- 1University of Pennsylvania, Philadelphia, PA, United States
- 2Consultant, Doylestown, PA, United States
Correlates of protection are key for vaccine development against any pathogen. In this paper we summarize recent information about correlates for vaccines against dengue, Ebola, influenza, pneumococcal, respiratory syncytial virus, rotavirus, shigella, tuberculosis and Zika virus.
Introduction
A correlate of protection (CoP) is an immune function that correlates with and may be biologically responsible for vaccine-induced efficacy. The literature on this subject has grown considerably since it was identified as an important issue in vaccinology (1–5). The importance of CoP with regard to vaccines against SARS-2, the coronavirus causing COVID-19, needs no emphasis, and numerous papers have been published on that subject (6). However, not so much has been published recently about vaccines against other diseases. This paper is an effort to summarize recent findings in a number of important examples.
It should be acknowledged that the subject of CoP has become more complex due to increasing knowledge concerning Fc Effector antibody mediated functions and T cell mediated functions (7, 8). However, while it is evident that CoPs are often multiple and synergistic, their utility depends on identifying responses that are major and measurable. The fact that immune responses are often synergistic does not negate the value of identifying the main immune function that correlates with the protection generated by vaccination.
The SARS-2 novel coronavirus has been with us for only the last two years, but much work has been expended on defining a CoP, as recently summarized (6). The chief CoP is clearly neutralizing antibodies, with a gradual increase in efficacy as the titer increases. Although T cell responses and Fc effector antibodies are important in modifying the results of infection, antibodies play the major role in preventing infection in the first place (9–11). However, antibodies must be specific for the variant virus, as the neutralizing epitopes differ between strains (12).
Dengue viruses
The correlates of protection against the four serotypes of dengue virus remain debatable, despite the development of several vaccines that have demonstrated some degree of efficacy (13–17). That efficacy has been influenced by age of the vaccinated population and serotype of the circulating dengue virus. It appears that efficacy is related to the induction of homotypic antibodies, whereas heterotypic antibody may actually enhance disease caused by other serotypes. The Dengvaxia vaccine is licensed only for those aged 9 years or above, and is most effective against dengue serotype 4, against which it induces homotypic specific antibodies. However, in a trial conducted in subjects aged 9 to 16 years with evidence of prior infection with a single serotype, efficacy was 67%, 67%, 80% and 89% respectively against types 1, 2, 3, and 4. Thus, homotypic neutralizing antibodies was the best correlate of protection against infection, but once an individual had infection by one serotype the Dengvaxia vaccine gave efficacy against other serotypes (18, 19). A live attenuated vaccine developed by Takeda was shown to induce that type of response (20). FC effector antibody functions may have a role in protection (21), and antibodies to NS1 reduce severity of disease (14) although no absolute correlate is available. However, at this point the best correlates of protection appears to be type-specific neutralizing antibodies (19).
Ebola virus
Vectored vaccines against the Ebola filovirus have been highly successful in controlling outbreaks of the disease in Africa. All of the vaccines are able to induce antibodies to the glycoprotein that is present in quantity on the elongated virus particle. However, the CoP is more complex than antibodies alone, and there is strong evidence that CD8+ T cells reacting against Ebola virus are necessary for high efficacy. Thus, Ebola is an example of where both arms of the immune system must respond in order for a vaccine to optimally prevent disease (22–28).
The functions of immune responses induced by successful Ebola vaccines are multiple, involving antibodies to the glycoprotein but also T cell responses (29). The role of the latter in protection appears to depend on the host species, being more important in infections occurring in primates (30). Study of vaccinated subjects also suggests important synergies between antibody and cellular immune functions. Moreover, the selection of adjuvant influences the mechanism of protection (31). For example, a CpG adjuvant stimulating the TLR-9 receptor gave superior survival. In summary, IgG antibody to the viral glycoprotein is the major CoP for Ebola, but is influenced by the type of adjuvant used. In addition, the sheer quantity of glycoprotein on the elongated virus particle may influence the quantity of responses correlated with protection (22, 32–38).
Influenza
The CoP for influenza that is commonly accepted for influenza is a 1/40 hemagglutinin-inhibition titer, which is credited with signifying a 50% protective ability. This is an oversimplification and ignores many other immunological functions that contribute to the efficacy of influenza vaccines (24, 39). Age of the vaccinee and the type of immunogen also influence the CoP. The widely used HAI titer of 1/40 corresponds to about 50% efficacy in young adults who have had immunologic priming by prior influenza infections. However, that titer conveys lower efficacy in older adults. The single radial hemolysis assay of >25 mm corresponds to about 70% efficacy in adults. In children who have not had prior infection or vaccination an HI titer of 110 gives 50% protection. In any case, in adults protection rises with HI titers, but protection is not guaranteed at higher titers nor absent at lower titers (24, 40).
