
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Immunol., 25 March 2020
Sec. Alloimmunity and Transplantation
Volume 11 - 2020 | https://doi.org/10.3389/fimmu.2020.00423
This article is part of the Research TopicTransplantation of Marginal Organs: Immunological Aspects and Therapeutic PerspectivesView all 17 articles
 Petra Hruba1
Petra Hruba1 Zdenek Krejcik2
Zdenek Krejcik2 Michaela Dostalova Merkerova2
Michaela Dostalova Merkerova2 Jiri Klema3
Jiri Klema3 Viktor Stranecky4
Viktor Stranecky4 Janka Slatinska5
Janka Slatinska5 Jana Maluskova6
Jana Maluskova6 Eva Honsova6
Eva Honsova6 Ondrej Viklicky1,5*
Ondrej Viklicky1,5*The fate of transplanted kidneys is substantially influenced by graft quality, with transplantation of kidneys from elderly and expanded criteria donors (ECDs) associated with higher occurrence of delayed graft function, rejection, and inferior long-term outcomes. However, little is known about early molecular fingerprints of these events in different donor categories. Borderline changes represent the most frequent histological finding early after kidney transplantation. Therefore, we examined outcomes and transcriptomic profiles of early-case biopsies diagnosed as borderline changes in different donor categories. In this single-center, retrospective, observational study, we compared midterm outcomes of kidney transplant recipients with early borderline changes as a first pathology between ECD (n = 109), standard criteria donor (SCDs, n = 109), and living donor (LD, n = 51) cohorts. Intragraft gene expression profiling by microarray was performed in part of these ECD, SCD, and LD cohorts. Although 5 year graft survival in patients with borderline changes in early-case biopsies was not influenced by donor category (log-rank P = 0.293), impaired kidney graft function (estimated glomerular filtration rate by Chronic Kidney Disease Epidemiology Collaboration equation) at M3, 1, 2, and 3 years was observed in the ECD cohort (P < 0.001). Graft biopsies from ECD donors had higher vascular intimal fibrosis and arteriolar hyalinosis compared to SCD and LD (P < 0.001), suggesting chronic vascular changes. Increased transcripts typical for ECD, as compared to both LD and SCD, showed enrichment of the inflammatory, defense, and wounding responses and the ECM–receptor interaction pathway. Additionally, increased transcripts in ECD vs. LD showed activation of complement and coagulation and cytokine–cytokine receptor pathways along with platelet activation and cell cycle regulation. Comparative gene expression overlaps of ECD, SCD, and LD using Venn diagrams found 64 up- and 16 down-regulated genes in ECD compared to both LD and SCD. Shared increased transcripts in ECD vs. both SCD and LD included thrombospondin-2 (THBS2), angiopoietin-like 4 (ANGPTL4), collagens (COL6A3, COL1A1), chemokine CCL13, and interleukin IL11, and most significantly, down-regulated transcripts included proline-rich 35 (PRR35) and fibroblast growth factor 9. Early borderline changes in ECD kidney transplantation are characterized by increased regulation of inflammation, extracellular matrix remodeling, and acute kidney injury transcripts in comparison with both LD and SCD grafts.
The association of aging with chronic and functional kidney changes has long been acknowledged (1). Kidney recipients from expanded criteria donors (ECDs) are supposed to have inferior midterm renal function and graft survival outcomes (2, 3). In addition to decreasing numbers of functional nephrons, deteriorating alloimmune mechanisms contribute to worse graft outcomes in marginal donors.
Increased transcriptional activation of acute-phase proteins, complement components, and chemokines has been observed during implantation biopsy of grafts from deceased donors vs. living donors (LDs) (4). These underlying molecular mechanisms thus reflect donor organ quality. After transplantation, ischemia/reperfusion injury leads to the up-regulation of inflammation- and apoptosis-related genes due to increased intragraft infiltration of immunocompetent cells (5). This may further aggravate existing injury in ECD grafts.
In recent years, there has been an increase in the use of ECD kidneys [reaching 42–65% (6)] toward meeting demand from patients with end-stage renal disease potentially benefitting from transplantation. Based on midterm follow-up data, marginal donors are associated with inferior renal graft function, higher incidence of delayed graft function (DGF), and infectious complications, despite incidence of acute rejections and long-term graft function being similar to standard criteria donors (SCDs) (2, 7).
In indication biopsies performed early after transplantation, a wide spectrum of diverse diagnoses can be observed, ranging from acute tubular necrosis to T cell– or antibody-mediated rejection. Some of the most frequent findings in early indication biopsies are borderline changes, despite their clinical significance being the subject of debate. Previously, we showed that early borderline changes (BL) biopsies are associated with increased expression patterns of immunity- and inflammation-related genes. Higher donor age as well as some inflammation-related genes additionally contributed to late graft dysfunction (8). Although the transcriptome of kidney graft biopsies in the early period reflects the early alloimmune response, it can also be influenced by ischemia/reperfusion injury and transferred chronic histological changes. While previous study (8) focused on outcomes of BL, in this study on another patient cohort and using different platform, we focus on molecular assessment of various donor categories. The aims of this single-center study were to evaluate renal transcripts associated with donor category in a cohort exhibiting early borderline changes and to identify organ quality-specific patterns, thus limiting any potential bias associated with different histological categories.
