- 1Institute of Human Virology, University of Maryland School of Medicine, Baltimore, MD, United States
- 2Cell Biology Lab, Division of Virology, Pathogenesis and Cancer, Institute of Human Virology, University of Maryland School of Medicine, Baltimore, MD, United States
The report is not a review or a summary. In a manner, it is a perspective but an unusual one. It looks back to the years my colleagues and I (RG) began preparing for human retroviruses (beginning in 1970), how they evolved, and attempts to bring to light or simply to emphasize many exceptional characteristics of a retrovirus known as HTLV-1 and some fortuitous coincidences, with emphasis on the needs of the field. These events cover over one half a century. We have had many reviews on HTLV-1 disease, epidemiology, and basic aspects of its replication, genome, gene functions, structure, and pathogenesis, though continued updates are needed. However, some of its truly exceptional features have not been highlighted, or at least not in a comprehensive manner. This article attempts to do so.
Lack of Adequate Attention
The first unusual feature mentioned is not exactly science-based, but it has been a recurrent one. The first submitted encompassing major manuscript describing this cancer virus (to be known as HTLV-1 later), the first known human leukemia virus, and the first human retrovirus was immediately rejected by the Journal of Virology with hostile comments from the editor that more or less concluded that everyone knows there are no human retroviruses and such reports, even such work, must stop.
Thankfully, there was the U.S. Proceedings of the National Academies of Science, which accepted the first few papers (1, 2), as did Nature (3). Not the least of these was the timing. The 1950s–1960s were years of acceptance of the possibility and even probability of finding human retroviruses. However, by the 1970s, there was a decline in interest in serious infectious diseases even to the point of the minimization of departments of microbiology and promotion of investment of funding to non-infectious “degenerative diseases”. Some of the reasons for a particular bias against human retroviruses are summarized in Table 1. Not included on the list was the reaction against claims made for detecting human retroviruses in many human cancers purely by a biochemical approach. Many publications appeared from a leading virology lab in NY on this subject (4), but were not substantiated. However, my colleagues and I (RG) soon showed that these were false positives, and their detection of a “retrovirus reverse transcriptase” was, in fact, DNA polymerase gamma, the mitochondrial DNA polymerase (5, 6).
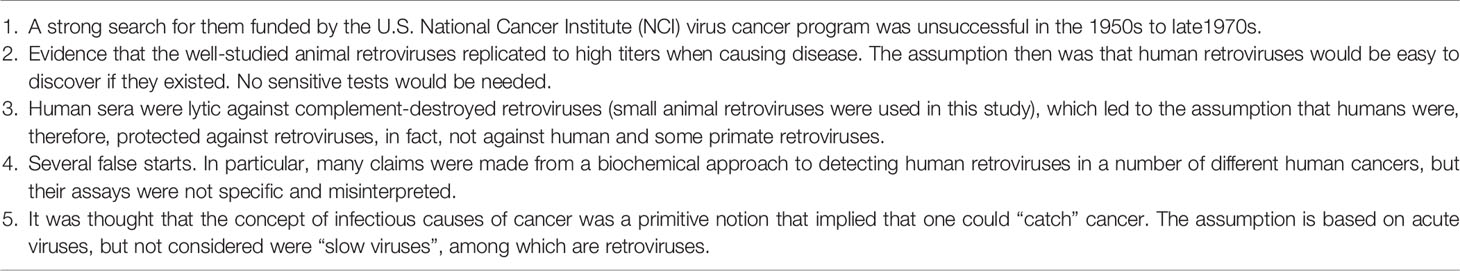
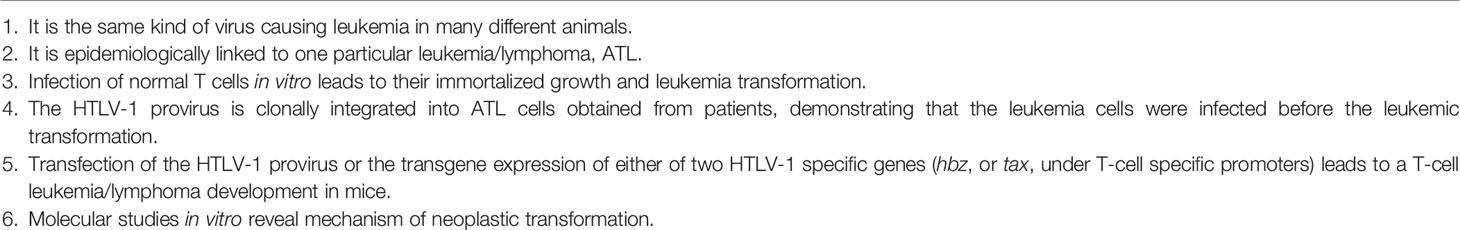
Table 1 Some considerations why resistance and bias against even the possibility of human retroviruses were prevalent in the 1970s.
