
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Hum. Neurosci. , 18 July 2024
Sec. Brain Health and Clinical Neuroscience
Volume 18 - 2024 | https://doi.org/10.3389/fnhum.2024.1432441
 Prerana Nandish1
Prerana Nandish1 Shrinivasa B. M.1*
Shrinivasa B. M.1* Sujith Nath N.1
Sujith Nath N.1 G. Shankar1
G. Shankar1 Praveen Kumar Tripathi2
Praveen Kumar Tripathi2 Himani Kashyap3
Himani Kashyap3 Animesh Jain4
Animesh Jain4 Anup Anvikar5
Anup Anvikar5 Vani H. Chalageri1,6*†
Vani H. Chalageri1,6*†Malaria morbidity has various presentations and the focus now shifts to uncommon signs and symptoms of malaria infection such as cognitive impairment to address the morbidity when the mortality declines. About 50% of children admitted to hospitals due to malaria experience neurological complications due to factors like low blood sugar, inflammation, elevated pressure, decreased oxygen levels, and excitotoxicity. Malaria during pregnancy negatively also impacts children’s cognitive, behavioral, and executive function leading to neurodevelopmental delay due to increased susceptibility which can significantly affect maternal and child health, leading to higher rates of underestimated factors like anxiety, depression, and PTSD. Despite having the world’s second-largest tribal population, India’s indigenous and tribal communities and their mental health are less explored and less understood. Western psychological tools and neurocognitive assessment tools are not universally applicable, thus necessitating the development of tailored tools to investigate psychological or neurocognitive impairment. This paper has illuminated the hidden mental health consequences of malaria infection, emphasizing the prevalence, nature, and implications of psychological distress among affected individuals. The findings underscore the importance of recognizing and addressing these psychological consequences in the holistic management and prevention of malaria and its mental health consequences.
To identify relevant studies, a systematic search was conducted across Google Scholar, Springer, Elsevier and PubMed. The following search terms and keywords were used: “Malaria,” “cerebral malaria,” “psychological impact,” “mental health,” “cognitive functions,” and “neurological impairment.” The search was limited to articles published in English between 2019 and 2023. A total of 90 papers were reviewed.
Studies included in this review met the following criteria:
• Examined Malaria patients, survivors, or communities affected by malaria.
• Presented primary data on psychological outcomes post-malaria infection.
• Focused on the psychological and neurological impact of malaria infection.
Approximately 6,08,000 malaria deaths were recorded worldwide in 2022, with India and Indonesia accounting for about 94% of all malaria deaths in the South East Asia region (World Health Organization, 2024). As the disease heads toward elimination (Singh et al., 2024), the focus now shifts to uncommon and lesser known signs and symptoms of malaria infection such as cognitive impairment (GBD 2021 Nervous System Disorders Collaborators, 2024) to address the morbidity when the mortality declines. In the past 15 years, malaria’s global burden has risen from infection and mortality to neurologic and cognitive impairment, necessitating further research, prevention, and treatment, especially in regions where neurodiagnostic resources are scarce and the disease is endemic, where confirming the diagnosis of cerebral malaria (CM) is a challenging task (Mung’Ala-Odera et al., 2004; Birbeck et al., 2010; Ranjha and Sharma, 2021). Although in CM, the severity of neurological impairment may stem from suppressed gene activity leading to cellular dysfunction, axonal issues, disrupted signaling pathways, and ultimately neurodegeneration due to inflammation and cellular stress; it is not limited to severe cases, affecting even non-cerebral severe malaria and mild malaria (Karikari et al., 2021). Post-CM, developmental, cognitive, and behavioral deficits in sub-Saharan Africa can persist for up to a year contributed by factors like HIV co-infection, stature, and MRI abnormalities which are a significant burden on families and communities due to limited resources for treatment, education, and rehabilitation (Langfitt et al., 2019). Children under the age of five, who account for 67% of all fatalities worldwide, bear the greatest burden of severe malaria (Varo et al., 2020) including the rising resistance to insecticides and antimalarials (Wicht et al., 2020; Shahbodaghi and Rathjen, 2022; Suh et al., 2023) and mental health risks leading to neurological impairment (Goyal et al., 2023), necessitate a comprehensive malaria elimination program involving vector control (Ogunah et al., 2020), chemoprevention, vaccination, improved and early diagnosis accuracy (Pradhan et al., 2019), neuroprotective agents (Arthur et al., 2022), neurorehabilitation (Boubour et al., 2020) and regionally tailored strategies to address mental health consequences.
In 2022, malaria cases worldwide increased by 5 million compared to the previous year, with India responsible for 66% of these cases, and 233 million malaria cases were reported in the WHO African Region, constituting 94% of the global total (World Health Organization, 2024). However, there was a 25% increase in malaria cases in the WHO South-East Asia Region between 2021 and 2022, and 35.4 million pregnancies were reported in the WHO African Region, with 36% of them associated with malaria during pregnancy. The WHO observed a 72.3% reduction in indigenous malaria cases from 2010 to 2022. Plasmodium falciparum is the primary cause of malaria, causing over 99% of cases in Africa (Varo et al., 2020) with 25 million pregnant women facing P. falciparum infection annually, with one in four showing signs of placental infection which despite efforts to improve healthcare quality, can lead to death or disability from preventable or treatable illnesses, deformities, and injuries (Goyal et al., 2023). Nonetheless, funding for malaria research and development (R&D) declined for the fourth consecutive year, particularly in vaccines and basic research, while medicines continued to receive the largest share of funding (Desai et al., 2007; World Health Organization, 2024).
Malaria progresses to CM due to the interaction between host and parasite proteins, especially during blood-stage infection where the parasite reproduces and matures, due to the activation of endothelial cells by parasite-derived molecules (Lima et al., 2021) causing its proteins to appear on infected red blood cells (iRBCs), which allows them to interact with brain endothelium cells. This promotes the attachment of iRBCs to small blood vessels, leading to the breakdown of the BBB (blood brain barrier) and brain inflammation (Tunon-Ortiz and Lamb, 2019) leading to severe pathologies such as inflammation, capillary congestion, and dysregulated coagulation. This among individuals exposed to P. falciparum, with tissue ischemia, could lead to neurological impairments, including hearing, cognition, language, visual and motor coordination (Cartwright, 1972; Beare, 2024). The neuroinflammation in the brain triggered by malaria also leads to neural damage and cognitive impairments due to hemozoin production during infection (Velagapudi et al., 2019). Understanding this process is crucial for brain-related issues as psychological distress caused by malaria infection among affected individuals due to immune and nervous system alterations influenced by stimuli and pro-inflammatory or anti-inflammatory responses in malaria cases can be exacerbated by fear of relapse, severe illness, trauma, and economic strain with untreated malaria persisting for 3–5 years, with recurring episodes determined by underlying infection factors (Ouma et al., 2021; White, 2022; Malaria, 2023).