To study the effect of donor category (deceased vs. living, ECDs vs. SCDs), we carried out a retrospective, single-center, observational, cohort analysis of patients with borderline changes early after transplantation. Of 6,197 kidney recipients transplanted at our center between January 2005 and January 2017, all borderline changes were retrospectively identified (12.6%). Only patients with BL from case biopsies performed early after transplantation [median 9 days (min 4, max 60)] were enrolled in our study cohort (n = 338) (Figure 1). To obtain a cohort of borderline changes as a first pathology, all cases with prior episodes of rejection or thrombotic microangiopathy were excluded. To determine pure BL pathology, cases with concurrent presence of antibody-mediated rejection (ABMR), thrombotic microangiopathy (TMA), recurrent glomerulonephritis, glomerulitis >1, and BK virus (BKV) nephropathy were excluded. Furthermore, patients with primary graft dysfunction were deemed ineligible to participate in the study. A final cohort of 269 patients with early BL biopsies as a first and sole pathology was formed, with midterm outcomes compared between ECD (n = 109), SCD (n = 109), and LD (n = 51) categories. Expanded criteria donor kidneys were obtained from deceased donors either aged ≥ 60 years or 50–59 years meeting at least two of the following conditions: serum creatinine >1.5 mg/dL (132.5 μmol/L), cerebrovascular accident as a cause of death, or history of hypertension (9). Standard criteria donors are all deceased donors who failed to meet the criteria for ECD (10). Living donor kidney transplantation was performed between ABO-compatible genetically related or unrelated relatives or friends or with non-directed donors when kidney paired donation was performed. All kidney transplant recipients were treated according to standard center protocol, receiving no induction, T cell–non-depletive (basiliximab, daclizumab) induction, or T cell–depletive induction (rATG or infliximab) followed by a standard triple immunosuppression regimen based on a combination of tacrolimus/cyclosporine, mycophenolate mofetil (MMF)/mycophenolic acid (MPA), and steroids.
For the purpose of the transcriptomic study, we analyzed only patients receiving no induction or non-depletive induction therapy to eliminate the effect of different posttransplant immunosuppression on expression profiles. Furthermore, only biopsies performed within the first 14 days after transplantation were analyzed to reduce time-dependent changes in transcriptional profiles. Thus, the final cohort for molecular analysis consisted of 21 patients across 3 donor categories: ECD, SCD, and LD. Demographics of the microarray cohort are given in Table 1.
The study was approved by ethics committee of the Institute for Clinical and Experimental Medicine and Thomayer Hospital With Multi-center Competence under number G-16-06-09.
Total RNA was isolated from renal biopsies using the RNeasy Micro Kit (Qiagen, Hilden, Germany). RNA quality and integrity were determined using the Agilent RNA 6000 Nano Kit on the Agilent 2100 Bioanalyzer (Agilent Technologies, Santa Clara, CA, USA). Samples with an RNA integrity number of <6 were excluded from the analysis. RNA concentration was determined using a Qubit® fluorometer with Qubit® RNA BR Assay (ThermoFisher Scientific, Waltham, MA, USA).
A total of 150 ng RNA served as a template for the amplification and generation of Cy3 fluorescent cRNA using the Low Input Quick Amp Labeling Kit, one-color (Agilent Technologies), according to the manufacturer's instructions. Labeling efficiency, yield, and purity of cRNA were determined using a NanoDrop spectrophotometer. Labeled cRNA (700 ng with specific activity >10.0 pmol Cy3/μg cRNA) was hybridized to Agilent SurePrintG3 Human Gene Expression v3 8×60K Array at 65°C for 17 h in a rotating hybridization oven at a speed of 10 rounds per minute. After hybridization, microarrays were washed sequentially for 1 min in wash buffer 1, for 1 min with prewarmed (37°C) wash buffer 2 (Agilent Technologies) and then immediately dried and scanned. Scanning was performed on the Agilent C Microarray Scanner, with data extraction and quality control performed using Agilent Feature Extraction Software (version 10.7.3.1). The resulting text files were analyzed using R software. The R software Lumi package was used to process raw data obtained from microarray analysis, with the quantile method used for normalization. Raw data sets used in the study were deposited at the Gene Expression Omnibus database (11) under ID GSE134386. When comparing particular donor subgroups, only two genes, PRR35 and CD163L1, differentially expressed between ECD and LD, remained significant after multiple corrections [(false discovery rate (FDR) P < 0.05, fold change >2]. Therefore, in further analysis, differentially expressed genes were chosen as those with a fold change >2 and an unadjusted P < 0.05. Affected genes were functionally annotated, with deregulated pathways identified using the David database (http://david.abcc.ncifcrf.gov). In order to compare lists of deregulated genes, we availed of an interactive online tool for Venn diagrams (http://bioinfogp.cnb.csic.es/tools/venny/index.html).
Data normality was tested using the Kolmogorov–Smirnov test. As most variables exhibited non-normal distribution, we compared two groups using the two-tailed Mann-Whitney U-test and three groups using the Kruskal–Wallis test, followed by the post hoc Dunn multiple-comparisons test. Categorical data were compared using the χ2 or Fisher exact test. Differences in kidney graft function between SCD, ECD, and LD were calculated using the General Linear Model (GLM) repeated-measures model. Graft survival was compared using Kaplan–Meier estimates and the log-rank test. Two-sided P ≤ 0.05 was considered statistically significant.
We compared midterm outcomes of kidney transplant recipients with borderline changes as a first pathology diagnosed at a median of 9 days after transplantation between ECD (n = 109), SCD (n = 109), and LD (n = 51) kidney transplantation cohorts. The ECD group had not only older donors but also higher recipients age (P = 0.029) and longer cold ischemia times than did the SCD group (P = 0.020). The LD group had the lowest recipient ages, cold ischemia times, and panel-reactive antibody levels and also the shortest dialysis spans (P < 0.001). The LD group contained a significantly higher proportion of female donors (P < 0.001) (Supplemental Table 1). The highest incidence of DGF was in the ECD group (37%) followed by SCD (32%), with prevalence of DGF only 6% in the LD group (P < 0.001).
