- 1Department of Rheumatology and Clinical Immunology, Jiangxi Provincial People’s Hospital, Medical College of Nanchang University, Nanchang, China
- 2Department of Rheumatology and Clinical Immunology, Jiangxi Provincial People’s Hospital, The First Affiliated Hospital of Nanchang Medical College, Nanchang, China
- 3Department of Internal Medicine, Patan Academy of Health Sciences, Kathmandu, Nepal
Rheumatoid arthritis (RA) is a chronic inflammatory disease characterized by multi-articular, symmetrical and invasive arthritis resulting from immune system abnormalities involving T and B lymphocytes. Although significant progress has been made in the understanding of RA pathogenesis, the underlying mechanisms are not fully understood. Recent studies suggest that NLRP3 inflammasome, a regulator of inflammation, might play an important role in the development of RA. There have been increasing clinical and pre-clinical evidence showing the treatment of NLRP3/IL-1β in inflammatory diseases. To provide a foundation for the development of therapeutic strategies, we will briefly summarize the roles of NLRP3 inflammasome in RA and explore its potential clinical treatment.
1 Introduction
Rheumatoid arthritis (RA) is a chronic systemic autoimmune disease with a pathological basis in synovitis, manifesting as symmetric polyarticular invasive joint inflammation with extra-articular organ involvement, and patients with rheumatoid arthritis are characterized by positive serum rheumatoid factor and Anti-citrullinated protein antibodies (ACPAs) (1). The global average prevalence of RA ranges from 0.5% to 1.0% (2), with a higher prevalence among women and the elderly (1, 2). However, the pathogenesis of RA is not fully understood, which hinders the diagnosis and treatment of RA. In addition, the use of biologics has improved the condition of patients with RA while increasing the risk of infection (3, 4). Therefore, indepth study of the pathogenesis of rheumatoid arthritis is of greater significance for the development of new treatment strategies, but the pursuit of curative effect needs to pay attention to the safety of drugs (5). The pathogenesis of RA involves many immune cells and cytokines, including interleukin-1 (IL-1), interleukin-6 (IL-6), interleukin-18 (IL-18), and tumor necrosis factor (TNF) as the main pro-inflammatory cytokines, which induce inflammatory response and osteoarthritis injury (6). The NLRP3 inflammasome is a key source of IL-1 and IL-18, and accumulating evidence suggests that the inflammasome plays a role in the pathogenesis of rheumatic diseases (7). Here we discuss the current progress of the NLRP3 inflammasome in rheumatoid arthritis.
2 Overview of NLRP3 Inflammasome
The inflammasome, a group of multimeric protein complexes, identifies pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) by pathogen-recognition receptors (PRRs) to mediate host immune responses. The inflammasome is generally composed of a PRR, pro-caspase-1, and an adaptor protein that connects the PRR with pro-caspase-1 (8). The inflammasome promotes the maturation and secretion of IL-1β and IL-18 during natural immune defense by activating caspase-1, and also regulates adaptive immunity (7). In addition, inflammasome also mediates the caspase-1-dependent programmed cell apoptosis (pyroptosis), which induces cell death under inflammatory and stressed pathological conditions (9–11).
2.1 Classification of Inflammasomes and Activation of NLRP3 Inflammasome
The nucleotide-binding domain(NOD)–like receptor(NLR) protein consists of an N-terminal recruitment domain, a central nucleotide-binding domain that mediates oligomerization, and carboxy-terminal Leucine Rich Repeats (LRRs) (12–14). Depending on the existence of NLR protein, inflammasomes are divided into NLR family and non-NLR family. The former includes nucleotide‐binding domain leucine‐rich repeat pyrin domain containing 1(NLRP1), NOD-like receptor family pyrin domain containing 3 (NLRP3), and NLR-family CARD-containing protein 4 (NLRC4), while the latter includes Absent in Melanoma 2 (AIM2), pyrin inflammasomes (15). Based on the activation of caspase during inflammasome formation, inflammasomes containing caspase 1 are known as canonical inflammasomes, and complexes containing caspase 4, caspase 5, or caspase 11 are known as non-canonical inflammasomes. The caspase recruitment domain(CARD) motifs of caspases 4, 5, and 11 can directly bind to a portion of the intracellular lipopolysaccharide, leading to the activation of these caspases and the subsequent secretion of IL1 and IL18 (16–18). The NLRP3 inflammasome is the most studied inflammasome, and the NLRP3 contains three domains: pyrin domain(PYD), NACHT and LRR (19, 20). Activation of the NLRP3 inflammasome requires two steps (21–23): In the priming step (signal 1), PRRs such as toll-like receptors (TLRs) recognize PAMPs or DAMPs to activate the NF-κB signaling pathway and upregulate the expression of NLRP3 and pro-IL-1β. During the activation step (signal 2), in response to multiple stimuli such as reactive oxygen species (ROS), K+ efflux, ATP, lysosomal rupture, and bacterial or fungal components (24–27),NLRP3 binds to the adaptor protein ASC through the PYD domain and recruits pro-caspase-1 through the CARD domain to finally form the NLRP3 inflammasome (28). After the activation, caspase-1 will cleave pro-IL-1, pro-IL-18, and gasdermin D (GSDMD), leading to an inflammatory response and pyroptosis (29–32).
2.2 Regulation of the NLRP3 Inflammasome Activation
The NLRP3 inflammasome can be activated by a variety of stimuli such as transmembrane movement of ions, mitochondrial dysfunction, lysosomal rupture, and ROS. Hence, the regulation of its activation process is quite complex. Some potential regulatory mechanisms have been studied, such as the role of NIMA-related kinase 7 (NEK7), the regulation of autophagy/mTOR pathway, and changes in subcellular localization (27, 33, 34).
2.2.1 Regulation of the Activation Step
NEK7 is involved in mitosis and plays a crucial role in the activation of the NLRP3 inflammasomes. Under the mediation of ROS and K+ efflux, NEK7 combines with the LRR domain of NLRP3, regulating NLRP3 inflammasome assembly as well as caspase-1 activation (35–37). A recent study showed that the stress granule protein DEAD-box helicase 3(DDX3X) can also contribute to NLRP3 activation by interacting with NLRP3 (38). Autophagy is a physiological process in which lysosomes degrade intracellular pathogens, damaged organelles, and proteins, contributing to host defense and cell homeostasis. It has been shown that the autophagosome directly encapsulates and degrades the NLRP3 inflammasome to prevent its activation (39, 40). Current studies have highlighted the emerging concept of organelles involved in NLRP3 activation. The NLRP3 inflammasome is composed of three different proteins, and recent studies have indicated that alterations in the subcellular localization of these molecules are also responsible for the assembly and activation of NLRP3 inflammasome. Activation of NLRP3 requires contributions from mitochondrial signals for priming, and the endoplasmic reticulum(ER), trans-Golgi network, cytoskeletal infrastructure, and microtubule-organizing center (MTOC) for transport and assembly (41). Mitochondria-associated ER membranes(MAM) and MTOC NLRP3 locates in the endoplasmic reticulum (ER) and cytosol, and NLRP3 in the endoplasmic reticulum binds to ASC on the adjacent mitochondria at the MAM upon various stimuli. NLRP3 relocates to the microtubule tissue center in the presence of microtubule affinity regulating kinase 4 (MARK4). When NLRP3 reaches the MTOC, NEK7 binds with NLRP3, and the inflammasome is assembled (42). In the absence of activation, NLRP3 localizes in the cytoplasm and endoplasmic reticulum but relocalizes in the mitochondria and Golgi apparatus after activation (43). Stimulation of NLRP3 destroys the trans Golgi network (TGN) and turns it into a dispersed TGN (dTGN). Furthermore, phosphatidylinositol-4-phosphate on dTGN promotes NLRP3 aggregation, which is essential for downstream ASC oligomerization and caspase-1 activation (44). Overall, these data suggest that spatially interaction among ER-mitochondria-Golgi apparatus is closely associated with NLRP3 activation, and understanding these regulatory processes may reveal new checkpoints for inflammasome.
A recent structural modeling study using cryo-electron microscopy described a double-ring cage structure held by 6-8 NLRP3 dimers via LRR-LRR interaction with the PYD shielded within the assembly to avoid premature activation. The cage structure may provide a mechanism for rapid activation of NLRP3 when NLRP3 monomers are assembled and in a standby state to sense signals and convert to their active conformation. They also confirmed that NLRP3 cage is also necessary for the dispersal of TGN. However, it is worth considering whether the conformation of cage is regulated by factors such as ion flux alteration and post-translational modifications (45). Moreover, Immunometabolism and circadian oscillation are also involved in regulating NLRP3 activation (46, 47).
