- 1Department of Kidney Transplantation, The Second Xiangya Hospital of Central South University, Changsha, China
- 2Clinical Research Center for Organ Transplantation in Hunan Province, Changsha, China
- 3Clinical Immunology Center, Central South University, Changsha, China
- 4Department of Occupational and Environmental Health, Xiangya School of Public Health, Central South University, Changsha, China
Background: Kidney transplantation from donors who weigh ≤5 kg is performed at only a few transplant centers owing to the high complication and low graft survival rates associated with this approach.
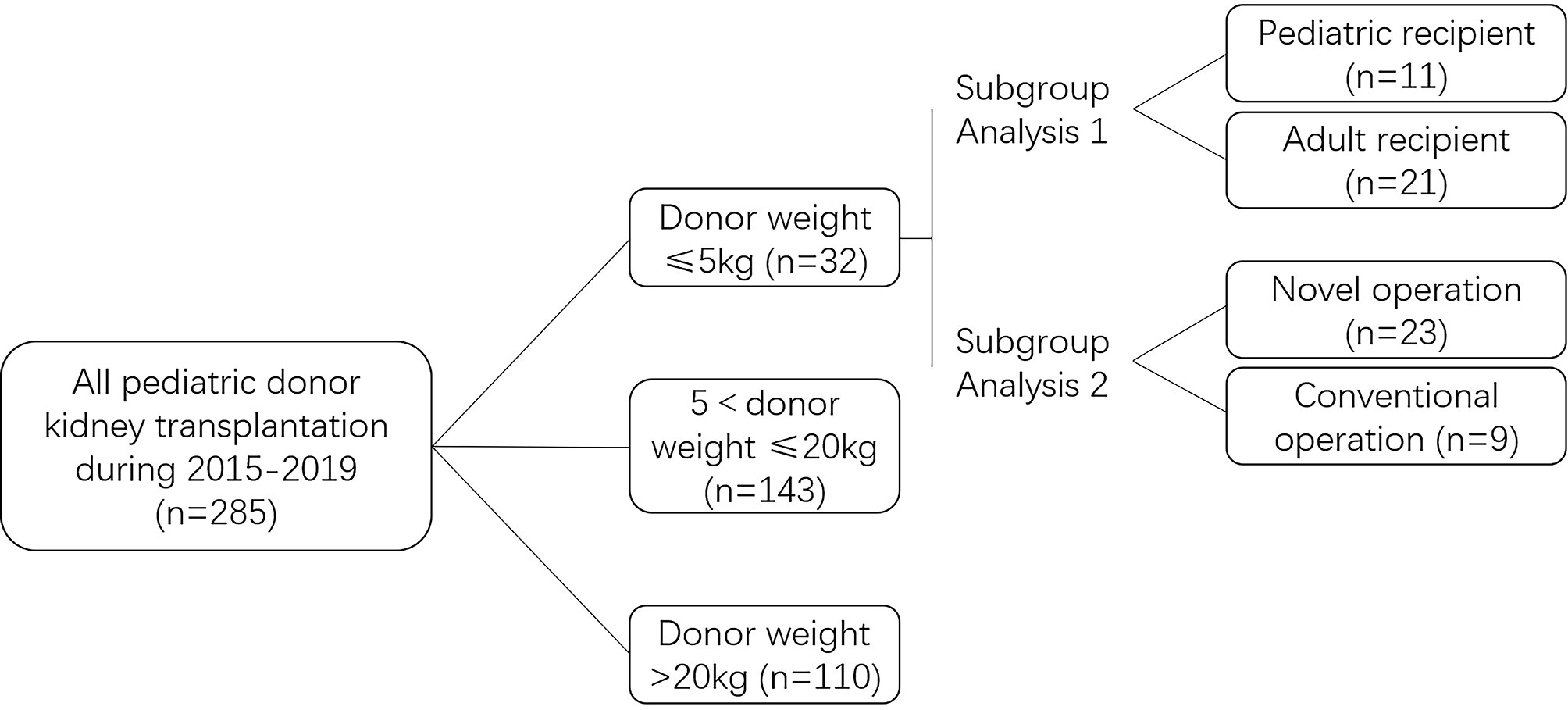
Methods: We retrospectively compared the results of kidney transplantation at our center between January 2015 and December 2019 based on the following pediatric donor criteria: donor body weight ≤5 kg (n=32), 5 kg< donor weight ≤20 kg (n=143), and donor weight >20 kg (n=110). We also perform subgroup analysis of kidney transplantation outcomes from ≤5 kg donors, using conventional (dual separate and classic en-bloc KTx)/novel (en-bloc KTx with outflow tract) surgical methods and allocating to adult/pediatric recipients.
Results: The death-censored graft survival rates from extremely low body weight ≤5kg at 1 month, and 1, 3, and 5 years were 90.6%, 80.9%, 77.5%, and 73.9%, respectively, which were significantly lower than that from larger body weight pediatric donors. However, the 3-, and 5-year post-transplantation eGFRs were not significantly different between the pediatric and adult recipient group. The thrombosis (18.8%) and urinary leakage (18.8%) rates were significantly higher in the donor weight ≤5 kg group. Compared with 5 kg< donor weight ≤20 kg group, donor weight ≤5kg group was at elevated risk of graft loss due to thrombosis (OR: 13.4) and acute rejection (OR: 6.7). No significant difference on the outcomes of extremely low body weight donor kidney transplantation was observed between adults and pediatric recipients. Urinary leakage rate is significantly lower in the novel operation (8.7%) than in the conventional operation group (44.4%).
Conclusions: Although the outcomes of donor body weight ≤5kg kidney transplantation is inferior to that from donors with large body weight, it can be improved through technical improvement. Donors with body weight ≤5 kg can be considered as an useful source to expand the donor pool.
Introduction
The number of patients diagnosed with end-stage kidney disease continues to increase worldwide, and dialysis or kidney transplantation is the therapeutic option available in such cases. Kidney transplantation, considered the treatment of choice in some patients with end-stage renal disease, is superior to dialysis with regard to patient survival and quality of life and is associated with better cognitive and mood regulation outcomes than those observed in patients who undergo dialysis (1–3). However, the demand for donor organs significantly exceeds the supply. Use of transplants from pediatric donors of extremely low body weight (≤5 kg) is viewed as a strategy to expand the donor pool.
Kidney transplantation using grafts obtained from pediatric donors of extremely low body weight is performed at only a few transplant centers, because pediatric donor kidney transplantation is associated with high rates of thrombotic and urinary tract complications, as well as acute rejection, delayed graft function (DGF), and hyperfiltration injury (4–9), particularly in cases of donors who weigh ≤5 kg (10–13). In this study, we performed an intergroup comparison of kidney transplantation outcomes based on the following pediatric donor criteria: donor body weight ≤5 kg, 5 kg< donor body weight ≤20 kg, and donor weight >20 kg. Additionally, we performed two subgroup analyses in the donor body weight ≤5 kg group, using conventional/novel surgical methods and allocating to adult/pediatric recipients.
Materials and Methods
Data Source
We retrospectively investigated 32 patients who underwent kidney transplantation using grafts obtained from infants of extremely low body weight (≤5 kg) at our center between January 2015 and December 2019 and compared our results with those in patients who received kidneys from other pediatric donors during the same period (Figure 1). The control group was classified into the following groups: 5 kg <donor body weight ≤20 kg and donor body weight >20 kg. The donor body weight ≤5 kg group was subcategorized into pediatric and adult recipient groups for subgroup analysis. Based on different surgical techniques used, the donor body weight ≤5 kg group was subcategorized into novel operation and conventional operation groups (classical en-bloc kidney transplantation and dual separating kidney transplantation) for subgroup analysis. All study procedures were approved by the Ethics Committee of the Second Xiangya Hospital of Central South University.
Donor and Recipient Selection
All donors in this study were aged <18 years. All donors in the experimental group (Group 1) weighed ≤5 kg. The control group included donors with the following body weight criteria: 5 kg <donor body weight ≤20 kg (Group 2) and donor body weight >20 kg (Group 3). All kidneys were obtained from deceased donors in accordance with the “Procedures and Standards for Organ Donation after the Death of Chinese Citizens”. The types of organ donation include DBD (donation after brain death) and DCD (donation after circulatory death). All donations were obtained after informed consent signed by guardians. All recipients were informed of the risks associated with pediatric donor kidney transplantation (14).