In the 1970s, there were also very strong biases against any role for any infectious agents in any human cancer. Of course, these biases came tumbling down by the 1980s, as human retroviruses were discovered, shown to cause human diseases, and overall, along with other human tumor viruses, a role for viruses in human cancer was estimated to be about 20%. Soon after we discovered the second human retrovirus, HTLV-2 (7, 8), the third human retrovirus (9–13) was now on “top” of us and causing, oddly enough, our first pandemic in some decades, AIDS (14, 15), a disease, if left untreated, would have killed almost all within a few years.
Though HIV has long held a prominent position (by necessity), attention to HTLV-1 quickly faded. This includes both knowledge about it and research support for it. This is not easy to understand. Though HTLV-1 is not widespread in the United States, most of Europe, China, and India, which form the largest centers for publicity and most of the world science support, it is very prominent in select places such as Japan; in Native Australians; in parts of Indonesia, Romania, and Iran; in several countries in South America but especially Peru and Brazil; in parts of equatorial Africa and migrants originating from Africa to Europe; in the United States; and especially in the islands of the Caribbean (16). The oddity of this distribution is itself fascinating but may be explained by the poor transmissibility of HTLV-1 and its tendency to remain in families and certain populations, making the virus a useful aid in historical demography (17, 18).
Discoveries of Human Retroviruses
One of us (RG) decided on two simultaneous efforts in a search for human retroviruses. One was to develop a sure surrogate marker for a retrovirus far more sensitive than electron microscopy because the titer of any putative retrovirus, if present, must be very low because of difficulty in finding one, a situation very different from the well-studied and well-known animal retroviruses that replicated to high levels. At the same time, we wanted this surrogate assay to allow frequent sampling of cultures because the virus may be expressed only in a “pulse”. Both were true, and our selection proved worthy. Indeed, very recent findings suggest that the plus-strand of the HTLV-1 provirus including tax remains transcriptionally silent, and only intermittently as bursts by cellular stress such as hypoxia and glycolysis (19–23). In 1970, reverse transcriptase (RT), the soon to be well-known DNA polymerase of retroviruses, was independently discovered by Howard Temin and David Baltimore. It had provided important support for Temin’s provirus hypothesis, a key tool in some gene cloning efforts, and for me, the needed surrogate for a retrovirus.
After years of studies, we could make retrovirus assay sensitive (×1,000 greater than electron microscopy) [the detail of the assay and its development was reviewed in ref (24)], readily applicable to the frequent sampling of cultures, and specific, i.e., distinguishable from the multiple human cellular DNA polymerases (5, 6, 24, 25). Among advances from others contributing to this were developments from a biotech company, Collaborative Research Inc., and the collaboration of their CEO, Ori Firdieman, with Baltimore in developing synthetic homopolymeric/oligomeric template/primers. We tested various forms of them over the years in the 1970s, and some were critical.
The second approach was attempted to grow primary human blood cells in sufficient amounts and over sufficient time to attempt proper culture. This would require growth factors, and a few were only recently discovered from conditional media. One key result we made was the discovery of a T-cell growth factor, later termed interleukin-2 (IL-2), which became the first studied cytokine (26–28). During the 1970s, the first infectious leukemia causing retroviruses of primates was discovered by Takeshi Kawakami in a Gibbon Ape (29), and in 1978, we found a new variant associated with T-cell leukemia among Gibbons in the wild (30). This Gibbon Ape T-cell leukemia virus coupled with IL-2 pushed us toward greater concentration on human T-cell leukemias, and with the good fortune of a thorough and dedicated post-doctoral working in my group, the key results were obtained (1–3, 7, 31–34).
Soon we found the second human retrovirus, HTLV-2, in a leukemic cell from a patient with a T-cell variant of having hairy cell leukemia (7). This virus is much less pathogenic than HTLV-1, differs mainly in some parts of the 3′ region of the genome, and likely had a different primate-to-man origin (8).
Exceptional Oncogenicity
It is estimated that HTLV-1 causes cancer in about 5% to 6% of infected people (16, 35, 36), but if the infection is acquired during infancy from, for example, mother’s milk, it may be as high as 20% (36). Either number is an exceptionally high rate of cancer causation from a single exposure to a carcinogen. This means the risk from HTLV-1 to cancer is one of the most dangerous pathogens known (35), but as we will mention later, HTLV-1 also causes other diseases. Another extraordinary feature of HTLV-1 is oncogenicity as proved by the amount of evidence available for its causative role summarized in Table 2 and the lack of any identifiable co-factors like HIV and AIDS—the virus and its human target seem sufficient. However, that does not mean there are no factors that promote the likelihood of cancer development. There may be many other factors limiting its oncogenicity, but to date, and unlike many other carcinogens, there is no known strong co-factor necessary for causation. This point is rather forcefully drawn home by in vitro transformation and in vivo transfection studies that lead to transformed cells that look and act like human adult T-cell leukemia/lymphoma (ATL) cells. Alone among known tumor viruses, HTLV-1 infection apparently does it all. Sometimes, the issue has been raised as to why so many do not get leukemia when infected. My hypothesis is that the HTLV-1 provirus drives the proliferation of infected cells for its survival since HTLV-1 is so poorly infectious and transmission comes mostly from infected cells. It is also plausible that the establishment of the in vivo leukemia may require the accumulation of somatic mutations in infected T cells, which is driven by the clastogenic nature of HTLV-1 with time. Recent whole-genome analyses of the ATL cells from many patients indeed demonstrate convergent patterns of genetic mutations (37–39). It is also suggested that aggressive (acute/lymphomatous subtypes) ATL is associated with an increased burden of genetic and epigenetic alterations (39), demonstrating the cumulative nature of genetic alterations in advancing the phenotype of ATL. Another recent finding that may corroborate this point is that ATL seems to be the leading cause of death even among human T lymphotropic virus type I-associated myelopathy/tropical spastic paraparesis (HAM/TSP) patients (40), suggesting that the process of cellular transformation by HTLV-1 indeed takes a long time but keeps accumulating while HTLV-1-infected cells manifest non-leukemic disorders.
