- 1Pharmacy Department, National Center for Cancer Care and Research, Hamad Medical Corporation, Doha, Qatar
- 2Department of Pharmacy Practice, College of Clinical Pharmacy, King Faisal University, Hofuf, Saudi Arabia
- 3Division of Cardiology, Department of Medicine, Harvard Medical School, Boston, MA, United States
- 4Clinical Pharmacy Department, School of Pharmacy, New Giza University, Giza, Egypt
- 5Faculty of Veterinary Medicine, Damanhour University, Damanhour, Egypt
- 6Department of Histology and Cytology, Faculty of Veterinary Medicine, Damanhour University, Damanhour, Egypt
- 7Basic Sciences Department, Faculty of Medicine, Algalala University, Suez, Egypt
- 8Medical Oncology-Hematology Section, National Center for Cancer Care and Research, Hamad Medical Corporation, Doha, Qatar
- 9National Centre for Cancer Care and Research, Hamad Medical Corporation, Doha, Qatar
There has been less volume of literature focusing on the Immune-related Hematological Adverse Drug Events (Hem-irAEs) of Immune Checkpoint Inhibitors (ICPis) in cancer patients. Furthermore, there has been no consensus about the management of hematological toxicity from immunotherapy in the recently published practice guidelines by the European Society for Medical Oncology (ESMO). We conducted a systematic review of case reports/series to describe the diagnosis and management of potentially rare and unrecognized Hem-irAEs. We searched Medline, OVID, Web of Science for eligible articles. Data were extracted on patient characteristics, Hem-irAEs, and management strategies. We performed quality assessment using the Pierson-5 evaluation scheme and causality assessment using the Naranjo scale. Our search retrieved 49 articles that described 118 cases. The majority of patients had melanoma (57.6%) and lung cancer (26.3%). The most common Hem-irAEs reported with ICPis (such as nivolumab, ipilimumab, and pembrolizumab) were thrombocytopenia, hemolytic and aplastic anemias. Less reported adverse events included agranulocytosis and neutropenia. Steroids were commonly used to treat these adverse events with frequent success. Other used strategies included intravenous immunoglobulins (IVIG), rituximab, and transfusion of blood components. The findings of this review provide more insights into the diagnosis and management of the rarely reported Hem-irAEs of ICPis.
Introduction
In the past decade, the enthusiasm for connecting the immune system and malignancy has expanded. Exploiting the host's immune system to treat cancers depends on immune surveillance: the ability of the immune system to identify foreign neo-antigens and target them for elimination (1). Immune checkpoint receptors, i.e., cytotoxic T-lymphocyte-associated protein 4 CTLA4 antibody ipilimumab, and programmed cell death protein-1 (PD-1) are critical for the physiological responses of the immune system. Checkpoint signaling triggers immune tolerance of T-cell activation to avoid autoimmunity and the adverse effects of excessive inflammatory responses. Tumor cells utilize these mechanisms to avoid destruction by the immune system (2).
In August, 18, 2010, the FDA approved the CTLA-4 ipilimumab antibody as the first ICPi for the treatment of metastatic melanoma (3). The filing was based on results from the primary analysis of the pivotal MDX010-020 trial, which were published online in the New England Journal of Medicine and presented in June 2010 during a plenary session at the 46th Annual Meeting of the American Society of Clinical Oncology (3). Despite its approval, ICPis have not been widely used except in the last 2 years. Recently, PD-1 inhibitors were approved for the treatment of non-small cell lung cancer (NSCLC) (4). Following their approval, these immunotherapeutics became integral parts of the treatment protocols against melanoma and NSCLC. Furthermore, they have shown promising responses [objective response rates (ORRs)] against different cancers, including mismatch repair deficient colorectal cancer (60%) and Hodgkin's disease (65–85%) (5).
Although the side effects of immunotherapy are less than chemotherapeutic agents (4), immunotherapy still may cause dermatological (reticular, maculopapular erythematous rash, and mucositis), gastrointestinal (diarrhea and colitis), hepatic (elevation of liver enzymes in serum), and endocrine adverse effects (involving pituitary, adrenal, or thyroid glands). This is because the immune response triggered by these drugs is not completely tumor-specific (6). The management of their adverse events usually includes various forms and regimens of corticosteroids (7).
With the expanding use of ICPis in clinical practice, more rare side effects are being discovered. Some Hem-irAEs were described, including immune thrombocytopenia, autoimmune hemolytic anemia, agranulocytosis, or pure red cell aplasia (8). The evidence focusing on the Hem-irAEs of ICPis is scarce. Moreover, there is no consensus on the management of hematologic toxicity from immunotherapy in the recently published practice guideline by ESMO (9). We aimed to evaluate the published literature on this topic and summarize the successful management approaches of the rare side effects.
Methods
Data Sources and Searches
We commenced this study in May 2018 and included all available updates published since 2008 till the present time.
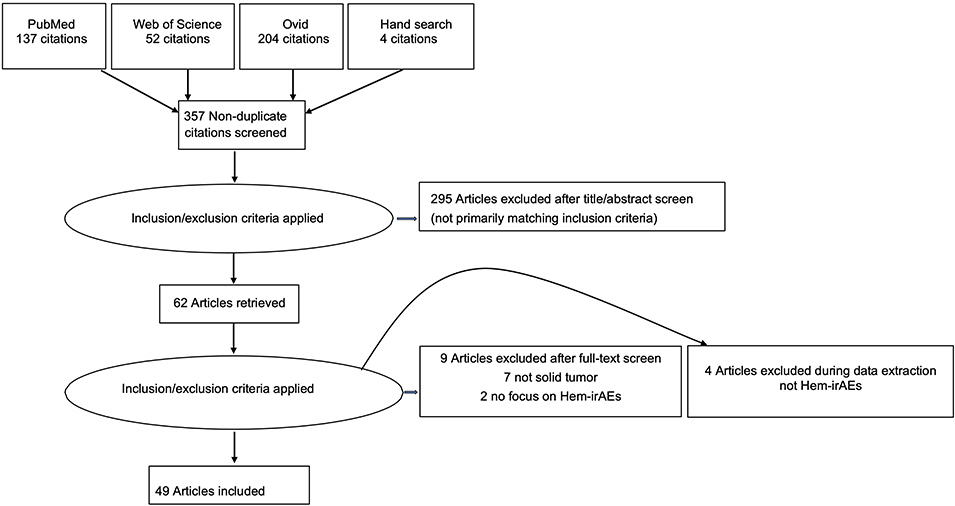
We conducted literature search using different databases: Medline, OVID, and Web of Science. Furthermore, we searched the gray literature; conference proceedings; using Web of Conferences, Open Grey up to January 2019. We searched the bibliographies of relevant studies for any eligible case reports/series up to January 2019. The flow of the article selection process is presented in the graphical abstract as Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) figure. We used no time limit to date.
