- 1Headache Group, School of Neuroscience, Wolfson Centre for Age-Related Diseases, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, United Kingdom
- 2NIHR King’s Clinical Research Facility, King’s College London, London, United Kingdom
- 3Department of Neurology, University of California, Los Angeles, Los Angeles, CA, United States
Objective: To provide an up-to-date narrative literature review of imaging in migraine with typical aura, as a means to understand better migraine subtypes and aura biology.
Background: Characterizing subtypes of migraine with typical aura and appreciating possible biological differences between migraine with and without aura, are important to understanding the neurobiology of aura and trying to advance personalized therapeutics in this area through imaging biomarkers. One means of doing this over recent years has been the use of increasingly advanced neuroimaging techniques.
Methods: We conducted a literature review of neuroimaging studies in migraine with aura, using a PubMed search for terms ‘imaging migraine’, ‘aura imaging’, ‘migraine with aura imaging’, ‘migraine functional imaging’ and ‘migraine structural imaging’. We collated the findings of the main studies, excluding small case reports and series with n < 6, and have summarized these and their implications for better understanding of aura mechanisms.
Results: Aura is likely mediated by widespread brain dysfunction in areas involving, but not limited to, visual cortex, somatosensory and insular cortex, and thalamus. Higher brain excitability in response to sensory stimulation and altered resting-state functional connectivity in migraine sufferers with aura could have a genetic component. Pure visual aura compared to visual aura with other sensory or speech symptoms as well, may involve different functional reorganization of brain networks and additional mitochondrial dysfunction mediating more aura symptoms.
Conclusion: There is a suggestion of at least some distinct neurobiological differences between migraine with and without aura, despite the shared phenotypic similarity in headache and other migraine-associated symptoms. It is clear from the vast majority of aura phenotypes being visual that there is a particular predisposition of the occipital cortex to aura mechanisms. Why this is the case, along with the relationships between cortical spreading depression and headache, and the reasons why aura does not consistently present in affected individuals, are all important research questions for the future.
Introduction
Whilst animal model and other experimental laboratory techniques have been valuable in studying migraine mechanisms, studying the multiple facets of the human disorder in humans is necessary to truly understand migraine and its related disability. The clinical phenotype of migraine in adults and in children and adolescents has evolved over time, and the International Classification of Headache Disorders (ICHD) has advanced with its different iterations to reflect this (Headache Classification Committee of the International Headache Society, 1988; Headache Classification Subcommittee of the International Headache Society, 2004; Headache Classification Committee of the International Headache Society [IHS], 2013, 2018).
Migraine aura is defined as ‘recurrent unilateral visual, sensory or other central nervous system symptoms lasting minutes, that usually develop gradually and are usually followed by headache and associated migraine symptoms’ (Headache Classification Committee of the International Headache Society [IHS], 2018). As well as aura as an accompanying symptom to headache in migraine, it is important to acknowledge other non-painful manifestations of the attack as part of the clinical phenotype, distinct from aura. The current version of the classification (ICHD3) (Headache Classification Committee of the International Headache Society [IHS], 2018) contains reference to premonitory symptoms (PS) which start ahead of pain and are clinically heterogenous, as well as vestibular migraine, in which vertigo is a prominent feature. Several childhood syndromes and symptoms may be early markers of migraine, and suggest that the disorder can manifest in different ways at different stages of brain and biological development (Gelfand, 2015). There is increasing evidence for the presence of cranial autonomic symptoms (CAS) in migraine as well as in the trigeminal autonomic cephalalgias (TAC’s) (in which these symptoms are canonical), and additional symptoms are being recognized as CAS (Gupta and Bhatia, 2007; Lai et al., 2009; Gelfand et al., 2013; Guven et al., 2013; Raieli et al., 2015; Shin et al., 2015; Barbanti et al., 2016; Riesco et al., 2016; Danno et al., 2020; Karsan et al., 2022). It has not been possible within ICHD3 to subtype every different manifestation of migraine, rather to acknowledge that some symptoms like PS and CAS can occur in addition to the so-called canonical migraine symptoms; movement sensitivity, photophobia, phonophobia and nausea or vomiting (Headache Classification Committee of the International Headache Society [IHS], 2018).
