- 1Pediatric Department, Hospital Universitario Puerta del Mar, Cádiz, Spain
- 2Biomedical Research and Innovation Institute of Cádiz (INiBICA), Cádiz, Spain
- 3Pediatric Department, Hospital Universitario Reina Sofia, Córdoba, Spain
- 4Instituto Maimónides de Investigación Biomédica de Córdoba (IMIBIC), Córdoba, Spain
- 5Endocrinology and Nutrition Department, Hospital Universitario Puerta del Mar, Cádiz, Spain
Introduction: Trans women are highly affected by the human papillomavirus (HPV) and are at risk of suffering from HPV-related diseases such as oropharyngeal, anal, penile, or neovaginal neoplasia. HPV vaccination seems to be a good strategy to reduce HPV-related diseases, mainly during the early age before the first sexual intercourse, but only cisgender girls are covered by the National Health Services, while some high-risk groups such as trans girls are not included. Achieving a high vaccination rate is important in the adolescent population, but there are many factors that could affect it, such as lack of knowledge about HPV or fear of side effects by patients and main caregivers. The aim of our study is to analyze the knowledge of trans girls’ main caregivers about HPV-related diseases in the general population and, in particular, in trans women, as well as factors associated with HPV vaccination intention.
Methods: A cross-sectional study was performed with the collaboration of main caregivers of adolescent trans girls, between 9 and 16 years old, assisted in two reference centers’ multidisciplinary Gender Diversity Units. Information was requested through a self-completed questionnaire: HPV-related diseases Knowledge Transwomen questionnaire (HPV-TQ) was elaborated based on a 19-item self-administered questionnaire and score was standardized from 0 to 19 points. Percentage of correct answers was calculated and defined by the group of high scores that showed over 70% correct answers.
Results: A total of 65 main caregivers were included. Almost all main caregivers were mothers with a Caucasian ethnicity. The HPV-TQ average score was 11 (3.7) with an average correct answer of 58.1% (19.6). Only 17/65 (26.1%) of main caregivers were highly knowledgeable in HPV. Of 65 trans girls, 14 were already vaccinated (29.8% of trans girls over 12 years old); 78.5% were not vaccinated and only 21.5% had intentions to be vaccinated. The group with a high score in HPV-TQ had a longer follow-up at the transgender unit, a higher maternal vaccination rate, and a positive family history of HPV-related disease, especially in mothers.
Conclusion: Adolescent trans girls attended to in our units had a low rate and a low intention of vaccination against HPV. Education on and promotion and prevention of transgender HPV-related diseases should probably be implemented to achieve a higher knowledge and vaccination coverage in adolescent trans girls.
1 Introduction
Human papillomavirus (HPV) infection is considered the most frequent sexually transmitted infection in the world (1). Several studies suggest a high lifetime probability of HPV acquisition early in life, as reported by a US cohort, in which more than 80% of women and men acquire HPV by the age of 45 years (2). HPV infection can lead to a variety of consequences besides cervical cancer, such as genital warts and oropharyngeal, penile, anal, vulvar, or vaginal cancer (3).
Transgender women are not exempted from HPV risk infection. Indeed, some studies demonstrate a high prevalence of high-risk serotypes and the presence of anogenital warts in adult trans women, such as that of Brown et al. (2016), which shows that up to 96% of trans women have HPV infection, 58.8% of whom were high-risk serotypes and up to 19.1% have anogenital warts (4). Along this line, Jalil et al. (2021) report that up to 77.9% of trans women were infected with HPV, with 60.7% being high-risk serotypes (5). In addition, an American study reports that transsexual women have a higher prevalence of anal HPV infection than men who have sex with men, 88.6% versus 70.9%, respectively (6). Moreover, although the prevalence of neovaginal infection is unknown, five cases of squamous cell carcinoma have been related to HPV infection in the neovagina of transgender women, some of which are at an advanced stage, perhaps due to the low concern about it (7–11).
HPV vaccination programs are mainly designed to protect people from cervical cancer. However, in recent years, scientific evidence suggests that the vaccine may protect against other neoplastic entities (12, 13). Furthermore, the World Health Organization recommends vaccination in adolescents of both genders (14). Main vaccination programs are focused on cisgender female adolescents prior to the first sexual intercourse, approximately 12–14 years old, and high-risk groups, such as those engaged in prostitution, people in contact with HIV, conizated women, and men who have sex with men (15). However, trans women are not included, probably due to a lack of knowledge, which could have a negative impact on their health. In fact, in a survey in which two trans women were recruited, only one received recommendation for HPV vaccination (16). Such data suggest missed opportunities to address the need for HPV vaccination among transgender people.
Achieving a high vaccination rate is important in the adolescent population, but many factors contribute to vaccination refusal by adolescents and their families (17). Many studies show the impact of acceptance or denial of the vaccination according to the opinion of the main caregiver of adolescents. Some factors, such as efficacy, the fear related to vaccine safety, or a poor knowledge about risk and consequences of HPV infection, are reported to be crucial when choosing to vaccinate or not (18, 19).
Currently, there is no published study that focused on the feelings and knowledge of main caregivers of trans adolescents, in order to improve the adherence to vaccination. Our aim is to determine the main trans women caregivers’ knowledge about HPV infection and risk, and to detect which factors could influence the intention of vaccination.
