
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Immunol., 22 February 2023
Sec. Nutritional Immunology
Volume 14 - 2023 | https://doi.org/10.3389/fimmu.2023.1126457
This article is part of the Research TopicDietary Habits, Microbiota and Autoimmune DiseasesView all 7 articles
Background: Previous research has found a link between dietary factors and asthma. However, few studies have analyzed the relationship between dietary factors and asthma using Mendelian randomization. Methods: The IEU Open GWAS project (https://gwas.mrcieu.ac.uk/) was the source of exposure and outcome datasets. The exposure datasets included Alcoholic drinks per week, Alcohol intake frequency, Processed meat intake, Poultry intake, Beef intake, Non-oily fish intake, Oily fish intake, Pork intake, Lamb/mutton intake, Bread intake, Cheese intake, Cooked vegetable intake, Tea intake, Fresh fruit intake, Cereal intake, Salad/raw vegetable intake, Coffee intake, and Dried fruit intake. The weighted median, MR-Egger, and Inverse Variance Weighted methods were used as the main methods of Mendelian randomization analysis. Heterogeneity and pleiotropic analysis were performed to ensure the accuracy of the results.
Results: Alcohol intake frequency (after removing outliers OR: 1.217; 95% CI: 1.048-1.413; p=0.00993) was related to an increased risk of Asthma. Fresh fruit intake (OR: 0.489; 95% CI: 0.320-0.748; p=0.000954) and Dried fruit intake (after removing outliers OR: 0.482; 95% CI: 0.325-0.717; p= 0.000312) were discovered as protective factors. Other dietary intakes found no causal relationship with asthma.
Conclusion: This study found that dried fruit intake and fresh fruit intake were associated with a reduced risk of asthma, and alcohol intake frequency was associated with an increased risk of asthma. This study also found that other factors included in this study were not associated with asthma.
As a common chronic disease, asthma is a major health problem worldwide (1). The incidence of asthma has increased rapidly over the past few decades (2–4). The goal of asthma treatment is to minimize both symptoms and the risk of adverse outcomes (5). The increase in asthmatic patients has increased the medical burden worldwide. In Western countries, the financial burden for an individual asthma patient ranges from US$300 to US$1,300 per year (6). Asthma patients in developing countries face both a financial burden and a higher risk of adverse outcomes due to appropriate treatment is deficient. Dietary factors may play an important role in this increase in asthma (7). In adults, the causes of asthma include environmental and lifestyle factors. A previous study has reported the critical role of diet in the development of allergic diseases (8). Dietary factors may be directly related to asthma pathogenesis (9). Knowing whether dietary changes benefit patients with asthma has important implications for both clinicians and patients with asthma. Previous studies have found that alcohol intake (10), fruit intake (11), vegetable intake (12), dairy intake (13), fish intake (14), and meat intake (15) were associated with asthma or asthma symptoms. Mendelian randomization (MR) uses genetic variants as instrumental variables (IVs), which has advantages over other research methods (16). However, there are few MR studies on the causal relationships between dietary factors and asthma. We, therefore, performed this MR analysis to explore the relationships between dietary factors and asthma.
The following basic assumptions constitute the premise of MR analysis. First, IVs must be intensely associated with the exposure factor(s). Second, IVs cannot be directly correlated to the outcome. Third, IVs were not related to any potential confounding factors. The GWAS summary-level data used in this study was issued by the IEU open GWAS project. This project, supported by the MRC Integrative Epidemiology Unit (IEU) at the University of Bristol, collated and analyzed GWAS data from UK Biobank, published articles, and FinnGen biobank. This study was exempt from the approval of the Ethical Review Authority because the data used in this study was public, anonymized, and de-identified.
Diet-Related Exposure factors used in this study included vegetable intake (Salad/raw vegetable intake and Cooked vegetable intake), meat intake (Processed meat intake, Poultry intake, Beef intake, Non-oily fish intake, Oily fish intake, Pork intake, and Lamb/mutton intake), staple food intake (Bread intake and Cereal intake), beverage intake (Alcoholic drinks per week, Alcohol intake frequency, Tea intake, and Coffee intake), fruit intake(Dried fruit intake and Fresh fruit intake), and another food intake (Cheese intake). These GWAS summary-level data were extracted directly or indirectly from UK Biobank by the IEU open GWAS project. The GWAS summary-level data of asthma was extracted from FinnGen biobank by the IEU open GWAS project. We did not use proxy SNPs when finding SNPs from the outcome, mainly because the FinnGen biobank contained enough SNPs (16,380,176 SNPs in the dataset of asthma). More information about the exposure and outcome datasets is presented in Table 1 and Supplementary Table 1.