Although neutralization is clearly an important function of antibodies, Fc effector functions such as antibody-dependent cellular cytotoxicity (ADCC) and antibody-dependent phagocytosis (ADP) play a role in protection. In addition, influenza vaccines contain neuraminidase, though often unmeasured, which contributes to protection (25, 26). Neuraminidase concentration may vary between strains (41). Finally, cell-mediated immunity has not received enough attention and probably contributes to controlling virus replication (42). In summary, multiple antibody functions contribute to influenza vaccine efficacy (43–46).
Pneumococci
The vaccines against pneumococcal disease are composed of pneumococcal capsular polysaccharides conjugated chemically with proteins to increase immunogenicity, especially in children. For many years an antibody response measured by ELISA with a level of 0.35 micrograms/ml was accepted as a CoP. However, a seminal paper has demonstrated that the protective level is very much dependent on serotype, with type 3 being the most resistant; types 1, 7F, 19A, and 19 F requiring high antibody levels; and types 6A, 6B, 18C and 23F being less resistant (47). Thus, 0.35 mcg gives only a general estimate of a CoP with little precision. For type 3 relatively high levels of antibody are needed, estimated to be 2.83 mcg/ml. This means that the efficacy of conjugated pneumococcal polysaccharide vaccines will vary with the epidemiology of serotypes, and that vaccines will vary in efficacy depending on the composition of serotypes and the sites of infections. The variability of CoPs for different serotypes was recently confirmed by the results of a study in African toddlers that gave 0.26 mcg/ml as CoP for type 14 but 1.93 mcg/ml as CoP for type 23F (28). The conclusion must be that the CoPs for pneumococcal serotypes are variable and must be determined individually.
Respiratory syncytial virus
Protection against RSV lower respiratory illness is complex: There are two distinct syndromes, one occurring in young infants who have only transplacental neutralizing antibodies to RSV, and a second occurring in the elderly, in whom the pathogenesis of disease is more complex. Antibodies having high neutralizing function are clearly protective in the very young, as shown by the correlation between antibody titer and protection, as well as the prophylactic value of administered monoclonal antibodies (23, 43, 44). A group A RSV inhibitory titer of 1/239 and a group B RSV inhibitory titer of 1/60 were associated with protection against disease (45). Antibodies against the prefusion form of the F protein are those that correlate best with protection. However, Fc effector as well as neutralizing functions of antibody are important, particularly in the lower respiratory tract (23, 34, 46, 47).
On the other hand, pathogenesis of RSV disease is less clear in seropositive elderly adults, in whom administration of antibodies is less effective. In part this may be due to the need to direct antibodies against other antigens of the virus and to elicit functions other than neutralization, particularly T cell functions (35). Antibodies and T cell responses against the small hydrophobic (SH) protein appear to be more important in adult infections. Thus, the problem of RSV vaccine development is less for infants, in whom monoclonal antibodies are protective. The level of neutralizing antibodies in infants predict protection from RSV (45) and thus the problem of vaccine development in infancy could be solved by developing a vaccine based on the prefusion form of the F protein (36, 37). Previously, numerous attempts to develop an RSV vaccine for the elderly have failed to give high levels of protection, despite the use of many strategies including nanoparticle, subunit, live-attenuated and vector-based (36–38, 48). However, the use of prefusion forms of the fusion protein rather than the post-fusion form has recently given encouraging immune responses in adults (49). Although it is uncertain as to whether the efficacy relates to serum or mucosal antibody responses. In addition, cell-mediated immunity may be important for protection of adults (50). However, a monoclonal antibody against prefusion F was successful in preventing RSV disease in children (51).
Rotavirus
Rotavirus vaccination has been spectacularly successful in high-income countries, though less so in poor countries where children are exposed to many pathogens soon after birth. Over the years since introduction of rotavirus vaccines, an intestinal IgA response and its surrogate, serum IgA, has been considered to be the principal CoP (52–54). A level of more than 20U/ml has been proposed as the protective level (55). However, other studies have not found serum IgA to be a convincing CoP, particularly in low-income countries (56, 57). A thorough review by Clarke and Desselburger (57) concluded that VP6 antibodies may be a better correlate. VP6 is part of the capsid of rotaviruses, and although it does not induce neutralizing antibodies, non-neutralizing antibodies to VP6 develop after infection or vaccination and thus may be a good correlate for protection. However, attempts to develop parenteral vaccines against rotavirus have so far failed, and it appears that secretory responses at the level of the intestine are the best correlates. However, serum IgA serves as an indicator of IgA responses in the intestine (52, 58).
