patients, to have lower education and income levels, to be current smokers, heavy drinkers, physically inactive, to have a higher BMI, and to have higher prevalence of hypertension and diabetes (P<0.05). In addition, all-cause deaths were more likely to have a higher value of all CBC-derived indicators (P<0.05).
3.2 Associations between CBC-derived indicators and the prevalence of asthma
All CBC-derived indicators were classified into four groups and assessed for their association with the prevalence of asthma (Table 2). The crude model revealed positive correlations between CBC-derived indicators (NLR, SIRI, and SII) and the prevalence of asthma. After adjusting for age, sex, and race, this relationship remained statistically significant.
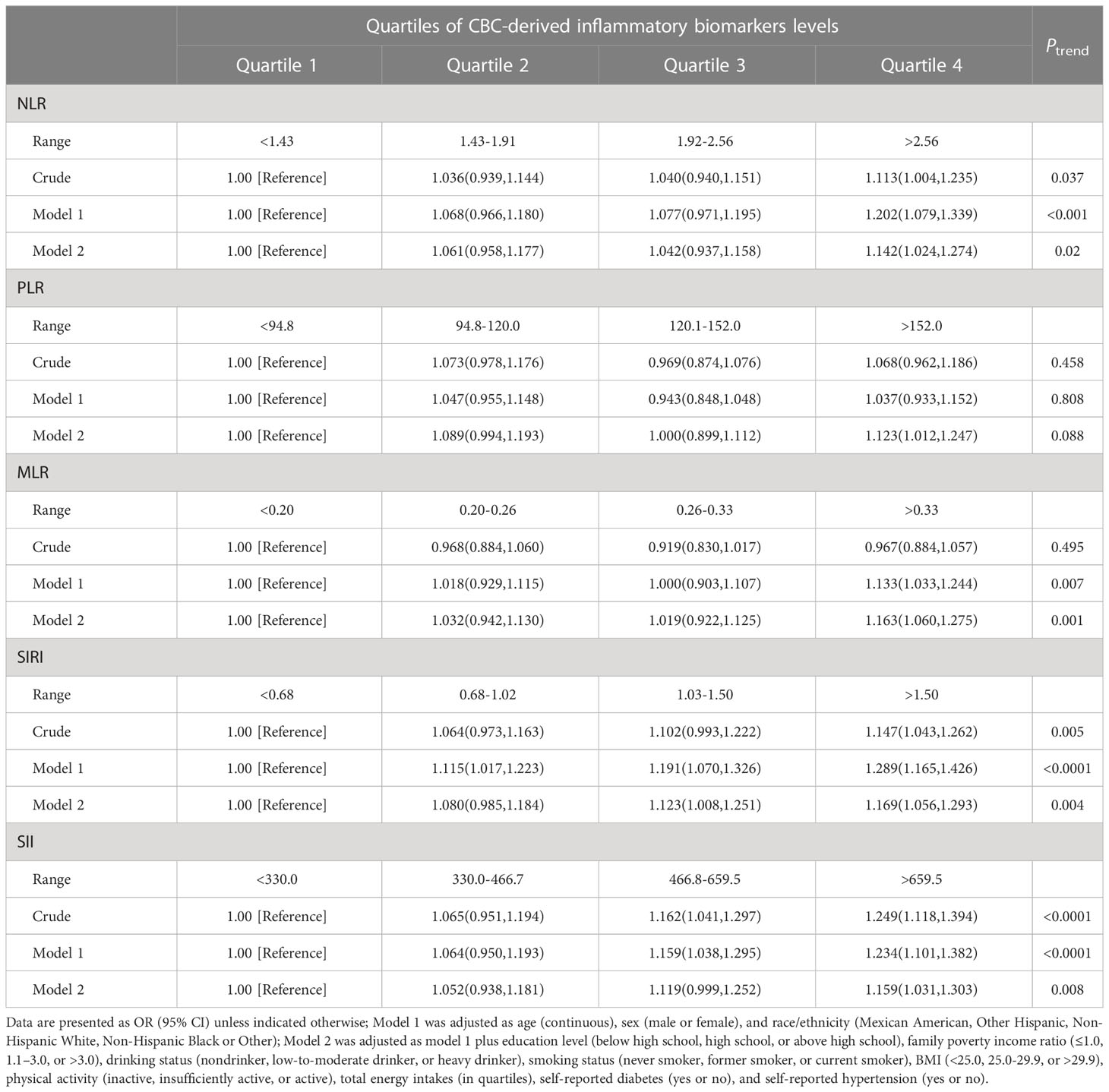
Table 2 OR (95% CIs) of the prevalence of asthma according to quartiles of complete blood cell (CBC)-derived inflammatory biomarkers among adults in NHANES 1999–2018.
In model 2, higher levels of NLR, PLR, MLR, SIRI, and SII were all significantly associated with an increased prevalence of asthma. Specifically, individuals in the fourth quartile of these inflammatory biomarkers had higher odds of having asthma than those in the first quartile. After adjusting for potential confounding factors, the odds ratios (ORs) and 95% confidence intervals (CIs) for the highest quartile compared to the lowest quartile were as follows: NLR (OR=1.142 [1.024-1.274], Ptrend=0.02), PLR (OR=1.123 [1.012-1.247], Ptrend=0.088), MLR (OR=1.163 [1.060-1.275], Ptrend=0.001), SIRI (OR=1.169 [1.056-1.293], Ptrend=0.004), and SII (OR=1.149 [1.031-1.303], Ptrend=0.008). We also analyzed the relationship between CBC parameters and the prevalence of asthma (Table S1). In the crude model, all CBC parameters were positively associated with the prevalence of asthma. After correcting for all confounding factors, we only found that WBC, neutrophils, monocyte were significantly associated with a higher prevalence of asthma.
3.3 Associations between CBC-derived indicators and mortality
As shown in Table 3, participants with asthma in quartile 4 had the highest risk of all-cause death. After multivariate adjustment in the Model 2, participants with asthma in quartile 4 of NLR (HR=1.765 [1.378-2.262]), MLR (HR=1.717 [1.316-2.241]), SIRI (HR=1.796 [1.353-2.383]) and SII (HR=1.432 [1.141-1.797]) remained significantly associated with an increased risk of all-cause mortality, compared with participants with asthma in quartile 4. CBC-derived indicators exhibited nonlinear associations with all-cause mortality of participants with asthma (P for nonlinearity<0.05, Figure 1). We also analyzed the relationship between CBC parameters and the risk of all-cause death in asthma patients (Table S3). After correcting for all confounding factors, we found that neutrophils (HR=1.364 [1.066-1.745]) and monocyte (HR=1.604 [1.208-2.129]) were significantly associated with a higher risk of all-cause mortality.