The effect of donor category on individual Banff indication biopsy scores with borderline change findings showed the greatest chronic changes in the ECD group (Table 2). Graft biopsies from ECD donors revealed significantly higher vascular intimal fibrosis (cv) and arteriolar hyalinosis (ah) compared to both SCD and LD (P < 0.001), pointing to chronic vascular changes as well as higher tubular atrophy scores (ct) in grafts from marginal donors. On the contrary, biopsies from the LD group had significantly lower arteriolar hyaline thickening (aah) scores than those from the ECD group (P < 0.001) and SCD group (P < 0.05).
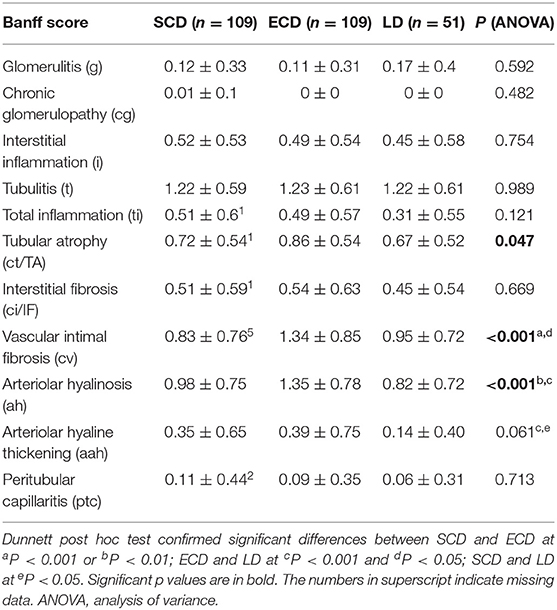
Table 2. Histological findings in indication biopsies with BL performed early after transplantation stratified according to donor type.
Patients from the ECD group had significantly worse renal graft function at biopsy, at 3 months, and in the first, second, and third years after biopsy [medians of estimated glomerular filtration rate (eGFR): 0.29, 0.59, 0.64, 0.67, 0.65 mL/s] compared to patients in the SCD (medians of eGFR 0.39, 0.79, 0.83, 0.84, 0.85 mL/s) and LD groups (medians of eGFR: 0.55, 0.79, 0.87, 0.85, 0.94 mL/s) (P < 0.001). The renal function of patients who received grafts from LD was better at biopsy compared to the SCD group (P < 0.001), despite no differences being found thereafter (Supplemental Figure 1).
Neither 5 year graft survival nor rejection-free intervals significantly differed among recipients with early borderline changes based on donor category (log-rank P = 0.293 and 0.219, respectively) (Supplemental Figure 2).
The effect of donor category on the intragraft transcriptional profile was studied in sections of the ECD (n = 9), SCD (n = 4), and LD (n = 8) cohorts. All biopsies were clinically indicated at a median of 9 days after transplantation (min 5, max 13 days) and diagnosed as borderline changes. There was no difference in the follow-up to biopsy among the ECD, SCD, and LD cohorts (P = 0.432). All patients had received their first transplants, had low levels of panel-reactive antibodies, and therefore received no induction or basiliximab. The demographics of this microarray set of patients are given in Table 1. Differences between groups, such as older donors (P = 0.044) in the ECD group or shorter cold ischemia times (P = 0.001) in the LD group, reflect particular donor category definitions. In addition, patients from the ECD group had the worst renal function at biopsy (median of creatinine was 397 μmol/L for the ECD group, 177 μmol/L for the SCD group, and 185 μmol/L for the LD group, P = 0.016).
Similar to our analysis of the larger clinical cohort (Table 2) also in microarray-analyzed biopsies, patients from the ECD group had significantly higher vascular intimal fibrosis (cv) (P = 0.028, Supplemental Table 2).
In the ECD group, microarray revealed higher expression of 244 transcripts compared to SCD and 437 compared to LD. Compared to both SCD and LD, gene annotation analysis of transcripts with increased expression in ECD grafts showed enrichment of the inflammatory response (P = 0.013, P = 7.4 × 10−8, respectively), the response to wounding (P = 0.001, 1.3 × 10−12, respectively), the defense response (P = 0.005, P = 5.5 × 10−7, respectively), and the ECM–receptor interaction pathway (P = 0.043, P = 0.004, respectively) (Table 3). Additionally, annotation analysis of increased transcripts in ECD vs. LD showed activation of complement and coagulation cascades (P = 0.0039), cytokine–cytokine receptor interaction pathways (P = 0.02), and other Gene Ontology (GO) terms such as regulation of the cell cycle process (P = 1.9 × 10−6) and platelet activation (P = 0.0001) (Table 3). Interestingly, GO term response to wounding was more activated in ECD kidneys in comparison with SCD (P = 0.001) and LD kidneys (1.3 × 10−12), and similarly, it was higher in SCD kidneys compared with LD ones (P = 0.005). Activation of the KEGG complement and coagulation cascades pathway was observed in both deceased donor categories (ECD and SCD) in comparison with LD (P = 0.039 and P = 0.019, respectively). Moreover, higher regulation of lipid transport was observed in SCD vs. LD (Table 3).