2.2.2 Regulation of the Priming Step
During the priming of NLRP3 inflammasome activation, NLRP3 protein expression is upregulated. And several mediators are involved in regulating NLRP3 transcription, including myeloid differentiation primary response 88 (MyD88) and TIR domain-containing adapter-inducing interferon-β (TRIF) (21), IL1 receptor-associated kinase (IRAK1) (48), Fas-associated protein with death domain (FADD) and caspase-8 (49). These mediators drive the transcription of the NLRP3 gene in preparation for activation. Additionally, it has been demonstrated that miRNAs regulate NLRP3 mRNA translation by binding to the untranslated regions (UTRs) of the transcript (50, 51). Post-translational modifications, such as ubiquitination and phosphorylation, are also important regulators of NLRP3 inflammasome activation. NLRP3 inflammasome ubiquitinates in macrophages when activated (52). It was reported that the vitamin D receptor negatively regulates NLRP3 activation by blocking deubiquitination (53). The process of ubiquitination is catalyzed by a series of enzymes, including E3 ubiquitin ligases. The E3 ligase tripartite motif-containing protein(TRIM31) has been reported to promote NLRP3 polyubiquitination thus inhibiting the excess activation of NLRP3 inflammasome (54). Dopamine inhibition of NLRP3 inflammasome is also achieved by the E3 ligase MARCH7-mediated ubiquitination of NLRP3 protein (55). However, another research showed that the E3 ligase Pellino2 promotes NLRP3 inflammasome activation through ubiquitination of NLRP3 (56). The exact mechanism by which multiple E3 ligases interact with different NLRP3 sites remains to be fully determined. Previous studies showed that NLRP3 is a substrate of protein kinase A (PKA), which phosphorylates NLRP3 at ser295 and inhibits the activation of the NLRP3 inflammasome (57, 58). However, protein kinase D plays a facilitating role in NLRP3 inflammasome activation at the same site (59). In addition, protein tyrosine phosphatase non-receptor type 22 (PTPN22) and phosphotase 2A (PP2A) can promote NLRP3 activation through dephosphorylation (60, 61). Epigenetic factors also regulate the activation of NLRP3 inflammasome, including DNA methylation and histone modifications. NLRP3 is methylated in health and mediates inflammatory suppression. Histone acetylation mediates the inflammatory response, while histone deacetylation induces inflammation resolution (62). It has been demonstrated that NLRP3 inflammasome expression can be down-regulated by inhibiting histone acetylation on NLRP3 promoter (63).
2.3 Immunomodulatory Effects of the NLRP3 Activation Products
The NLRP3 inflammasome is an important bridge connecting innate and adaptive immunity, and the activated NLRP3 inflammasome activates caspase-1 to produce biologically active IL-1 and IL-18. IL-1 and IL-18 belong to the IL-1 family and play a critical role in host immune regulation. IL-1 is a potent proinflammatory cytokine, mainly expressed on monocytes, macrophages and dendritic cells (DCs). IL-1β induces the upregulation of adhesion molecules and chemokines, leading to leukocytes recruitment and ultimately triggering a series of inflammatory responses (64). DC is an antigen-presenting cell that induces T cell activation (65). IL-1 activates DC to generate interferon-gamma (IFN-γ) in T cells. As a T cell co-stimulator, IL-1 induces T cell differentiation and polarization, especially toward T helper type 17 (Th17)cells. And IL-1β induces differentiation of naive CD4 + T cells into Th17 and also promotes Th9 differentiation in concert with other cytokines (66, 67). Moreover, IL-1β also facilitates the proliferation of B cells and the production of antibodies. IL-18, also known as IFN-γ inducing factor, drives the production of IFN-γ in Th1 cells and also works with IL-12 and IL-15 to activate natural killer (NK) cells to induce IFN-γ production (68). In epithelial cells, IL-18 regulates the function of Th17 cells and regulatory T(Treg) cells, resulting in an imbalance of Th17/Treg (69).As activation products of NLRP3 inflammasome, IL-1β and IL-18 contribute to proinflammatory T cell differentiation and activate adaptive immune responses (70). Accordingly, the NLRP3 inflammasome plays a vital role in immune regulation through leading to autoimmune diseases by its dysfunction or hyperactivation, and rheumatoid arthritis is one of them.
2.4 Role of IL-1β and IL18 in RA
The IL-1 family is the important inflammatory regulator that promotes the activation of innate immune system cells and is involved in the pathological process of various diseases. IL-1β, the best functionally member of the IL-1 family, is one of the major pathogenic factors of RA and mediates the destruction of bone and cartilage (71). Receptor activator of nuclear factor kappa-B ligand (RANKL)is the key osteoclastogenic cytokine that binds receptor activator of NF-kB(RANK) on osteoclast precursor cells and mediates osteoclast differentiation and activation, leading to bone resorption. IL-1β upregulates RANKL production, enhances its activity and stimulates osteoclast production to induce bone erosion (72). IL-1β also acts on osteoclast progenitors to stimulate osteoclastogenesis (73). In addition, IL-1β acts in concert with other inflammatory factors such as TNF-α to amplify the inflammatory response and induce bone loss (71). In rheumatoid arthritis synovium, IL1β is involved in cartilage degeneration by stimulating fibroblasts and chondrocytes to secrete matrix metalloproteinase (MMF), which in turn exacerbates synovial inflammation and bone destruction (73). Meanwhile, IL-1β impairs the synthesis of new bone matrix and inhibits osteoblast production in RA, thereby reducing new bone generation (74).
IL-18 is a pleiotropic cytokine that plays an important role in the flare and maintenance of the inflammatory response during RA. IL-18 plays a role by activating T cells in synovium to produce inflammatory cytokines, RANKL and so on, mediating bone destruction (75). Pannus formation is one of the pathological features of RA, and is also the main cause of joint lesions and cartilage destruction. In vitro, IL-18 triggers the production of vascular growth factors such as vascular endothelial growth factor, monocyte chemotactic protein 1, and stromal cell-derived factor 1, and facilitates the formation of vascular opacities (76).
3 The NLRP3 Inflammasome and RA
Rheumatoid arthritis (RA) is one of the most common autoimmune diseases. Increasing evidence suggests that the NLRP3 inflammasome is involved in the pathogenesis of RA. Anti-citrullinated protein antibodies are a group of autoantibodies against citrullinated proteins/peptides and are biomarkers of RA. ACPA promotes IL-1 production in rheumatoid arthritis by activating the NLRP3 inflammasome (77, 78). Several studies have shown an upregulation of NLRP3 mRNA and NLRP3-associated proteins in monocytes, macrophages, and dendritic cells in RA patients (79–81). Polymorphisms in the NLRP3 gene indirectly reflect the susceptibility, disease severity and treatment effect of RA. Rs4612666, rs10754558, rs10159239, and rs35829419 have been investigated as NLRP3 single nucleotide polymorphisms (SNPs) associated with susceptibility to rheumatoid arthritis, in which rs35829419 and CARD8 rs2043211 mutations are related to disease severity, while rs10159239 and rs4612666 are related to the therapeutic response of RA on anti-TNF (12, 82–85).
3.1 NLRP3 Inflammasome Mediates the Pathogenesis of RA
The involvement of the NLRP3 inflammasome in RA pathogenesis has been demonstrated in both animal and cell experiments. Genetics is closely linked to susceptibility to RA (86). The RA susceptibility gene A20, also called tumor necrosis factor alpha-induced protein 3 gene (TNFAIP3), is a cytokine-inducible protein that inhibits apoptosis and activates NF-κB. A20-deficient mice were prone to spontaneous erosive arthritis, which was found to be related to elevated NLRP3 expression and IL-1β secretion (87). Collagen-induced arthritis (CIA) is the most commonly used animal model to support the role of inflammasome in inflammatory arthritis (88). The expression of NLRP3 was proved to be positively correlated with arthritis severity in the synovium of CIA mice (89). Likewise, antigen-induced arthritis (AIA) mice exhibit severe joint inflammation with increased expression of IL-1β and NLRP3 inflammasome in their synovium (90). In CFA-induced arthritic rats, cinnamaldehyde alleviates the inflammatory response by activating succinate/hypoxia-inducible factor-1 (HIF-1) to suppress NLRP3-derived IL-1β (91). These data indicate that NLRP3 inflammasome is involved in the pathogenesis of RA. Activation of inflammasome can also occur in non-phagocytes, such as T cells, endothelial cells, and epithelial cells. Th17 cells mediate pro-inflammatory responses through the secretion of IL-17A and TNF-α, leading to tissue destruction, articular cartilage and bone damage. In contrast, Tregs mediate anti-inflammatory responses through the secretion of IL-10 and TGF-β. Recent studies have noted that the imbalance of Treg/Th17 cells affects the inflammatory response in RA (92). It is known that tofacitinib also restores the balance of Treg/Th17 cells in rheumatoid arthritis and alleviates the inflammatory response by inhibiting NLRP3 inflammasome (93). Furthermore, elevated extracellular Ca2+ concentration promotes the uptake of colloidal calciprotein particles (CPPs) by monocytes in RA patients and contributes to NLRP3 inflammasome activation (94). The above studies showed NLRP3 inflammasome is involved in RA by regulating different cells.