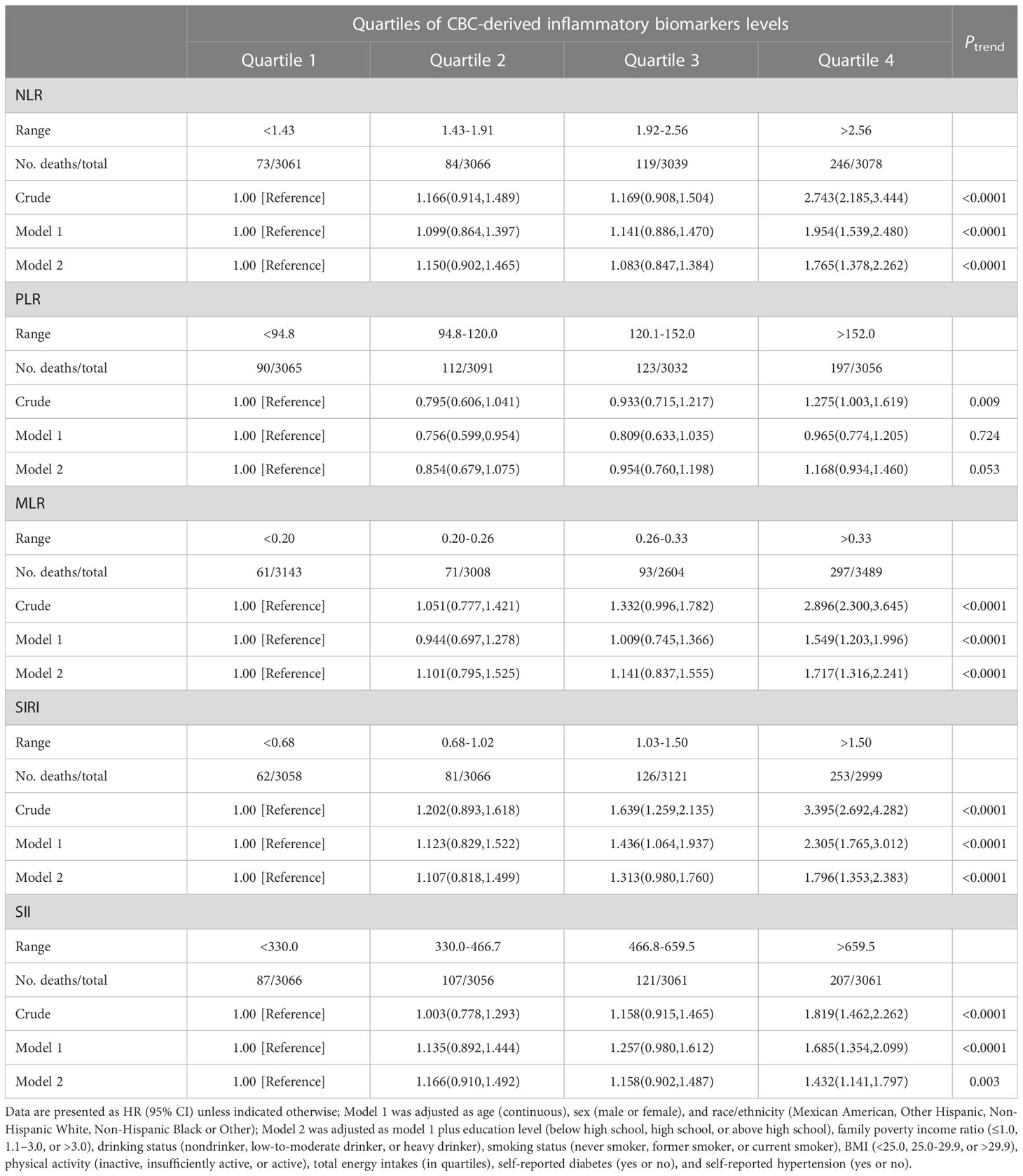
Table 3 HRs (95% CIs) of all-cause mortality according to quartiles of complete blood cell (CBC)-derived inflammatory biomarkers among adults with asthma in NHANES 1999–2018.
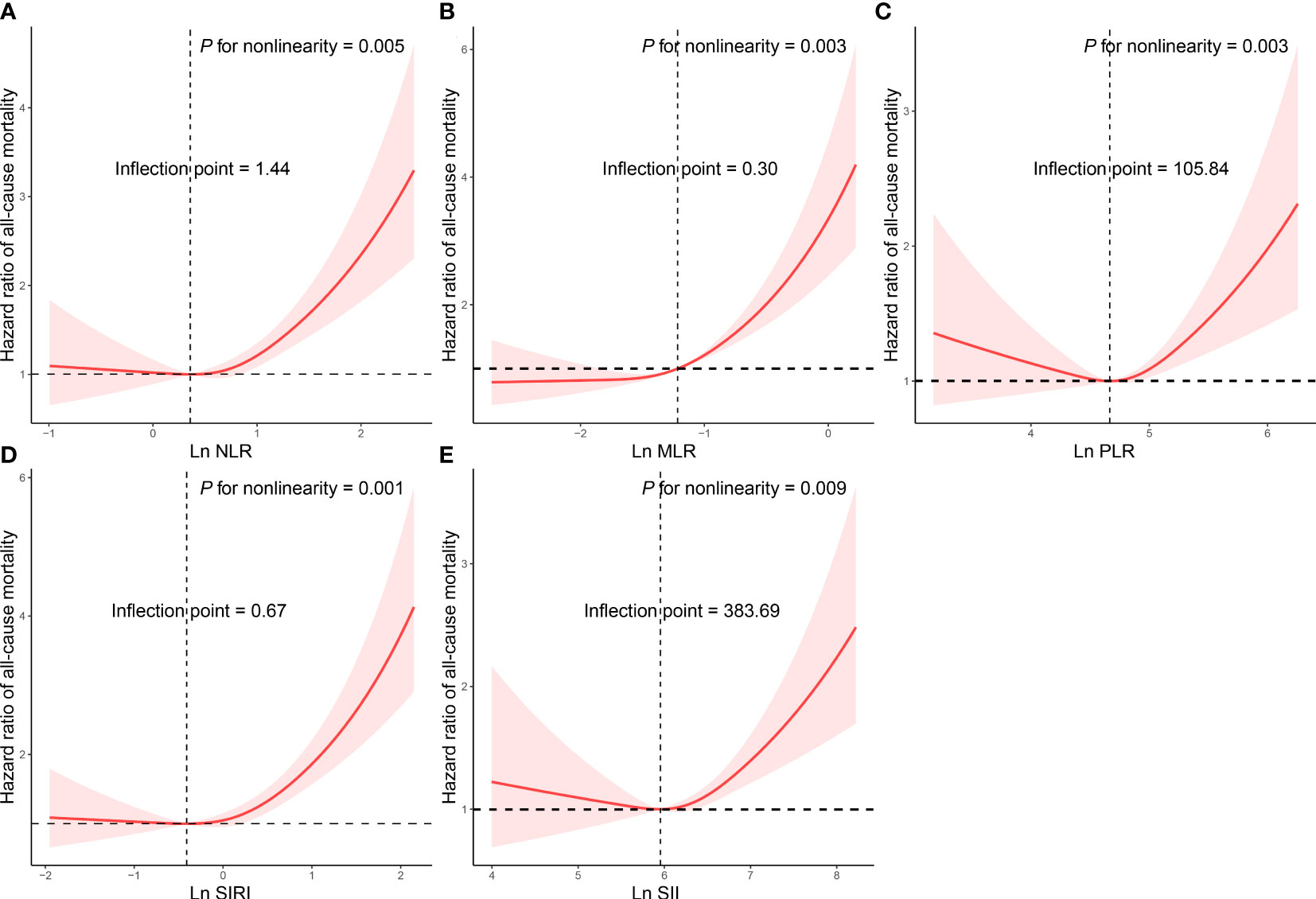
Figure 1 Restricted cubic spline analyses the association of complete blood cell count (CBC)-derived indicators (A: NLR; B: MLR; C: PLR; D: SIRI; E: SII) with all-cause mortality in adults with asthma. Adjusted for age (continuous), sex (male or female), race/ethnicity (Mexican American, Other Hispanic, Non-Hispanic White, Non-Hispanic Black or Other), education level (below high school, high school, or above high school), family poverty income ratio (≤1.0, 1.1–3.0, or >3.0), drinking status (nondrinker, low-to-moderate drinker, or heavy drinker), smoking status (never smoker, former smoker, or current smoker), BMI (<25.0, 25.0-29.9, or >29.9), physical activity (inactive, insufficiently active, or active), total energy intakes (in quartiles), self-reported diabetes (yes or no), and self-reported hypertension (yes or no).