In MR analysis, IVs were utilized as mediators between exposure factors and outcomes to explore the causal relationship between exposure and outcomes. IVs are generally genetic variations, among which Single nucleotide polymorphisms (SNPs) are the most commonly used. SNPs associated with dietary factors were extracted from the IEU open GWAS project (https://gwas.mrcieu.ac.uk/). we screened the SNPs intensely related with exposures at the genome-wide significance level (p < 5×10–8), clumping window > 10,000 kb, and the linkage disequilibrium level (r2 < 0.001). More information is shown in Table 1. The F statistic was used to ensure the strong association between IVs and exposure, The F statistic greater than 10 was generally considered to meet the requirements of strong association (17).
We conducted the inverse variance weighted (IVW) method as the primary method for calculating the causal effect. The IVW model is the method with the strongest ability to detect causation in the two-sample MR analysis (18). We contrasted the consequences of the IVW method with the weighted median and the MR-Egger methods. The weighted median method allows no more than 50% of invalid IVs, and the MR-Egger method allows all IVs to be voided. Therefore, it will be more convincing when the three models are consistent. The heterogeneity of the IVW model was assessed by Cochran’s Q test. Cochran’s Q-test p<0.05 indicated heterogeneity. However, the existence of heterogeneity does not mean that the IVW model is necessarily invalid. The MR-Egger method allows for the existence of non-zero intercepts and was used to detect directional pleiotropy. Leave-one-out analysis was performed to assess whether there was a significant effect on the results after the removal of a single SNP. We use the MR-PRESSO method to detect outliers. Once outliers were found, they will be removed immediately. After removing outliers, the MR analysis will be performed again. All analyses were performed in R software (version 4.2.0) using the TwoSampleMR package (19).
The causal relationship between dietary factors and asthma were analyzed using 18 different exposure factors. The amounts of SNPs used in this study ranged from 7 to 92. The F-statistics are all greater than 10 (range: 15.502 to 112.254). The number of European-descent individuals included in the exposures ranged from 335,394 to 462,346. The outcome included 20 629 European-descent asthma cases and 135 449 European-descent controls from the FinnGen biobank, and there was little overlap between the populations involved in exposures and outcome. See Table 1 for more information on exposures and results. The number of SNPs used for different exposures in this study ranged from 7 to 92, and the range after removing outliers was between 5 and 90 (the number of outliers found in different exposures ranged from 0 to 2). See Table 2 for more information. As shown in Table 1, the F statistic (after removing outliers) ranges from 15.502 to 112.254, which indicates that IVs used in our study satisfies the requirements of strong association with exposures.