2 Materials and methods
A cross-sectional study was conducted based on interviews of main caregivers of adolescents under 16 years old followed up in two reference centers with a multidisciplinary Sex Reassignment Treatment Unit: Hospital Puerta del Mar (Cádiz, Spain) and Hospital Universitario Reina Sofia (Cordoba, Spain). Inclusion criteria were as follows: main caregivers of transgender women between 9 and 16 years old who were involved in Sex Reassignment Treatment Units between January 2022 and July 2022, completed the questionnaire, and signed the consent form.
The survey instrument was HPV-related diseases Knowledge Transwomen questionnaire (HPV-TQ), a 19-item self-administered questionnaire with True–False forced-response questions based on a validated survey but adapted to the transgender population (20). It covers basic knowledge of HPV infection as its characteristics, including transmission, viral properties, treatment, prevalence, vaccination, perception of sexual risk behavior, and specific risk in trans women. The content, readability, and comprehensiveness of the questionnaire were reviewed by clinicians and health educators. Answers were evaluated. Correct answers were scored as 1 point, and wrong answers received 0 points. The final score was the result of the sum of all points, ranging from 0 to 19. This score was converted into percentage, standardized from 0 to 100. A score equal to and/or over 70% was classified as high HPV knowledge. HPV vaccination status and demographic and clinical data were collected from the clinical history of trans girls.
All participants provided a written informed consent before data collection in accordance with the Declaration of Helsinki, and researchers guaranteed the anonymity of data. The study was approved by the Ethics Committee of Puerta del Mar University Hospital (ethical approval code number PEIBA 0474-N-22).