3.2 NLRP3 Inflammasome as a Protective Factor in RA
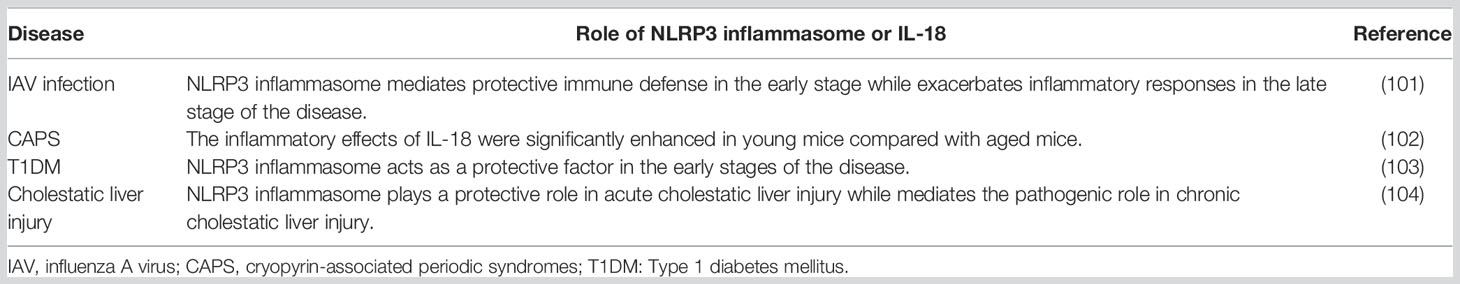
However, neutrophils were less sensitive to pyroptosis compared with macrophages (95, 96), and expression of NLRP3 and ASC were significantly decreased in neutrophils of RA patients. Meanwhile, mRNA expression of NLRP3 in neutrophils was negatively correlated with the 28-joint Disease Activity Score based on C-reactive protein (DAS28-CRP) in patients with RA (97, 98). These results indicate that different cell types exhibit different responses to inflammasome stimulation, and NLRP3 inflammasome may be protective in RA. The conclusion was also confirmed in another research (99). The pathogenic role of NLRP3 has been demonstrated in systemic lupus erythematosus, inflammatory bowel disease, and type 1 diabetes mellitus(T1DM). Nevertheless, the protective effect of NLRP3 inflammasome has also been illustrated in these diseases (34). The exact mechanism of this effect is not specified, requiring a deeper understanding of the role of NLRP3 inflammasome in diseases. But it may be explained by the following speculations: a)NLRP3 performs different functions at different stages of the disease (Table1) (102); b) NLRP3 exerts opposite effects through the regulation of other cytokines (104); c) NLRP3 maintains immune homeostasis and thus plays a protective role. Recent studies showed that NLRP3 inflammasome is a crucial regulator of intestinal homeostasis. NLRP3 inflammasome supports the integrity of the intestinal mucosal barrier and also has a regulatory impact on intestinal flora (105, 106).
4 Potential Therapeutic Targets for the NLRP3 Inflammasome in Rheumatoid Arthritis
4.1 Blockade of NLRP3 Activation Products
Targeted treatment of rheumatoid arthritis by blocking cytokines has been recognized. Anakinra is a recombinant form of a human IL-1 receptor antagonist that competitively inhibits IL-1αand IL-1β (107). Although approved by the Food & Drug Administration (FDA) for some patients with rheumatoid arthritis (108), Anakinra is only moderately effective and is inferior to TNF-α inhibitors, indicating its poor applicability (109). Additionally, a human monoclonal IL-1β antibody canakinumab, and a decoy receptor of IL-1α and IL-1β rilonacept have been focused on in rheumatoid arthritis (27). Inhibition of caspase-1 blocks the downstream signaling of inflammasome and the release of active IL-1β, thereby resolving the inflammation. The most studied caspase-1 inhibitors are VX-765 (belnacasan) and VX-740 (pralnacasan).VX-740 attenuated the joint damage in both RA and OA mice, but its application was limited by animal hepatotoxicity (110, 111). VX-765 is structurally similar to VX-740, acting by covalent modification of the catalytic cysteine residues in the caspase-1 active site, which has been tested in phase II trials for psoriasis and epilepsy, but not yet in rheumatoid arthritis (112, 113). Non-steroidal anti-inflammatory drugs (NSAIDs) are universally used and their anti-inflammatory property is the inhibition of cyclooxygenase (COX) isozymes. It has been proposed that inhibition of caspase enzymes reduces the production of proinflammatory cytokines, suggesting that there may be other targets for NSAIDs to promote anti-inflammatory responses beyond the COX pathway (114).
4.2 Inhibition of NLRP3 Inflammasome Activation
Inhibition of the NLRP3 inflammasome includes the blockage of the NLRP3 inflammasome assembly and the suppression of the NLRP3-related signaling pathways (115).
4.2.1 Inhibition of NLRP3 Inflammasome Assembly
Compound MCC950 is the most widely studied inhibitor of NLRP3 inflammasome with high efficiency and specificity. MCC950 ameliorates rheumatoid arthritis injury by inhibiting NLRP3 activation and subsequent IL-1β production (79). It has been reported that MCC950 blocks ATP hydrolysis and suppresses NLRP3 inflammasome formation and activation by directly interacting with the NACHT domain of NLRP3 (116, 117). However, the application of MCC950 was limited by hepatotoxicity in a phase II clinical trial of RA (27). Both CY-09 and tranilast (TR) (118–120) bind directly to the ATP-binding motif of the NACHT domain of NLRP3 to inhibit ATPase activity and thus prevent the assembly of NLRP3 inflammasome, which may be promising in the management of rheumatoid arthritis. RRX-001 is a highly selective NLRP3 inflammasome inhibitor that acts by covalently binding to cysteine 409 of NLRP3 to interfere with its assembly. It is a novel NLRP3-related disease therapeutic target identified in recent years (121). However, RRX001 contains high-energy nitro functional groups, which may cause drug toxicity. Compound 149-01, an analog of RRX001 without high-energy nitro functional groups, was recently identified as a potent and specific NLRP3 inhibitor that inhibits NLRP3 activation and attenuates inflammatory responses in vivo and vitro by preventing NLRP3 from binding to NEK7 (122). Licochalcone B (LicoB), a major component of traditional medicinal herb licorice, was also found to disturb the interaction between NLRP3 and NEK7, thus inhibiting NLRP3 activation (123). LL-Z1640-2(LLZ) is a preclinical drug that primarily targets TGF-β-activated kinase-1(TAK1), which produces a variety of proinflammatory cytokines and inflammatory mediators in RA. LLZ showed superior therapeutic efficacy against RA in preclinical trials. In CIA mice, LLZ was observed to significantly prevent the formation and activation of NLRP3 inflammasome in synovial macrophages and osteoclasts (124). A recently identified novel compound 59 known as J114 was shown to interfere with NLRP3-ASC interaction and potently suppress ASC oligomerization during NLRP3 activation. Interestingly, the function of J114 exhibits species differences (125). Although research on this compound is still in the very beginning stage, J114 may be useful for further exploration of the exact modulatory mechanism of NLRP3 inflammasome.
4.2.2 Inhibition of NLRP3 Inflammasome Related Signaling Pathway
As previously mentioned, the priming and activation of the NLRP3 inflammasome are regulated by multiple signaling pathways, and a number of NLRP3 inflammasome inhibitors have been developed to target these regulators. For example, taraxasterol and parthenolide suppress the activation of NLRP3 inflammasome by blocking the activation of NF-κB (126, 127), and celastrol resolves the inflammatory response to RA through inhibition of the ROS/NF-κB/NLRP3 axis (128). In addition, β-arrestins are vital regulators of G protein-coupled receptors (GPCRs), and β-arrestin-2(βArr2) has anti-inflammatory effects in a variety of inflammation-related diseases. Current study demonstrated that βArr2 effectively alleviates joint inflammation by inhibiting the NF-κB/NLRP3 signaling pathway in CIA mice (129). The traditional disease-modifying anti-rheumatic drug hydroxychloroquine is widely recognized in RA treatment. Hydroxychloroquine (HCQ) inhibits Ca2+-activated K+Channels, resulting in an impaired NLRP3 inflammasome activation (130). The mammalian target of rapamycin (mTOR) which regulates cellular metabolism and plays a negative role in regulating autophagy, is a serine-threonine protein kinase and belongs to the phosphatidylinositol 3-kinase-related kinase (PIKK) family. As an mTOR inhibitor, rapamycin treats RA by inducing autophagy to inhibit NLRP3 inflammasome and inflammation (131).