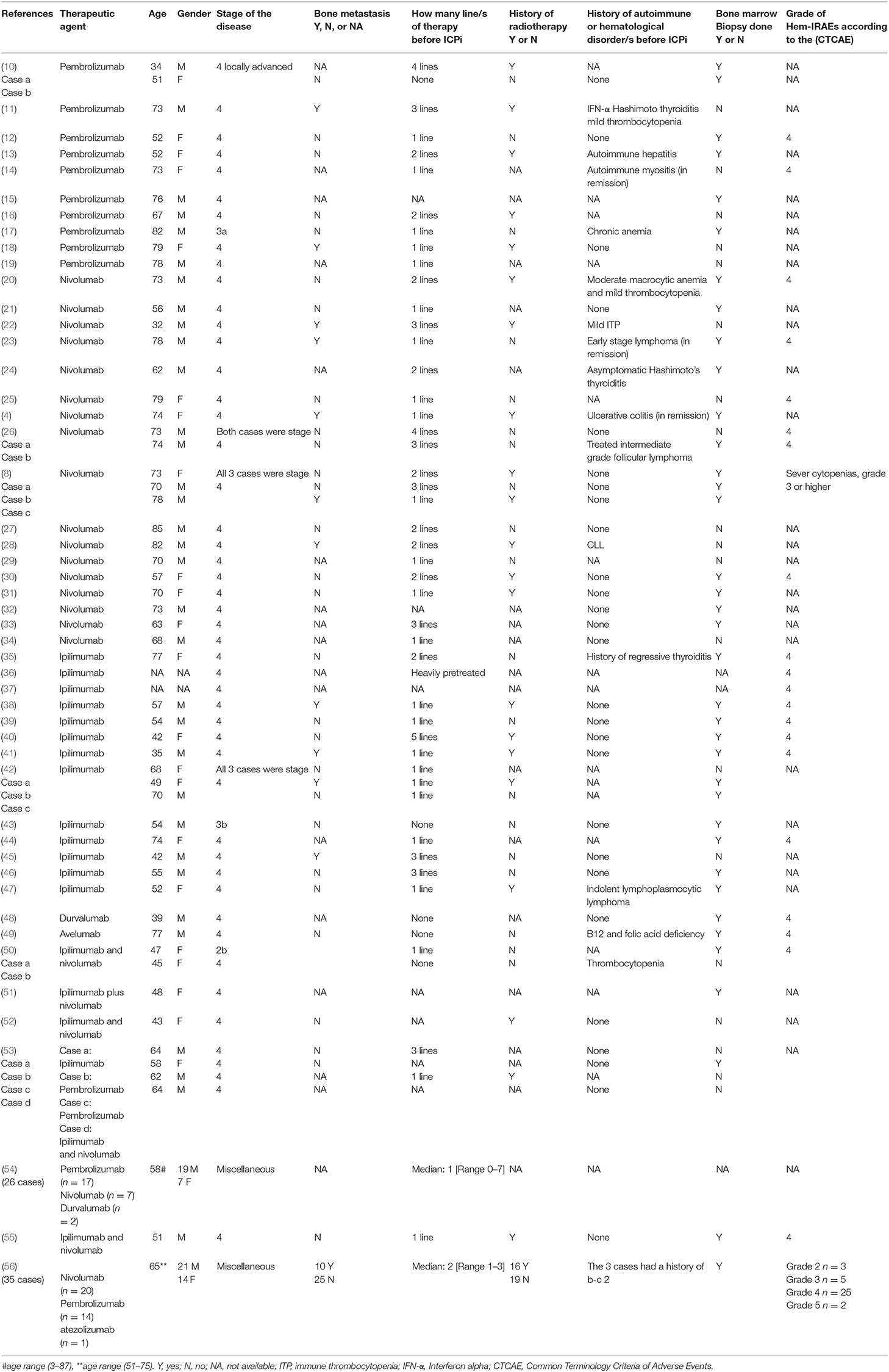
We used well-defined keywords. The search terms are listed in Appendix 1. The following keywords: (immune checkpoint inhibitors), (ICPis), (immunotherapy) (ipilimumab), (programmed cell death), (Programmed Cell Death 1 Receptor), (Programmed death ligand), (pembrolizumab), (nivolumab), (atezolizumab), (durvalumab), (avelumab) (adverse drug reaction), (adverse effects) (hematological adverse effect), Immune related adverse event (pancytopenia), (immune thrombocytopenic purpura), (thrombocytopenia), (leucopenia), (anemia) and (neutropenia) were entered, and the search was limited to articles in English. A summary of the 49 enrolled studies, clustered based on the medication used and Hem-irAEs experienced is shown in Table 1.