Surgical Technique
Classical en-bloc kidney transplantation: We performed end-to-side anastomosis of the proximal end of the donor vena cava to the recipient’s external iliac artery and end-to-side anastomosis of the proximal end of the abdominal aorta to the recipient’s common iliac or external iliac artery. The distal end of the abdominal aorta and the inferior vena cava were ligated, and the bilateral ureters were successively anastomosed to the bladder apex using the Lich-Gregoir technique (15).
Our novel technique improved the classical en-bloc kidney transplantation method using the distal abdominal aorta to establish an outflow tract (Figure 2): We performed end-to-side anastomosis of the proximal end of the donor renal inferior vena cava to the external iliac vein, and the distal end of the inferior vena cava was ligated. We performed end-to-side anastomosis of the proximal end of the aorta to the common iliac or external iliac artery and end-to-end anastomosis of the distal abdominal aorta of the donor to the inferior epigastric artery of the recipient to establish an outflow tract. The bilateral ureters were anastomosed to the recipient’s bladder (16).
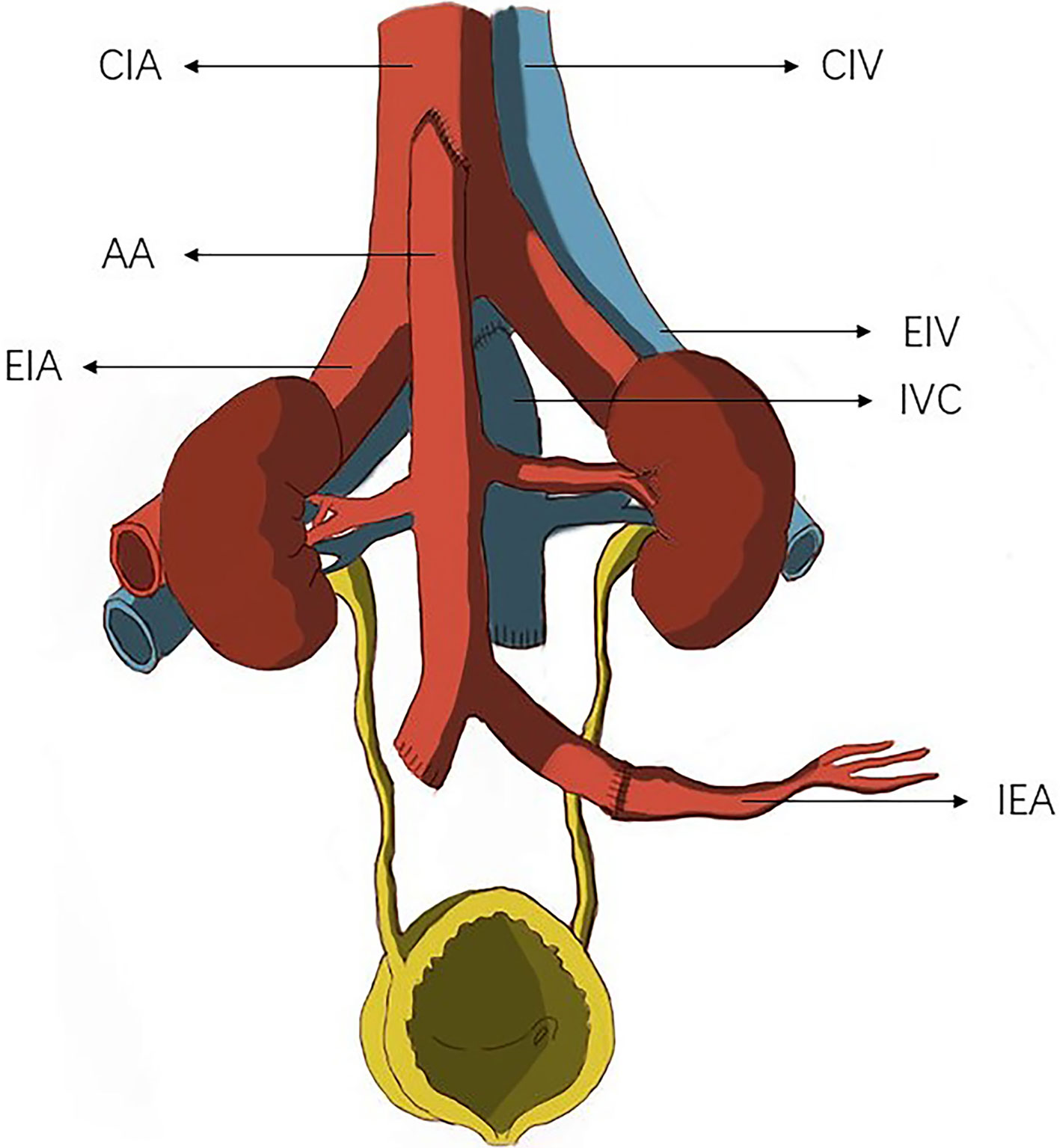
Figure 2 The donor common iliac artery or external iliac artery was anastomosed to the recipient inferior epigastric artery to establish an outflow tract. CIA, common iliac. artery; AA, abdominal aorta; EIA, external iliac artery; CIV, common iliac vein; EIV, external iliac vein; IVC, inferior vena cava; IEA, inferior epigastric artery.
Dual separating kidney transplantation: The left and right kidneys were separated and successively implanted into the ipsilateral iliac fossa. We performed end-to-side anastomosis of the renal veins of both grafts to the external iliac vein and end-to-end anastomosis of the renal artery to the internal iliac artery or end-to-side anastomosis of the renal artery to the external iliac artery. We performed end-to-side anastomosis of the renal artery of the distal graft to the external iliac artery, and the bilateral ureters were anastomosed to the bladder apex (15).
Single kidney transplantation: We performed end-to-side anastomosis of the graft renal vein to the external iliac vein, end-to-end anastomosis of the graft renal artery to the internal iliac artery or end-to-side anastomosis to the external iliac artery, based on the specific vascular conditions. The ureter was anastomosed to the bladder.
Immunosuppression
All patients received mycophenolate mofetil (MMF) (1 g) and intravenous methylprednisolone (500 mg) pre-transplantation. The dosage of Immunosuppressant drugs was reduced in some pediatric KTx recipients based on physicians’ individual experience. Antithymocyte globulin or basiliximab was used for induction therapy and tacrolimus, MMF, and methylprednisolone were administered post-transplantation. The valley concentration of tacrolimus was maintained at 7–9 ng/mL during the first 3 months and 6–8 ng/mL during the first year post-transplantation. MMF was administered as an oral dose of 0.75 g twice a day, and the MMF area under the curve was maintained at 30–60 mg · hour/L. Methylprednisolone was administered at an initial dose of 64 mg/day, which was reduced by 8 mg/day and was eventually maintained at 8–16 mg/day.
Post-Transplant Management
All patients received post-transplantation antibiotic prophylaxis against infection. Patients’ blood pressure was strictly controlled, with early systolic blood pressure maintained at 120–160 mmHg. The systolic blood pressure was maintained at levels <180 mmHg to avoid graft rupture. Anticoagulation was given to 7 out of 23 patients in novel operation group and 6 out of 9 in conventional operation group base on the surgeon’s intraoperative graft reperfusion assessment. Low-molecular-weight heparin (4100 IU) was injected subcutaneously twice a day during the first 3 days postoperatively, and this medication was switched to oral anticoagulation therapy (aspirin 100 mg/day or rivaroxaban 5 mg/day), 3 days later. Medication doses were reduced or the medication was discontinued in patients with a risk of bleeding. Double-J stents were removed a month after transplantation.
Statistical Analysis
All statistical analysis were performed using the SPSS software, version 22. Normally distributed continuous variables are expressed as means ± standard deviation and non-normally distributed continuous variables as medians (range). Quantitative data were compared using the one-way analysis of variance, Kruskal-Wallis rank sum test, Mann-Whitney U test, and the t-test. Qualitative data were analyzed using the chi-square test, and the log-rank test was used for intergroup comparison of the overall differences in survival curves. A p value <0.05 was considered statistically significant.