The interconnected immune and nervous systems and exogenous stimuli like infectious agents and vaccines can alter the immune system’s structure and function which can impact the functioning of the central nervous system (CNS) and cognitive behavioral responses (de Sousa et al., 2023). MRI and fluorescence angiography have been linked to severe cases of malarial retinopathy, longer unconsciousness periods, and neurological issues (MacCormick et al., 2022). A 2010 Ugandan study found that children with childhood malaria had retinopathy, severe hearing impairment, aphasia, dysarthria, motor deficits, movement disorders, gait disorders, behavior problems, and bilateral temporal lobe atrophy (Idro et al., 2010). Children with malaria retinopathy show significant clinical and laboratory differences compared to those without retinopathy, meeting the standard clinical case definition for CM. Early detection, intervention, and long-term follow-up studies are crucial for improving pediatric CM outcomes. Including malaria retinopathy in diagnostic criteria may enhance accuracy and prevent pre-existing CNS injuries as it is an in vivo perspective on the brain pathophysiology of CM that is not achievable by any other means (Beare, 2024). CM and hemoglobinuria are signs of retinopathy, requiring regular fundoscopic checks and comprehensive ophthalmoscopic training for healthcare professionals to manage severe cases (Olayinka et al., 2023). Experimental studies on CM in mice reveal that inflammation and bleeding can cause brain injury, affecting critical cognitive regions, and malaria-induced immune responses disrupting balance, leading to neurological impairments like seizures, altered consciousness, psychomotor difficulties, and behavioral abnormalities among other complications such as neurocognitive function, behavior, and thought processes, with coma development occurring gradually in adults (Velagapudi et al., 2019; GBD 2021 Nervous System Disorders Collaborators, 2024).
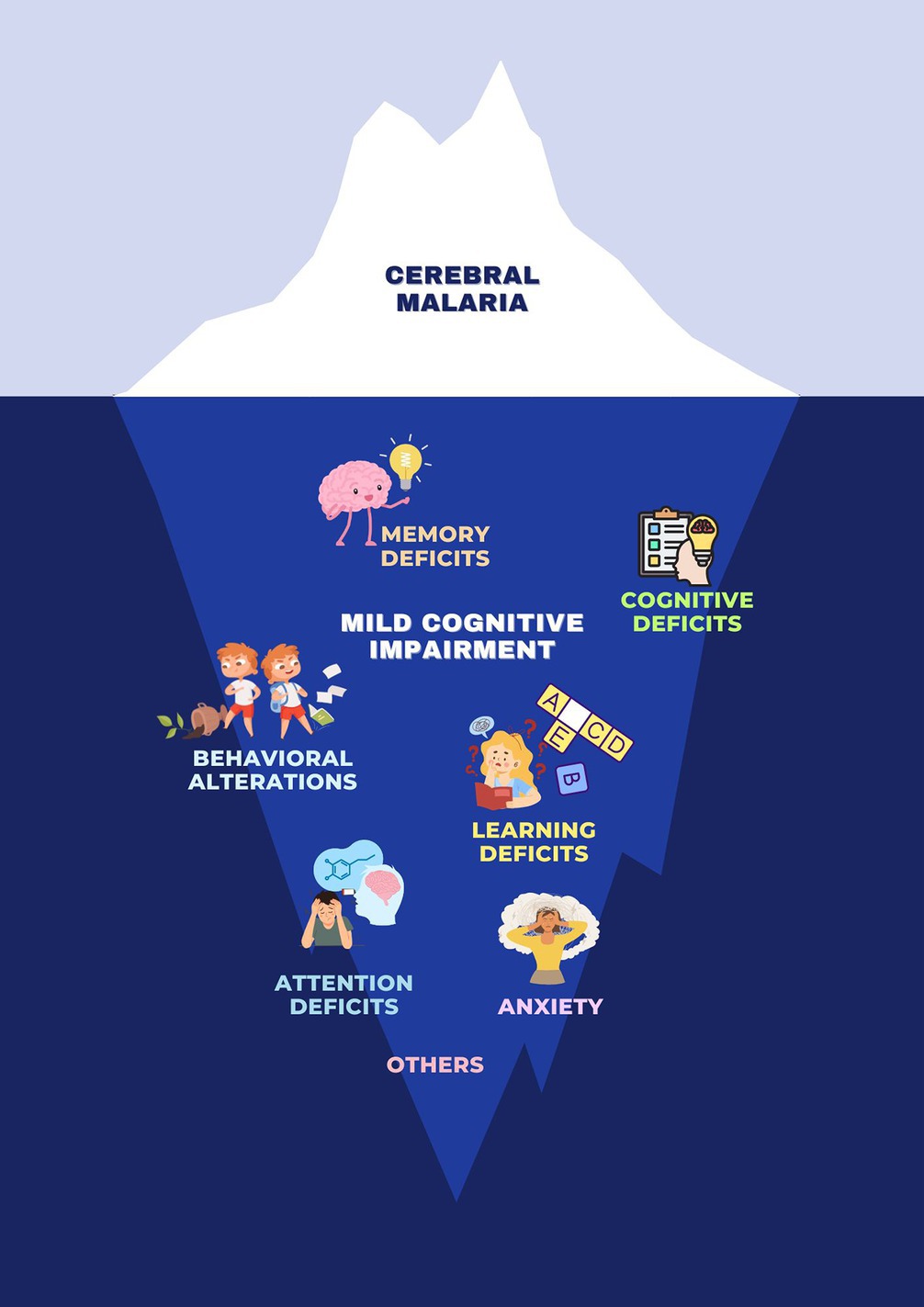
. Clinical spectrum of neurological manifestations of malaria. Malaria is commonly associated with a range of physical symptoms and diseases, but it also has significant psychological and neurological impacts. These can include mild cognitive impairment, behavioral alterations, attention deficits, memory deficits, anxiety, learning deficits, and broader cognitive deficits.