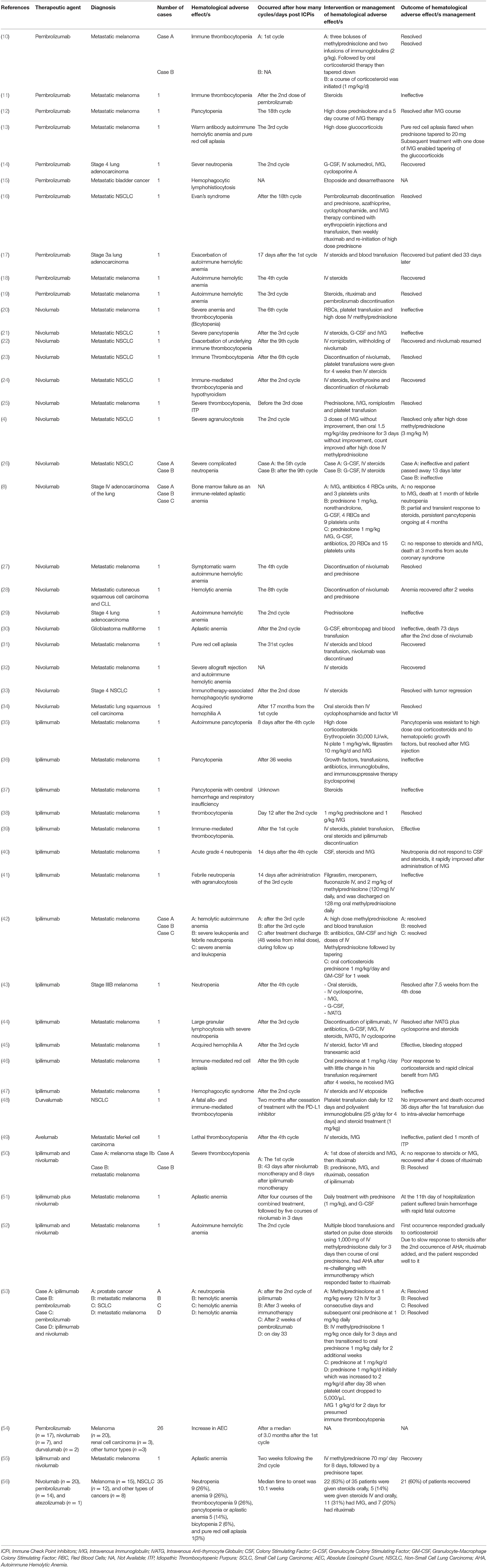
Table 1. Summary of available literature about immune check point inhibitors-associated hematological adverse effects.
Initial screening of the eligible articles was done independently by two authors NO and NE. The articles were screened first based on their titles and abstracts, and then the full text was reviewed to decide the eligibility. Any conflict was solved by a third author KE. Only full-text articles published in peer-reviewed journals were retrieved for review according to the following criteria. AA, MY, AH, SE contributed to data analysis.
Inclusion Criteria
1. Case reports/series of solid tumors;
2. Reporting Hem-irAEs;
3. Using ICPis, monotherapy or combinations either as part of a clinical trial or during clinical practice;
4. English language;
5. Adults or pediatrics.
Exclusion Criteria
6. Other irAEs than Hem-irAEs;
7. Non-solid tumors;
8. Article reporting side effects which are not immune related;
9. Use other medications than ICPis causing Hem-irAEs;
10. Use of non-FDA approved ICPis up to the date of data extraction.
Data Extraction and Quality Assessment
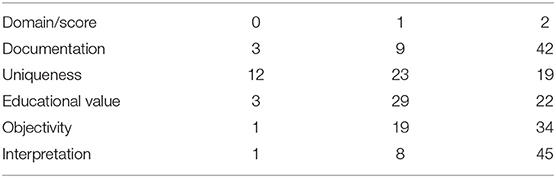
Data was extracted by NO and NE, then was revised by KE. The extracted data included type of cancer, ICPis, number of cases, Hem-irAEs, onset of the adverse events, management of Hem-irAEs, and management outcomes. We used the Pierson-5 evaluation scheme (57) to assess quality of case reports based on 5 domains: documentation, uniqueness, educational value, objectivity, and interpretation as shown in Table 2. Each domain is scored, for example (0, 1, or 2 points, the upper score is 10 points). When a case report scores 9–10 points, the report contributes to the literature; a 6–8 points indicates validity and clinical value of the report are doubtful; a 5 points or less indicates insufficient quality. The assessment was carried out by KE and a random sample was crosschecked by NO and NE.
Causality Assessment
Each case report was assessed according to Naranjo scale (58) for causality as shown in Supplementary Table 1. Naranjo scale was used for causality assessment of the case reports, that allows categorical classification of adverse events as “definite,” “probable,” “possible,” or “doubtful” based on the answers to 10 questions. One investigator KE carried out the assessment and NO and NE randomly re-checked it.
Results
Patient Characteristics
Patient characteristics are described in Table 3. One hundred and eighteen cases were identified in 49 articles. The median age of cases was 54 years (range 32–85 years). The majority of cases were males (n = 73, 61.8%). Most patients had melanoma (57.6%) and lung cancer (26.3%). Other cancer sites included prostate (n = 1), bladder (n = 1), glioblastoma multiforme (n = 1), renal cell carcinoma (n = 4), and others (n = 10). Fifty three (44.9%) cases were labeled as stage 4, two cases as stage 3, one case as locally advanced disease, while in 61 (51.7%) cases, the stage of cancer was not mentioned. Twenty one (17.8%) cases were confirmed to have bone metastasis, while 55 (46.6%) cases did not have bone metastasis and no data were mentioned for the remaining 42 (35.5%) cases.
Thirty seven (31.3%) cases were treated with radiotherapy, while 38 (32.2%) cases did not receive radiotherapy and no history of exposure to radiotherapy in 43 (36.5%) cases.
Heavily pretreated patients were defined as patients who previously received two or more lines of treatment; 56 (47.5%) cases were heavily pretreated; 50 (42.4) cases received only one previous line of treatment; 5 cases were treatment naïve. With respect to history of autoimmune or hematological disorders before the use of ICPis; no data was provided in 73 (61.8%) cases, while 18 (15.3%) cases had history of either autoimmune or hematological disorder before ICPis usage, while 27 (22.9%) cases did not have history. A bone marrow biopsy was done to confirm the Hem-irAEs in 71 (61.2%) cases, but it was not done in 19 (16.1%) cases. The grade of Hem-irAEs was labeled as grade 2 in 3 cases, grade 3 in 5 cases, grade 4 in 50 (42.3%) case, and grade 5 in 2 cases.
