- 1Department of Hematology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China
- 2Department of Hematology, Southwest Hospital, Third Military Medical University (Army Medical University), Chongqing, China
Haploidentical stem cell transplantation (haploSCT) has advanced to a common procedure for treating patients with hematological malignancies and immunodeficiency diseases. However, cure is seriously hampered by cytomegalovirus (CMV) infections and delayed immune reconstitution for the majority of haploidentical transplant recipients compared to HLA-matched stem cell transplantation. Three major approaches, including in vivo T-cell depletion (TCD) using antithymocyte globulin for haploSCT (in vivo TCD-haploSCT), ex vivo TCD using CD34 + positive selection for haploSCT (ex vivo TCD-haploSCT), and T-cell replete haploSCT using posttransplant cyclophosphamide (PTCy-haploSCT), are currently used worldwide. We provide an update on CMV infection and CMV-specific immune recovery in this fast-evolving field. The progress made in cellular immunotherapy of CMV infection after haploSCT is also addressed. Groundwork has been prepared for the creation of personalized avenues to enhance immune reconstitution and decrease the incidence of CMV infection after haploSCT.
Introduction
HLA-haploidentical stem cell transplantation (haploSCT) has spread rapidly worldwide in recent years. HLA-haploidentical donors sharing a single HLA haplotype with transplant recipients are almost always available, so haploSCT can be performed for patients who are lacking HLA-matched donors and/or are urgently needing transplantation. The major approaches for T-cell depletion are in vivo T-cell depletion using antithymocyte globulin (ATG) (in vivo TCD-haploSCT), ex vivo T-cell depletion (TCD) using CD34 + positive selection (ex vivo TCD-haploSCT), and T-cell replete haploSCT using posttransplant cyclophosphamide (PTCy-haploSCT). Compared with HLA-identical sibling transplantation, patients undergoing haploSCT usually receive more intensive immunosuppressors to guarantee engraftment and later prevent graft-versus-host disease (GVHD). Therefore, these patients always have impaired immune reconstitution after transplantation and a high incidence of CMV infection and CMV disease (Figure 1). As the use of haploidentical transplantation has increased substantially, we summarize current data on CMV infection and its immune reconstitution after haploSCT during the last decade.
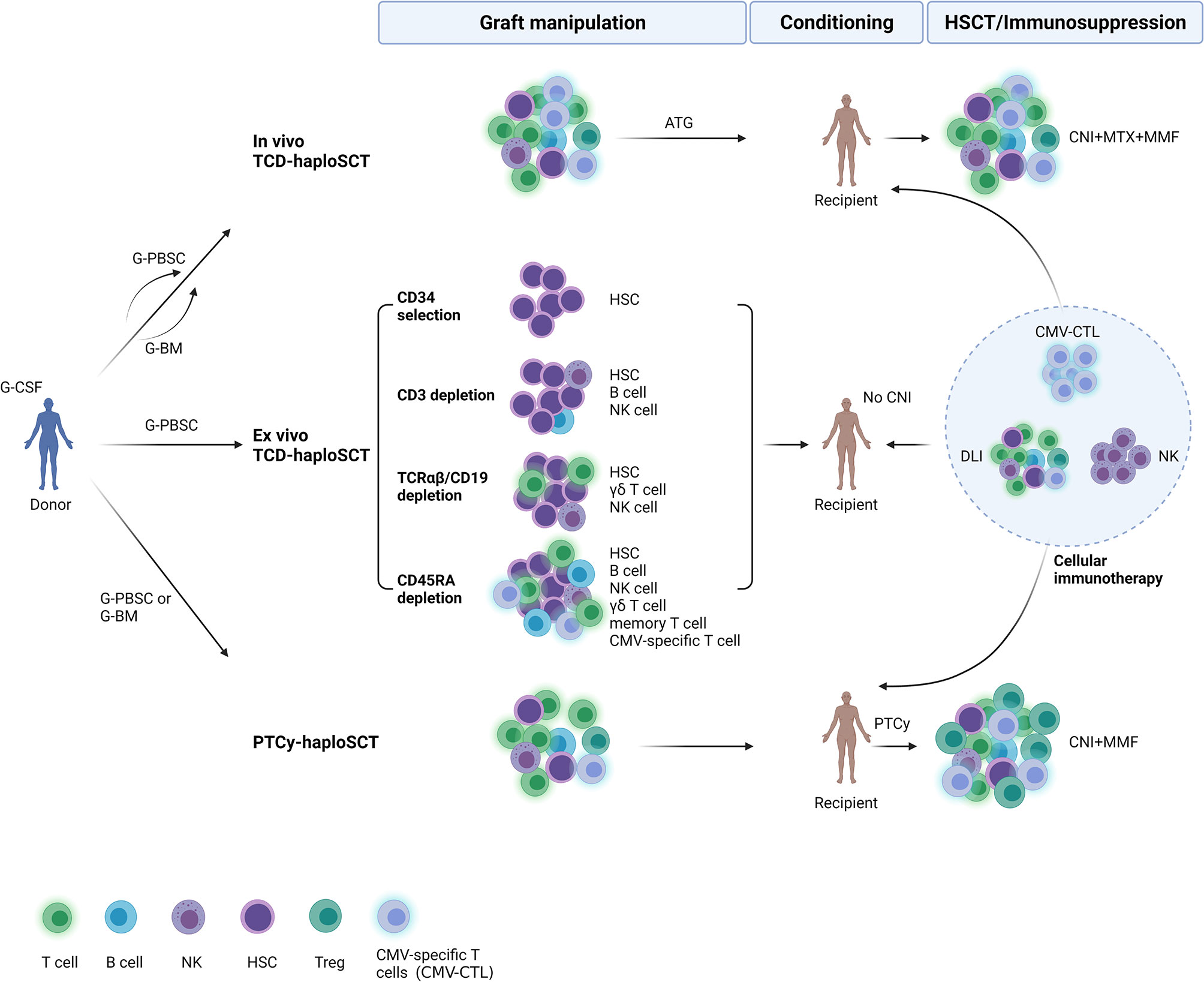
Figure 1 Overview of immune reconstitution to cytomegalovirus and cellular immunotherapy after three major approaches of haploidentical stem cell transplantation (haploSCT). In vivo TCD-haploSCT, in vivo T-cell depletion (TCD) using antithymocyte globulin for haploSCT; Ex vivo TCD-haploSCT, ex vivo TCD using CD34 + positive selection for haploSCT; PTCy-haploSCT, T-cell replete haploSCT using posttransplant cyclophosphamide. G-CSF, granulocyte-colony stimulating factor; G-PBSC, G-CSF primed peripheral blood stem cells; G-BM, G-CSF primed bone marrow; HSC, hematopoietic stem cell; CMV, cytomegalovirus; CNI, calcineurin inhibitors; MTX, methotrexate; MMF, mycophenolate mofetil; DLI, donor lymphocyte infusion; NK cell, natural killer cell; Treg, regulatory T cell; HSCT, hematopoietic stem cell transplantation. Created with BioRender (https://biorender.com/).
Incidence of Cytomegalovirus Infection After haploSCT
In Vivo TCD-haploSCT (Anti-Thymocytic Globulin/ATG-Based)
Using the Beijing protocol at Peking University (1–7), there was a high incidence of CMV reactivation early after haploSCT (59.5-66%), whereas the rate of CMV disease was actually low (2.92-17%). CMV DNAemia was initially detected after a median of 35 days with a mean duration of positivity of 15 days (5, 6). Most (91.2%) cases of CMV gastroenteritis developed within 100 days, whereas most (90.3%) cases of CMV retinitis were late onset with the cumulative incidence of CMV retinitis at 2.3% one year (a median onset of 167 days) after haploSCT (6, 7). Einat Shmueli et al. from Israel designed a conditioning protocol for haploSCT including fludarabine, thiotepa, anti-thymocytic globulin, and total body irradiation (8). After receiving preemptive therapy, the incidence of CMV infection was 66.7% in haploSCT, and 11.6% of haploSCT transplant recipients with CMV reactivation developed CMV disease. Importantly, drug-resistance mutations and clinically suspected resistance were discovered only in haploSCT recipients (8), favoring prophylactic over preemptive treatment in high-risk patients and highlighting the need for better anti-CMV drugs.
It remains unclear whether primary disease affects CMV infection after haploSCT. Lan‐Ping Xu et al. from Peking University conducted studies to confirm the feasibility of haploidentical transplantation in patients with severe aplastic anemia (SAA) as salvage therapy (9–12). CMV viremia occurred in 51.7~84.00% of SAA patients. However, no difference in the rates of early CMV disease between haploidentical patients and matched related patients was found (9, 10). Consistently, several centers in China obtained similar results for SAA patients (13–15). The haploSCT cohorts with AML, MDS, or Ph+ ALL, including haplo-cord-HSCT, had higher CMV viremia than the HLA-matched HSCT cohorts (16–19), but the incidence of CMV disease was not significantly different between the two groups. Even in pediatric patients with MDS or patients with relapsed/refractory acute lymphoblastic leukemia after CAR-T therapy who underwent haploSCT, the incidence of CMV reactivation/infection was less than 60%, and very few patients developed CMV disease (20, 21).
Using a similar protocol, several transplant centers have reported promising results for unmanipulated haploidentical peripheral blood stem cell transplantation (PBSCT) (22, 23) or cotransplantation of unrelated cord blood (UCB) (24–26) or mesenchymal stem cells (MSCs) (27, 28). The 1-year cumulative incidence of CMV DNAemia in patients with hematologic malignancies was 23.5-41.7% in the matched sibling donor (MSD)-SCT group versus 62.1-81.0% in the haploSCT group with peripheral blood stem cells (PBSCs) (29, 30). The median time to the onset of CMV DNAemia in the haploSCT group was 33 days (range, 10–159 days) with the 1-year cumulative incidence of CMV disease at 7.9% (95% CI, 3.6–14.3%) (29). In addition, a total of 19.4%-92% of these patients experienced CMV reactivation after combination of haploSCT with UCB or MSCs (24–28). There was no statistical significance in the incidence of CMV viremia in terms of haplo-cord SCT vs HLA-matched donor SCT (MD-SCT) or haplo-cord SCT vs haploSCT (24–26).
As the use of ATG as a regimen for in vivo TCD and immunosuppressants is limited by impaired immune restoration and a high risk of severe infections, researchers are working on their impact after haploSCT. Peking University performed a study comparing 6 mg/kg ATG versus 10 mg/kg ATG in patients who underwent haploSCT (31). The 1-year cumulative incidence of CMV reactivation was similar between the ATG-6 and ATG-10 groups[(75.0% (66.8–83.2%) vs 78.6% (75.2–82.0%)]. Another multicenter study investigated the impact of 7.5 mg/kg and 10.0 mg/kg rabbit ATG on GVHD and virus reactivation after haploSCT (32). The 1-year incidence of CMV DNAemia was higher in the 10.0 mg/kg group [83.4% (77.5-87.9)] than in the 7.5 mg/kg group [73.4% (67.2-79.4)], whereas the 2-year incidence of CMV-associated diseases was also higher in the 10.0 mg/kg group [5.9% (3.2–9.7%)] than in the 7.5 mg/kg group [1.5% (0.4–4.0%)]. Yu Wang et al. recently extended follow-up from this original trial (33). They found that patients undergoing haploSCT benefit from 7.5 mg/kg ATG compared to 10.0 mg/kg ATG based on a balance between GVHD and infection control. The data supports ATG (7.5 mg/kg) is potentially the standard regimen in this platform. Researchers from Japan and the Republic of Korea later performed haploSCT using low-dose thymoglobulin at 5 mg/kg (34, 35). CMV reactivated in 41.67% and 72.7% of patients, but CMV disease developed in 0 and 19.4% of patients, respectively. A recent report from the Republic of Korea indicated that the cumulative incidence of CMV DNAemia at 3 years was 45.7% (30.7-59.4) for ATG (5-10 mg/kg)-based haploSCT (36). Moreover, a short-term tacrolimus regimen for the prophylaxis of GVHD in haploSCT did not increase the incidence of CMV infection compared with the Cyclosporine A regimen (39.5% vs. 37.5%, p = 0.783) (37).