Cox proportional regression results showed that NLR, MLR, SIRI and SII were associated with an increased risk of respiratory disease mortality in asthma patients (Table 4). After multivariate adjustment, the HR of NLR, MLR, SIRI and SII were 2.622, 2.812, 3.208, and 1.988, respectively (P<0.05). NLR, MLR, SIRI and SII exhibited linear associations with respiratory disease mortality of participants with asthma (P for nonlinearity>0.05, Figure 2). We also analyzed the relationship between CBC parameters and the risk of respiratory disease death in asthma patients (Table S3). After correcting for all confounding factors, we found that all CBC parameters were significantly associated with a higher risk of respiratory disease mortality (P<0.05).
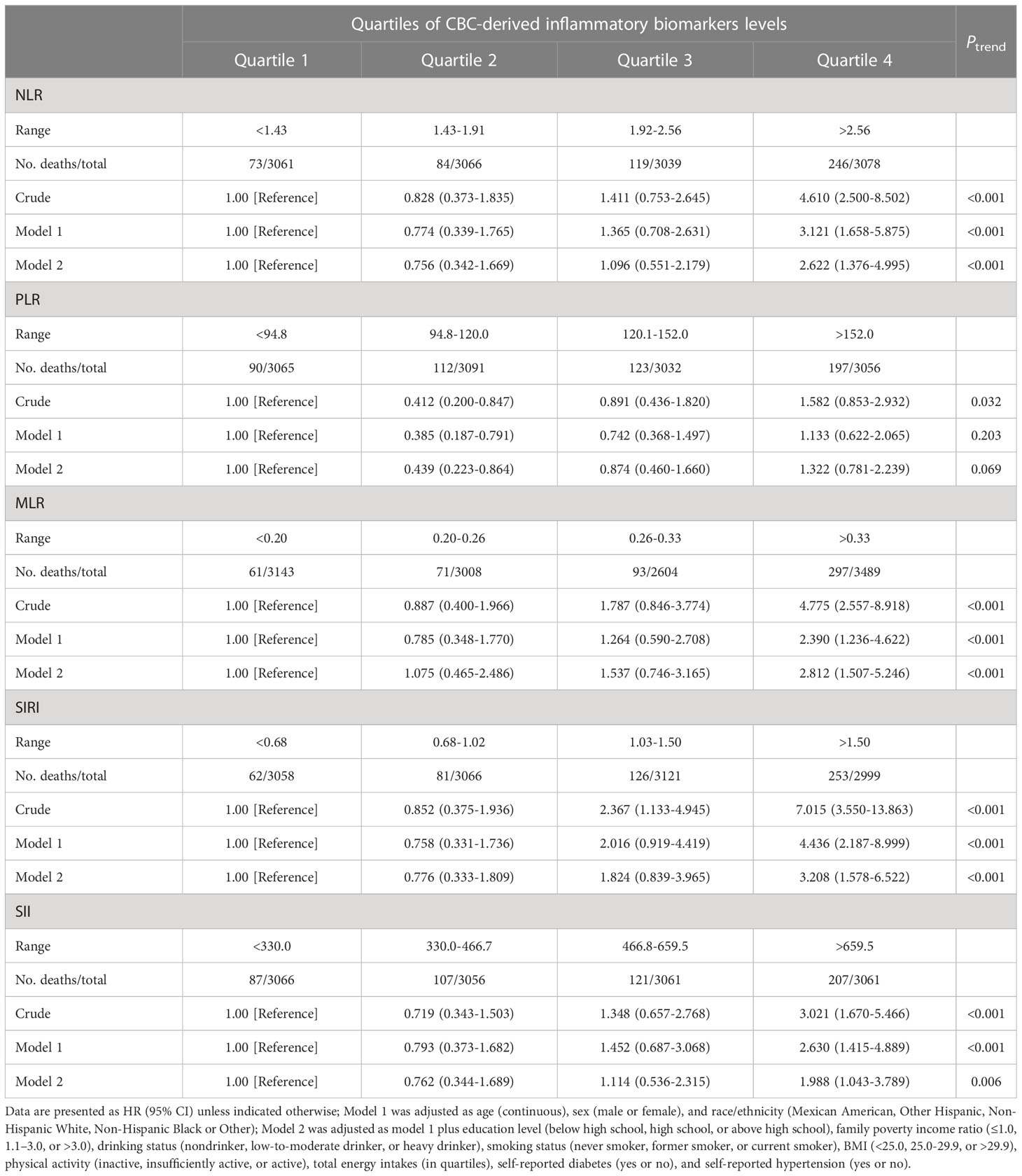
Table 4 HRs (95% CIs) of respiratory disease mortality according to quartiles of complete blood cell (CBC)-derived inflammatory biomarkers among adults with asthma in NHANES 1999–2018.
