
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Immunol., 01 February 2023
Sec. Autoimmune and Autoinflammatory Disorders : Autoimmune Disorders
Volume 14 - 2023 | https://doi.org/10.3389/fimmu.2023.1087925
This article is part of the Research TopicMethods in Autoimmune and Autoinflammatory Disorders: 2022View all 11 articles
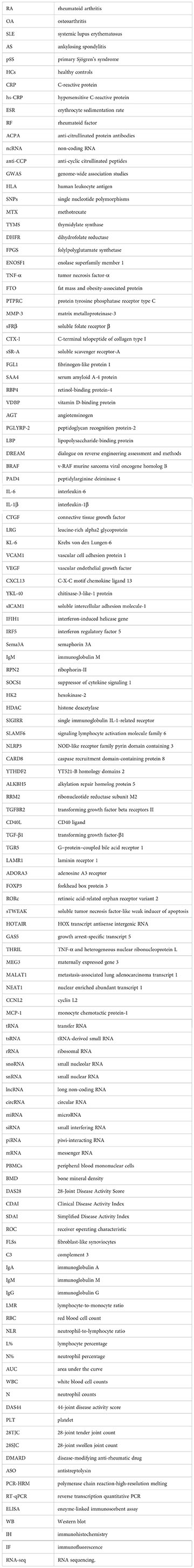
In recent years, diagnostic and therapeutic approaches for rheumatoid arthritis (RA) have continued to improve. However, in the advanced stages of the disease, patients are unable to achieve long-term clinical remission and often suffer from systemic multi-organ damage and severe complications. Patients with RA usually have no overt clinical manifestations in the early stages, and by the time a definitive diagnosis is made, the disease is already at an advanced stage. RA is diagnosed clinically and with laboratory tests, including the blood markers C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) and the autoantibodies rheumatoid factor (RF) and anticitrullinated protein antibodies (ACPA). However, the presence of RF and ACPA autoantibodies is associated with aggravated disease, joint damage, and increased mortality, and these autoantibodies have low specificity and sensitivity. The etiology of RA is unknown, with the pathogenesis involving multiple factors and clinical heterogeneity. The early diagnosis, subtype classification, and prognosis of RA remain challenging, and studies to develop minimally invasive or non-invasive biomarkers in the form of biofluid biopsies are becoming more common. Non-coding RNA (ncRNA) molecules are composed of long non-coding RNAs, small nucleolar RNAs, microRNAs, and circular RNAs, which play an essential role in disease onset and progression and can be used in the early diagnosis and prognosis of RA. In this review of the diagnostic and prognostic approaches to RA disease, we provide an overview of the current knowledge on the subject, focusing on recent advances in mRNA–ncRNA as diagnostic and prognostic biomarkers from the biofluid to the tissue level.
Rheumatoid arthritis (RA) is the most common chronic systemic autoimmune disease. Its etiology is unknown. The current global prevalence of RA, increasing over time (1), is approximately 0.5% to 1%. Occurring primarily in women, RA is associated with considerable disability and mortality, presenting a serious public health problem (2). The prognosis of RA is closely associated with the disease stage at the time of diagnosis. The lack of treatment in the setting of a late RA diagnosis leads to serious systemic disease with systemic multi-tissue and multi-organ damage, with a consequent high disability, mortality, and negative socioeconomic consequences (3). On the other hand, the early diagnosis and treatment of RA can prevent or significantly delay disease progression in up to 90% of patients, thereby preventing irreversible joint damage and disability (4).
The ability to detect reliable RA biomarkers early would be a promising medical advantage, shifting the “window of opportunity” to the preclinical phases of RA (5). These markers can be utilized to identify the early stages or susceptibility to the disease and to monitor the effects of treatment during the course of the disease, thereby determining the prognosis of the patient. In addition, those who undergo early screening may benefit from active early treatment, and patients at high risk of developing RA could receive preventive interventions to reduce the risk of RA progression from an indiscriminate inflammatory arthritis to classifiable RA (6), minimize RA risk factors, and adjust treatment regimens based on frequent surveillance results.
Although RA develops with genetic and epigenetic components, environmental factors also play an important role (7). Gene–environment interactions trigger autoimmune dysregulation (8), and sustained immune cell activation leads to a chronic inflammatory state. Progressive accumulation results in the loss of joint function and systemic multi-tissue organ damage. Studies have estimated the genetic risk of RA to be approximately 50%, and two types of RA can be classified according to the presence or absence of ACPA, with associated differences in risk factors, including ACPA+ patients showing a higher correlation with genetic factors (9).
Ubiquitous RA-specific autoantigens cannot be completely removed, and antigens modified by citrullination, acetylation, and carbamylation trigger antibody responses relevant to RA pathogenesis (10, 11). These autoantibodies form immune complexes that attract immune cells (12), which is believed to be the principal molecular mechanism contributing to RA pathogenesis. RA is a highly heterogeneous disease because of molecular variation in primary genetic factors and the various expression patterns of synovial tissue, as well as the heterogeneity of cells associated with RA pathogenesis [e.g., fibroblast-like synoviocytes (FLSs), macrophages, monocytes, and mast cells] (13). This heterogeneity in the molecular pathogenesis of RA is important in clinical practice because identifying these subtypes with different subtype-specific genetic markers can direct the “precision individualized diagnosis and treatment management” of RA patients. In addition, clinical monitoring of RA symptoms can improve patients’ physical and mental health (14).
According to the ACR/EULAR (the American College of Rheumatology and the European League Against Rheumatism) 2010 RA classification criteria, the diagnosis of RA requires patients to have swelling in at least one joint on clinical examination. Confirmation is followed by a sensitive assessment of the involved joint (those with tenderness, with positive plain film/CT, or ultrasound or MRI are classified as active), combined with serological biomarkers (RF and ACPA) and acute phase reactants (ESR and CRP). Finally, a scoring system is applied (patients with a score ≥6 are classified as having RA). However, when the imaging shows RA erosion features, the scoring system may not be applied, and RA can be classified directly (1, 15). The original impetus for the RA classification criteria was to include patients in the early stages of the disease so they could benefit from early and active treatment. Before reaching the clinical symptom phase, the patient has gone through the preclinical “healthy life” phase, and the pathophysiological changes of RA have occurred throughout the body without treatment (16).
All of these diagnostic methods have certain limitations. Ultrasound is an operator skill- and experience-dependent technology in terms of measurement and quality evaluation (17). Plain film/CT examinations can be harmful with ionizing radiation and have limited soft tissue contrast (18). Although MRI is highly accurate for early RA detection, it is limited by the cost of routine use and the inability to image multiple sites with a single test (19). For laboratory tests, ESR and CRP are usually used to check the general inflammatory status of patients, and RF and ACPA are found in RA and healthy donors and patients with other diseases; notably, ACPA is harmful in some RA patients (20). These laboratory tests are used in clinical practice, but their sensitivity and specificity are moderate and have limited value for early diagnosis, subtype classification, and prognosis (21). Therefore, many studies used biofluids or tissues to establish innovative screening programs targeting abnormal proteins, mRNA expression, genetic variation, and epigenetic variation (e.g., DNA methylation, histone modification, ncRNA, bromodomain, and sirtuin) (22–26). Identifying molecular markers based on protein, DNA, or RNA to develop novel non-invasive or minimally invasive blood or tissue RA biomarker detection methods has become a worldwide research focus (22, 27–29).
Many genome-wide association studies (GWAS) have identified genetic factors and the molecular variation underlying them (30–33), with the most evident aspects including class II human leukocyte antigen (HLA) genes (e.g., HLA-DRB1), protein tyrosine phosphatase non-receptor 22 (PTPN22), peptidyl arginine deiminase type IV (PADI4) (34), chemokine receptor genes (e.g., CCR6), signal transducer and activator of transcription 4 protein (STAT4), cytotoxic T-lymphocyte antigen 4 (CTLA4), and the B-cell cell surface receptor gene (CD40) (35). These genetic factors predispose individuals to RA and may serve as a susceptibility criterion for early RA diagnosis (13). Similarly, in another GWAS comprising 262 ACPA-negative early RA patients, 33 single nucleotide polymorphisms (SNPs) were shown to be associated with joint destruction, with rs2833522 being related to the severity of bone destruction (36). In addition, the GWAS analysis of 457 RA patients’ response to methotrexate (MTX) therapy identified 10 novel risk loci associated with a poor response to MTX, of which thymidylate synthase (TYMS), dihydrofolate reductase (DHFR), folylpolyglutamate synthetase (FPGS), and enolase superfamily member 1 (ENOSF1) were validated genes (37). In a GWAS analysis of 2,706 RA patients, Ming Li et al. identified an SNP (rs6427528) at the 1q23 locus that was related to changes in the disease activity scores of patients undergoing etanercept [an anti-tumor necrosis factor-α (TNF-α) drug] treatment. This SNP could disrupt transcription factor binding site motifs in the 3′UTR of CD84 (an immune-related gene), and the allele correlated with a better etanercept response was related to higher CD84 gene expression levels in peripheral blood mononuclear cells (38). Moreover, other studies have shown that the rs7195994 variant at the fat mass and obesity-associated protein (FTO) gene locus was associated with an improved clinical response to infliximab (39) and that the protein tyrosine phosphatase receptor type C (PTPRC) rs10919563 SNP was relevant to having an excellent response to anti-TNF-α therapy in RA patients (40).
Sperm-associated antigen 16 (SPAG16) has a protective effect on the joints by influencing the regulation of matrix metalloproteinase-3 (MMP-3) in autoantibody-positive RA and is associated with a good prognosis in RA patients (23). Elevated serum 14-3-3η protein was associated with more serious joint erosion and worse treatment outcomes in RA patients. It could be used as a biomarker to assess the diagnosis, prognosis, and therapy response (41). In addition, serum soluble folate receptor β (sFRβ) levels could act as a biomarker of disease activation and the anti-TNF drug response (42). Studies have shown that the C-terminal telopeptide of collagen type I (CTX-I) and CTX-II in biofluids could be used as markers of bone resorption and cartilage degradation in RA, respectively, to predict the degree of joint damage and monitor the therapy response (43). A large study showed that serum calcineurin levels correlate with disease activity and severity in RA (44). A multicenter study identified soluble scavenger receptor-A (sSR-A) as a potential diagnostic biomarker and therapeutic target of RA and fibrinogen-like protein 1 (FGL1) as a specific biomarker that could help predict RA progression (45, 46). The four-biomarker panel [serum amyloid A-4 protein (SAA4), retinol-binding protein-4 (RBP4), vitamin D-binding protein (VDBP), and angiotensinogen (AGT)], autoantibodies against peptidoglycan recognition protein-2 (PGLYRP-2), and lipopolysaccharide-binding protein (LBP) could be promising serum biomarkers for early diagnosis and disease activity assessment in seronegative RA patients (47–49).
A study predicting the anti-TNF-α drug response of RA patients by machine learning using the Dialogue on Reverse Engineering Assessment and Methods (DREAM) to validate and evaluate patient data correctly categorized responses from 78% of patients and found that specific genetic markers were shared by distinct populations and identifying them could improve the prediction of anti-TNF-α therapy efficacy (50).
Furthermore, the following are some examples of currently used and well-studied biomarkers that play a crucial role in the diagnosis and prognosis of RA: acute phase (serum amyloid A, ferritin, and procalcitonin), antibody [antibodies against v-RAF murine sarcoma viral oncogene homolog B (BRAF), antibodies against peptidyl arginine deiminase 4 (PAD4), anti-mutated citrullinated vimentin antibodies, and anti-carbamylated and anti-acetylated protein antibodies], pathogenesis- and bone metabolism-related [interleukin-6 (IL-6)/interleukin-1β (IL-1β)/TNF-α, connective tissue growth factor (CTGF), leucine-rich alpha2 glycoprotein (LRG), Krebs von den Lungen-6 (KL-6), vascular cell adhesion protein 1 (VCAM1), vascular endothelial growth factor (VEGF)/EGF, MMP1/MMP3, C-X-C motif chemokine ligand 13 (CXCL13)/CXCL16/chitinase-3-like-1 protein (YKL-40), and soluble intercellular adhesion molecule-1 (sICAM1)] (20, 26, 51). Currently, the diagnostic test markers for RA also include ESR, CRP, RF, ACPA, serum DNA, cell-free nucleic acid, histone modification, and other circulating DNA methylation biomarkers (hypermethylated genes: DUSP22, DR3, IL-10; hypomethylated genes: IL-6, STA3, STAT4, CXCL12, IFIH1, DUSP22, IRF5 (52), mRNA, and ncRNA) (53).
The complete analysis of the whole human genome has shown that nearly 70%–90% of the genome has been transcribed into RNA (54). Only 1.1% of the genome comprises coding sequences, and approximately 24% has been transcribed into pre-mRNAs with introns. Finally, ncRNAs are transcripts explaining the role of the remaining 75% of the genome (55, 56). The biological importance of ncRNAs has been demonstrated by their discovery in almost all joint tissues and biofluids of different species. Furthermore, ncRNAs could act as master regulators of gene expression in a series of biological processes such as epigenetic, transcriptional, splicing, and translation. The specific expression profiles of ncRNAs in various disease states support their roles as mediators of pathogenic mechanisms, potential therapeutic targets, and promising candidate biomarkers (57) and their extensive involvement in the development and progression of many diseases, including RA (58).