Perhaps it is just a matter of time. The median value for the time required for HTLV-1-infected cells to accumulate sufficient mutations to become leukemic may be larger than the average life of humans. Given a far greater life span, we suspect that transformation might occur in most infected persons. So it is interesting to raise the question as to whether the early formation of the ATL cells is multifactorial as human cancer formation is in general or if HTLV-1 does it all. Also, is there any co-factor that might accelerate/diminish the speed of genetic alterations in HTLV-1-infected cells? Table 2 lists the exceptional evidence showing that HTLV-1 causes leukemia.
A Challenge to the Prevailing Dogma: One Gene Sequence→One Protein. One Protein→One Function. One Agent (Like a Virus)→One Disease
These were simple statements many of us heard when were still students, but, of course, as we have learned, none are true. I cannot think of any situation where these are all illustrated more clearly than HTLV-1 infection and disease. HTLV-1 is the first virus where multiple splicing of its primary RNA transcript was demonstrated (41), revealing that one genetic sequence could and indeed regularly contribute to the encoding of several proteins.
So too, some of its proteins unexpectedly reveal functions beyond the main and obvious one. For example, we know tax protein not only has trans-acting transcriptional activity but may be released from cells and have effects on other (by-stander) cells (42, 43), or the HBZ factor, which contributes to neoplastic transformation, impacting cell growth prior to transformation as well as controlling inflammation as protein and RNA (44–50).
Above, it was already noted that HTLV-1 causes more than ATL. It also induces spastic paralytic disease (HAM/TSP, HTLV-1 associated myelopathy/Tropical spastic paraparesis) immune mechanisms (51–54). Additionally, a slight variant from more common forms of HTLV-1 and known as HTLV-1c causes severe bronchiectasis, impacting the lives of native Australians (55–59). Several less crippling (yet are public health burden) disorders (including dermatitis and uveitis) are also associated with HTLV-1 (60–62). Infectious dermatitis is drawing clinical attention due to its manifestation among children and because it could develop into ATL or HAM/TSP later (63, 64). Overall, about 10% of HTLV-1 infections lead to multiple diseases.
HTLV Research Leads to HIV Discovery: An Unusual Coincidence of Their Discoveries Coming Just Before AIDS Was First Recognized
As noted above, in the 1970s, there was broad and strong resistance even to the possible existence of human retroviruses. The discoveries of the HTLVs (HTLV-1 reported in 1980 and HTLV-2 in 1982) were just being accepted when AIDS was first recognized in 1981, opening up the idea that AIDS might have a similar origin. However, by the time a patient was recognized as having AIDS, usually, the patient had many microbial infections. The question was which one was the cause? It turned out to be quite challenging; a hidden retrovirus was suggested and shown to be the cause. We can say with confidence that without the HTLV experience, this would have been thought of as a wild and unacceptable notion. Further, the key technology utilized for the discovery of HIV came out of HTLV research, namely, the growth of primary human blood T cells with IL-2 and a very sensitive and specific assay for a retrovirus (proper assays of RT), which were key to the findings on HIV.
HTLVs as Model Systems
We think of studies of HTLVs as significant not only for the cancer it causes but also for lessons provided from studies on the mechanisms that can cause spastic paralysis or immune disorders. There are many ways of exploiting HTLV infections to these ends. In vitro transformation of umbilical cord T cells (65) through co-culture with patient-derived ATL cells and the establishment of ATL cell lines from ATL patients (66, 67) were the first step that enabled the extensive research on how HTLV-1 transforms host cells. The cells display full ATL-like cancer characteristics (cellular and molecular features as well as their capacity to grow in animal models to form ATL-like leukemia/lymphoma), and the mechanisms underlying the cellular transformation by HTLV-1 have been widely studied using these ATL cell lines, to give rise to quite a few publications. This, in turn, has been made into in vivo models by expressing the HTLV-1 tax (68, 69) or hbz (45) genes as a transgene in mice. Both tumors and central nervous system (CNS) animal models are available (70). A prime example of a clinical advance to unrelated diseases came out of a drug development program planned as a limitation on CNS attack by immune cells and by drug developments against ATL. One of these drugs that we are developing (BNZ-1) is now undergoing trials for a similar CD4 T-cell malignancy (cutaneous T-cell lymphoma), which is not directly related to HTLV-1 (71, 72). As to the bronchiectasis/pulmonary disease frequently observed among native Australians (55, 56, 58, 59), this may have something to do with the unique origin and divergent DNA sequence of the HTLV-1c (57) compared with globally dominant HTLV-1 strains. Of interest is that the same region adjacent to the 3’ end of the viral genome is what chiefly distinguishes HTLV-1 from the less pathogenic HTLV-2 (8), suggesting that this region of HTLVs may control the pathogenesis of individual HTLV strains/subtypes. It will, of course, be most interesting to define how differences in sequences among HTLVs affect their pathogenesis, if they do.