The main subtypes of migraine identified within the classification are migraine with (1.2) and without (1.1) aura (Headache Classification Committee of the International Headache Society [IHS], 2018). Migraine with typical aura (1.2.1) is the focus of this review, and is a type of migraine with aura, involving visual, sensory or speech symptoms without motor weakness (Headache Classification Committee of the International Headache Society [IHS], 2018). Aura when present is most commonly visual in phenotype (Viana et al., 2017). Whilst ICHD3 claims the aura duration should be less than an hour in typical aura, and occur preceding or associated with headache, it is clear in clinical practice, aura more prolonged than an hour can be reported by patients (Viana et al., 2018), and that aura can occur at any time during the course of the migraine attack (Viana et al., 2016). It can also be persistent (although perhaps for less than a week), particularly in chronic migraine (Schankin et al., 2017). Persistent aura without infarction lasting over a week is defined separately in ICHD3 (1.4.2), as is typical aura without headache (1.2.1.2) (Headache Classification Committee of the International Headache Society [IHS], 2018). Typical aura in ICHD3 does not include hemiplegic or brainstem aura and these aura subtypes will therefore not be discussed in this review.
Aura attacks in migraine present in around a third of sufferers and clinically most often present initially as visual disturbances (Russell and Olesen, 1996). These disturbances can take a variety of forms and severities, including flashes of light, zig zag lines and loss of visual field (positive or negative symptoms). In a subgroup of patients, sensory (typically paraesthesiae) or language (paraphasia or aphasia) disturbances can either co-exist with visual aura or occur in isolation. These are likely mediated by the consecutive and successive involvement of different cortical areas beyond the occipital cortex in some individuals. The visual, sensory and speech symptoms in the typical migraine with aura subtype are thought to be mediated cortically, by involvement of the relevant part of the cerebral cortex. It is thought that the neurophysiological correlate of aura is a wave of spreading depolarization and subsequent repolarization called cortical spreading depression (CSD), first described by Leao (1944) in the rabbit cortex. Given this is a neurophysiological phenomenon, it has been largely observed in animal models rather than in the human disease, but increasing imaging evidence in humans has contributed to this being a feasible mechanism in aura (Olesen et al., 1981; Lauritzen et al., 1982, 1983; Lauritzen and Olesen, 1984; Cao et al., 1999; Hadjikhani et al., 2001), although ictal electroencephalography (EEG) studies in humans are lacking (Ogunyemi, 1995). A contributor to the clinical and biological heterogeneity of migraine is that different aura symptoms can co-exist in the same individual and can occur together simultaneously or in quick succession during the same attack (Viana et al., 2016). What mediates this propensity to aura in some individuals and why the occipital cortex is most likely to be involved in this phenomenon are areas that remain poorly understood.
There is no consensus about the relationship, or lack thereof, between CSD and trigeminal nociception (Borgdorff, 2018). Given the high frequency of aura and complexity of aura phenotypes in the monogenic genetic forms of migraine (Tolner et al., 2015), there is likely to be a strong genetic basis to the propensity to aura, although in most cases this cannot be attributed to a single gene. Aura can occur in the absence of headache and can also occur in different conditions. Most migraine with aura sufferers will experience more attacks of migraine without aura than with aura and the majority of migraine sufferers have similar headache and other associated symptom phenotypes whether they experience aura or not. These issues raise important questions as to whether CSD and migraine headache are directly related or are separate mechanisms entirely. Understanding this clinical and biological heterogeneity in migraine is vital to developing disease biomarkers and therapeutics, in an area where despite the current evolution of novel treatment options for migraine, there remains limited evidence for efficacy differences of migraine treatments between different migraine subtypes, and indeed a scarcity of treatments available for those in whom the aura itself is particularly problematic, due to severity, frequency, duration or persistence, thus leaving an underserved population of patients.
Many insights into understanding aura mechanisms have come from animal models of CSD (Harriott et al., 2019) and interictal human neurophysiological studies (Coppola et al., 2019). In recent times, the development of functional neuroimaging methods and the ability to study the human migraine attack, at times ictally, and mostly interictally, and its symptoms phenotypically, have advanced our understanding of the neural substrates for migraine aura and alluded to therapeutic substrates that may be explored for aura treatment. There seems to be a predisposition to cortical excitability and sensory hypersensitivity in migraine with aura, which is enhanced when compared to migraine without aura (Demarquay and Mauguière, 2016). As visual aura is the most common aura subtype, even in those who may also have other aura symptoms, it has been the most frequently studied. Sensory and speech aura (as well as motor, hemiplegic and brainstem aura) have also been studied to a lesser extent. This review will summarize the current imaging literature in migraine with typical aura and the insights that these studies and imaging methodologies have provided into the neurobiology of aura and its subtypes.