The ncRNAs are divided into two major categories: housekeeping ncRNAs comprise transfer RNA (tRNA), ribosomal RNA (rRNA), small nucleolar RNA (snoRNA), and small nuclear RNA (snRNA), and regulatory ncRNAs, which are involved in regulating transcription and RNA processing and translation, comprise long non-coding RNA (lncRNA), circular RNA (circRNA), microRNA (miRNA), small interfering RNA (siRNA), and Piwi-interacting RNA (piRNA) (59–61).
mRNAs are transcribed from DNA, carry genetic information, and act as templates in protein synthesis (62). In a study including 130 RA patients, semaphorin 3A (Sema3A) mRNA expression was 1.8-fold higher in peripheral blood mononuclear cells (PBMCs) of RA patients than in healthy controls (HCs). It was correlated with RF, immunoglobulin M (IgM), ESR, platelet counts, lumbar spine bone mineral density (BMD), and the Sharp score. The optimal diagnostic cutoff value of 10.881 ng/ml for Sema3A was based on the receiver operating characteristic (ROC) curve (63). In addition, ribophorin-II (RPN2) mRNA expression was significantly upregulated in the PBMCs of RA patients in a case–control study sample. The RPN2 gene affects the growth and activation of T lymphocytes and is involved in the pathogenesis of RA; it could serve as a novel biomarker for RA diagnosis (64). IL-37 mRNA levels in the plasma of RA patients in the training cohort were measured by reverse transcription quantitative PCR (RT-qPCR) and found to be significantly increased compared with HCs. The levels were also correlated with 28-Joint Disease Activity Score (DAS28)-ESR and CRP, which have good diagnostic ability to predict RA [area under the curve (AUC) = 0.97]. Furthermore, in a validation cohort of 598 patients comprising 230 RA patients, this finding suggested a higher specificity of IL-37 in identifying RA compared with patients with OA (AUC = 0.87), systemic lupus erythematosus (SLE) (0.86), gout (0.91), ankylosing spondylitis (AS) (0.92), and primary Sjögren’s syndrome (pSS) (0.87) (65). A significant inverse association between the suppressor of cytokine signaling 1 (SOCS1) mRNA expression levels in the PBMCs of RA patients and disease activity was seen in four independent patient cohort studies comprising 281 RA patients, a finding that can guide prognostic stratification and treatment decisions (66).
A study including 65 RA patients showed that hexokinase-2 (HK2) mRNA levels in PBMCs were positively associated with Clinical Disease Activity Index (CDAI), DAS28-ESR, and Simplified Disease Activity Index (SDAI) scores, independently correlated with increased disease activity risk, and may be involved in the molecular mechanisms of RA, and that HK2 could be a prospective candidate marker for RA diagnosis (RA vs. HCs, AUC = 0.808; RA vs. OA, AUC = 0.655) (67). Analysis of histone deacetylase (HDAC) mRNA expression levels in the PBMCs of 48 RA patients revealed a significant reduction and negative association with disease characteristics. Therefore, HDAC mRNA might play an essential role in the pathogenesis of RA (68). The single immunoglobulin IL-1-related receptor (SIGIRR) mRNA expression was decreased in the PBMCs of RA patients in a study including 79 such patients, and SIGIRR dysregulation might be related to RA pathogenesis and susceptibility (69). In a recently published study of 650 patients with RA, signaling lymphocyte activation molecule family 6 (SLAMF6) expression in the synovial tissue was 1.6-fold higher than in the controls and correlated with the severity and susceptibility of RA (70). An analysis showed that mRNA expression of the inflammasome genes NOD-like receptor family pyrin domain containing 3 (NLRP3) and caspase recruitment domain-containing protein 8 (CARD8) in the PBMCs of 230 RA patients from two different populations was correlated with susceptibility and RA progression (p = 0.044) and with severity (p = 0.03), respectively; in addition, the NLRP3 expression levels were also significantly elevated (71).
One study showed that serum mRNA expression levels of YT521-B homology domains 2 (YTHDF2), alkylation repair homolog protein 5 (ALKBH5), and FTO from a population of 79 RA patients were significantly decreased (p < 0.05). The expression of ALKBH5 mRNA was significantly upregulated after regular treatment (therapeutic regimens with corticosteroids and immunosuppressive drugs) (72). FTO mRNA expression occurs in association with DAS28, IgG, complement 3 (C3), and lymphocyte-to-monocyte ratio (LMR), and YTHDF2 mRNA expression was correlated with red blood cell count (RBC), neutrophil-to-lymphocyte ratio (NLR), LMR, lymphocyte percentage (L%), and neutrophil counts (N%) (72). The serum mRNA levels of ribonucleotide reductase subunit M2 (RRM2) were elevated, and the PBMCs of RA patients had an area under the curve (AUC) of 0.941 (p < 0.0001; sensitivity = 86.7%; specificity = 90.4%); in addition, significant correlations were observed between RRM2 and DAS-28, CDAI, and swollen and tender joints (73). Furthermore, a study comprising two cohorts with 17 RA patients showed that transforming growth factor beta receptors II (TGFBR2) was lacking in PBMCs, and the expression level of TGFBR2 mRNA might reflect RA disease activity (74). An analysis of 38 female RA patients revealed that CD40 ligand (CD40L) mRNA was overexpressed (p < 0.0001) and showed a clear correlation with clinical activity when the data were stratified per DAS28 and a progressive increase in CD40L expression (75). Another study analyzed plasma IL-38 mRNA expression levels in RA patients in a training cohort that included 130 RA patients and a validation cohort of 250 RA patients, respectively, showing that the levels were significantly higher in the RA patient group. In addition, its expression levels correlated with inflammatory parameters at baseline and in subsequent studies, and treatment significantly decreased IL-38 expression, suggesting that IL-38 might be a potential biomarker for RA (sensitivity = 0.723, specificity = 0.906, and AUC = 0.840) (76).
CD26 mRNA expression was found to be 1.68 times higher in RA patients compared with controls (p = 0.001), and there was a strong positive association between DAS28 (p = 0.002) and bone erosion in the hands (p = 0.049) (77). In a study including 104 RA patients, FURIN mRNA expression was significantly increased in the peripheral blood of RA patients (p < 0.001), and this was positively correlated with TGF-β1, RF, and anti-CCP (78). Another study comprising 187 patients with RA showed that serum IL-10 mRNA expression was 3.63-fold higher than in controls. There appeared to be a significantly positive correlation with anti-CCP, RF, and CRP (79).
One study comprising 74 RA patients found that YTHDF2 mRNA expression was significantly decreased in RA PBMCs and negatively associated with IL-1β, CRP, ESR, white blood cell counts (WBC), neutrophil counts (N), N%, and NLR values but was correlated with RF and the treatment response (80). G−protein−coupled bile acid receptor 1 (TGR5) mRNA expression was significantly decreased (p < 0.001) in RA PBMCs (n = 50), and there was a negative correlation between DAS28 (p = 0.006) and CRP (p = 0.002) (81). Furthermore, IL-35 mRNA expression and Treg frequency were significantly lower in RA patients (n = 55) than HCs (n = 20), and IL-35 levels were negatively associated with ESR and DAS28, suggesting that IL-35 and Tregs play a protective role in the development of RA (82).
Microarray analysis revealed that class 3 and 4 semaphorins and their receptors are overexpressed in RA patients. The serum mRNA levels of semaphorins were associated with the levels of proangiogenic and inflammatory markers, thus identifying them as therapeutic candidates and potential biomarkers for RA (83). The PBMC levels of laminin receptor 1 (LAMR1) mRNA are downregulated in early RA patients and might be an independent predictor of poor anti-TNF-α therapy response; in addition, these levels are associated with increased disease activity scores (84). IL-32 mRNA expression was higher in PBMCs from RA patients compared with healthy individuals and might play a role in predicting the response to anti-TNF-α therapy (85). FPGS 8PR/8WT ratios in the whole blood of RA patients might have a predictive value for the treatment response to MTX, with higher baseline ratios tending toward a poorer treatment response and higher DAS44 scores (86). Similarly, the whole blood mRNA levels of adenosine A3 receptor (ADORA3) in RA patients were correlated with a non-response to MTX therapy (AUC = 0.7, p = 0.006), and the baseline expression levels of ADORA3 mRNA might be a predictive biomarker of MTX response (87).
In summary, the abnormal expression of mRNAs in peripheral blood, plasma, serum, PBMCs, synovial tissue, and T cells of RA patients has potential application prospects for the early diagnosis, prognostic assessment, disease activity, and treatment response monitoring in RA. These examples demonstrate that mRNA expression patterns are, to some extent, potentially disease-specific but still have limitations. To date, the number of conducted studies remains small, and the lack of high-quality studies inevitably reduces their credibility. Moreover, the biofluids and tissues involved in these studies remain limited. Future studies should include urine, meniscus, and macrophages, among other factors. These potential mRNA-based biomarkers are summarized in Table 1.
miRNAs are small endogenous ncRNAs of 18–24 nucleotides in length that participate in the post-transcriptional regulation of gene expression (94). miRNAs can act as inhibitory regulators by inhibiting the translation or degradation of mRNAs and can also increase the expression of target genes by improving the translation rates (95). They are essential for developing the immune system and regulation (96). In addition, miRNAs have high tissue specificity and are expressed differentially in various tissues (97). An analysis of circulatory miRNAs comprising 50 RA patients showed that miR-126-3p, miR-221-3p, let-7d-5p, miR-431-3p, miR-24-3p, and miR-130a-3p were significantly elevated in the serum of RA patients and “at-risk individuals,” as well as miR-130a-3p combined with the remaining five to yield a higher AUC. Both let-7i-5p and miR-339-5p are significantly decreased post-MTX, which may help in the early diagnosis of RA and monitoring of treatment response or risk of recurrence (98). miR-223 serum expression levels are significantly upregulated in RA patients and could distinguish RA patients from HCs with the AUC (0.85), serving as a potential biomarker for RA diagnosis and risk prediction (99).
An analysis using a next-generation sequencing approach suggested that serum levels of miR-16-5p and miR-223-3p were significantly lower in early RA patients than in established RA patients and HCs and were involved in the pathophysiology of RA. Furthermore, miR-16-5p and miR-223-3p could serve as biomarkers and possible predictors of disease outcomes for early RA (100). The expression of miR-224, miR-483-5p, miR-760, miR-375, and miR-378 is significantly upregulated in the serum of RA patients (n = 80) compared with controls (p < 0.05), and there is a significantly positive association between these miRNAs and DAS28 scores (p < 0.001), suggesting that the serum expression of these miRNAs could be used as biomarkers for the early diagnosis of RA and targets for therapy (101).
The expression of miR-146a was found to be significantly elevated in the peripheral blood of RA patients (n = 76) and positively correlated with RA severity, retinoic acid-related orphan receptor variant 2 (RORc), IL-17 levels, and the Th17 cell ratio, yet significantly negatively associated with the Treg cell ratio, TGF-β1, and forkhead box protein 3 (FOXP3) levels, suggesting that it may serve as a biomarker for disease progression and prognosis in RA patients (102). miR-361-5p is significantly more highly expressed in whole blood from early RA patients, with ROC analysis showing AUC = 0.76 and p < 0.05, identifying it as a potential biomarker for early RA (103).
A study including 125 patients with RA showed that circulating plasma miR-155 levels were significantly downregulated in RA patients compared with HCs. In contrast, the levels of whole blood miR-155 gene methylation were upregulated, suggesting that these were potentially helpful biomarkers for RA diagnosis (104). miR-146a-5p, miR-125a-5p, and miR-24-3p were upregulated in the plasma of RA patients, and their expression was significantly different in the subgroups of RA patients with varying disease activity. ROC curve analysis indicated good AUC values, sensitivity, and specificity for all three miRNAs, suggesting that these miRNAs could be used as biomarkers for RA diagnosis and disease activity (105). The expression of miR-22-3p and let-7a-5p was significantly upregulated in the plasma of RA patients, which could identify the RA populations and, in combination with anti-CCP and RF, could improve the diagnostic ability of RA (especially seronegative RA) (106).
miR-23b levels were found to be significantly elevated in the synovial tissue cells and plasma of RA patients and positively correlated with platelet (PLT) counts, CRP, hypersensitive-CRP (hs-CRP), ESR, and DAS28 (p < 0.05), and treatment reversed the trend of elevated plasma miR-23b levels (107). Moreover, miR-23 could regulate CXCL12 through the NF-κB signaling pathway to suppress the inflammation involved in RA pathogenesis (108). The miR-5571-3p and miR-135b-5p levels in the synovial tissues of RA patients were positively associated with disease activity and the inflammation level, with an AUC of 0.833 when the two were combined and had a good predictive value for RA risk (109).
An analysis of 79 RA patients revealed that serum exosome-encapsulated miR-6089 was significantly reduced in RA patients and may regulate inflammatory responses by directly targeting TLR4 signaling (110). miR-204-5p expression was downregulated in the plasma exosomes of RA patients. It was inversely associated with disease parameters (e.g., RF, CRP, and ESR), which translates communication between immune cells and FLSs and could be used as a potential biomarker for the diagnosis and treatment of RA (111). miR-451a and miR-25-3p are significantly elevated in serum exosomes (secretory extracellular vesicles) from patients with early RA, and when combined with soluble tumor necrosis factor-like weak inducer of apoptosis (sTWEAK), they correctly distinguish 95.6% of patients (ROC = 0.983, specificity = 100%, and sensitivity = 85.7%); they could be used as a panel of serum biomarkers for early RA diagnosis (112). The levels of miR-548a-3p in serum exosomes and PBMCs of RA patients are significantly downregulated and negatively correlated with the levels of RF, ESR, and CRP, suggesting that the miR-548a-3p/TLR4/NF-κB axis could be used as a biomarker for RA diagnosis and targets for therapy (113). Serum exosome miR-1915-3p expression is significantly elevated in RA patients with clinical remission and negatively associated with CRP levels, which may be a potential biomarker of disease activity in Korean RA patients (114). Exosomes participate in cell-to-cell communication via the packaging and shuttling of diverse cargo molecules (including miRNAs) to recipient cells and have a crucial role in autoimmune-related disorders (115, 116). In addition, miRNA cargo of exosomes has shown potential diagnostic value as biomarkers in several autoimmune diseases (117).