Results
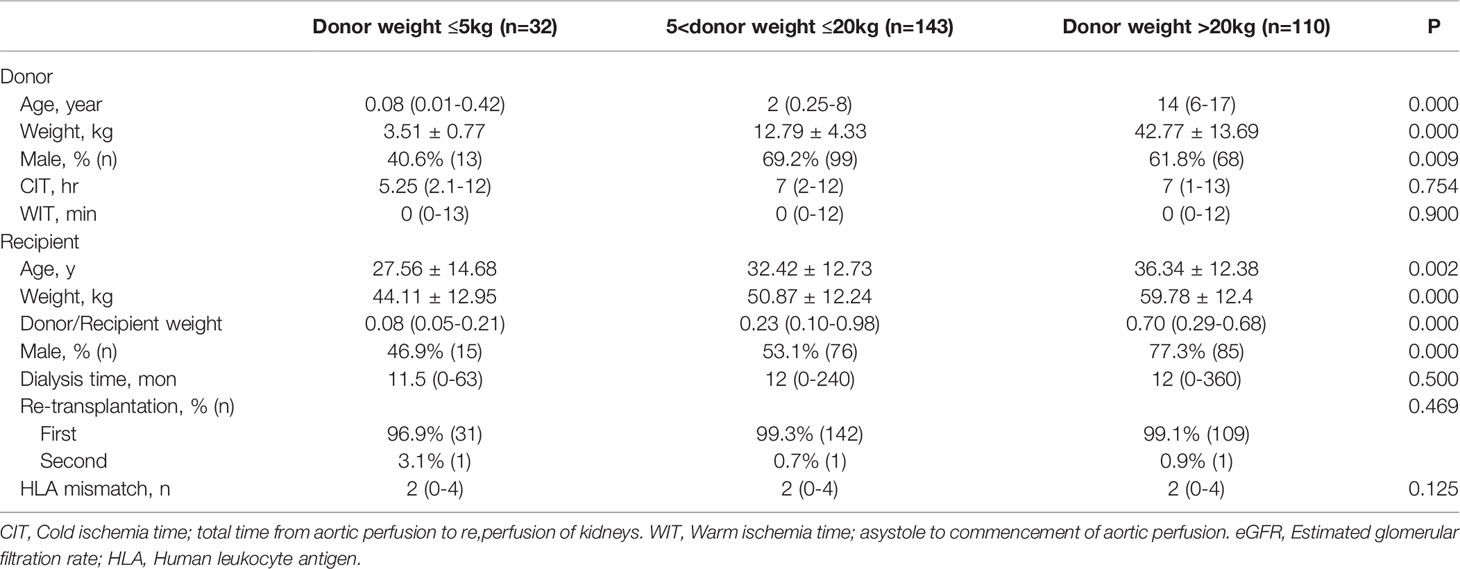
Table 1 shows the demographic data of donors and recipients. No significant intergroup differences were observed in the cold ischemia time (CIT), warm ischemia time (WIT), pre-transplantation dialysis time, re-transplantation rates, and human leukocyte antigen mismatches. The age and body weight of donors and recipients and donor/recipient weight ratio were significantly lower in Group 1 than in Groups 2 and 3. The percentage of male donors and recipients was 40.6% and 46.9%, respectively in Group 1, which were lower than the percentages in groups 2 and 3.
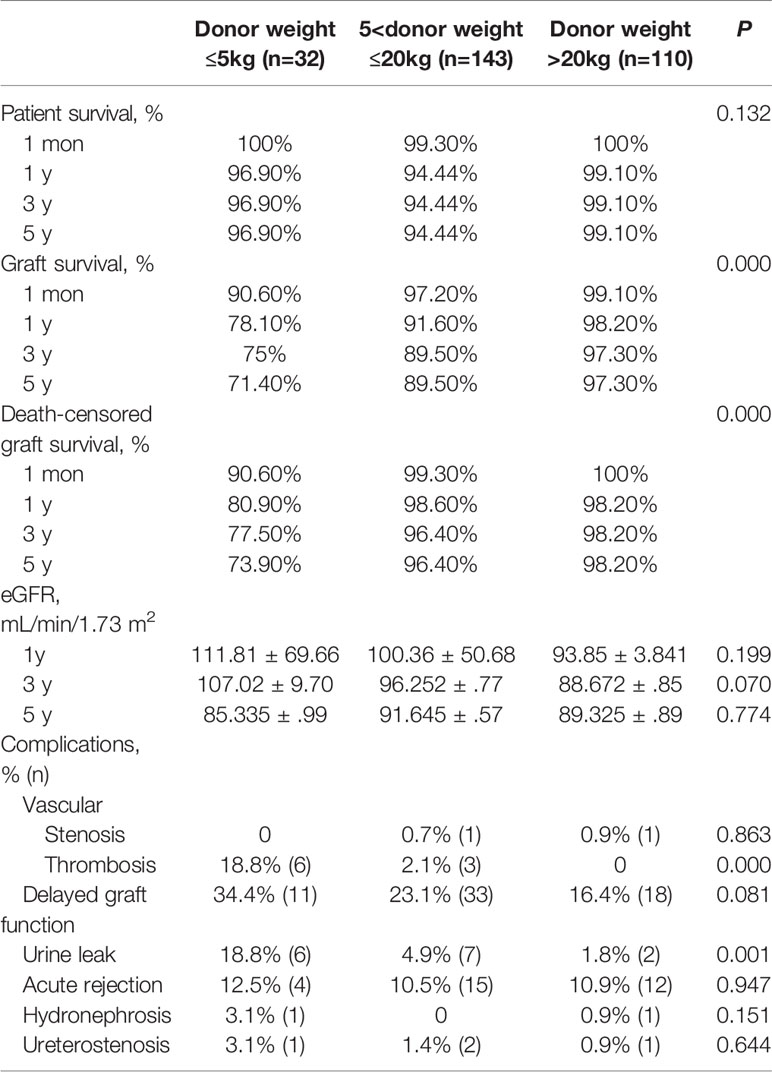
Patient survival rates at 1 month, as well as 1, 3, and 5 years were 100%, 96.9%, 96.9%, and 96.9%, respectively in Group 1, which did not significantly differ from those in Groups 2 and 3. The graft survival and death-censored graft survival rates at 1 month, as well as 1, 3, and 5 years were 90.6%, 78.1%, 75%, 71.4% and 90.6%, 80.9%, 77.5%, 73.9%, respectively in Group 1, which were significantly lower than those in Groups 2 and 3 (Table 2 and Figure 3). No significant intergroup differences were observed in the 1-, 3-, and 5-year estimated glomerular filtration rate (eGFR) (Figure 4A). The thrombosis and urinary leakage rates were significantly higher in Group 1 than in Groups 2 and 3; however, we observed no significant intergroup differences in arterial stenosis, DGF, acute rejection, hydronephrosis, and ureteral stenosis rates.