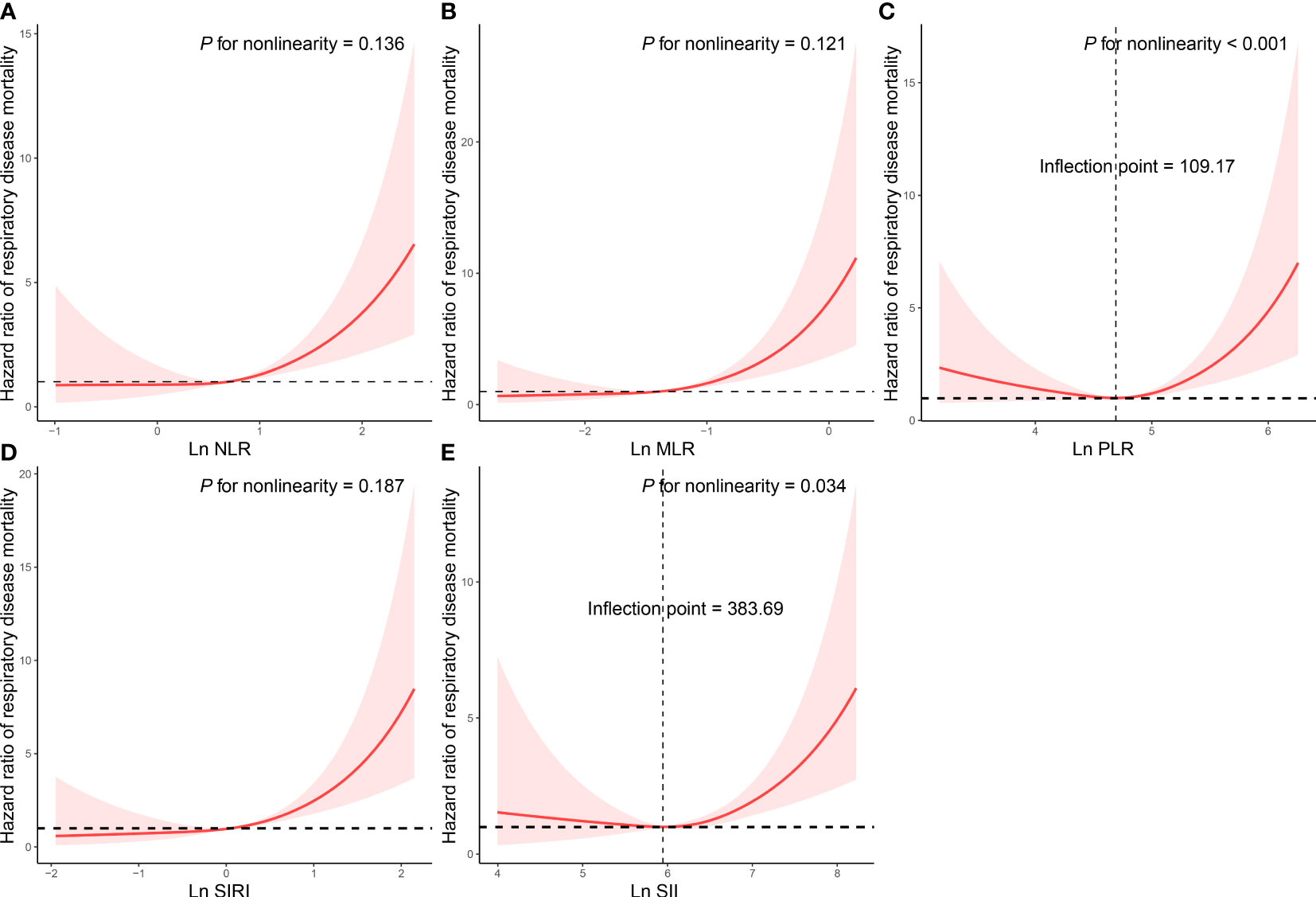
Figure 2 Restricted cubic spline analyses the association of complete blood cell count (CBC)-derived indicators (A: NLR; B: MLR; C: PLR; D: SIRI; E: SII) with respiratory disease mortality in adults with asthma. Adjusted for age (continuous), sex (male or female), race/ethnicity (Mexican American, Other Hispanic, Non-Hispanic White, Non-Hispanic Black or Other), education level (below high school, high school, or above high school), family poverty income ratio (≤1.0, 1.1–3.0, or >3.0), drinking status (nondrinker, low-to-moderate drinker, or heavy drinker), smoking status (never smoker, former smoker, or current smoker), BMI (<25.0, 25.0-29.9, or >29.9), physical activity (inactive, insufficiently active, or active), total energy intakes (in quartiles), self-reported diabetes (yes or no), and self-reported hypertension (yes or no).
We performed a sensitivity analysis to investigate the robustness of our findings. Firstly, we excluded participants who died within two years of follow-up, and conducted a Cox regression analysis again. The results revealed that the relationship between CBC-derived indicators and all-cause and respiratory disease mortality persisted, as evidenced by the statistically significant association reported in Table S4. Furthermore, we conducted another sensitivity analysis by excluding participants who had a cancer history at baseline. The results of this analysis were also stable and consistent with our original findings, as demonstrated by the statistically significant association reported in Table S5.
3.4 Prognostic value of CBC-derived indicators
We examined the correlation between CBC parameters and CBC-derived inflammatory biomarkers (Figure 3A). There was a significant positive correlation between platelet and SII (r=0.85) and a significant negative correlation between lymphocyte and PLR (r=-0.71). We utilized a RSF analysis to compare the prognostic value of complete blood count (CBC) parameters and CBC-derived inflammatory biomarkers for predicting all-cause and respiratory disease mortality in adults with asthma. Our findings demonstrated that among the CBC-derived inflammatory biomarkers, monocyte-to-lymphocyte ratio (MLR) had the highest prognostic value for both all-cause and respiratory disease mortality (Figures 3B, C). These results indicate that MLR is a strong predictor of mortality in this population and may have important clinical implications for risk stratification and disease management.