Notably, hsa-miR-146a-5p, hsa-miR-132-3p, and hsa-miR-155-5p were found to be expressed at high levels in the whole blood of RA patients (n = 94). Baseline levels of all three miRNAs were reduced in responders compared with non-responders post-MTX. They were also shown to be potential biomarkers of response to MTX treatment by ROC curve analysis (118). miR-29, miR-26b, miR-522, and miR-451 are significantly differentially expressed in responders compared with non-responders to olokizumab treatment in the plasma of RA patients. ROC curve and regression analyses showed that all four miRNAs were statistically associated with olokizumab treatment efficiency scores and might be potential biomarkers of therapeutic response (119). One study showed no direct effect of tofacitinib treatment on measured miRNA expression in RA patients but found that changes in has-miR-194-5p and has-miR-432-5p might be correlated with proinflammatory pathway regulation and RA flare-ups (120). Another study of 96 RA patients showed a significant upregulation of miRNA-125a and miRNA-125b expression in the plasma of RA patients, which was positively correlated with CRP and tender joint count (TJC), swollen joint count (SJC), ESR, CRR, and DAS28-ESR. The biomarker expression was gradually decreased post-infliximab and was significantly higher in responders at baseline, suggesting that these biomarkers indicate disease activity and response to infliximab treatment (121).
In conclusion, the aberrant expression of miRNAs in the peripheral blood, plasma, serum, PBMCs, synovial tissue, and exosomes of RA patients provides promising new directions for early diagnosis, prognostic assessment, disease activity, and treatment response monitoring in RA. Studies of ncRNAs in RA have focused on miRNAs and have concentrated on circulating biofluids, available through minimally invasive blood draws. These examples suggest that miRNA expression patterns are, to some extent, not only body fluid- or tissue-specific but may also be disease-specific. However, the selection of participants should consider the use of appropriate inclusion and exclusion criteria to facilitate the interpretation of study results and to combine them with other studies for more in-depth analysis. The potential miRNA-based biomarkers for the diagnostic and prognostic assessment of RA are summarized in Table 2.
lncRNA plays a crucial role in different biological processes by interacting with DNA to modulate epigenetic modifications, transcription, post-translational modifications, and protein/RNA stability (143). The ROC curve analysis of the expression of lncRNA TSPEAR-AS2 and its target miR-212-3p in the plasma of 73 RA patients showed that TSPEAR-AS2 expression was significantly downregulated and inversely associated with miR-212-3p levels. Regulation of HFLS apoptosis by the TSPEAR-AS2/miR-212-3p axis is involved in the pathogenesis of RA (144). lnc-ITSN1-2 could be a convincing biomarker for RA diagnosis and monitoring of disease activity as it is significantly upregulated in the plasma and synovial tissues of RA patients and positively correlated with DAS28, ESR, and CRP. Notably, the ROC curve analysis showed that lnc-ITSN1-2 had good diagnostic value (AUC = 0.898, specificity = 80%, and sensitivity = 90%) (145, 146).
The expression levels of HOX transcript antisense intergenic RNA (HOTAIR) and lnc-Cox2 were found to be significantly higher in the serum of RA patients compared with healthy subjects, and the ROC curve indicated that it could distinguish RA patients from other populations, serving as a novel non-invasive biomarker for RA diagnosis (147). LINC00305 expression was significantly upregulated in the serum of RA patients and was positively associated with DAS28, anti-CCP, RF, ESR, and CRP. In addition, patients carrying the LINC00305 AT and TT genotypes (rs2850711 polymorphism) had significantly increased DAS28 scores and LINC00305, NF-κB, and MMP-3 levels, suggesting that LINC00305 and its variant rs2850711 (A/T) might serve as biomarkers for the diagnosis and management of RA (148). PlncRNA-1 and its target TGF-β1 expression are significantly decreased and positively correlated in the serum and FLSs of patients with active RA compared with HCs. The levels of plncRNA-1 could differentiate active RA patients from other populations, and it may be involved in the pathogenesis of RA by regulating TGF-β1 (149). Based on the results of ROC analysis, OSER1-AS1 levels in serum and synovial tissue could differentiate RA from HCs with better specificity and sensitivity than RF and anti-CCP, and OSER1-AS1 could be used as a potentially promising biomarker for diagnosis and treatment (150).
RNA sequencing and qPCR validation analysis showed that lnc-AL928768.3 and lnc-AC091493.1 expression levels were elevated in the synovial tissues of RA patients and positively correlated with DAS28-ESR and CRP, which when combined with ROC curve analysis suggested that they are good biomarkers for predicting RA risk and disease activity (151). LINK-A was significantly highly expressed in synovial tissues and FLSs of RA patients and positively associated with the severity of synovitis in RA patients. LINK-A regulates RA FLS invasion and inflammation through HIF-1α and/or miR-1262 pathways, which might be a promising therapeutic target for RA (152). lncRNA growth arrest-specific transcript 5 (GAS5) is significantly downregulated in synovial tissues, serum, and PBMCs of RA patients compared with HCs and negatively correlated with IL6, IL-17, CRP, ESR, DAS28, and anti-CCP, suggesting that it could be used as a potential biomarker for RA diagnosis (153–156). Interestingly, lncRNAs GAS5 (3.31-fold), RNA component of mitochondrial RNA-processing endoribonuclease (RMRP) (2.43-fold), and TNF-α and heterogeneous nuclear ribonucleoprotein L (THRIL) (2.14-fold) were significantly upregulated in the circulating T cells of RA patients compared with controls, and the ROC curve analysis of the three indicated their value in discriminating RA patients from controls (157).
The expression level of RP11-83J16.1 was found to be increased in the synovial fluid of RA patients, which correlated with increased disease activity and inflammation in RA patients (158). Maternally expressed gene 3 (MEG3) expression was downregulated, and metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) and nuclear enriched abundant transcript 1 (NEAT1) expression were upregulated in the synovial fluid, plasma, and PBMCs of RA patients, and MEG3 and NEAT1 with TJC, NEAT1 with SJC, and DAS28-CRP showed significant correlations, suggesting that they might be used as biomarkers to monitor disease activity (159). Another study showed that MEG3 in PBMCs was negatively associated with disease activity, lesion joints, and inflammation in RA patients (n = 191), which could be used as a biomarker in monitoring the treatment efficacy of RA (160).
Compared with HCs, the expression of ENST00000619282 and MIR22HG was found to be upregulated in the PBMCs of RA patients. However, the expression of DSCR9, MAPKAPK5-AS1, and LINC01189 was downregulated. These five lncRNAs were associated with patients’ self-perception and with their clinical indexes (e.g., RF, IgA, IgG, and C3). The ROC curve analysis suggested that these lncRNAs were correlated with apoptosis and autophagy and could be used as promising biomarkers for diagnosing and monitoring RA progression (161). LINC00638 levels were significantly reduced in the PBMCs of RA patients (n = 45) compared with normal controls. The levels were negatively associated with DAS28, ROS, IL-17, and ESR, which might inhibit inflammation and oxidative stress by activating the Nrf2/HO-1 pathway (162).
The upregulation of lnc-NEAT1 levels in the PBMCs of RA patients was found to be negatively associated with the expression levels of its targets (miR-125a and miR-21). They were significantly associated with ESR, CRP, and DAS28-ESR scores, and lnc-NEAT1 expression levels were significantly decreased in remission compared with non-remission patients; these biomarkers might indicate RA treatment efficacy and disease activity (163). The lnc-RNU12 expression levels were significantly downregulated in the PBMCs and T-cell subsets of RA patients. This finding suggested that these biomarkers might be involved in the pathogenesis of RA by targeting cyclin L2 (CCNL2) and c-JUN, which affect the T-cell cycle (164). The expression levels of LINC00304, LINC01504, FAM95B1, and lncRNAs were decreased in the PBMCs of RA patients, but the MIR503HG level was increased. Based on the correlation analysis, these lncRNAs were correlated with clinical or laboratory indicators such as disease duration, joint tenderness, arthrocele, RF, and IgG. The lncRNAs might be potential biomarkers for diagnosing RA (165).
The clinical response prediction model comprising lncRNAs RP3-466P17.2, RP11-20D14.6, RP11-844P9.2, and TAS2R64P in PBMCs showed good predictive capability for the etanercept treatment response (AUC = 0.956). This finding suggests that they might be useful biomarkers for the response to etanercept treatment in RA patients (166).
Therefore, the abnormal expression of lncRNAs in RA patients’ peripheral blood, plasma, serum, PBMCs, synovial tissue, synovial fluid, and T cells could be promising for early diagnosis, prognostic assessment, disease activity, and treatment response monitoring in RA. Most of these studies above were limited to the differential expression levels of ncRNAs in single biofluids or tissues. However, some suggested that the ncRNAs in the circulation might not be expressed at the same level as in the tissues. Therefore, multilevel analysis is necessary in the future. Currently, there is no consistent profile of ncRNAs identified or validated in RA studies, and the answer is even more unclear for clinical practice. The utility of these ncRNAs as biomarkers requires rigorous large-scale studies. The challenges of this approach include how to define patient groups, disease characteristics across studies, the analytical platforms used, and biofluid handling measures, which are unresolved and make it difficult to conduct direct comparisons of the findings across studies. These potential lncRNA-based biomarkers for RA diagnosis and prognosis are summarized in Table 3.
circRNAs are novel, approximately 500-nt endogenous ncRNAs noted to comprise closed round structures with high stability and are often characterized by tissue-specific expression and evolution-based conservation (186). circRNAs play many roles in various biological processes, including RNA maturation regulation, alternative splicing, protein localization, miRNA sponging, histone modifications, and protein translation (187). The levels of circ_0002715 and circ_0035197 have been found to be significantly elevated in the peripheral blood of RA patients compared with HCs, and circ_0002715 expression correlates with disease duration, RF, ACPA, TJC, and SJC. Studies on ROC curve analysis and logistic regression models have suggested that the combination of circ_0002715 and circ_0035197 might be a biomarker for diagnosis and disease activity in new-onset RA (AUC = 0.758, sensitivity = 72.9%, and specificity = 71.4%). They can differentiate RA patients from patients with SLE or AS and HCs (188).
circ_AFF2 levels were found in one study to be upregulated in the peripheral blood of RA patients, increasing TAB2 expression to promote RA progression by sponging miR-375, which can be used as a biomarker for RA diagnosis and treatment (189). circ-AFF2 overexpression induced an inflammatory response, proliferation, migration, and invasion of RA FLSs through regulation of the miR-650/CNP axis (190). A study including 77 RA patients showed that circ_0044235 was significantly downregulated in the peripheral blood of RA patients and might specifically identify RA patients from SLE patients. This finding suggests that circ_0044235 could serve as a potential biomarker for diagnosing RA patients (AUC = 0.779) (191). In addition, circ_0044235 is involved in RA development by promoting SIRT1 expression through sponge miR-135b-5p, which acts on the NLRP3-mediated pyroptosis pathway (192). circ_0005198 and circ_0005008 have been found to be significantly upregulated in the plasma from new-onset RA patients compared with SLE patients and HCs when evaluated by microarray and RT-qPCR analysis. These biomarkers are positively correlated with DAS28, RF, CRP, and ESR levels, suggesting that the circRNAs can be used as biomarkers of diagnosis (AUC = 0.783; 0.829) and disease activity for new-onset RA (193). The expression of circHIPK3 was found to be significantly upregulated in the serum of RA patients. It might be involved in RA pathogenesis by increasing monocyte chemotactic protein-1 (MCP-1) secretion through interactions with miRNA-124a to induce joint inflammation (194).
According to the ROC curve analysis, the diagnostic value of circPTPN22 could discriminate RA patients from SLE patients and HCs (AUC = 0.781; 0.934). circPTPN22 levels were found to be significantly downregulated in the PBMCs of RA patients and negatively correlated with RF, anti-CCP, CRP, IgA, IgM, and IgG levels. Further analysis suggested that this may be a potential biomarker for the diagnosis of RA and is involved in RA’s pathogenesis (195). ciRS-7 expression was significantly elevated in the PBMCs of RA patients and may potentially distinguish RA patients from HCs (AUC = 0.766). In addition, ciRS-7 sponges may relieve the inhibitory effect on mTOR by adsorbing miR-7 (196). The expression of hsa_circ_0140271 was found to be significantly upregulated in the PBMCs of female RA patients and positively associated with antistreptolysin (ASO). The hsa_circ_0140271 could discriminate female RA patients from those from populations with AS or OA and HCs, according to ROC curve analysis, which could increase diagnostic accuracy when combined with anti-CCP (AUC = 0.818) (197).
The expression levels of circNUP214 in PBMCs could distinguish RA patients from HCs (AUC = 0.76, sensitivity = 42.86%, and specificity = 96.43%). circNUP214 is highly expressed in RA patients and is positively correlated with serum anti-CCP and IL-23 receptor (IL-23R) expression levels. It is also involved in RA pathogenesis by regulating IL-23R in RA patients to promote Th17 cell response (198). The expression levels of circ_0000396 and circ_0130438 in the PBMCs of RA patients (n = 36) could serve as potential biomarkers for RA diagnosis, and they are significantly reduced in RA patients compared with HCs (199). Notably, circ_0008410 was significantly upregulated in the PBMCs of RA patients, while circ_0000175 was downregulated, and their expression levels were correlated with RA disease activity and severity. ROC curve analysis showed that the combination of both can improve the accuracy of RA diagnosis (AUC = 0.971, sensitivity = 93.10%, and specificity = 93.33%) and can distinguish RA patients from AS and SLE patients (200). hsa_circ_101328 was found to be significantly decreased in the PBMCs of RA patients and inversely associated with CRP. The ROC curve analysis (AUC = 0.957, sensitivity = 95.2%, and specificity = 95%) indicated that it might be an effective biomarker for RA diagnosis (201). In addition, circ_0001200, circ_0001566, circ_0003972, and circ_0008360 were significantly differentially expressed in the PBMCs of RA patients. These circRNAs were also significantly associated with clinical indicators of patient disease severity (e.g., DAS28, joint induration, and anti-CCP, IgG), which could serve as biomarkers for RA diagnosis (202).