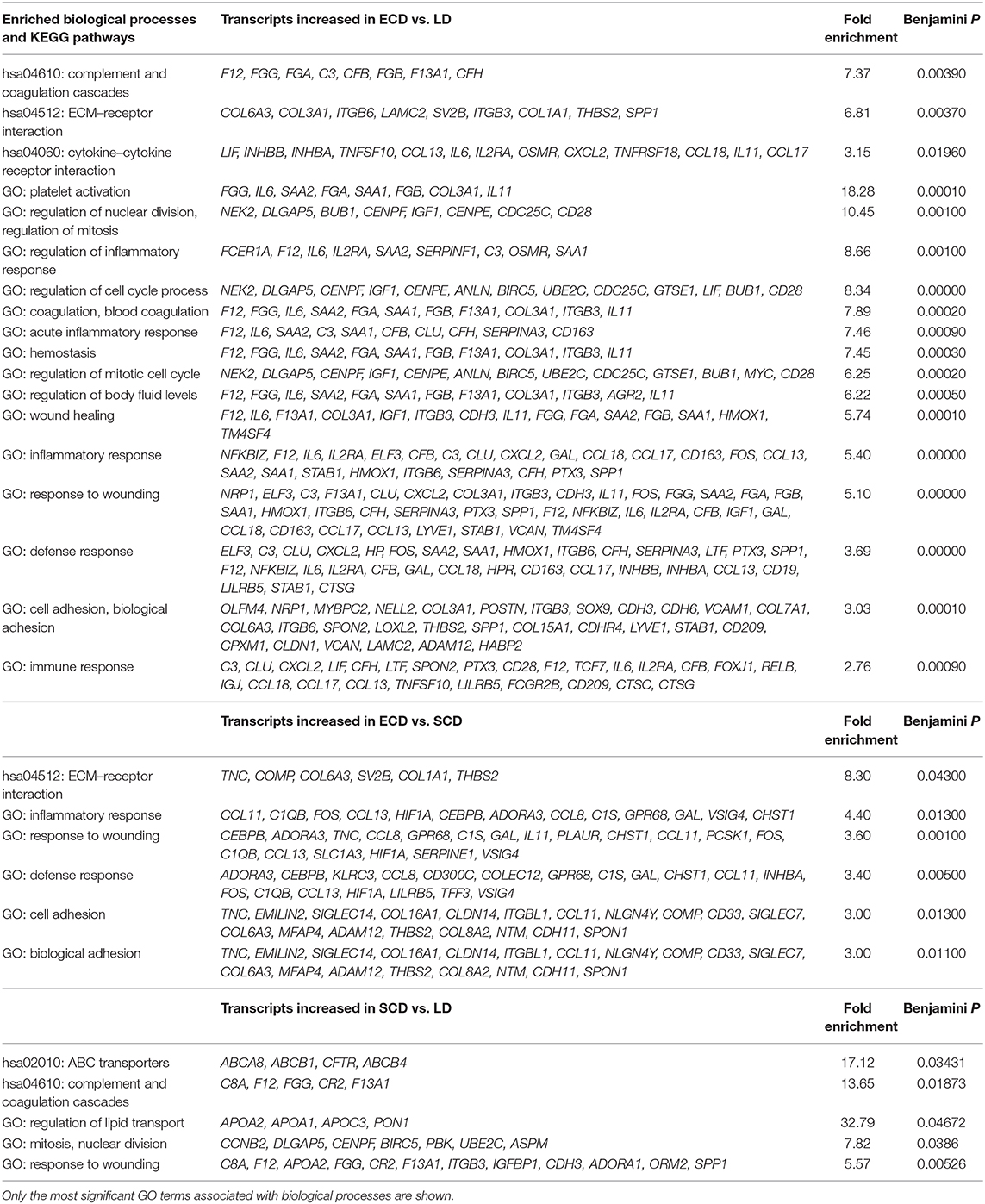
Table 3. Biological processes and KEGG pathway–enriched case biopsies with borderline changes in ECD compared to SCD, in ECD compared to LD, and in SCD compared to LD.
Comparative gene expression overlaps of differentially expressed genes between ECD vs. SCD and ECD vs. LD using Venn diagrams (Figure 2) found 64 up- and 16 down-regulated genes in ECD compared to both LD and SCD. Shared increased transcripts in ECD vs. both SCD and LD included thrombospondin 2 (THBS2), synaptic vesicle glycoprotein (SV2B), angiopoietin-like 4 (ANGPTL4), collagens (COL6A3, COL1A1), chemokines CCL13, and interleukin IL11 and, most significantly, down-regulated transcripts including proline-rich 35 (PRR35) and fibroblast growth factor 9 (FGF9).