Shigella
In a review published in 2007 Levine et al. (59) wrote that “Identification of protection is arguably the most crucial catalyst needed to accelerate the development of effective Shigella vaccines,” but added that no clear correlate had been identified. Multiple candidate vaccines against shigella continue to be studied, including those containing the surface O antigen, antibodies to which are one proposed correlate (60, 61). In a detailed analysis Clarkson et al. (62) conclude that there are multiple CoPs, which may differ from one species to another. It appears that both serum and mucosal responses may serve as CoP depending on the challenge situation. This may simply reflect a situation in which the shigella organism must first replicate in the intestine by overcoming mucosal antibodies, but then invade the intestine, where systemic antibodies may be more important. Nevertheless, serum antibodies measured in various ways correlate with efficacy of shigella vaccines (63).
Tuberculosis
Bacille Calmette-Guérin, an attenuated Mycobacterium bovis, has been used for many years as a vaccine against TB, but with efficacy largely confined to vaccination at birth. Many attempts have been made to improve on BCG, for which identification of a CoP would be key. Studies in cows confirm that protective immunity correlates with a Th1 bias and induction of interferon gamma producing T lymphocytes. The presence of central memory T cells also correlates with protection (64). Intravenous BCG given to macaque monkeys also protected against active tuberculosis, which correlated with induction of T cells reacting to tuberculosis antigens (65).
The search for an easily administered and more effective vaccine against human tuberculosis continues. There is agreement that T cells, both CD4+ and CD8+, are key to protection particularly with regard to interferon secretion, but Th17 cells may also play a role. Vaccine delivery by an aerosol route might be preferable (66). A recent review concluded that BCG is only effective in children (67). In any case, it is likely that a T cell function that has not yet been identified will provide the best correlate of protection against tuberculosis (68).
Zika
As Zika virus is transmitted by mosquito bite, it is not surprising that antibodies in the blood stream are protective. In macaques neutralizing antibody titers of about 1/100 induced by inactivated virus vaccines were shown to be highly protective (69, 70). However, cross-reactive antibodies with other flaviviruses raise questions about whether inducing Zika antibodies might enhance their replication (71).
Summary
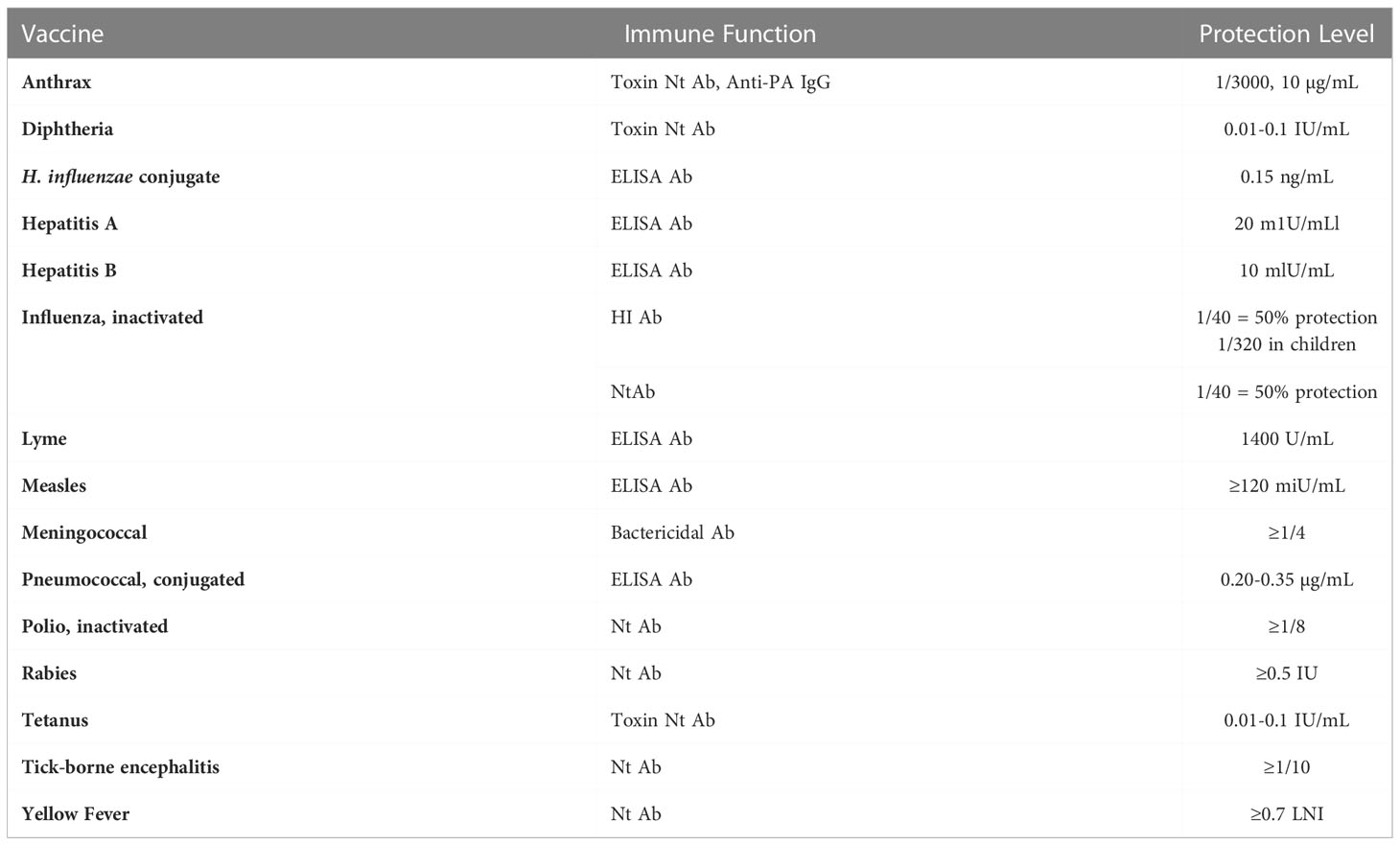
Knowledge concerning correlates of protection by vaccines is critical to their application and continues to grow (5). In this article we report some recent findings for selected vaccines. Although from a biological point of view vaccines produce a variety of protective functions, some are more important than others, and are useful to predict efficacy. Table 1 lists correlates of protection for some major vaccines.
Current interest in correlates has been raised by the SARS-2 new coronavirus vaccines. As discussed elsewhere (6), the principal correlate of protection is antibodies measured by neutralization or ELISA. However, although there is no threshold value for protection, titers of approximately 1/100 give efficacy against disease better than 50%, whereas titers of 1/1000 or more give efficacy over 90%.