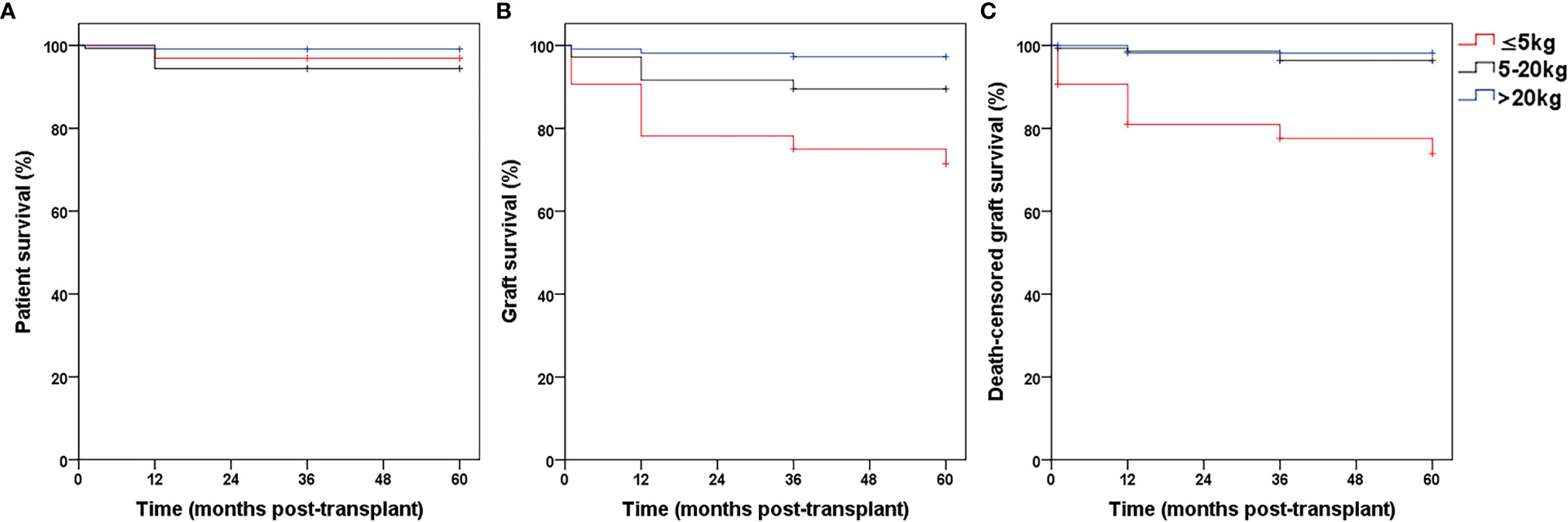
Figure 3 The patient survival (A, P > 0.05), graft survival (B, P < 0.05) and death-censored graft survival (C, P < 0.05) rates in Group 1, 2 and 3.

Figure 4 (A) The 1, 3, and 5 years eGFR in Group 1, 2 and 3, P > 0.05. (B) The 1, 3, and 5 years eGFR in Group pediatric recipients and adult recipients, P in 1 year < 0.05, P in 3 and 5 years > 0.05. (C) The 1, 3, and 5 years eGFR in Group novel operation and conventional, P > 0.05.
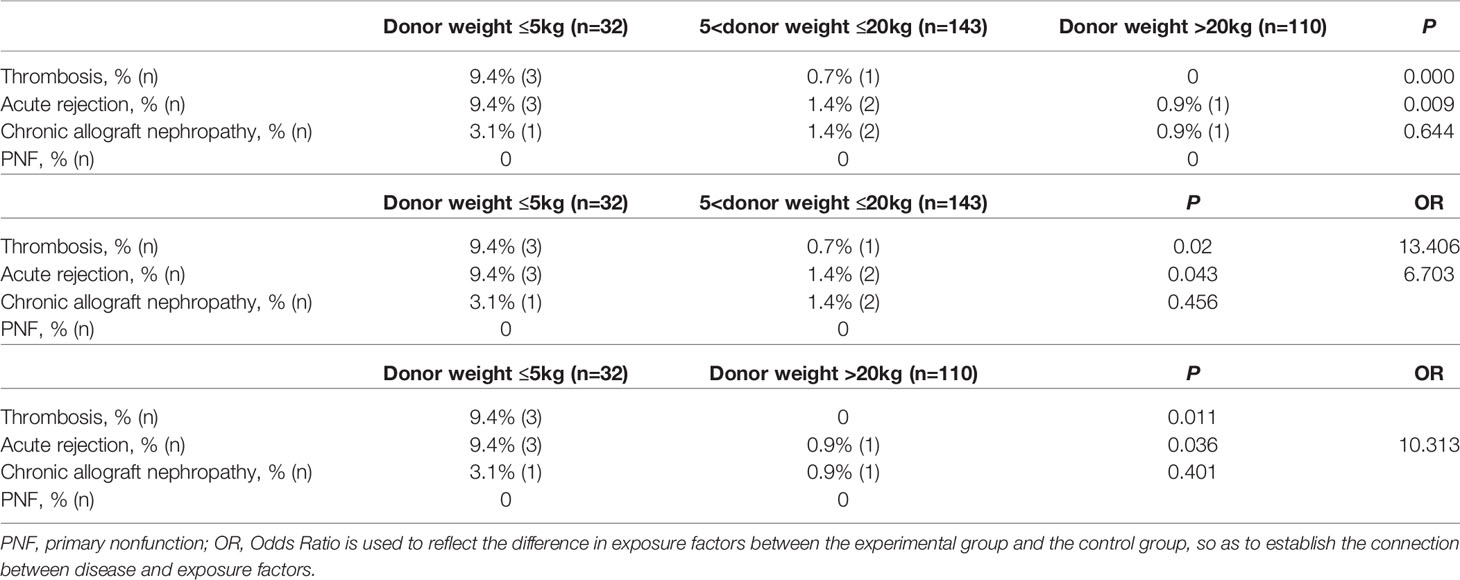
Graft loss was primarily attributable to thrombosis and acute rejection (Table 3). No significant differences in chronic allograft nephropathy and primary non function were observed between Groups 1, 2 and 3 as shown in Table 3. The odds ratio (OR) of thrombosis was 13.406-fold higher in Group 1 than in Group 2. Although no significant intergroup difference on acute rejection incidence is observed, acute rejection is inclined to cause graft loss in donor body weight ≤5kg group. The OR of acute rejection leading to graft loss was 6.703- and 10.313-fold higher in Group 1 than in Groups 2 and 3, respectively.
No significant differences were observed in age, sex, CIT and WIT of donors and sex of recipients and donor/recipient weight ratio between the pediatric recipient and adult recipient groups (Table 4). Donors’ weight was significantly lower in the pediatric recipient than in the adult recipient group due to donor/recipient body weight match principle. The patient survival, graft survival, and death-censored graft survival rates at 1 month, as well as 1, 3, and 5 years were statistically nonsignificant in the adult recipient and pediatric recipient group (Figure 5). The 1-year post-transplantation eGFR was significantly higher in the pediatric recipient than in the adult recipient group; however, the 3-, and 5-year post-transplantation eGFRs were not significantly different between these subgroups (Figure 4B). We observed no significant differences in thrombosis, DGF, urine leak, acute rejection, hydronephrosis, ureterostenosis.
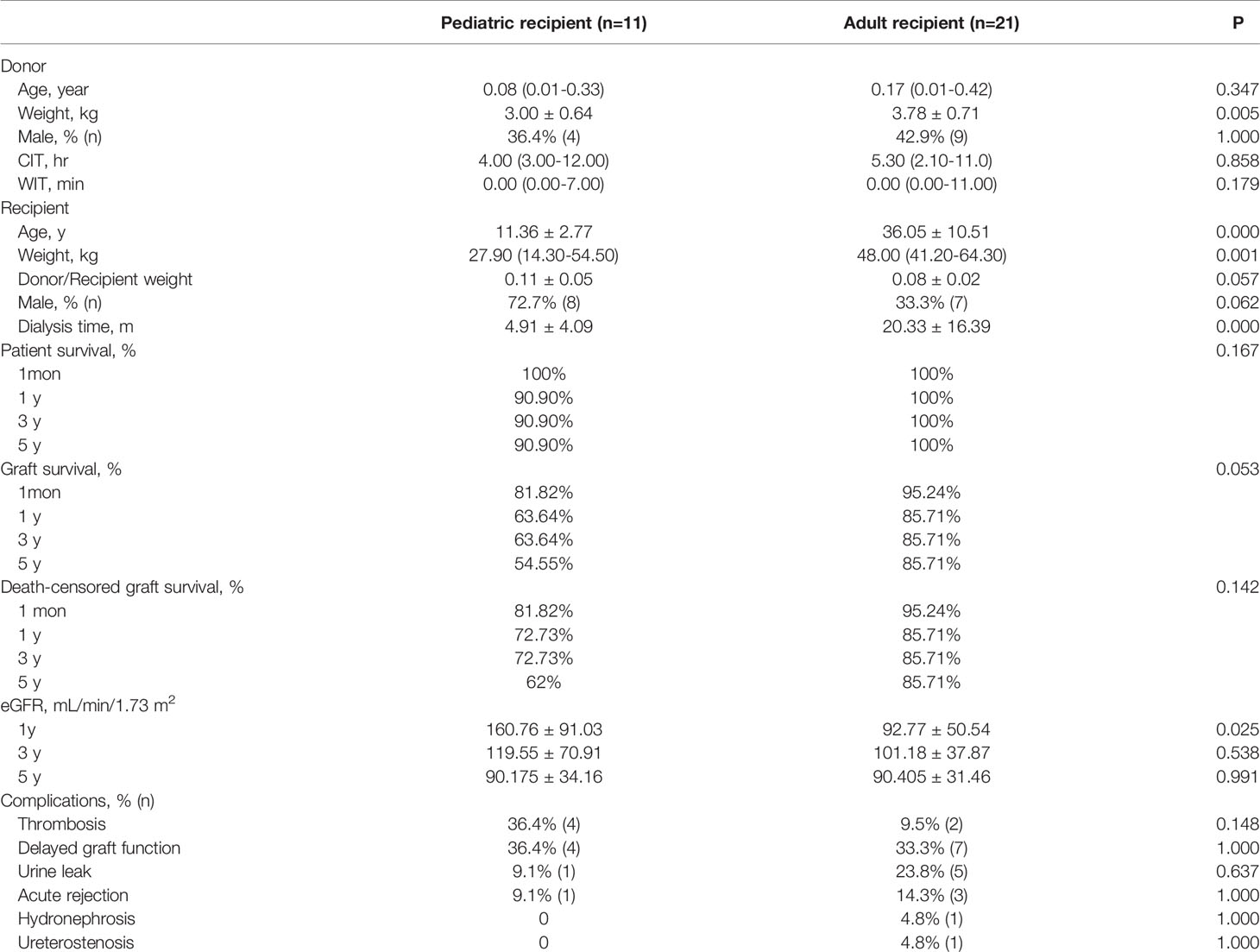
Table 4 Subgroup comparison of kidney transplantation using grafts obtained from pediatric donors of extremely low body weight with different recipients.