Therefore, the abnormal expression of circRNAs in RA patients’ peripheral blood, plasma, serum, and PBMCs may be significant in early diagnosis, prognostic assessment, disease activity, and treatment response monitoring in RA. Circulating levels of lncRNAs or circRNAs can function as sponges of miRNA and protein or scaffolds for translation. lncRNAs and circRNAs can act by sponging miRNAs and consequently blocking their activity, and this sponging is also the mechanism by which different types of ncRNAs can interact. circRNAs can function by sponging miRNAs to reduce the number of miRNAs available to target mRNA, thus contributing to mRNA stability or protein expression. All these mechanisms allow lncRNAs and circRNAs to play an essential role in the differential expression and pathogenesis of RA (57). These potential circRNA-based biomarkers for RA diagnosis and prognosis are summarized in Table 4.
The tRNAs are essential components of the translation machinery that deliver amino acids to the ribosome and synthesize proteins under mRNA guidance. tRNA-encoding genes show tissue-specific and cell-type-specific expression patterns, and dysregulation of tRNAs and tRNA-derived small RNAs (tsRNAs) is involved in pathological processes (211). In addition, tsRNAs are involved in the regulation of rRNA synthesis, mRNA stability, transcription, and RNA reverse transcription and play an important role in cellular functions and in the occurrence and development of various diseases. tsRNAs may be potential biomarkers and therapeutic targets due to their structural stability, high conservation, and extensive distribution (particularly in biofluids, tissues, and exosomes) (212). The snoRNAs are primarily in charge of post-transcriptional modifications, directing the chemical modifications of rRNAs and snRNAs and fine-tuning spliceosome and ribosome function. The dysregulation of snoRNAs, potential biomarkers of disease, in various diseases has been widely reported, and they are potential candidates for biomarkers (213).
piRNAs are probably the most abundant (30,000 members in humans) sncRNAs of 24–31 nt in length, newly identified within the genome, and play important roles in the maintenance of germline integrity, transposon silencing, epigenetic regulation, and post-transcriptional and translational control. Many studies have implicated piRNAs as regulators of various diseases (214). Sequencing analysis of sncRNAs in the sera of DMARD-naive patients receiving 6 months of triple DMARD therapy identified five sncRNAs that were differentially expressed between responders and non-responders at baseline. The baseline expression levels of chr1.tRNA131-GlyCCC, chr2.tRNA13-AlaCGC, chr1.tRNA131-GlyCCC 5′ tiRNA, chr2.tRNA13-AlaCGC 5′ tiRNAs, snoRNA U2-L166, and piR35982 were significantly upregulated in non-responders compared with responders, while rRNA 5S-L612 was the unique sncRNA that was significantly elevated among responders. After treatment, chr1.tRNA131-GlyCCC expression was significantly reduced in ACPA and RF-positive patients and showed a significant positive association with TJC28, suggesting that elevated circulating levels of chr1.tRNA131-GlyCCC 5′ tiRNA may indicate increased inflammation. Similarly, snoRNA U2-L166 was positively correlated with TJC28. In addition, piR-35982 was significantly reduced in RF-positive patients and inversely associated with CRP and ESR levels. These findings suggest that baseline levels of sncRNAs could be a clinically useful biomarker of triple DMARD responsiveness (215). However, there are few studies on applying tRNAs, tsRNAs, snoRNAs, piRNAs, and rRNAs as biomarkers for RA. These potential biomarkers for the diagnostic and prognostic assessment of RA are summarized in Table 5.
RA is one of the most common and highly heterogeneous autoimmune diseases associated with a considerable increase in disability and mortality (216). Delayed diagnosis is one of the most critical problems in RA management. In the later stages of the disease, patients often experience functional decline and disability or even systemic multi-organ damage (2). Early RA diagnosis and treatment can prevent or significantly delay disease progression in up to 90% of patients, making early diagnosis of RA critical to patient prognosis (4). The 2010 ACR/EULAR criteria have enabled more early RA patients to be diagnosed compared with the 1987 ACR criteria, which are still limited, and many early RA patients are not diagnosed soon enough, thereby missing early disease management (217). Many countries are increasingly focusing on early screening and are exploring and developing less invasive or non-invasive techniques to improve the accuracy of early RA diagnosis. Therefore, significant progress is needed in this area to achieve an early and accurate diagnosis, personalized treatment, and monitoring of RA disease activity and treatment response.
Increasing evidence suggests that ncRNAs play a crucial role in the onset and progression of RA. Studies in transcriptomics and epigenetics and the maturation of high-throughput sequencing technologies have further improved our understanding of RA pathophysiology and pathogenesis. In this review, we described the potential of various RNAs to be promising biomarkers for RA, allowing biofluid biopsies in place of tissue samples and cell line models. Furthermore, not only do individual RNA biomarkers have diagnostic and prognostic value, but also the combined application of multiple RNA biomarkers often exhibits a higher diagnostic and prognostic specificity and sensitivity. The main advantage of RNAs as biomarkers is that they can be detected in various biofluids, which permits a non-invasive diagnosis to be made. There are many studies on RNA biomarkers in RA, but opinion is divided. There is lack of research on tRNA, tsRNA, snoRNA, snRNA, and piRNA as biomarkers for RA. Furthermore, future studies aim to identify which non-invasive diagnostic biomarkers for RA are feasible and cost-effective, to understand which biomarkers can better guide “precision individualized diagnosis and treatment management” of patients, and to better predict patient prognosis.
YJ and SZ organized the literature and original draft writing. JW and LL contributed to literature retrieval and data collation. SZ, SH, and JW contributed to the manuscript revision. HC and YY were responsible for the conception, writing review, and approval of the submitted version. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China (No. 81729003), the Science and Technology Program of Panyu (No. 2020-Z04-054), the Science and Technology Project of Guangzhou Health Commission (No. 20211A011114), and the Internal Scientific Research Fund of Guangzhou Panyu Central Hospital (2021Z001).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Smolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet (London England) (2016) 388(10055):2023–38. doi: 10.1016/s0140-6736(16)30173-8
2. Giles JT. Extra-articular manifestations and comorbidity in rheumatoid arthritis: Potential impact of pre-rheumatoid arthritis prevention. Clin Ther (2019) 41(7):1246–55. doi: 10.1016/j.clinthera.2019.04.018
3. Guo Q, Wang Y, Xu D, Nossent J, Pavlos NJ, Xu J. Rheumatoid arthritis: pathological mechanisms and modern pharmacologic therapies. Bone Res (2018) 6:15. doi: 10.1038/s41413-018-0016-9
4. Aletaha D, Smolen JS. Diagnosis and management of rheumatoid arthritis: A review. JAMA (2018) 320(13):1360–72. doi: 10.1001/jama.2018.13103
5. Petrovská N, Prajzlerová K, Vencovský J, Šenolt L, Filková M. The pre-clinical phase of rheumatoid arthritis: From risk factors to prevention of arthritis. Autoimmun Rev (2021) 20(5):102797. doi: 10.1016/j.autrev.2021.102797
6. Demoruelle MK, Deane KD. Treatment strategies in early rheumatoid arthritis and prevention of rheumatoid arthritis. Curr Rheumatol Rep (2012) 14(5):472–80. doi: 10.1007/s11926-012-0275-1
7. Scherer HU, Häupl T, Burmester GR. The etiology of rheumatoid arthritis. J Autoimmun (2020) 110:102400. doi: 10.1016/j.jaut.2019.102400
8. van der Woude D, Alemayehu WG, Verduijn W, de Vries RR, Houwing-Duistermaat JJ, Huizinga TW, et al. Gene-environment interaction influences the reactivity of autoantibodies to citrullinated antigens in rheumatoid arthritis. Nat Genet (2010) 42(10):814–6; author reply 6. doi: 10.1038/ng1010-814
9. Radu AF, Bungau SG. Management of Rheumatoid Arthritis: An Overview. Cells (2021) 10(11):2857. doi: 10.3390/cells10112857
10. Kronzer VL, Davis JM 3rd. Etiologies of rheumatoid arthritis: Update on mucosal, genetic, and cellular pathogenesis. Curr Rheumatol Rep (2021) 23(4):21. doi: 10.1007/s11926-021-00993-0
11. Lin YJ, Anzaghe M, Schülke S. Update on the Pathomechanism, Diagnosis, and Treatment Options for Rheumatoid Arthritis. Cells (2020) 9(4):800. doi: 10.3390/cells9040880
12. van Delft MAM, Huizinga TWJ. An overview of autoantibodies in rheumatoid arthritis. J Autoimmun (2020) 110:102392. doi: 10.1016/j.jaut.2019.102392
13. Zhao J, Guo S, Schrodi SJ, He D. Molecular and cellular heterogeneity in rheumatoid arthritis: Mechanisms and clinical implications. Front Immunol (2021) 12:790122. doi: 10.3389/fimmu.2021.790122
14. Hensvold A, Klareskog L. Towards prevention of autoimmune diseases: The example of rheumatoid arthritis. Eur J Immunol (2021) 51(8):1921–33. doi: 10.1002/eji.202048952
15. Kay J, Upchurch KS. ACR/EULAR 2010 rheumatoid arthritis classification criteria. Rheumatol (Oxford) (2012) 51 Suppl 6:vi5–9. doi: 10.1093/rheumatology/kes279
16. Rantapää Dahlqvist S, Andrade F. Individuals at risk of seropositive rheumatoid arthritis: the evolving story. J Intern Med (2019) 286(6):627–43. doi: 10.1111/joim.12980
17. Takase-Minegishi K, Horita N, Kobayashi K, Yoshimi R, Kirino Y, Ohno S, et al. Diagnostic test accuracy of ultrasound for synovitis in rheumatoid arthritis: systematic review and meta-analysis. Rheumatol (Oxford) (2018) 57(1):49–58. doi: 10.1093/rheumatology/kex036
18. Vyas S, Bhalla AS, Ranjan P, Kumar S, Kumar U, Gupta AK. Rheumatoid arthritis revisited - advanced imaging review. Pol J Radiol (2016) 81:629–35. doi: 10.12659/pjr.899317
19. Cohen SB, Potter H, Deodhar A, Emery P, Conaghan P, Ostergaard M. Extremity magnetic resonance imaging in rheumatoid arthritis: Updated literature review. Arthritis Care Res (Hoboken) (2011) 63(5):660–5. doi: 10.1002/acr.20413
20. Savvateeva E, Smoldovskaya O, Feyzkhanova G, Rubina A. Multiple biomarker approach for the diagnosis and therapy of rheumatoid arthritis. Crit Rev Clin Lab Sci (2021) 58(1):17–28. doi: 10.1080/10408363.2020.1775545
21. Radner H, Neogi T, Smolen JS, Aletaha D. Performance of the 2010 ACR/EULAR classification criteria for rheumatoid arthritis: a systematic literature review. Ann Rheum Dis (2014) 73(1):114–23. doi: 10.1136/annrheumdis-2013-203284
22. Chen Y, Ma C, Liu L, He J, Zhu C, Zheng F, et al. Analysis of gut microbiota and metabolites in patients with rheumatoid arthritis and identification of potential biomarkers. Aging (Albany NY) (2021) 13(20):23689–701. doi: 10.18632/aging.203641
23. Knevel R, Klein K, Somers K, Ospelt C, Houwing-Duistermaat JJ, van Nies JA, et al. Identification of a genetic variant for joint damage progression in autoantibody-positive rheumatoid arthritis. Ann Rheum Dis (2014) 73(11):2038–46. doi: 10.1136/annrheumdis-2013-204050
24. Nemtsova MV, Zaletaev DV, Bure IV, Mikhaylenko DS, Kuznetsova EB, Alekseeva EA, et al. Epigenetic changes in the pathogenesis of rheumatoid arthritis. Front Genet (2019) 10:570. doi: 10.3389/fgene.2019.00570
25. Viatte S, Plant D, Raychaudhuri S. Genetics and epigenetics of rheumatoid arthritis. Nat Rev Rheumatol (2013) 9(3):141–53. doi: 10.1038/nrrheum.2012.237
26. Takeuchi T. Biomarkers as a treatment guide in rheumatoid arthritis. Clin Immunol (2018) 186:59–62. doi: 10.1016/j.clim.2017.07.019
27. Lourido L, Blanco FJ, Ruiz-Romero C. Defining the proteomic landscape of rheumatoid arthritis: progress and prospective clinical applications. Expert Rev Proteomics (2017) 14(5):431–44. doi: 10.1080/14789450.2017.1321481
28. Luan H, Gu W, Li H, Wang Z, Lu L, Ke M, et al. Serum metabolomic and lipidomic profiling identifies diagnostic biomarkers for seropositive and seronegative rheumatoid arthritis patients. J Transl Med (2021) 19(1):500. doi: 10.1186/s12967-021-03169-7
29. Noh CK, Lee E, Park B, Ahn SS. A positive faecal immunochemical test result and its association with the incidence of rheumatoid arthritis, systemic lupus erythematosus, and psoriatic arthritis: an analysis of one-million national colorectal cancer screening programme results. BMC Med (2022) 20(1):226. doi: 10.1186/s12916-022-02416-y
30. Eyre S, Bowes J, Diogo D, Lee A, Barton A, Martin P, et al. High-density genetic mapping identifies new susceptibility loci for rheumatoid arthritis. Nat Genet (2012) 44(12):1336–40. doi: 10.1038/ng.2462
31. Okada Y, Wu D, Trynka G, Raj T, Terao C, Ikari K, et al. Genetics of rheumatoid arthritis contributes to biology and drug discovery. Nature (2014) 506(7488):376–81. doi: 10.1038/nature12873
32. Laufer VA, Tiwari HK, Reynolds RJ, Danila MI, Wang J, Edberg JC, et al. Genetic influences on susceptibility to rheumatoid arthritis in African-americans. Hum Mol Genet (2019) 28(5):858–74. doi: 10.1093/hmg/ddy395
33. Márquez A, Kerick M, Zhernakova A, Gutierrez-Achury J, Chen WM, Onengut-Gumuscu S, et al. Meta-analysis of immunochip data of four autoimmune diseases reveals novel single-disease and cross-phenotype associations. Genome Med (2018) 10(1):97. doi: 10.1186/s13073-018-0604-8