There is a need for serious funding programs aimed at obtaining effective therapy and preventive vaccine for HTLV-1. This must be done in a climate of much greater attention and appreciation of the field along with greater funding.
Where HTLV Research Might Focus
First, more attention to the field is needed. This can only come from strong promotion, as has been carried out by Fabiola Martin for HTLV-1 research in Australia and in discussions with WHO (73, 74), but all in the field can do more. Those in areas of the world that are hardest hit by HTLV-1 are primed to be the most important activists. At present, this is in South America, Japan, and the native population of Australia. Eduardo Gotuzzo of Peru has been one such leader from South America, as have Toshi Watanabe, Yoshi Yamano, and Masao Matsuoka for Japan. Iran and Romania are enigmas. Hopefully, we will soon learn more about their HTLV-1 cases and research from “neighbors” like Ali Bazarbachi of Lebanon and with close ties with outstanding groups in Europe, notably the one led by Charles Bangham in London and several Italian groups including the one led by Roberto Accolla and colleagues.
Clearly understudied and underfunded are efforts directed to developing effective therapy and a preventive vaccine. We are hopeful that this will soon change.
Author Contributions
RGC and YT wrote the paper together. All authors listed have made a substantial, direct, and intellectual contributions to the work and approved it for publication.
Funding
This work was supported by the departmental funding of the Institute of Human Virology at the University of Maryland School of Medicine, Baltimore.
Conflict of Interest
YT holds financial interests with BIONIZ Therapeutics LLC, now Equillium Inc., (San Diego, CA) which holds the patent and intellectual property for the BNZ-1 peptide mentioned in this article.
The remaining author declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Poiesz BJ, Ruscetti FW, Gazdar AF, Bunn PA, Minna JD, Gallo RC. Detection and Isolation of Type C Retrovirus Particles From Fresh and Cultured Lymphocytes of a Patient With Cutaneous T-Cell Lymphoma. Proc Natl Acad Sci USA (1980) 77:7415–9. doi: 10.1073/pnas.77.12.7415
2. Poiesz BJ, Ruscetti FW, Mier JW, Woods AM, Gallo RC. T-Cell Lines Established From Human T-Lymphocytic Neoplasias by Direct Response to T-Cell Growth Factor. Proc Natl Acad Sci USA (1980) 77:6815–9. doi: 10.1073/pnas.77.11.6815
3. Poiesz BJ, Ruscetti FW, Reitz MS, Kalyanaraman VS, Gallo RC. Isolation of a New Type C Retrovirus (HTLV) in Primary Uncultured Cells of a Patient With Sezary T-Cell Leukaemia. Nature (1981) 294:268–71. doi: 10.1038/294268a0
4. Spiegelman S. Molecular Evidence for the Association of RNA Tumor Viruses With Human Mesenchymal Malignancies. Hamatol Bluttransfus (1976) 19:391–429. doi: 10.1007/978-3-642-87524-3_38
5. Bobrow SN, Smith RG, Reitz MS, Gallo RC. Stimulated Normal Human Lymphocytes Contain a Ribonuclease-Sensitive DNA Polymerase Distinct From Viral RNA-Directed DNA Polymerase. Proc Natl Acad Sci USA (1972) 69:3228–32. doi: 10.1073/pnas.69.11.3228
6. Reitz MS Jr, Smith RG, Roseberry EA, Gallo RC. DNA-Direced and RNA-Primed DNA Synthesis in Microsomal and Mitochondrial Fractions of Normal Human Lymphocytes. Biochem Biophys Res Commun (1974) 57:934–48. doi: 10.1016/0006-291X(74)90635-4
7. Kalyanaraman VS, Sarngadharan MG, Robert-Guroff M, Miyoshi I, Golde D, Gallo RC. A New Subtype of Human T-Cell Leukemia Virus (HTLV-II) Associated With a T-Cell Variant of Hairy Cell Leukemia. Science (1982) 218:571–3. doi: 10.1126/science.6981847
8. Sodroski J, Patarca R, Perkins D, Briggs D, Lee TH, Essex M, et al. Sequence of the Envelope Glycoprotein Gene of Type II Human T Lymphotropic Virus. Science (1984) 225:421–4. doi: 10.1126/science.6204380
9. Sarngadharan MG, Popovic M, Bruch L, Schupbach J, Gallo RC. Antibodies Reactive With Human T-Lymphotropic Retroviruses (HTLV-III) in the Serum of Patients With AIDS. Science (1984) 224:506–8. doi: 10.1126/science.6324345