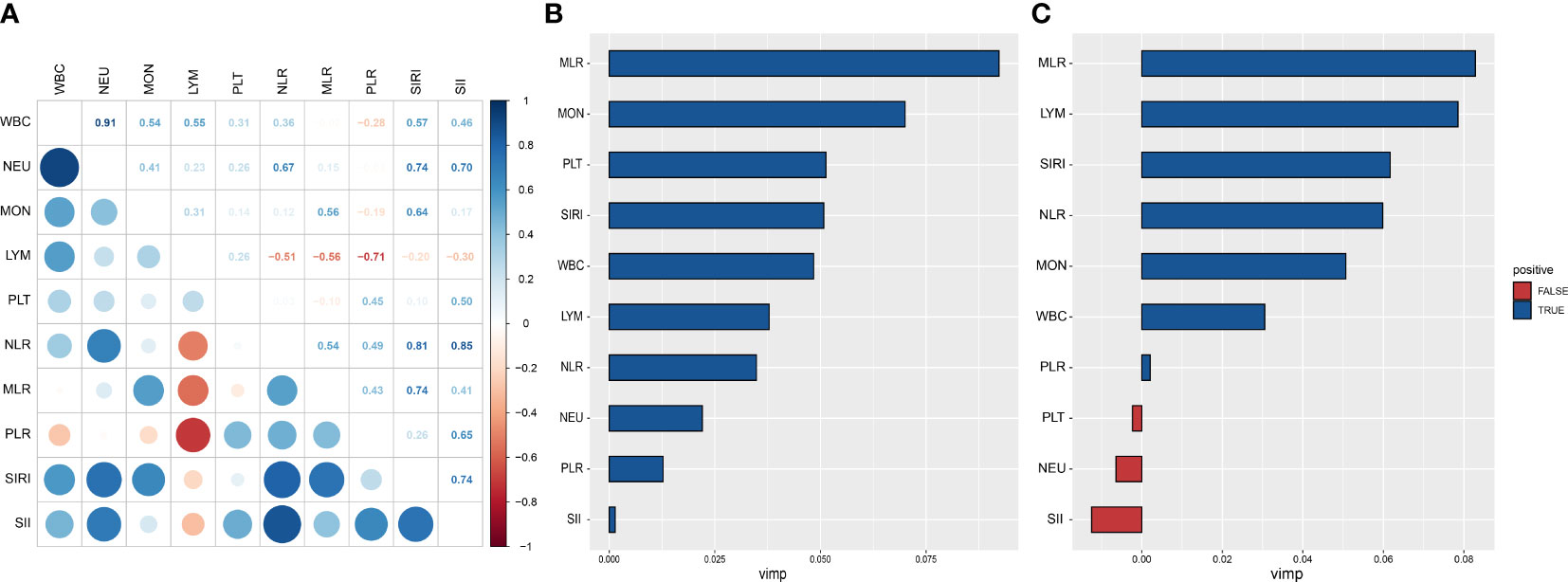
Figure 3 Prognostic value of complete blood cell count (CBC)-derived indicators. Spearman correlation analysis was used to calculate the correlation coefficients among CBC parameters and CBC-derived inflammatory biomarkers (A). A random subsistence forest method was used to compare the value of CBC parameters and CBC-derived inflammatory biomarkers in predicting all-cause (B) and respiratory disease (C) mortality in adults with asthma.
3.5 Stratified analysis
Table S4 presents the results of the comprehensive stratified analyses examining the associations between quartiles of CBC-derived inflammatory biomarkers levels and all-cause and respiratory disease mortality by smoking among adults with asthma. Stratified analysis revealed a significant association between higher levels of CBC-derived inflammatory biomarkers and increased risk of all-cause and respiratory disease mortality in both subgroups, the smoking and never-smoking groups. Thus, smoking status did not have a significant effect on the relationship between whole blood cell-derived inflammatory biomarkers and the risk of mortality (all P for interaction > 0.05).
3.6 Sensitivity analyses
In sensitivity analyses, we further adjusted the full model for anti-asthma medications as well as lung function parameters, and the results similarly showed that CBC-derived inflammatory markers were associated with all-cause mortality and respiratory disease mortality (Tables S5, S6). If participants with adult asthma who died during the first two years of follow-up were excluded, we observed similar results in the adjusted full model (Table S7). In addition, after participants with a history of cancer, HIV infection, or respiratory infection at baseline were also excluded from the study, a repeat COX regression similarly showed that higher CBC-derived inflammatory markers were associated with an increased risk of all-cause and respiratory disease mortality (Table S8). Finally, if we exclude participants with self-reported COPD at baseline from the study, the relationship remains (Table S9).
4 Discussion
We conducted a cross-sectional study of 48,305 adults to investigate the association between CBC-derived inflammatory biomarkers and the prevalence and mortality risk of asthma in the US population from 1999 to 2018. Our findings indicate that NLR, PLR, MLR, SIRI, and SII were positively associated with the prevalence of asthma in the population studied. We conducted a longitudinal cohort study of 6,403 individuals with asthma to investigate the association between CBC-derived inflammatory biomarkers and mortality risk. After adjusting for relevant confounding factors, we found that higher levels of NLR, MLR, SIRI, and SII were significantly associated with increased risk of all-cause and respiratory disease mortality in adults with asthma. Furthermore, our results from the random survival forest analysis demonstrated that MLR was the most predictive biomarker of mortality risk in this population. These findings suggest that CBC-derived inflammatory biomarkers, particularly MLR, may be useful clinical tools for assessing mortality risk in individuals with asthma. Overall, our study highlights the importance of considering the inflammatory status reflected by CBC-derived markers as an independent risk factor for all-cause and respiratory disease mortality in individuals with asthma.
Asthma is a chronic inflammatory disease of the airways involving multiple cells (eosinophils, neutrophils, lymphocytes, and macrophages) and cellular components (26, 27). In the past, many studies have focused on the role of eosinophils as blood biomarkers for asthma (28). Recently, CBC parameters are recommended as supplemental markers for asthma core outcome (29). In our study, the counts of WBC, neutrophils, monocyte were significantly associated with a higher prevalence of asthma. In addition, we found that neutrophils and monocyte were significantly associated with a higher risk of all-cause and respiratory disease mortality. Girdhar et al. (30) found that the total number of WBC in plasma was negatively correlated with lung function in asthma patients, which supported our view. Patients with asthma persistence were older and had higher levels of blood neutrophils as compared to patients who experienced clinical remission (31). Aberrant differentiation of monocytes and increased monocyte-derived TGF-β1 can identify severe asthma patients (32).