Mental health is more than the absence of mental disorders. It exists on a complex continuum, which is experienced differently from one person to the next, with varying degrees of difficulty and distress and potentially very different social and clinical outcomes (World Health Organization, 2024). Malaria has a complex psychological impact (Tapajós et al., 2019; Pessoa et al., 2022; Nakitende et al., 2023), where both malaria and anti-malarial drugs are linked to neuropsychiatric symptoms, often causing acute anxiety, fear, and obsessive-compulsive behaviors, leading to disruptive actions like aggression and defiance (Okojie et al., 2019; Reddy, 2019; Chaudhry et al., 2022). Guillain-Barré syndrome (GBS), also known as acute inflammatory demyelinating polyneuropathy (AIDP), is a neurological side effect of malaria treatment in patients experiencing aparasitaemic symptoms (Carreira et al., 2019). Post-malaria neurological syndrome (PMNS), a distinct neurological disorder results during severe P. falciparum recovery, and is distinct from other post-malaria neurological disorders (Poulet et al., 2019) as it arises within two months after CM, once parasites have cleared with symptoms like confusion, fever, seizures, aphasia, tremors, and myoclonus (Poulet et al., 2019). Opsoclonus-myoclonus syndrome is characterized by repeated jerks and movements of eyes and limbs, occuring as a neurological complication following the acute phase of PMNS (Lev et al., 2020). There may also be a higher chance of dementia associated later in life with cerebral malaria, according to research (Benyumiza et al., 2023). Factors, such as headaches, body aches, sensory symptoms, tiredness, and weakness, also increase susceptibility to mental disorders. About 50% of children admitted to hospitals due to malaria experience neurological complications due to factors like low blood sugar, inflammation, elevated pressure, decreased oxygen levels, and excitotoxicity. Customized evaluations of their performance and patient outcomes can identify key drivers and post-malaria effects (Lima et al., 2021).
This is crucial as some of these symptoms and outcomes are not only limited to CM but are also seen in non severe malaria among both children and adults (Vitor-Silva et al., 2009; Fink et al., 2013; Tapajós et al., 2019; de Sousa et al., 2021).
Malaria has a noticeable effect on children’s cognitive development, which is often overlooked as it is still unclear how CM impacts a child’s abilities and functions beyond the aspects related to neurological consequences (Fernando et al., 2010; White, 2022). However, it affects children’s cognitive development, leading to neurological, cognitive, and behavioral issues exacerbated by anemia and malnutrition, especially in low- and middle-income countries (LMICs), due to disruption of brain oxygen delivery and impaired cognition in infected adults which hinders education and employment leading to adverse cognitive and behavioral outcomes, particularly affecting memory, attention, language, and externalizing behavioral issues (Ssemata et al., 2020). Research in Uganda shows that children with severe malarial anemia (SMA) and CM have lower reading scores in comparison to uncomplicated malaria, suggesting post-discharge malaria chemoprevention measures that could improve long-term academic performance (Nakitende et al., 2023). CM and SMA are linked to neuro-developmental impairment in African children, but long-term mental health disorders are not well-understood (Trivedi and Chakravarty, 2022). The impact on cognitive and behavioral abilities leads to poorer performance in one out of four children after more than five episodes compared to those with up to three fever episodes (John et al., 2008; Rosa-Gonçalves et al., 2022).
A study based on children aged 0–18 years showed clinical features like impaired consciousness, respiratory distress, multiple convulsions, prostration, abnormal bleeding, jaundice, severe anemia, hypoglycemia, acidosis, hyperlactatemia, renal impairment, hyperparasitemia, CM, or SMA, often faced neurological impairments, limitations in daily activities, and restrictions in life participation with disability aspects including issues in mental, sensory, and neuromusculoskeletal functions (Engeda et al., 2023). A 2022 study found that Computerized Cognitive Rehabilitation Therapy (CCRT) did not significantly improve academic performance in Ugandan schoolchildren aged five to twelve years, with age, socioeconomic status, gender, and home environment playing significant roles (Miller et al., 2022) while another study evaluating CCRT on children recovering from severe malaria (SM) showed some improvement in learning outcomes, but the intervention group showed lower working memory scores.
In severe cases, being in the hospital also can be stressful for children, making them feel like they have little control over what’s happening to them as illness, injury, and hospital stays can impact a child’s development, including thinking, physical abilities, emotions, and social skills. Such traumatic experiences can lead to immediate or long-term psychological effects which can improve through collaboration with psychologists, human development, and counseling globally (Claridge and Powell, 2023). Establishing childhood disability clinics with interdisciplinary teams could help reduce the prevalence and severity of these disabilities, especially considering malaria’s significant impact (Abdullahi et al., 2022).
In Sub-Saharan Africa (SSA), malaria is a major cause of illness and death (Datta et al., 2023) particularly during the pregnancy of the first trimester (Accrombessi et al., 2019; Elphinstone et al., 2019; Garrison et al., 2022), with an increased risk of P. falciparum infection leading to severe consequences like pregnancy loss (Mahamar et al., 2021), reduced head circumference (Dombrowski et al., 2019), multiple organ dysfunctions (Tripathy et al., 2007), anemia, pulmonary edema, and hypoglycemia due to asymptomatic or low parasitic presence that causes severe consequences with mortality rates reaching up to 50% in the second and third trimesters (Reddy, 2019). Parasitized erythrocytes in the placenta cause maternal immune-inflammatory response, placental pathological changes, poor birth outcomes (Omer et al., 2021). Placental malaria significantly endangers maternal and fetal health and may contribute to impaired neurodevelopment and future developmental disorders (Lawford et al., 2019) which negatively impacts children’s cognitive, behavioral, and executive function (Bangirana et al., 2023) leading to neurodevelopmental delay (Weckman et al., 2021; Garrison et al., 2022) due to increased susceptibility which can significantly affect maternal as well as child health, that leads to higher rates of underestimated factors like anxiety, depression, and PTSD. A case report reveals PM discordance in twins, with a submicroscopic infection in the mother causing worse birth and neurodevelopmental outcomes which raises questions about long-term neurodevelopmental effects from in utero infection (Conroy et al., 2019). No studies have yet reported on the neurological functioning of neonates exposed to malaria in utero which calls for further studies to evaluate its impact on pregnancy as it is essential to understand the mechanism which will enable healthcare professionals to provide effective postpartum care and develop preventive measures as common psychological challenges like chronic worry, depression, social isolation, financial strain, and self-esteem issues are to be addressed for maintaining well-being by validating tools for accurate diagnosis (Chi et al., 2021; Westby et al., 2021). As mental disorders are highest among illiterate and unemployed individuals, with socioeconomic factors like deprivation and poverty strongly linked to these conditions strengthening these needs at the primary healthcare level is crucial for reducing mental morbidity, as mental health is essential for overall health (Reddy, 2019).