10. Schupbach J, Popovic M, Gilden RV, Gonda MA, Sarngadharan MG, Gallo RC. Serological Analysis of a Subgroup of Human T-Lymphotropic Retroviruses (HTLV-III) Associated With AIDS. Science (1984) 224:503–5. doi: 10.1126/science.6200937
11. Gallo RC, Salahuddin SZ, Popovic M, Shearer GM, Kaplan M, Haynes BF, et al. Frequent Detection and Isolation of Cytopathic Retroviruses (HTLV-III) From Patients With AIDS and at Risk for AIDS. Science (1984) 224:500–3. doi: 10.1126/science.6200936
12. Popovic M, Sarngadharan MG, Read E, Gallo RC. Detection, Isolation, and Continuous Production of Cytopathic Retroviruses (HTLV-III) From Patients With AIDS and Pre-AIDS. Science (1984) 224:497–500. doi: 10.1126/science.6200935
13. Schupbach J, Sarngadharan MG, Gallo RC. Antigens on HTLV-Infected Cells Recognized by Leukemia and AIDS Sera are Related to HTLV Viral Glycoprotein. Science (1984) 224:607–10. doi: 10.1126/science.6324349
15. Gallo RC, Sarngadharan MG, Popovic M, Shaw GM, Hahn B, Wong-Staal F, et al. HTLV-III and the Etiology of AIDS. Prog Allergy (1986) 37:1–45. doi: 10.1159/000412125
16. Gessain A, Cassar O. Epidemiological Aspects and World Distribution of HTLV-1 Infection. Front Microbiol (2012) 3:388. doi: 10.3389/fmicb.2012.00388
17. Gessain A, Gallo RC, Franchini G. Low Degree of Human T-Cell Leukemia/Lymphoma Virus Type I Genetic Drift In Vivo as a Means of Monitoring Viral Transmission and Movement of Ancient Human Populations. J Virol (1992) 66:2288–95. doi: 10.1128/jvi.66.4.2288-2295.1992
18. Yanagihara R. Geographic-Specific Genotypes or Topotypes of Human T-Cell Lymphotropic Virus Type I as Markers for Early and Recent Migrations of Human Populations. Adv Virus Res (1994) 43:147–86. doi: 10.1016/S0065-3527(08)60048-2
19. Mahgoub M, Yasunaga JI, Iwami S, Nakaoka S, Koizumi Y, Shimura K, et al. Sporadic on/Off Switching of HTLV-1 Tax Expression is Crucial to Maintain the Whole Population of Virus-Induced Leukemic Cells. Proc Natl Acad Sci USA (2018) 115:E1269–78. doi: 10.1073/pnas.1715724115
20. Kulkarni A, Mateus M, Thinnes CC, McCullagh JS, Schofield CJ, Taylor GP, et al. Glucose Metabolism and Oxygen Availability Govern Reactivation of the Latent Human Retrovirus HTLV-1. Cell Chem Biol (2017) 24:1377–1387 e3. doi: 10.1016/j.chembiol.2017.08.016
21. Kulkarni A, Taylor GP, Klose RJ, Schofield CJ, Bangham CR. Histone H2A Monoubiquitylation and P38-MAPKs Regulate Immediate-Early Gene-Like Reactivation of Latent Retrovirus HTLV-1. JCI Insight (2018) 3 (20):e123196. doi: 10.1172/jci.insight.123196
22. Miura M, Dey S, Ramanayake S, Singh A, Rueda DS, Bangham CRM. Kinetics of HTLV-1 Reactivation From Latency Quantified by Single-Molecule RNA FISH and Stochastic Modelling. PloS Pathog (2019) 15:e1008164. doi: 10.1371/journal.ppat.1008164
23. Bangham CRM, Miura M, Kulkarni A, Matsuoka M. Regulation of Latency in the Human T Cell Leukemia Virus, HTLV-1. Annu Rev Virol (2019) 6:365–85. doi: 10.1146/annurev-virology-092818-015501
24. Sarngadharan MG, Robert-Guroff M, Gallo RC. DNA Polymerases of Normal and Neoplastic Mammalian Cells. Biochim Biophys Acta (1978) 516:419–87. doi: 10.1016/0304-419X(78)90019-7
25. Allaudeen HS, Sarngadharan MG, Gallo RC. A Comparative Evaluation of Methods for Isolation of RNA-Directed DNA Polymerase From Cells in a Reconstituted System. Biochim Biophys Acta (1976) 435:45–62. doi: 10.1016/0005-2787(76)90190-8
26. Morgan DA, Ruscetti FW, Gallo R. Selective In Vitro Growth of T Lymphocytes From Normal Human Bone Marrows. Science (1976) 193:1007–8. doi: 10.1126/science.181845
27. Ruscetti FW, Mier JW, Gallo RC. Human T-Cell Growth Factor: Parameters for Production. J Supramol Struct (1980) 13:229–41. doi: 10.1002/jss.400130211
28. Gallo RC. Growth of Human Normal and Leukemic T Cells: T-Cell Growth Factor (TCGF) and the Isolation of a New Class of RNA Tumor Viruses (HTLV). Blood Cells (1981) 7:313–29.