Discussion
NLRP3 inflammasome-driven inflammation accompanies the pathogenesis of autoimmune diseases which includes rheumatoid arthritis and makes NLRP3 inflammasome an attractive drug target. Meanwhile, NLRP3-mediated immune responses are critical for host defense against bacteria, viruses, and fungi (132–134). Therefore, a balance between activators and inactivators of NLRP3 inflammasomes are required to maintain immune homeostasis. Compared with cytokine blockade, molecules directly targeting NLRP3 inflammasome are more advantageous (135, 136), but there are no clinically available therapeutic agents now. Given the important role of NLRP3 inflammasome in both innate and adaptive immunity, the development of NLRP3 inhibitory drugs should be handled with caution. Many inhibitors of NLRP3 inflammasome have been identified, and several small molecule compounds are in clinical trials. Further elucidation of the clinical efficacy and safety of these inhibitors is still needed.
Summary
Inflammasomes have become the focus of research in the field of inflammatory diseases. Increasing evidence suggests that the NLPR3 inflammasome plays a key role in the pathogenesis of rheumatic diseases. Excessive inhibition or activation leads to immune disorders that require precise regulation during NLPR3 inflammasome activation. Therefore, it is necessary to understand the mechanism of the NLPR3 inflammasome to explore promising therapeutic strategies for autoimmune diseases such as RA. Cytokines inhibitors remain limited due to infection risk, whereas NLRP3 inflammasome inhibitors show the best anti-inflammatory effects in animal models. The side effects of drugs may be unavoidable, while drug structure optimization is expected to break this dilemma and provide a practical and effective way for the treatment of RA.
Author Contributions
HY and NL reviewed the literature and wrote the first draft. HY, NL, and LD reviewed the literature and finalized the manuscript. HY, YL, and LD revised the manuscript. All authors have read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (81960296 and 81871286), JiangXi Provincial Natural Science Foundation of China (20192ACB21006), Interdisciplinary Innovation Team, Frontier Science Key Research Project of Jiangxi Provincial People’s Hospital (19-008), Long-term (Youth) Project for Leading Innovative Talents in Jiangxi Province (Lihua Duan), Jiangxi Provincial Clinical Research Center for Rheumatic and Immunologic Diseases (20192BCD42005), Jiangxi Province Medical Leading Discipline Construction Project (Rheumatology), and Provincial and municipal joint construction projects of medical disciplines in Jiangxi Province (Rheumatology).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Scott DL, Wolfe F, Huizinga TW. Rheumatoid Arthritis. Lancet (2010) 376:1094–108. doi: 10.1016/S0140-6736(10)60826-4
2. Rudan I, Sidhu S, Papana A, Meng SJ, Xin-Wei Y, Wang W, et al. Prevalence of Rheumatoid Arthritis in Low- and Middle-Income Countries: A Systematic Review and Analysis. J Glob Health (2015) 5:010409. doi: 10.7189/jogh.05.010409
3. Doran MF, Crowson CS, Pond GR, O'Fallon WM, Gabriel SE. Frequency of Infection in Patients With Rheumatoid Arthritis Compared With Controls: A Population-Based Study. Arthritis Rheum (2002) 46:2287–93. doi: 10.1002/art.10524
4. Atzeni F, Masala IF, di Franco M, Sarzi-Puttini P. Infections in Rheumatoid Arthritis. Curr Opin Rheumatol (2017) 29:323–30. doi: 10.1097/BOR.0000000000000389
5. Siebert S, Tsoukas A, Robertson J, McInnes I. Cytokines as Therapeutic Targets in Rheumatoid Arthritis and Other Inflammatory Diseases. Pharmacol Rev (2015) 67:280–309. doi: 10.1124/pr.114.009639
6. Alippe Y, Mbalaviele G. Omnipresence of Inflammasome Activities in Inflammatory Bone Diseases. Semin Immunopathol (2019) 41:607–18. doi: 10.1007/s00281-019-00753-4
7. Shin JI, Lee KH, Joo YH, Lee JM, Jeon J, Jung HJ, et al. Inflammasomes and Autoimmune and Rheumatic Diseases: A Comprehensive Review. J Autoimmun (2019) 103:102299. doi: 10.1016/j.jaut.2019.06.010
8. Broz P, Dixit VM. Inflammasomes: Mechanism of Assembly, Regulation and Signalling. Nat Rev Immunol (2016) 16:407–20. doi: 10.1038/nri.2016.58
9. Malik A, Kanneganti TD. Inflammasome Activation and Assembly at a Glance. J Cell Sci (2017) 130:3955–63. doi: 10.1242/jcs.207365
10. Sharma D, Kanneganti TD. The Cell Biology of Inflammasomes: Mechanisms of Inflammasome Activation and Regulation. J Cell Biol (2016) 213:617–29. doi: 10.1083/jcb.201602089
11. Mangan MSJ, Olhava EJ, Roush WR, Seidel HM, Glick GD, Latz E. Targeting the NLRP3 Inflammasome in Inflammatory Diseases. Nat Rev Drug Discov (2018) 17:588–606. doi: 10.1038/nrd.2018.97
12. Spel L, Martinon F. Inflammasomes Contributing to Inflammation in Arthritis. Immunol Rev (2020) 294:48–62. doi: 10.1111/imr.12839
13. Burdett H, Bentham AR, Williams SJ, Dodds PN, Anderson PA, Banfield MJ, et al. The Plant "Resistosome": Structural Insights Into Immune Signaling. Cell Host Microbe (2019) 26:193–201. doi: 10.1016/j.chom.2019.07.020
14. Wang J, Hu M, Wang J, Qi J, Han Z, Wang G, et al. Reconstitution and Structure of a Plant NLR Resistosome Conferring Immunity. Science (2019) 364:5868–70. doi: 10.1126/science.aav5870
15. Kahlenberg JM, Kang I. Advances in Disease Mechanisms and Translational Technologies: Clinicopathologic Significance of Inflammasome Activation in Autoimmune Diseases. Arthritis Rheumatol (2020) 72:386–95. doi: 10.1002/art.41127
16. Kayagaki N, Warming S, Lamkanfi M, Vande Walle L, Louie S, Dong J, et al. Non-Canonical Inflammasome Activation Targets Caspase-11. Nature (2011) 479:117–21. doi: 10.1038/nature10558
17. Yang J, Zhao Y, Shao F. Non-Canonical Activation of Inflammatory Caspases by Cytosolic LPS in Innate Immunity. Curr Opin Immunol (2015) 32:78–83. doi: 10.1016/j.coi.2015.01.007
18. Shi J, Zhao Y, Wang Y, Gao W, Ding J, Li P, et al. Inflammatory Caspases are Innate Immune Receptors for Intracellular LPS. Nature (2014) 514:187–92. doi: 10.1038/nature13683
19. Yi YS. Role of Inflammasomes in Inflammatory Autoimmune Rheumatic Diseases. Korean J Physiol Pharmacol (2018) 22:1–15. doi: 10.4196/kjpp.2018.22.1.1
20. Martinon F, Tschopp J. NLRs Join TLRs as Innate Sensors of Pathogens. Trends Immunol (2005) 26:447–54. doi: 10.1016/j.it.2005.06.004
21. Bauernfeind FG, Horvath G, Stutz A, Alnemri ES, MacDonald K, Speert D, et al. Cutting Edge: NF-kappaB Activating Pattern Recognition and Cytokine Receptors License NLRP3 Inflammasome Activation by Regulating NLRP3 Expression. J Immunol (2009) 183:787–91. doi: 10.4049/jimmunol.0901363
22. Franchi L, Eigenbrod T, Núñez G. Cutting Edge: TNF-Alpha Mediates Sensitization to ATP and Silica via the NLRP3 Inflammasome in the Absence of Microbial Stimulation. J Immunol (2009) 183:792–6. doi: 10.4049/jimmunol.0900173
23. Lu A, Magupalli VG, Ruan J, Yin Q, Atianand MK, Vos MR, et al. Unified Polymerization Mechanism for the Assembly of ASC-Dependent Inflammasomes. Cell (2014) 156:1193–206. doi: 10.1016/j.cell.2014.02.008
24. Latz E, Xiao TS, Stutz A. Activation and Regulation of the Inflammasomes. Nat Rev Immunol (2013) 13:397–411. doi: 10.1038/nri3452