Nivolumab
Seventeen case studies (out of 49) reported Hem-irAEs with nivolumab in 20 cases (13 lung cancer, 5 melanoma, 1 cutaneous squamous cell carcinoma, and 1 glioblastoma). Anemia was reported in 7 cases; two had aplastic anemia and five had hemolytic anemia. Thrombocytopenia was reported in five cases. Bone marrow failure was reported in three cases, pancytopenia in one case, neutropenia in one case, red cell aplasia in one case, hemophagocytic syndrome in one case, agranulocytosis in one case and acquired hemophilia A in one case.
Treatment was reported for all patients. Resolution of the adverse events was reported in 11 cases (55%) and treatment was ineffective in 8 cases (40%). One case showed partial and transient response to treatment. In the 11 cases that showed response, the most common treatment for Hem-irAEs was IV corticosteroids, however, IV romiplostim, platelets transfusion, IVIG, and oral steroids were used. Many patients had to discontinue nivolumab with the treatment used.
Another two-case series reported Hem-irAEs with nivolumab in 27 cases. An increase in the absolute eosinophil count was reported by Bernard-Tessier et al. (54). No treatment was mentioned in this report. Delanoy et al. (56) reported neutropenia, anemia, thrombocytopenia, pancytopenia, bicytopenia, pure red cell aplasia with nivolumab, pembrolizumab, and atezolizumab. Twenty one patients had resolved symptoms with oral steroids, IV steroids, IVIG, and rituximab.
Ipilimumab
Fourteen articles reported Hem-irAEs with ipilimumab in 16 cases (15 melanomas and one with prostate cancer). The adverse events reported were neutropenia (5 cases), pancytopenia (3 cases), leukopenia (3 cases), thrombocytopenia (2 cases), anemia (2 cases), and 5 cases showed one of the following adverse events: agranulocytosis, lymphocytosis, hemophagocytic syndrome, acquired hemophilia A, and red cell aplasia. Eleven cases (68.75%) recovered after treatment. Steroids (8 cases) and IVIG (7 cases) were the most commonly used treatments.
Pembrolizumab
Twelve reports described Hem-irAEs with pembrolizumab in 13 cases (7 melanomas, 4 lung cancer, and 1 bladder cancer). In these cases, hemolytic anemia was reported in five cases and thrombocytopenia in two cases. Neutropenia, pancytopenia, red cell aplasia, hemophagocytic lymphohistiocytosis, and Evan's syndrome were reported in one case each. Adverse events were resolved in 11 cases. Steroids (whether IV or oral) were used in all the managed cases, and IVIG was used in five cases.
Combination of Ipilimumab—Nivolumab
This combination of ipilimumab and nivolumab, used to treat metastatic melanoma, was associated with Hem-irAEs in 6 cases (5 reports). Thrombocytopenia, aplastic anemia, and hemolytic anemia were reported in two cases each. The adverse events were resolved in 5 cases. One case died with refractory aplastic anemia. Rituximab was a commonly used treatment; one patient with thrombocytopenia recovered after 4 doses of rituximab following IVIG failure. The second occurrence of hemolytic anemia in one of the cases resolved with rituximab use.
Durvalumab
A fatal allo- and immune-mediated thrombocytopenia was reported with durvalumab use in one NSCLC case. Platelet transfusion, polyvalent immunoglobulins and steroid treatments were used to treat the patient without improvement.
Avelumab
One patient with metastatic Merkel cell carcinoma developed lethal immune thrombocytopenia (ITP) after avelumab administration. Treatments with steroids and IVIG were ineffective and the patient died after 1 month from initial diagnosis.
Concerning the treatment of Hem-irAEs reported, steroids were the most commonly used (80/118, 67.7%), with a failure rate of (16/80 = 20%) out of 118 cases. Other treatment options included IVIG, rituximab, and combination of the three options at varying doses.
Quality Assessment
Table 2 shows quality assessment of the extracted citations using Pierson-5. The number of case reports is based on five domains: uniqueness, documentation, objectivity, interpretation, and educational value. Every domain is scored with 2 points, the upper score is 10 points. Naranjo scale was used for causality assessment of the case reports, that allows categorical classification of adverse events as “definite,” “probable,” “possible,” or “doubtful” based on the answers to 10 questions.
Fifty-four case reports were retrieved from the literature and assessed. Out of the 54 reports, 5 (9.2%) could not be assessed, since the data presented were insufficient for assessment for 4 of them, while 1 study was an observational study. Seven cases (12.9%) were rated as “of insufficient quality for publication” because they scored 5 or less. The second case reported in Shiuan et al. (50) got zero score in the five domains. Twenty-six studies (48.1%) were assessed as “reader should be cautious about validity and clinical value of the report” because they scored 7–8. Twenty-one cases (38.8%) were rated as “likely to be a worthwhile contribution to the literature” as they scored 9–10.
Causality Assessment
Eight studies were ranked as “possible” adverse drug reaction, scoring 3 (one study) and 4 (7 studies). Two studies were not assessed because their data were insufficient. Sixteen studies were ranked as “probable” adverse drug reaction as they scored between 5 and 8. No cases were ranked as “definite” or “doubtful” adverse drug reaction.
For pembrolizumb case reports (13 reports), 8 of them (61.5%) were assessed as probable Hem-irAEs. Next to pembrolizumab, nivolumab (20 reports), 12 of which (60%) were assessed as probable, then comes ipilimumab (14 reports), 8 of which (57%) were assessed as probable. For the combination of ipilimumab and nivolumab (6 reports), 3 of them (50%) were assessed as probable. Finally, only one case report was assessed for durvalamab where the causality assessment yielded as a possible Hem-irAEs.
Discussion
Immunotherapeutics are increasingly used in cancer patients. However, adverse events can limit their use and may result in serious adverse outcomes, including death. While some adverse events have been well-described in clinical trials (e.g., dermatitis and colitis), other inflammatory and autoimmune manifestations are reported. Case reports can provide vital clues and signals to identify rare but serious events and can generate hypotheses that can direct ongoing scientific research. We conducted a systematic review of case reports/series of patients treated with checkpoint blockade to identify the scope of rare Hem-irAEs that may occur with these therapies. We included publications that had adequate description of the clinical manifestations of the patients reported.