Data availability statement
The original contributions presented in the study are included in the article/supplementary materials. Further inquiries can be directed to the corresponding author.
Author contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Plotkin SA. Immunologic correlates of protection induced by vaccination. Pediat Infect Dis (2001) 20(1):63–75. doi: 10.1097/00006454-200101000-00013
2. Plotkin SA. Vaccines: Correlates of vaccine-induced immunity. Clin Infect Dis (2008) 47(3):401–9. doi: 10.1086/589862
3. Plotkin SA, Gilbert PB. Nomenclature for immune correlates of protection after vaccination. Clin Infect Dis (2012) 54(11):1615–7. doi: 10.1093/cid/cis238
4. Plotkin SA. Increasing complexity of vaccine development. J Infect Dis (2015) 212 Suppl 1:S12–6. doi: 10.1093/infdis/jiu568
5. Plotkin SA. Updates on immunologic correlates of vaccine-induced protection. Vaccine. (2020) 38(9):2250–7. doi: 10.1016/j.vaccine.2019.10.046
6. Goldblatt D, Alter G, Crotty S, Plotkin SA. Correlates of protection against SARS-CoV-2 infection and COVID-19 disease. Immunol Rev (2022) 310(1):6–26. doi: 10.1111/imr.13091
7. Boudreau CM, Alter G. Extra-neutralizing FcR-mediated antibody functions for a universal influenza vaccine. Front Immunol (2019) 10:440. doi: 10.3389/fimmu.2019.00440
8. Tarke A, Potesta M, Varchetta S, Fenoglio D, Iannetta M, Sarmati L, et al. Early and polyantigenic CD4 T cell responses correlate with mild disease in acute COVID-19 donors. Int J Mol Sci (2022) 23(13):7155. doi: 10.3390/ijms23137155
9. Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med (2021) 27(7):1205–11. doi: 10.1038/s41591-021-01377-8
10. Earle KA, Ambrosino DM, Fiore-Gartland A, Goldblatt D, Gilbert PB, Siber GR, et al. Evidence for antibody as a protective correlate for COVID-19 vaccines. Vaccine. (2021) 39(32):4423–8. doi: 10.1016/j.vaccine.2021.05.063
11. Gilbert PB, Montefiori DC, McDermott AB, Fong Y, Benkeser D, Deng W, et al. Team§; coronavirus vaccine prevention network (CoVPN)/Coronavirus efficacy (COVE) team§; united states government (USG)/CoVPN biostatistics team§. immune correlates analysis of the mRNA-1273 COVID-19 vaccine efficacy clinical trial. Science. (2022) 375(6576):43–50. doi: 10.1126/science.abm3425
12. Feng S, Phillips DJ, White T, Sayal H, Aley PK, Bibi S, et al. Correlates of protection against symptomatic and asymptomatic SARS-CoV-2 infection. Nat Med (2021) 27(11):2032–40. doi: 10.1038/s41591-021-01540-1
13. Srikiatkhachorn A, Yoon IK. Immune correlates for dengue vaccine development. Expert Rev Vaccines (2016) 15(4):455–65. doi: 10.1586/14760584.2016.1116949
14. Katzelnick LC, Baric R, Coller B, Coloma J, Crowe J, Cummings D, et al. Participants in the summit on dengue immune correlates of protection. immune correlates of protection for dengue: State of the art and research agenda. Vaccine. (2017) 35(36):4659–69. doi: 10.1016/j.vaccine.2017.07.045
15. Wilder-Smith A, Ooi EE, Horstick O, Wills B. Dengue. Lancet. (2019) 393(10169):350–63. doi: 10.1016/S0140-6736(18)32560-1
16. Halstead S. Recent advances in understanding dengue. F1000Res (2019) 8:1279. doi: 10.12688/f1000research.19197.1