34. Ikari K, Kuwahara M, Nakamura T, Momohara S, Hara M, Yamanaka H, et al. Association between PADI4 and rheumatoid arthritis: a replication study. Arthritis Rheumatol (2005) 52(10):3054–7. doi: 10.1002/art.21309
35. Raychaudhuri S, Remmers EF, Lee AT, Hackett R, Guiducci C, Burtt NP, et al. Common variants at CD40 and other loci confer risk of rheumatoid arthritis. Nat Genet (2008) 40(10):1216–23. doi: 10.1038/ng.233
36. de Rooy DP, Tsonaka R, Andersson ML, Forslind K, Zhernakova A, Frank-Bertoncelj M, et al. Genetic factors for the severity of ACPA-negative rheumatoid arthritis in 2 cohorts of early disease: A genome-wide study. J Rheumatol (2015) 42(8):1383–91. doi: 10.3899/jrheum.140741
37. Senapati S, Singh S, Das M, Kumar A, Gupta R, Kumar U, et al. Genome-wide analysis of methotrexate pharmacogenomics in rheumatoid arthritis shows multiple novel risk variants and leads for TYMS regulation. Pharmacogenet Genomics (2014) 24(4):211–9. doi: 10.1097/fpc.0000000000000036
38. Cui J, Stahl EA, Saevarsdottir S, Miceli C, Diogo D, Trynka G, et al. Genome-wide association study and gene expression analysis identifies CD84 as a predictor of response to etanercept therapy in rheumatoid arthritis. PLoS Genet (2013) 9(3):e1003394. doi: 10.1371/journal.pgen.1003394
39. Massey J, Plant D, Hyrich K, Morgan AW, Wilson AG, Spiliopoulou A, et al. Genome-wide association study of response to tumour necrosis factor inhibitor therapy in rheumatoid arthritis. Pharmacogenomics J (2018) 18(5):657–64. doi: 10.1038/s41397-018-0040-6
40. Plant D, Prajapati R, Hyrich KL, Morgan AW, Wilson AG, Isaacs JD, et al. Replication of association of the PTPRC gene with response to anti-tumor necrosis factor therapy in a large UK cohort. Arthritis Rheumatol (2012) 64(3):665–70. doi: 10.1002/art.33381
41. Zeng T, Tan L. 14-3-3η protein: a promising biomarker for rheumatoid arthritis. biomark Med (2018) 12(8):917–25. doi: 10.2217/bmm-2017-0385
42. Otsubo H, Tsuneyoshi Y, Nakamura T, Matsuda T, Komiya S, Matsuyama T. Serum-soluble folate receptor β as a biomarker for the activity of rheumatoid arthritis synovitis and the response to anti-TNF agents. Clin Rheumatol (2018) 37(11):2939–45. doi: 10.1007/s10067-018-4202-3
43. Karsdal MA, Woodworth T, Henriksen K, Maksymowych WP, Genant H, Vergnaud P, et al. Biochemical markers of ongoing joint damage in rheumatoid arthritis–current and future applications, limitations and opportunities. Arthritis Res Ther (2011) 13(2):215. doi: 10.1186/ar3280
44. Jarlborg M, Courvoisier DS, Lamacchia C, Martinez Prat L, Mahler M, Bentow C, et al. Serum calprotectin: a promising biomarker in rheumatoid arthritis and axial spondyloarthritis. Arthritis Res Ther (2020) 22(1):105. doi: 10.1186/s13075-020-02190-3
45. Hu F, Jiang X, Guo C, Li Y, Chen S, Zhang W, et al. Scavenger receptor-a is a biomarker and effector of rheumatoid arthritis: A large-scale multicenter study. Nat Commun (2020) 11(1):1911. doi: 10.1038/s41467-020-15700-3
46. Liu S, Guo Y, Lu L, Lu J, Ke M, Xu T, et al. Fibrinogen-like protein 1 is a novel biomarker for predicting disease activity and prognosis of rheumatoid arthritis. Front Immunol (2020) 11:579228. doi: 10.3389/fimmu.2020.579228
47. Huang F, Liu X, Cheng Y, Sun X, Li Y, Zhao J, et al. Antibody to peptidoglycan recognition protein (PGLYRP)-2 as a novel biomarker in rheumatoid arthritis. Clin Exp Rheumatol (2021) 39(5):988–94. doi: 10.55563/clinexprheumatol/vlvlqu
48. Mun S, Lee J, Park M, Shin J, Lim MK, Kang HG. Serum biomarker panel for the diagnosis of rheumatoid arthritis. Arthritis Res Ther (2021) 23(1):31. doi: 10.1186/s13075-020-02405-7
49. Wen W, Li Y, Cheng Y, He J, Jia R, Li C, et al. Lipopolysaccharide-binding protein is a sensitive disease activity biomarker for rheumatoid arthritis. Clin Exp Rheumatol (2018) 36(2):233–40.
50. Guan Y, Zhang H, Quang D, Wang Z, Parker SCJ, Pappas DA, et al. Machine learning to predict anti-tumor necrosis factor drug responses of rheumatoid arthritis patients by integrating clinical and genetic markers. Arthritis Rheumatol (2019) 71(12):1987–96. doi: 10.1002/art.41056
51. Ma MHY, Defranoux N, Li W, Sasso EH, Ibrahim F, Scott DL, et al. A multi-biomarker disease activity score can predict sustained remission in rheumatoid arthritis. Arthritis Res Ther (2020) 22(1):158. doi: 10.1186/s13075-020-02240-w
52. Ciechomska M, Roszkowski L, Maslinski W. DNA Methylation as a Future Therapeutic and Diagnostic Target in Rheumatoid Arthritis. Cells (2019) 8(9):953. doi: 10.3390/cells8090953
53. Wang J, Yan S, Yang J, Lu H, Xu D, Wang Z. Non-coding RNAs in rheumatoid arthritis: From bench to bedside. Front Immunol (2019) 10:3129. doi: 10.3389/fimmu.2019.03129
54. Kung JT, Colognori D, Lee JT. Long noncoding RNAs: past, present, and future. Genetics (2013) 193(3):651–69. doi: 10.1534/genetics.112.146704
55. Venter JC, Adams MD, Myers EW, Li PW, Mural RJ, Sutton GG, et al. The sequence of the human genome. Science (2001) 291(5507):1304–51. doi: 10.1126/science.1058040
56. Lander ES, Linton LM, Birren B, Nusbaum C, Zody MC, Baldwin J, et al. Initial sequencing and analysis of the human genome. Nature (2001) 409(6822):860–921. doi: 10.1038/35057062
57. Ali SA, Peffers MJ, Ormseth MJ, Jurisica I, Kapoor M. The non-coding RNA interactome in joint health and disease. Nat Rev Rheumatol (2021) 17(11):692–705. doi: 10.1038/s41584-021-00687-y
58. Taheri M, Eghtedarian R, Dinger ME, Ghafouri-Fard S. Dysregulation of non-coding RNAs in rheumatoid arthritis. BioMed Pharmacother (2020) 130:110617. doi: 10.1016/j.biopha.2020.110617
59. Storz G. An expanding universe of noncoding RNAs. Science (2002) 296(5571):1260–3. doi: 10.1126/science.1072249
60. Cech TR, Steitz JA. The noncoding RNA revolution-trashing old rules to forge new ones. Cell (2014) 157(1):77–94. doi: 10.1016/j.cell.2014.03.008
61. Zhang P, Wu W, Chen Q, Chen M. Non-Coding RNAs and their Integrated Networks. J Integr Bioinform (2019) 16(3):20190027. doi: 10.1515/jib-2019-0027
62. Katahira J. Nuclear export of messenger RNA. Genes (Basel) (2015) 6(2):163–84. doi: 10.3390/genes6020163
63. Gao H, Ma XX, Guo Q, Xie LF, Zhong YC, Zhang XW. Expression of circulating Semaphorin3A and its association with inflammation and bone destruction in rheumatoid arthritis. Clin Rheumatol (2018) 37(8):2073–80. doi: 10.1007/s10067-018-4070-x
64. He P, Deng FY, Wang BH, Wu LF, Zhou X, Lei SF. Epigenetically-regulated RPN2 gene influences lymphocyte activation and is involved in pathogenesis of rheumatoid arthritis. Gene (2022) 810:146059. doi: 10.1016/j.gene.2021.146059
65. Yuan ZC, Wang JM, Huang AF, Su LC, Li SJ, Xu WD. Elevated expression of interleukin-37 in patients with rheumatoid arthritis. Int J Rheum Dis (2019) 22(6):1123–9. doi: 10.1111/1756-185x.13539
66. Lamana A, Villares R, Seoane IV, Andrés N, Lucas P, Emery P, et al. Identification of a human SOCS1 polymorphism that predicts rheumatoid arthritis severity. Front Immunol (2020) 11:1336. doi: 10.3389/fimmu.2020.01336
67. Zhou KL, Zhu ZH, Zhou JP, Zhao JJ, Zhang Y, Jiang B. Increased hexokinase-2 as a novel biomarker for the diagnosis and correlating with disease severity in rheumatoid arthritis. Medicine (2021) 100(25):e26504. doi: 10.1097/md.0000000000026504
68. Li Y, Zhou M, Lv X, Song L, Zhang D, He Y, et al. Reduced activity of HDAC3 and increased acetylation of histones H3 in peripheral blood mononuclear cells of patients with rheumatoid arthritis. J Immunol Res (2018) 2018:7313515. doi: 10.1155/2018/7313515
69. Yang X, Zhang M, Xu S, Pan H, Leng R, Shuai Z. Single immunoglobulin IL-1-Related receptor (SIGIRR) gene rs7396562 polymorphism and expression level in rheumatoid arthritis. BioMed Res Int (2021) 2021:6683148. doi: 10.1155/2021/6683148
70. Xia G, Li Y, Pan W, Qian C, Ma L, Zhou J, et al. SLAMF6 is associated with the susceptibility and severity of rheumatoid arthritis in the Chinese population. J Orthop Surg Res (2022) 17(1):13. doi: 10.1186/s13018-021-02901-9
71. Addobbati C, da Cruz HLA, Adelino JE, Melo Tavares Ramos AL, Fragoso TS, Domingues A, et al. Polymorphisms and expression of inflammasome genes are associated with the development and severity of rheumatoid arthritis in Brazilian patients. Inflammation Res (2018) 67(3):255–64. doi: 10.1007/s00011-017-1119-2
72. Luo Q, Gao Y, Zhang L, Rao J, Guo Y, Huang Z, et al. Decreased ALKBH5, FTO, and YTHDF2 in peripheral blood are as risk factors for rheumatoid arthritis. BioMed Res Int (2020) 2020:5735279. doi: 10.1155/2020/5735279
73. Wu B, Peng R, Chen Y, Zhong J, Zhong S, Wang B, et al. Identification of RRM2 in peripheral blood mononuclear cells as a novel biomarker for the diagnosis of rheumatoid arthritis. Clin Exp Rheumatol (2022) 40(11):2109–18. doi: 10.55563/clinexprheumatol/ixdaek
74. Carrea A, Preisegger MA, Velasco Zamora J, Dewey RA. The mRNA levels of TGF-β type II receptor splice variants in monocytes are associated with disease activity in patients with rheumatoid arthritis. Clin Exp Rheumatol (2021) 39(2):310–8. doi: 10.55563/clinexprheumatol/ck1ksi
75. Román-Fernández IV, García-Chagollán M, Cerpa-Cruz S, Jave-Suárez LF, Palafox-Sánchez CA, García-Arellano S, et al. Assessment of CD40 and CD40L expression in rheumatoid arthritis patients, association with clinical features and DAS28. Clin Exp Med (2019) 19(4):427–37. doi: 10.1007/s10238-019-00568-5
76. Xu WD, Su LC, He CS, Huang AF. Plasma interleukin-38 in patients with rheumatoid arthritis. Int Immunopharmacol (2018) 65:1–7. doi: 10.1016/j.intimp.2018.09.028
77. Yeganeh F, Mousavi SMJ, Hosseinzadeh-Sarband S, Ahmadzadeh A, Bahrami-Motlagh H, Hoseini MHM, et al. Association of CD26/dipeptidyl peptidase IV mRNA level in peripheral blood mononuclear cells with disease activity and bone erosion in rheumatoid arthritis. Clin Rheumatol (2018) 37(12):3183–90. doi: 10.1007/s10067-018-4268-y
78. Cao R, Zhang Y, Du J, Chen S, Wang N, Ying H, et al. Increased FURIN expression in rheumatoid arthritis patients and its anti-inflammatory effect. J Clin Lab Anal (2020) 34(12):e23530. doi: 10.1002/jcla.23530
79. Jahid M, Rehan Ul H, Avasthi R, Ahmed RS. Interleukin10-1082 A/G polymorphism: Allele frequency, correlation with disease markers, messenger RNA and serum levels in north Indian rheumatoid arthritis patients. Clin Biochem (2018) 55:80–5. doi: 10.1016/j.clinbiochem.2018.03.024
80. Yao F, Xu C, Gao Y, Fu B, Zhang L, Guo Y, et al. Expression and clinical significance of the m6A reader YTHDF2 in peripheral blood mononuclear cells from rheumatoid arthritis patients. J Immunotoxicol (2022) 19(1):53–60. doi: 10.1080/1547691x.2022.2067916
81. Li ZY, Zhou JJ, Luo CL, Zhang LM. Activation of TGR5 alleviates inflammation in rheumatoid arthritis peripheral blood mononuclear cells and in mice with collagen II−induced arthritis. Mol Med Rep (2019) 20(5):4540–50. doi: 10.3892/mmr.2019.10711
82. Zhang X, Zhang X, Zhuang L, Xu C, Li T, Zhang G, et al. Decreased regulatory T-cell frequency and interleukin-35 levels in patients with rheumatoid arthritis. Exp Ther Med (2018) 16(6):5366–72. doi: 10.3892/etm.2018.6885
83. Avouac J, Pezet S, Vandebeuque E, Orvain C, Gonzalez V, Marin G, et al. Semaphorins: From angiogenesis to inflammation in rheumatoid arthritis. Arthritis Rheumatol (2021) 73(9):1579–88. doi: 10.1002/art.41701
84. Kane BA, An H, Rajasekariah P, McNeil HP, Bryant K, Tedla N. Differential expression and regulation of the non-integrin 37/67-kDa laminin receptor on peripheral blood leukocytes of healthy individuals and patients with rheumatoid arthritis. Sci Rep (2019) 9(1):1149. doi: 10.1038/s41598-018-37907-7
85. Damen M, Schraa K, Tweehuysen L, den Broeder AA, Netea MG, Popa CD, et al. Genetic variant in IL-32 is associated with the ex vivo cytokine production of anti-TNF treated PBMCs from rheumatoid arthritis patients. Sci Rep (2018) 8(1):14050. doi: 10.1038/s41598-018-32485-0
86. Muller IB, Lin M, Lems WF, Ter Wee MM, Wojtuszkiewicz A, Nurmohamed MT, et al. Association of altered folylpolyglutamate synthetase pre-mRNA splicing with methotrexate unresponsiveness in early rheumatoid arthritis. Rheumatol (Oxford) (2021) 60(3):1273–81. doi: 10.1093/rheumatology/keaa428
87. Singh A, Misra R, Aggarwal A. Baseline adenosine receptor mRNA expression in blood as predictor of response to methotrexate therapy in patients with rheumatoid arthritis. Rheumatol Int (2019) 39(8):1431–8. doi: 10.1007/s00296-019-04344-2
88. Mo XB, Sun YH, Wu LF, He P, Cao RR, Lu X, et al. A Novel Long Noncoding RNA, lnc-RNU12, Influences the T-Cell Cycle via c-JUN and CCNL2 in Rheumatoid Arthritis. Rheumatol (Oxford) (2022) 27:keac553. doi: 10.1093/rheumatology/keac553
89. Long Y, Liu J, Jiang H, Xin L, Wan L, Sun Y, et al. Network analysis and transcriptome profiling in peripheral blood mononuclear cells of patients with rheumatoid arthritis. Exp Ther Med (2021) 21(2):170. doi: 10.3892/etm.2020.9601
90. Wang Q, Huang X, Shao Y, Liu Q, Shen J, Xia J, et al. The implication of long non-coding RNA expression profile in rheumatoid arthritis: Correlation with treatment response to tumor necrosis factor inhibitor. Mod Rheumatol (2022) 33(1):111–21. doi: 10.1093/mr/roab128
91. Mo BY, Guo XH, Yang MR, Liu F, Bi X, Liu Y, et al. Long non-coding RNA GAPLINC promotes tumor-like biologic behaviors of fibroblast-like synoviocytes as MicroRNA sponging in rheumatoid arthritis patients. Front Immunol (2018) 9:702. doi: 10.3389/fimmu.2018.00702
92. Piao X, Zhou J, Hu J. Role of RP11-83J16.1, a novel long non-coding RNA, in rheumatoid arthritis. Am J Trans Res (2020) 12(4):1397–414.