In India, malaria cases primarily originate from rural and tribal areas (World Health Organization, 2024), with a lack of awareness about the disease despite primary health centers it is a multifactorial problem (Sivanandan et al., 2020; Nema and Ghosh, 2022; Rahi and Sharma, 2022; Kafczyk and Hämel, 2024). This could be a reason why India’s mental disorder prevalence rates are lower than those of Western countries, possibly due to genetic predispositions, family support systems, cultural influences, lifestyles, and coping mechanisms. The scarcity of trained healthcare professionals and traditional beliefs in supernatural powers contribute to delays in diagnosis and treatment which could be bridged by recruiting tribal individuals, training healers and community health workers to understand traditional herbal medicines to strengthen the primary healthcare system (Negi and Singh, 2019; Nema et al., 2019; Kumar et al., 2020) by integrating mental health support into primary healthcare settings as the success of any healthcare intervention program relies on the effective acceptance and utilization of the services provided within the community which in malaria-endemic regions is often limited by factors like household income, proximity to healthcare facilities, and communal beliefs (Singh et al., 2017; Awasthi et al., 2024). However, acceptance of this could significantly assist individuals affected by malaria’s physical and psychological aspects, as it extends beyond individuals, affecting families and communities with increased caregiver burden, reduced productivity, and strained social relationships, particularly in Africa and South Asia among LMICs where research has shown a links malaria to arterial hypertension and depression which increases susceptibility to malaria by affecting immunity and behavior (Jenkins et al., 2017; Volpe and Battistoni, 2019) risking both malaria and mental health disorders impeding treatment and recovery (Jenkins et al., 2019).
This review, despite the significant lack of research and characterization of malaria and mental health status (Cianconi et al., 2019), highlights the pressing need for further research on the psychological impact of malaria as a successful treatment, particularly for non-severe malaria which requires understanding cognitive and behavioral consequences, enabling targeted therapies (Rosa-Gonçalves et al., 2022). A study reveals that type 2 stimuli-induced immune responses positively impact long-term recognition memory in healthy mice, which confirms the late neurocognitive behavioral dysfunction following non-severe malaria indicating a potential for vaccinations to improve memory weakened by aging and chronic diseases (de Sousa et al., 2021). Among children hospitalized with CM or severe malarial anemia (SMA) with neurologic injury and higher plasma tau levels suggest that plasma tau could be a reliable biomarker for identifying children at risk of persistent neurocognitive impairment (NCI), potentially aiding in acute cognitive rehabilitation (Datta et al., 2021). Despite having the world’s second-largest tribal population, India’s indigenous and tribal communities and their mental health are underdeveloped, and Western psychological tools are not universally applicable, necessitating the development of tailored tools to investigate malaria’s link to psychological distress and evaluate intervention’s effectiveness (Okumu et al., 2022). With the help of the community’s teachers, activists, and volunteers, states must assess this at a tribal and cross-border level by establishing goals using evidence-based public health strategies (Gordon et al., 2019; Lawford et al., 2019; Bangirana et al., 2023) to spread essential lessons about preventing malaria as P. falciparum infections can trigger relapses months or even years following the initial infection (de Sousa Pinto et al., 2021; Sato, 2021).
Malaria has a profound impact on endemic regions. Throughout the world, it is characterized by high incidence, mortality, and morbidity rates, with enduring consequences that require integrated management using preventive treatment (Rehman et al., 2019; Cohee et al., 2020), understanding pathogenesis (Bauserman et al., 2019), addressing socioeconomic barriers (Anjorin et al., 2023; Guin et al., 2023; Kooko et al., 2023) and extending vector control measures (Nema et al., 2019; Kafczyk and Hämel, 2024) to support mental health morbidity caused by malaria. Limited healthcare access has to be addressed with the help of advanced and upcoming methods like placental impression smears (Ouédraogo et al., 2019) for early detection of malaria. The accurate diagnosis of malaria is vital given the similarity in symptoms between malaria and other diseases like COVID-19 as there’s a risk of clinicians misdiagnosing one as the other, potentially overlooking the possibility of a co-infection (Gutman et al., 2020; Hussein et al., 2020). In terms of lowering mortality or treatment-related effects such as neurocognitive impairments, current malarial biology therapeutics are still insufficient and (Siddiqui et al., 2020) there is no effective therapy available for addressing the cognitive and behavioral effects resulting from malaria, which necessitates the need for conducting psychological research, developing comprehensive healthcare strategies, and targeted therapies, and collaborating across sectors to address malaria’s impact on cognition. Implementing preventive measures like insecticide-treated bed nets and rapid access to care and effective treatment of uncomplicated malaria is crucial for preventing SM and its complications (Conroy et al., 2019; Boëte et al., 2021).
PN: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. SBM: Formal analysis, Investigation, Supervision, Validation, Writing – review & editing. SN: Writing – review & editing. GS: Writing – review & editing. PKT: Writing – review & editing. HK: Writing – review & editing. AJ: Writing review & editing. AA: Writing – review & editing. VHC: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Grant-in-aid Scheme of the Department of Health Research for ‘Inter-Sectoral Convergence & Coordination for Promotion and Guidance on Health Research-approval’ to the research project entitled “Assessment of impact of malaria disease on cognitive and executive functions among the adult malaria patients in Mangaluru - cohort study” covered under the component Mental Health to ‘Research Studies With Emphasis on Public Health’ of the aforesaid scheme and the “Longitudinal community evaluation of survivorship, biological efficacy, fabric integrity and community acceptability of long-lasting insecticidal net MiraNet in comparison with Magnet LN® as positive control in India” project funded by Ifakara Health Institute, Tanzania.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abdullahi, A., Wong, T. W. L., and Ng, S. S. M. (2022). Establishing childhood disability clinics may help reduce the prevalence of disability among children in Africa: A viewpoint. Front. Public Health 10:1010437. doi: 10.3389/fpubh.2022.1010437
Accrombessi, M., Yovo, E., Fievet, N., Cottrell, G., Agbota, G., Gartner, A., et al. (2019). Effects of malaria in the first trimester of pregnancy on poor maternal and birth outcomes in Benin. Clin. Infect. Dis. 69, 1385–1393. doi: 10.1093/cid/ciy1073