17. Hou R, Tomalin LE, Silva JP, Kim-Schulze S, Whitehead SS, Fernandez-Sesma A, et al. The innate immune response following multivalent dengue vaccination and implications for protection against dengue challenge. JCI Insight (2022) 7(11):e157811. doi: 10.1172/jci.insight.157811
18. Wong JM, Adams LE, Durbin AP, Muñoz-Jordán JL, Poehling KA, Sánchez-González LM, et al. Dengue: A growing problem with new interventions. Pediatrics. (2022) 149(6):e2021055522. doi: 10.1542/peds.2021-055522
19. Torres-Flores JM, Reyes-Sandoval A, Salazar MI. Dengue vaccines: An update. BioDrugs. (2022) 36(3):325–36. doi: 10.1007/s40259-022-00531-z
20. DeMaso CR, Karwal L, Zahralban-Steele M, Dominguez D, Springer ZL, Kaiser M, et al. Specificity and breadth of the neutralizing antibody response to a live attenuated tetravalent dengue vaccine. J Infect Dis (2022) 226:jiac272. doi: 10.1093/infdis/jiac272
21. Dias AG Jr, Atyeo C, Loos C, Montoya M, Roy V, Bos S, et al. Antibody fc characteristics and effector functions correlate with protection from symptomatic dengue virus type 3 infection. Sci Transl Med (2022) 14(651):eabm3151. doi: 10.1126/scitranslmed.abm3151
22. Medaglini D, Santoro F, Siegrist CA. Correlates of vaccine-induced protective immunity against Ebola virus disease. Semin Immunol (2018) 39:65–72. doi: 10.1016/j.smim.2018.07.003
23. Taleb SA, Al-Ansari K, Nasrallah GK, Elrayess MA, Al-Thani AA, Derrien-Colemyn A, et al. Level of maternal respiratory syncytial virus (RSV) f antibodies in hospitalized children and correlates of protection. Int J Infect Dis (2021) 109:56–62. doi: 10.1016/j.ijid.2021.06.015
24. Trombetta CM, Montomoli E. Influenza immunology evaluation and correlates of protection: a focus on vaccines. Expert Rev Vaccines (2016) 15(8):967–76. doi: 10.1586/14760584.2016.1164046
25. Zhou F, Hansen L, Pedersen G, Grødeland G, Cox R. Matrix m adjuvanted H5N1 vaccine elicits broadly neutralizing antibodies and neuraminidase inhibiting antibodies in humans that correlate with In vivo protection. Front Immunol (2021) 12:747774. doi: 10.3389/fimmu.2021.747774
26. Monto AS, Petrie JG, Cross RT, Johnson E, Liu M, Zhong W, et al. Antibody to influenza virus neuraminidase: An independent correlate of protection. J Infect Dis (2015) 212(8):1191–9. doi: 10.1093/infdis/jiv195
27. Petrie JG, Martin ET, Truscon R, Johnson E, Cheng CK, McSpadden EJ, et al. Evaluation of correlates of protection against influenza A(H3N2) and A(H1N1)pdm09 infection: Applications to the hospitalized patient population. Vaccine. (2019) 37(10):1284–92. doi: 10.1016/j.vaccine.2019.01.055
28. Ojal J, Hammitt LL, Gaitho J, Scott JAG, Goldblatt D. Pneumococcal conjugate vaccine induced IgG and nasopharyngeal carriage of pneumococci: Hyporesponsiveness and immune correlates of protection for carriage. Vaccine (2017) 35(35):4652–7. doi: 10.1016/j.vaccine.2017.05.088
29. Ledgerwood JE, DeZure AD, Stanley DA, Coates EE, Novik L, Enama ME, et al. Chimpanzee adenovirus vector Ebola vaccine. N Engl J Med (2017) 376(10):928–38. doi: 10.1056/NEJMoa1410863
30. Sullivan NJ, Martin JE, Graham BS, Nabel GJ. Correlates of protective immunity for Ebola vaccines: Implications for regulatory approval by the animal rule. Nat Rev Microbiol (2009) 7(5):393–400. doi: 10.1038/nrmicro2129
31. Stronsky SM, Cooper CL, Steffens J, Van Tongeren S, Bavari S, Martins KA, et al. Adjuvant selection impacts the correlates of vaccine protection against Ebola infection. Vaccine. (2020) 38(29):4601–8. doi: 10.1016/j.vaccine.2020.05.009