In this study, a total of 3 causalities were identified (p < 0.05 by IVW method). We found that alcohol intake frequency (after removing outliers OR: 1.217; 95% CI: 1.048-1.413; p=0.00993) was related to an increased risk of Asthma. This discovery was further verified by the consequences of the MR-Egger (after removing outliers OR: 1.624; 95% CI: 1.010-2.610; p= 0.0483) and weighted median (after removing outliers OR: 1.270; 95% CI: 1.046-1.542; p=0.0157) model. Fresh fruit intake (OR: 0.489; 95% CI: 0.320-0.748; p=0.000954) and Dried fruit intake (after removing outliers OR: 0.482; 95% CI: 0.325-0.717; p= 0.000312) were discovered as protective factors. And we have reached the same conclusion in the Weighted median model (Fresh fruit intake OR: 0.462; 95% CI: 0.255-0.838; p=0.011; Dried fruit intake OR: 0.477; 95% CI: 0.284-0.801; p=0.0051). However, there were no significant results in the MR-Egger model (P>0.05). Cereal intake showed a positive result before the outliers were not removed, and the positive result disappeared after the outlier was removed (P= 0.0256 VS 0.0508). This study also found that Alcoholic drinks per week (OR: 0.903; 95% CI: 0.599-1.359; p=0.624; Outliers excluded: OR:0.804; 95% CI:0.577-1.120; p=0.196), Processed meat intake (OR: 1.315; 95% CI: 0.797-2.168; p=0.284; Outliers excluded: OR:1.136; 95% CI:0.721-1.790; p=0.583), Poultry intake (OR: 1.101; 95% CI: 0.151-8.051; p= 0.924; Outliers excluded: OR:1.827; 95% CI:0.565-5.906; p=0.314), Beef intake (OR: 0.807; 95% CI: 0.307-2.124; p= 0.664; Outliers excluded: OR:0.479; 95% CI:0.227-1.012; p=0.0538), Non-oily fish intake (OR: 0.957; 95% CI: 0.302-3.029; p= 0.940; Outliers excluded: OR:0.648; 95% CI:0.219-1.923; p=0.435), Oily fish intake (OR: 0.739; 95% CI: 0.501-1.091; p= 0.128; Outliers excluded: OR:0.751; 95% CI:0.543-1.038; p=0.0831), Pork intake (OR: 1.287; 95% CI: 0.429-3.863; p= 0.653; Outliers excluded: OR:1.225; 95% CI:0.498-3.013; p=0.658), and Lamb/mutton intake (OR: 1.127; 95% CI: 0.564-2.251; p= 0.735; Outliers excluded: OR:0.875; 95% CI:0.454-1.687; p=0.691), Bread intake(OR: 0.942; 95% CI: 0.615-1.442; p= 0.784; No outliers), Cheese intake(OR: 0.876; 95% CI: 0.678-1.132; p= 0.310; No outliers), Cooked vegetable intake(OR: 1.230; 95% CI: 0.558-2.710; p= 0.607; Outliers excluded: OR:0.982; 95% CI:0.475-2.031; p= 0.962), Tea intake(OR: 0.827; 95% CI: 0.621-1.101; p= 0.192; Outliers excluded: OR:0.793; 95% CI:0.608-1.034; p=0.0865), Salad/raw vegetable intake(OR: 0.810; 95% CI: 0.287-2.284; p= 0.691; Outliers excluded: OR:1.026; 95% CI:0.396-2.660; p=0.957), and Coffee intake(OR: 0.947; 95% CI: 0.676-1.328; p= 0.754; No outliers) were not associated with asthma either before or after exclusion of outliers. More MR analysis results are in Table 2. Although heterogeneity was discovered in a considerable number of exposures (Cochrane’s Q test P<0.05), the consequences of the MR-Egger intercept suggested that no directional pleiotropy was discovered (Table 2). Leave-one-out analysis indicated that the causalities of the positive results were very robust (Figure 1). As shown in Table 2, the results of the MR-PRESSO analysis were greatly consistent with the results of the IVW model (causal relationships were only shown in Alcohol intake frequency, Fresh fruit intake, and Dried fruit intake).
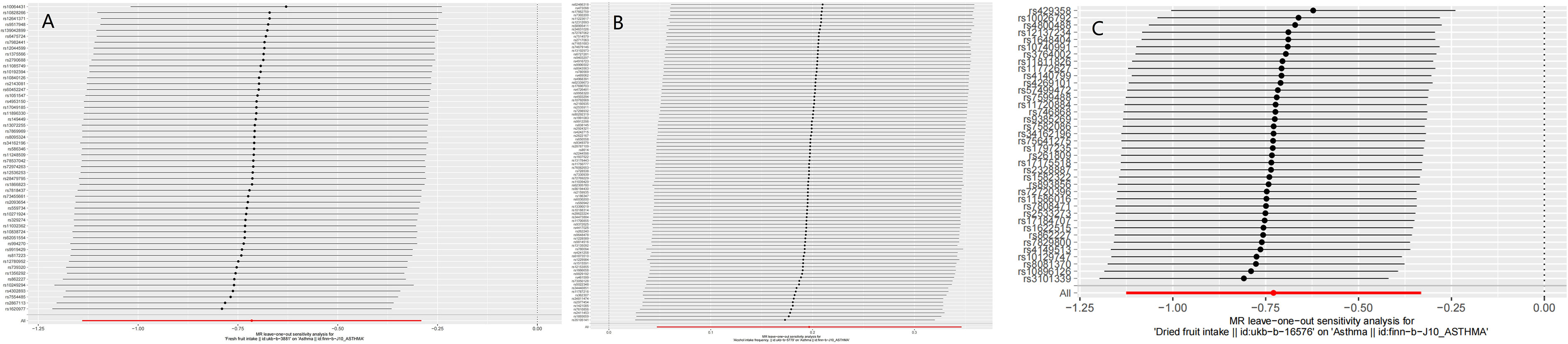
Figure 1 The results of Leave-one-out analyses (A) Fresh fruit intake (B) Alcohol intake frequency (C) Dried fruit intake.