Anjorin, S., Okolie, E., and Yaya, S. (2023). Malaria profile and socioeconomic predictors among under-five children: an analysis of 11 sub-Saharan African countries. Malar. J. 22:55. doi: 10.1186/s12936-023-04484-8
Arthur, R., Navik, U., and Kumar, P. (2022). Repurposing artemisinins as neuroprotective agents: a focus on the PI3k/Akt signalling pathway. Naunyn Schmiedeberg's Arch. Pharmacol. 396, 1–13. doi: 10.1007/s00210-022-02350-z
Awasthi, K. R., Jancey, J., Clements, A. C. A., Rai, R., and Leavy, J. E. (2024). Community engagement approaches for malaria prevention, control and elimination: a scoping review. BMJ Open 14:e081982. doi: 10.1136/bmjopen-2023-081982
Bangirana, P., Conroy, A. L., Opoka, R. O., Semrud-Clikeman, M., Jang, J. H., Apayi, C., et al. (2023). Effect of malaria and malaria chemoprevention regimens in pregnancy and childhood on neurodevelopmental and behavioral outcomes in children at 12, 24, and 36 months: a randomized clinical trial. Clin. Infect. Dis. 76, 600–608. doi: 10.1093/cid/ciac815
Bauserman, M., Conroy, A. L., North, K., Patterson, J., Bose, C., and Meshnick, S. (2019). An overview of malaria in pregnancy. Semin. Perinatol. 43, 282–290. doi: 10.1053/j.semperi.2019.03.018
Beare, N. A. V. (2024). Cerebral malaria—using the retina to study the brain. Eye [Internet]. Available at: https://www.nature.com/articles/s41433-023-02432-z
Benyumiza, D., Kumakech, E., Gutu, J., Banihani, J., Mandap, J., Talib, Z. M., et al. (2023). Prevalence of dementia and its association with central nervous system infections among older persons in northern Uganda: cross-sectional community-based study. BMC Geriatr. 23:551. doi: 10.1186/s12877-023-04174-9
Birbeck, G. L., Beare, N., Lewallen, S., Glover, S. J., Molyneux, M. E., Kaplan, P. W., et al. (2010). Identification of malaria retinopathy improves the specificity of the clinical diagnosis of cerebral malaria: Findings from a prospective cohort study. Am. J. Trop. Med. Hyg. 82, 231–234. doi: 10.4269/ajtmh.2010.09-0532
Boëte, C., Burza, S., Lasry, E., Moriana, S., and Robertson, W. (2021). Malaria vector control tools in emergency settings: what do experts think? Results from a DELPHI survey. Confl. Heal. 15:93. doi: 10.1186/s13031-021-00424-y
Boubour, A., Mboma, S., TVõ, G. L. B., Seydel, K. B., Mallewa, M., et al. (2020). “We can’t handle things we don’t know about”: Perceived neurorehabilitation challenges for Malawian paediatric cerebral malaria survivors. BMC Pediatr. 20:503. doi: 10.1186/s12887-020-02405-1
Carreira, J., Casella, M. I., Ascenção, B. B., Luis, N. P., Gonçalves, A. C., Brito, A. P., et al. (2019). Acute disseminated encephalomyelitis, a rare post-malaria neurological complication: case report and review of the literature. Travel Med. Infect. Dis. 28, 81–85. doi: 10.1016/j.tmaid.2018.03.005
Cartwright, F. (1972). Disease and history. Pers. Res. Collect. [Internet]. Available at: https://scholar.dominican.edu/cynthia-stokes-brown-books-personal-research/205
Chaudhry, H. E., Khan, S., Jamil, S., Shaik, T. A., Ehsan Ullah, S., Bseiso, A., et al. (2022). Chloroquine-induced psychosis: a case report. Cureus 14:e30498. doi: 10.7759/cureus.30498
Chi, P., Owino, E., IJao, F. O., Ogutu, B., Bejon, P., et al. (2021). Understanding the benefits and burdens associated with a malaria human infection study in Kenya: experiences of study volunteers and other stakeholders. Trials 22:494. doi: 10.1186/s13063-021-05455-7
Cianconi, P., Lesmana, C. B. J., Ventriglio, A., and Janiri, L. (2019). Mental health issues among indigenous communities and the role of traditional medicine. Int. J. Soc. Psychiatry 65, 289–299. doi: 10.1177/0020764019840060
Claridge, A. M., and Powell, O. J. (2023). Children’s experiences of stress and coping during hospitalization: a mixed-methods examination. J. Child Health Care 27, 531–546. doi: 10.1177/13674935221078060
Cohee, L. M., Opondo, C., Clarke, S. E., Halliday, K. E., Cano, J., Shipper, A. G., et al. (2020). Preventive malaria treatment among school-aged children in sub-Saharan Africa: a systematic review and meta-analyses. Lancet Glob. Health 8, e1499–e1511. doi: 10.1016/S2214-109X(20)30325-9
Conroy, A. L., Bangirana, P., Muhindo, M. K., Kakuru, A., Jagannathan, P., Opoka, R. O., et al. (2019). Case report: birth outcome and neurodevelopment in placental malaria discordant twins. Am. J. Trop. Med. Hyg. 100, 552–555. doi: 10.4269/ajtmh.18-0659
Conroy, A. L., Datta, D., and John, C. C. (2019). What causes severe malaria and its complications in children? Lessons learned over the past 15 years. BMC Med. 17:52. doi: 10.1186/s12916-019-1291-z
Datta, D., Bangirana, P., Opoka, R. O., Conroy, A. L., Co, K., Bond, C., et al. (2021). Association of Plasma tau with Mortality and Long-term Neurocognitive Impairment in survivors of pediatric cerebral malaria and severe malarial Anemia. JAMA Netw. Open 4:e2138515. doi: 10.1001/jamanetworkopen.2021.38515
Datta, D., Gopinadhan, A., Soto, A., Bangirana, P., Opoka, R. O., Conroy, A. L., et al. (2023). Blood biomarkers of neuronal injury in paediatric cerebral malaria and severe malarial anaemia. Brain Commun. 5:fcad323. doi: 10.1093/braincomms/fcad323
Desai, M., ter Kuile, F. O., Nosten, F., McGready, R., Asamoa, K., Brabin, B., et al. (2007). Epidemiology and burden of malaria in pregnancy - the lancet infectious diseases. Lancet Infect. Dis. 7, 93–104. doi: 10.1016/S1473-3099(07)70021-X
de Sousa, L. P., Ribeiro-Gomes, F. L., de Almeida, R. F., Souza, T. M., Werneck, G. L., Souza, D. O., et al. (2021). Immune system challenge improves recognition memory and reverses malaria-induced cognitive impairment in mice. Sci. Rep. 11:14857. doi: 10.1038/s41598-021-94167-8
de Sousa, L. P., Rosa-Gonçalves, P., Ribeiro-Gomes, F. L., and Daniel-Ribeiro, C. T. (2023). Interplay between the immune and nervous cognitive Systems in Homeostasis and in malaria. Int. J. Biol. Sci. 19, 3383–3394. doi: 10.7150/ijbs.82556
de Sousa Pinto, L., Arroz, J. A. H., Martins, M., Hartz, Z., Negrao, N., Muchanga, V., et al. (2021). Malaria prevention knowledge, attitudes, and practices in Zambezia Province, Mozambique. Malar. J. 20:293. doi: 10.1186/s12936-021-03825-9
Dombrowski, J. G., Souza, R. M. d., Lima, F. A., Bandeira, C. L., Murillo, O., Costa, D. d. S., et al. (2019). Association of Malaria Infection during Pregnancy with Head Circumference of newborns in the Brazilian Amazon. JAMA Netw. Open 2:e193300. doi: 10.1001/jamanetworkopen.2019.3300
Elphinstone, R. E., Weckman, A. M., McDonald, C. R., Tran, V., Zhong, K., Madanitsa, M., et al. (2019). Early malaria infection, dysregulation of angiogenesis, metabolism and inflammation across pregnancy, and risk of preterm birth in Malawi: a cohort study. PLoS Med. 16:e1002914. doi: 10.1371/journal.pmed.1002914
Engeda, E., Aldersey, H., Davison, C., Gelaye, K., and Fayed, N. (2023). Severe malaria-related disability in Ethiopian children from the perspectives of caregivers: an interpretive description study. Disabil. Rehabil. 46, 2327–2337. doi: 10.1080/09638288.2023.2221457
Fernando, S. D., Rodrigo, C., and Rajapakse, S. (2010). The “hidden” burden of malaria: cognitive impairment following infection. Malar. J. 9:366. doi: 10.1186/1475-2875-9-366
Fink, G., Olgiati, A., Hawela, M., Miller, J. M., and Matafwali, B. (2013). Association between early childhood exposure to malaria and children’s pre-school development: evidence from the Zambia early childhood development project. Malar. J. 12, 1–9.