Ex Vivo TCD-haploSCT
CD34+ selection was initially used as a method for TCD, but it resulted in delayed immune reconstitution and a high incidence of opportunistic infections and nonrelapse mortality. The ex vivo TCD techniques have developed from CD34+ selection, CD3+ cell depletion, and αβ+/CD19+ cell depletion to recent CD45RA+ depletion. Compared with CD34+ cell selection, after CD3+ cell depletion, the graft has more natural killer (NK) cells, monocytes, and other immunomodulating cells with better outcomes. Sameh Gaballa et al. retrospectively compared data on patients undergoing a two-step (a fixed T cell infusion followed 2 days later by cyclophosphamide, and then a CD34-selected stem cell product infused) haploidentical or matched related PBSCT for high-risk hematological malignancies and aplastic anemia (38). Compared with the matched related PBSCT group (matched related, 19%), the 100-day cumulative incidence of CMV viremia was higher in the haploidentical group (haploidentical, 67%). The median time to develop CMV reactivation was 26 days in the haploSCT group and 36 days in the matched related PBSCT group.
The cumulative incidence of CMV DNAemia in patients with acute leukemia was 73.5-81% after ex vivo αβ T cell-depleted haploSCT (39, 40). No patient developed CMV disease or died (39). A more recent study explored the role of interim-foscarnet prophylaxis in preventing CMV infection after ex vivo αβ T cell-depleted haploSCT in children between May 2012 and May 2018 (41). Forty (50.8%) of 81 patients developed CMV reactivation at a median of 41.3 days (range, 13–132) after haploSCT. The median duration of CMV reactivation was 28.5 days (range, 1–179), and the peak PCR level was 3.82 log copies/mL (range, 2.85–6.03) (41). In nonmalignant disease, ganciclovir/foscarnet significantly decreased CMV reactivation incidence (43.7% vs. 78.3%), whereas the prophylaxis strategy had no significant impact in patients with hematological malignancies. No significant difference was found in the rate of CMV disease according to prophylaxis method. It suggests that this intensified antiviral strategy may be necessary for αβ T cell-depleted haploSCT patients with nonmalignant disease who require higher doses of ATG.
Through TCR α+β+/CD19+ cell-depleted haploSCT, it is feasible to transfer to the transplant recipient both donor hematopoietic stem cells (HSCs) and hematopoietic progenitors as well as NK and γδ T cells, which could protect against leukemia and life-threatening infections, including posttransplant lymphoproliferative disease (PTLD). A total of 7.27-75% of patients undergoing TCR α+β+/CD19+ cell depleted HSCT experienced CMV reactivation (42–46). Most patients experienced CMV viremia during the first month after haploSCT (days +1 to +24) (45). In a report including three sickle cell disease and 11 thalassemia patients, Gaziev J et al. stated that viral reactivation occurred in the vast majority of patients after TCR α+β+/CD19+ cell–depleted haploSCT, with CMV reactivation in 64%, although no cases of CMV were noted (47).
After removal of potentially alloreactive CD45RA+ cell depletion, memory T cells, including virus-specific T cells left in grafts, could shorten viremia and reduce GVHD (48). B M Triplett et al. reported data from 17 patients with poor-prognosis hematologic malignancy who underwent haploSCT with CD45RA-depleted grafts after a reduced intensity conditioning regimen without TBI or serotherapy (49). Three patients of 17 received anti-CMV treatment after CMV reactivation. None of the patients experienced CMV disease, and all of them cleared CMV viremia without donor lymphocyte infusion (DLI). Early T-cell reconstitution was directly linked to the CD45RA-depleted graft content. This group then compared 41 patients receiving CD3‐depleted (CD3dep recipients) grafts with 26 receiving CD45RA‐depleted grafts (CD45dep recipients) after haploSCT (50). CD3dep recipients were more likely to develop CMV reactivation—23 (56%) vs 5 (19%). All CD3dep recipients with CMV received treatment, and eight (36%) were also infused with donor lymphocytes for CMV, whereas CMV treatment was needed for only three of the five CD45RAdep recipients. Although three CD3dep recipients died with active CMV viremia, CMV was not detected in CD45RAdep recipients at the time of death. It seems that CD45RA-depleted haploSCT confers enhanced T-cell recovery and reduced infection without increase in severe GVHD among these ex vivo TCD methods.
PTCy-haploSCT
PTCy is a method of in vivo T cell depletion that mainly acts on alloreactive T cells after haploSCT. CMV reactivation was noticed in 42%-69.2% of patients who underwent PTCy-haploSCT (51–58). A total of 2.8%-4.5% of patients experienced CMV-associated disease (51, 52). CMV reactivation occurred at a median time of 35-39 days (51, 52, 57). The median time to first episode of CMV DNAemia was 33 days (range, −7 to 123 days) after haploSCT (58). Moreover, the CMV DNA peak load was remarkably higher in haploSCT recipients, but the mortality by days 180 and 365 did not differ among comparison groups (55). García-Cadenas Irene et al. studied the impact of HLA donor matching on infection in patients receiving PTCy-based alloSCT (59). They found that haploSCT recipients had a higher incidence of CMV infection/reactivation at 18 months than other transplant modalities [(61% (95% CI: 41–74%) vs. 44% (95% CI: 31–54%)], whereas lethal infections were uncommon across all these groups. In their study, severe infections were common in transplant patients using PTCy. A more recent CIBMTR analysis reported (51) that PTCy increased the risk of CMV infection among CMV-seropositive recipients in both haploSCT and matched sibling donor HSCT compared with calcineurin inhibitor–based sibling donor transplantation, suggesting intensive CMV prevention strategies in all receiving PTCy. This is supported by the fact that an intensified method to prevent CMV reactivation correlated with a lower incidence of CMV reactivation (67% intensified group versus 81% traditional group) and less CMV disease (0% hybrid/intermediate dose versus 8% traditional dose) without increased toxicity after PTCy-haploSCT compared with a traditional antiviral prophylaxis regimen (60).
Primary disease and conditioning regimen could also impact CMV infection after PTCy-haploSCT. CMV reactivation post engraftment was noted in 43.7% and 62% of transplant recipients with primary immune deficiency disorders (PIDs) (61) and relapsed/refractory SAA (62) undergoing PTCy-haploSCT, respectively. R V Raj et al. then investigated the effect of conditioning intensity on the incidence of viral infection after PTCy-haploSCT (63). Their study found that challenging viral infections after haploSCT cause significant morbidity in this patient population. It appears that the incidence of viral complications is higher following myeloablative doses of busulfan-containing conditioning regimens (63). Emmanuel Katsanis et al. recently performed a single center phase I study substituting day +4 PTCy with bendamustine (PT‐BEN) following myeloablative conditioning and T‐cell replete haploidentical bone marrow transplantation (64). CMV reactivation was notably less common in trial patients receiving PTCy/BEN, with one out of eight at-risk (seropositive recipient and/or seropositive donor) of experiencing CMV reactivation, whereas 71.4% of the at‐risk PTCy patients reactivated CMV.
Compared with bone marrow (BM) as a graft source, PBSCs could yield higher CD34+ cell counts but were possibly accompanied by increased GVHD; however, no difference in GVHD was observed in haploSCT (65). A total of 46-68% of patients with PTCy-haploSCT and PBSC grafts had posttransplant CMV viremia (65–69). The median time to viremia was 24 days (range: 3–68). CMV disease occurred in 17-28.8% of patients with CMV viremia (65, 68). Sirolimus with micophenolate mofetil (MMF) has recently been regarded as an alternative to calcineurin inhibitor-containing approaches, as this combination has a decreased risk of acute renal failure, decreased incidence of CMV reactivation, and better regulatory T cell reconstitution. Some groups have introduced PTCy plus sirolimus and MMF (PT-CY-Sir-MMF) as GVHD prophylaxis in allo-HSCT, regardless of donor type (70, 71). CMV DNAemia occurred in 52-63% of patients after haploSCT. The cumulative incidence of CMV DNAemia in patients who received pre-emptive antiviral therapy at one year was 39% (95% CI, 31–47%), and the 1-year cumulative incidence of CMV disease was 2.6% (95% CI, 0.09–5%) (70).
ATG+ PTCy-haploSCT
As ATG is usually used to reduce the risk of graft rejection and GVHD, it is assumed that ATG combined with PTCy in T-cell replete-haploSCT would minimize GVHD risk but not impact engraftment and risk of relapse. Princes Margaret Cancer Centre from Canada established unmanipulated haploidentical PBSC transplantation following RIC with ATG (total 4.5 mg/kg), PTCy (cyclophosphamide 50 mg/kg/day i.v. on days +3 and +4), and cyclosporine as a GVHD prevention strategy (72–74). CMV reactivation occurred in 74% of cases with CMV disease in 11.5% of cases (72). Cheng‐Hsien Lin et al. retrospectively compared the cumulative incidence of CMV DNAemia, two‐year OS, and leukemia‐free survival rates in acute leukemia patients with MSD, matched unrelated donor (MUD), and haploidentical donor allografts (ATG: 2 mg·kg-1 day-1, from day -3 to day -2; PTCy) (75). The cumulative incidences of CMV DNAemia at day 180 in the haploidentical groups were 85.7%, which were higher than those in the MSD and MUD allo‐HSCT groups. For the haploidentical groups, CMV DNAemia was detected at a median time of 29 days.
Yu Wang et al. from Peking University initiated a prospective study in patients with a standard-dose ATG/granulocyte colony-stimulating factor (G-CSF)-based regimen (ATG-PTCy) followed by low-dose PTCy (14.5 mg/kg on days 3 and 4) for haploSCT (76, 77). The 100-day cumulative incidence of CMV reactivation in the ATG-PTCy cohort was markedly higher than that in the ATG cohort (74% vs 30%), with a comparable incidence of CMV disease between the two cohorts (8% vs 8%) (77), indicating that dual T cell depletion with PTCy and ATG may bring about a higher incidence of CMV reactivation.