CBC-derived indicators are markers that reflect the immune and chronic inflammatory states of the body (33, 34), which have been studied in recent years (35, 36). The role of CBC-derived indicators in respiratory diseases has aroused strong interest among researchers. Citu et al. (37) identified elevated NLR and MLR as independent factors for poor clinical outcome of COVID-19. In agreement with previous studies (15, 38), Fois et al. (39) found increased values of NLR in severe COVID-19 disease patients. However, they also reported that other CBC-derived inflammation indexes, such as SII and SIRI are also significantly associated with disease severity. The patients with PLR, NLR, MLR, and SII above the cut-off had a survival probability of COVID-19 50% lower (14).
However, the role of CBC-derived indicators in the diagnosis and prognosis of asthma is not clear. A meta-analysis showed that the NLR values are a reasonable and easy-to-use marker for asthma and its exacerbations (40). Shi et al. showed that NLR, as a non-specific inflammatory index, can effectively diagnose patients with an acute attack of asthma and is related to the severity of the disease (41). Compared to lower SII levels, higher SII levels increased mortality risk in people with asthma (19). In our study, NLR, MLR, SIRI and SII were significantly associated with the prevalence of asthma and increased the risk of all-cause and respiratory disease mortality in patients with asthma. In addition, MLR was proved to be an independent predictor of prognosis in patients with asthma. MLR is calculated based on monocyte and lymphocyte counts, so an elevated MLR indicates an increase in monocytes. Studies have shown that monocytes promote inflammatory processes by differentiating into macrophages or dendritic cells, which can impair lung function and promote asthma (42–45). We speculate that increased MLR levels predict a poor outcome for asthma.
Our study revealed that among the five blood-derived inflammatory markers analyzed, the MLR emerged as the most valuable predictor of mortality in participants with asthma. Asthma, a chronic inflammatory disorder of the airways, is associated with complex immunological processes (46). MLR reflects the interplay between innate and adaptive immune responses (47–49). Elevated MLR levels have been shown to be indicative of increased systemic inflammation and immune dysregulation (50). In the context of asthma, MLR holds particular significance due to its potential role in capturing the dynamic balance between pro-inflammatory monocytes and anti-inflammatory lymphocytes. The higher MLR values observed in individuals who experience adverse outcomes suggest a skewed immune response towards a more pro-inflammatory state (51–53). This dysregulation in the MLR may contribute to the progression of inflammation, exacerbation of airway hyperresponsiveness, and ultimately, increased mortality risk in asthma patients (42–45). These findings highlight the relevance of MLR as a comprehensive inflammatory marker, encompassing both innate and adaptive immunity, and its potential to provide valuable insights into the underlying biological mechanisms contributing to asthma mortality.
Our study has several advantages compared to previous investigations. Firstly, our large sample size enabled us to detect significant associations between CBC-derived indicators and both the prevalence of asthma and mortality risk in participants. Secondly, we adjusted for several key confounding factors that may have affected our results, including personal habits, personal history, and socioeconomic status. Thirdly, CBC-derived indicators are composed of multiple CBC parameters, which may provide more comprehensive information than single indices, making them valuable tools in clinical settings for the management and treatment of asthma in adults. Lastly, we employed a robust analysis method, RSF, which overcomes the issue of high collinearity between inflammatory biomarkers and identified MLR as the most valuable predictor of all-cause and respiratory disease mortality in adults with asthma. Overall, our study provides novel insights into the prognostic value of CBC-derived indicators in asthma and has important implications for clinical management and future research in this field.
This study also has several limitations. First, the NHANES findings were based on the self-reports of the patients, which may lead to recall bias. Second, the results of the studies were adjusted for age, sex, smoking status, and other confounding factors, but there may be unknown confounding factors affecting the analyses. Third, we calculated CBC-derived indicators with one-time CBC parameters which might cause bias.
5 Conclusions
The findings of this study suggest that among adults with asthma, increased levels of NLR, PLR, SIRI, and SII are associated with higher risks of all-cause and respiratory disease mortality. The measurement of MLR may serve as a useful tool for identifying high-risk adults with asthma in a simple and cost-effective manner. These findings contribute to the growing body of evidence on the potential utility of these biomarkers in predicting asthma outcomes and may inform clinical decision-making in the management of asthma patients.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes.
Ethics statement
The studies involving human participants were reviewed and approved by The National Center for Health Statistics (NCHS) Research Ethics Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
The authors’ responsibilities were as follows—SW: designed the research, and had primary responsibility for the final content; JK: conducted analyses and wrote the first draft of the paper; FQ and WF: revised the manuscript; All authors contributed to the article and approved the submitted version.
Acknowledgments
We appreciate the people who contributed to the NHANES data we studied.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2023.1205687/full#supplementary-material
References
1. Mazurek JM, Syamlal G. Prevalence of asthma, asthma attacks, and emergency department visits for asthma among working adults - national health interview survey, 2011-2016. MMWR Morb Mortal Wkly Rep (2018) 67(13):377–86. doi: 10.15585/mmwr.mm6713a1
2. Fahy JV. Type 2 inflammation in asthma–present in most, absent in many. Nat Rev Immunol (2015) 15(1):57–65. doi: 10.1038/nri3786
3. Miller RL, Grayson MH, Strothman K. Advances in asthma: New understandings of asthma's natural history, risk factors, underlying mechanisms, and clinical management. J Allergy Clin Immunol (2021) 148(6):1430–41. doi: 10.1016/j.jaci.2021.10.001
4. Cazzola M, Rogliani P, Ora J, Calzetta L, Matera MG. Asthma and comorbidities: recent advances. Pol Arch Intern Med (2022) 132(4):16250. doi: 10.20452/pamw.16250
5. Nygaard UC, Xiao L, Nadeau KC, Hew KM, Lv N, Camargo CA, et al. Improved diet quality is associated with decreased concentrations of inflammatory markers in adults with uncontrolled asthma. Am J Clin Nutr (2021) 114(3):1012–27. doi: 10.1093/ajcn/nqab063
6. Chen F, Yu M, Zhong Y, Hua W, Huang H. The role of neutrophils in asthma. Zhejiang Da Xue Xue Bao Yi Xue Ban (2021) 50(1):123–30. doi: 10.3724/zdxbyxb-2021-0030
7. Burke LA, Wilkinson JR, Howell CJ, Lee TH. Interactions of macrophages and monocytes with granulocytes in asthma. Eur Respir J Suppl (1991) 13:85s–90s.