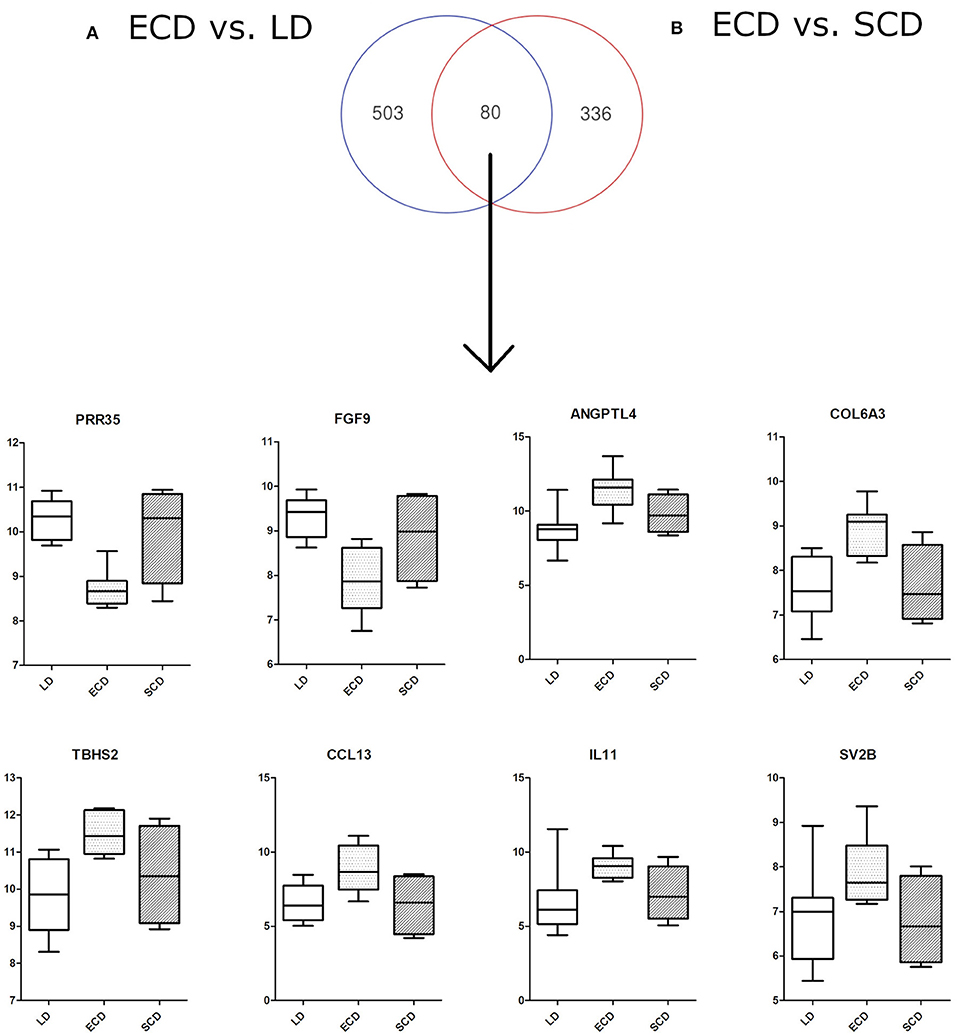
Figure 2. Venn diagram showing overlap of deregulated genes (80 transcripts) for particular comparisons of donor categories: (A) ECD vs. LD (583 deregulated transcripts), (B) ECD vs. SCD (416 deregulated transcripts). The overlap of some genes shows differential expression of ECD compared with SCD and LD. PRR35, proline-rich 35 protein; FGF9, fibroblast growth factor 9; ANGPTL4, angiopoietin-like 4; COL6A3, collagen, type VI, alpha 3; TBHS2, thrombospondin 2; CCL13, chemokine (C-C motif) ligand 13; IL11, interleukin 11; SV2B, synaptic vesicle glycoprotein 2B.
From 30 injury-repaired associated transcripts related to acute kidney injury (AKI) described by Famulski et al. (12), 28 were measured on the chip in our study, and 19 (64%) of those transcripts were significantly up-regulated in ECD compared to LD donors (Figure 3). Five of those transcripts, LCN2, lipocalin 2; LTF, lactotransferrin; VCAN, versican; ITGB6, integrin beta 6; and SERPINA3, serpin peptidase inhibitor, were among top ranked significant transcripts that differentiated ECD from LD. Of note, three of 19 AKI transcripts (LTF, LCN2, and SERPINA3) were more than 10 times more regulated in ECD as compared to LDs (fold change >10).
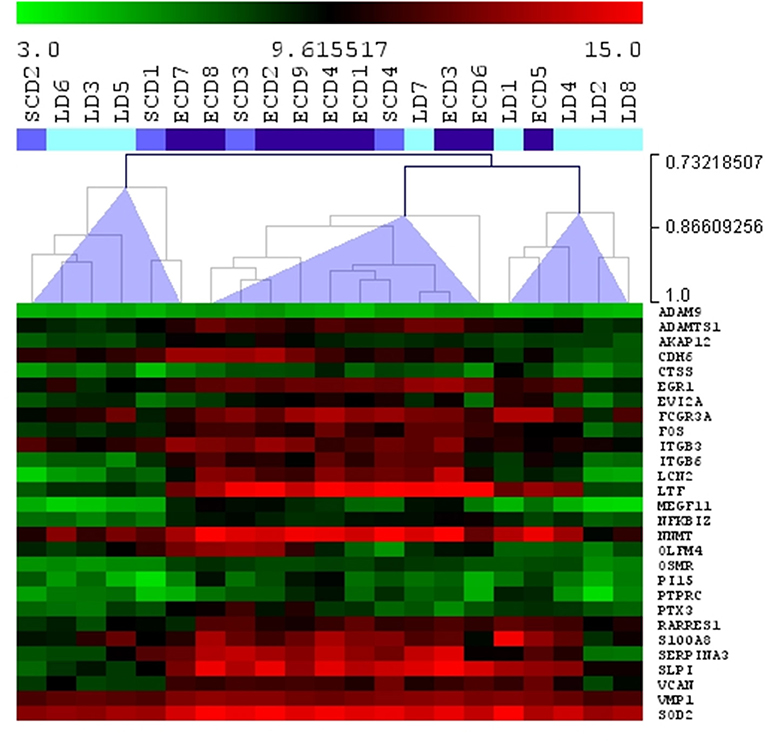
Figure 3. Hierarchical clustering (Spearman rank correlation) for 28 injury-repaired associated transcripts related to acute kidney injury measured in early indication biopsies with borderline changes in different donor categories using Agilent microarray. Light blue: LD, living donor; intermediate blue: SCD, standard criteria donor; dark blue: ECD, expanded criteria donor. Most acute kidney injury transcripts were increased in the second cluster, formed in 70% by grafts from ECD donors.