The most important finding of this MR analysis is that Alcohol intake frequency, Fresh fruit intake, and Dried fruit intake were associated with asthma. Other findings are also noteworthy. First of all, a causal relationship between Cereal intake and asthma cannot be completely ruled out. In our analysis, if there were any outliers, we repeated the MR analysis and used the new results of the IVW model as a basis for determining whether there was a causal relationship. When we analyzed whether there was a causal relationship between grain intake and asthma, we found no causal relationship after excluding outliers (OR: 0.671; 95% CI: 0.450-1.001; p=0.0508). And a causal relationship was shown in the IVW model (OR: 0.617; 95% CI: 0.404-0.943; p= 0.0256) and the weighted median model (OR: 0.607; 95% CI: 0.373-0.987; p= 0.0442) before excluding outliers. We, therefore, think that the 95% confidence intervals and p-values at critical value have limited convincing power. Secondly, Alcoholic drinks per week, meat intake (Processed meat intake, Poultry intake, Beef intake, Non-oily fish intake, Oily fish intake, Pork intake, and Lamb/mutton intake), Bread intake, Cheese intake, Cooked vegetable intake, Tea intake, Salad/raw vegetable intake, and Coffee intake were not associated with asthma. To our knowledge, there have been many MR studies on the risk or protective factors of asthma (20, 21). However, there are few studies involving meat intake, staple food intake, fruit and vegetable intake, and beverage intake. Asthma imposes a heavy economic burden on the world every year. Asthma and asthma complications also seriously affect the quality of life of patients with asthma. The conclusions of our study can help clinicians to improve their health education for patients with asthma, and encourage patients with asthma to change their eating habits (such as reducing the frequency of alcohol intake and increasing fruit intake). For those at high risk for asthma, adjusting dietary habits also reduces the risk of developing asthma. Therefore, this study has important implications for deepening the understanding of the risk and protective factors of asthma.
Alcohol can affect the human immune system (22, 23). Numerous studies have shown that heavy drinking is associated with higher immunoglobulin E (IgE) levels (24–26). Alcohol consumption is also associated with the development of allergic diseases, such as allergic rhinitis and atopic dermatitis (27, 28). A prospective study found a U-shaped association between alcohol consumption and the risk of asthma, with moderate alcohol consumption having the lowest asthma risk (10). However, Mendelian randomization analysis did not find a causal relationship between alcohol intake and asthma (29, 30). Unlike observational studies, MR studies using genetic variations (primarily SNPs) as instrumental variables are immune to confounding factors and reverse causality. This study found no causality between Alcoholic drinks per week and asthma, however, there was a causal relationship between the frequency of alcohol intake and asthma. We believe that the possible reasons for the differences between MR studies and observational studies in the relationship between alcohol intake and asthma are as follows: First, although possible confounding factors have been adjusted, observational studies may still be affected by other confounding factors. Second, there is indeed a U-shaped association between alcohol intake and asthma, which was not detected by the MR study. Therefore, more observational studies and more ingenious MR studies are needed in the future to further reveal the relationship between alcohol intake and asthma. Our study indicated that there may indeed be a causal relationship between alcohol intake and asthma, and this causal relationship is more about the frequency of alcohol intake than the amount of alcohol intake.
The airway is particularly vulnerable to oxidative damage. In experiments, oxidants can induce many symptoms of asthma by inducing the release of pro-inflammatory mediators including cytokines and chemokines (31). Vegetables and fruits contain many antioxidants. Studies in children showed that asthma symptoms were inversely correlated with fish, vegetable, and fruit intake (14, 32). Several studies in adults have linked high fruit and vegetable intake to a lower risk of asthma (33–36). However, not all studies have shown an association between vegetable intake and asthma. However, not all studies have shown an association between vegetable intake and asthma. A study found no association between vegetable intake and asthma (37). This study used the MR analysis method to find a causal relationship between fruit intake and asthma, but not vegetable intake. There have been many studies on the relationship between fish intake and asthma (38–41). Most of these studies supported an association between fish intake and a reduced risk of asthma (38–41). A Japanese study found that the risk of childhood asthma increased with the frequency of fish intake (42). However, our study showed no causal relationship between fish intake (including Oily fish intake and Non-oily fish intake) and asthma. This study provides powerful new evidence for insights into the relationship between fish intake and asthma. A study from Singapore suggested that a diet rich in meats may increase the risk of cough with phlegm (15). A study from Australia found a positive association between meat/cheese intake, poultry/seafood intake and asthma or hayfever (43). However, this study found no causal relationship between either meat intake or poultry intake and asthma. A study from South Korea found coffee intake had a protective effect on asthma (44). A prospective cohort study from the UK Biobank has found that coffee and tea intake may be protective against asthma (45). This study found coffee and tea intake were not associated with asthma. We must correctly understand the relationship between MR and randomized controlled trials (RCTs). On the one hand, MR can effectively overcome the bias caused by confounding (16). on the other hand, As a powerful supplement to randomized controlled trials, MR is not a substitute for RCTs. Therefore, this conclusion must be viewed with caution.