Statistical analysis was performed with SPSS version 23.0 (IBM, Armonk, NY, USA). Descriptive statistics were calculated for all variables. Continuous measures were summarized by using mean and standard deviation, and dichotomous measures were summarized by using proportions. Student’s t-test was performed to compare continuous variables and χ2 was used when proportions are compared. p < 0.05 was considered statistically significant.
3 Results
3.1 Clinical and sociodemographic characteristics
A total of 65 main trans women adolescent caregivers were included. The average age of trans girls was 13.3 (2.7) years, and the mean age of those visiting the unit was 9.1 (3.4) years old; the main ethnic group was Caucasian (62/65, or 95.4%). Currently, puberal blockage and crossed hormone therapy have been started in 41/65 (63.1%) and 26/65 (40%) women, respectively. Comparing this variable within low- and high-HPV knowledge groups, we only found longer follow-up in the high-HPV knowledge group in comparison with its low counterpart, with differences being statistically significant. Almost all main caregivers were the trans girls’ mothers, whose mean age was 44.1 (5.6) years old. The most frequent educational level was general certificate of secondary education in 27/65 caregivers (41.5%), followed by university studies with 17/65 caregivers (26.2%); 44/65 caregivers (67.7%) were married. No differences were found in the sociodemographic characteristics of the main caregivers when they were compared by HPV knowledge level. All data are shown in Table 1.
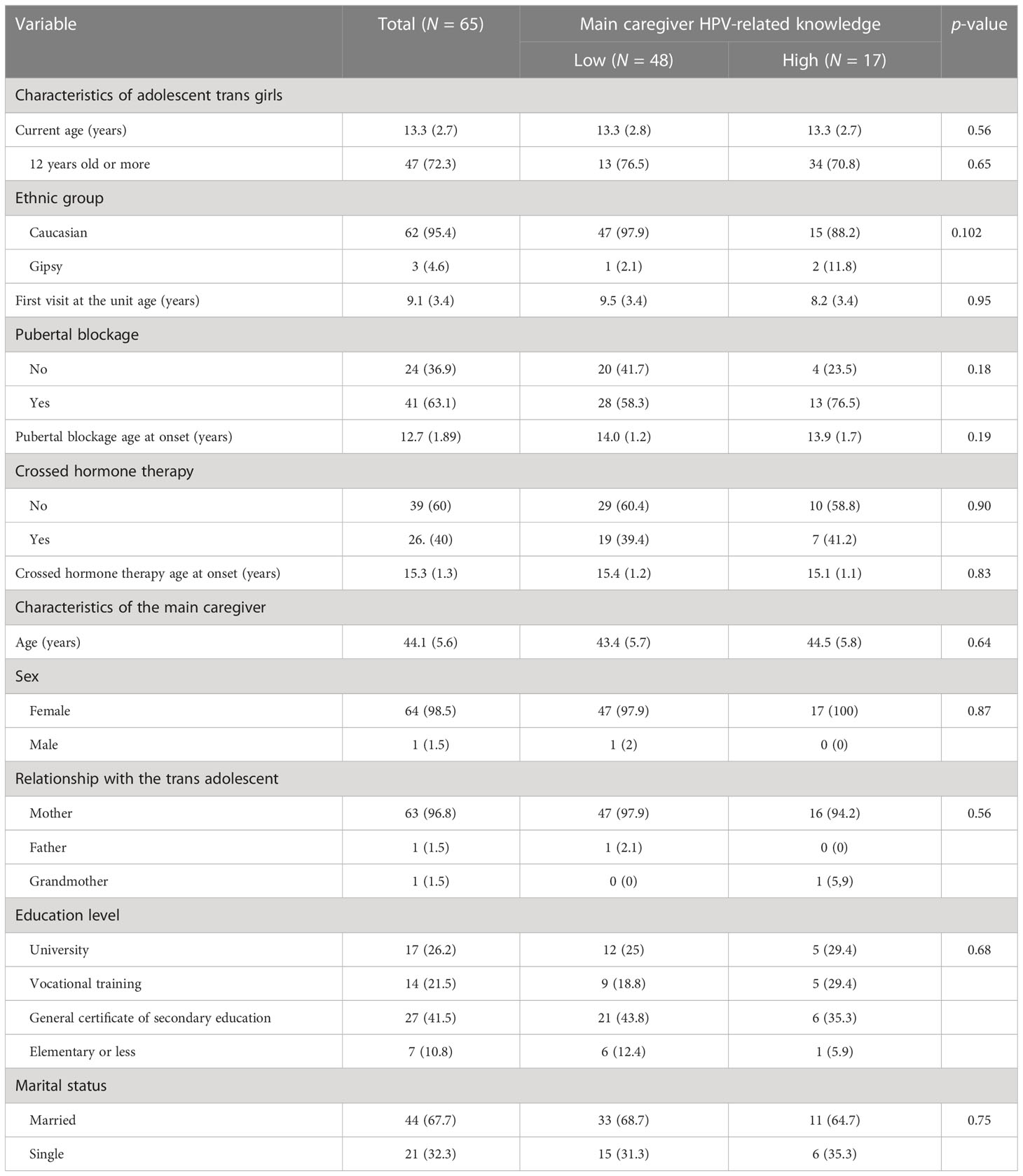
Table 1 Clinical and sociodemographic characteristics of adolescent trans girls and their main caregiver.
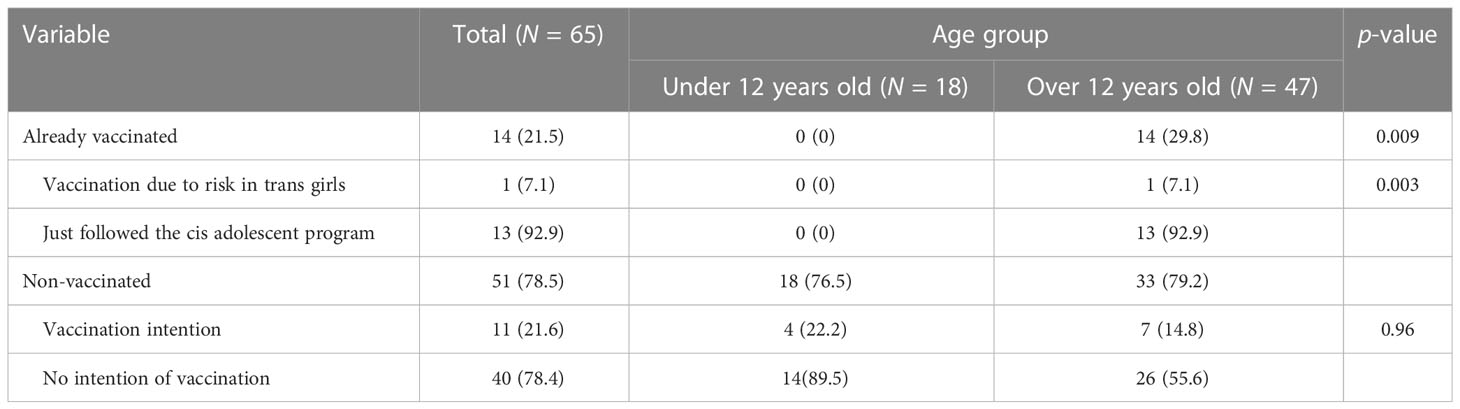
3.2 Adolescent trans girls’ vaccination status and intentions
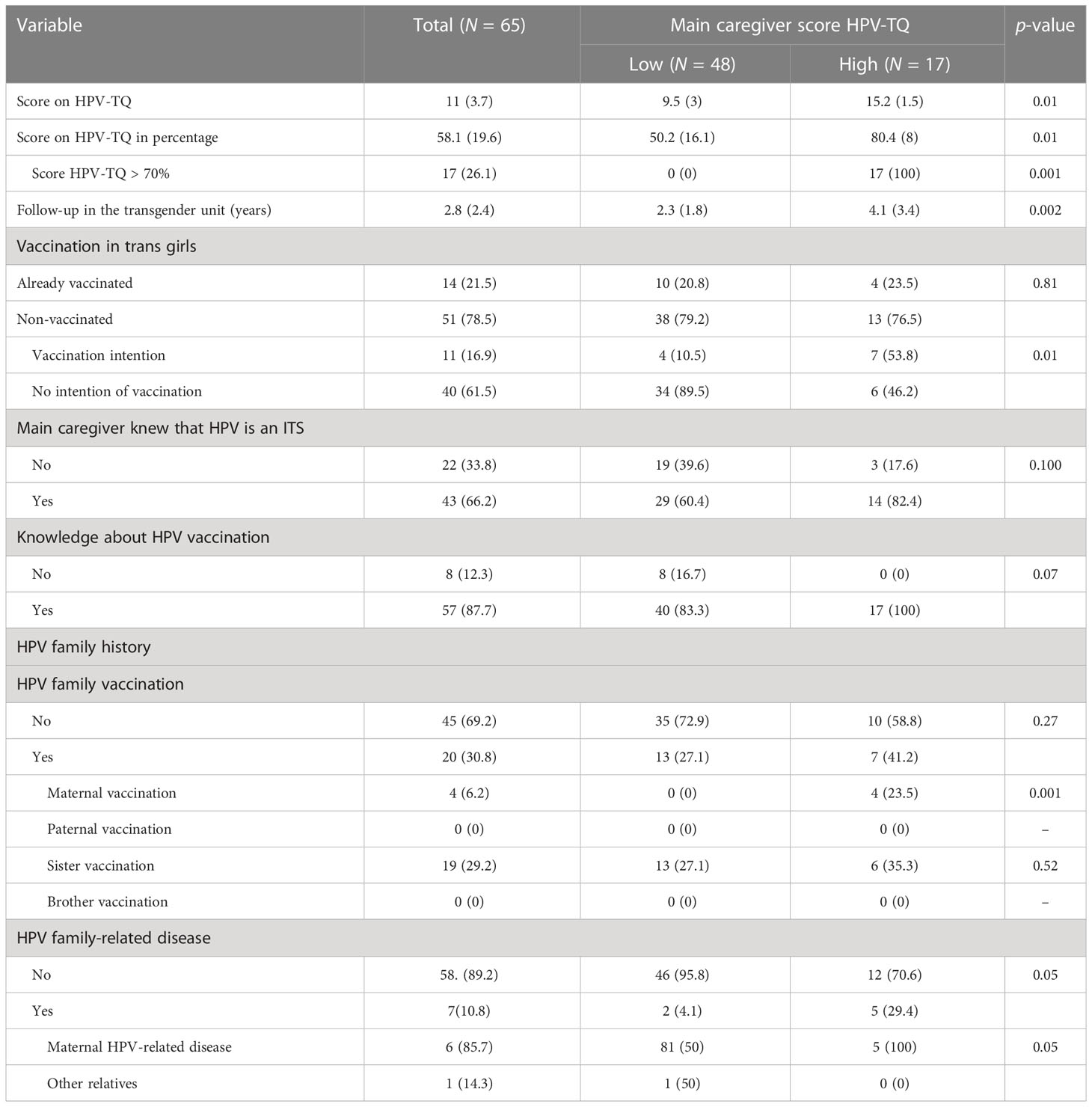
Of 65 girls, 14 were already vaccinated, all over 12 years old. They represent 21.5% of the total sample and 29.8% of the total girls over 12 years old in the sample, which is the recommended age for vaccination in cisgender girls. Only 1/7 (7.1%) of all vaccinated trans girls was vaccinated to prevent transgirl HPV-related risk, while the rest were vaccinated by following a cisgender girl program. The non-vaccinated rate was high, 51/65 (78.5%), and only 11/51 (21.5%) intended to be vaccinated. Similar data are shown in groups under and over 12 years old, 22.2% and 14.8%, respectively; thus, no differences were found. Data are shown in Table 2. Although we did not find differences in the rate of vaccination, Table 3 shows higher intention of vaccination in the high-HPV knowledge group in comparison to the low-HPV knowledge group, 53.8% and 10.5%, respectively.
3.3 HPV-related knowledge
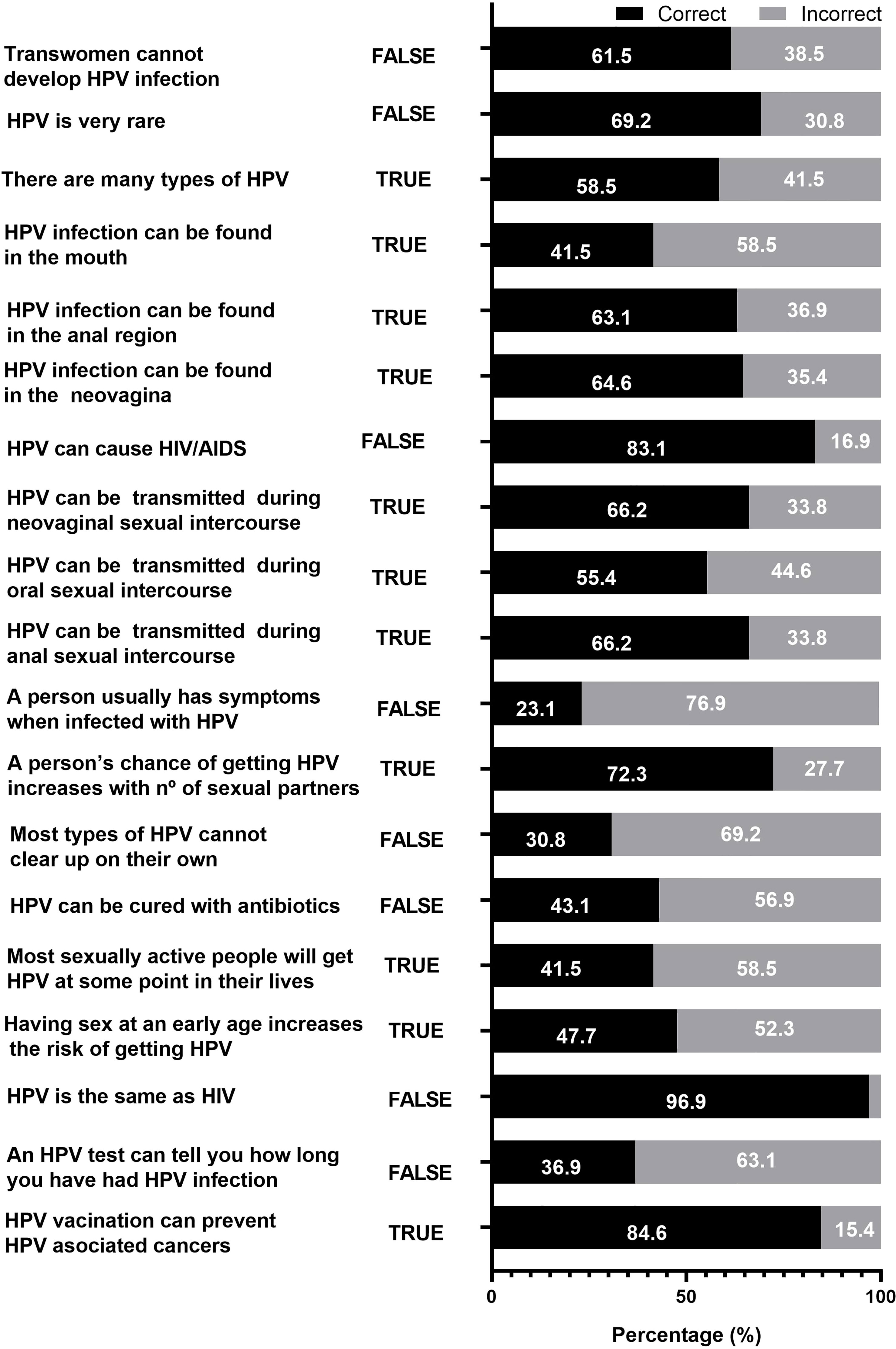
The HPV-TQ mean score was 11 (3.7), and the mean percentage of correct answers was 58.1% (19.6). Only 17/65 (26.1%) main caregivers were highly knowledgeable in HPV. Figure 1 shows the percentage of correct and incorrect answers to each question. The highest rates were found in the two questions about differentiation with human immunodeficiency virus (HIV): “HPV can cause AIDS” and “HPV is the same as HIV”, with 83.1% and 96.9%, respectively. Also, we found a correct answer of 84.6% to the question “HPV vaccination can prevent HPV-associated cancers”. The lowest rates were found in questions related to clinical presentation, physiopathology, diagnosis, or prevalence, such as “A person usually has symptoms when is infected by HPV” (23.1%); “Most types of HPV cannot clear up on their own” (30.8%); “Most sexually active people will get HPV at some point in their lives” (41.5%); “HPV infection can be found in the mouth” (41.5%); or “HPV can be cured by antibiotics” (43.1%). Questions about transgender risk of HPV contagion such as “Trans women cannot develop HPV infections”, “HPV infection can be found in the neovagina”, and “HPV can be transmitted by neovaginal intercourse” had correct responses of 61.5%, 64.6%, and 66.2%, respectively.
3.4 Related factors’ influence on HPV-related knowledge
Table 3 summarizes the personal and family history of HPV-related disease. We found that the group with a high score in HPV-TQ had a longer follow-up at the transgender units, a higher proportion in maternal vaccination, and a positive family history of HPV-related disease, especially in mothers. History of trans girls’ or trans girls’ sisters’ vaccination did not have statistically significant differences. Although it seemed that we found a higher rate of main caregivers who knew that HPV was an ITS and who knew about the HPV vaccine, no statistically significant differences were found.