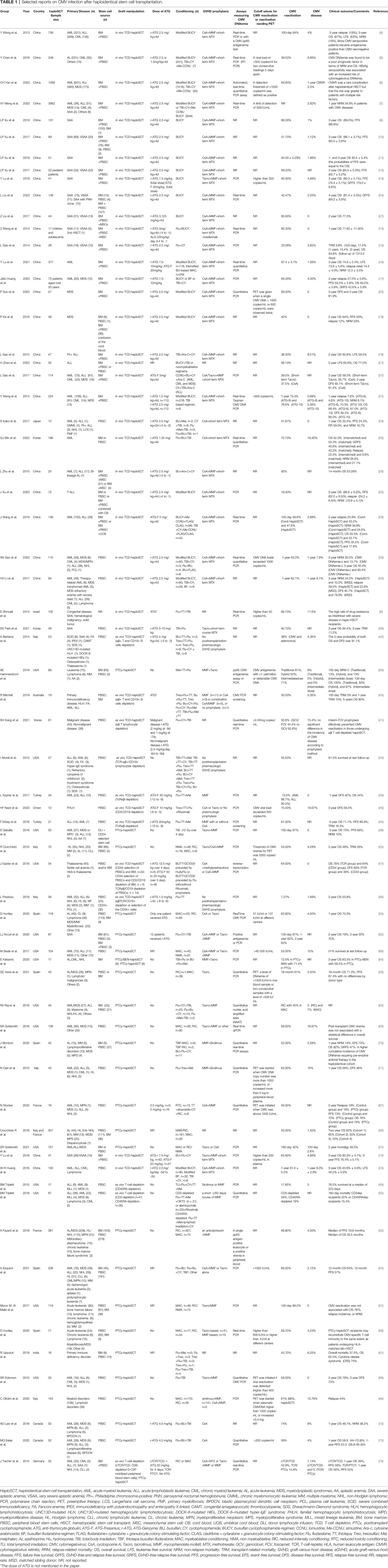
Comparison Among These Approaches
Published data have been inconsistent on the incidence of CMV reactivation and CMV disease after haploSCT (Table 1). It indicates that haploSCT carries a substantially higher risk for CMV infection compared with HLA‐matched related or unrelated allo‐HSCTs, but this seemed not to impact overall and non‐relapse mortality. Hence, some data suggest the use of prophylactic anti-CMV antivirals when PTCy is used because a higher incidence of CMV reactivation was associated with the use of PTCy (51, 60). Surprisingly, a systematic review and meta-analysis of studies on haploSCT in idiopathic AA suggested that the addition of PTCy correlated with a lower risk of CMV viremia (10.4%) to a larger extent than MTX-containing (55.7%) and other (38.6%) regimens (79). The opposite results can be partly explained by the absence of an approved threshold of viral load to initiate anti-CMV treatment, considering the different transplant centers. The heterogeneous CMV serological status in the donor/recipient on account of geographical and ethnological characteristics is another possible explanation because the CMV seroprevalence is usually much higher (>=90%) in adult populations of China than in Europe and the USA (80–84). This issue could be better investigated in a future clinical trial.
Johanna Tischer et al. retrospectively compared the incidence of virus infections and outcome in two different haploSCT settings (78). The first approach was the combination of T cell repletion and T cell depletion (CD6 deletion) using ATG prior to haploSCT (cTCR/TCD group). The second was T cell repletion (TCR) using high-dose posttransplantation cyclophosphamide (TCR/PTCy group). CMV reactivation occurred more frequently in the cTCR/TCD group (57%) than in the TCR/PTCy group (31%). Furthermore, pre-emptive treatment of CMV reactivation was successful in the TCR/PTCy group, whereas CMV DNA became undetectable in only 50% of the cTCR/TCD group.
CMV-Specific Immune Reconstitution and Its Association With CMV Reactivation After haploSCT
CMV-Specific T Cell (CTL)
We previously investigated CMV-specific T cell (CMV-CTL) reconstitution post in vivo TCD-haploSCT (85–87). The CD8+ T cell number in transplant recipients was comparable to that of controls at day 60 after transplantation. The median number of CMV-CTLs and their subsets was equal to those of the controls from day 30 to day 360. In addition, haploSCT recipients had a high frequency of CMV-CTLs with strong proliferation capacities and interferon-γ production at one year after transplantation (86). CMV-specific T cells with the central memory CD45RO+CD62L+ cell phenotype were significantly expanded when CMV was reactivated early after transplantation (87). Ruri Kato et al. demonstrated that there were considerably lower maximum numbers of CMV-CTLs in the CMV antigenemia resolved group than in the persistent group (median, 22.15 vs. 50 cells/μl) (88). Nevertheless, CMV-CTLs reached a peak more quickly in the resolved group than in the persistent group (median, 21 vs. 78 days) (88).
M Noviello et al. retrospectively explored either CD34 selection or posttransplant sirolimus as GVHD prophylaxis for haploSCT recipients (89). At 30 days, 21.7% of patients had CMV-specific T cells higher than 1 sfc/μL measured by enzyme-linked immunosorbent spot (ELISPOT), whereas CMV viremia occurred in only one patient who received anti-CMV treatment. At 90 days, 29.0% of patients reached this threshold, and no patients experienced clinically relevant viremia. At 180 days, 52.9% of patients finally reached the threshold, and none of them experienced CMV viremia. They found the protective value of 1 CMV sfc/μL against CMV reactivation posttransplant (89).
Dixie Huntley et al. performed a multicenter observational study to monitor CMV-specific T cell kinetics in PTCy-haploSCT patients and compared it with HLA-matched transplantation (58). In their analysis, CMV DNAemia developed at a similar frequency with equal numbers of CMV-specific T-cell at most time points examined between PTCy-haploSCT and MRD/MUD recipients. CMV DNAemia did not affect CMV-specific CD8+ and CD4+ T-cell reconstitution by the end of the follow-up period (day +180) in either allo-HSCT modality. They claimed that PTCy-haploSCT recipients may restore CMV-specific T-cell immunity to the same extent as HLA-matched allo-HSCT patients (58). The same group also reported that CMV infection was related to high levels of CD27−CD28− T cells, which behave like Tregs (90). They found a suboptimal correlation between CMV-specific CD4+ or CD8+ T cells and Tregs in peripheral blood (PB), which was weaker in patients with CMV reactivation prior to immunological monitoring. This suggests that recovery of PB Tregs and that of CMV-specific T-cell subsets show distinct kinetics, particularly after CMV reactivation.
More recently, Jasper J. P. van Beek et al. conducted longitudinal analysis of high-dimensional T-cell immunophenotypes in 21 recipients of PTCy-haploSCT (91). CMV-specific T-cells were primed early after PTCy-haploSCT and initially showed a proliferating/activated phenotype, that was quickly replaced by a terminal effector phenotype, while uncontrolled viral replication associated with lower abundance of distinct CMV-specific CD4+ T-cell immunophenotypes, hinting at a possible role of these cells in CMV control. CMV-specific T-cell features were similar to those of the CMV-seropositive donor one year posttransplantation, implying reestablishment of physiological homeostasis.
NK
NK cells similarly play an essential role in defense against infections and leukemia relapse after hapoSCT. Fengyan Jin et al. explored NK cell dynamics in 29 patients after haploSCT between August 2011 and November 2014 (92). IFNγ-producing NK cells expanded in 19 patients after CMV reactivation, and the percentages of IFNγ-producing NK cells in these patients greatly increased from day 60 to 180 after transplantation compared to those of their donors. The percentage of KIR-expressing NK cells and IFNγ-producing NKG2C+ NK cells was significantly higher in haploSCT recipients with CMV reactivation than in those without CMV reactivation. Moreover, CMV reactivation was associated with expansion of the CD56brightCD16dim/−DNAM1+ NK cell subset between days 30 and 90 after haploSCT (93). Patients with increased CD56brightCD16dim/−DNAM1+ NK cells also had a remarkably higher CMV viral load (93).
Letizia Muccio et al. reported that CMV reactivation boosted the arrival of mature NK cells in pediatric patients with hematological malignancies receiving HLA-haploSCT after removal of both αβT cells and CD19 B cells (94). A memory-like NK cell subset expressing NKG2C and CD57 progressively expanded in most children. NKG2C+CD57+ NK cells were detected by month 3 after allo-SCT and expanded until at least month 12. These cells characteristically expressed high levels of killer Ig-like receptors (KIRs) and leukocyte inhibitory receptor 1 (LIR-1) and low levels of Siglec-7, NKG2A and interleukin-18Rα. Additionally, they poorly secreted interferon-γ in response to interleukin-12 and interleukin-18. The compromised response to these cytokines as well as their highly differentiated profile may reflect their skewing toward immune control of human cytomegalovirus.
Xiang‐Yu Zhao et al. from Peking University previously found that donor-recipient KIR ligand matching decreased CMV reactivation and refractory CMV infection by day 100 post-transplantation (95). This indicates that donor-recipient KIR ligand matching might improve the NK cell licensing process and promote NK cell-mediated control of CMV reactivation. The same group then prospectively assessed NK cell reconstitution in patients undergoing matched sibling transplantation and haploSCT (96). CD107a was increasingly expressed in NK cells after versus before CMV reactivation at days 60, 100, and 180 after transplantation, but CMV reactivation did not impact the maturation process of NK cells after transplantation. In addition, KIR expression and NKp30 expression were lower on NK cells in patients with CMV reactivation than in those without CMV reactivation at day 30. The NK-to-T-cell (NK/T) ratio was persistently higher in patients with CMV reactivation than in those without CMV reactivation from 30 days to one year after haploSCT.
An emerging report from Elisa Zaghi et al. demonstrated impaired adaptive NK cells expanded after CMV reactivation in PTCy-haploSCT (97). By a longitudinal single-cell computational profiling of multiparametric flow cytometry, they found that CMV accelerates NK cell immune recovery with the expansion of CD158b1b2jpos/NKG2Aneg/NKG2Cpos/NKp30lo NK cells. The number of this subset is associated with CMV reactivation, further increases in recipients with multiple viral reactivations and persists for months after the infection. The transcriptional characteristics of FACS-sorted CD158b1b2jpos NK cells confirmed the capacity of CMV to deregulate NKG2C, NKG2A, and NKp30 gene expression, thus mediating the expansion of NK cells with adaptive traits. These results imply that the dysfunction/exhaustion of “adaptive” KIRpos NK cells in patients with CMV reactivated is induced, at least partially, by the CMV-induced expression of checkpoint inhibitors.
γδ T
Fifty pediatric patients undergoing αβ T cell-depleted haploSCT between August 2012 and December 2015 were analyzed (98). CMV reactivation developed in 19 transplantations at a median of 30 days (range, 13-318 days) after haploSCT. Higher γδ T cells were observed in patients without CMV reactivation than in patients with CMV reactivation at day 30 (197.8 ± 153.9 vs 53.9 ± 58.7). There was a significantly higher incidence of CMV reactivation in patients with a low percentage of γδ T cells at day 30 than in patients with a high percentage of γδ T cells (78.0 ± 15.3% vs 22.2 ± 13.9%). No difference in day 30 γδ T cells was found between patients with and without CMV disease.
Irma Airoldi et al. prospectively monitored the functional and phenotypic characteristics of γδ T cells up to 7 months after αβ+ T cells and CD19+ B cells depleted haploSCT in 27 children (44). They reported that γδ T cells are the foremost T-cell population in patients during the first weeks and are mainly derived from the graft content and expanded in vivo after transplantation. Central memory cells predominated very early after haploSCT for both the Vδ1 and the Vδ2 subsets. Vδ1 cells are specifically expanded in patients with CMV reactivation and are more cytotoxic than those of children without reactivation.
CMV-specific T-cell, NK cell, and γδ T-cell are vital to immune control of CMV infection post haploSCT, but it seems that γδ T-cell is more likely responsible for viral reactivation in the context of ex vivo TCD-haploSCT. Although NK cells and γδ T cells are the first lymphocytes that recover after transplantation, CMV-specific T cells are dominant in number in case of viral infection. The majority of studies state that impaired T-cell and NK-cell reconstitution and increased risk of CMV infection after haploSCT, so seeking factors influencing CMV-specific immune reconstitution and interventions to improve immune reconstitution is urgent at the moment. Although data from Dixie Huntley et al. supported similar incidence of CMV infection and restored CMV-specific T cells after PTCy-haploSCT compared to MRD/MUD transplantation (58), the scarce number of MUD and MRD recipients and more sirolimus used in PTCy-haploSCT group preclude any definitive conclusion and further studies are warranted to validate their findings.