This systematic review showed thrombocytopenia, hemolytic and aplastic anemias as the most commonly associated with ICPis use, i.e., nivolumab, ipilimumab, and pembrolizumab. Less reported adverse events included agranulocytosis and neutropenia. Steroids (either intravenous or oral) were commonly used to treat these adverse events with frequent success. Other strategies used IVIG, rituximab and transfusion of blood components.
The mechanisms of the recorded adverse events in the included articles remain elusive. The most plausible theory is activation of T-cells, leading to the secretion of different cytokines from T-helper cells and consequent tissue infiltration with cluster of differentiation 8 (CD8) T-cytotoxic cells (59). Another suggested mechanism was immune-mediated dysfunction in hematopoietic cell maturation and proliferation, yet, the exact intermediate mechanism is unknown (20). The response to steroids in the majority of these cases potentiates the theory of immune-mediated mechanisms that occur centrally (in the bone marrow) or peripherally (in the circulation).
We used the Naranjo scale to infer causality of the reported adverse event to the used ICPi drug. Although data were not available for some reports, we showed possible or probable causality in several included reports. In some of these reports, the ICPi was the only new treatment introduced and the events diminished after the drug withdrawal. Further, the temporal relationship between ICPis administration and the occurrence of the adverse effect implicates these drugs. Hem-irAEs are known to occur within 12 to 16 weeks of treatment initiation (60).
As reflected from the causality assessment results, the majority of cases reported were “probable”; being at the near top of the causality continuum of the Naranjo scale (just before definite). Consequently, the association between ICPis and Hem-irAEs cannot be ignored.
This review provides insights into the proper management strategies for Hem-irAEs. Previously, it was thought that cancer patients receiving immunotherapy should not receive immunosuppressive drugs. This view has significantly changed over the past few years and the use of immunosuppressive agents has been proven not to impair the efficacy of ICPis (61). Corticosteroids should be the first resource and some reports highlighted the benefit of high dose steroids therapy. In grade 3/4 adverse events, the ICPis should be discontinued and steroids can later be tapered off in 4 to 6 weeks with close monitoring of blood counts (7). Other immunosuppressive drugs as IVIG, rituximab or tumor necrosis factor antagonists may also be effective. In case the immunosuppressive therapy is prolonged, immunization against pneumocystis is recommended (4).
Definitions of the side effects in the registries of rare events are poor. Therefore, we focused on the qualitative features such as demographic characteristics of patients, diagnosis and management. We did not perform quantitative analysis of these case reports because risk analysis was not possible. Randomized clinical trials were not related to our objective and were excluded in this systematic review. Limiting the inclusion criteria to studies published in English was challenging. However, a former analysis showed that this language limitation does not usually alter the study results (62).
Future case reports/series should follow a standardized approach in reporting their patients characteristics and findings. Further attention should be given to Hem-irAEs in ICPis randomized controlled trials to provide higher quality data in this regard. Moreover, the mechanisms of these adverse events should be investigated on the molecular and cellular levels to specify more effective pharmacological interventions. The management of Hem-irAEs in patients receiving ICPis needs evidence-based guidelines to inform future practice and research in this area.
Concerning the factors that may have predisposed patients to the adverse effects, there was no clear pattern for age. Patients characteristics were heterogenous for age with high interpatient variability with median age of 54 years and wide range 32–85 years. For gender, most patients were males (n = 73, 61.8%); although the percentage is not conclusive, it warrants further investigations and more research.
There was no predictor for the response to treatment. However, steroids were the most commonly used option. This can be explained secondary to its relative availability, low cost, and physicians' experience compared to other options. Furthermore, steroid was not always successful (20% failure rate) which implies seeking other treatment options and keeping patients on steroids for Hem-irAEs closely monitored.
Conclusion
Although rare, Hem-irAEs are serious adverse events that may be associated with checkpoint blockade therapy. Depending on the grade of the adverse event, the ICPi therapy may be discontinued and steroid therapy should be initiated. Steroids were the most commonly management strategy with considerable failure rate. There were no detected underlying factors predicting the outcome to steroid therapy. Other promising management strategies for some events include IVIG, rituximab, and transfusion of blood components.
Future Research Recommendation
Further research should focus on the plausible mechanisms contributing to these adverse events, to develop more specific management strategies.
Data Availability Statement
Datasets are available on request from the authors.
Author Contributions
NO and NE extracted eligible articles. KE-F conducted initial screening of the eligible articles. Any conflict was solved by KE-F. The assessment was carried out by KE-F. A random sample was cross checked by NO and NE. AA, MY, AH, and SE contributed to the analysis. DJ, AA, AB, and AN contributed to writing of the manuscript and discussion. SD contributed to the discussion and reviewing the scientific background. All authors approved the article for submission.
Funding
This work was funded by the Medical Research Center, Hamad Medical Corporation, Qatar, as part of MRC-01-20-376 grant.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2020.01354/full#supplementary-material
Abbreviations
Hem-irAEs, Hematological Immune-Related Adverse Events; ICPis, Immune Checkpoint Inhibitors; ITP, Immune Thrombocytopenia; IVIG, Intravenous Immunoglobulins; ESMO, The European Society for Medical Oncology; CTLA4, Cytotoxic T-Lymphocyte-Associated Protein 4; PD-1, Programmed Cell Death Protein-1; SCLC, Small Cell Lung Carcinoma; NSCLC, Non-Small Cell Lung Cancer; ORRs, Objective Response Rates; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; CD8, Cluster of Differentiation 8; IVATG, Intravenous Anti-thymocyte Globulin; CSF, Colony Stimulating Factor; G-CSF, Granulocyte Colony Stimulating Factor; GM-CSF, Granulocyte-Macrophage Colony Stimulating Factor; RBC, Red Blood Cells; AEC, Absolute Eosinophil Count; AHA, Autoimmune Hemolytic Anemia; IFN-α, Interferon alpha; CTCAE, Common Terminology Criteria of Adverse Events.