29. Sun L, Kawakami TG. Isolation and Identification of Lymphocytic and Myelogenous Leukemia-Specific Sequences in Genomes of Gibbon Oncornaviruses. J Virol (1980) 35:400–8. doi: 10.1128/jvi.35.2.400-408.1980
30. Gallo RC, Gallagher RE, Wong-Staal F, Aoki T, Markham PD, Schetters H, et al. Isolation and Tissue Distribution of Type-C Virus and Viral Components From a Gibbon Ape (Hylobates Lar) With Lymphocytic Leukemia. Virology (1978) 84:359–73. doi: 10.1016/0042-6822(78)90255-6
31. Rho HM, Poiesz B, Ruscetti FW, Gallo RC. Characterization of the Reverse Transcriptase From a New Retrovirus (HTLV) Produced by a Human Cutaneous T-Cell Lymphoma Cell Line. Virology (1981) 112:355–60. doi: 10.1016/0042-6822(81)90642-5
32. Oroszlan S, Sarngadharan MG, Copeland TD, Kalyanaraman VS, Gilden RV, Gallo RC. Primary Structure Analysis of the Major Internal Protein P24 of Human Type C T-Cell Leukemia Virus. Proc Natl Acad Sci USA (1982) 79:1291–4. doi: 10.1073/pnas.79.4.1291
33. Kalyanaraman VS, Sarngadharan MG, Poiesz B, Ruscetti FW, Gallo RC. Immunological Properties of a Type C Retrovirus Isolated From Cultured Human T-Lymphoma Cells and Comparison to Other Mammalian Retroviruses. J Virol (1981) 38:906–15. doi: 10.1128/jvi.38.3.906-915.1981
34. Popovic M, Reitz MS Jr, Sarngadharan MG, Robert-Guroff M, Kalyanaraman VS, Nakao Y, et al. The Virus of Japanese Adult T-Cell Leukaemia is a Member of the Human T-Cell Leukaemia Virus Group. Nature (1982) 300:63–6. doi: 10.1038/300063a0
35. Tagaya Y, Gallo RC. The Exceptional Oncogenicity of HTLV-1. Front Microbiol (2017) 8:1425. doi: 10.3389/fmicb.2017.01425
36. Malik B, Taylor GP. Can We Reduce the Incidence of Adult T-Cell Leukaemia/Lymphoma? Cost-Effectiveness of Human T-Lymphotropic Virus Type 1 (HTLV-1) Antenatal Screening in the United Kingdom. Br J Haematol (2019) 184:1040–3. doi: 10.1111/bjh.15234
37. Kogure Y, Kataoka K. Genetic Alterations in Adult T-Cell Leukemia/Lymphoma. Cancer Sci (2017) 108:1719–25. doi: 10.1111/cas.13303
38. Kataoka K, Nagata Y, Kitanaka A, Shiraishi Y, Shimamura T, Yasunaga J, et al. Integrated Molecular Analysis of Adult T Cell Leukemia/Lymphoma. Nat Genet (2015) 47:1304–15. doi: 10.1038/ng.3415
39. Kataoka K, Iwanaga M, Yasunaga JI, Nagata Y, Kitanaka A, Kameda T, et al. Prognostic Relevance of Integrated Genetic Profiling in Adult T-Cell Leukemia/Lymphoma. Blood (2018) 131:215–25. doi: 10.1182/blood-2017-01-761874
40. Nagasaka M, Yamagishi M, Yagishita N, Araya N, Kobayashi S, Makiyama J, et al. Mortality and Risk of Progression to Adult T Cell Leukemia/Lymphoma in HTLV-1-Associated Myelopathy/Tropical Spastic Paraparesis. Proc Natl Acad Sci USA (2020) 117:11685–91. doi: 10.1073/pnas.1920346117
41. Manzari V, Wong-Staal F, Franchini G, Colombini S, Gelmann EP, Oroszlan S, et al. Human T-Cell Leukemia-Lymphoma Virus (HTLV): Cloning of an Integrated Defective Provirus and Flanking Cellular Sequences. Proc Natl Acad Sci USA (1983) 80:1574–8. doi: 10.1073/pnas.80.6.1574
42. Matsuoka M, Jeang KT. Human T-Cell Leukemia Virus Type 1 (HTLV-1) and Leukemic Transformation: Viral Infectivity, Tax, HBZ and Therapy. Oncogene (2011) 30:1379–89. doi: 10.1038/onc.2010.537
43. Currer R, Van Duyne R, Jaworski E, Guendel I, Sampey G, Das R, et al. HTLV Tax: A Fascinating Multifunctional Co-Regulator of Viral and Cellular Pathways. Front Microbiol (2012) 3:406. doi: 10.3389/fmicb.2012.00406
44. Satou Y, Yasunaga J, Yoshida M, Matsuoka M. [HTLV-1 bZIP Factor (HBZ) Gene has a Growth-Promoting Effect on Adult T-Cell Leukemia Cells]. Rinsho Ketsueki (2008) 49:1525–9.