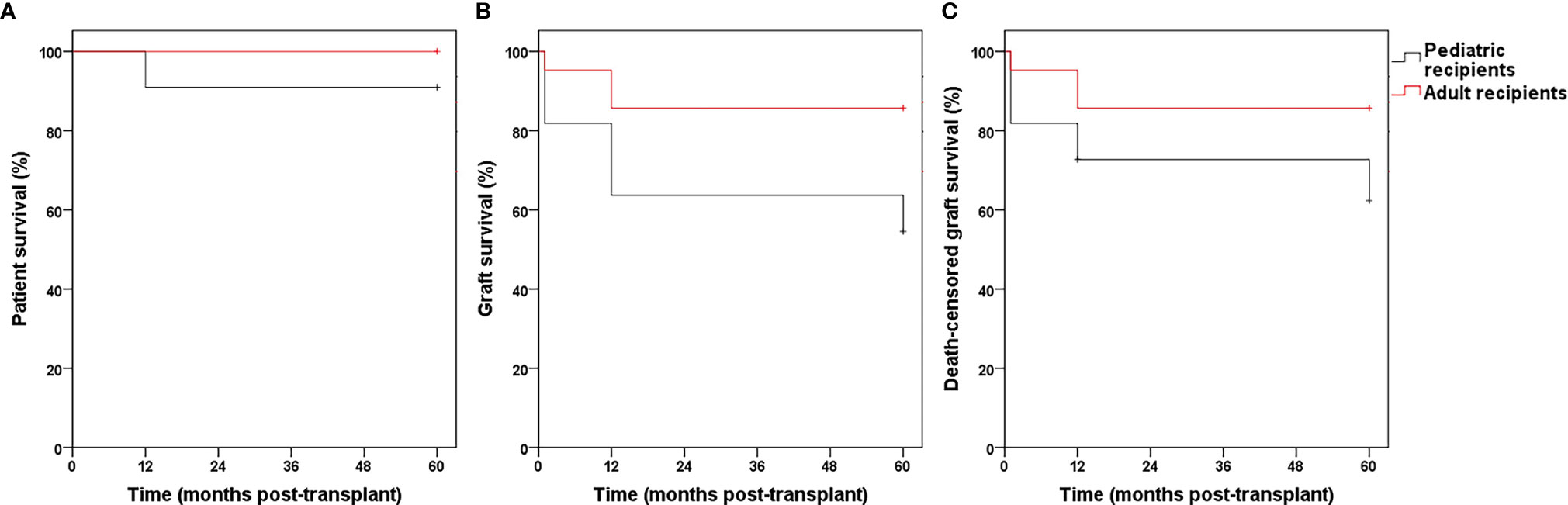
Figure 5 The patient survival (A, P > 0.05), graft survival (B, P > 0.05) and death-censored graft survival (C, P > 0.05) rates in Group pediatric recipients and adult recipients.
We observed no significant differences in donor weight and sex, as well as CIT and WIT and sex, and dialysis time of the recipients and donor/recipient weight ratio between the two subgroups (Table 5). Donor age and the age and weight of recipients were significantly lower in the novel operation than in the conventional operation group. We observed no significant intergroup differences in patient survival, graft survival, death-censored graft survival rates (Figure 6) and post-transplantation eGFR (Figure 4C). Urinary leakage rates were significantly lower in the novel operation than in the conventional operation group. The urine leakage rate in the novel operation group was 0.196-fold less than conventional operation group. The thrombosis, DGF, hydronephrosis, and ureteral stenosis rates were lower in the novel operation than in the conventional operation group; however, the difference was statistically nonsignificant. Therefore, it is reasonable to conclude that the novel operation scores over the conventional operation with regard to complication rates, although further accumulation of cases is essential to support these findings.
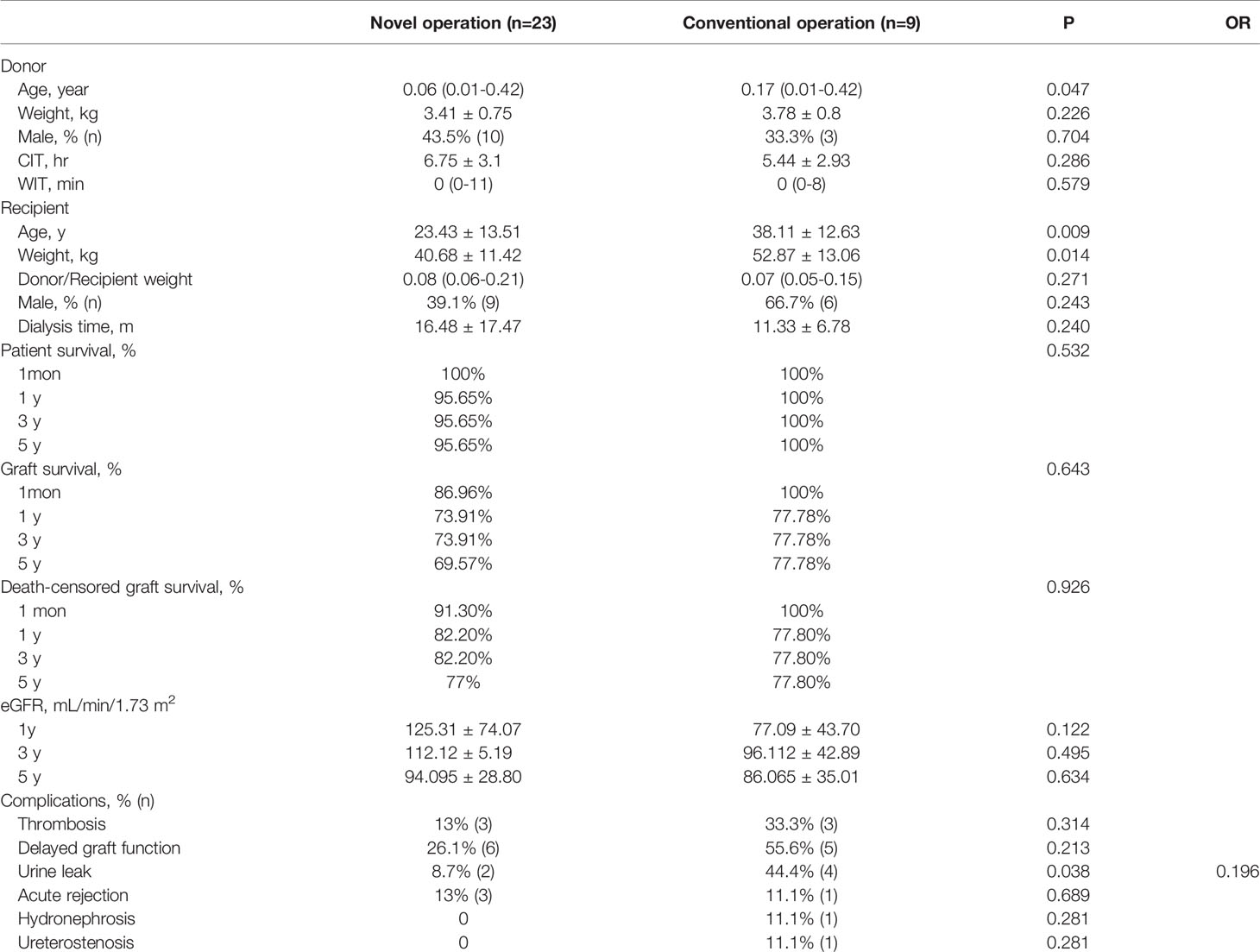
Table 5 Subgroup comparison of kidney transplantation using grafts obtained from pediatric donors of extremely low body weight with different surgical methods.