8. Huang C, Li F, Wang J, Tian Z. Innate-like lymphocytes and innate lymphoid cells in asthma. Clin Rev Allergy Immunol (2020) 59(3):359–70. doi: 10.1007/s12016-019-08773-6
9. Tillie-Leblond I, Montani D, Crestani B, de Blic J, Humbert M, Tunon-de-Lara M, et al. Relation between inflammation and symptoms in asthma. Allergy (2009) 64(3):354–67. doi: 10.1111/j.1398-9995.2009.01971.x
10. Fatemi F, Sadroddiny E, Gheibi A, Mohammadi Farsani T, Kardar GA. Biomolecular markers in assessment and treatment of asthma. Respirology (2014) 19(4):514–23. doi: 10.1111/resp.12284
11. Tartibi HM, Bahna SL. Clinical and biological markers of asthma control. Expert Rev Clin Immunol (2014) 10(11):1453–61. doi: 10.1586/1744666X.2014.962516
12. Shoji F, Kozuma Y, Toyokawa G, Yamazaki K, Takeo S. Complete blood cell count-derived inflammatory biomarkers in early-stage non-small-cell lung cancer. Ann Thorac Cardiovasc Surg (2020) 26(5):248–55. doi: 10.5761/atcs.oa.19-00315
13. Zhou D, Yang H, Zeng L, Yang W, Guo F, Cui W, et al. Calculated inflammatory markers derived from complete blood count results, along with routine laboratory and clinical data, predict treatment failure of acute peritonitis in chronic peritoneal dialysis patients. Ren Fail (2023) 45(1):2179856. doi: 10.1080/0886022X.2023.2179856
14. Gutierrez-Perez IA, Buendia-Roldan I, Perez-Rubio G, Chavez-Galan L, Hernandez-Zenteno RJ, Aguilar-Duran H, et al. Outcome predictors in COVID-19: An analysis of emergent systemic inflammation indices in Mexican population. Front Med (Lausanne) (2022) 9:1000147. doi: 10.3389/fmed.2022.1000147
15. Ghobadi H, Mohammadshahi J, Javaheri N, Fouladi N, Mirzazadeh Y, Aslani MR. Role of leukocytes and systemic inflammation indexes (NLR, PLR, MLP, dNLR, NLPR, AISI, SIR-I, and SII) on admission predicts in-hospital mortality in non-elderly and elderly COVID-19 patients. Front Med (Lausanne) (2022) 9:916453. doi: 10.3389/fmed.2022.916453
16. Kuikel S, Pathak N, Poudel S, Thapa S, Bhattarai SL, Chaudhary G, et al. Neutrophil-lymphocyte ratio as a predictor of adverse outcome in patients with community-acquired pneumonia: A systematic review. Health Sci Rep (2022) 5(3):e630. doi: 10.1002/hsr2.630
17. Zinellu A, Zinellu E, Mangoni AA, Pau MC, Carru C, Pirina P, et al. Clinical significance of the neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in acute exacerbations of COPD: present and future. Eur Respir Rev (2022) 31(166):220095. doi: 10.1183/16000617.0095-2022
18. Zinellu A, Zinellu E, Pau MC, Carru C, Pirina P, Fois AG, et al. A comprehensive systematic review and meta-analysis of the association between the neutrophil-to-lymphocyte ratio and adverse outcomes in patients with acute exacerbation of chronic obstructive pulmonary disease. J Clin Med (2022) 11(12):3365. doi: 10.3390/jcm11123365
19. Benz E, Wijnant SRA, Trajanoska K, Arinze JT, de Roos EW, de Ridder M, et al. Sarcopenia, systemic immune-inflammation index and all-cause mortality in middle-aged and older people with COPD and asthma: a population-based study. ERJ Open Res (2022) 8(1):00628–2021. doi: 10.1183/23120541.00628-2021
20. Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National health and nutrition examination survey: plan and operations, 1999-2010. Vital Health Stat 1 (2013) 56):1–37.
21. Li Z, Shi P, Chen Z, Zhang W, Lin S, Zheng T, et al. The association between ethylene oxide exposure and asthma risk: a population-based study. Environ Sci pollut Res Int (2023) 30(9):24154–67. doi: 10.1007/s11356-022-23782-3
23. Qiu Z, Chen X, Geng T, Wan Z, Lu Q, Li L, et al. Associations of serum carotenoids with risk of cardiovascular mortality among individuals with type 2 diabetes: results from NHANES. Diabetes Care (2022) 45(6):1453–61. doi: 10.2337/dc21-2371
24. Beddhu S, Baird BC, Zitterkoph J, Neilson J, Greene T. Physical activity and mortality in chronic kidney disease (NHANES III). Clin J Am Soc Nephrol (2009) 4(12):1901–6. doi: 10.2215/CJN.01970309
25. Zhu X, Cheang I, Tang Y, Shi M, Zhu Q, Gao R, et al. Associations of serum carotenoids with risk of all-cause and cardiovascular mortality in hypertensive adults. J Am Heart Assoc (2023) 12(4):e027568. doi: 10.1161/jaha.122.027568
26. Durack J, Boushey HA, Lynch SV. Airway microbiota and the implications of dysbiosis in asthma. Curr Allergy Asthma Rep (2016) 16(8):52. doi: 10.1007/s11882-016-0631-8
27. Alobaidi AH, Alsamarai AM, Alsamarai MA. Inflammation in asthma pathogenesis: role of T cells, macrophages, epithelial cells and type 2 inflammation. Antiinflamm Antiallergy Agents Med Chem (2021) 20(4):317–32. doi: 10.2174/1871523020666210920100707
28. Tupper OD, Hakansson KEJ, Ulrik CS. Remission and changes in severity over 30 years in an adult asthma cohort. J Allergy Clin Immunol Pract (2021) 9(4):1595–1603 e1595. doi: 10.1016/j.jaip.2020.11.013
29. Szefler SJ, Wenzel S, Brown R, Erzurum SC, Fahy JV, Hamilton RG, et al. Asthma outcomes: biomarkers. J Allergy Clin Immunol (2012) 129(3 Suppl):S9–23. doi: 10.1016/j.jaci.2011.12.979
30. Girdhar A, Kumar V, Singh A, Menon B, Vijayan VK. Systemic inflammation and its response to treatment in patients with asthma. Respir Care (2011) 56(6):800–5. doi: 10.4187/respcare.00601
31. Westerhof GA, Coumou H, de Nijs SB, Weersink EJ, Bel EH. Clinical predictors of remission and persistence of adult-onset asthma. J Allergy Clin Immunol (2018) 141(1):104–109 e103. doi: 10.1016/j.jaci.2017.03.034