45. Satou Y, Yasunaga J, Zhao T, Yoshida M, Miyazato P, Takai K, et al. HTLV-1 bZIP Factor Induces T-Cell Lymphoma and Systemic Inflammation In Vivo. PloS Pathog (2011) 7:e1001274. doi: 10.1371/journal.ppat.1001274
46. Matsuoka M, Mesnard JM. HTLV-1 bZIP Factor: The Key Viral Gene for Pathogenesis. Retrovirology (2020) 17:2. doi: 10.1186/s12977-020-0511-0
47. Enose-Akahata Y, Vellucci A, Jacobson S. Role of HTLV-1 Tax and HBZ in the Pathogenesis of HAM/TSP. Front Microbiol (2017) 8:2563. doi: 10.3389/fmicb.2017.02563
48. Ma G, Yasunaga J, Matsuoka M. Multifaceted Functions and Roles of HBZ in HTLV-1 Pathogenesis. Retrovirology (2016) 13:16. doi: 10.1186/s12977-016-0249-x
49. Forlani G, Shallak M, Tedeschi A, Cavallari I, Marcais A, Hermine O, et al. Dual Cytoplasmic and Nuclear Localization of HTLV-1-Encoded HBZ Protein is a Unique Feature of Adult T-Cell Leukemia. Haematologica (2021) 106:2076–85. doi: 10.3324/haematol.2020.272468
50. Forlani G, Baratella M, Tedeschi A, Pique C, Jacobson S, Accolla RS. HTLV-1 HBZ Protein Resides Exclusively in the Cytoplasm of Infected Cells in Asymptomatic Carriers and HAM/TSP Patients. Front Microbiol (2019) 10:819. doi: 10.3389/fmicb.2019.00819
51. Gessain A, Barin F, Vernant JC, Gout O, Maurs L, Calender A, et al. Antibodies to Human T-Lymphotropic Virus Type-I in Patients With Tropical Spastic Paraparesis. Lancet (1985) 2:407–10. doi: 10.1016/S0140-6736(85)92734-5
52. Osame M, Usuku K, Izumo S, Ijichi N, Amitani H, Igata A, et al. HTLV-I Associated Myelopathy, a New Clinical Entity. Lancet (1986) 1:1031–2. doi: 10.1016/S0140-6736(86)91298-5
53. Bangham CR, Araujo A, Yamano Y, Taylor GP. HTLV-1-Associated Myelopathy/Tropical Spastic Paraparesis. Nat Rev Dis Primers (2015) 1:15012. doi: 10.1038/nrdp.2015.12
54. Matsuura E, Yamano Y, Jacobson S. Neuroimmunity of HTLV-I Infection. J Neuroimmune Pharmacol (2010) 5:310–25. doi: 10.1007/s11481-010-9216-9
55. Steinfort DP, Brady S, Weisinger HS, Einsiedel L. Bronchiectasis in Central Australia: A Young Face to an Old Disease. Respir Med (2008) 102:574–8. doi: 10.1016/j.rmed.2007.11.007
56. Einsiedel L, Fernandes L, Spelman T, Steinfort D, Gotuzzo E. Bronchiectasis is Associated With Human T-Lymphotropic Virus 1 Infection in an Indigenous Australian Population. Clin Infect Dis (2012) 54:43–50. doi: 10.1093/cid/cir766
57. Cassar O, Einsiedel L, Afonso PV, Gessain A. Human T-Cell Lymphotropic Virus Type 1 Subtype C Molecular Variants Among Indigenous Australians: New Insights Into the Molecular Epidemiology of HTLV-1 in Australo-Melanesia. PloS Negl Trop Dis (2013) 7:e2418. doi: 10.1371/journal.pntd.0002418
58. Einsiedel L, Chiong F, Jersmann H, Taylor GP. Human T-Cell Leukaemia Virus Type 1 Associated Pulmonary Disease: Clinical and Pathological Features of an Under-Recognised Complication of HTLV-1 Infection. Retrovirology (2021) 18:1. doi: 10.1186/s12977-020-00543-z
59. Einsiedel L, Pham H, Talukder MRR, Liddle J, Taylor K, Wilson K, et al. Pulmonary Disease Is Associated With Human T-Cell Leukemia Virus Type 1c Infection: A Cross-Sectional Survey in Remote Aboriginal Communities. Clin Infect Dis (2021) 73:e1498–506. doi: 10.1093/cid/ciaa1401
60. Uchiyama T. Human T Cell Leukemia Virus Type I (HTLV-I) and Human Diseases. Annu Rev Immunol (1997) 15:15–37. doi: 10.1146/annurev.immunol.15.1.15
61. Martin F, Taylor GP, Jacobson S. Inflammatory Manifestations of HTLV-1 and Their Therapeutic Options. Expert Rev Clin Immunol (2014) 10:1531–46. doi: 10.1586/1744666X.2014.966690
62. Schierhout G, McGregor S, Gessain A, Einsiedel L, Martinello M, Kaldor J. Association Between HTLV-1 Infection and Adverse Health Outcomes: A Systematic Review and Meta-Analysis of Epidemiological Studies. Lancet Infect Dis (2020) 20:133–43. doi: 10.1016/S1473-3099(19)30402-5
63. LaGrenade L, Hanchard B, Fletcher V, Cranston B, Blattner W. Infective Dermatitis of Jamaican Children: A Marker for HTLV-I Infection. Lancet (1990) 336:1345–7. doi: 10.1016/0140-6736(90)92896-P
64. Benencio P, Ducasa N, Arruvito L, Irurzun I, Praino L, Lamberti M, et al. Case Report: Relevance of an Accurate Diagnosis and Monitoring of Infective Dermatitis Associated With Human T-Lymphotropic Virus Type 1 in Childhood. Front Med (Lausanne) (2021) 8:758352. doi: 10.3389/fmed.2021.758352
65. Miyoshi I, Kubonishi I, Yoshimoto S, Shiraishi Y. A T-Cell Line Derived From Normal Human Cord Leukocytes by Co-Culturing With Human Leukemic T-Cells. Gan (1981) 72:978–81.