The mechanisms by which dietary factors affect asthma are not fully understood. Antioxidants and lipids may play an important role (46). Another possible pathway is through the gut microbiome. The intake of different foods can affect the composition of bacteria in the gut, which will affect the metabolism of nutrients (47, 48). A link between changes in the gut microbiome and improvements in airway hyperresponsiveness was found in a mouse model (49).
Although this MR analysis suggested associations between Fresh fruit intake, Dried fruit intake, and alcohol intake and asthma, the MR analysis should be interpreted with more caution. First, the causality found by the MR analysis reflected the effects of long-term exposure to associated factors. Therefore, short-term exposures may not be of clinical significance. Second, another notable problem is that MR cannot distinguish causal relationships between different periods. For example, an MR study found a causality between vitamin D and multiple sclerosis (50). However, this effect was only present in childhood or earlier (51). Third, Univariate MR analyses revealed only overall effects between exposures and outcomes, not direct effects between them. There can be extremely complex mechanisms between exposures and outcomes.
This study has some strengths and limitations. MR uses genetic variation as IVs to infer the causality, which can effectively overcome the bias caused by reverse causality and confounding (16). In order to ensure the accuracy of MR analysis, we performed sensitivity and pleiotropic analysis. We used European populations from different countries in exposures and outcome to avoid unnecessary bias. Of course, the limitations of this study cannot be ignored. First, the F-statistics indicated that the IVs used in this study satisfied the requirement of strong associations with exposure (F-statistics>10). however, a considerable part of the F-statistics is lower than 100, so this may affect the accuracy of the consequences. Second, we cannot further subdivide different types of dietary intake, nor can we distinguish the effects of different dietary combinations. Third, we were unable to conduct a sex-stratified analysis due to the lack of summary-level GWAS data for different sexes.
This study found that dried fruit intake and fresh fruit intake were associated with a reduced risk of asthma, and alcohol intake frequency was associated with an increased risk of asthma. This study also found that alcoholic drinks per week, processed meat intake, poultry intake, beef intake, non-oily fish intake, oily fish intake, pork intake, lamb/mutton intake, bread intake, cheese intake, cooked vegetable intake, tea intake, cereal intake, salad/raw vegetable intake, and coffee intake were not associated with asthma.
Publicly available datasets were analyzed in this study. This data can be found here: All GWAS data used in this study are available in the IEU open GWAS project (https://gwas.mrcieu.ac.uk/).
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent was not provided because All GWAS data used in this study are available in the IEU open GWAS project (https://gwas.mrcieu.ac.uk/). This study was exempt from the approval of the Ethical Review Authority because the data used in this study was public, anonymized, and de-identified.
The study was designed by WY and BH. Statistical analyses were performed by WY, LH, MZ, SS, FW and YY. The manuscript was written by WY and YY. All authors contributed to the interpretation of data and commented on the manuscript. All authors read and approved the manuscript. All authors contributed to the article and approved the submitted version.
Supported by Natural Science Foundation of Gansu Province (21JR1RA118) and Gansu Provincial Youth Science and Technology Fund (21JR1RA107, 18JR3RA305).
Special thanks to the IEU open GWAS project developed by The MRC Integrative Epidemiology Unit (IEU) at the University of Bristol. Thank them for extracting relevant GWAS summary-level data from published articles, UK Biobank, and FinnGen biobank.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2023.1126457/full#supplementary-material
1. Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet (2006) 368(9537):733–43. doi: 10.1016/S0140-6736(06)69283-0
2. Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National surveillance of asthma: United states, 2001-2010. In: Vital & health statistics. series 3, analytical and epidemiological studies (2012) (Hyattsville, Maryland: National Center for Health Statistics), vol. 2012. . p. 1–58 Available at: https://www.cdc.gov/nchs/data/series/sr_03/sr03_035.pdf.
3. Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. Trends in asthma prevalence, health care use, and mortality in the united states, 2001-2010. In: NCHS data brief (2012(94) (Hyattsville, Maryland: National Center for Health Statistics). p. 1–8.
4. Stern J, Pier J, Litonjua AA. Asthma epidemiology and risk factors. Semin immunopathology. (2020) 42(1):5–15. doi: 10.1007/s00281-020-00785-1
5. Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet (2018) 391(10122):783–800. doi: 10.1016/S0140-6736(17)33311-1
6. Braman SS. The global burden of asthma. Chest (2006) 130(1 Suppl):4s–12s. doi: 10.1378/chest.130.1_suppl.4S
7. Seaton A, Godden DJ, Brown K. Increase in asthma: a more toxic environment or a more susceptible population? Thorax (1994) 49(2):171–4. doi: 10.1136/thx.49.2.171
8. Julia V, Macia L, Dombrowicz D. The impact of diet on asthma and allergic diseases. Nat Rev Immunol (2015) 15(5):308–22. doi: 10.1038/nri3830
9. Guo CH, Liu PJ, Lin KP, Chen PC. Nutritional supplement therapy improves oxidative stress, immune response, pulmonary function, and quality of life in allergic asthma patients: an open-label pilot study. Altern Med Rev J Clin therapeutic. (2012) 17(1):42–56.
10. Lieberoth S, Backer V, Kyvik KO, Skadhauge LR, Tolstrup JS, Grønbæk M, et al. Intake of alcohol and risk of adult-onset asthma. Respir Med (2012) 106(2):184–8. doi: 10.1016/j.rmed.2011.11.004
11. Butland BK, Strachan DP, Anderson HR. Fresh fruit intake and asthma symptoms in young British adults: confounding or effect modification by smoking? Eur Respir J (1999) 13(4):744–50. doi: 10.1034/j.1399-3003.1999.13d08.x
12. Seyedrezazadeh E, Moghaddam MP, Ansarin K, Vafa MR, Sharma S, Kolahdooz F. Fruit and vegetable intake and risk of wheezing and asthma: a systematic review and meta-analysis. Nutr Rev (2014) 72(7):411–28. doi: 10.1111/nure.12121
13. Woods RK, Walters EH, Raven JM, Wolfe R, Ireland PD, Thien FC, et al. Food and nutrient intakes and asthma risk in young adults. Am J Clin Nutr (2003) 78(3):414–21. doi: 10.1093/ajcn/78.3.414
14. Chatzi L, Torrent M, Romieu I, Garcia-Esteban R, Ferrer C, Vioque J, et al. Diet, wheeze, and atopy in school children in menorca, Spain. Pediatr Allergy Immunol (2007) 18(6):480–5. doi: 10.1111/j.1399-3038.2007.00596.x
15. Butler LM, Koh WP, Lee HP, Tseng M, Yu MC, London SJ. Prospective study of dietary patterns and persistent cough with phlegm among Chinese singaporeans. Am J Respir Crit Care Med (2006) 173(3):264–70. doi: 10.1164/rccm.200506-901OC
16. Boyko EJ. Observational research–opportunities and limitations. J Diabetes its complications. (2013) 27(6):642–8. doi: 10.1016/j.jdiacomp.2013.07.007
17. Staiger DO, Stock JH. Instrumental variables regression with weak instruments. Mass., USA: National Bureau of Economic Research Cambridge (1994).
18. Hartwig FP, Davey Smith G, Bowden J. Robust inference in summary data mendelian randomization via the zero modal pleiotropy assumption. Int J Epidemiol. (2017) 46(6):1985–98. doi: 10.1093/ije/dyx102
19. Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, et al. The MR-base platform supports systematic causal inference across the human phenome. Elife (2018) 7, e34408. doi: 10.7554/eLife.34408
20. Mikkelsen H, Landt EM, Benn M, Nordestgaard BG, Dahl M. Causal risk factors for asthma in mendelian randomization studies: A systematic review and meta-analysis. Clin Trans Allergy (2022) 12(11):e12207. doi: 10.1002/clt2.12207
21. Skaaby T, Kilpeläinen TO, Mahendran Y, Huang LO, Sallis H, Thuesen BH, et al. Association of milk intake with hay fever, asthma, and lung function: a mendelian randomization analysis. Eur J Epidemiol. (2022) 37(7):713–22. doi: 10.1007/s10654-021-00826-5
22. Pasala S, Barr T, Messaoudi I. Impact of alcohol abuse on the adaptive immune system. Alcohol Res Curr Rev (2015) 37(2):185–97.