Garrison, A., Boivin, M. J., Fiévet, N., Zoumenou, R., Alao, J. M., Massougbodji, A., et al. (2022). The effects of malaria in pregnancy on neurocognitive development in children at 1 and 6 years of age in Benin: a prospective mother-child cohort. Clin. Infect. Dis. 74, 766–775. doi: 10.1093/cid/ciab569
Garrison, A., Maselko, J., Saurel-Cubizolles, M. J., Courtin, D., Zoumenou, R., Boivin, M. J., et al. (2022). The impact of maternal depression and parent–child interactions on risk of parasitic infections in early childhood: a prospective cohort in Benin. Matern. Child Health J. 26, 1049–1058. doi: 10.1007/s10995-021-03317-x
GBD 2021 Nervous System Disorders Collaborators (2024). Global, regional, and national burden of disorders affecting the nervous system, 1990-2021: a systematic analysis for the global burden of disease study 2021. Lancet Neurol. 23, 344–381. doi: 10.1016/S1474-4422(24)00038-3
Gordon, A., Vander Meulen, R. J., and Maglior, A. (2019). The 2019 Isdell:flowers cross border malaria initiative round table: community engagement in the context of malaria elimination. Malar. J. 18:432. doi: 10.1186/s12936-019-3054-x
Goyal, G., Kaur, U., Sharma, M., and Sehgal, R. (2023). Neuropsychiatric aspects of parasitic infections-a review. Neurol. India 71, 228–232. doi: 10.4103/0028-3886.375424
Guin, P., Kumar, E. L., and Mukhopadhyay, I. (2023). Do climatic and socioeconomic factors explain population vulnerability to malaria? Evidence from a national survey, India. Ind. J. Public Health 67, 226–234. doi: 10.4103/ijph.ijph_964_22
Gutman, J. R., Lucchi, N. W., Cantey, P. T., Steinhardt, L. C., Samuels, A. M., Kamb, M. L., et al. (2020). Malaria and parasitic neglected tropical diseases: potential Syndemics with COVID-19? Am. J. Trop. Med. Hyg. 103, 572–577. doi: 10.4269/ajtmh.20-0516
Hussein, M. I. H., Albashir, A. A. D., Elawad, O. A. M. A., and Homeida, A. (2020). Malaria and COVID-19: unmasking their ties. Malaria J. 19:457. doi: 10.1186/s12936-020-03541-w
Idro, R., Kakooza-Mwesige, A., Balyejjussa, S., Mirembe, G., Mugasha, C., Tugumisirize, J., et al. (2010). Severe neurological sequelae and behaviour problems after cerebral malaria in Ugandan children. BMC. Res. Notes 3:104. doi: 10.1186/1756-0500-3-104
Jenkins, R., Ong'echa, M., Othieno, C., Ongeri, L., Sifuna, P., Omollo, R., et al. (2019). Malaria, mental disorders, immunity and their inter-relationships - a cross sectional study in a household population in a health and demographic surveillance site in Kenya. EBioMedicine 39, 369–376. doi: 10.1016/j.ebiom.2018.11.064
Jenkins, R., Othieno, C., Ongeri, L., Ongecha, M., Sifuna, P., Omollo, R., et al. (2017). Malaria and mental disorder: a population study in an area endemic for malaria in Kenya. World Psychiatry 16, 324–325. doi: 10.1002/wps.20473
John, C. C., Bangirana, P., Byarugaba, J., Opoka, R. O., Idro, R., and Jurek, A. M. (2008). Cerebral malaria in children is associated with long-term cognitive impairment. Pediatrics 122, e92–e99. doi: 10.1542/peds.2007-3709
Kafczyk, T., and Hämel, K. (2024). Challenges and opportunities in strengthening primary mental healthcare for older people in India: a qualitative stakeholder analysis. BMC Health Serv. Res. 24:206. doi: 10.1186/s12913-024-10622-y
Karikari, A. A., Wruck, W., and Adjaye, J. (2021). Inflammation and cellular stress induced neurological sequelae of plasmodium falciparum malaria [internet]. bioRxiv. doi: 10.1101/2021.06.16.448682v1
Kooko, R., Wafula, S. T., and Orishaba, P. (2023). Socioeconomic determinants of malaria prevalence among under five children in Uganda: evidence from 2018-19 Uganda malaria Indicator survey. J. Vector Borne Dis. 60, 38–48. doi: 10.4103/0972-9062.353251
Kumar, M. M., Pathak, V. K., and Ruikar, M. (2020). Tribal population in India: a public health challenge and road to future. J. Family Med. Prim. Care 9, 508–512. doi: 10.4103/jfmpc.jfmpc_992_19
Langfitt, J. T., McDermott, M. P., Brim, R., Mboma, S., Potchen, M. J., Kampondeni, S. D., et al. (2019). Neurodevelopmental impairments 1 year after cerebral malaria. Pediatrics 143:e20181026. doi: 10.1542/peds.2018-1026
Lawford, H. L. S., Lee, A. C., Kumar, S., Liley, H. G., and Bora, S. (2019). Establishing a conceptual framework of the impact of placental malaria on infant neurodevelopment. Int. J. Infect. Dis. 84, 54–65. doi: 10.1016/j.ijid.2019.04.019
Lev, D., Yahalom, G., Rabinowicz, S., Leshem, E., and Schwartz, E. (2020). Opsoclonus-myoclonus as a presentation of post-malaria neurological syndrome. J. Travel Med. 27:taaa051. doi: 10.1093/jtm/taaa051
Lima, M. N., Freitas, R. J. R. X., Passos, B. A. B. R., Darze, A. M. G., Castro-Faria-Neto, H. C., and Maron-Gutierrez, T. (2021). Neurovascular interactions in malaria. Neuroimmunomodulation 28, 108–117. doi: 10.1159/000515557
MacCormick, I. J. C., Barrera, V., Beare, N. A. V., Czanner, G., Potchen, M., Kampondeni, S., et al. (2022). How does blood-retinal barrier breakdown relate to death and disability in pediatric cerebral malaria? J. Infect. Dis. 225, 1070–1080. doi: 10.1093/infdis/jiaa541
Mahamar, A., Andemel, N., Swihart, B., Sidibe, Y., Gaoussou, S., Barry, A., et al. (2021). Malaria infection is common and associated with perinatal mortality and preterm delivery despite widespread use of chemoprevention in Mali_ an observational study 2010 to 2014. Clin. Infect. Dis. 73, 1355–1361. doi: 10.1093/cid/ciab301
Malaria: The past and the present [internet]. (2023). Available at: https://www.mdpi.com/2076-2607/7/6/179.