Search strategy
This was not formulated to be a systematic review, more a summary of some key findings of imaging studies in this area. A search was conducted of the PubMed database between October and December 2022. The search terms were “migraine” AND “aura” AND (“neuroimaging” OR “neuro-imaging” OR “structural” OR “functional”). In addition, review articles and the reference lists of the included articles were also checked to identify potential omitted studies in the search. Case reports and case series with less than 6 subjects were excluded based on the vastness of the literature in this area. There is one exception to this, which is a landmark study by Hadjikhani et al. (2001), which managed to capture ictal aura and was the first to demonstrate real time alterations in the visual cortex, likely correlating with CSD mechanisms previously only demonstrated neurophysiologically in animal models.
Findings from the remaining studies were collated into the appropriate tables and text within this review.
Means of imaging aura
Clinical imaging
In the clinical setting, imaging with computerized tomography (CT) and magnetic resonance imaging (MRI) is usually performed if a patient presents with their first aura, change in aura phenotype or prolonged aura. Migraine aura is a common clinical stroke mimic, when presenting for the first time so it is standard to have urgent CT or MRI performed acutely in these situations. A non-contract CT of the head is expected to be normal in migraine with aura (Ridolfi et al., 2018), as are conventional MR sequences (Hougaard et al., 2017a).
Ictal or peri-ictal imaging
In the ictal or perictal phase, it is not uncommon for reversible transient diffusion restriction (Bereczki et al., 2008; Parks et al., 2014) to be observed during aura, and during a prolonged period of oligemia, migrainous infarction has also been reported (Serrano et al., 2018). Many of these ictal or peri-ictal studies are small, owing to the challenges in capturing spontaneous aura with imaging, and in triggering aura experimentally. Whilst prolonged oligemia can cause tissue infarction, one study has suggested that flow rates to involved brain tissue during migraine aura are higher than those when compared to stroke (Förster et al., 2014). Some case reports of reversible lesions of the corpus callosum in patients with migraine with typical aura exist (Lin and Yang, 2011; Lewis et al., 2020), with these lesions likely resulting from the high vulnerability of this area to non-specific cytotoxic damage. Such damage is felt to be likely mediated by glutamate, and callosal changes have also been demonstrated in migraine in general (Tantik Pak et al., 2022).
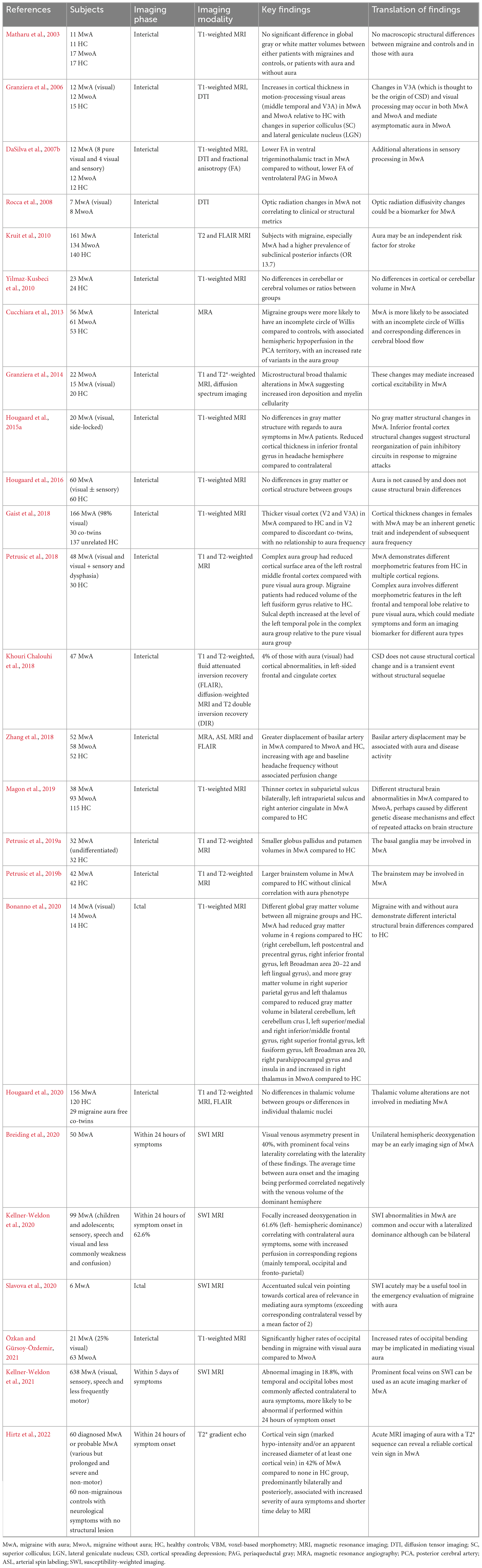
During CSD, neurovascular coupling is disturbed and the increase in tissue demand is accompanied by a reduction in arterial supply and therefore an increase in deoxygenated hemoglobin. This change can be exploited with susceptibility weighted MR imaging (SWI) or T2* gradient echo sequences on MRI, both of which are routinely available in many centers, in particular those managing hyperacute and acute stroke (Kellner-Weldon et al., 2021). These MR techniques can ictally show engorgement of veins, prominent focal veins (PFV), and this finding is more frequently documented less than 24 h from the onset of symptoms, with a possible increase in oxygen extraction in areas where the CSD wave has passed (Kellner-Weldon et al., 2021). Various studies over recent years have utilized this technique and postulated the possible acute clinical use in the emergency setting for differentiating migraine aura from other diagnostic mimics (Breiding et al., 2020; Kellner-Weldon et al., 2020, 2021; Slavova et al., 2020; Hirtz et al., 2022). The findings of these studies are included in Table 1.