References
1. Mellman I, Coukos G, Dranoff G. Cancer immunotherapy comes of age. Nature. (2011) 480:480–9. doi: 10.1038/nature10673
2. Pico de Coaña Y, Choudhury A, Kiessling R. Checkpoint blockade for cancer therapy : revitalizing a suppressed immune system. Trends Mol Med. (2015) 21:482–91. doi: 10.1016/j.molmed.2015.05.005
3. Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. (2010) 363:711–23. doi: 10.1056/NEJMx100063
4. Tabchi S, Weng X, Blais N. Severe agranulocytosis in a patient with metastatic non-small-cell lung cancer treated with nivolumab. Lung Cancer. (2016) 99:123–6. doi: 10.1016/j.lungcan.2016.06.026
5. Champiat S, Lambotte O, Barreau E, Belkhir R, Berdelou A, Carbonnel F, et al. Management of immune checkpoint blockade dysimmune toxicities: a collaborative position paper. Ann Oncol. (2016) 27:559–74. doi: 10.1093/annonc/mdv623
6. Spallarossa P, Meliota G, Brunelli C, Arboscello E, Ameri P, Dessalvi CC, et al. Potential cardiac risk of immune-checkpoint blockade as anticancer treatment: what we know, what we do not know, and what we can do to prevent adverse effects. Med Res Rev. (2018) 38:1447–68. doi: 10.1002/med.21478
7. Fay AP, Moreira RB, Nunes Filho PRS, Albuquerque C, Barrios CH. The management of immune-related adverse events associated with immune checkpoint blockade. Expert Rev Qual Life Cancer Care. (2016) 1:89–97. doi: 10.1080/23809000.2016.1142827
8. Michot JM, Vargaftig J, Leduc C, Quere G, Burroni B, Lazarovici J, et al. Immune-related bone marrow failure following anti-PD1 therapy. Eur J Cancer. (2017) 80:1–4. doi: 10.1016/j.ejca.2017.04.004
9. Haanen JBAG, Carbonnel F, Robert C, Kerr KM, Peters S, Larkin J, et al. Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. (2017) 28:iv119–42. doi: 10.1093/annonc/mdx225
10. Le Roy A, Kempf E, Ackermann F, Routier E, Robert C, Turpin A, et al. Two cases of immune thrombocytopenia associated with pembrolizumab. Eur J Cancer. (2016) 54:172–4. doi: 10.1016/j.ejca.2015.10.073
11. Pföhler C, Eichler H, Burgard B, Krecké N, Müller CSL, Vogt T. A case of immune thrombocytopenia as a rare side effect of an immunotherapy with PD1-blocking agents for metastatic melanoma. Transfus Med Hemother. (2017) 44:426–8. doi: 10.1159/000479237
12. Atwal D, Joshi KP, Ravilla R, Mahmoud F. Pembrolizumab-Induced pancytopenia: a case report. Perm J. (2017) 21:17–004. doi: 10.7812/TPP/17-004
13. Nair R, Gheith S, Nair SG. Immunotherapy-associated hemolytic anemia with pure red-cell aplasia. N Engl J Med. (2016) 374:1096–7. doi: 10.1056/NEJMc1509362
14. Barbacki A, Maliha PG, Hudson M, Small D. A case of severe pembrolizumab-induced neutropenia. Anticancer Drugs. (2018) 29:817–9. doi: 10.1097/CAD.0000000000000661
15. Shah D, Shrestha R, Ramlal R, Hatton J, Saeed H. Pembrolizumab associated hemophagocytic lymphohistiocytosis. Ann Oncol. (2017) 28:1403. doi: 10.1093/annonc/mdx113
16. Lott A, Butler M, Leighl N, Cserti-Gazdewich CM. Evan's syndrome associated with pembrolizumab therapy in metastatic non-small cell lung cancer. Blood. (2015) 126:4543. doi: 10.1182/blood.V126.23.4543.4543
17. Ogawa K, Ito J, Fujimoto D, Morita M, Yoshizumi Y, Ariyoshi K, et al. Exacerbation of autoimmune hemolytic anemia induced by the first dose of programmed death-1 inhibitor pembrolizumab: a case report. Invest New Drugs. (2018) 36:509–12. doi: 10.1007/s10637-018-0561-5
18. Robilliard B, Arnaud E, Gastaud L, Broner J. A case of pembrolizumab-induced autoimmune haemolytic anaemia with polymyalgia rheumatica. Eur J Cancer. (2018) 103:281–3. doi: 10.1016/j.ejca.2018.07.318
19. Sherbeck JP, Hugan S, Novak B, Ahmed A, Cooling L. IGT84: pembrolizumab induced autoimmune hemolytic anemia with possible. In: American Association of Blood Banks (AABB) Annual Meeting. (2018) 1–2.