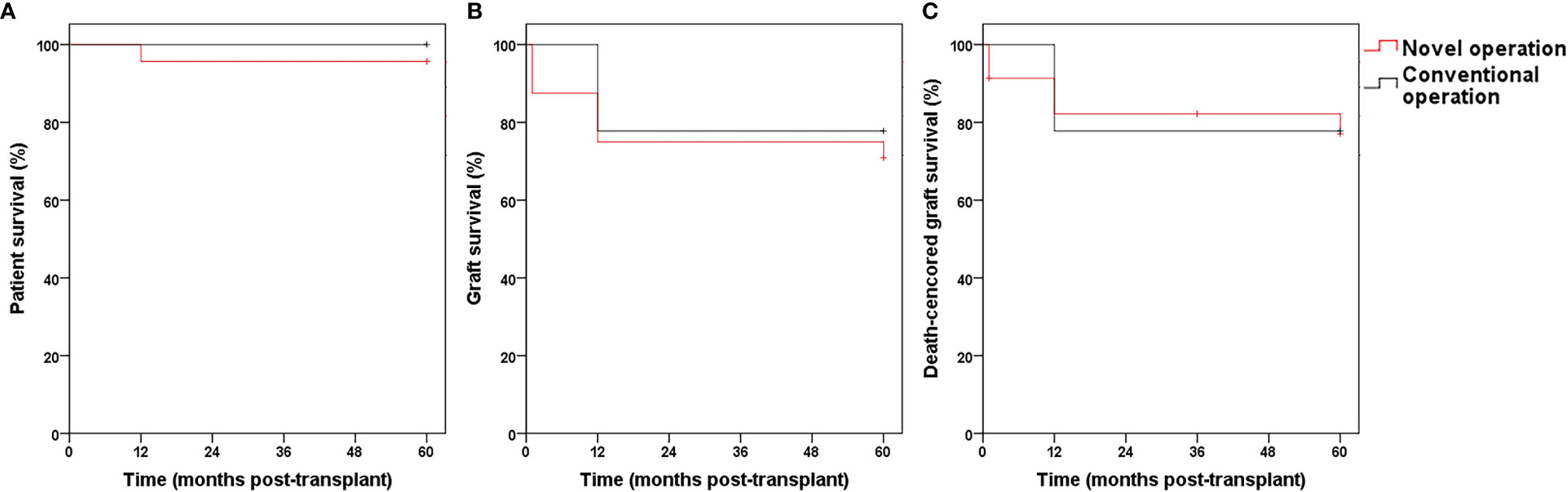
Figure 6 The patient survival (A, P >0.05), graft survival (B, P >0.05) and death-censored graft survival (C, P >0.05) rates in Group novel operation and conventional.
Discussion
The widening gap between organ demand and supply is a worldwide concern. The infant mortality rate in China is ≥1.39% (13, 17). A survey has shown that young parents are more likely to consent to organ donation, following cardiac death in an infant (13). Although this is a good source to expand the donor pool, many low body weight ≤20kg donor kidneys are discarded (18, 19) owing to the general opinion that kidneys from low body weight donors are prone to thrombotic and urinary tract complications, acute rejection, DGF, and hyperfiltration injury (4–9). However, in recent times, research centers are increasingly using small pediatric donor kidneys, which have shown similar or better short-/long-term results compared with adult donor kidneys (20–22). Sharma et al. and Sureshkumar et al. compared deceased small pediatric donor kidneys with living donor kidneys and concluded that the long-term outcomes of pediatric en-bloc kidney transplantation using grafts from deceased donors are similar to or better than those of living donor kidneys, although early thrombosis remains a challenging complication associated with pediatric en-bloc kidney transplantation (23, 24). As previously mentioned, low body weight (≤20kg) pediatric donor kidneys can be utilized safely and effectively. However, when the pediatric donor weight comes down to ≤5kg, it gets considerably trickier.
Currently only a few research centers have reported the use of kidneys from donors who weigh ≤5 kg. Wijetunga et al. performed kidney transplantation in 15 patients who received kidneys from donors who weighed ≤5 kg and observed a 1-year graft survival rate of 86.7% with thrombosis in 3 patients (20%) (12). Sui et al. performed kidney transplantation in 10 patients who received kidneys from donors who weighed ≤5 kg and observed thrombosis in 3 patients (30%). Zhao et al. performed kidney transplantation in 4 patients who received kidneys from donors who weighed ≤5 kg, and observed thrombosis in 2 patients (25%) (13). We performed kidney transplantation in 32 patients who received grafts from donors who weighed ≤5 kg (the thrombosis rate was 18.8%) and compared with those using grafts from donors who weighed 5–20 kg and donors who weighed >20 kg. The eGFR and patient survival in Group 1 was not significantly different from that observed in groups that included patients of greater body weight. However, the graft survival and death-censored graft survival rate were significantly lower in Group 1 than in Groups 2 and 3, and the thrombosis and urinary leakage rates were significantly higher in Group 1 than in Groups 2 and 3, which may be attributable to the long learning curve of kidney transplantation surgery using organs from infants of extremely low body weight, the fact that we did not select the appropriate surgical methods during the early stages, and smaller blood vessels may have predisposed patients to thrombosis and graft loss.
Some research centers recommend that pediatric donor kidneys primarily be used in children and this practice is associated with favorable outcomes (5, 23, 25–28). However, others are of the view that pediatric donor kidneys should primarily be used in adult recipients (29–32). This recommendation is based on the fact that the total number of nephrons in the kidney (approximately 1 million) is determined in utero, and no new nephrons are formed after 36 weeks of gestation (33); therefore, the number of renal units in pediatric donor kidneys is the same as those in adult donor kidneys, with a difference only in their size. Based on an individual’s requirements, a pediatric donor kidney shows compensatory hypertrophy after transplantation in an adult, whereas the pediatric donor kidney tends to grow slowly in pediatric recipients (6, 28, 34–36). We observed that 1month, as well as 1, 3, and 5 years post-transplantation patient survival, graft survival, and death-censored graft survival rates were statistically nonsignificant between pediatric and adult recipients. Although the 1-year post-transplantation eGFR was significantly higher in the pediatric recipient than in the adult recipient group, no significant intergroup differences was observed at 3 and 5 years, which may be attributable to dynamic renal function and recipient body weight change. We observed no significant intergroup differences in the complications rates. This observation indicates no difference between adult and pediatric recipients using kidneys obtained from extremely low body weight donors.