Interictal imaging
A new structural technique which has been used, is that of assessing occipital bending on structural MR sequences in migraine with aura patients (Özkan and Gürsoy-Özdemir, 2021). This is a human anatomical asymmetrical variant in which one occipital pole crosses the midline and bends over the contralateral pole. This anatomical variant has been thought to be three times more common in those with certain psychiatric disorders including major depression (Maller et al., 2014), bipolar affective disorder (Maller et al., 2015) and schizophrenia (Maller et al., 2017). Given only one study to our knowledge has been conducted using this technique in migraine, further studies assessing the reliability of this sign are awaited and this is not a widely used clinical technique at the moment.
Abnormalities on MR angiography (MRA) sequences have also been described in migraine with aura; one study suggests that in an incomplete circle of Willis is more common in migraine than healthy controls, with an increased risk of variants in those with aura (Cucchiara et al., 2015), and another hypothesizing that lateral basilar artery displacement is a feature interictally in migraine with aura (Zhang et al., 2018). Whilst MRA is not routinely used to evaluate aura, it may be performed as part of a workup for possible stroke, and further systematic studies looking into possible interictal arterial changes in aura are warranted. The two available studies do suggest that there may be alterations to posterior circulation vasculature in migraine with aura with one of these studies suggesting associated perfusion changes (Cucchiara et al., 2015) and one not (Zhang et al., 2018).
Structural imaging
Volumetric and cortical thickness changes
Advanced macro and microstructural imaging techniques, such as voxel-based morphometry (VBM) and diffusion tensor imaging (DTI), have allowed detailed comparison of interictal brain structure between migraine with and without aura and comparison to healthy controls. Increased cortical thickness in the V3A area of visual cortex has been demonstrated in both migraine with and without aura, suggesting that extrastriate visual areas are implicated in both migraine subtypes, irrespective of aura symptoms being present or not (Granziera et al., 2006). This study postulated that asymptomatic or silent CSD could be a phenomenon in those with migraine without aura clinically.
Further studies have confirmed findings of increased cortical thickness in visual cortical areas in migraine with aura compared to healthy controls and co-twins without aura (Gaist et al., 2018). Other studies have demonstrated differences in cortical thickness in areas outside of visual cortex in subjects with migraine (with and without aura) compared to healthy controls, involving somatosensory cortex (DaSilva et al., 2007a,b), executive and visual cortical areas (Messina et al., 2013) and inferior frontal gyrus (Hougaard et al., 2015a). Whilst it is perhaps unsurprising that brain areas that could feasibly be mediating additional aura symptoms and those that are involved in other pain processing and modulation may be involved in migraine with aura, it is difficult to know if such changes are the result of the condition or are a predisposition to the condition. There have been some inconsistences between studies, with some studies failing to replicate structural findings and instead demonstrating no macrostructural differences between migraine with and without aura and when compared to healthy controls (Datta et al., 2011; Hougaard et al., 2016). Given the variability in findings in these studies in migraine with aura, and similar findings in other studies between migraine with and without aura, it is difficult to conclude whether there are fundamental gray matter structural differences between migraine with and without aura and compared to healthy controls. A meta-analysis also failed to provide consistency of findings for gray matter volume differences in migraine compared to controls in studies using VBM (although migraine with aura was not sub-analyzed) (Mehnert et al., 2020). Nine studies using either VBM or DTI were examined in a meta-analysis by Bashir et al. (2013), and the authors found that five studies reported reductions in gray matter volume associated with increasing attack frequency and disease duration. One study reported increased periaqueductal gray and dorsolateral pons volume in migraine with aura compared to migraine without aura, and these findings have also been supported by another study (Petrusic et al., 2019b).