24. Domínguez-Santalla MJ, Vidal C, Viñuela J, Pérez LF, González-Quintela A. Increased serum IgE in alcoholics: relationship with Th1/Th2 cytokine production by stimulated blood mononuclear cells. Alcoholism Clin Exp Res (2001) 25(8):1198–205. doi: 10.1111/j.1530-0277.2001.tb02336.x
25. González-Quintela A, Vidal C, Gude F, Tomé S, Lojo S, Lorenzo MJ, et al. Increased serum IgE in alcohol abusers. Clin Exp Allergy (1995) 25(8):756–64. doi: 10.1111/j.1365-2222.1995.tb00014.x
26. González-Quintela A, Vidal C, Lojo S, Pérez LF, Otero-Antón E, Gude F, et al. Serum cytokines and increased total serum IgE in alcoholics. Ann allergy Asthma Immunol (1999) 83(1):61–7. doi: 10.1016/S1081-1206(10)63514-4
27. Bendtsen P, Grønbaek M, Kjaer SK, Munk C, Linneberg A, Tolstrup JS. Alcohol consumption and the risk of self-reported perennial and seasonal allergic rhinitis in young adult women in a population-based cohort study. Clin Exp Allergy (2008) 38(7):1179–85. doi: 10.1111/j.1365-2222.2008.02945.x
28. Linneberg A, Petersen J, Grønbaek M, Benn CS. Alcohol during pregnancy and atopic dermatitis in the offspring. Clin Exp Allergy (2004) 34(11):1678–83. doi: 10.1111/j.1365-2222.2004.02101.x
29. Skaaby T, Kilpeläinen TO, Taylor AE, Mahendran Y, Wong A, Ahluwalia TS, et al. Association of alcohol consumption with allergic disease and asthma: a multi-centre mendelian randomization analysis. Addict (Abingdon England). (2019) 114(2):216–25. doi: 10.1111/add.14438
30. Lomholt FK, Nielsen SF, Nordestgaard BG. High alcohol consumption causes high IgE levels but not high risk of allergic disease. J Allergy Clin Immunol (2016) 138(5):1404–1413.e1413. doi: 10.1016/j.jaci.2016.05.022
31. Caramori G, Papi A. Oxidants and asthma. Thorax (2004) 59(2):170–3. doi: 10.1136/thorax.2002.002477
32. Chatzi L, Apostolaki G, Bibakis I, Skypala I, Bibaki-Liakou V, Tzanakis N, et al. Protective effect of fruits, vegetables and the Mediterranean diet on asthma and allergies among children in Crete. Thorax (2007) 62(8):677–83. doi: 10.1136/thx.2006.069419
33. Patel BD, Welch AA, Bingham SA, Luben RN, Day NE, Khaw KT, et al. Dietary antioxidants and asthma in adults. Thorax (2006) 61(5):388–93. doi: 10.1136/thx.2004.024935
34. Shaheen SO, Sterne JA, Thompson RL, Songhurst CE, Margetts BM, Burney PG. Dietary antioxidants and asthma in adults: population-based case-control study. Am J Respir Crit Care Med (2001) 164(10 Pt 1):1823–8. doi: 10.1164/ajrccm.164.10.2104061
35. Romieu I, Varraso R, Avenel V, Leynaert B, Kauffmann F, Clavel-Chapelon F. Fruit and vegetable intakes and asthma in the E3N study. Thorax (2006) 61(3):209–15. doi: 10.1136/thx.2004.039123
36. Garcia V, Arts IC, Sterne JA, Thompson RL, Shaheen SO. Dietary intake of flavonoids and asthma in adults. Eur Respir J (2005) 26(3):449–52. doi: 10.1183/09031936.05.00142104
37. Hijazi N, Abalkhail B, Seaton A. Diet and childhood asthma in a society in transition: a study in urban and rural Saudi Arabia. Thorax (2000) 55(9):775–9. doi: 10.1136/thorax.55.9.775
38. Laerum BN, Wentzel-Larsen T, Gulsvik A, Omenaas E, Gíslason T, Janson C, et al. Relationship of fish and cod oil intake with adult asthma. Clin Exp Allergy J Br Soc Allergy Clin Immunol (2007) 37(11):1616–23. doi: 10.1111/j.1365-2222.2007.02821.x
39. Miyamoto S, Miyake Y, Sasaki S, Tanaka K, Ohya Y, Matsunaga I, et al. Fat and fish intake and asthma in Japanese women: baseline data from the Osaka maternal and child health study. Int J tuberculosis Lung disease. (2007) 11(1):103–9.