25. Lee MS, Kwon H, Lee EY, Kim DJ, Park JH, Tesh VL, et al. Shiga Toxins Activate the NLRP3 Inflammasome Pathway To Promote Both Production of the Proinflammatory Cytokine Interleukin-1β and Apoptotic Cell Death. Infect Immun (2016) 84:172–86. doi: 10.1128/IAI.01095-15
26. Erdei J, Tóth A, Balogh E, Nyakundi BB, Bányai E, Ryffel B, et al. Induction of NLRP3 Inflammasome Activation by Heme in Human Endothelial Cells. Oxid Med Cell Longev (2018) 2018:4310816. doi: 10.1155/2018/4310816
27. Swanson KV, Deng M, Ting JP. The NLRP3 Inflammasome: Molecular Activation and Regulation to Therapeutics. Nat Rev Immunol (2019) 19:477–89. doi: 10.1038/s41577-019-0165-0
28. Fernandes-Alnemri T, Wu J, Yu JW, Datta P, Miller B, Jankowski W, et al. The Pyroptosome: A Supramolecular Assembly of ASC Dimers Mediating Inflammatory Cell Death via Caspase-1 Activation. Cell Death Differ (2007) 14:1590–604. doi: 10.1038/sj.cdd.4402194
29. Boucher D, Monteleone M, Coll RC, Chen KW, Ross CM, Teo JL, et al. Caspase-1 Self-Cleavage is an Intrinsic Mechanism to Terminate Inflammasome Activity. J Exp Med (2018) 215:827–40. doi: 10.1084/jem.20172222
30. Shi J, Zhao Y, Wang K, Shi X, Wang Y, Huang H, et al. Cleavage of GSDMD by Inflammatory Caspases Determines Pyroptotic Cell Death. Nature (2015) 526:660–5. doi: 10.1038/nature15514
31. He WT, Wan H, Hu L, Chen P, Wang X, Huang Z, et al. Gasdermin D is an Executor of Pyroptosis and Required for Interleukin-1β Secretion. Cell Res (2015) 25:1285–98. doi: 10.1038/cr.2015.139
32. Liu X, Zhang Z, Ruan J, Pan Y, Magupalli VG, Wu H, et al. Inflammasome-Activated Gasdermin D Causes Pyroptosis by Forming Membrane Pores. Nature (2016) 535:153–8. doi: 10.1038/nature18629
33. Li Z, Guo J, Bi L. Role of the NLRP3 Inflammasome in Autoimmune Diseases. BioMed Pharmacother (2020) 130:110542. doi: 10.1016/j.biopha.2020.110542
34. Zhang Y, Yang W, Li W, Zhao Y. NLRP3 Inflammasome: Checkpoint Connecting Innate and Adaptive Immunity in Autoimmune Diseases. Front Immunol (2021) 12:732933. doi: 10.3389/fimmu.2021.732933
35. He Y, Zeng MY, Yang D, Motro B, Núñez G. NEK7 is an Essential Mediator of NLRP3 Activation Downstream of Potassium Efflux. Nature (2016) 530:354–7. doi: 10.1038/nature16959
36. Shi H, Wang Y, Li X, Zhan X, Tang M, Fina M, et al. NLRP3 Activation and Mitosis are Mutually Exclusive Events Coordinated by NEK7, A New Inflammasome Component. Nat Immunol (2016) 17:250–8. doi: 10.1038/ni.3333
37. Schmid-Burgk JL, Chauhan D, Schmidt T, Ebert TS, Reinhardt J, Endl E, et al. (Clustered Regularly Interspaced Short Palindromic Repeats) Screen Identifies NEK7 as an Essential Component of NLRP3 Inflammasome Activation. J Biol Chem (2016) 291:103–9. doi: 10.1074/jbc.C115.700492
38. Samir P, Kesavardhana S, Patmore DM, Gingras S, Malireddi RKS, Karki R, et al. DDX3X Acts as a Live-or-Die Checkpoint in Stressed Cells by Regulating NLRP3 Inflammasome. Nature (2019) 573:590–4. doi: 10.1038/s41586-019-1551-2
39. Cao Z, Wang Y, Long Z, He G. Interaction Between Autophagy and the NLRP3 Inflammasome. Acta Biochim Biophys Sin (Shanghai) (2019) 51:1087–95. doi: 10.1093/abbs/gmz098
40. Shi CS, Shenderov K, Huang NN, Kabat J, Abu-Asab M, Fitzgerald KA, et al. Activation of Autophagy by Inflammatory Signals Limits IL-1β Production by Targeting Ubiquitinated Inflammasomes for Destruction. Nat Immunol (2012) 13:255–63. doi: 10.1038/ni.2215
41. Pandey A, Shen C, Feng S, Man SM. Cell Biology of Inflammasome Activation. Trends Cell Biol (2021) 31:924–39. doi: 10.1016/j.tcb.2021.06.010
42. Paik S, Kim JK, Silwal P, Sasakawa C, Jo EK. An Update on the Regulatory Mechanisms of NLRP3 Inflammasome Activation. Cell Mol Immunol (2021) 18:1141–60. doi: 10.1038/s41423-021-00670-3
43. Moretti J, Blander JM. Increasing Complexity of NLRP3 Inflammasome Regulation. J Leukoc Biol (2021) 109:561–71. doi: 10.1002/JLB.3MR0520-104RR
44. Chen J, Chen ZJ. PtdIns4P on Dispersed Trans-Golgi Network Mediates NLRP3 Inflammasome Activation. Nature (2018) 564:71–6. doi: 10.1038/s41586-018-0761-3
45. Andreeva L, David L, Rawson S, Shen C, Pasricha T, Pelegrin P, et al. NLRP3 Cages Revealed by Full-Length Mouse NLRP3 Structure Control Pathway Activation. Cell (2021) 184:6299–312.e22. doi: 10.1016/j.cell.2021.11.011
46. Pourcet B, Duez H. Circadian Control of Inflammasome Pathways: Implications for Circadian Medicine. Front Immunol (2020) 11:1630. doi: 10.3389/fimmu.2020.01630
47. Spadaro O, Youm Y, Shchukina I, Ryu S, Sidorov S, Ravussin A, et al. Caloric Restriction in Humans Reveals Immunometabolic Regulators of Health Span. Science (2022) 375:671–7. doi: 10.1126/science.abg7292
48. Lin KM, Hu W, Troutman TD, Jennings M, Brewer T, Li X, et al. IRAK-1 Bypasses Priming and Directly Links TLRs to Rapid NLRP3 Inflammasome Activation. Proc Natl Acad Sci U.S.A. (2014) 111:775–80. doi: 10.1073/pnas.1320294111
49. Gurung P, Anand PK, Malireddi RK, Vande Walle L, Van Opdenbosch N, Dillon CP, et al. FADD and Caspase-8 Mediate Priming and Activation of the Canonical and Noncanonical Nlrp3 Inflammasomes. J Immunol (2014) 192:1835–46. doi: 10.4049/jimmunol.1302839
50. Wu ZM, Luo J, Shi XD, Zhang SX, Zhu XB, Guo J. Icariin Alleviates Rheumatoid Arthritis via Regulating miR-223-3p/NLRP3 Signalling Axis. Autoimmunity (2020) 53:450–8. doi: 10.1080/08916934.2020.1836488
51. Chen S, Luo Z, Chen X. Hsa_circ_0044235 Regulates the Pyroptosis of Rheumatoid Arthritis via MiR-135b-5p-SIRT1 Axis. Cell Cycle (2021) 20:1107–21. doi: 10.1080/15384101.2021.1916272
52. Py BF, Kim MS, Vakifahmetoglu-Norberg H, Yuan J. Deubiquitination of NLRP3 by BRCC3 Critically Regulates Inflammasome Activity. Mol Cell (2013) 49:331–8. doi: 10.1016/j.molcel.2012.11.009
53. Rao Z, Chen X, Wu J, Xiao M, Zhang J, Wang B, et al. Vitamin D Receptor Inhibits NLRP3 Activation by Impeding Its BRCC3-Mediated Deubiquitination. Front Immunol (2019) 10:2783. doi: 10.3389/fimmu.2019.02783
54. Song H, Liu B, Huai W, Yu Z, Wang W, Zhao J, et al. The E3 Ubiquitin Ligase TRIM31 Attenuates NLRP3 Inflammasome Activation by Promoting Proteasomal Degradation of NLRP3. Nat Commun (2016) 7:13727. doi: 10.1038/ncomms13727
55. Yan Y, Jiang W, Liu L, Wang X, Ding C, Tian Z, et al. Dopamine Controls Systemic Inflammation Through Inhibition of NLRP3 Inflammasome. Cell (2015) 160:62–73. doi: 10.1016/j.cell.2014.11.047
56. Humphries F, Bergin R, Jackson R, Delagic N, Wang B, Yang S, et al. The E3 Ubiquitin Ligase Pellino2 Mediates Priming of the NLRP3 Inflammasome. Nat Commun (2018) 9:1560. doi: 10.1038/s41467-018-03669-z
57. Hughes MM, O'Neill LAJ. Metabolic Regulation of NLRP3. Immunol Rev (2018) 281:88–98. doi: 10.1111/imr.12608
58. Mortimer L, Moreau F, MacDonald JA, Chadee K. NLRP3 Inflammasome Inhibition is Disrupted in a Group of Auto-Inflammatory Disease CAPS Mutations. Nat Immunol (2016) 17:1176–86. doi: 10.1038/ni.3538
59. Zhang Z, Meszaros G, He WT, Xu Y, de Fatima Magliarelli H, Mailly L, et al. Protein Kinase D at the Golgi Controls NLRP3 Inflammasome Activation. J Exp Med (2017) 214:2671–93. doi: 10.1084/jem.20162040
60. Spalinger MR, Kasper S, Gottier C, Lang S, Atrott K, Vavricka SR, et al. NLRP3 Tyrosine Phosphorylation is Controlled by Protein Tyrosine Phosphatase PTPN22. J Clin Invest (2016) 126:1783–800. doi: 10.1172/JCI83669