Cellular Immunotherapy of CMV Infection
Delayed CMV-specific immune reconstitution has been consistently associated with the development of CMV infection and CMV disease after allo-SCT. Accordingly, adoptive transfer of CMV-specific T cells has been employed to treat CMV infection. Several clinical trials and case reports have confirmed the safety and efficacy of this strategy for the prophylaxis and treatment of CMV infection after haploSCT. Table 2 lists cellular approaches currently in clinical trials and serves as evidence that CMV-targeting immune-based interventions could provide a safe, novel treatment option while offering clinical benefit to CMV reactivated recipients after haploSCT.
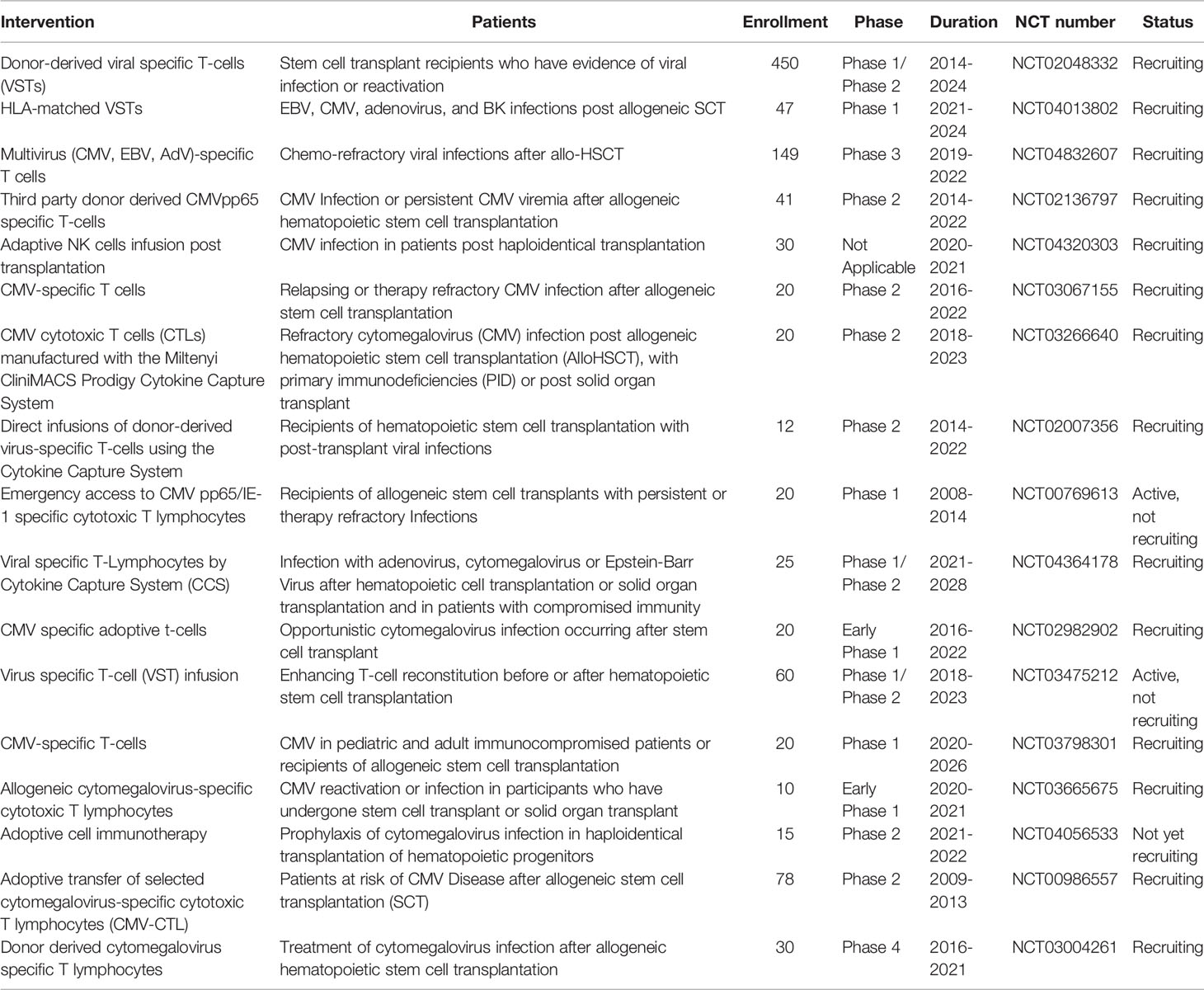
Table 2 Ongoing clinical trials using cytomegalovirus-specific cellular immunotherapy for allo-SCT patients including haploidentical SCT (accessed on 5 Oct 2021, ClinicalTrials.gov).
Therapeutical CMV-Specific T-Cell Approaches
Feuchtinger T et al. treated 18 patients after allo-SCT from HLA–mismatched/haploidentical or HLA–matched unrelated donors with polyclonal CMV-specific T cells (99). These T cells were generated by isolation of interferon-γ–producing cells after stimulation with pp65 antigen. Patients with refractory CMV disease or viremia received a mean of 21 × 103/kg pp65-specific T cells. CMV infection was cleared, or viral burden was significantly decreased in 83% of these patients, even in patients with CMV encephalitis. Viral control was related to improved antiviral T-cell reconstitution and in vivo expansion of CMV-specific T cells in 12 of 16 evaluable cases without inducing GVHD or acute side effects.
In another CMV infection refractory cohort (100), 27 of 32 treated patients after haploSCT cleared CMV within four weeks after adoptive T-cell therapy without recurrence. After cellular transfer, CMV-specific T cells expanded in vivo with improved cytokine production and proliferation ability. In addition, the expression of programmed death-1 (PD-1) on CMV-specific T cells was reduced. In the early effective group, patients who cleared viremia within four weeks after T-cell infusion, CMV-specific CD8+ IFN-γ+ and CD4+ IFN-γ+ T cells were rapidly and massively expanded in vivo, whereas in the late effective group, there was no significant expansion of CMV-specific T cells. Xiang-Yu Zhao et al. further evaluated the safety and efficacy of donor-derived CMV-specific cytotoxic T cells (CTLs) as a first-line therapy for CMV infection after haploSCT (101). They observed that first-line therapy with CTLs significantly reduced the incidence of CMV infection with lower 1-year treatment-related mortality and better 1-year overall survival. Moreover, first-line therapy with CTLs promoted the recovery of CTLs in patients, which correlated with CMV clearance.
A case report described two patients with drug-resistant CMV encephalitis after haploSCT successfully received donor CMV-specific CTLs (102). In the first case, a 27-year-old male developed CMV encephalitis during ganciclovir maintenance treatment after haploSCT. After administering foscarnet and donor CMV-specific CTLs, CMV-DNA of his cerebrospinal fluid (CSF) was negative by RT-PCR, and the lesions on brain magnetic resonance imaging (MRI) were reduced. Another case, a 57-year-old female, also experienced CMV encephalitis during maintenance treatment with ganciclovir after haploSCT. After intrathecal treatment with donor CMV-specific CTLs, the CMV load of the CSF was reduced.
Prophylactic DLI
Prophylactic and therapeutic DLI are administered to improve posttransplant immune restoration to reduce both infectious complications and disease relapse. Michael Maschan et al. investigated low-dose memory (CD45RA-depleted) donor lymphocyte infusion (mDLI) after αβ T-cell depleted HSCT (103–105). The incidence of CMV reactivation was 45-50% in the experimental mDLI arm and 54-55% in the control arm. The median duration of CMV viremia was 3 weeks (range, 1-9) in the prospective cohort and 4 weeks (range, 1-26) in the historical cohort (105). Memory DLI was associated with improved CMV-specific T-cell reconstitution in a subcohort of CMV IgG seropositive recipients. Analysis of a subcohort of CMV seropositive recipients indicated remarkably better CMV-specific T-cell reconstitution on day 30 in the experimental arm (104). Compared to that of the historical cohort, restoration of CMV-specific immunity at day 30 was significantly enhanced in the prospective cohort (40% versus 25%) (105). Luca Castagna et al. prospectively evaluated a CD45RA+ depleted DLI in terms of reducing viral infection early after PTCy-haploSCT (106). CMV reactivation occurred in 28% of patients. Although the majority of the patients received the planned three infusions, only one patient developed grade 2 acute GVHD, and two patients had moderate chronic GVHD.
Therapeutic DLI
Park HJ et al. reported the successful treatment of refractory CMV colitis after PTCy-haploSCT using CD45RA+ depleted DLI (107). After failure of ganciclovir and foscarnet, granulocyte colony-stimulating factor-primed, CD45RA+ depleted DLI was administered to treat refractory CMV colitis. CMV pp65-specific CTLs were found in recipients four weeks after DLI. Meanwhile, diffuse wall thickening involving the entire colon was also normalized in the abdominal CT scan.
As manipulated DLI approaches are still not widely used due to high cost and intensive labor, unmanipulated donor lymphocytes (U-DLIs), if feasible by harvesting CTLs directly from the peripheral blood of seropositive donors, are used for refractory or relapsed patients with CMV infection. Researchers from Turkey enrolled five pediatric patients receiving U-DLI for CMV infection after transplantation (108). Among them, three patients underwent haploSCT. One patient who was transplanted from an unrelated donor received U-DLI from his haploidentical mother. CMV titers were dramatically reduced after U-DLI in these patients.
Summary and Outlook
Despite the use of prophylactic or preemptive treatments, CMV infection remains an obstacle for successful haploSCT and the improvement of immunologic reconstitution is the primary strategy for infection prevention. A higher rate of CMV reactivation occurred early after haploSCT compared to HLA-matched HSCT, but CMV disease rates were low after haploSCT, particularly in in vivo TCD-haploSCT and PTCy-haploSCT. It results from expansion of CMV-specific central memory T-cells in the setting of CMV antigenemia or acceptable CMV-specific T-cell reconstitution. Traditional ex vivo TCD-haploSCT successfully prevents lethal GVHD without any posttransplantation immunosuppression, but the small number of T cells in the graft results in impaired immune recovery, which could be overcome by novel ex vivo TCD-haploSCT and adoptive cellular therapy. In vivo TCD-haploSCT and PTCy-haploSCT indicated low treatment‐related mortality (TRM) and an acceptable safety profile, which appears to compare favorably with ex vivo TCD-haploSCT in terms of infections. However, synergistic immunosuppression by PTCy and ATG has led to a higher incidence of CMV infection. We now have a better understanding of CMV reactivation and immune reconstitution post haploSCT. Our data demonstrate that novel ex vivo TCD techniques followed by prophylactic and therapeutic DLI, a low dose of ATG, an intensified antiviral prophylaxis regimen, sirolimus-containing immunosuppressors and CMV-specific cellular immunotherapy can boost immune recovery and decrease the incidence of CMV reactivation. Furthermore, the majority of patients receiving the RIC regimen might be less susceptible to infections (63). In this context, it would be essential to perform a prospective study comparing the risk of infectious complications after in vivo TCD-haploSCT vs. ex vivo TCD-haploSCT or PTCy-haploSCT in patients who received a similar conditioning regimen.