33. Nyamathi AM, Fahey JL, Sands H, Casillas AM. Ebola Virus: immune mechanisms of protection and vaccine development. Biol Res Nurs. (2003) 4(4):276–81. doi: 10.1177/1099800403252574
34. Walsh EE, Falsey AR, Scott DA, Gurtman A, Zareba AM, Jansen KU, et al. A randomized phase 1/2 study of a respiratory syncytial virus prefusion f vaccine. J Infect Dis (2021) 225:jiab612. doi: 10.1093/infdis/jiab612
35. Torrey HL, Kaliaperumal V, Bramhecha Y, Weir GM, Falsey AR, Walsh EE, et al. Evaluation of the protective potential of antibody and T cell responses elicited by a novel preventative vaccine towards respiratory syncytial virus small hydrophobic protein. Hum Vaccin Immunother. (2020) 16(9):2007–17. doi: 10.1080/21645515.2020.1756671
36. Foley DA, Phuong LK, Englund JA. Respiratory syncytial virus immunisation overview. J Paediatr Child Health (2020) 56(12):1865–7. doi: 10.1111/jpc.15232
37. Biagi C, Dondi A, Scarpini S, Rocca A, Vandini S, Poletti G, et al. Current state and challenges in developing respiratory syncytial virus vaccines. Vaccines (Basel). (2020) 8(4):672. doi: 10.3390/vaccines8040672
38. Mazur NI, Higgins D, Nunes MC, Melero JA, Langedijk AC, Horsley N, et al. The respiratory syncytial virus vaccine landscape: lessons from the graveyard and promising candidates. Lancet Infect Dis (2018) 18(10):e295–311. doi: 10.1016/S1473-3099(18)30292-5
39. Cox RJ. Correlates of protection to influenza virus, where do we go from here? Hum Vaccin Immunother (2013) 9(2):405–8. doi: 10.4161/hv.22908
40. Coudeville L, Bailleux F, Riche B, Megas F, Andre P, Ecochard R. Relationship between haemagglutination-inhibiting antibody titres and clinical protection against influenza: Development and application of a bayesian random-effects model. BMC Med Res Methodol (2010) 10:18. doi: 10.1186/1471-2288-10-18
41. Creytens S, Pascha MN, Ballegeer M, Saelens X, de Haan CAM. Influenza neuraminidase characteristics and potential as a vaccine target. Front Immunol (2021) 12:786617. doi: 10.3389/fimmu.2021.786617
42. McIlwain DR, Chen H, Rahil Z, Bidoki NH, Jiang S, Bjornson Z, et al. Human influenza virus challenge identifies cellular correlates of protection for oral vaccination. Cell Host Microbe (2021) 29(12):1828–1837.e5. doi: 10.1016/j.chom.2021.10.009
43. Karron RA. Preventing respiratory syncytial virus (RSV) disease in children. Science. (2021) 372(6543):686–7. doi: 10.1126/science.abf9571
44. Kulkarni PS, Hurwitz JL, Simões EAF, Piedra PA. Establishing correlates of protection for vaccine development: Considerations for the respiratory syncytial virus vaccine field. Viral Immunol (2018) 31(2):195–203. doi: 10.1089/vim.2017.0147
45. Buchwald AG, Graham BS, Traore A, Haidara FC, Chen M, Morabito K, et al. Respiratory syncytial virus (RSV) neutralizing antibodies at birth predict protection from RSV illness in infants in the first 3 months of life. Clin Infect Dis (2021) 73(11):e4421–7. doi: 10.1093/cid/ciaa648
46. Saeland E, van der Fits L, Bolder R, Heemskerk-van der Meer M, Drijver J, van Polanen Y, et al. Immunogenicity and protective efficacy of adenoviral and subunit RSV vaccines based on stabilized prefusion f protein in pre-clinical models. Vaccine (2021) 40:S0264–410X(21)01651-0. doi: 10.1016/j.vaccine.2021.12.043