Based on lessons learned from previous failures, we did not perform dual separating kidney transplantation in cases of kidneys obtained from donors with body weight ≤5 kg and also adopted an improved surgical technique of en-bloc kidney transplantation during which the distal abdominal aorta was used as the outflow tract and was anastomosed to the external iliac or inferior epigastric artery of the recipient, thereby minimizing the risk of thrombosis and postoperative bleeding without the administration of conventional anticoagulants postoperatively (16, 37). We also modified the operative procedure and protected the arterial sheath of the transplanted kidney based on the following rationale: (a) The graft artery wall receives a part of its blood supply from the vascular sheath. Complete separation of the renal artery sheath may cause ischemic contracture of the renal artery wall. (b) It is important to maintain the integrity of the graft renal artery sheath to ensure adequate blood supply for the growth of the renal artery and to improve the quantity of antibiotics delivered to the renal vascular wall to prevent infection-induced vascular rupture. (c) The graft artery sheath supports small renal vessels and prevents distortion and angling of the graft artery.
We categorized the donor weight ≤5 kg group into the novel operation and conventional operation subgroups (including en-bloc kidney and dual separating kidney transplantation). The thrombosis, DGF, hydronephrosis, and ureteral stenosis rates were lower in the novel operation than in the conventional operation group; however, the difference was statistically nonsignificant. The urine leak rate was significantly lower in the novel operation than in the conventional operation group, without any significant intergroup differences in patient survival, graft survival, and death-censored graft survival rates which might attribute to the fact that during back- table graft preparation tissue surrounding ureter has been well conserved for better ureter blood supply. This suggests that the novel operation offers certain advantages over the conventional operative approach.
In our opinion, the results of the novel transplantation method described in our study are replicable and may be further improved over time; however, large-scale studies with long-term follow-up are warranted to validate our results. In this study, the lowest weight of donors was 1.9 kg and the kidneys of which are transplanted to a 12-years-old male child with the novel surgery method. Thus far this recipient has been followed up for 5 years with the kidney allograft functioning. We intend to perform further research with large-scale studies that include longer follow-up to investigate graft allocation policies, graft growth, blood pressure control, immune suppression, and other relevant issues in this domain.
Conclusion
To summarize, graft survival rates of kidney transplantation using kidneys from donors of extremely low body weight ≤5kg were lower than those from donors of greater body weight. However, renal function was unaffected by differences in donor body weight. Donor body weight ≤5kg group is at elevated risk of graft loss caused by thrombosis and acute rejection. In our view, the outcome of extremely low body weight donor kidney transplantation is independent of whether the recipient is adult or child. And the novel operation mentioned in this study may also reduce complication rates. Although there are still many challenges in kidney transplantation of donor body weight ≤5kg, it can be improved through technical improvement such as the novel operation proposed by our center. In conclusion, donors with body weight ≤5 kg can be considered as an useful source to expand the donor pool to enable treatment of a larger number of patients with end-stage renal disease.
Data Availability Statement
The datasets presented in this article are not readily available because of participants identifiable data. Requests to access the datasets should be directed to Longkai Peng, cGVuZ2xvbmdrYWlAY3N1LmVkdS5jbg==.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Second Xiangya Hospital of Central South University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JP drafted the manuscript. JP, MZ, ZT, TL, SS, HY, and JH collected data. RH designed statistical method. JP and MZ generated the figures. LP, XX, SY, FP, GL, YW, and XT performed the surgery. SY revised the manuscript. LP, HD, and HZ designed the outline of the manuscript and revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work is supported by the National Science Foundation of China (82070776, 81900370, 81800664 and 81970655), Excellent Youth Foundation of Hunan Province of China (2021JJ10076) and Huxiang Young Talents of Hunan Province (2019RS2013).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ozcan H, Yucel A, Avsar UZ, Cankaya E, Yucel N, Gozubuyuk H, et al. Kidney Transplantation Is Superior to Hemodialysis and Peritoneal Dialysis in Terms of Cognitive Function, Anxiety, and Depression Symptoms in Chronic Kidney Disease. Transplant Proc (2015) 47(5):1348–51. doi: 10.1016/j.transproceed.2015.04.032
2. Zhang Y, Gerdtham U-G, Rydell H, Jarl J. Quantifying the Treatment Effect of Kidney Transplantation Relative to Dialysis on Survival Time: New Results Based on Propensity Score Weighting and Longitudinal Observational Data From Sweden. Int J Environ Res Public Health (2020) 17(19):7318. doi: 10.3390/ijerph17197318
3. Yoo KD, Kim CT, Kim M-H, Noh J, Kim G, Kim H, et al. Superior Outcomes of Kidney Transplantation Compared With Dialysis. Medicine (2016) 95(33):e4352. doi: 10.1097/MD.0000000000004352
4. Sharma A, Ramanathan R, Behnke M, Fisher R, Posner MJT. Single Pediatric Kidney Transplantation in Adult Recipients: Comparable Outcomes With Standard-Criteria Deceased-Donor Kidney Transplantation. Transplantation (2013) 95(11):1354–9. doi: 10.1097/TP.0b013e31828a9493
5. Sui M, Zhao W, Chen Y, Zhu F, Zhu Y, Zeng L, et al. Optimizing the Utilization of Kidneys From Small Pediatric Deceased Donors Under 15 Kg by Choosing Pediatric Recipients. Pediatr Transplant (2016) 20(1):39–43. doi: 10.1111/petr.12645
6. Mitrou N, Aquil S, Dion M, McAlister V, Sener A, Luke P, et al. Transplantation of Pediatric Renal Allografts From Donors Less Than 10 Kg. Am J Transplant (2018) 18(11):2689–94. doi: 10.1111/ajt.14946
7. Fananapazir G, Tse G, Di Geronimo R, McVicar J, Perez R, Santhanakrishnan C, et al. Urologic Complications After Transplantation of 225 En Bloc Kidneys From Small Pediatric Donors ≤20 Kg: Incidence, Management, and Impact on Graft Survival. Am J Transplant (2020) 20(8):2126–32. doi: 10.1111/ajt.15792
8. Zhu L, Fu C, Chen S, Liu B, Du D, Chang S, et al. Successful Single-Kidney Transplantation in Adult Recipients Using Pediatric Donors Aged 8 to 36 Months: Comparable Outcomes With Those Using Pediatric Donors Aged >3 Years. Transplantation (2019) 103(11):2388–96. doi: 10.1097/TP.0000000000002618
9. Balachandran V, Aull M, Goris M, Figueiro J, Leeser D, Kapur SJT. Successful Transplantation of Single Kidneys From Pediatric Donors Weighing Less Than or Equal to 10 Kg Into Standard Weight Adult Recipients. Transplantation (2010) 90(5):518–22. doi: 10.1097/TP.0b013e3181e98d35
10. Bent C, Fananapazir G, Tse G, Corwin M, Vu C, Santhanakrishnan C, et al. Graft Arterial Stenosis in Kidney En Bloc Grafts From Very Small Pediatric Donors: Incidence, Timing, and Role of Ultrasound in Screening. Am J Transplant (2015) 15(11):2940–6. doi: 10.1111/ajt.13365