CMV reactivation is associated with delayed immune reconstitution, although this reactivation could also leave a profound imprint on the recovering T cell compartment long-term following allo-SCT (91, 109, 110). Several studies have reported that CMV serostatus and CMV reactivation may be more predictive of T-cell restoration after allo-SCT than GVHD, highlighting the deep impact of this virus on reconstituting T-cells, considering the high incidence of CMV reactivation after haploSCT. More importantly, CMV infection is increasingly recognized as an immunomodulator in cancer patients (111), even in the context of allo-SCT, which is associated with a decreased risk of leukemia relapse, although it is still conflicting (112–115). There is evidence of a bidirectional relationship between CMV reactivation and acute GVHD (116, 117). We should take these into account and balance the merit and disadvantage of taking steps to enhance CMV-specific immune reconstitution and decrease CMV infection.
Author Contributions
X-HL wrote the first draft of the manuscript, conducted the literature search, reviewed the abstracts, performed analysis and contributed to the final draft. YZ contributed to revising the manuscript and provided scientific input. Y-TC and L-PS conducted the literature search. LL revised and wrote the final draft, and contributed to the analysis. All authors contributed to the article and approved the submitted version.
Funding
X-HL was supported by the National Natural Science Foundation of China [grant 81100388, grant 81470344].
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors apologize to all authors whose work could not be cited because of length restrictions of this update on CMV infection and CMV-specific immune reconstitution after haploidentical stem cell transplantation.
References
1. Lu DP, Dong L, Wu T, Huang XJ, Zhang MJ, Han W, et al. Conditioning Including Antithymocyte Globulin Followed by Unmanipulated HLA-Mismatched/Haploidentical Blood and Marrow Transplantation can Achieve Comparable Outcomes With HLA-Identical Sibling Transplantation. Blood (2006) 107:3065–73. doi: 10.1182/blood-2005-05-2146
2. Huang XJ, Liu DH, Liu KY, Xu LP, Chen H, Han W, et al. Haploidentical Hematopoietic Stem Cell Transplantation Without In Vitro T-Cell Depletion for the Treatment of Hematological Malignancies. Bone Marrow Transplant (2006) 38:291–7. doi: 10.1038/sj.bmt.1705445
3. Xiao-Jun H, Lan-Ping X, Kai-Yan L, Dai-Hong L, Yu W, Huan C, et al. Partially Matched Related Donor Transplantation can Achieve Outcomes Comparable With Unrelated Donor Transplantation for Patients With Hematologic Malignancies. Clin Cancer Res (2009) 15:4777–83. doi: 10.1158/1078-0432.CCR-09-0691
4. Wang Y, Liu D-H, Liu K-Y, Xu L-P, Zhang X-H, Han W, et al. Long-Term Follow-Up of Haploidentical Hematopoietic Stem Cell Transplantation Without In Vitro T Cell Depletion for the Treatment of Leukemia. Cancer (2013) 119:978–85. doi: 10.1002/cncr.27761
5. Chen Y, Xu LP, Liu KY, Chen H, Chen YH, Zhang XH, et al. Risk Factors for Cytomegalovirus DNAemia Following Haploidentical Stem Cell Transplantation and Its Association With Host Hepatitis B Virus Serostatus. J Clin Virol (2016) 75:10–5. doi: 10.1016/j.jcv.2015.12.003
6. Yan CH, Wang Y, Mo XD, Sun YQ, Wang FR, Fu HX, et al. Incidence, Risk Factors, and Outcomes of Cytomegalovirus Retinitis After Haploidentical Hematopoietic Stem Cell Transplantation. Bone Marrow Transplant (2020) 55:1147–60. doi: 10.1038/s41409-020-0790-z
7. Meng X-Y, Fu H-X, Zhu X-L, Wang J-Z, Liu X, Yan C-H, et al. Comparison of Different Cytomegalovirus Diseases Following Haploidentical Hematopoietic Stem Cell Transplantation. Ann Hematol (2020) 99:2659–70. doi: 10.1007/s00277-020-04201-4
8. Shmueli E, Or R, Shapira MY, Resnick IB, Caplan O, Bdolah-Abram T, et al. High Rate of Cytomegalovirus Drug Resistance Among Patients Receiving Preemptive Antiviral Treatment After Haploidentical Stem Cell Transplantation. J Infect Dis (2014) 209:557–61. doi: 10.1093/infdis/jit475
9. Xu L-P, Wang S-Q, Wu D-P, Wang J-M, Gao S-J, Jiang M, et al. Haplo-Identical Transplantation for Acquired Severe Aplastic Anaemia in a Multicentre Prospective Study. Br J Haematol (2016) 175:265–74. doi: 10.1111/bjh.14225
10. Xu L-P, Jin S, Wang S-Q, Xia L-H, Bai H, Gao S-J, et al. Upfront Haploidentical Transplant for Acquired Severe Aplastic Anemia: Registry-Based Comparison With Matched Related Transplant. J Hematol Oncol (2017) 10:25. doi: 10.1186/s13045-017-0398-y
11. Xu LP, Xu ZL, Wang FR, Mo XD, Han TT, Han W, et al. Unmanipulated Haploidentical Transplantation Conditioning With Busulfan, Cyclophosphamide and Anti-Thymoglobulin for Adult Severe Aplastic Anaemia. Bone Marrow Transplant (2018) 53:188–92. doi: 10.1038/bmt.2017.237
12. Xu LP, Zhang XH, Wang FR, Mo XD, Han TT, Han W, et al. Haploidentical Transplantation for Pediatric Patients With Acquired Severe Aplastic Anemia. Bone Marrow Transplant (2017) 52:381–7. doi: 10.1038/bmt.2016.281
13. Lu Y, Sun R-J, Zhao Y-L, Xiong M, Cao X-Y, Zhang J-P, et al. Unmanipulated Haploidentical Hematopoietic Stem Cell Transplantation Achieved Outcomes Comparable With Matched Unrelated Donor Transplantation in Young Acquired Severe Aplastic Anemia. Biol Blood Marrow Transplant (2018) 24:1881–7. doi: 10.1016/j.bbmt.2018.05.015
14. Wang Z, Zheng X, Yan H, li D, Wang H. Good Outcome of Haploidentical Hematopoietic SCT as a Salvage Therapy in Children and Adolescents With Acquired Severe Aplastic Anemia. Bone Marrow Transplant (2014) 49:1481–5. doi: 10.1038/bmt.2014.187
15. Gao L, Li Y, Zhang Y, Chen X, Gao L, Zhang C, et al. Long-Term Outcome of HLA-Haploidentical Hematopoietic SCT Without In Vitro T-Cell Depletion for Adult Severe Aplastic Anemia After Modified Conditioning and Supportive Therapy. Bone Marrow Transplant (2014) 49:519–24. doi: 10.1038/bmt.2013.224
16. Lu Y, Zhao YL, Zhang JP, Xiong M, Cao XY, Liu DY, et al. Comparable Outcomes Among Unmanipulated Haploidentical, Matched Unrelated, and Matched Sibling Donors in BU-Based Myeloablative Hematopoietic Stem Cell Transplantation for Intermediate and Adverse Risk Acute Myeloid Leukemia in Complete Remission: A Single-Center Study. Ann Hematol (2021) 100(6):1579–91. doi: 10.1007/s00277-020-04355-1
17. Huang J, Huang F, Fan Z, Xu N, Xuan L, Liu H, et al. Haploidentical Related Donor vs Matched Sibling Donor Allogeneic Hematopoietic Stem Cell Transplantation for Acute Myeloid Leukemia and Myelodysplastic Syndrome Aged Over 50 Years: A Single-Center Retrospective Study. Cancer Med (2020) 9:6244–55. doi: 10.1002/cam4.3290
18. Gao L, Zhang C, Gao L, Liu Y, Su Y, Wang S, et al. Favorable Outcome of Haploidentical Hematopoietic Stem Cell Transplantation in Philadelphia Chromosome-Positive Acute Lymphoblastic Leukemia: A Multicenter Study in Southwest China. J Hematol Oncol (2015) 8:90. doi: 10.1186/s13045-015-0186-5
19. Ke P, Bao XB, Hu XH, Zhuang J, Wu XJ, Liu YJ, et al. Myeloablative Conditioning Regimens With Combined of Haploidentical and Cord Blood Transplantation for Myelodysplastic Syndrome Patients. Bone Marrow Transplant (2018) 53:162–8. doi: 10.1038/bmt.2017.229
20. Suo P, Wang S, Xue Y, Cheng Y, Kong J, Yan C, et al. Unmanipulated Haploidentical Hematopoietic Stem Cell Transplantation for Children With Myelodysplastic Syndrome. Pediatr Transplant (2020) 24:e13864. doi: 10.1111/petr.13864
21. Zhao H, Wei J, Wei G, Luo Y, Shi J, Cui Q, et al. Pre-Transplant MRD Negativity Predicts Favorable Outcomes of CAR-T Therapy Followed by Haploidentical HSCT for Relapsed/Refractory Acute Lymphoblastic Leukemia: A Multi-Center Retrospective Study. J Hematol Oncol (2020) 13:42. doi: 10.1186/s13045-020-00873-7
22. Luo Y, Xiao H, Lai X, Shi J, Tan Y, He J, et al. T-Cell-Replete Haploidentical HSCT With Low-Dose Anti-T-Lymphocyte Globulin Compared With Matched Sibling HSCT and Unrelated HSCT. Blood (2014) 124:2735–43. doi: 10.1182/blood-2014-04-571570
23. Huang WR, Li HH, Gao CJ, Bo J, Li F, Dou LP, et al. Haploidentical, Unmanipulated G-CSF-Primed Peripheral Blood Stem Cell Transplantation for High-Risk Hematologic Malignancies: An Update. Bone Marrow Transplant (2016) 51:1464–9. doi: 10.1038/bmt.2016.166
24. Liu L, Zhang Y, Jiao W, Zhou H, Wang Q, Qiu H, et al. Combination of Haploidentical Haematopoietic Stem Cell Transplantation With an Unrelated Cord-Blood Unit in Patients With Severe Aplastic Anemia: A Report of 146 Cases. Bone Marrow Transplant (2020) 55:2017–25. doi: 10.1038/s41409-020-0874-9