47. Zohar T, Hsiao JC, Mehta N, Das J, Devadhasan A, Karpinski W, et al. Upper and lower respiratory tract correlates of protection against respiratory syncytial virus following vaccination of nonhuman primates. Cell Host Microbe (2022) 30(1):41–52.e5. doi: 10.1016/j.chom.2021.11.006
48. Phung E, Chang LA, Mukhamedova M, Yang L, Nair D, Rush SA, et al. Elicitation of pneumovirus-specific b cell responses by a prefusion-stabilized respiratory syncytial virus f subunit vaccine. Sci Transl Med (2022) 14(650):eabo5032. doi: 10.1126/scitranslmed.abo5032
49. Ruckwardt TJ, Morabito KM, Phung E, Crank MC, Costner PJ, Holman LA, et al. Safety, tolerability, and immunogenicity of the respiratory syncytial virus prefusion f subunit vaccine DS-Cav1: A phase 1, randomised, open-label, dose-escalation clinical trial. Lancet Respir Med (2021) 9(10):1111–20. doi: 10.1016/S2213-2600(21)00098-9
50. Stephens LM, Ross KA, Waldstein KA, Legge KL, McLellan JS, Narasimhan B, et al. Prefusion f-based polyanhydride nanovaccine induces both humoral and cell-mediated immunity resulting in long-lasting protection against respiratory syncytial virus. J Immunol (2021) 206(9):2122–34. doi: 10.4049/jimmunol.2100018
51. Hammitt LL, Dagan R, Yuan Y, Baca Cots M, Bosheva M, Madhi SA, et al. Nirsevimab for prevention of RSV in healthy late-preterm and term infants. N Engl J Med (2022) 386(9):837–46. doi: 10.1056/NEJMoa2110275
52. Angel J, Steele AD, Franco MA. Correlates of protection for rotavirus vaccines: Possible alternative trial endpoints, opportunities, and challenges. Hum Vaccin Immunother. (2014) 10(12):3659–71. doi: 10.4161/hv.34361
53. Pollock L, Bennett A, Jere KC, Mandolo J, Dube Q, Bar-Zeev N, et al. Plasma rotavirus-specific IgA and risk of rotavirus vaccine failure in infants in Malawi. Clin Infect Dis (2021) 75:ciab895. doi: 10.1093/cid/ciab895
54. Baker JM, Tate JE, Leon J, Haber MJ, Pitzer VE, Lopman BA. Postvaccination serum antirotavirus immunoglobulin a as a correlate of protection against rotavirus gastroenteritis across settings. J Infect Dis (2020) 222(2):309–18. doi: 10.1093/infdis/jiaa068
55. Cheuvart B, Neuzil KM, Steele AD, Cunliffe N, Madhi SA, Karkada N, et al. Association of serum anti-rotavirus immunoglobulin a antibody seropositivity and protection against severe rotavirus gastroenteritis: Analysis of clinical trials of human rotavirus vaccine. Hum Vaccin Immunother. (2014) 10(2):505–11. doi: 10.4161/hv.27097
56. Lee B, Carmolli M, Dickson DM, Colgate ER, Diehl SA, Uddin MI, et al. Rotavirus-specific immunoglobulin a responses are impaired and serve as a suboptimal correlate of protection among infants in Bangladesh. Clin Infect Dis (2018) 67(2):186–92. doi: 10.1093/cid/ciy076
57. Clarke E, Desselberger U. Correlates of protection against human rotavirus disease and the factors influencing protection in low-income settings. Mucosal Immunol (2015) 8(1):1–17. doi: 10.1038/mi.2014.114
58. Patel M, Glass RI, Jiang B, Santosham M, Lopman B, Parashar U. A systematic review of anti-rotavirus serum IgA antibody titer as a potential correlate of rotavirus vaccine efficacy. J Infect Dis (2013) 208(2):284–94. doi: 10.1093/infdis/jit166
59. Levine MM, Kotloff KL, Barry EM, Pasetti MF, Sztein MB. Clinical trials of shigella vaccines: two steps forward and one step back on a long, hard road. Nat Rev Microbiol (2007) 5(7):540–53. doi: 10.1038/nrmicro1662