11. Fananapazir G, Tse G, Corwin M, Santhanakrishnan C, Perez R, McGahan J, et al. Pediatric En Bloc Kidney Transplants: Clinical and Immediate Postoperative US Factors Associated With Vascular Thrombosis. Radiology (2016) 279(3):935–42. doi: 10.1148/radiol.2015150430
12. Wijetunga I, Ecuyer C, Martinez-Lopez S, Jameel M, Baker RJ, Welberry Smith M, et al. Renal Transplant From Infant and Neonatal Donors Is a Feasible Option for the Treatment of End-Stage Renal Disease But Is Associated With Increased Early Graft Loss. Am J Transplant (2018) 18(11):2679–88. doi: 10.1111/ajt.15006
13. Zhao W, Zhang L, Zhu Y, Chen Y, Zhu F, Shen Q, et al. En Bloc Kidneys Transplanted From Infant Donors Less Than 5 Kg Into Pediatric Recipients. Transplantation (2014) 97(5):555–8. doi: 10.1097/01.tp.0000437174.55798.0b
14. Peng F, Yu S, Peng L, Xie X, Gao C, Tan L, et al. Transplantation of En Bloc Kidneys From Cardiac Deceased Small Pediatric Donors: 2 Case Reports and Literature Review. Zhong Nan Da Xue Xue Bao Yi Xue Ban (2014) 39(2):204–8. doi: 10.11817/j.issn.1672-7347.2014.02.017
15. Yu SJ, Liu HC, Song L, Dai HL, Peng FH, Peng LK. Dual Kidney Transplantation From Pediatric Donors to Adult Recipients. Transplant Proc (2015) 47(6):1727–31. doi: 10.1016/j.transproceed.2015.04.100
16. Dai H, Peng L, Peng F, Lan G, Wang Y, Chen J, et al. A Novel Technique for En Bloc Kidney Transplantation From Infant Donors With Extremely Low Body Weight by Using the Distal Abdominal Aorta as an Outflow Tract. Am J Transplant (2018) 18(9):2200–7. doi: 10.1111/ajt.14692
17. Xu Y, Zhang W, Yang R, Zou C, Zhao Z. Infant Mortality and Life Expectancy in China. Med Sci Monit (2014) 20:379–85. doi: 10.12659/MSM.890204
18. Maluf DG, Carrico RJ, Rosendale JD, Perez RV, Feng S. Optimizing Recovery, Utilization and Transplantation Outcomes for Kidneys From Small, ≤20 Kg, Pediatric Donors. Am J Transplant (2013) 13(10):2703–12. doi: 10.1111/ajt.12410
19. Pelletier S, Guidinger M, Merion R, Englesbe M, Wolfe R, Magee J, et al. Recovery and Utilization of Deceased Donor Kidneys From Small Pediatric Donors. Am J Transplant (2006) 6(7):1646–52. doi: 10.1111/j.1600-6143.2006.01353.x
20. Sanchez-Fructuoso AI, Prats D, Perez-Contin MJ, Marques M, Torrente J, Conesa J, et al. Increasing the Donor Pool Using En Bloc Pediatric Kidneys for Transplant. Transplantation (2003) 76(8):1180–4. doi: 10.1097/01.TP.0000090395.98045.09
21. Thomusch O, Tittelbach-Helmrich D, Meyer S, Drognitz O, Pisarski P. Twenty-Year Graft Survival and Graft Function Analysis by a Matched Pair Study Between Pediatric En Bloc Kidney and Deceased Adult Donors Grafts. Transplantation (2009) 88(7):920–5. doi: 10.1097/TP.0b013e3181b74e84
22. Merkel F. Five and 10 Year Follow-Up of En Bloc Small Pediatric Kidneys in Adult Recipients. Transplant Proc (2001) 33:1168–9. doi: 10.1016/S0041-1345(00)02446-5
23. Sharma A, Fisher R, Cotterell A, King A, Maluf D, Posner MJT. En Bloc Kidney Transplantation From Pediatric Donors: Comparable Outcomes With Living Donor Kidney Transplantation. Transplantation (2011) 92(5):564–9. doi: 10.1097/TP.0b013e3182279107
24. Sureshkumar K, Reddy C, Nghiem D, Sandroni S, Carpenter BJT. Superiority of Pediatric En Bloc Renal Allografts Over Living Donor Kidneys: A Long-Term Functional Study. Transplantation (2006) 82(3):348–53. doi: 10.1097/01.tp.0000228872.89572.d3
25. Dubourg L, Cochat P, Hadj-Aïssa A, Tydén G, Berg U. Better Long-Term Functional Adaptation to the Child's Size With Pediatric Compared to Adult Kidney Donors. Kidney Int (2002) 62(4):1454–60. doi: 10.1111/j.1523-1755.2002.kid576.x
26. Afanetti M, Niaudet P, Niel O, Saint Faust M, Cochat P, Berard E. Pediatric En Bloc Kidney Transplantation Into Pediatric Recipients: The French Experience. Pediatr Transplant (2012) 16(2):183–6. doi: 10.1111/j.1399-3046.2012.01654.x
27. Pape L, Hoppe J, Becker T, Ehrich J, Neipp M, Ahlenstiel T, et al. Superior Long-Term Graft Function and Better Growth of Grafts in Children Receiving Kidneys From Paediatric Compared With Adult Donors. Nephrol Dial Transplant (2006) 21(9):2596–600. doi: 10.1093/ndt/gfl119
28. Wang H, Li J, Liu L, Deng R, Fu Q, Ko D, et al. En Bloc Kidney Transplantation From Infant Donors Younger Than 10 Months Into Pediatric Recipients. Pediatr Transplant (2017) 21(2):e12845. doi: 10.1111/petr.12845
29. Dharnidharka V, Fiorina P, Harmon WE. Kidney Transplantation in Children. N Engl J Med (2014) 371(6):549–58. doi: 10.1056/NEJMra1314376
30. Singh A, Stablein D, Tejani AJT. Risk Factors for Vascular Thrombosis in Pediatric Renal Transplantation: A Special Report of the North American Pediatric Renal Transplant Cooperative Study. Transplantation (1997) 63(9):1263–7. doi: 10.1097/00007890-199705150-00012
31. Kayler L, Magliocca J, Kim R, Howard R, Schold J. Single Kidney Transplantation From Young Pediatric Donors in the United States. Am J Transplant (2009) 9(12):2745–51. doi: 10.1111/j.1600-6143.2009.02809.x
32. El-Sheikh M, Gok M, Buckley P, Soomro N, Jacques B, Manas D, et al. En Bloc Pediatric Into Adult Recipients: The Newcastle Experience. Transplant Proc (2003) 35(2):786–8. doi: 10.1016/S0041-1345(03)00044-7
33. Hinchliffe S, Sargent P, Howard C, Chan Y, van Velzen D. Human Intrauterine Renal Growth Expressed in Absolute Number of Glomeruli Assessed by the Disector Method and Cavalieri Principle. Lab Invest (1991) 64(6):777–84. doi: 10.1121/1.400690
34. Wang Y, Lv J, Xie W, Huang H, Peng W, Wu J, et al. Outcome of Single Kidney Transplant From Pediatric Donors Younger Than 5 Years of Age After Cardiac Death in China: A Single Center Experience. Exp Clin Transplant (2015) 13(3):239–42. doi: 10.6002/ect.2014.0177
35. Uemura T, Liang J, Khan A, Kwon O, Ghahramani N, Wang L, et al. Outcomes of Transplantation of Single Pediatric Renal Allografts Equal to or More Than 6 Cm in Length. Transplantation (2010) 89(6):710–3. doi: 10.1097/TP.0b013e3181c90226
36. Mohanka R, Basu A, Shapiro R, Kayler LJT. Single Versus En Bloc Kidney Transplantation From Pediatric Donors Less Than or Equal to 15 Kg. Transplantation (2008) 86(2):264–8. doi: 10.1097/TP.0b013e318177894e
Keywords: center experience, kidney transplantation, extremely low body weight, pediatric donor, graft survival, utilization
Citation: Peng J, Dai H, Zhang H, Yu S, Xie X, Peng F, Lan G, Hu S, Wang Y, Tang X, Guo Y, Gao C, Fang C, Nie M, Yuan X, Zhong M, Tang Z, Li T, Sun S, Yao H, Hou J, Huang R and Peng L (2021) Comparison of Outcomes of Kidney Transplantation From Extremely Low Body Weight ≤5kg Versus Larger Body Weight Pediatric Donors. Front. Immunol. 12:738749. doi: 10.3389/fimmu.2021.738749
Received: 09 July 2021; Accepted: 16 August 2021;
Published: 31 August 2021.
Edited by:
Zhenhua Dai, Guangdong Provincial Academy of Chinese Medical Sciences, ChinaReviewed by:
Zhangfei Shou, Shulan Hangzhou Hospital, ChinaLongshan Liu, Sun Yat-sen University, China
Copyright © 2021 Peng, Dai, Zhang, Yu, Xie, Peng, Lan, Hu, Wang, Tang, Guo, Gao, Fang, Nie, Yuan, Zhong, Tang, Li, Sun, Yao, Hou, Huang and Peng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Longkai Peng, cGVuZ2xvbmdrYWlAY3N1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Jiawei Peng1,2†
Jiawei Peng1,2† Helong Dai
Helong Dai Hedong Zhang
Hedong Zhang Xubiao Xie
Xubiao Xie Yong Guo
Yong Guo Ruixue Huang
Ruixue Huang