93. Bi X, Guo XH, Mo BY, Wang ML, Luo XQ, Chen YX, et al. LncRNA PICSAR promotes cell proliferation, migration and invasion of fibroblast-like synoviocytes by sponging miRNA-4701-5p in rheumatoid arthritis. EBioMedicine (2019) 50:408–20. doi: 10.1016/j.ebiom.2019.11.024
94. Aiman AQ, Nesrin M, Amal A, Nassar AD. A new tool for early diagnosis of rheumatoid arthritis using combined biomarkers; synovial MAGE-1 mRNA and serum anti-CCP and RF. Pan Afr Med J (2020) 36:270. doi: 10.11604/pamj.2020.36.270.21827
95. Huang Z, Niu Q, Yang B, Zhang J, Yang M, Xu H, et al. Genetic polymorphism of rs9277535 in HLA-DP associated with rheumatoid arthritis and anti-CCP production in a Chinese population. Clin Rheumatol (2018) 37(7):1799–805. doi: 10.1007/s10067-018-4030-5
96. Cheng L, Liang X, Qian L, Luo C, Li D. NLRP3 gene polymorphisms and expression in rheumatoid arthritis. Exp Ther Med (2021) 22(4):1110. doi: 10.3892/etm.2021.10544
97. Muto S, Minamitani N, Ogura T, Nakajima A, Nakagawa K, Masaka T, et al. Good response to methotrexate is associated with a decrease in the gene expression of ABCG2, a drug transporter, in patients with rheumatoid arthritis. Mod Rheumatol (2021) 31(6):1079–86. doi: 10.1080/14397595.2021.1879429
98. Yang X, Chen B, Zhang M, Xu S, Shuai Z. Tristetraprolin gene single-nucleotide polymorphisms and mRNA level in patients with rheumatoid arthritis. Front Pharmacol (2021) 12:728015. doi: 10.3389/fphar.2021.728015
99. Zhu J, Xie C, Qiu H, Shi L. Correlation between level of interleukin-37 and rheumatoid arthritis progression. Int J Gen Med (2021) 14:1905–10. doi: 10.2147/ijgm.S309436
100. Vicente R, Noël D, Pers YM, Apparailly F, Jorgensen C. Deregulation and therapeutic potential of microRNAs in arthritic diseases. Nat Rev Rheumatol (2016) 12(4):211–20. doi: 10.1038/nrrheum.2015.162
101. Catalanotto C, Cogoni C, Zardo G. MicroRNA in Control of Gene Expression: An Overview of Nuclear Functions. Int J Mol Sci (2016) 17(10):1712. doi: 10.3390/ijms17101712
102. Chen JQ, Papp G, Szodoray P, Zeher M. The role of microRNAs in the pathogenesis of autoimmune diseases. Autoimmun Rev (2016) 15(12):1171–80. doi: 10.1016/j.autrev.2016.09.003
103. Ali Syeda Z, Langden SSS, Munkhzul C, Lee M, Song SJ. Regulatory Mechanism of MicroRNA Expression in Cancer. Int J Mol Sci (2020) 21(5):1723. doi: 10.3390/ijms21051723
104. Cunningham CC, Wade S, Floudas A, Orr C, McGarry T, Wade S, et al. Serum miRNA signature in rheumatoid arthritis and "At-risk individuals". Front Immunol (2021) 12:633201. doi: 10.3389/fimmu.2021.633201
105. Taha M, Shaker OG, Abdelsalam E, Taha N. Serum a proliferation-inducing ligand and MicroRNA-223 are associated with rheumatoid arthritis: diagnostic and prognostic implications. Mol Med (2020) 26(1):92. doi: 10.1186/s10020-020-00199-7
106. Dunaeva M, Blom J, Thurlings R, Pruijn GJM. Circulating serum miR-223-3p and miR-16-5p as possible biomarkers of early rheumatoid arthritis. Clin Exp Immunol (2018) 193(3):376–85. doi: 10.1111/cei.13156
107. Abdelaleem OO, Fouad NA, Shaker OG, Ahmed TI, Abdelghaffar NK, Eid HM, et al. Serum miR-224, miR-760, miR-483-5p, miR-378 and miR-375 as potential novel biomarkers in rheumatoid arthritis. Int J Clin Pract (2021) 75(11):e14651. doi: 10.1111/ijcp.14651
108. Liu M, Ren T, Lin Z, Hua M. Upregulated miR-146a expression in peripheral blood relates to Th17 and treg imbalance in elder rheumatoid arthritis patients. Lifestyle Genom (2022) 15(3):98–106. doi: 10.1159/000525112
109. Romo-García MF, Bastian Y, Zapata-Zuñiga M, Macías-Segura N, Castillo-Ortiz JD, Lara-Ramírez EE, et al. Identification of putative miRNA biomarkers in early rheumatoid arthritis by genome-wide microarray profiling: A pilot study. Gene (2019) 720:144081. doi: 10.1016/j.gene.2019.144081
110. Kolarz B, Ciesla M, Dryglewska M, Rosenthal AK, Majdan M. Hypermethylation of the miR-155 gene in the whole blood and decreased plasma level of miR-155 in rheumatoid arthritis. PLoS One (2020) 15(6):e0233897. doi: 10.1371/journal.pone.0233897
111. Safari F, Damavandi E, Rostamian AR, Movassaghi S, Imani-Saber Z, Saffari M, et al. Plasma levels of MicroRNA-146a-5p, MicroRNA-24-3p, and MicroRNA-125a-5p as potential diagnostic biomarkers for rheumatoid arthris. Iran J Allergy Asthma Immunol (2021) 20(3):326–37. doi: 10.18502/ijaai.v20i3.6334
112. Tang J, Lin J, Yu Z, Jiang R, Xia J, Yang B, et al. Identification of circulating miR-22-3p and let-7a-5p as novel diagnostic biomarkers for rheumatoid arthritis. Clin Exp Rheumatol (2022) 40(1):69–77. doi: 10.55563/clinexprheumatol/4me6tg
113. Liu X, Ni S, Li C, Xu N, Chen W, Wu M, et al. Circulating microRNA-23b as a new biomarker for rheumatoid arthritis. Gene (2019) 712:143911. doi: 10.1016/j.gene.2019.06.001
114. Gao B, Sun G, Wang Y, Geng Y, Zhou L, Chen X. microRNA-23 inhibits inflammation to alleviate rheumatoid arthritis via regulating CXCL12. Exp Ther Med (2021) 21(5):459. doi: 10.3892/etm.2021.9890
115. Liu C, Pan A, Chen X, Tu J, Xia X, Sun L. MiR-5571-3p and miR-135b-5p, derived from analyses of microRNA profile sequencing, correlate with increased disease risk and activity of rheumatoid arthritis. Clin Rheumatol (2019) 38(6):1753–65. doi: 10.1007/s10067-018-04417-w
116. Xu D, Song M, Chai C, Wang J, Jin C, Wang X, et al. Exosome-encapsulated miR-6089 regulates inflammatory response via targeting TLR4. J Cell Physiol (2019) 234(2):1502–11. doi: 10.1002/jcp.27014
117. Wu LF, Zhang Q, Mo XB, Lin J, Wu YL, Lu X, et al. Identification of novel rheumatoid arthritis-associated MiRNA-204-5p from plasma exosomes. Exp Mol Med (2022) 54(3):334–45. doi: 10.1038/s12276-022-00751-x
118. Rodríguez-Muguruza S, Altuna-Coy A, Castro-Oreiro S, Poveda-Elices MJ, Fontova-Garrofé R, Chacón MR. A serum biomarker panel of exomiR-451a, exomiR-25-3p and soluble TWEAK for early diagnosis of rheumatoid arthritis. Front Immunol (2021) 12:790880. doi: 10.3389/fimmu.2021.790880
119. Wang Y, Zheng F, Gao G, Yan S, Zhang L, Wang L, et al. MiR-548a-3p regulates inflammatory response via TLR4/NF-κB signaling pathway in rheumatoid arthritis. J Cell Biochem (2018) 6. doi: 10.1002/jcb.26659
120. Lim MK, Yoo J, Sheen DH, Ihm C, Lee SK, Kim SA. Serum exosomal miRNA-1915-3p is correlated with disease activity of Korean rheumatoid arthritis. In Vivo (2020) 34(5):2941–5. doi: 10.21873/invivo.12124
121. Duan W, Zhang W, Jia J, Lu Q, Eric Gershwin M. Exosomal microRNA in autoimmunity. Cell Mol Immunol (2019) 16(12):932–4. doi: 10.1038/s41423-019-0319-9
122. Ye Y, Gao X, Yang N. LncRNA ZFAS1 promotes cell migration and invasion of fibroblast-like synoviocytes by suppression of miR-27a in rheumatoid arthritis. Hum Cell (2018) 31(1):14–21. doi: 10.1007/s13577-017-0179-5
123. Xiao J, Wang R, Zhou W, Cai X, Ye Z. LncRNA NEAT1 regulates the proliferation and production of the inflammatory cytokines in rheumatoid arthritis fibroblast-like synoviocytes by targeting miR-204-5p. Hum Cell (2021) 34(2):372–82. doi: 10.1007/s13577-020-00461-4
124. Zhang M, Lu N, Li HJ, Guo XY, Lu L, Guo Y. Inhibition of lncRNA NEAT1 induces dysfunction of fibroblast-like synoviocytes in rheumatoid arthritis via miRNA-338-3p-mediated regulation of glutamine metabolism. J Orthop Surg Res (2022) 17(1):401. doi: 10.1186/s13018-022-03295-y
125. Erfan R, Shaker OG, Khalil MAF, Elsabagh YA, Ahmed AM, Abu-El-Azayem AK, et al. Long non-coding RNA PVT1 and its target miRNA-146a as potential prognostic biomarkers in rheumatoid arthritis patients. Life (Basel) (2021) 11(12). doi: 10.3390/life11121382
126. Tang J, Yi S, Liu Y. Long non-coding RNA PVT1 can regulate the proliferation and inflammatory responses of rheumatoid arthritis fibroblast-like synoviocytes by targeting microRNA-145-5p. Hum Cell (2020) 33(4):1081–90. doi: 10.1007/s13577-020-00419-6
127. Zhao Q, Zhao F, Liu C, Xu T, Song K. LncRNA FOXD2-AS1 promotes cell proliferation and invasion of fibroblast-like synoviocytes by regulation of miR-331-3p/PIAS3 pathway in rheumatoid arthritis. Autoimmunity (2021) 54(5):254–63. doi: 10.1080/08916934.2021.1919879
128. Ye Z, Wei L, Yin X, Li H, Qin G, Li S, et al. Long non-coding RNA cancer susceptibility candidate 2 regulates the function of human fibroblast-like synoviocytes via the microRNA-18a-5p/B-cell translocation gene 3 signaling axis in rheumatoid arthritis. Bioengineered (2022) 13(2):3240–50. doi: 10.1080/21655979.2021.2022075
129. Qiu H, Liu M, Shi X, Ma M, Zhang J, Liu H. LncRNA HOTAIR inhibits the progression of fibroblast-like synoviocytes by sponging miRNA-106b-5p in rheumatoid arthritis. Autoimmunity (2022) 55(8):567–76. doi: 10.1080/08916934.2022.2126460
130. Xu D, Jiang Y, Yang L, Hou X, Wang J, Gu W, et al. Long noncoding RNAs expression profile and functional networks in rheumatoid arthritis. Oncotarget (2017) 8(56):95280–92. doi: 10.18632/oncotarget.20036
131. Liang Y, Li H, Gong X, Ding C. Long non-coding RNA THRIL mediates cell growth and inflammatory response of fibroblast-like synoviocytes by activating PI3.