20. Inadomi K, Kumagai H, Arita S, Tsuruta N, Takayoshi K, Mishima K, et al. Bi-cytopenia possibly induced by anti-PD-1 antibody for primary malignant melanoma of the esophagus: a case report. Medicine. (2016) 95:e4283. doi: 10.1097/MD.0000000000004283
21. Tokumo K, Masuda T, Miyama T, Miura S, Yamaguchi K, Sakamoto S, et al. Nivolumab-induced severe pancytopenia in a patient with lung adenocarcinoma. Lung Cancer. (2018) 119:21–4. doi: 10.1016/j.lungcan.2018.02.018
22. Bagley SJ, Kosteva JA, Evans TL, Langer CJ. Immune thrombocytopenia exacerbated by nivolumab in a patient with non-small-cell lung cancer. Cancer Treat Commun. (2016) 6:20–3. doi: 10.1016/j.ctrc.2016.02.009
23. Karakas Y, Yuce D, Kilickap S. Immune thrombocytopenia induced by nivolumab in a metastatic non-small cell lung cancer patient. Oncol Res Treat. (2017) 40:621–2. doi: 10.1159/000477968
24. Jotatsu T, Oda K, Yamaguchi Y, Noguchi S, Kawanami T, Kido T, et al. Immune-mediated thrombocytopenia and hypothyroidism in a lung cancer patient treated with nivolumab. Immunotherapy. (2018) 10:85–91. doi: 10.2217/imt-2017-0100
25. Kanameishi S, Otsuka A, Nonomura Y, Fujisawa A, Endo Y, Kabashima K. Idiopathic thrombocytopenic purpura induced by nivolumab in a metastatic melanoma patient with elevated PD-1 expression on B cells. Ann Oncol. (2016) 27:546–47. doi: 10.1093/annonc/mdv580
26. Turgeman I, Wollner M, Hassoun G, Bonstein L, Bar-Sela G. Severe complicated neutropenia in two patients with metastatic non-small-cell lung cancer treated with nivolumab. Anticancer Drugs. (2017) 28:811–4. doi: 10.1097/CAD.0000000000000520
27. Kong BY, Micklethwaite KP, Swaminathan S, Kefford RF, Carlino MS. Autoimmune hemolytic anemia induced by anti-PD-1 therapy in metastatic melanoma. Melanoma Res. (2016) 26:202–4. doi: 10.1097/CMR.0000000000000232
28. Schwab KS, Heine A, Weimann T, Kristiansen G, Brossart P. Development of hemolytic anemia in a nivolumab-treated patient with refractory metastatic squamous cell skin cancer and chronic lymphatic leukemia. Case Rep Oncol. (2016) 9:373–8. doi: 10.1159/000447508
29. Palla AR, Kennedy D, Mosharraf H, Doll D. Autoimmune hemolytic anemia as a complication of nivolumab therapy. Case Rep Oncol. (2016) 9:691–7. doi: 10.1159/000452296
30. Comito RR, Badu LA, Forcello N. Nivolumab-induced aplastic anemia: a case report and literature review. J Oncol Pharm Pract. (2019) 25:221–5. doi: 10.1177/1078155217726159
31. Yuki A, Takenouchi T, Takatsuka S, Ishiguro T. A case of pure red cell aplasia during nivolumab therapy for cardiac metastatic melanoma. Melanoma Res. (2017) 27:635–7. doi: 10.1097/CMR.0000000000000392
32. Deltombe C, Garandeau C, Renaudin K, Hourmant M. Severe allograft rejection and autoimmune hemolytic anemia after anti-PD1 therapy in a kidney transplanted patient. Transplantation. (2017) 101:e291. doi: 10.1097/TP.0000000000001861
33. Takeshita M, Anai S, Mishima S, Inoue K. Coincidence of immunotherapy-associated hemophagocytic syndrome and rapid tumor regression. Ann Oncol. (2016) 28:mdw537. doi: 10.1093/annonc/mdw537
34. Kato R, Hayashi H, Sano K, Handa K, Kumode T, Ueda H, et al. Nivolumab-induced hemophilia a presenting as gastric ulcer bleeding in a patient with NSCLC. J Thorac Oncol. (2018) 13:e239–41. doi: 10.1016/j.jtho.2018.06.024
35. du Rusquec P, Saint-Jean M, Brocard A, Peuvrel L, Khammari A, Quéreux G, et al. Ipilimumab-induced autoimmune pancytopenia in a case of metastatic melanoma. J Immunother. (2014) 37:348–50. doi: 10.1097/CJI.0000000000000041
36. Di Giacomo AM, Danielli R, Calabrò L, Bertocci E, Nannicini C, Giannarelli D, et al. Ipilimumab experience in heavily pretreated patients with melanoma in an expanded access program at the University Hospital of Siena (Italy). Cancer Immunol Immunother. (2011) 60:467–77. doi: 10.1007/s00262-010-0958-2
37. Zimmer L, Vaubel J, Mohr P, Hauschild A, Utikal J, Simon J, et al. Phase II DeCOG-study of ipilimumab in pretreated and treatment-naïve patients with metastatic uveal melanoma. PLoS ONE. (2015) 10:e0118564. doi: 10.1371/journal.pone.0118564
38. Ahmad S, Lewis M, Corrie P, Iddawela M. Ipilimumab-induced thrombocytopenia in a patient with metastatic melanoma. J Oncol Pharm Pract. (2012) 18:287–92. doi: 10.1177/1078155211411001
39. Kopecký J, Trojanová P, Kubecěk O, Kopecký O. Treatment possibilities of ipilimumab-induced thrombocytopenia–case study and literature review. Jpn J Clin Oncol. (2015) 45:381–4. doi: 10.1093/jjco/hyu222
40. Akhtari M, Waller EK, Jaye DL, Lawson DH, Ibrahim R, Papadopoulos NE, et al. Neutropenia in a patient treated with ipilimumab (anti–CTLA-4 Antibody). J Immunother. (2009) 32:322–4. doi: 10.1097/CJI.0b013e31819aa40b
41. Wozniak S, Mackiewicz-Wysocka M, Krokowicz Ł, Kwinta Ł, Mackiewicz J. Febrile neutropenia in a metastatic melanoma patient treated with ipilimumab - case report. Oncol Res Treat. (2015) 38:105–8. doi: 10.1159/000377650
42. Simeone E, Grimaldi AM, Esposito A, Curvietto M, Palla M, Paone M, et al. Serious haematological toxicity during and after ipilimumab treatment: a case series. J Med Case Rep. (2014) 8:240. doi: 10.1186/1752-1947-8-240
43. Ban-Hoefen M, Burack R, Sievert L, Sahasrabudhe D. Ipilimumab-induced neutropenia in melanoma. J Investig Med High Impact Case Rep. (2016) 4:232470961666183. doi: 10.1177/2324709616661835