61. Stutz A, Kolbe CC, Stahl R, Horvath GL, Franklin BS, van Ray O, et al. NLRP3 Inflammasome Assembly is Regulated by Phosphorylation of the Pyrin Domain. J Exp Med (2017) 214:1725–36. doi: 10.1084/jem.20160933
62. Tezcan G, Martynova EV, Gilazieva ZE, McIntyre A, Rizvanov AA, Khaiboullina SF. MicroRNA Post-Transcriptional Regulation of the NLRP3 Inflammasome in Immunopathologies. Front Pharmacol (2019) 10:451. doi: 10.3389/fphar.2019.00451
63. Zhu H, Jian Z, Zhong Y, Ye Y, Zhang Y, Hu X, et al. Janus Kinase Inhibition Ameliorates Ischemic Stroke Injury and Neuroinflammation Through Reducing NLRP3 Inflammasome Activation via JAK2/STAT3 Pathway Inhibition. Front Immunol (2021) 12:714943. doi: 10.3389/fimmu.2021.714943
64. Dinarello CA. Immunological and Inflammatory Functions of the Interleukin-1 Family. Annu Rev Immunol (2009) 27:519–50. doi: 10.1146/annurev.immunol.021908.132612
65. Waisman A, Lukas D, Clausen BE, Yogev N. Dendritic Cells as Gatekeepers of Tolerance. Semin Immunopathol (2017) 39:153–63. doi: 10.1007/s00281-016-0583-z
66. Xue G, Jin G, Fang J, Lu Y. IL-4 Together with IL-1b Induces Antitumor Th9 Cell Differentiation in the Absence of TGF-b Signaling. Nat Commun (2019) 1376.
67. Acosta-Rodriguez EV, Napolitani G, Lanzavecchia A, Sallusto F. Interleukins 1beta and 6 but not Transforming Growth Factor-beta are Essential for the Differentiation of Interleukin 17-Producing Human T Helper Cells. Nat Immunol (2019) 8:942–9.
68. Lusty E, Poznanski SM, Kwofie K, Mandur TS, Lee DA, Richards CD, et al. IL-18/IL-15/IL-12 Synergy Induces Elevated and Prolonged IFN-γ Production by Ex Vivo Expanded NK Cells Which is Not Due to Enhanced STAT4 Activation. Mol Immunol (2017) 88:138–47. doi: 10.1016/j.molimm.2017.06.025
69. Harrison OJ, Srinivasan N, Pott J, Schiering C, Krausgruber T, Ilott NE, et al. Epithelial-Derived IL-18 Regulates Th17 Cell Differentiation and Foxp3+ Treg Cell Function in the Intestine. Mucosal Immunol (2015) 8:1226–36. doi: 10.1038/mi.2015.13
70. Shen HH, Yang YX, Meng X, Luo XY, Li XM, Shuai ZW, et al. NLRP3: A Promising Therapeutic Target for Autoimmune Diseases. Autoimmun Rev (2018) 17:694–702. doi: 10.1016/j.autrev.2018.01.020
71. Ruscitti P, Cipriani P, Carubbi F, Liakouli V, Zazzeroni F, Di Benedetto P, et al. The Role of IL-1β in the Bone Loss During Rheumatic Diseases. Mediators Inflammation (2015) 2015:782382. doi: 10.1155/2015/782382
72. Nakamura I, Jimi E. Regulation of Osteoclast Differentiation and Function by Interleukin-1. Vitam Horm (2006) 74:357–70. doi: 10.1016/S0083-6729(06)74015-8
73. Strand V, Kavanaugh AF. The Role of Interleukin-1 in Bone Resorption in Rheumatoid Arthritis. Rheumatol (Oxford) (2004) 43 Suppl 3:iii10–6. doi: 10.1093/rheumatology/keh202
74. Redlich K, Smolen JS. Inflammatory Bone Loss: Pathogenesis and Therapeutic Intervention. Nat Rev Drug Discovery (2012) 11:234–50. doi: 10.1038/nrd3669
75. Zhang W, Cong XL, Qin YH, He ZW, He DY, Dai SM. IL-18 Upregulates the Production of Key Regulators of Osteoclastogenesis From Fibroblast-Like Synoviocytes in Rheumatoid Arthritis. Inflammation (2013) 36:103–9. doi: 10.1007/s10753-012-9524-8
76. Fahey E, Doyle SL. IL-1 Family Cytokine Regulation of Vascular Permeability and Angiogenesis. Front Immunol (2019) 10:1426. doi: 10.3389/fimmu.2019.01426
77. Dong X, Zheng Z, Lin P, Fu X, Li F, Jiang J, et al. ACPAs Promote IL-1β Production in Rheumatoid Arthritis by Activating the NLRP3 Inflammasome. Cell Mol Immunol (2020) 17:261–71. doi: 10.1038/s41423-019-0201-9
78. Unterberger S, Davies KA, Rambhatla SB, Sacre S. Contribution of Toll-Like Receptors and the NLRP3 Inflammasome in Rheumatoid Arthritis Pathophysiology. Immunotargets Ther (2021) 10:285–98. doi: 10.2147/ITT.S288547
79. Guo C, Fu R, Wang S, Huang Y, Li X, Zhou M, et al. NLRP3 Inflammasome Activation Contributes to the Pathogenesis of Rheumatoid Arthritis. Clin Exp Immunol (2018) 194:231–43. doi: 10.1111/cei.13167
80. Choulaki C, Papadaki G, Repa A, Kampouraki E, Kambas K, Ritis K, et al. Enhanced Activity of NLRP3 Inflammasome in Peripheral Blood Cells of Patients With Active Rheumatoid Arthritis. Arthritis Res Ther (2015) 17:257. doi: 10.1186/s13075-015-0775-2
81. Ruscitti P, Cipriani P, Di Benedetto P, Liakouli V, Berardicurti O, Carubbi F, et al. Monocytes From Patients With Rheumatoid Arthritis and Type 2 Diabetes Mellitus Display an Increased Production of Interleukin (IL)-1β via the Nucleotide-Binding Domain and Leucine-Rich Repeat Containing Family Pyrin 3(NLRP3)-Inflammasome Activation: A Possible Implication for Therapeutic Decision in These Patients. Clin Exp Immunol (2015) 182:35–44. doi: 10.1111/cei.12667
82. Cheng L, Liang X, Qian L, Luo C, Li D. NLRP3 Gene Polymorphisms and Expression in Rheumatoid Arthritis. Exp Ther Med (2021) 22:1110. doi: 10.3892/etm.2021.10544
83. Mathews RJ, Robinson JI, Battellino M, Wong C, Taylor JC, Eyre S, et al. Evidence of NLRP3-Inflammasome Activation in Rheumatoid Arthritis (RA); Genetic Variants Within the NLRP3-Inflammasome Complex in Relation to Susceptibility to RA and Response to Anti-TNF Treatment. Ann Rheum Dis (2014) 73:1202–10. doi: 10.1136/annrheumdis-2013-203276
84. Sode J, Vogel U, Bank S, Andersen PS, Thomsen MK, Hetland ML, et al. Anti-TNF Treatment Response in Rheumatoid Arthritis Patients is Associated With Genetic Variation in the NLRP3-Inflammasome. PloS One (2014) 9:e100361. doi: 10.1371/journal.pone.0100361
85. Jenko B, Praprotnik S, Tomšic M, Dolžan V. NLRP3 and CARD8 Polymorphisms Influence Higher Disease Activity in Rheumatoid Arthritis. J Med Biochem (2016) 35:319–23. doi: 10.1515/jomb-2016-0008
86. Klareskog L, Padyukov L, Lorentzen J, Alfredsson L. Mechanisms of Disease: Genetic Susceptibility and Environmental Triggers in the Development of Rheumatoid Arthritis. Nat Clin Pract Rheumatol (2006) 2:425–33. doi: 10.1038/ncprheum0249
87. Vande Walle L, Van Opdenbosch N, Jacques P, Fossoul A, Verheugen E, Vogel P, et al. Negative Regulation of the NLRP3 Inflammasome by A20 Protects Against Arthritis. Nature (2014) 512:69–73. doi: 10.1038/nature13322
88. Sardar S, Andersson Å. Old and New Therapeutics for Rheumatoid Arthritis: In Vivo Models and Drug Development. Immunopharmacol Immunotoxicol (2016) 38:2–13. doi: 10.3109/08923973.2015.1125917
89. Zhang Y, Zheng Y, Li H. NLRP3 Inflammasome Plays an Important Role in the Pathogenesis of Collagen-Induced Arthritis. Mediators Inflammation (2016) 2016:9656270. doi: 10.1155/2016/9656270
90. Greenhill CJ, Jones GW, Nowell MA, Newton Z, Harvey AK, Moideen AN, et al. Interleukin-10 Regulates the Inflammasome-Driven Augmentation of Inflammatory Arthritis and Joint Destruction. Arthritis Res Ther (2014) 16:419. doi: 10.1186/s13075-014-0419-y
91. Liu P, Wang J, Wen W, Pan T, Chen H, Fu Y, et al. Cinnamaldehyde Suppresses NLRP3 Derived IL-1β via Activating Succinate/HIF-1 in Rheumatoid Arthritis Rats. Int Immunopharmacol (2020) 84:106570. doi: 10.1016/j.intimp.2020.106570
92. Jin S, Sun S, Ling H, Ma J, Zhang X, Xie Z, et al. Protectin DX Restores Treg/T(h)17 Cell Balance in Rheumatoid Arthritis by Inhibiting NLRP3Inflammasome via miR-20a. Cell Death Dis (2021) 12:280.