Donor kidney quality significantly affects kidney transplantation outcomes. It is widely accepted that transplantation of kidneys from elderly marginal donors results in inferior renal function and limited graft life. Expanded criteria donor kidney graft recipients typically suffer from more frequent DGF and acute rejection. In this study, however, the DGF rate was similar between ECD and SCD cohort but much higher than in the LD group (37, 32, and 6%, respectively). Similarly, higher DGF rate was found in respective groups when analyzing a larger cohort of 254 late biopsies (22% in SCD, 18% in ECD, and 4.5% in LD), which may reflect different therapy used in the ECD group. A recent multicenter study reported DGF frequency to be 2.24× higher in ECD compared to SCD recipients (P = 0.02) (13). The reason seems to be associated with aggravated alloimmune response and fibrogenesis in already-injured organs. Apart from conventional histological assessment, little is known about molecular pathways typical of marginal kidney grafts. Increasing knowledge in this area may lead to improvements in predicting premature graft loss and adapting therapy appropriately.
To the best of our knowledge, our study is the first to compare intragraft transcriptional profiles from different donor categories in the early posttransplant period, in fact within first 14 posttransplant days. Previous studies have compared preimplant donor biopsies (14) and 0 h (4, 15–17) or postreperfusion (18) graft biopsies from different donor categories. Because all of the indication biopsies we analyzed were diagnosed as borderline changes with no previous pathology, modifications in the transcriptome among donor categories could not have been influenced by different underlying pathological processes. Using microarray, we found higher expression of inflammation- and extracellular matrix remodeling–associated transcripts in the kidney allografts of ECD donors compared with other donor categories.
Compared to the ideal LD group, we observed increased transcripts associated with inflammatory, wounding, and defense responses; complement and coagulation cascades; and cytokine–cytokine receptor interaction pathways in the ECD cohort. This observation seems to be in line with a study by Mueller describing up-regulation of acute phase proteins, complement components, and chemokines in postreperfusion implant biopsies obtained from deceased (compared to living) donors (4). Collectively, this suggests that early transcriptional activations persist at least up to 14 days posttransplant, during which time the biopsies in our study were performed.
In our study, ECD-derived biopsies exhibited increases in several transcripts associated with extracellular matrix remodeling such as thrombospondin 2 (THBS2), collagens (COL6A3, COL1A1), synaptic vesicle glycoprotein (SV2B), and interleukin 11 (IL11). Increased expression of THBS2, which plays a role in extracellular matrix remodeling, was previously detected in kidney allografts suffering from acute rejection (19). The dominant profibrotic role of IL11 in the heart and kidneys was recently described (20). An experimental study found increased expression of ANGPTL4 to be an early biomarker of podocyte injury in a minimal change disease rat model (21). It's up-regulation preceded heavy proteinuria and increased urinary ANGPTL4 protein levels.
Next, in our study, proline-rich 35 (PRR35) and FGF9 were significantly down-regulated in biopsies from ECD donors compared to other cohorts. In another study, expression of FGF9 in biopsies with AKI was lower than in biopsies with primary graft function (22).
Interestingly, PRR35 and CD163L were the most significantly deregulated genes in ECD and LD cohorts, with PRR35 gene transcripts nearly three times lower in biopsies from ECD donors compared to LD. PRR35 is a protein-coding gene of unknown function. CD163L, a macrophage scavenger receptor associated with the anti-inflammatory response and tissue remodeling, has been shown to exhibit three times higher expression in ECD donors (23).
Most importantly, we found significant expression of AKI-related transcripts in ECD kidney grafts. This information is in line with previous “0 h” biopsies study (17). Thus, higher AKI transcripts reflect parenchymal injury associated with donor age and ischemia time and sustain at least 14 days after transplantation, the most critical time period for generation of initial alloimmune response.
In our study, patients with ECD grafts experienced worse renal function at 3 years (median eGFR, 0.65 mL/s) compared to SCD (median eGFR, 0.85 mL/s) and LD grafts (median, 0.94 mL/s). This suggests a higher risk of premature graft loss, although in our study we found no differences in 5 year graft survival between donor categories, which is perhaps unsurprising given the inconclusive results of other studies (2, 7, 24–26). Although the effect of marginal kidneys on graft outcomes has been previously described, it has not been evaluated in a well-defined cohort of patients with the same first pathology of “mild rejection” during the early posttransplant period.
In our early biopsies of ECD patients with borderline changes, the transmission of chronic histological changes was more common, represented by vascular intimal fibrosis (cv), arteriolar hyalinosis (ah), and tubular atrophy (ct) Banff scores compared to biopsies of both SCD and LD categories. The association of higher chronic histopathological Banff scores in biopsies from marginal donors with graft dysfunction or DGF has been reported by other studies (6, 27, 28). In our study, we did not find significantly higher interstitial fibrosis (ci) scores or higher expression of fibroblast-associated transcripts in early BL biopsies of ECD individuals compared to other donor categories. This corresponds to the results of a recent study where indication biopsies performed early after transplantation had higher expression of AKI-associated transcripts than fibroblast-associated transcripts (29).