44. Wei G, Nwakuche U, Cadavid G, Ajaz A, Seiter K, Liu D. Large granular lymphocytosis with severe neutropenia following ipilimumab therapy for metastatic melanoma. Exp Hematol Oncol. (2012) 1:3. doi: 10.1186/2162-3619-1-3
45. Delyon J, Mateus C, Lambert T. Hemophilia A induced by ipilimumab. N Engl J Med. (2012) 366:280–1. doi: 10.1056/NEJMc1113863
46. Gordon IO, Wade T, Chin K, Dickstein J, Gajewski TF. Immune-mediated red cell aplasia after anti-CTLA-4 immunotherapy for metastatic melanoma. Cancer Immunol Immunother. (2009) 58:1351–3. doi: 10.1007/s00262-008-0627-x
47. Michot JM, Pruvost R, Mateus C, Champiat S, Voisin AL, Marabelle A, et al. Fever reaction and haemophagocytic syndrome induced by immune checkpoint inhibitors. Ann Oncol. (2018) 29:518–20. doi: 10.1093/annonc/mdx701
48. Leroy L, Lafarge X, Blouin L, Bijou F, Durrieu F, Olivier E, et al. A fatal allo- and immune-mediated thrombocytopenia with a PD-L1 inhibitor. Ann Oncol. (2018) 29:514–5. doi: 10.1093/annonc/mdx693
49. Kratzsch D, Simon JC, Pönitzsch I, Ziemer M. Lethal thrombocytopenia in a patient treated with avelumab for metastatic Merkel cell carcinoma. J Dtsch Dermatol Ges. (2018) 17:73–5. doi: 10.1111/ddg.13722
50. Shiuan E, Beckermann KE, Ozgun A, Kelly C, McKean M, McQuade J, et al. Thrombocytopenia in patients with melanoma receiving immune checkpoint inhibitor therapy. J Immunother Cancer. (2017) 5:8. doi: 10.1186/s40425-017-0210-0
51. Helgadottir H, Kis L, Ljungman P, Larkin J, Kefford R, Ascierto PA, et al. Lethal aplastic anemia caused by dual immune checkpoint blockade in metastatic melanoma. Ann Oncol. (2017) 28:1672–3. doi: 10.1093/annonc/mdx177
52. Khan U, Ali F, Khurram MS, Zaka A, Hadid T. Immunotherapy-associated autoimmune hemolytic anemia. J Immunother Cancer. (2017) 5:15. doi: 10.1186/s40425-017-0214-9
53. Sun Y, Lee SK, Oo TH, Rojas-Hernandez CM. Management of immune-mediated cytopenias in the era of cancer immunotherapy. J Immunother. (2018) 41:32–4. doi: 10.1097/CJI.0000000000000194
54. Bernard-Tessier A, Jeanville P, Champiat S, Lazarovici J, Voisin AL, Mateus C, et al. Immune-related eosinophilia induced by anti-programmed death 1 or death-ligand 1 antibodies. Eur J Cancer. (2017) 81:135–7. doi: 10.1016/j.ejca.2017.05.017
55. Meyers DE, Hill WF, Suo A, Jimenez-Zepeda V, Cheng T, Nixon NA. Aplastic anemia secondary to nivolumab and ipilimumab in a patient with metastatic melanoma: a case report. Exp Hematol Oncol. (2018) 7:4–9. doi: 10.1186/s40164-018-0098-5
56. Delanoy N, Michot JM, Comont T, Kramkimel N, Lazarovici J, Dupont R, et al. Haematological immune-related adverse events induced by anti-PD-1 or anti-PD-L1 immunotherapy: a descriptive observational study. Lancet Haematol. (2019) 6:e48–57. doi: 10.1016/S2352-3026(18)30175-3
57. Pierson DJ. How to read a case report (or teaching case of the month). Respir Care. (2009) 54:1372–8.
58. Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. (1981) 30:239–45. doi: 10.1038/clpt.1981.154
59. Quirk SK, Shure AK, Agrawal DK. Immune-mediated adverse events of anticytotoxic T lymphocyte-associated antigen 4 antibody therapy in metastatic melanoma. Transl Res. (2015) 166:412–24. doi: 10.1016/j.trsl.2015.06.005
60. Weber JS, Dummer R, de Pril V, Lebb? C, Hodi FS. Patterns of onset and resolution of immune-related adverse events of special interest with ipilimumab: detailed safety analysis from a phase 3 trial in patients with advanced melanoma. Cancer. (2013) 119:1675–82. doi: 10.1002/cncr.27969
61. Horvat TZ, Adel NG, Dang TO, Momtaz P, Postow MA, Callahan MK, et al. Immune-related adverse events, need for systemic immunosuppression, and effects on survival and time to treatment failure in patients with melanoma treated with ipilimumab at memorial sloan kettering cancer center. J Clin Oncol. (2015) 33:3193–8. doi: 10.1200/JCO.2015.60.8448
Keywords: immune checkpoint inhibitors, immune-related adverse events, ipilimumab, pembrolizumab, nivolumab, atezolizumab, durvalumab, avelumab
Citation: Omar NE, El-Fass KA, Abushouk AI, Elbaghdady N, Barakat AEM, Noreldin AE, Johar D, Yassin M, Hamad A, Elazzazy S and Dermime S (2020) Diagnosis and Management of Hematological Adverse Events Induced by Immune Checkpoint Inhibitors: A Systematic Review. Front. Immunol. 11:1354. doi: 10.3389/fimmu.2020.01354
Received: 01 February 2020; Accepted: 27 May 2020;
Published: 21 October 2020.
Edited by:
Zhihai Qin, Institute of Biophysics (CAS), ChinaReviewed by:
Ryota Tanaka, University of Tsukuba, JapanWei Chen, Stanford University, United States
Copyright © 2020 Omar, El-Fass, Abushouk, Elbaghdady, Barakat, Noreldin, Johar, Yassin, Hamad, Elazzazy and Dermime. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dina Johar, dW1qb2hhckBteXVtYW5pdG9iYS5jYQ==; ZGluYWpvaGFyQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
 Nabil E. Omar
Nabil E. Omar Kareem A. El-Fass
Kareem A. El-Fass Abdelrahman I. Abushouk
Abdelrahman I. Abushouk Noha Elbaghdady
Noha Elbaghdady Abd Elmonem M. Barakat
Abd Elmonem M. Barakat Ahmed E. Noreldin
Ahmed E. Noreldin Dina Johar
Dina Johar Mohamed Yassin
Mohamed Yassin Anas Hamad
Anas Hamad Shereen Elazzazy
Shereen Elazzazy Said Dermime
Said Dermime