32. Hung CH, Wang CC, Suen JL, Sheu CC, Kuo CH, Liao WT, et al. et al: Altered pattern of monocyte differentiation and monocyte-derived TGF-beta1 in severe asthma. Sci Rep (2018) 8(1):919. doi: 10.1038/s41598-017-19105-z
33. Xing Y, Tian Z, Jiang Y, Guan G, Niu Q, Sun X, et al. A practical nomogram based on systemic inflammatory markers for predicting portal vein thrombosis in patients with liver cirrhosis. Ann Med (2022) 54(1):302–9. doi: 10.1080/07853890.2022.2028893
34. Li Q, Ma X, Shao Q, Yang Z, Wang Y, Gao F, et al. Prognostic impact of multiple lymphocyte-based inflammatory indices in acute coronary syndrome patients. Front Cardiovasc Med (2022) 9:811790. doi: 10.3389/fcvm.2022.811790
35. Halmaciu I, Arbanasi EM, Kaller R, Muresan AV, Arbanasi EM, Bacalbasa N, et al. Chest CT severity score and systemic inflammatory biomarkers as predictors of the need for invasive mechanical ventilation and of COVID-19 patients' Mortality. Diagnostics (Basel) (2022) 12(9):2089. doi: 10.3390/diagnostics12092089
36. He P, Yang H, Lai Q, Kuang Y, Huang Z, Liang X, et al. The diagnostic value of blood cell-derived indexes in subacute thyroiditis patients with thyrotoxicosis: a retrospective study. Ann Transl Med (2022) 10(6):322. doi: 10.21037/atm-22-719
37. Citu C, Gorun F, Motoc A, Sas I, Gorun OM, Burlea B, et al. The predictive role of NLR, d-NLR, MLR, and SIRI in COVID-19 mortality. Diagnostics (Basel) (2022) 12(1):122. doi: 10.3390/diagnostics12010122
38. Chen L, Yu J, He W, Chen L, Yuan G, Dong F, et al. Risk factors for death in 1859 subjects with COVID-19. Leukemia (2020) 34(8):2173–83. doi: 10.1038/s41375-020-0911-0
39. Fois AG, Paliogiannis P, Scano V, Cau S, Babudieri S, Perra R, et al. The systemic inflammation index on admission predicts in-Hospital mortality in COVID-19 patients. Molecules (2020) 25(23):5725. doi: 10.3390/molecules25235725
40. Huang WJ, Huang GT, Zhan QM, Chen JL, Luo WT, Wu LH, et al. The neutrophil to lymphocyte ratio as a novel predictor of asthma and its exacerbation: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci (2020) 24(22):11719–28. doi: 10.26355/eurrev_202011_23819
41. Shi G, Zhao JW, Ming L. [Clinical significance of peripheral blood neutrophil-lymphocyte ratio and platelet- lymphocyte ratio in patients with asthma]. Nan Fang Yi Ke Da Xue Xue Bao (2017) 37(1):84–8. doi: 10.3969/j.issn.1673-4254.2017.01.15
42. Rastogi D, Fraser S, Oh J, Huber AM, Schulman Y, Bhagtani RH, et al. Inflammation, metabolic dysregulation, and pulmonary function among obese urban adolescents with asthma. Am J Respir Crit Care Med (2015) 191(2):149–60. doi: 10.1164/rccm.201409-1587OC
43. Paplinska-Goryca M, Misiukiewicz-Stepien P, Proboszcz M, Nejman-Gryz P, Gorska K, Krenke R. The expressions of TSLP, IL-33, and IL-17A in monocyte derived dendritic cells from asthma and COPD patients are related to epithelial-macrophage interactions. Cells (2020) 9(9):1944. doi: 10.3390/cells9091944
44. Zhang M, Yu Q, Tang W, Wu Y, Lv J, Sun L, et al. Epithelial exosomal contactin-1 promotes monocyte-derived dendritic cell-dominant T-cell responses in asthma. J Allergy Clin Immunol (2021) 148(6):1545–58. doi: 10.1016/j.jaci.2021.04.025
45. Han P, Chen L, Chen D, Yang R, Wang W, Liu J, et al. Upregulated expression of substance P and NK1R in blood monocytes and B cells of patients with allergic rhinitis and asthma. Clin Exp Immunol (2022) 210(1):39–52. doi: 10.1093/cei/uxac074
46. Hammad H, Lambrecht BN. The basic immunology of asthma. Cell (2021) 184(6):1469–85. doi: 10.1016/j.cell.2021.02.016
47. Iwasaki A, Medzhitov R. Regulation of adaptive immunity by the innate immune system. Science (2010) 327(5963):291–5. doi: 10.1126/science.1183021
48. León B, Ardavín C. Monocyte-derived dendritic cells in innate and adaptive immunity. Immunol Cell Biol (2008) 86(4):320–4. doi: 10.1038/icb.2008.14
49. Harms AS, Ferreira SA, Romero-Ramos M. Periphery and brain, innate and adaptive immunity in Parkinson's disease. Acta Neuropathol (2021) 141(4):527–45. doi: 10.1007/s00401-021-02268-5
50. Nagy N, Kuipers HF, Marshall PL, Wang E, Kaber G, Bollyky PL. Hyaluronan in immune dysregulation and autoimmune diseases. Matrix Biol (2019) 78-79:292–313. doi: 10.1016/j.matbio.2018.03.022
51. Hua Y, Sun JY, Lou YX, Sun W, Kong XQ. Monocyte-to-lymphocyte ratio predicts mortality and cardiovascular mortality in the general population. Int J Cardiol (2023) 379:118–26. doi: 10.1016/j.ijcard.2023.03.016
52. Cheang I, Zhu X, Lu X, Yue X, Tang Y, Gao R, et al. Associations of inflammation with risk of cardiovascular and all-Cause mortality in adults with hypertension: an inflammatory prognostic scoring system. J Inflammation Res (2022) 15:6125–36. doi: 10.2147/JIR.S384977
Keywords: CBC-derived inflammatory biomarkers, asthma, mortality, RSF, NHANES
Citation: Ke J, Qiu F, Fan W and Wei S (2023) Associations of complete blood cell count-derived inflammatory biomarkers with asthma and mortality in adults: a population-based study. Front. Immunol. 14:1205687. doi: 10.3389/fimmu.2023.1205687
Received: 14 April 2023; Accepted: 12 July 2023;
Published: 28 July 2023.
Edited by:
Naveena Yanamala, Rutgers, The State University of New Jersey, United StatesReviewed by:
Giuseppe Spadaro, University of Naples Federico II, ItalyAayush Visaria, Rutgers, The State University of New Jersey, United States
Copyright © 2023 Ke, Qiu, Fan and Wei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Songqing Wei, d3NxNjA2QDE2My5jb20=
 Junhua Ke
Junhua Ke Fushan Qiu1
Fushan Qiu1 Songqing Wei
Songqing Wei