Miller, K., Lori, J., Liu, X., Boivin, M., and Giordani, B. (2022). The cognitive burden of severe malaria in the Ugandan classroom and the effects of a computerized intervention. Appl. Nurs. Res. 63:151551. doi: 10.1016/j.apnr.2021.151551
Mung’Ala-Odera, V., Snow, R. W., and CRJC, N. (2004). “The burden of the neurocognitive impairment associated with plasmodium falciparum malaria in sub-Saharan Africa” in The intolerable burden of malaria II: What’s new, What’s needed: Supplement to volume 71(2) of the American journal of tropical medicine and hygiene [internet] (American Society of Tropical Medicine and Hygiene). Available at: https://www.ncbi.nlm.nih.gov/books/NBK3755/
Nakitende, A. J., Bangirana, P., Nakasujja, N., Ssenkusu, J. M., Bond, C., Idro, R., et al. (2023). Severe malaria and academic achievement. Pediatrics 151:e2022058310. doi: 10.1542/peds.2022-058310
Negi, D. P., and Singh, D. M. M. (2019). Tribal health in India: a need for a comprehensive health policy. Int. J. Health Sci. 9, 3–5.
Nema, S., and Ghosh, S. K. (2022). Malaria and malnutrition together jeopardizes India’s tribal community and disease elimination. Pathog. Glob. Health 116, 463–464. doi: 10.1080/20477724.2022.2100190
Nema, S., Verma, A. K., and Bharti, P. K. (2019). Strengthening diagnosis is key to eliminating malaria in India. Lancet Infect. Dis. 19, 1277–1278. doi: 10.1016/S1473-3099(19)30544-4
Ogunah, J. A., Lalah, J. O., and Schramm, K. W. (2020). Malaria vector control strategies. What is appropriate towards sustainable global eradication? Sustain. Chem. Pharm. 18:100339. doi: 10.1016/j.scp.2020.100339
Okojie, A. K., Rauf, K., and Iyare, E. (2019). The impact of plasmodium Berghei exposure in-utero on neurobehavioral profile in mice. Basic Clin. Neurosci. 10, 99–107. doi: 10.32598/bcn.9.10.95
Okumu, F., Gyapong, M., Casamitjana, N., Castro, M. C., Itoe, M. A., Okonofua, F., et al. (2022). What Africa can do to accelerate and sustain progress against malaria. PLoS Glob Public Health 2:e0000262. doi: 10.1371/journal.pgph.0000262
Olayinka, O. O., Abiodun, P. O., Jegede TOFasoranti, I. O., Salau, Q. O., Kareem, A. J., et al. (2023). Malaria retinopathy among under-five children with severe and uncomplicated malaria in a tertiary health institution in Southwest Nigeria: a comparative study. Adv. Infect. Dis. 13, 355–374. doi: 10.4236/aid.2023.133031
Omer, S., Franco-Jarava, C., Noureldien, A., Omer, M., Abdelrahim, M., Molina, I., et al. (2021). Impact of placental malaria on maternal, placental and fetal cord responses and its role in pregnancy outcomes in women from Blue Nile state, Sudan. Malar. J. 20:35. doi: 10.1186/s12936-021-03580-x
Ouédraogo, S., Accrombessi, M., Diallo, I., Codo, R., Ouattara, A., Ouédraogo, L., et al. (2019). Placental impression smears is a good indicator of placental malaria in sub-Saharan Africa. Pan Afr. Med. J. 34:30. doi: 10.11604/pamj.2019.34.30.20013
Ouma, B. J., Bangirana, P., Ssenkusu, J. M., Datta, D., Opoka, R. O., Idro, R., et al. (2021). Plasma angiopoietin-2 is associated with age-related deficits in cognitive sub-scales in Ugandan children following severe malaria. Malar. J. 20:17. doi: 10.1186/s12936-020-03545-6
Pessoa, R. C., Oliveira-Pessoa, G. F., Souza, B. K. A., Sampaio, V. S., Pinto, A. L. C. B., Barboza, L. L., et al. (2022). Impact of plasmodium vivax malaria on executive and cognitive functions in elderlies in the Brazilian Amazon. Sci. Rep. 12:10361. doi: 10.1038/s41598-022-14175-0
Poulet, A., Bou Ali, H., Savini, H., Kaphan, E., and Parola, P. (2019). Post-malaria neurological syndrome: imported case series and literature review to unscramble the auto-immune hypothesis. Travel Med. Infect. Dis. 29, 16–20. doi: 10.1016/j.tmaid.2018.09.003
Pradhan, S., Pradhan, M. M., Dutta, A., Shah, N. K., Joshi, P. L., Pradhan, K., et al. (2019). Improved access to early diagnosis and complete treatment of malaria in Odisha, India. PLoS ONE 14:e0208943. doi: 10.1371/journal.pone.0208943
Rahi, M., and Sharma, A. (2022). Malaria control initiatives that have the potential to be gamechangers in India’s quest for malaria elimination. Lancet Reg. Health Southeast Asia 2:100009. doi: 10.1016/j.lansea.2022.04.005
Ranjha, R., and Sharma, A. (2021). Forest malaria: the prevailing obstacle for malaria control and elimination in India. BMJ Glob. Health 6:e005391. doi: 10.1136/bmjgh-2021-005391
Reddy, V. (2019). Mental health issues and challenges in India: a review. Int. J. Sci. Res. Publ. 3, 1–3.