4 Discussion
Gay, bisexual, and other men who have sex with men and transgender women are disproportionately affected by HPV. HPV vaccination is most effective when given before exposure to HPV through sexual activity. Vaccination is routinely recommended in some countries such as USA for adolescents at age 11–12 years, with catch-up vaccination through age 26 years. However, Meites et al. (2022) showed a median age at first dose of 19 years and a median age at first sexual intercourse of 17 years; 493 (73.3%) reported that their age at first dose was older than their age at first sexual intercourse (21). Spain probably had a similar situation, which could explain the low vaccination rate in the recommended age group. National vaccination surveys reported that our region, Andalusia (Spain), has the lowest vaccination rate in the country. Only 75% of adolescent cisgender girls had the first vaccine dose, and 59.9% had the second one (22), but adolescent trans girls have lower rates: only 28.9% of those over 12 years old have been vaccinated. The rate in our study might not be considered the real prevalence, because not all trans adolescents of the region were evaluated in our study, but the rate could be representative of the population. Also, we observed a low vaccination intention; only 16.9% of trans girl main caregivers considered the vaccination important for their minor children. Similar data were reported in studies focused on main caregivers of adolescent cisgender boys (23, 24), cisgender adult men (25), and men who have sex with men, probably because of the lack of knowledge of the risk for oral, penile, and anal cancer (26), and because HPV infection was considered an issue only for cisgender girls or women, due to health marketing and campaign efforts to achieve higher vaccination in this population (24).