40. Hodge L, Salome CM, Peat JK, Haby MM, Xuan W, Woolcock AJ. Consumption of oily fish and childhood asthma risk. Med J Australia. (1996) 164(3):137–40. doi: 10.5694/j.1326-5377.1996.tb122010.x
41. Yang H, Xun P, He K. Fish and fish oil intake in relation to risk of asthma: a systematic review and meta-analysis. PloS One (2013) 8(11):e80048. doi: 10.1371/journal.pone.0080048
42. Takemura Y, Sakurai Y, Honjo S, Tokimatsu A, Gibo M, Hara T, et al. The relationship between fish intake and the prevalence of asthma: the tokorozawa childhood asthma and pollinosis study. Prev Med (2002) 34(2):221–5. doi: 10.1006/pmed.2001.0978
43. Hooper R, Heinrich J, Omenaas E, Sausenthaler S, Garcia-Larsen V, Bakolis I, et al. Dietary patterns and risk of asthma: results from three countries in European community respiratory health survey-II. Br J Nutr (2010) 103(9):1354–65. doi: 10.1017/S0007114509993266
44. Wee JH, Yoo DM, Byun SH, Song CM, Lee HJ, Park B, et al. Analysis of the relationship between asthma and Coffee/Green Tea/Soda intake. Int J Environ Res Public Health (2020) 17(20):7471. doi: 10.3390/ijerph17207471
45. Lin F, Zhu Y, Liang H, Li D, Jing D, Liu H, et al. Association of coffee and tea consumption with the risk of asthma: A prospective cohort study from the UK biobank. Nutrients (2022) 14(19):4039. doi: 10.3390/nu14194039
46. Devereux G, Seaton A. Diet as a risk factor for atopy and asthma. J Allergy Clin Immunol (2005) 115(6):1109–17; quiz 1118. doi: 10.1016/j.jaci.2004.12.1139
47. Kau AL, Ahern PP, Griffin NW, Goodman AL, Gordon JI. Human nutrition, the gut microbiome and the immune system. Nature (2011) 474(7351):327–36. doi: 10.1038/nature10213
48. Muegge BD, Kuczynski J, Knights D, Clemente JC, González A, Fontana L, et al. Diet drives convergence in gut microbiome functions across mammalian phylogeny and within humans. Sci (New York N.Y.). (2011) 332(6032):970–4. doi: 10.1126/science.1198719
49. Trompette A, Gollwitzer ES, Yadava K, Sichelstiel AK, Sprenger N, Ngom-Bru C, et al. Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nat Med (2014) 20(2):159–66. doi: 10.1038/nm.3444
50. Mokry LE, Ross S, Ahmad OS, Forgetta V, Smith GD, Goltzman D, et al. Vitamin d and risk of multiple sclerosis: A mendelian randomization study. PloS Med (2015) 12(8):e1001866. doi: 10.1371/journal.pmed.1001866
Keywords: Mendelian randomization, dietary intake, asthma, alcohol intake, fruit intake
Citation: Yang W, Yang Y, He L, Zhang M, Sun S, Wang F and Han B (2023) Dietary factors and risk for asthma: A Mendelian randomization analysis. Front. Immunol. 14:1126457. doi: 10.3389/fimmu.2023.1126457
Received: 17 December 2022; Accepted: 09 February 2023;
Published: 22 February 2023.
Edited by:
Manuela Berto Pucca, Federal University of Roraima, BrazilReviewed by:
Isabela Gobbo Ferreira, University of São Paulo, Ribeirão Preto, BrazilCopyright © 2023 Yang, Yang, He, Zhang, Sun, Wang and Han. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Biao Han, aGFuYmlhbzY2QDE2My5jb20=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.