25. Xu J, Zhao R, Yang L, Gong H, Ma S, Chen J, et al. Haploidentical Stem Cells Combined With a Small Dose of Umbilical Cord Blood Transplantation Exert Similar Survival Outcome of HLA-Matched Stem Cells Transplantation in T-Cell Acute Lymphoblastic Leukemia. Bone Marrow Transplant (2020) 55:1197–9. doi: 10.1038/s41409-019-0666-2
26. Wang J, Wang Z, Wei W, Zhang W, Zhang T, Cheng H, et al. Cord Haploidentical Non-In Vitro T Cell Depletion Allogeneic Hematopoietic Stem Cell Transplantation Reduces Relapse of Refractory Acute Leukemia. Biol Blood Marrow Transplant (2019) 25:121–8. doi: 10.1016/j.bbmt.2018.09.002
27. Liu Z, Zhang Y, Xiao H, Yao Z, Zhang H, Liu Q, et al. Cotransplantation of Bone Marrow-Derived Mesenchymal Stem Cells in Haploidentical Hematopoietic Stem Cell Transplantation in Patients With Severe Aplastic Anemia: An Interim Summary for a Multicenter Phase II Trial Results. Bone Marrow Transplant (2017) 52:704–10. doi: 10.1038/bmt.2016.347
28. Zhu L, Wang Z, Zheng X, Ding L, Han D, Yan H, et al. Haploidentical Hematopoietic Stem Cell Transplant With Umbilical Cord-Derived Multipotent Mesenchymal Cell Infusion for the Treatment of High-Risk Acute Leukemia in Children. Leuk Lymphoma (2015) 56:1346–52. doi: 10.3109/10428194.2014.939970
29. Gao XN, Lin J, Wang LJ, Li F, Li HH, Wang SH, et al. Risk Factors and Associations With Clinical Outcomes of Cytomegalovirus Reactivation After Haploidentical Versus Matched-Sibling Unmanipulated PBSCT in Patients With Hematologic Malignancies. Ann Hematol (2020) 99:1883–93. doi: 10.1007/s00277-020-04156-6
30. Li H-H, Li F, Gao C-J, Huang W-R, Bo J, Dou L-P, et al. Similar Incidence of Severe Acute GVHD and Less Severe Chronic GVHD in PBSCT From Unmanipulated, Haploidentical Donors Compared With That From Matched Sibling Donors for Patients With Haematological Malignancies. Br J Haematol (2017) 176:92–100. doi: 10.1111/bjh.14331
31. Wang Y, Fu HX, Liu DH, Xu LP, Zhang XH, Chang YJ, et al. Influence of Two Different Doses of Antithymocyte Globulin in Patients With Standard-Risk Disease Following Haploidentical Transplantation: A Randomized Trial. Bone Marrow Transplant (2014) 49:426–33. doi: 10.1038/bmt.2013.191
32. Lin R, Wang Y, Huang F, Fan Z, Zhang S, Yang T, et al. Two Dose Levels of Rabbit Antithymocyte Globulin as Graft-Versus-Host Disease Prophylaxis in Haploidentical Stem Cell Transplantation: A Multicenter Randomized Study. BMC Med (2019) 17:156. doi: 10.1186/s12916-019-1393-7
33. Wang Y, Liu Q-F, Lin R, Yang T, Xu Y-J, Mo X-D, et al. Optimizing Antithymocyte Globulin Dosing in Haploidentical Hematopoietic Cell Transplantation: Long-Term Follow-Up of a Multicenter, Randomized Controlled Trial. Sci Bull (2021). doi: 10.1016/j.scib.2021.06.002
34. Kako S, Akahoshi Y, Harada N, Nakano H, Kameda K, Ugai T, et al. HLA-Mismatched Haploidentical Transplantation Using Low-Dose Anti-Thymocyte Globulin (ATG: Thymoglobulin). Hematology (2017) 22:129–35. doi: 10.1080/10245332.2016.1231968
35. Min GJ, Kim HJ, Kim TG, Hyun YS, Hyun SJ, Baek IC, et al. Specific Donor HLA Allotypes as Predictors of Cytomegalovirus Disease Risk in Acute Myeloid Leukemia. Hla (2020) 96:445–55. doi: 10.1111/tan.13966
36. Park SS, Min GJ, Park S, Lee SE, Yoon JH, Shin SH, et al. Comparable Outcomes Between Unrelated and Haploidentical Stem Cell Transplantation in Adult Patients With Severe Aplastic Anemia. Transplantation (2021) 105(5):1097–105. doi: 10.1097/tp.0000000000003342
37. Gao L, Liu J, Zhang Y, Chen X, Gao L, Zhang C, et al. Low Incidence of Acute Graft-Versus-Host Disease With Short-Term Tacrolimus in Haploidentical Hematopoietic Stem Cell Transplantation. Leuk Res (2017) 57:27–36. doi: 10.1016/j.leukres.2017.02.006
38. Gaballa S, Palmisiano N, Alpdogan O, Carabasi M, Filicko-O’Hara J, Kasner M, et al. A Two-Step Haploidentical Versus a Two-Step Matched Related Allogeneic Myeloablative Peripheral Blood Stem Cell Transplantation. Biol Blood Marrow Transplant (2016) 22:141–8. doi: 10.1016/j.bbmt.2015.09.017
39. Kaynar L, Demir K, Turak EE, Öztürk ÇP, Zararsız G, Gönen ZB, et al. Tcrαβ-Depleted Haploidentical Transplantation Results in Adult Acute Leukemia Patients. Hematology (2017) 22:136–44. doi: 10.1080/10245332.2016.1238182
40. Erbey F, Akçay A, Atay D, Ovalı E, Öztürk G. Comparison of Outcomes After HLA-Matched Unrelated and αβ T-Cell-Depleted Haploidentical Hematopoietic Stem Cell Transplantation for Children With High-Risk Acute Leukemia. Pediatr Transplant (2018) 22:e13192. doi: 10.1111/petr.13192
41. Kang SH, Yoo JW, Seo JK, Kim H, Koh KN, Choi ES, et al. The Role of Interim-Foscarnet Prophylaxis in Preventing Cytomegalovirus Infection After Ex Vivo αβ T Cell-Depleted Haploidentical Hematopoietic Cell Transplant in Children. Bone Marrow Transplant (2021) 56(2):505–7. doi: 10.1038/s41409-020-01020-z
42. Bertaina A, Merli P, Rutella S, Pagliara D, Bernardo ME, Masetti R, et al. HLA-Haploidentical Stem Cell Transplantation After Removal of αβ+ T and B Cells in Children With Nonmalignant Disorders. Blood (2014) 124:822–6. doi: 10.1182/blood-2014-03-563817
43. Mitchell R, Cole T, Shaw PJ, Mechinaud F, O’Brien T, Fraser C. TCR α+β+/CD19+ Cell–Depleted Hematopoietic Stem Cell Transplantation for Pediatric Patients. Pediatr Transplant (2019) 23:e13517. doi: 10.1111/petr.13517
44. Airoldi I, Bertaina A, Prigione I, Zorzoli A, Pagliara D, Cocco C, et al. γδ T-Cell Reconstitution After HLA-Haploidentical Hematopoietic Transplantation Depleted of TCR-αβ+/CD19+ Lymphocytes. Blood (2015) 125:2349–58. doi: 10.1182/blood-2014-09-599423
45. Nazir HF, Ba Alawi FS, Al Hosni S, Al Rawas A, Dennison D. T Cell Depleted Haploidentical Hematopoietic Stem Cell Transplantation for Patients With Familial Hemophagocytic Lymphohistiocytosis Who Do Not Have Matched Family Donors: Experience in Oman. Biol Blood Marrow Transplant (2020) 26:1119–23. doi: 10.1016/j.bbmt.2020.02.014
46. Prezioso L, Manfra I, Bonomini S, Schifano C, Segreto R, Monti A, et al. Haploidentical Hematopoietic Stem Cell Transplantation in Adults Using the αβtcr/CD19-Based Depletion of G-CSF-Mobilized Peripheral Blood Progenitor Cells. Bone Marrow Transplant (2019) 54:698–702. doi: 10.1038/s41409-019-0608-z
47. Gaziev J, Isgrò A, Sodani P, Paciaroni K, De Angelis G, Marziali M, et al. Haploidentical HSCT for Hemoglobinopathies: Improved Outcomes With Tcrαβ(+)/CD19(+)-Depleted Grafts. Blood Adv (2018) 2:263–70. doi: 10.1182/bloodadvances.2017012005
48. Bleakley M, Heimfeld S, Loeb KR, Jones LA, Chaney C, Seropian S, et al. Outcomes of Acute Leukemia Patients Transplanted With Naive T Cell–Depleted Stem Cell Grafts. J Clin Invest (2015) 125:2677–89. doi: 10.1172/JCI81229
49. Triplett BM, Shook DR, Eldridge P, Li Y, Kang G, Dallas M, et al. Rapid Memory T-Cell Reconstitution Recapitulating CD45RA-Depleted Haploidentical Transplant Graft Content in Patients With Hematologic Malignancies. Bone Marrow Transplant (2015) 50:968–77. doi: 10.1038/bmt.2014.324
50. Triplett BM, Muller B, Kang G, Li Y, Cross SJ, Moen J, et al. Selective T-Cell Depletion Targeting CD45RA Reduces Viremia and Enhances Early T-Cell Recovery Compared With CD3-Targeted T-Cell Depletion. Transplant Infect Dis (2018) 20:e12823. doi: 10.1111/tid.12823
51. Goldsmith SR, Abid MB, Auletta JJ, Bashey A, Beitinjaneh A, Castillo P, et al. Posttransplant Cyclophosphamide Is Associated With Increased Cytomegalovirus Infection: A CIBMTR Analysis. Blood (2021) 137:3291–305. doi: 10.1182/blood.2020009362
52. Fayard A, Daguenet E, Blaise D, Chevallier P, Labussière H, Berceanu A, et al. Evaluation of Infectious Complications After Haploidentical Hematopoietic Stem Cell Transplantation With Post-Transplant Cyclophosphamide Following Reduced-Intensity and Myeloablative Conditioning: A Study on Behalf of the Francophone Society of Stem Cell Transplantation and Cellular Therapy (SFGM-Tc). Bone Marrow Transplant (2019) 54:1586–94. doi: 10.1038/s41409-019-0475-7
53. Crocchiolo R, Bramanti S, Vai A, Sarina B, Mineri R, Casari E, et al. Infections After T-Replete Haploidentical Transplantation and High-Dose Cyclophosphamide as Graft-Versus-Host Disease Prophylaxis. Transplant Infect Dis (2015) 17:242–9. doi: 10.1111/tid.12365
54. Esquirol A, Pascual MJ, Kwon M, Pérez A, Parody R, Ferra C, et al. Severe Infections and Infection-Related Mortality in a Large Series of Haploidentical Hematopoietic Stem Cell Transplantation With Post-Transplant Cyclophosphamide. Bone Marrow Transplant (2021) 56:2432–44. doi: 10.1038/s41409-021-01328-4