The group of main caregivers who were highly knowledgeable about HPV showed a significantly longer follow-up at our specialized units, which might be explained by the fact that related information about risk of HPV in trans girls could be provided by gender diversity unit specialists who are knowledgeable about the importance of HPV vaccination. Vaccination in our region is programmed in primary care centers. A study in Andalusian primary care revealed that low knowledge of professionals leads to doubts in vaccination as well as unclear information provided to patients and families (27). In addition, professionals need to be sensitive to the specific health problems of trans women, such as HPV-related diseases, in order to reduce stigma and healthcare barriers (28). It is important for professionals to transmit reliable information to main caregivers and adolescent trans girls.
A similar situation has been experienced in other countries. In a 2014 survey conducted in USA involving rural participants enrolled online that included 23 transgender women who were age-eligible for HPV vaccination, only one reported receiving a healthcare provider recommendation for HPV vaccination, and only one reported ever receiving ≥1 dose of HPV vaccine. Such data suggest missed opportunities to address the need for HPV vaccination among transgender people as well as in our country (29). Increasing both routine and catch-up vaccination will improve coverage among transgender women (21).
Several studies revealed the main predictors of vaccination, which included, apart from healthcare provider recommendation, younger age, having a healthcare visit in the past year, receiving other recommended vaccinations, and living with HIV (21, 29, 30). Another interesting point is reported by Pho et al. (2022), which is associated with online health information seeking and HPV vaccination (31). Decreased reporting of HPV vaccination among trans people after searching for vaccine information online suggests vaccine hesitancy, which may potentially be related to the quality of online content. Increased reporting of vaccination after using social media may be related to peer validation. Future studies should investigate potential deterrents to HPV vaccination in online health information to enhance its effectiveness and further explore which aspects of social media might increase vaccine uptake among trans people.
Although other studies revealed higher knowledge in vaccinated adolescents’ parents (32), we did not observe this effect, because almost all adolescent trans girls in our study were vaccinated without any specific motivation; they just followed the cis girl program. We observed that a previous history of HPV disease in the first-line family is associated with a higher knowledge score and higher intention of vaccination. Other studies found an inverse correlation between knowledge and age of main caregivers (33), but our data did not support this. Moreover, educational level is reported as important. Higher HPV knowledge has been related to higher educational attainment (34); however, our study showed equally distributed educational levels. Gender and ethnicity influence could not be analyzed in our study because almost all participants were Caucasian and women.
Mean knowledge in our study was acceptable but some questions had a low proportion of correct responses such as those related to clinical presentation, natural history of HPV infection, diagnosis method, and treatment. This could reflect ignorance about basic aspects of HPV infection. These findings are similar to a study involving the main caregivers of adolescent cis boys from UK. Firstly, in the question “HPV can be cured by antibiotics” in our study, only 43.1% of main caregivers answered correctly, compared to 48.5% in the adolescent cis boys’ main caregiver study (23). Also, the question “Most sexually active people will get HPV at some point in their lives” had 41.5% and 32.3% correct responses, respectively (23). Interestingly, oropharyngeal infection by HPV is unknown for many main caregivers in our study; only 41.5% knew that it could be found in the mouth, lower than that reported by the adolescent cis boys’ main caregiver survey study (49.5%) (23) and that reported by a study in an adult population in USA (49.3%) (20).
The strength of our study resides in the fact that limited data about HPV in the trans population are available (35). In fact, in USA, database searches and manual searching yielded 843 citations. After screening, eight articles were retained in the review. Seven were cross-sectional studies and one was a qualitative focus group. The low proportion of transgender participants in the retained studies highlights a gap in knowledge about HPV vaccination among this population. Future studies of HPV vaccination should recruit trans people to better represent their perspectives and data (31). There are some limitations in our study, such as having a small sample size and the low diversity in caregivers, because most of them were mothers. Two main caregivers refused to participate. Thus, our results could be susceptible to selection bias because the main caregivers who participated might be more health conscious and curious about HPV. In that case, HPV knowledge could be lower if this is true.
5 Conclusions
This study showed a low vaccination proportion, only 21.5%. Also, 21.5% of main caregivers of unvaccinated adolescent trans girls intend to be vaccinated. We observe that intention of vaccination is related to HPV knowledge. Knowledge in HPV was related to a previous family history of HPV-related disease, maternal HPV vaccination, and longer time of follow-up in our units. The results should encourage the development and implementation of health education programs that discuss the HPV vaccine and its benefits for trans women at early age. General recognition and approval of vaccination programs for trans women by health international institutions and campaigns focused on main caregivers to increase knowledge and awareness about the virus and vaccination can help raise the vaccination rate and improve health equality.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by COMITÉ DE ÉTICA DE LA INVESTIGACIÓN DE CÁDIZ. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
JD-R and IM-G conceptualized and designed the study, contributed to the clinical recruitment of participants, supervised the database, performed statistical analyses, drafted the initial manuscript, revised it, and wrote the final version. CB-C performed the dataset and reviewed and revised the manuscript. A-BA-J reviewed the study design, contributed to the clinical recruitment of participants, and reviewed and revised the manuscript for the final version. All authors contributed to the article and approved the submitted version.
Acknowledgments
We thank all our study families and the staff at our study sites for their continued cooperation and collaboration.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Forman D, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, Bruni L, et al. Global burden of human papillomavirus and related diseases. Vaccine (2012) 30:F12–23. doi: 10.1016/j.vaccine.2012.07.055
2. Chesson HW, Dunne EF, Hariri S, Markowitz LE. The estimated lifetime probability of acquiring human papillomavirus in the united states. Sex Transm Dis (2014) 41(11):660–4. doi: 10.1097/OLQ.0000000000000193
3. Factsheet about human papillomavirus. European centre for disease prevention and control. Available at: https://www.ecdc.europa.eu/en/human-papillomavirus/factsheet (Accessed October 19, 2022).