The sample size for our analysis of graft function and survival (n = 269) among particular categories was satisfactorily large. Nevertheless, microarray transcriptome analysis was performed only in a small subgroup (n = 21) of patients, representing a possible limitation of our study. However, the main conclusion drawn from our transcriptome analysis is higher activation of immunity, inflammation, and extracellular matrix remodeling in biopsies from marginal donors seen even within 14 days post-transplant. Additionally, because of low number of differentially expressed genes after correction for multiple testing, the unadjusted p cutoff < 0.05 and fold change >2 were used instead in statistical analysis. Nevertheless, the high overlap of increased transcripts in marginal donors with the already described molecular AKI injury (12)–related transcript set supports our results of gene annotation analysis. The aim of our study was not to search for any biomarkers requiring larger sample size and validation, but to examine the main transcriptional pathways activated in marginal donors in the early posttransplant period.
In our study, the early borderline changes in ECD kidneys were characterized by the most increased regulation of inflammation, extracellular matrix remodeling, and AKI transcripts in comparison with SCD and LD grafts, respectively. It is likely that ECD-related transcripts were boosted by already present vascular changes in comparison with SCD kidneys and similarly in SCD kidneys by longer ischemia in comparison with LD kidneys. Therefore, chronic vascular changes and cold ischemia time aggravate inflammation and thus contribute to worse outcomes of these grafts. Our data are therefore in line with current praxis where ECD kidney recipients often receive T cell–depletive induction therapy.
The datasets generated for this study can be found in the Gene Expression Omnibus database under ID GSE134386.
The study was approved by Ethics Committee of the Institute for Clinical and Experimental Medicine and Thomayer Hospital with Multi-Centre Competence under number G-16-06-09. The patients/participants provided their written informed consent to participate in this study.
PH and OV designed and wrote the manuscript. PH, ZK, MD, JS, JM, and EH performed the research. VS, JK, and PH participated in the data analysis. OV supervised the research.
This study was supported by the Ministry of Health of the Czech Republic under grant 17-28778A.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2020.00423/full#supplementary-material
AKI, Acute kidney injury; CI, Confidence interval; DGF, Delayed graft function; ECD, Expanded criteria donor; eGFR, Estimated glomerular filtration rate; HLA, Human leukocyte antigen; LD, Living donor; rATG, Rabbit polyclonal antithymocyte globulin; PRA, Panel-reactive antibody; SCD, Standard criteria donor; HR, Hazard ratio.
1. DAVIES DF, SHOCK NW. Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J Clin Invest. (1950) 29:496–507. doi: 10.1172/JCI102286
2. Hwang JK, Park SC, Kwon KH, Choi BS, Kim JI, Yang CW, et al. Long-term outcomes of kidney transplantation from expanded criteria deceased donors at a single center: comparison with standard criteria deceased donors. Transplant Proc. (2014) 46:431–6. doi: 10.1016/j.transproceed.2013.11.061
3. Ferreira E, Costa J, Romãozinho C, Santos L, Macário F, Bastos C, et al. Long-term outcomes of kidney transplantation from expanded-criteria deceased donors: a single-center experience. Transplant Proc. (2017) 49:770–6. doi: 10.1016/j.transproceed.2017.01.051
4. Mueller TF, Reeve J, Jhangri GS, Mengel M, Jacaj Z, Cairo L, et al. The transcriptome of the implant biopsy identifies donor kidneys at increased risk of delayed graft function. Am J Transplant. (2008) 8:78–85. doi: 10.1111/j.1600-6143.2007.02032.x
5. Wohlfahrtova M, Brabcova I, Zelezny F, Balaz P, Janousek L, Honsova E, et al. Tubular atrophy and low netrin-1 gene expression are associated with delayed kidney allograft function. Transplantation. (2014) 97:176–83. doi: 10.1097/TP.0b013e3182a95d04
6. Balaz P, Rokosny S, Wohlfahrtova M, Wohlfahrt P, Bartonova A, Pokorna E, et al. Identification of expanded-criteria donor kidney grafts at lower risk of delayed graft function. Transplantation. (2013) 96:633–8. doi: 10.1097/TP.0b013e31829d9225
7. Ko KJ, Kim YH, Kwon KH, Kim MH, Jun KW, Hwang JK, et al. Kidney transplantation using expanded-criteria deceased donors: a comparison with ideal deceased donors and non-expanded-criteria deceased donors. Transplant Proc. (2018) 50:3222–7. doi: 10.1016/j.transproceed.2018.05.028
8. Hrubá P, Brabcová I, Gueler F, Krejčík Z, Stránecký V, Svobodová E, et al. Molecular diagnostics identifies risks for graft dysfunction despite borderline histologic changes. Kidney Int. (2015) 88:785–95. doi: 10.1038/ki.2015.211
9. Port FK, Bragg-Gresham JL, Metzger RA, Dykstra DM, Gillespie BW, Young EW, et al. Donor characteristics associated with reduced graft survival: an approach to expanding the pool of kidney donors. Transplantation. (2002) 74:1281–6. doi: 10.1097/00007890-200211150-00014
10. Rao PS, Ojo A. The alphabet soup of kidney transplantation: SCD, DCD, ECD–fundamentals for the practicing nephrologist. Clin J Am Soc Nephrol. (2009) 4:1827–31. doi: 10.2215/CJN.02270409