93. Yang X, Zhan N, Jin Y, Ling H, Xiao C, Xie Z, et al. Tofacitinib Restores the Balance of γδtreg/γδt17 Cells in Rheumatoid Arthritis by Inhibiting the NLRP3 Inflammasome. Theranostics (2021) 11:1446–57. doi: 10.7150/thno.47860
94. Jäger E, Murthy S, Schmidt C, Hahn M, Strobel S, Peters A, et al. Calcium-Sensing Receptor-Mediated NLRP3 Inflammasome Response to Calciprotein Particles Drives Inflammation in Rheumatoid Arthritis. Nat Commun (2020) 11:4243. doi: 10.1038/s41467-020-17749-6
95. Chen KW, Groß CJ, Sotomayor FV, Stacey KJ, Tschopp J, Sweet MJ, et al. The Neutrophil NLRC4 Inflammasome Selectively Promotes IL-1β Maturation Without Pyroptosis During Acute Salmonella Challenge. Cell Rep (2014) 8:570–82. doi: 10.1016/j.celrep.2014.06.028
96. Gaidt MM, Ebert TS, Chauhan D, Schmidt T, Schmid-Burgk JL, Rapino F, et al. Human Monocytes Engage an Alternative Inflammasome Pathway. Immunity (2016) 44:833–46. doi: 10.1016/j.immuni.2016.01.012
97. Bakele M, Joos M, Burdi S, Allgaier N, Pöschel S, Fehrenbacher B, et al. Localization and Functionality of the Inflammasome in Neutrophils. J Biol Chem (2014) 289:5320–9. doi: 10.1074/jbc.M113.505636
98. Yang Z, Cao J, Yu C, Yang Q, Zhang Y, Han L. Caspase-1 Mediated Interleukin-18 Activation in Neutrophils Promotes the Activity of Rheumatoid Arthritis in a NLRP3 Inflammasome Independent Manner. Joint Bone Spine (2016) 83:282–9. doi: 10.1016/j.jbspin.2015.07.006
99. Wang T, Zhu CL, Wang S, Mo LW, Yang GD, Hu J, et al. Role of NLRP3 and NLRP1 Inflammasomes Signaling Pathways in Pathogenesis of Rheumatoid Arthritis. Asian Pac J Trop Med (2014) 7:827–31. doi: 10.1016/S1995-7645(14)60145-0
100. Tate MD, Ong JDH, Dowling JK, McAuley JL, Robertson AB, Latz E, et al. Reassessing the Role of the NLRP3 Inflammasome During Pathogenic Influenza A Virus Infection via Temporal Inhibition. Sci Rep (2016) 6:27912. doi: 10.1038/srep27912
101. Brydges SD, Broderick L, McGeough MD, Pena CA, Mueller JL, Hoffman HM. Divergence of IL-1, IL-18, and Cell Death in NLRP3 Inflammasomopathies. J Clin Invest (2013) 123:4695–705. doi: 10.1172/JCI71543
102. Liu H, Xu R, Kong Q, Liu J, Yu Z, Zhao C. Downregulated NLRP3 and NLRP1 Inflammasomes Signaling Pathways in the Development and Progression of Type 1 Diabetes Mellitus. BioMed Pharmacother (2017) 94:619–26. doi: 10.1016/j.biopha.2017.07.102
103. Frissen M, Liao L, Schneider KM, Djudjaj S, Haybaeck J, Wree A, et al. Bidirectional Role of NLRP3 During Acute and Chronic Cholestatic Liver Injury. Hepatology (2021) 73:1836–54. doi: 10.1002/hep.31494
104. Lech M, Lorenz G, Kulkarni OP, Grosser MO, Stigrot N, Darisipudi MN, et al. NLRP3 and ASC Suppress Lupus-Like Autoimmunity by Driving the Immunosuppressive Effects of TGF-β Receptor Signalling. Ann Rheum Dis (2015) 74:2224–35. doi: 10.1136/annrheumdis-2014-205496
105. Zaki MH, Lamkanfi M, Kanneganti TD. The Nlrp3 Inflammasome: Contributions to Intestinal Homeostasis. Trends Immunol (2011) 32:171–9. doi: 10.1016/j.it.2011.02.002
106. Pellegrini C, Antonioli L, Calderone V, Colucci R, Fornai M, Blandizzi C. Microbiota-Gut-Brain Axis in Health and Disease: Is NLRP3 Inflammasome at the Crossroads of Microbiota-Gut-Brain Communications? Prog Neurobiol (2020) 191:101806. doi: 10.1016/j.pneurobio.2020.101806
107. Schwaid AG, Spencer KB. Strategies for Targeting the NLRP3 Inflammasome in the Clinical and Preclinical Space. J Med Chem (2021) 64:101–22. doi: 10.1021/acs.jmedchem.0c01307
108. Mertens M, Singh JA. Anakinra for Rheumatoid Arthritis: A Systematic Review. J Rheumatol (2009) 36:1118–25. doi: 10.3899/jrheum.090074
109. Ramírez J, Cañete JD. Anakinra for the Treatment of Rheumatoid Arthritis: A Safety Evaluation. Expert Opin Drug Saf (2018) 17:727–32. doi: 10.1080/14740338.2018.1486819
110. Rudolphi K, Gerwin N, Verzijl N, van der Kraan P, van den Berg W. Pralnacasan, an Inhibitor of Interleukin-1beta Converting Enzyme, Reduces Joint Damage in Two Murine Models of Osteoarthritis. Osteoarthritis Cartilage (2003) 11:738–46. doi: 10.1016/S1063-4584(03)00153-5
111. Fischer U, Schulze-Osthoff K. Apoptosis-Based Therapies and Drug Targets. Cell Death Differ (2005) 12 Suppl 1:942–61. doi: 10.1038/sj.cdd.4401556
112. Wannamaker W, Davies R, Namchuk M, Pollard J, Ford P, Ku G, et al. (S)-1-((S)-2-{[1-(4-Amino-3-Chloro-Phenyl)-Methanoyl]-Amino}-3,3-Dimethyl-Butanoyl)-Pyrrolidine-2-Carboxylic Acid ((2R,3S)-2-Ethoxy-5-Oxo-Tetrahydro-Furan-3-Yl)-Amide (VX-765), an Orally Available Selective Interleukin (IL)-Converting Enzyme/Caspase-1 Inhibitor, Exhibits Potent Anti-Inflammatory Activities by Inhibiting the Release of IL-1beta and IL-18. J Pharmacol Exp Ther (2007) 321:509–16. doi: 10.1124/jpet.106.111344
113. Maroso M, Balosso S, Ravizza T, Liu J, Bianchi ME, Vezzani A. Interleukin-1 Type 1 Receptor/Toll-Like Receptor Signalling in Epilepsy: The Importance of IL-1beta and High-Mobility Group Box 1. J Intern Med (2011) 270:319–26. doi: 10.1111/j.1365-2796.2011.02431.x
114. Smith CE, Soti S, Jones TA, Nakagawa A, Xue D, Yin H. Non-Steroidal Anti-Inflammatory Drugs Are Caspase Inhibitors. Cell Chem Biol (2017) 24:281–92. doi: 10.1016/j.chembiol.2017.02.003
115. Coll RC, Robertson AA, Chae JJ, Higgins SC, Muñoz-Planillo R, Inserra MC, et al. A Small-Molecule Inhibitor of the NLRP3 Inflammasome for the Treatment of Inflammatory Diseases. Nat Med (2015) 21:248–55. doi: 10.1038/nm.3806