132. Wang G, Tang L, Zhang X, Li Y. LncRNA DILC participates in rheumatoid arthritis by inducing apoptosis of fibroblast-like synoviocytes and down-regulating IL-6. Biosci Rep (2019) 39(5). doi: 10.1042/bsr20182374
133. Liu C, Guo X, Bai S, Zeng G, Wang H. lncRNA CASC2 downregulation participates in rheumatoid arthritis, and CASC2 overexpression promotes the apoptosis of fibroblast-like synoviocytes by downregulating IL-17. Mol Med Rep (2020) 21(5):2131–7. doi: 10.3892/mmr.2020.11018
134. Dolcino M, Tinazzi E, Puccetti A, Lunardi C. Long non-coding RNAs target pathogenetically relevant genes and pathways in rheumatoid arthritis. Cells (2019) 8(8). doi: 10.3390/cells8080816
135. Wu LF, Mo XB, He JH, He P, Lu X, Deng HW, et al. Integrative lncRNA-mRNA co-expression network analysis identifies novel lncRNA E2F3-IT1 for rheumatoid arthritis. Clin Transl Med (2021) 11(2):e325. doi: 10.1002/ctm2.325
136. Peng H, Ren S, Liu Y, Zhou H, Tang X, Yang J, et al. Elevated expression of the long noncoding RNA IFNG-AS1 in the peripheral blood from patients with rheumatoid arthritis. J Immunol Res (2020) 2020:6401978. doi: 10.1155/2020/6401978
137. Li M, Ma K, Feng Z, Wang J, Zhou X, Zhou L. Differential long non-coding RNA expression profiles in the peripheral blood and CD4(+) T cells of patients with active rheumatoid arthritis. Exp Ther Med (2020) 20(1):461–71. doi: 10.3892/etm.2020.8681
138. Zhou Z, Sun B, Huang S, Zhao L. Roles of circular RNAs in immune regulation and autoimmune diseases. Cell Death Dis (2019) 10(7):503. doi: 10.1038/s41419-019-1744-5
139. Xia X, Tang X, Wang S. Roles of CircRNAs in autoimmune diseases. Front Immunol (2019) 10:639. doi: 10.3389/fimmu.2019.00639
140. Luo Q, Liu J, Fu B, Zhang L, Guo Y, Huang Z, et al. Circular RNAs Hsa_circ_0002715 and Hsa_circ_0035197 in peripheral blood are novel potential biomarkers for new-onset rheumatoid arthritis. Dis Markers (2019) 2019:2073139. doi: 10.1155/2019/2073139
141. Zhi L, Liang J, Huang W, Ma J, Qing Z, Wang X. Circ_AFF2 facilitates proliferation and inflammatory response of fibroblast-like synoviocytes in rheumatoid arthritis via the miR-375/TAB2 axis. Exp Mol Pathol (2021) 119:104617. doi: 10.1016/j.yexmp.2021.104617
142. Qu W, Jiang L, Hou G. Circ-AFF2/miR-650/CNP axis promotes proliferation, inflammatory response, migration, and invasion of rheumatoid arthritis synovial fibroblasts. J Orthop Surg Res (2021) 16(1):165. doi: 10.1186/s13018-021-02306-8
143. Zhang J, Li S, Li L, Li M, Guo C, Yao J, et al. Exosome and exosomal microRNA: trafficking, sorting, and function. Genomics Proteomics Bioinf (2015) 13(1):17–24. doi: 10.1016/j.gpb.2015.02.001
144. Mirzaei R, Zamani F, Hajibaba M, Rasouli-Saravani A, Noroozbeygi M, Gorgani M, et al. The pathogenic, therapeutic and diagnostic role of exosomal microRNA in the autoimmune diseases. J Neuroimmunol (2021) 358:577640. doi: 10.1016/j.jneuroim.2021.577640
145. Singh A, Patro PS, Aggarwal A. MicroRNA-132, miR-146a, and miR-155 as potential biomarkers of methotrexate response in patients with rheumatoid arthritis. Clin Rheumatol (2019) 38(3):877–84. doi: 10.1007/s10067-018-4380-z
146. Bure IV, Mikhaylenko DS, Kuznetsova EB, Alekseeva EA, Bondareva KI, Kalinkin AI, et al. Analysis of miRNA Expression in Patients with Rheumatoid Arthritis during Olokizumab Treatment. J Pers Med (2020) 10(4):205. doi: 10.3390/jpm10040205
147. Fernández-Ruiz JC, Ramos-Remus C, Sánchez-Corona J, Castillo-Ortiz JD, Castañeda-Sánchez JJ, Bastian Y, et al. Analysis of miRNA expression in patients with rheumatoid arthritis during remission and relapse after a 5-year trial of tofacitinib treatment. Int Immunopharmacol (2018) 63:35–42. doi: 10.1016/j.intimp.2018.07.028
148. Cheng P, Wang J. The potential of circulating microRNA-125a and microRNA-125b as markers for inflammation and clinical response to infliximab in rheumatoid arthritis patients. J Clin Lab Anal (2020) 34(8):e23329. doi: 10.1002/jcla.23329
149. Yang Z, Wang J, Pan Z, Zhang Y. miR-143-3p regulates cell proliferation and apoptosis by targeting IGF1R and IGFBP5 and regulating the Ras/p38 MAPK signaling pathway in rheumatoid arthritis. Exp Ther Med (2018) 15(4):3781–90. doi: 10.3892/etm.2018.5907
150. Li S, Jin Z, Lu X. MicroRNA-192 suppresses cell proliferation and induces apoptosis in human rheumatoid arthritis fibroblast-like synoviocytes by downregulating caveolin 1. Mol Cell Biochem (2017) 432(1-2):123–30. doi: 10.1007/s11010-017-3003-3
151. Liu Y, Qian K, Li C, Ma Y, Chen X. Roles of microRNA-539 and osteopontin in rheumatoid arthritis. Exp Ther Med (2018) 15(3):2681–7. doi: 10.3892/etm.2017.5665
152. Rezaeepoor M, Pourjafar M, Tahamoli-Roudsari A, Basiri Z, Hajilooi M, Solgi G. Altered expression of microRNAs may predict therapeutic response in rheumatoid arthritis patients. Int Immunopharmacol. (2020) 83:106404. doi: 10.1016/j.intimp.2020.106404
153. Erfan R, Shaker OG, Khalil MAF, Elsabagh YA, Ahmed AM, Abu-El-Azayem AK, et al. Long non-coding RNA PVT1 and its target miRNA-146a as potential prognostic biomarkers in rheumatoid arthritis patients. Life (Basel) (2021) 11(12). doi: 10.3390/life11121382
154. Ayeldeen G, Nassar Y, Ahmed H, Shaker O, Gheita T. Possible use of miRNAs-146a and -499 expression and their polymorphisms as diagnostic markers for rheumatoid arthritis. Mol Cell Biochem (2018) 449(1-2):145–56. doi: 10.1007/s11010-018-3351-7
155. Ciechomska M, Bonek K, Merdas M, Zarecki P, Swierkot J, Gluszko P, et al. Changes in MiRNA-5196 expression as a potential biomarker of anti-TNF-α therapy in rheumatoid arthritis and ankylosing spondylitis patients. Arch Immunol Ther Exp (Warsz). (2018) 66(5):389–97. doi: 10.1007/s00005-018-0513-y
156. Sui X, Liu H, Zhou Y. Expression of miR-495 and miR-326 in peripheral blood of rheumatoid arthritis patients and its significance. Exp Ther Med (2020) 20(4):3766–74. doi: 10.3892/etm.2020.9124
157. Abdul-Maksoud RS, Sediq AM, Kattaia A, Elsayed W, Ezzeldin N, Abdel Galil SM, et al. Serum miR-210 and miR-155 expression levels as novel biomarkers for rheumatoid arthritis diagnosis. Br J BioMed Sci (2017) 74(4):209–13. doi: 10.1080/09674845.2017.1343545
158. Hong H, Yang H, Xia Y. Circulating miR-10a as predictor of therapy response in rheumatoid arthritis patients treated with methotrexate. Curr Pharm Biotechnol (2018) 19(1):79–86. doi: 10.2174/1389201019666180417155140
159. Cieśla M, Kolarz B, Majdan M, Darmochwał-Kolarz D. Plasma micro-RNA-22 is associated with disease activity in well-established rheumatoid arthritis. Clin Exp Rheumatol (2022) 40(5):945–51. doi: 10.55563/clinexprheumatol/zdhkrp
160. Sode J, Krintel SB, Carlsen AL, Hetland ML, Johansen JS, Hørslev-Petersen K, et al. Plasma MicroRNA profiles in patients with early rheumatoid arthritis responding to adalimumab plus methotrexate vs methotrexate alone: A placebo-controlled clinical trial. J Rheumatol (2018) 45(1):53–61. doi: 10.3899/jrheum.170266
161. Yue J, Lau TCK, Griffith JF, Xu J, Xiao F, Shi L, et al. Circulating miR-99b-5p as a novel predictor of erosion progression on high-resolution peripheral quantitative computed tomography in early rheumatoid arthritis: A prospective cohort study. Int J Rheum Dis (2019) 22(9):1724–33. doi: 10.1111/1756-185x.13644
162. Prajzlerová K, Kryštůfková O, Hánová P, Horváthová V, Gregová M, Pavelka K, et al. High miR-451 expression in peripheral blood mononuclear cells from subjects at risk of developing rheumatoid arthritis. Sci Rep (2021) 11(1):4719. doi: 10.1038/s41598-021-84004-3
163. Zhu X, Wu L, Mo X, Xia W, Guo Y, Wang M, et al. Identification of PBMC-expressed miRNAs for rheumatoid arthritis. Epigenetics (2020) 15(4):386–97. doi: 10.1080/15592294.2019.1676613
164. Abo ElAtta AS, Ali YBM, Bassyouni IH, Talaat RM. Upregulation of miR-221/222 expression in rheumatoid arthritis (RA) patients: correlation with disease activity. Clin Exp Med (2019) 19(1):47–53. doi: 10.1007/s10238-018-0524-3
165. Anaparti V, Smolik I, Meng X, Spicer V, Mookherjee N, El-Gabalawy H. Whole blood microRNA expression pattern differentiates patients with rheumatoid arthritis, their seropositive first-degree relatives, and healthy unrelated control subjects. Arthritis Res Ther (2017) 19(1):249. doi: 10.1186/s13075-017-1459-x
166. Liu Y, Han Y, Qu H, Fang J, Ye M, Yin W. Correlation of microRNA expression profile with clinical response to tumor necrosis factor inhibitor in treating rheumatoid arthritis patients: A prospective cohort study. J Clin Lab Anal (2019) 33(7):e22953. doi: 10.1002/jcla.22953
167. Luo Q, Zhang L, Li X, Fu B, Deng Z, Qing C, et al. Identification of circular RNAs hsa_circ_0044235 in peripheral blood as novel biomarkers for rheumatoid arthritis. Clin Exp Immunol (2018) 194(1):118–24. doi: 10.1111/cei.13181
168. Chen S, Luo Z, Chen X. Hsa_circ_0044235 regulates the pyroptosis of rheumatoid arthritis via MiR-135b-5p-SIRT1 axis. Cell Cycle (2021) 20(12):1107–21. doi: 10.1080/15384101.2021.1916272
169. Ouyang Q, Liu C, Lu X, Liang R, Zhao J, Yang M. Identification of circular RNAs Circ_0005008 and Circ_0005198 in plasma as novel biomarkers for new-onset rheumatoid arthritis. Front Pharmacol (2021) 12:722017. doi: 10.3389/fphar.2021.722017
170. Saad El-Din S, Ahmed Rashed L, Eissa M, Eldemery AB, Abdelkareem Mohammed O, Abdelgwad M. Potential role of circRNA-HIPK3/microRNA-124a crosstalk in the pathogenesis of rheumatoid arthritis. Rep Biochem Mol Biol (2022) 10(4):527–36. doi: 10.52547/rbmb.10.4.527
171. Jiang Z, Zhong Z, Miao Q, Zhang Y, Ni B, Zhang M, et al. circPTPN22 as a novel biomarker and ceRNA in peripheral blood mononuclear cells of rheumatoid arthritis. Mol Med Rep (2021) 24(2):617. doi: 10.3892/mmr.2021.12256
172. Tang X, Wang J, Xia X, Tian J, Rui K, Xu H, et al. Elevated expression of ciRS-7 in peripheral blood mononuclear cells from rheumatoid arthritis patients. Diagn Pathol (2019) 14(1):11. doi: 10.1186/s13000-019-0783-7
173. Chen Y, Xu X, Li X, Zhong J, Wu B, Shang J, et al. Identification of circular RNAs hsa_circ_0140271 in peripheral blood mononuclear cells as a novel diagnostic biomarker for female rheumatoid arthritis. J Orthop Surg Res (2021) 16(1):647. doi: 10.1186/s13018-021-02794-8
174. Peng H, Xing J, Wang X, Ding X, Tang X, Zou J, et al. Circular RNA circNUP214 modulates the T helper 17 cell response in patients with rheumatoid arthritis. Front Immunol (2022) 13:885896. doi: 10.3389/fimmu.2022.885896
175. Yang X, Li J, Wu Y, Ni B, Zhang B. Aberrant dysregulated circular RNAs in the peripheral blood mononuclear cells of patients with rheumatoid arthritis revealed by RNA sequencing: novel diagnostic markers for RA. Scand J Clin Lab Invest (2019) 79(8):551–9. doi: 10.1080/00365513.2019.1674004