11. Edgar R, Domrachev M, Lash AE. Gene expression omnibus: NCBI gene expression and hybridization array data repository. Nucleic Acids Res. (2002) 30:207–10. doi: 10.1093/nar/30.1.207
12. Famulski KS, de Freitas DG, Kreepala C, Chang J, Sellares J, Sis B, et al. Molecular phenotypes of acute kidney injury in kidney transplants. J Am Soc Nephrol. (2012) 23:948–58. doi: 10.1681/ASN.2011090887
13. Cardinal H, Lamarche F, Grondin S, Marsolais P, Lagacé AM, Duca A, et al. Organ donor management and delayed graft function in kidney transplant recipients: A multicenter retrospective cohort study. Am J Transplant. (2019) 19:277–84. doi: 10.1111/ajt.15127
14. Mas VR, Scian MJ, Archer KJ, Suh JL, David KG, Ren Q, et al. Pretransplant transcriptome profiles identify among kidneys with delayed graft function those with poorer quality and outcome. Molecular Med. (2011) 17:1311–22. doi: 10.2119/molmed.2011.00159
15. Kotsch K, Kunert K, Merk V, Reutzel-Selke A, Pascher A, Fritzsche F, et al. Novel markers in zero-hour kidney biopsies indicate graft quality and clinical outcome. Transplantation. (2010) 90:958–65. doi: 10.1097/TP.0b013e3181f546e8
16. Günther J, Resch T, Hackl H, Sattler A, Ebner S, Ritschl PV, et al. Identification of the activating cytotoxicity receptor NKG2D as a senescence marker in zero-hour kidney biopsies is indicative for clinical outcome. Kidney Int. (2017) 91:1447–63. doi: 10.1016/j.kint.2016.12.018
17. Kreepala C, Famulski KS, Chang J, Halloran PF. Comparing molecular assessment of implantation biopsies with histologic and demographic risk assessment. Am J Transplant. (2013) 13:415–26. doi: 10.1111/ajt.12043
18. Cravedi P, Maggiore U, Mannon RB. Low-density array PCR analysis of reperfusion biopsies: an adjunct to histological analysis. Nephrol Dial Transplant. (2010) 25:4077–86. doi: 10.1093/ndt/gfq297
19. Rödder S, Scherer A, Körner M, Eisenberger U, Hertig A, Raulf F, et al. Meta-analyses qualify metzincins and related genes as acute rejection markers in renal transplant patients. Am J Transplant. (2010) 10:286–97. doi: 10.1111/j.1600-6143.2009.02928.x
20. Schafer S, Viswanathan S, Widjaja AA, Lim WW, Moreno-Moral A, DeLaughter DM, et al. IL-11 is a crucial determinant of cardiovascular fibrosis. Nature. (2017) 552:110–5. doi: 10.1038/nature24676
21. Li JS, Chen X, Peng L, Wei SY, Zhao SL, Diao TT, et al. Angiopoietin-like-4, a potential target of tacrolimus, predicts earlier podocyte injury in minimal change disease. PLoS ONE. (2015) 10:e0137049. doi: 10.1371/journal.pone.0137049
22. Wilflingseder J, Sunzenauer J, Toronyi E, Heinzel A, Kainz A, Mayer B., et al. Molecular pathogenesis of post-transplant acute kidney injury: assessment of whole-genome mRNA and miRNA profiles. PLoS ONE. (2014) 9:e104164. doi: 10.1371/journal.pone.0104164
23. González-Domínguez É, Samaniego R, Flores-Sevilla JL, Campos-Campos SF, Gómez-Campos G, Salas A, et al. CD163L1 and CLEC5A discriminate subsets of human resident and inflammatory macrophages in vivo. J Leukoc Biol. (2015) 98:453–66. doi: 10.1189/jlb.3HI1114-531R
24. Fraser SM, Rajasundaram R, Aldouri A, Farid S, Morris-Stiff G, Baker R, et al. Acceptable outcome after kidney transplantation using “expanded criteria donor” grafts. Transplantation. (2010) 89:88–96. doi: 10.1097/TP.0b013e3181c343a5
25. Querard AH, Foucher Y, Combescure C, Dantan E, Larmet D, Lorent M., et al. Comparison of survival outcomes between expanded criteria donor and standard criteria donor kidney transplant recipients: a systematic review and meta-analysis. Transplant Int. (2016) 29:403–15. doi: 10.1111/tri.12736
26. van Ittersum FJ, Hemke AC, Dekker FW, Hilbrands LB, Christiaans MH, Roodnat JI, et al. Increased risk of graft failure and mortality in dutch recipients receiving an expanded criteria donor kidney transplant. Transplant Int. (2017) 30:14–28. doi: 10.1111/tri.12863
27. Randhawa PS, Minervini MI, Lombardero M, Duquesnoy R, Fung J, Shapiro R, et al. Biopsy of marginal donor kidneys: correlation of histologic findings with graft dysfunction. Transplantation. (2000) 69:1352–7. doi: 10.1097/00007890-200004150-00024
28. Anglicheau D, Loupy A, Lefaucheur C, Pessione F, Létourneau I, Côté I, et al. A simple clinico-histopathological composite scoring system is highly predictive of graft outcomes in marginal donors. Am J Transplant. (2008) 8:2325–34. doi: 10.1111/j.1600-6143.2008.02394.x
Keywords: marginal donor, borderline changes, kidney transplantation, gene expression, microarray
Citation: Hruba P, Krejcik Z, Dostalova Merkerova M, Klema J, Stranecky V, Slatinska J, Maluskova J, Honsova E and Viklicky O (2020) Molecular Fingerprints of Borderline Changes in Kidney Allografts Are Influenced by Donor Category. Front. Immunol. 11:423. doi: 10.3389/fimmu.2020.00423
Received: 20 September 2019; Accepted: 24 February 2020;
Published: 25 March 2020.
Edited by:
Thomas Friedrich Mueller, University Hospital Zürich, SwitzerlandReviewed by:
Luiza Guilherme, University of São Paulo, BrazilCopyright © 2020 Hruba, Krejcik, Dostalova Merkerova, Klema, Stranecky, Slatinska, Maluskova, Honsova and Viklicky. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ondrej Viklicky, b25kcmVqLnZpa2xpY2t5QGlrZW0uY3o=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.