Rehman, A. M., Maiteki-Sebuguzi, C., Gonahasa, S., Okiring, J., Kigozi, S. P., Chandler, C. I. R., et al. (2019). Intermittent preventive treatment of malaria delivered to primary schoolchildren provided effective individual protection in Jinja, Uganda: secondary outcomes of a cluster-randomized trial (START-IPT). Malar. J. 18:318. doi: 10.1186/s12936-019-2954-0
Rosa-Gonçalves, P., Ribeiro-Gomes, F. L., and Daniel-Ribeiro, C. T. (2022). Malaria related neurocognitive deficits and behavioral alterations. Front. Cell. Infect. Microbiol. 12:829413. doi: 10.3389/fcimb.2022.829413/full
Sato, S. (2021). Plasmodium—a brief introduction to the parasites causing human malaria and their basic biology. J. Physiol. Anthropol. 40:1. doi: 10.1186/s40101-020-00251-9
Shahbodaghi, S. D., and Rathjen, N. A. (2022). Malaria: prevention, diagnosis, and treatment. Am. Fam. Physician 106, 270–278.
Siddiqui, A. J., Adnan, M., Jahan, S., Redman, W., Saeed, M., and Patel, M. (2020). Neurological disorder and psychosocial aspects of cerebral malaria: what is new on its pathogenesis and complications? A minireview. Folia Parasitol. (Praha) :67. doi: 10.14411/fp.2020.015.html
Singh, M. P., Rajvanshi, H., Bharti, P. K., Anvikar, A. R., and Lal, A. A. (2024). Time series analysis of malaria cases to assess the impact of various interventions over the last three decades and forecasting malaria in India towards the 2030 elimination goals. Malar. J. 23:50. doi: 10.1186/s12936-024-04872-8
Singh, M. P., Saha, K. B., Chand, S. K., and Anvikar, A. (2017). Factors associated with treatment seeking for malaria in Madhya Pradesh, India. Trop. Med. Int. Health 22, 1377–1384. doi: 10.1111/tmi.12973
Sivanandan, A., Kumar, S. G., and Krishnamoorthy, Y. (2020). Awareness and preference in utilizing primary health-care services from rural health center as first point-of-care: a community-based cross-sectional study in South India. J. Educ. Health Promot. 9:85. doi: 10.4103/jehp.jehp_593_19
Ssemata, A. S., Nakitende, J. A., Kizito, S., Whipple, E. C., Bangirana, P., Nakasujja, N., et al. (2020). Associations of childhood exposure to malaria with cognition and behaviour outcomes: a systematic review protocol. Syst. Rev. 9:174. doi: 10.1186/s13643-020-01434-2
Suh, P. F., Elanga-Ndille, E., Tchouakui, M., Sandeu, M. M., Tagne, D., Wondji, C., et al. (2023). Impact of insecticide resistance on malaria vector competence: a literature review. Malar. J. 22:19. doi: 10.1186/s12936-023-04444-2
Tapajós, R., Castro, D., Melo, G., Balogun, S., James, M., Pessoa, R., et al. (2019). Malaria impact on cognitive function of children in a peri-urban community in the Brazilian Amazon. Malar. J. 18:173. doi: 10.1186/s12936-019-2802-2
Tripathy, R., Parida, S., Das, L., Mishra, D. P., Tripathy, D., Das, M. C., et al. (2007). Clinical manifestations and predictors of severe malaria in Indian children. Pediatrics 120, e454–e460. doi: 10.1542/peds.2006-3171
Trivedi, S., and Chakravarty, A. (2022). Neurological complications of malaria. Curr. Neurol. Neurosci. Rep. 22, 499–513. doi: 10.1007/s11910-022-01214-6
Tunon-Ortiz, A., and Lamb, T. J. (2019). Blood brain barrier disruption in cerebral malaria: beyond endothelial cell activation. PLoS Pathog. 15:e1007786. doi: 10.1371/journal.ppat.1007786
Varo, R., Chaccour, C., and Bassa, Q. (2020). Update on malaria. Medicina Clínica 55, 395–402. doi: 10.1016/j.medcle.2020.05.024
Velagapudi, R., Kosoko, A. M., and Olajide, O. A. (2019). Induction of Neuroinflammation and neurotoxicity by synthetic Hemozoin. Cell. Mol. Neurobiol. 39, 1187–1200. doi: 10.1007/s10571-019-00713-4
Vitor-Silva, S., Reyes-Lecca, R. C., Pinheiro, T. R., and Lacerda, M. V. (2009). Malaria is associated with poor school performance in an endemic area of the Brazilian Amazon. Malar. J. 8, 1–7.
Volpe, M., and Battistoni, A. (2019). An evolutionary rebus: the complex link between malaria and hypertension. J. Hypertens. 37, 1344–1346. doi: 10.1097/HJH.0000000000002090
Weckman, A. M., Conroy, A. L., Madanitsa, M., Gnaneswaran, B., McDonald, C. R., Kalilani-Phiri, L., et al. (2021). Neurocognitive outcomes in Malawian children exposed to malaria during pregnancy: an observational birth cohort study. PLoS Med. 18:e1003701. doi: 10.1371/journal.pmed.1003701
Westby, C. L., Erlandsen, A. R., Nilsen, S. A., Visted, E., and Thimm, J. C. (2021). Depression, anxiety, PTSD, and OCD after stillbirth: a systematic review. BMC Pregnancy Childbirth 21:782. doi: 10.1186/s12884-021-04254-x
Wicht, K. J., Mok, S., and Fidock, D. A. (2020). Molecular mechanisms of drug resistance in plasmodium falciparum malaria. Ann. Rev. Microbiol. 74, 431–454. doi: 10.1146/annurev-micro-020518-115546
World Health Organization. Mental health [internet]. (2024). Available at: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response.
World Health Organization. World malaria report 2023 [Internet]. (2024). Available at: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2023.
World Health Organization. World Malaria Report 2021 [Internet] (2024). Available at: https://www.who.int/publications-detail-redirect/9789240040496.
Keywords: malaria, malaria morbidity, mental health, cerebral malaria, cognitive impairment, neurological impairment, neurocognition
Citation: Nandish P, B. M. S, N. SN, Shankar G, Tripathi PK, Kashyap H, Jain A, Anvikar A and Chalageri VH (2024) Exploring the hidden mental health consequences of malaria beyond the fever. Front. Hum. Neurosci. 18:1432441. doi: 10.3389/fnhum.2024.1432441
Received: 14 May 2024; Accepted: 25 June 2024;
Published: 18 July 2024.
Edited by:
Prakashbabu Phanithi, University of Hyderabad, IndiaReviewed by:
Roseline Ekanem Duke, University of Calabar, NigeriaCopyright © 2024 Nandish, B. M., N., Shankar, Tripathi, Kashyap, Jain, Anvikar and Chalageri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shrinivasa B. M., ZHJzYm0xOTgzQGdtYWlsLmNvbQ==; Vani H. Chalageri, ZHJ2YW5paGMyMDIxQGdtYWlsLmNvbQ==
†Senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.