116. Coll RC, Hill JR, Day CJ, Zamoshnikova A, Boucher D, Massey NL, et al. MCC950 Directly Targets the NLRP3 ATP-Hydrolysis Motif for Inflammasome Inhibition. Nat Chem Biol (2019) 15:556–9. doi: 10.1038/s41589-019-0277-7
117. Tapia-Abellán A, Angosto-Bazarra D, Martínez-Banaclocha H, de Torre-Minguela C, Cerón-Carrasco JP, Pérez-Sánchez H, et al. MCC950 Closes the Active Conformation of NLRP3 to an Inactive State. Nat Chem Biol (2019) 15:560–4. doi: 10.1038/s41589-019-0278-6
118. Huang Y, Jiang H, Chen Y, Wang X, Yang Y, Tao J, et al. Tranilast Directly Targets NLRP3 to Treat Inflammasome-Driven Diseases. EMBO Mol Med 10 (2018) 10(4):e8689. doi: 10.15252/emmm.201708689
119. Shiota N, Kovanen PT, Eklund KK, Shibata N, Shimoura K, Niibayashi T, et al. The Anti-Allergic Compound Tranilast Attenuates Inflammation and Inhibits Bone Destruction in Collagen-Induced Arthritis in Mice. Br J Pharmacol (2010) 159:626–35. doi: 10.1111/j.1476-5381.2009.00561.x
120. Nagate T, Tamura T, Sato F, Kuroda J, Nakayama J, Shibata N. Tranilast Suppresses the Disease Development of the Adjuvant- and Streptococcal Cell Wall-Induced Arthritis in Rats. J Pharmacol Sci (2007) 105:48–56. doi: 10.1254/jphs.FP0070534
121. Chen Y, He H, Lin B, Chen Y, Deng X, Jiang W, et al. RRx-001 Ameliorates Inflammatory Diseases by Acting as a Potent Covalent NLRP3 Inhibitor. Cell Mol Immunol (2021) 18:1425–36. doi: 10.1038/s41423-021-00683-y
122. Lin H, Yang M, Li C, Lin B, Deng X, He H, et al. An RRx-001 Analogue With Potent Anti-NLRP3 Inflammasome Activity But Without High-Energy Nitro Functional Groups. Front Pharmacol (2022) 13:822833. doi: 10.3389/fphar.2022.822833
123. Li Q, Feng H, Wang H, Wang Y, Mou W, Xu G, et al. Licochalcone B Specifically Inhibits the NLRP3 Inflammasome by Disrupting NEK7-NLRP3 Interaction. EMBO Rep (2022) 23:e53499. doi: 10.15252/embr.202153499
124. Tenshin H, Teramachi J, Ashtar M, Hiasa M, Inoue Y, Oda A, et al. TGF-β-Activated Kinase-1 Inhibitor LL-Z1640-2 Reduces Joint Inflammation and Bone Destruction in Mouse Models of Rheumatoid Arthritis by Inhibiting NLRP3 Inflammasome, TACE, TNF-α and RANKL Expression. Clin Transl Immunol (2022) 11:e1371. doi: 10.1002/cti2.1371
125. Jiao Y, Nan J, Mu B, Zhang Y, Zhou N, Yang S, et al. Discovery of a Novel and Potent Inhibitor With Differential Species-Specific Effects Against NLRP3 and AIM2 Inflammasome-Dependent Pyroptosis. Eur J Med Chem (2022) 232:114194. doi: 10.1016/j.ejmech.2022.114194
126. Chen J, Wu W, Zhang M, Chen C. Taraxasterol Suppresses Inflammation in IL-1b-Induced Rheumatoid Arthritis Fibroblast-like Synoviocytes and Rheumatoid Arthritis Progression in Mice.. Int Immunopharmacol (2019) 70:274–283.
127. Li N, Wang Y, Wang X, Sun N, Gong YH. Pathway Network of Pyroptosis and its Potential Inhibitors in Acute Kidney Injury. Pharmacol Res (2022) 175:106033.
128. Jing M, Yang J, Zhang L, Liu J, Xu S, Wang M, et al. Celastrol Inhibits Rheumatoid Arthritis Through the ROS-NF-κb-NLRP3 Inflammasome Axis. Int Immunopharmacol (2021) 98:107879. doi: 10.1016/j.intimp.2021.107879
129. Cao F, Huang C, Cheng J, He Z. β-Arrestin-2 Alleviates Rheumatoid Arthritis Injury by Suppressing NLRP3 Inflammasome Activation and NF- κb Pathway in Macrophages. Bioengineered (2022) 13:38–47. doi: 10.1080/21655979.2021.2003678
130. Eugenia Schroeder M, Russo S, Costa C, Hori J, Tiscornia I, Bollati-Fogolín M, et al. Pro-Inflammatory Ca(++)-Activated K(+) Channels are Inhibited by Hydroxychloroquine. Sci Rep (2017) 7:1892. doi: 10.1038/s41598-017-01836-8
131. Chen Y, Meng J, Xu Q, Long T, Bi F, Chang C, et al. Rapamycin Improves the Neuroprotection Effect of Inhibition of NLRP3 Inflammasome Activation After TBI. Brain Res (2019) 1710:163–72. doi: 10.1016/j.brainres.2019.01.005
132. Niu J, Wu S, Chen M, Xu K, Guo Q, Lu A, et al. Hyperactivation of the NLRP3 Inflammasome Protects Mice Against Influenza A Virus Infection via IL-1β Mediated Neutrophil Recruitment. Cytokine (2019) 120:115–24. doi: 10.1016/j.cyto.2019.04.019
133. Witzenrath M, Pache F, Lorenz D, Koppe U, Gutbier B, Tabeling C, et al. The NLRP3 Inflammasome is Differentially Activated by Pneumolysin Variants and Contributes to Host Defense in Pneumococcal Pneumonia. J Immunol (2011) 187:434–40. doi: 10.4049/jimmunol.1003143
134. Hise AG, Tomalka J, Ganesan S, Patel K, Hall BA, Brown GD, et al. An Essential Role for the NLRP3 Inflammasome in Host Defense Against the Human Fungal Pathogen Candida Albicans. Cell Host Microbe (2009) 5:487–97. doi: 10.1016/j.chom.2009.05.002
135. Liu D, Zeng X, Li X, Cui C, Hou R, Guo Z, et al. Advances in the Molecular Mechanisms of NLRP3 Inflammasome Activators and Inactivators. Biochem Pharmacol (2020) 175:113863. doi: 10.1016/j.bcp.2020.113863
Keywords: inflammasome, NOD-like receptor protein 3 (NLRP3), rheumatoid arthritis, IL-1β, inflammation
Citation: Yin H, Liu N, Sigdel KR and Duan L (2022) Role of NLRP3 Inflammasome in Rheumatoid Arthritis. Front. Immunol. 13:931690. doi: 10.3389/fimmu.2022.931690
Received: 29 April 2022; Accepted: 30 May 2022;
Published: 27 June 2022.
Edited by:
Zhu Chen, University of Science and Technology of China, ChinaReviewed by:
Li Guoqing, Affiliated Hospital of Yangzhou University, ChinaYanying Liu, Peking University People’s Hospital, China
Copyright © 2022 Yin, Liu, Sigdel and Duan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lihua Duan, bGgtZHVhbkAxNjMuY29t
†These authors have contributed equally to this work
 Hui Yin
Hui Yin Na Liu
Na Liu Keshav Raj Sigdel3
Keshav Raj Sigdel3 Lihua Duan
Lihua Duan