60. Cohen D, Meron-Sudai S, Bialik A, Asato V, Ashkenazi S. Detoxified O-specific polysaccharide (O-SP)-Protein conjugates: Emerging approach in the Shigella vaccine development scene. Vaccines (Basel). (2022) 10(5):675. doi: 10.3390/vaccines10050675
61. MacLennan CA, Talaat KR, Kaminski RW, Cohen D, Riddle MS, Giersing BK. Critical needs in advancing shigella vaccines for global health. J Infect Dis (2022) 225(9):1500–3. doi: 10.1093/infdis/jiab462
62. Clarkson KA, Porter CK, Talaat KR, Kapulu MC, Chen WH, Frenck RW Jr, et al. Shigella-controlled human infection models: Current and future perspectives. Curr Top Microbiol Immunol (2022) 1–57. doi: 10.1007/82_2021_248
63. Herrera CM, Schmitt JS, Chowdhry EI, Riddle MS. From kiyoshi shiga to present-day shigella vaccines: A historical narrative review. Vaccines (Basel). (2022) 10(5):645. doi: 10.3390/vaccines10050645
64. Hope JC, Thom ML, McAulay M, Mead E, Vordermeier HM, Clifford D, et al. Identification of surrogates and correlates of protection in protective immunity against mycobacterium bovis infection induced in neonatal calves by vaccination with m. bovis BCG pasteur and m. bovis BCG Danish. Clin Vaccine Immunol (2011) 18(3):373–9. doi: 10.1128/CVI.00543-10
65. Darrah PA, Zeppa JJ, Maiello P, Hackney JA, Wadsworth n, Hughes TK, et al. Prevention of tuberculosis in macaques after intravenous BCG immunization. Nat (London) (2020) 577(7788):95–102. doi: 10.1038/s41586-019-1817-8
66. Counoupas C, Triccas JA, Britton WJ. Deciphering protective immunity against tuberculosis: Implications for vaccine development. Expert Rev Vaccines (2019) 18(4):353–64. doi: 10.1080/14760584.2019.1585246
67. Martinez L, Cords O, Liu Q, Acuna-Villaorduna C, Bonnet M, Fox GJ, et al. Infant BCG vaccination and risk of pulmonary and extrapulmonary tuberculosis throughout the life course: a systematic review and individual participant data meta-analysis. Lancet Glob Health (2022) 10(9):e1307–16. doi: 10.1016/S2214-109X(22)00283-2
68. Satti I, McShane H. Current approaches toward identifying a correlate of immune protection from tuberculosis. Expert Rev Vaccines (2019) 18(1):43–59. doi: 10.1080/14760584.2019.1552140
69. Abbink P, Larocca RA, Visitsunthorn K, Boyd M, de la Barrera RA, Gromowski GD, et al. Durability and correlates of vaccine protection against zika virus in rhesus monkeys. Sci Transl Med (2017) 9(420):eaao4163. doi: 10.1126/scitranslmed.aao4163
70. Young G, Bohning KJ, Zahralban-Steele M, Hather G, Tadepalli S, Mickey K, et al. Complete protection in macaques conferred by purified inactivated zika vaccine: Defining a correlate of protection. Sci Rep (2020) 10(1):3488–8. doi: 10.1038/s41598-020-60415-6
Keywords: dengue, Ebola, influenza, pneumococcal, respiratory syncytial virus, rotavirus, shigella, tuberculosis
Citation: Plotkin SA (2023) Recent updates on correlates of vaccine-induced protection. Front. Immunol. 13:1081107. doi: 10.3389/fimmu.2022.1081107
Received: 26 October 2022; Accepted: 02 December 2022;
Published: 27 January 2023.
Edited by:
Javier Castillo-Olivares, University of Cambridge, United KingdomReviewed by:
Scott B. Biering, University of California, Berkeley, United StatesCopyright © 2023 Plotkin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stanley A. Plotkin, Stanley.plotkin@vaxconsult.com
 Stanley A. Plotkin
Stanley A. Plotkin