4. Brown B, Galea JT, Byraiah G, Poteat HT, Leon SR, Calvo G, et al.Anogenital human papillomavirus infection and HIV infection outcomes among Peruvian transgender women: Results from a cohort study. Transgender Health (2016) 1(1):94–8. doi: 10.1089/trgh.2016.0001
5. Jalil EM, Wilson EC, Monteiro L, de Velasque LS, Ferreira ACG, Nazer SC, et al. High prevalence of anal high-risk HPV infection among transwomen: Estimates from a Brazilian RDS study. J Int AIDS Soc (2021) 24(3):e25691. doi: 10.1002/jia2.25691
6. Singh V, Gratzer B, Gorbach PM, Crosby RA, Panicker G, Steinau M, et al. Transgender women have higher human papillomavirus prevalence than men who have sex with men–two U.S. cities, 2012–2014. Sex Transm Dis (2019) 46(10):657–62. doi: 10.1097/OLQ.0000000000001051
7. Fernandes HM, Manolitsas TP, Jobling TW. Carcinoma of the neovagina after male-to-female reassignment. J Low Genit Tract Dis (2014) 18(2):E43–45. doi: 10.1097/LGT.0b013e3182976219
8. Wang G, Ferguson D, Ionescu DN, Hoang L, Barrett S, van Niekerk D, et al. HPV-related neovaginal squamous cell carcinoma presenting as lung metastasis after Male-to-Female gender confirmation surgery. Case Rep Oncol (2020) 13(1):17–22. doi: 10.1159/000504936
9. Bollo J, Balla A, Rodriguez Luppi C, Martinez C, Quaresima S, Targarona EM. HPV-related squamous cell carcinoma in a neovagina after male-to-female gender confirmation surgery. Int J STD AIDS (2017) 29(3):306–8. doi: 10.1177/0956462417728856
10. Fierz R, Ghisu GP, Fink D. Squamous carcinoma of the neovagina after Male-to-Female reconstruction surgery: A case report and review of the literature. Case Rep Obstet Gynecol (2019) 2019:4820396. doi: 10.1155/2019/4820396
11. Harder Y, Erni D, Banic A. Squamous cell carcinoma of the penile skin in a neovagina 20 years after male-to-female reassignment. Br J Plast Surg (2002) 55(5):449–51. doi: 10.1054/bjps.2002.3868
12. Yousefi Z, Aria H, Ghaedrahmati F, Bakhtiari T, Azizi M, Bastan R, et al. An update on human papilloma virus vaccines: History, types, protection, and efficacy. Front Immunol (2021) 12:805695. doi: 10.3389/fimmu.2021.805695
13. Kamolratanakul S, Pitisuttithum P. Human papillomavirus vaccine efficacy and effectiveness against cancer. Vaccines (2021) 9(12):1413. doi: 10.3390/vaccines9121413
14. Human papillomavirus vaccines: WHO position paper. Available at: https://www.who.int/publications-detail-redirect/who-wer9219-241-268 (Accessed October 20, 2022).
15. Colzani E, Johansen K, Johnson H, Pastore Celentano L. Human papillomavirus vaccination in the European Union/European economic area and globally: A moral dilemma. Eurosurveillance (2021) 26(50). doi: 10.2807/1560-7917.ES.2021.26.50.2001659
16. Bednarczyk RA, Whitehead JL, Stephenson R. Moving beyond sex: Assessing the impact of gender identity on human papillomavirus vaccine recommendations and uptake among a national sample of rural-residing LGBT young adults. Papillomavirus Res (2017) 3:121–5. doi: 10.1016/j.pvr.2017.04.002
17. Wemrell M, Gunnarsson L. Attitudes toward HPV vaccination in Sweden: A survey study. Front Public Health (2022) 10:729497. doi: 10.3389/fpubh.2022.729497
18. Gottvall M, Grandahl M, Höglund AT, Larsson M, Stenhammar C, Andrae B, et al. Trust versus concerns–how parents reason when they accept HPV vaccination for their young daughter. Ups J Med Sci (2013) 118(4):263–70. doi: 10.3109/03009734.2013.809039
19. Oldach BR, Katz ML. Ohio Appalachia Public health department personnel: Human papillomavirus (HPV) vaccine availability, and acceptance and concerns among parents of Male and female adolescents. J Community Health (2012) 37(6):1157–63. doi: 10.1007/s10900-012-9613-5
20. Osazuwa-Peters N, Adjei Boakye E, Chen BY, Clancy J, Vallot PL, Su JL, et al. Sociodemographic factors associated with knowledge and risk perception of human papillomavirus and human papillomavirus–associated oropharyngeal squamous cell carcinoma among a predominantly black population. JAMA Otolaryngol Neck Surg (2016) 143(2):117. doi: 10.1001/jamaoto.2016.2784
21. Meites E, Wilkin TJ, Markowitz LE. Review of human papillomavirus (HPV) burden and HPV vaccination for gay, bisexual, and other men who have sex with men and transgender women in the United States. Hum Vaccines Immunother (2021) 18(1):2016007. doi: 10.1080/21645515.2021.2016007
22. Ministerio de sanidad . Consulta Interactiva del SNS. Available at: https://pestadistico.inteligenciadegestion.sanidad.gob.es/publicoSNS/I/sivamin/sivamin (Accessed November 13, 2022).