176. Luo Q, Zeng L, Zeng L, Rao J, Zhang L, Guo Y, et al. Expression and clinical significance of circular RNAs hsa_circ_0000175 and hsa_circ_0008410 in peripheral blood mononuclear cells from patients with rheumatoid arthritis. Int J Mol Med (2020) 45(4):1203–12. doi: 10.3892/ijmm.2020.4498
177. Lu H, Yang Y, Kuang D, Liu P, Yang J. Expression profile of circRNA in peripheral blood mononuclear cells of patients with rheumatoid arthritis. BMC Med Genomics (2022) 15(1):77. doi: 10.1186/s12920-022-01225-9
178. Wen J, Liu J, Zhang P, Jiang H, Xin L, Wan L, et al. RNA-Seq reveals the circular RNA and miRNA expression profile of peripheral blood mononuclear cells in patients with rheumatoid arthritis. Biosci Rep (2020) 40(4):BSR20193160. doi: 10.1042/bsr20193160
179. Cai Y, Liang R, Xiao S, Huang Q, Zhu D, Shi GP, et al. Circ_0088194 promotes the invasion and migration of rheumatoid arthritis fibroblast-like synoviocytes via the miR-766-3p/MMP2 axis. Front Immunol (2021) 12:628654. doi: 10.3389/fimmu.2021.628654
180. Luo Z, Chen S, Chen X. CircMAPK9 promotes the progression of fibroblast-like synoviocytes in rheumatoid arthritis via the miR-140-3p/PPM1A axis. J Orthop Surg Res (2021) 16(1):395. doi: 10.1186/s13018-021-02550-y
181. Wang R, Li H, Han Y, Li L. Knockdown of circ_0025908 inhibits proliferation, migration, invasion, and inflammation while stimulates apoptosis in fibroblast-like synoviocytes by regulating miR-650-dependent SCUBE2. Autoimmunity (2022) 55(7):473–84. doi: 10.1080/08916934.2022.2102164
182. Li J, Liu D, Wu K, Chen Q, Lei J. Circ_0003972 promotes the proliferation and inflammation of fibroblast-like synovial cells in rheumatoid arthritis through regulation of the miR-654-5p/FZD4 axis. Immunol Invest. (2022) 51(5):1437–51. doi: 10.1080/08820139.2021.1958837
183. Wang L, Zhao Q, Wang N, Ding Y, Kong L, Wang J. Circ_0000396 inhibits rheumatoid arthritis synovial fibroblast growth and inflammatory response via miR-203/HBP1 axis. J Biol Res (Thessalon). (2021) 28(1):1. doi: 10.1186/s40709-020-00131-4
184. Hao J, Chen Y, Yu Y. Circular RNA circ_0008360 inhibits the proliferation, migration, and inflammation and promotes apoptosis of fibroblast-like synoviocytes by regulating miR-135b-5p/HDAC4 axis in rheumatoid arthritis. Inflammation (2022) 45(1):196–211. doi: 10.1007/s10753-021-01538-4
185. Wen J, Liu J, Wang X, Wang J. Expression and clinical significance of circular RNAs related to immunity and inflammation in patients with rheumatoid arthritis. Int Immunopharmacol. (2021) 92:107366. doi: 10.1016/j.intimp.2021.107366
186. Ciechomska M, Wojtas B, Bonek K, Roszkowski L, Gluszko P, Benes V, et al. Comprehensive microRNA and transcriptomic profiling of rheumatoid arthritis monocytes: role of microRNA-146b in pro-inflammatory progression. Rheumatol (Oxford). (2021) 60(11):5424–35. doi: 10.1093/rheumatology/keab407
187. Wang Y, Zheng F, Gao G, Yan S, Zhang L, Wang L, et al. MiR-548a-3p regulates inflammatory response via TLR4/NF-κB signaling pathway in rheumatoid arthritis. J Cell Biochem (2018). doi: 10.1002/jcb.26659
188. Wielińska J, Crossland RE, Łacina P, Świerkot J, Bugaj B, Dickinson AM, et al. Exploring the extracellular vesicle MicroRNA expression repertoire in patients with rheumatoid arthritis and ankylosing spondylitis treated with TNF inhibitors. Dis Markers. (2021) 2021:2924935. doi: 10.1155/2021/2924935
189. Ponting CP, Oliver PL, Reik W. Evolution and functions of long noncoding RNAs. Cell (2009) 136(4):629–41. doi: 10.1016/j.cell.2009.02.006
190. Lv Z, Ye S, Wang Z, Xin P, Chen Y, Tan Z, et al. Long non-coding RNA TSPEAR antisense RNA 2 is downregulated in rheumatoid arthritis and inhibits the apoptosis of fibroblast-like synoviocytes by downregulating microRNA-212-3p (miR-212-3p). Bioengineered (2022) 13(2):4166–72. doi: 10.1080/21655979.2021.2021347
191. Gong X, Fan X, Zhang Z, Cai Q, Guo M, Gao C, et al. Circulating lnc-ITSN1-2 expression presents a high value in diagnosis of rheumatoid arthritis and correlates with disease activity. Int J Clin Exp pathol (2017) 10(10):10451–8.
192. Yue T, Fan X, Zhang Z, Liu Z, Guo M, Bai F, et al. Downregulation of lncRNA ITSN1-2 correlates with decreased disease risk and activity of rheumatoid arthritis (RA), and reduces RA fibroblast-like synoviocytes proliferation and inflammation via inhibiting NOD2/RIP2 signaling pathway. Am J Trans Res (2019) 11(8):4650–66.
193. Shaker OG, Mahmoud RH, Abdelaleem OO, Ahmed TI, Fouad NA, Hussein HA, et al. Expression profile of long noncoding RNAs, lnc-Cox2, and HOTAIR in rheumatoid arthritis patients. J Interferon Cytokine Res (2019) 39(3):174–80. doi: 10.1089/jir.2018.0117
194. Wahba AS, Ibrahim ME, Mesbah NM, Saleh SM, Abo-Elmatty DM, Mehanna ET. Serum LINC00305 expression and its genetic variant rs2850711 are associated with clinical and laboratory features of rheumatoid arthritis. Br J BioMed Sci (2020) 77(3):142–7. doi: 10.1080/09674845.2020.1744942
195. Wang Y, Li G, Guo W, Ji B, Aisikeerbayi A, Boratibai Y, et al. LncRNA PlncRNA-1 participates in rheumatoid arthritis by regulating transforming growth factor β1. Autoimmunity (2020) 53(6):297–302. doi: 10.1080/08916934.2020.1750010
196. Fu Q, Song MJ, Fang J. LncRNA OSER1-AS1 regulates the inflammation and apoptosis of rheumatoid arthritis fibroblast like synoviocytes via regulating miR-1298-5p/E2F1 axis. Bioengineered (2022) 13(3):4951–63. doi: 10.1080/21655979.2022.2037854
197. Sun L, Tu J, Liu C, Pan A, Xia X, Chen X. Analysis of lncRNA expression profiles by sequencing reveals that lnc-AL928768.3 and lnc-AC091493.1 are novel biomarkers for disease risk and activity of rheumatoid arthritis. Inflammopharmacology (2020) 28(2):437–50. doi: 10.1007/s10787-019-00666-6
198. Wang J, Shen C, Li R, Wang C, Xiao Y, Kuang Y, et al. Increased Long Noncoding RNA LINK-a Contributes to Rheumatoid Synovial Inflammation and Aggression. JCI Insight (2021) 6(23):e146757. doi: 10.1172/jci.insight.146757
199. Cao J, Lv X, Zhang Y, Xu A, Jiang T. LncRNA GAS5 activates the AMPK pathway in peripheral blood mononuclear cells derived from rheumatoid arthritis patients. Int J Rheum Dis (2020) 23(10):1318–27. doi: 10.1111/1756-185x.13930
200. Peng T, Ji D, Jiang Y. Long non-coding RNA GAS5 suppresses rheumatoid arthritis progression via miR-128-3p/HDAC4 axis. Mol Cell Biochem (2021) 476(6):2491–501. doi: 10.1007/s11010-021-04098-1
201. Elamir AM, Senara S, Abdelghaffar NK, Gaber SN, El Sayed HS. Diagnostic role of lncRNA GAS5 and its genetic polymorphisms rs2067079, rs6790 and rs17359906 in rheumatoid arthritis. BioMed Rep (2021) 15(5):93. doi: 10.3892/br.2021.1469
202. Yang Z, Lin SD, Zhan F, Liu Y, Zhan YW. LncRNA GAS5 alleviates rheumatoid arthritis through regulating miR-222-3p/Sirt1 signalling axis. Autoimmunity (2021) 54(1):13–22. doi: 10.1080/08916934.2020.1846183
203. Ouyang Q, Wu J, Jiang Z, Zhao J, Wang R, Lou A, et al. Microarray expression profile of circular RNAs in peripheral blood mononuclear cells from rheumatoid arthritis patients. Cell Physiol Biochem (2017) 42(2):651–9. doi: 10.1159/000477883
204. Orellana EA, Siegal E, Gregory RI. tRNA dysregulation and disease. Nat Rev Genet (2022) 23(11):651–64. doi: 10.1038/s41576-022-00501-9
205. Zong T, Yang Y, Zhao H, Li L, Liu M, Fu X, et al. tsRNAs: Novel small molecules from cell function and regulatory mechanism to therapeutic targets. Cell Prolif (2021) 54(3):e12977. doi: 10.1111/cpr.12977
206. Wajahat M, Bracken CP, Orang A. Emerging Functions for snoRNAs and snoRNA-Derived Fragments. Int J Mol Sci (2021) 22(19):10193. doi: 10.3390/ijms221910193
207. Rayford KJ, Cooley A, Rumph JT, Arun A, Rachakonda G, Villalta F, et al. piRNAs as Modulators of Disease Pathogenesis. Int J Mol Sci (2021) 22(5):2373. doi: 10.3390/ijms22052373
208. Foers AD, Garnham AL, Smyth GK, Proudman SM, Cheng L, Hill AF, et al. Circulating small noncoding RNA biomarkers of response to triple disease-modifying antirheumatic drug therapy in white women with early rheumatoid arthritis. J Rheumatol (2020) 47(12):1746–51. doi: 10.3899/jrheum.191012
209. Rudan I, Sidhu S, Papana A, Meng SJ, Xin-Wei Y, Wang W, et al. Prevalence of rheumatoid arthritis in low- and middle-income countries: A systematic review and analysis. J Glob Health (2015) 5(1):10409. doi: 10.7189/jogh.05.010409
210. van der Linden MP, Knevel R, Huizinga TW, van der Helm-van Mil AH. Classification of rheumatoid arthritis: comparison of the 1987 American college of rheumatology criteria and the 2010 American college of Rheumatology/European league against rheumatism criteria. Arthritis Rheumatol (2011) 63(1):37–42. doi: 10.1002/art.30100
211. Moharamoghli M, Hassan-Zadeh V, Dolatshahi E, Alizadeh Z, Farazmand A. The expression of GAS5, THRIL, and RMRP lncRNAs is increased in T cells of patients with rheumatoid arthritis. Clin Rheumatol (2019) 38(11):3073–80. doi: 10.1007/s10067-019-04694-z
212. Piao X, Zhou J, Hu J. Role of RP11-83J16.1, a novel long non-coding RNA, in rheumatoid arthritis. Am J Trans Res (2020) 12(4):1397–414.
213. Chatterjee S, Bhattcharjee D, Misra S, Saha A, Bhattacharyya NP, Ghosh A. Increase in MEG3, MALAT1, NEAT1 significantly predicts the clinical parameters in patients with rheumatoid arthritis. Per Med (2020) 17(6):445–57. doi: 10.2217/pme-2020-0009
214. Wang Z, Zhang W, Li S, Chen D, Wang L, Xu B, et al. Multiple time-point assessment of lncRNA MEG3 shows potential to monitor treatment efficacy in rheumatoid arthritis patients. biomark Med (2021) 15(14):1261–70. doi: 10.2217/bmm-2021-0070
215. Wen J, Liu J, Jiang H, Wan L, Xin L, Sun Y, et al. lncRNA expression profiles related to apoptosis and autophagy in peripheral blood mononuclear cells of patients with rheumatoid arthritis. FEBS Open Bio (2020) 10(8):1642–54. doi: 10.1002/2211-5463.12913
216. Sun Y, Liu J, Wen J, Huang D, Zhou Q, Zhang X, et al. Overexpression of long noncoding RNA LINC00638 inhibits inflammation and oxidative stress in rheumatoid arthritis fibroblast-like synoviocytes by regulating the Nrf2/HO-1 pathway. Immun Inflammation Dis (2022) 10(7):e663. doi: 10.1002/iid3.663
Keywords: rheumatoid arthritis, biomarkers, mRNA, non-coding RNA, prognosis, diagnosis
Citation: Jiang Y, Zhong S, He S, Weng J, Liu L, Ye Y and Chen H (2023) Biomarkers (mRNAs and non-coding RNAs) for the diagnosis and prognosis of rheumatoid arthritis. Front. Immunol. 14:1087925. doi: 10.3389/fimmu.2023.1087925
Received: 02 November 2022; Accepted: 09 January 2023;
Published: 01 February 2023.
Edited by:
Amra Adrovic, Koç University Hospital, TürkiyeReviewed by:
S. Amanda Ali, Henry Ford Health System, United StatesCopyright © 2023 Jiang, Zhong, He, Weng, Liu, Ye and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hanwei Chen, ZG9jdGVyd2VpQHNpbmEuY29t; Yufeng Ye, ODM4NTU0MzI1QHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.