55. Huntley D, Giménez E, Pascual MJ, Hernández-Boluda JC, Gago B, Vázquez L, et al. Incidence, Features, and Outcomes of Cytomegalovirus DNAemia in Unmanipulated Haploidentical Allogeneic Hematopoietic Stem Cell Transplantation With Post-Transplantation Cyclophosphamide. Transpl Infect Dis (2020) 22:e13206. doi: 10.1111/tid.13206
56. Crocchiolo R, Castagna L, Furst S, Devillier R, Sarina B, Bramanti S, et al. The Patient’s CMV Serological Status Affects Clinical Outcome After T-Cell Replete Haplo-HSCT and Post-Transplant Cyclophosphamide. Bone Marrow Transplant (2016) 51:1134–6. doi: 10.1038/bmt.2016.69
57. Al Malki MM, Dadwal S, Yang D, Mokhtari S, Cao T, Gendzekhadze K, et al. High Incidence of CMV Reactivation After Haploidentical Donor Hematopoietic Cell Transplantation Using High-Dose Post-Transplant Cyclophosphamide, and Its Impact on Transplant Outcomes. Blood (2017) 130:4494–4. doi: 10.1182/blood.V130.Suppl_1.4494.4494
58. Huntley D, Giménez E, Pascual MJ, Remigia MJ, Amat P, Vázquez L, et al. Reconstitution of Cytomegalovirus-Specific T-Cell Immunity Following Unmanipulated Haploidentical Allogeneic Hematopoietic Stem Cell Transplantation With Posttransplant Cyclophosphamide. Bone Marrow Transplant (2020) 55:1347–56. doi: 10.1038/s41409-020-0865-x
59. Irene G-C, Albert E, Anna B-V, Rahinatu A, Silvana N, Silvana S, et al. Patterns of Infection and Infectious-Related Mortality in Patients Receiving Post-Transplant High Dose Cyclophosphamide as Graft-Versus-Host-Disease Prophylaxis: Impact of HLA Donor Matching. Bone Marrow Transplant (2021) 56(4):818–27. doi: 10.1038/s41409-020-01092-x
60. Hammerstrom AE, Lombardi LR, Pingali SR, Rondon G, Chen J, Milton DR, et al. Prevention of Cytomegalovirus Reactivation in Haploidentical Stem Cell Transplantation. Biol Blood Marrow Transplant (2018) 24:353–8. doi: 10.1016/j.bbmt.2017.09.018
61. Uppuluri R, Sivasankaran M, Patel S, Swaminathan VV, Ramanan KM, Ravichandran N, et al. Haploidentical Stem Cell Transplantation With Post-Transplant Cyclophosphamide for Primary Immune Deficiency Disorders in Children: Challenges and Outcome From a Tertiary Care Center in South India. J Clin Immunol (2019) 39:182–7. doi: 10.1007/s10875-019-00600-z
62. Arcuri LJ, Nabhan SK, Cunha R, Nichele S, Ribeiro AAF, Fernandes JF, et al. Impact of CD34 Cell Dose and Conditioning Regimen on Outcomes After Haploidentical Donor Hematopoietic Stem Cell Transplantation With Post-Transplantation Cyclophosphamide for Relapsed/Refractory Severe Aplastic Anemia. Biol Blood Marrow Transplant (2020) 26:2311–7. doi: 10.1016/j.bbmt.2020.09.007
63. Raj RV, Hari P, Pasquini M, Epperla N, D’Souza A, Fenske T, et al. Impact of Haploidentical Hematopoietic Cell Transplantation Conditioning Intensity on the Incidence and Severity of Post-Transplantation Viral Infections. Bone Marrow Transplant (2016) 51:1602–4. doi: 10.1038/bmt.2016.216
64. Katsanis E, Maher K, Roe DJ, Simpson RJ. Progressive Substitution of Posttransplant Cyclophosphamide With Bendamustine: A Phase I Study in Haploidentical Bone Marrow Transplantation. eJHaem (2020) 1:286–92. doi: 10.1002/jha2.20
65. Goldsmith SR, Slade M, DiPersio JF, Westervelt P, Lawrence SJ, Uy GL, et al. Cytomegalovirus Viremia, Disease, and Impact on Relapse in T-Cell Replete Peripheral Blood Haploidentical Hematopoietic Cell Transplantation With Post-Transplant Cyclophosphamide. Haematologica (2016) 101:e465–8. doi: 10.3324/haematol.2016.149880
66. Solomon SR, Sizemore CA, Sanacore M, Zhang X, Brown S, Holland HK, et al. Total Body Irradiation–Based Myeloablative Haploidentical Stem Cell Transplantation Is a Safe and Effective Alternative to Unrelated Donor Transplantation in Patients Without Matched Sibling Donors. Biol Blood Marrow Transplant (2015) 21:1299–307. doi: 10.1016/j.bbmt.2015.03.003
67. Stocker N, Gaugler B, Labopin M, Farge A, Ye Y, Ricard L, et al. High-Dose Post-Transplant Cyclophosphamide Impairs γδ T-Cell Reconstitution After Haploidentical Haematopoietic Stem Cell Transplantation Using Low-Dose Antithymocyte Globulin and Peripheral Blood Stem Cell Graft. Clin Trans Immunol (2020) 9:e1171. doi: 10.1002/cti2.1171
68. Oltolini C, Greco R, Galli L, Clerici D, Lorentino F, Xue E, et al. Infections After Allogenic Transplant With Post-Transplant Cyclophosphamide: Impact of Donor HLA Matching. Biol Blood Marrow Transplant (2020) 26:1179–88. doi: 10.1016/j.bbmt.2020.01.013
69. Slade M, Goldsmith S, Romee R, DiPersio JF, Dubberke ER, Westervelt P, et al. Epidemiology of Infections Following Haploidentical Peripheral Blood Hematopoietic Cell Transplantation. Transpl Infect Dis (2017) 19:e12629. doi: 10.1111/tid.12629
70. Montoro J, Piñana JL, Hernández-Boluda JC, Hernani R, Lorenzo I, Pérez A, et al. Uniform Graft-Versus-Host Disease Prophylaxis With Posttransplant Cyclophosphamide, Sirolimus, and Mycophenolate Mofetil Following Hematopoietic Stem Cell Transplantation From Haploidentical, Matched Sibling and Unrelated Donors. Bone Marrow Transplant (2020) 55:2147–59. doi: 10.1038/s41409-020-0921-6
71. Cieri N, Greco R, Crucitti L, Morelli M, Giglio F, Levati G, et al. Post-Transplantation Cyclophosphamide and Sirolimus After Haploidentical Hematopoietic Stem Cell Transplantation Using a Treosulfan-Based Myeloablative Conditioning and Peripheral Blood Stem Cells. Biol Blood Marrow Transplant (2015) 21:1506–14. doi: 10.1016/j.bbmt.2015.04.025
72. Law AD, Salas MQ, Lam W, Michelis FV, Thyagu S, Kim DDH, et al. Reduced-Intensity Conditioning and Dual T Lymphocyte Suppression With Antithymocyte Globulin and Post-Transplant Cyclophosphamide as Graft-Versus-Host Disease Prophylaxis in Haploidentical Hematopoietic Stem Cell Transplants for Hematological Malignancies. Biol Blood Marrow Transplant (2018) 24:2259–64. doi: 10.1016/j.bbmt.2018.07.008
73. Salas MQ, Prem S, Atenafu EG, Datt Law A, Lam W, Al-Shaibani Z, et al. Dual T-Cell Depletion With ATG and PTCy for Peripheral Blood Reduced Intensity Conditioning Allo-HSCT Results in Very Low Rates of GVHD. Bone Marrow Transplant (2020) 55:1773–83. doi: 10.1038/s41409-020-0813-9
74. Salas MQ, Prem S, Atenafu EG, Law AD, Lam W, Al-Shaibani Z, et al. Reduced Intensity Allogeneic Stem Cell Transplant With Anti-Thymocyte Globulin and Post-Transplant Cyclophosphamide in Acute Myeloid Leukemia. Eur J Haematol (2019) 103:510–8. doi: 10.1111/ejh.13321
75. Lint CH, Su YJ, Hsu CY, Wang PN, Teng CL. Haploidentical Allogeneic Hematopoietic Stem Cell Transplantation Increases the Risk of Cytomegalovirus Infection in adult Patients With Acute Leukemia. Transpl Infect Dis (2019) 21(4):e13096.
76. Wang Y, Chang Y-J, Chen L, Xu L-P, Bian Z-L, Zhang X-H, et al. Low-Dose Post-Transplant Cyclophosphamide can Mitigate GVHD and Enhance the G-CSF/ATG Induced GVHD Protective Activity and Improve Haploidentical Transplant Outcomes. OncoImmunology (2017) 6:e1356152. doi: 10.1080/2162402X.2017.1356152
77. Wang Y, Wu D-P, Liu Q-F, Xu L-P, Liu K-Y, Zhang X-H, et al. Low-Dose Post-Transplant Cyclophosphamide and Anti-Thymocyte Globulin as an Effective Strategy for GVHD Prevention in Haploidentical Patients. J Hematol Oncol (2019) 12:88. doi: 10.1186/s13045-019-0781-y
78. Tischer J, Engel N, Fritsch S, Prevalsek D, Hubmann M, Schulz C, et al. Virus Infection in HLA-Haploidentical Hematopoietic Stem Cell Transplantation: Incidence in the Context of Immune Recovery in Two Different Transplantation Settings. Ann Hematol (2015) 94:1677–88. doi: 10.1007/s00277-015-2423-y
79. ElGohary G, El Fakih R, de Latour R, Risitano A, Marsh J, Schrezenmeier H, et al. Haploidentical Hematopoietic Stem Cell Transplantation in Aplastic Anemia: A Systematic Review and Meta-Analysis of Clinical Outcome on Behalf of the Severe Aplastic Anemia Working Party of the European Group for Blood and Marrow Transplantation (SAAWP of EBMT). Bone Marrow Transplant (2020) 55:1906–17. doi: 10.1038/s41409-020-0897-2
80. Li J-J, Huang X, Wang H, Guo X-Y, Ge S-X, Zhang J. Baseline Antibody Level may Help Predict the Risk of Active Human Cytomegalovirus Infection in a HCMV Seropositive Population. Eur J Clin Microbiol Infect Dis (2017) 36:863–8. doi: 10.1007/s10096-016-2873-8
81. Lu S-C, Chin L-T, Wu F-M, Hsieh G-J, Haung S-P, Chen J-C, et al. Seroprevalence of CMV Antibodies in a Blood Donor Population and Premature Neonates in the South-Central Taiwan. Kaohsiung J Med Sci (1999) 15:603–10.