23. Sherman SM, Nailer E. Attitudes towards and knowledge about human papillomavirus (HPV) and the HPV vaccination in parents of teenage boys in the UK. PloS One (2018) 13(4):e0195801. doi: 10.1371/journal.pone.0195801
24. Venderbos JR, Eilers R, de Vries H, van Zoonen K. A qualitative study of parental associations and beliefs regarding the HPV vaccination for Dutch boys. BMC Public Health (2022) 22(1):1188. doi: 10.1186/s12889-022-13605-y
25. Jeannot E, Viviano M, Follonier MC, Kaech C, Oberhauser N, Mpinga EK, et al. Human papillomavirus infection and vaccination: Knowledge, attitude and perception among undergraduate men and women healthcare university students in Switzerland. Vaccines (2019) 7(4):130. doi: 10.3390/vaccines7040130
26. Zhao Y, Xin X, Deng H, Xu J, Weng W, Zhang M, et al. Improving the acceptability of human papillomavirus vaccines among men who have sex with men according to the associated factors: A systematic review and meta-analysis. Front Pharmacol (2021) 12:600273. doi: 10.3389/fphar.2021.600273
27. González Cano-Caballero M, Gil García E, Garrido Peña F, Cano-Caballero Galvez MD. Opinions of andalusian primary health care professionals. Sist Sanit Navar (2018) 41(1):27–34. doi: 10.23938/ASSN.0126
28. Aleshire ME, Ashford K, Fallin-Bennett A, Hatcher J. Primary care providers’ attitudes related to LGBTQ people: A narrative literature review. Health Promot Pract (2018) 20(2):173–87. doi: 10.1177/1524839918778835
29. Amiling R, Winer RL, Newcomb ME, Gorbach PM, Lin J, Crosby RA, et al. Human papillomavirus vaccination coverage among young, gay, bisexual, and other men who have sex with men and transgender women — 3 U.S. cities, 2016–2018. Hum Vaccines Immunother (2021) 17(12):5407–12. doi: 10.1080/21645515.2021.2005436
30. Gorbach PM, Cook R, Gratzer B, Collins T, Parrish A, Moore J, et al. Human papillomavirus vaccination among young men who have sex with men and transgender women in 2 US cities, 2012–2014. Sex Transm Dis (2017) 44(7):436–41. doi: 10.1097/OLQ.0000000000000626
31. Pho AT, Bakken S, Lunn MR, Lubensky ME, Flentje A, Dastur Z, et al. Online health information seeking, health literacy, and human papillomavirus vaccination among transgender and gender-diverse people. J Am Med Inform Assoc (2021) 29(2):285–95. doi: 10.1093/jamia/ocab150
32. González-Cano M, Garrido-Peña F, Gil-Garcia E, Lima-Serrano M, Cano-Caballero MD. Sexual behaviour, human papillomavirus and its vaccine: A qualitative study of adolescents and parents in Andalusia. BMC Public Health (2021) 21(1):1476. doi: 10.1186/s12889-021-11510-4
33. Capogrosso P, Ventimiglia E, Matloob R, Colicchia M, Serino A, Castagna G, et al. Awareness and knowledge of human papillomavirus-related diseases are still dramatically insufficient in the era of high-coverage vaccination programs. World J Urol (2014) 33(6):873–80. doi: 10.1007/s00345-014-1379-1
34. Petrovic K, Burney S, Fletcher J. The relationship of knowledge, health value and health self-efficacy with men’s intentions to receive the human papillomavirus (HPV) vaccine. J Health Psychol (2011) 16(8):1198–207. doi: 10.1177/1359105311402861
Keywords: transwomen, adolescents, main caregiver, HPV knowledge, human papilloma virus - HPV, vaccination intention
Citation: Domínguez-Riscart J, Ariza-Jimenez A-B, Baez-Castillo C and Mateo-Gavira I (2023) Factors associated with knowledge and vaccination intention for human papillomavirus on trans girls by their main caregiver: A cross-sectional study. Front. Immunol. 14:1097449. doi: 10.3389/fimmu.2023.1097449
Received: 13 November 2022; Accepted: 16 March 2023;
Published: 30 March 2023.
Edited by:
Pei-Hui Wang, Shandong University, ChinaReviewed by:
Catalina Lunca, Grigore T. Popa University of Medicine and Pharmacy, RomaniaHuachun Zou, Sun Yat-sen University, China
Copyright © 2023 Domínguez-Riscart, Ariza-Jimenez, Baez-Castillo and Mateo-Gavira. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jesus Domínguez-Riscart, amVzdXMuZG9taW5ndWV6cmlzY2FydEBnbWFpbC5jb20=
 Jesus Domínguez-Riscart
Jesus Domínguez-Riscart Ana-Belen Ariza-Jimenez
Ana-Belen Ariza-Jimenez Celia Baez-Castillo2
Celia Baez-Castillo2 Isabel Mateo-Gavira
Isabel Mateo-Gavira