66. Miyoshi I, Miyamoto K, Sumida M, Nishihara R, Lai M, Yoshimoto S, et al. Chromosome 14q+ in Adult T-Cell Leukemia. Cancer Genet Cytogenet (1981) 3:251–9. doi: 10.1016/0165-4608(81)90092-3
67. Maeda M, Arima N, Daitoku Y, Kashihara M, Okamoto H, Uchiyama T, et al. Evidence for the Interleukin-2 Dependent Expansion of Leukemic Cells in Adult T Cell Leukemia. Blood (1987) 70:1407–11. doi: 10.1182/blood.V70.5.1407.bloodjournal7051407
68. Kitajima I, Shinohara T, Bilakovics J, Brown DA, Xu X, Nerenberg M. Ablation of Transplanted HTLV-I Tax-Transformed Tumors in Mice by Antisense Inhibition of NF-Kappa B. Science (1992) 258:1792–5. doi: 10.1126/science.1299224
69. Hasegawa H, Sawa H, Lewis MJ, Orba Y, Sheehy N, Yamamoto Y, et al. Thymus-Derived Leukemia-Lymphoma in Mice Transgenic for the Tax Gene of Human T-Lymphotropic Virus Type I. Nat Med (2006) 12:466–72. doi: 10.1038/nm1389
70. Forlani G, Shallak M, Accolla RS, Romanelli MG. HTLV-1 Infection and Pathogenesis: New Insights From Cellular and Animal Models. Int J Mol Sci (2022) 22:8001–24. doi: 10.3390/ijms22158001
71. Moignet AL, Larny T. Latest Advances in the Diagnosis and Treatment of Large Granular Lymphocytic Leukemia. In: American Society of Clinical Oncology Educational Book. Alexandria, VA: American Society of Clinical Oncology. (2018). p. 616–25.
72. Frohna PA, Ratnayake A, Doerr N, Basheer A, Al-Mawsawi LQ, Kim WJ, et al. Results From a First-In-Human Study of BNZ-1, a Selective Multicytokine Inhibitor Targeting Members of the Common Gamma (Gammac) Family of Cytokines. J Clin Pharmacol (2020) 60:264–73. doi: 10.1002/jcph.1522
73. Martin F, Tagaya Y, Gallo R. Time to Eradicate HTLV-1: An Open Letter to WHO. Lancet (2018) 391:1893–4. doi: 10.1016/S0140-6736(18)30974-7
74. New WHO Report on Human T-Lymphotropic Virus Type 1 Highlights Strategies for its Prevention and Control, in: (2021). Available at: https://www.who.int/news/item/03-03-2021-new-who-report-on-human-t-lymphotropic-virus-type-1-indicates-the-future-path-for-its-prevention-and-control.
Keywords: HTLV-1, human retrovirus, human oncovirus, leukemogenesis, development of a concept
Citation: Gallo RC and Tagaya Y (2022) Reflections on Some of the Exceptional Features of HTLV-1 and HTLV-1 Research: A Perspective. Front. Immunol. 13:859654. doi: 10.3389/fimmu.2022.859654
Received: 21 January 2022; Accepted: 28 February 2022;
Published: 01 April 2022.
Edited by:
Roberto S. Accolla, University of Insubria, ItalyReviewed by:
Antoine Gessain, Institut Pasteur, FranceCopyright © 2022 Gallo and Tagaya. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Robert C. Gallo, cmdhbGxvQElodi51bWFyeWxhbmQuZWR1
 Robert C. Gallo
Robert C. Gallo Yutaka Tagaya
Yutaka Tagaya