82. Zuhair M, Smit GSA, Wallis G, Jabbar F, Smith C, Devleesschauwer B, et al. Estimation of the Worldwide Seroprevalence of Cytomegalovirus: A Systematic Review and Meta-Analysis. Rev Med Virol (2019) 29:e2034. doi: 10.1002/rmv.2034
83. Lachmann R, Loenenbach A, Waterboer T, Brenner N, Pawlita M, Michel A, et al. Cytomegalovirus (CMV) Seroprevalence in the Adult Population of Germany. PloS One (2018) 13:e0200267. doi: 10.1371/journal.pone.0200267
84. Antona D, Lepoutre A, Fonteneau L, Baudon C, Halftermeyer-Zhou F, Le Strat Y, et al. Seroprevalence of Cytomegalovirus Infection in France in 2010. Epidemiol Infect (2017) 145:1471–8. doi: 10.1017/S0950268817000103
85. Luo XH, Chang YJ, Huang XJ. Improving Cytomegalovirus-Specific T Cell Reconstitution After Haploidentical Stem Cell Transplantation. J Immunol Res (2014) 2014. doi: 10.1155/2014/631951
86. Luo XH, Huang XJ, Li D, Liu KY, Xu LP, Liu DH. Immune Reconstitution to Cytomegalovirus Following Partially Matched-Related Donor Transplantation: Impact of In Vivo T-Cell Depletion and Granulocyte Colony-Stimulating Factor-Primed Peripheral Blood/Bone Marrow Mixed Grafts. Transplant Infect Dis (2013) 15:22–33. doi: 10.1111/j.1399-3062.2012.00722.x
87. Luo X-H, Huang X-J, Liu K-Y, Xu L-P, Liu D-H. Protective Immunity Transferred by Infusion of Cytomegalovirus-Specific CD8+ T Cells Within Donor Grafts: Its Associations With Cytomegalovirus Reactivation Following Unmanipulated Allogeneic Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant (2010) 16:994–1004. doi: 10.1016/j.bbmt.2010.02.007
88. Kato R, Tamaki H, Ikegame K, Yoshihara S, Kaida K, Taniguchi K, et al. Early Detection of Cytomegalovirus-Specific Cytotoxic T Lymphocytes Against Cytomegalovirus Antigenemia in Human Leukocyte Antigen Haploidentical Hematopoietic Stem Cell Transplantation. Ann Hematol (2015) 94:1707–15. doi: 10.1007/s00277-015-2446-4
89. Noviello M, Forcina A, Veronica V, Crocchiolo R, Stanghellini MT, Carrabba M, et al. Early Recovery of CMV Immunity After HLA-Haploidentical Hematopoietic Stem Cell Transplantation as a Surrogate Biomarker for a Reduced Risk of Severe Infections Overall. Bone Marrow Transplant (2015) 50:1262–4. doi: 10.1038/bmt.2015.132
90. Huntley D, Giménez E, Pascual MJ, Vázquez L, Amat P, Remigia MJ, et al. Peripheral Blood Regulatory T Cells and Occurrence of Cytomegalovirus DNAemia After Unmanipulated Haploidentical Allogeneic Hematopoietic Stem Cell Transplantation With Posttransplant Cyclophosphamide. Bone Marrow Transplant (2020) 55:1493–6. doi: 10.1038/s41409-020-0950-1
91. van Beek JJP, Puccio S, Roberto A, De Paoli F, Graziano G, Salviato E, et al. Single-Cell Profiling Reveals the Dynamics of Cytomegalovirusspecific T-Cells in Haploidentical Hematopoietic Stem Cell Transplantation. Haematologica (2021) 106(10):2768–73. doi: 10.3324/haematol.2020.276352
92. Jin F, Lin H, Gao S, Wang H, Yan H, Guo J, et al. Characterization of Ifnγ-Producing Natural Killer Cells Induced by Cytomegalovirus Reactivation After Haploidentical Hematopoietic Stem Cell Transplantation. Oncotarget (2017) 8:51–63. doi: 10.18632/oncotarget.13916
93. Jang JE, Hwang DY, Chung H, Kim SJ, Eom JI, Jeung HK, et al. Early Cytomegalovirus Reactivation and Expansion of CD56(bright)CD16(dim/-)DNAM1(+) Natural Killer Cells Are Associated With Antileukemia Effect After Haploidentical Stem Cell Transplantation in Acute Leukemia. Biol Blood Marrow Transplant (2019) 25:2070–8. doi: 10.1016/j.bbmt.2019.06.008
94. Muccio L, Bertaina A, Falco M, Pende D, Meazza R, Lopez-Botet M, et al. Analysis of Memory-Like Natural Killer Cells in Human Cytomegalovirus-Infected Children Undergoing αβ+T and B Cell-Depleted Hematopoietic Stem Cell Transplantation for Hematological Malignancies. Haematologica (2016) 101:371–81. doi: 10.3324/haematol.2015.134155
95. Zhao XY, Luo XY, Yu XX, Zhao XS, Han TT, Chang YJ, et al. Recipient-Donor KIR Ligand Matching Prevents CMV Reactivation Post-Haploidentical T Cell-Replete Transplantation. Br J Haematol (2017) 177:766–81. doi: 10.1111/bjh.14622
96. Hu L-J, Cao X-H, Yu X-X, Liu X-F, Zhao X-S, Chang Y-J, et al. NK Cell Reconstitution Following Unmanipulated HLA-Mismatched/Haploidentical Transplantation Compared With Matched Sibling Transplantation. Sci China Life Sci (2020) 63:781–4. doi: 10.1007/s11427-018-9565-5
97. Zaghi E, Calvi M, Puccio S, Spata G, Terzoli S, Peano C, et al. Single-Cell Profiling Identifies Impaired Adaptive NK Cells Expanded After HCMV Reactivation in Haploidentical-HSCT. JCI Insight (2021) 6(12):e146973. doi: 10.1172/jci.insight.146973
98. Park M, Im HJ, Lee Y-J, Park N, Jang S, Kwon SW, et al. Reconstitution of T and NK Cells After Haploidentical Hematopoietic Cell Transplantation Using αβ T Cell-Depleted Grafts and the Clinical Implication of γδ T Cells. Clin Transplant (2018) 32:e13147. doi: 10.1111/ctr.13147
99. Feuchtinger T, Opherk K, Bethge WA, Topp MS, Schuster FR, Weissinger EM, et al. Adoptive Transfer of Pp65-Specific T Cells for the Treatment of Chemorefractory Cytomegalovirus Disease or Reactivation After Haploidentical and Matched Unrelated Stem Cell Transplantation. Blood (2010) 116:4360–7. doi: 10.1182/blood-2010-01-262089
100. Pei XY, Zhao XY, Chang YJ, Liu J, Xu LP, Wang Y, et al. Cytomegalovirus-Specific T-Cell Transfer for Refractory Cytomegalovirus Infection After Haploidentical Stem Cell Transplantation: The Quantitative and Qualitative Immune Recovery for Cytomegalovirus. J Infect Dis (2017) 216:945–56. doi: 10.1093/infdis/jix357
101. Zhao X-Y, Pei X-Y, Chang Y-J, Yu X-X, Xu L-P, Wang Y, et al. First-Line Therapy With Donor-Derived Human Cytomegalovirus (HCMV)–specific T Cells Reduces Persistent HCMV Infection by Promoting Antiviral Immunity After Allogenic Stem Cell Transplantation. Clin Infect Dis (2019) 70:1429–37. doi: 10.1093/cid/ciz368
102. Ke P, Bao X, Zhou J, Li X, Zhuang J, He X, et al. Donor CMV-Specific Cytotoxic T Lymphocytes Successfully Treated Drug-Resistant Cytomegalovirus Encephalitis After Allogeneic Hematopoietic Stem Cell Transplantation. Hematology (2020) 25:43–7. doi: 10.1080/16078454.2019.1710945
103. Maschan M, Blagov S, Shelikhova L, Shekhovtsova Z, Balashov D, Starichkova J, et al. Low-Dose Donor Memory T-Cell Infusion After TCR Alpha/Beta Depleted Unrelated and Haploidentical Transplantation: Results of a Pilot Trial. Bone Marrow Transplant (2018) 53:264–73. doi: 10.1038/s41409-017-0035-y
104. Dunaikina M, Zhekhovtsova Z, Shelikhova L, Glushkova S, Nikolaev R, Blagov S, et al. Safety and Efficacy of the Low-Dose Memory (CD45RA-Depleted) Donor Lymphocyte Infusion in Recipients of αβ T Cell-Depleted Haploidentical Grafts: Results of a Prospective Randomized Trial in High-Risk Childhood Leukemia. Bone Marrow Transplant (2021) 56:1614–24. doi: 10.1038/s41409-021-01232-x
105. Shelikhova L, Glushkova S, Nikolaev R, Dunaikina M, Zhekhovtsova Z, Blagov S, et al. Serotherapy-Free Regimen Improves Non-Relapse Mortality and Immune Recovery Among the Recipients of αβ TCell–Depleted Haploidentical Grafts: Retrospective Study in Childhood Leukemia. Transplant Cell Ther (2021) 27:330.e1–.e9. doi: 10.1016/j.jtct.2021.01.010
106. Castagna L, Valli V, Timofeeva I, Capizzuto R, Bramanti S, Mariotti J, et al. Feasibility and Efficacy of CD45RA+ Depleted Donor Lymphocytes Infusion After Haploidentical Transplantation With Post-Transplantation Cyclophosphamide in Patients With Hematological Malignancies. Transplant Cell Ther (2021) 27:478.e1–.e5. doi: 10.1016/j.jtct.2021.03.010
107. Park HJ, Hong KT, Yun SO, Ahn HY, Choi JY, Shin HY, et al. Successful Treatment of Refractory CMV Colitis After Haploidentical HSCT With Post-Transplant Cyclophosphamide Using CD45RA+ Depleted Donor Lymphocyte Infusion. Bone Marrow Transplant (2020) 55:1674–6. doi: 10.1038/s41409-019-0685-z
108. Uygun V, Karasu G, Daloğlu H, Öztürkmen S, Yalçın K, Çelen SS, et al. Use of Low Cell Dose for Unmanipulated Donor Lymphocyte for Management of Cytomegalovirus Infection: A Single-Center Experience. Pediatr Transplant (2020) 24:e13882. doi: 10.1111/petr.13882
109. Lugthart G, van Ostaijen-ten Dam MM, Jol - van der Zijde CM, van Holten TC, Kester MGD, Heemskerk MHM, et al. Early Cytomegalovirus Reactivation Leaves a Specific and Dynamic Imprint on the Reconstituting T Cell Compartment Long-Term After Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant (2014) 20:655–61. doi: 10.1016/j.bbmt.2014.01.018
110. Raphael I, Marie R, Helene M-T, Marc D, Marc B, Aliénor X, et al. Cytomegalovirus Shapes Long-Term Immune Reconstitution After Allogeneic Stem Cell Transplantation. Haematologica (2015) 100:114–23. doi: 10.3324/haematol.2014.113415
111. Luo XH, Meng Q, Rao M, Liu Z, Paraschoudi G, Dodoo E, et al. The Impact of Inflationary Cytomegalovirus-Specific Memory T Cells on Anti-Tumour Immune Responses in Patients With Cancer. Immunology (2018) 155:294–308. doi: 10.1111/imm.12991
112. Zhang Y-L, Zhu Y, Xiao Q, Wang L, Liu L, Luo X-H. Cytomegalovirus Infection is Associated With AML Relapse After Allo-HSCT: A Meta-Analysis of Observational Studies. Ann Hematol (2019) 98:1009–20. doi: 10.1007/s00277-018-3585-1
113. Elmaagacli AH, Steckel NK, Koldehoff M, Hegerfeldt Y, Trenschel R, Ditschkowski M, et al. Early Human Cytomegalovirus Replication After Transplantation is Associated With a Decreased Relapse Risk: Evidence for a Putative Virus-Versus-Leukemia Effect in Acute Myeloid Leukemia Patients. Blood (2011) 118:1402–12. doi: 10.1182/blood-2010-08-304121
114. Green ML, Leisenring WM, Xie H, Walter RB, Mielcarek M, Sandmaier BM, et al. CMV Reactivation After Allogeneic HCT and Relapse Risk: Evidence for Early Protection in Acute Myeloid Leukemia. Blood J Am Soc Hematol (2013) 122:1316–24. doi: 10.1182/blood-2013-02-487074
115. Teira P, Battiwalla M, Ramanathan M, Barrett AJ, Ahn KW, Chen M, et al. Early Cytomegalovirus Reactivation Remains Associated With Increased Transplant-Related Mortality in the Current Era: A CIBMTR Analysis. Blood (2016) 127:2427–38. doi: 10.1182/blood-2015-11-679639
116. Cantoni N, Hirsch HH, Khanna N, Gerull S, Buser A, Bucher C, et al. Evidence for a Bidirectional Relationship Between Cytomegalovirus Replication and Acute Graft-Versus-Host Disease. Biol Blood Marrow Transplant (2010) 16:1309–14. doi: 10.1016/j.bbmt.2010.03.020
Keywords: cytomegalovirus, infection, immune reconstitution, haploidentical, stem cell transplantation
Citation: Luo X-H, Zhu Y, Chen Y-T, Shui L-P and Liu L (2021) CMV Infection and CMV-Specific Immune Reconstitution Following Haploidentical Stem Cell Transplantation: An Update. Front. Immunol. 12:732826. doi: 10.3389/fimmu.2021.732826
Received: 29 June 2021; Accepted: 14 September 2021;
Published: 28 October 2021.
Edited by:
Marco Antonio Moro-García, Central University Hospital of Asturias, SpainReviewed by:
Yu Wang, Peking University People’s Hospital, ChinaLuca Castagna, Azienda Ospedaliera Ospedali Riuniti Villa Sofia Cervello, Italy
Copyright © 2021 Luo, Zhu, Chen, Shui and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiao-Hua Luo, eGlhb2h1YS5sdW9AZ21haWwuY29t; orcid.org/0000-0002-0657-7738
 Xiao-Hua Luo
Xiao-Hua Luo Yan Zhu2
Yan Zhu2