A study by Hougaard et al. (2015a) studied the laterality of structural gray matter changes and compared cortical thickness in 20 subjects with side-locked visual aura with their migraine attacks. The authors demonstrated no gray matter structural changes but reduced inferior frontal gryus cortical thickness on the headache hemisphere compared to the contralateral hemisphere and suggested that alterations in frontal cortex structure are a result of repeated migraine attacks altering pain modulation circuits. Hougaard et al. (2016) also demonstrated that whilst gray matter volume in the anterior cingulate was reduced in migraine with aura relative to controls, there was no difference in gray matter volume or cortical thickness in those with and without sensory aura. A further study by Petrusic et al. (2018) found differences in brain structure when comparing pure visual aura to visual aura with sensory and dysphasic symptoms and suggested that the additional findings in this group could serve as an imaging biomarker for distinguishing aura subtypes.
Other studies have specifically examined subcortical nuclei volumes between migraine with and without aura and compared to healthy controls, again with conflicting results. One study demonstrated broad thalamic structure alterations in migraine with aura (Granziera et al., 2014), and another failed to replicate these findings (Hougaard et al., 2020). Another study suggested other deep brain nuclei differences in the putamen and globus pallidus in migraine with aura (Petrusic et al., 2019a), with reduced volumes but larger brainstem volumes in migraine with aura compared to healthy controls (Petrusic et al., 2019b), suggesting that deep subcortical brain nuclei and brainstem structures may be altered in migraine with aura. The influence of disease activity, that is underlying headache frequency and disease duration, on structural imaging findings in migraine is unclear as various studies have reported conflicting findings (Sheng et al., 2020, 2021).
A meta-analysis of VBM studies in migraine published recently suggested a range of findings in migraine in general compared to healthy controls, with areas involved in sensory, cognitive, pain and affective processing being implicated. Their pooled analysis of migraine subtypes suggested distinct patterns of gray matter volume change between migraine with aura (more occipital and temporal involvement) and migraine without aura (Zhang et al., 2023).
White matter hyperintensities
White matter disease has also been evaluated in migraine given early observations of an increase in white matter disease burden on brain imaging in patients with migraine (Igarashi et al., 1991). These observations led to a large population-based study called the CAMERA study, which evaluated large groups of migraine with and without aura and healthy controls and compared baseline interictal MR brain imaging between the groups (Kruit et al., 2004). The study demonstrated that women with migraine are more likely to have supratentorial white matter hyperintensities, with the number correlating with baseline attack frequency. A sub-analysis demonstrated that this was more common in those with migraine with aura, particularly in the posterior circulation (Kruit et al., 2010). A subsequent 9-year follow up study (CAMERA 2) showed no other progressive structural brain changes and no cognitive impact of the white matter hyperintensities (Palm-Meinders et al., 2012). A subsequent meta-analysis of 19 studies has confirmed the suggestion of an increased risk of white matter hyperintensities in migraine compared to healthy controls, with a particular risk in those with aura, without an association in this group with silent brain infarcts (Bashir et al., 2013).
The mechanisms behind these white matter changes are unknown but have been hypothesized as being related to cerebral blood flow changes (Kruit et al., 2010; Zhang et al., 2017), arterial narrowing (Kruit et al., 2005), as well as the presence of a patent foramen ovale (PFO) (Yeo et al., 2022) and blood brain barrier disruption (Albrecht et al., 2019), among others. As the majority of patients with migraine with aura do not have a PFO (although it is 2-3 times more common in migraine without aura compared to the normal population (Caputi et al., 2009; Liu et al., 2020), and other imaging studies have suggested an intact blood brain barrier during attacks of migraine with (Hougaard et al., 2017a) and without aura (Amin et al., 2017), the presence of these lesions is likely to be multifactorial. In particular, age and cardiovascular risk factors are likely to play a role, and these have not been evaluated in subgroup analyses of the population data from CAMERA (Kruit et al., 2005).
Whilst the studies discussed have yielded conflicting results (Masson et al., 2021), it is possible that fundamental structural differences in migraine with aura involving areas like visual and extrastriate cortex, are likely mediating the disease process and clinical phenotypes. These may be caused by an underlying genetic predisposition to migraine with aura differentially affecting these brain regions, rather than being influenced by underlying attack frequency or disease activity. Interestingly, there does not seem to be a clinical correlation between structural brain areas involved and clinical aura phenotypes. It is clear that on a population level, younger women with migraine with aura are more likely to have white matter hyperintensities on structural brain imaging which are largely posterior and supratentorial, correlating with baseline attack frequency and disease duration, and not associated with progressive cognitive impairment at follow up.
Some of the main structural brain imaging studies evaluating migraine with aura are summarized in Table 1.
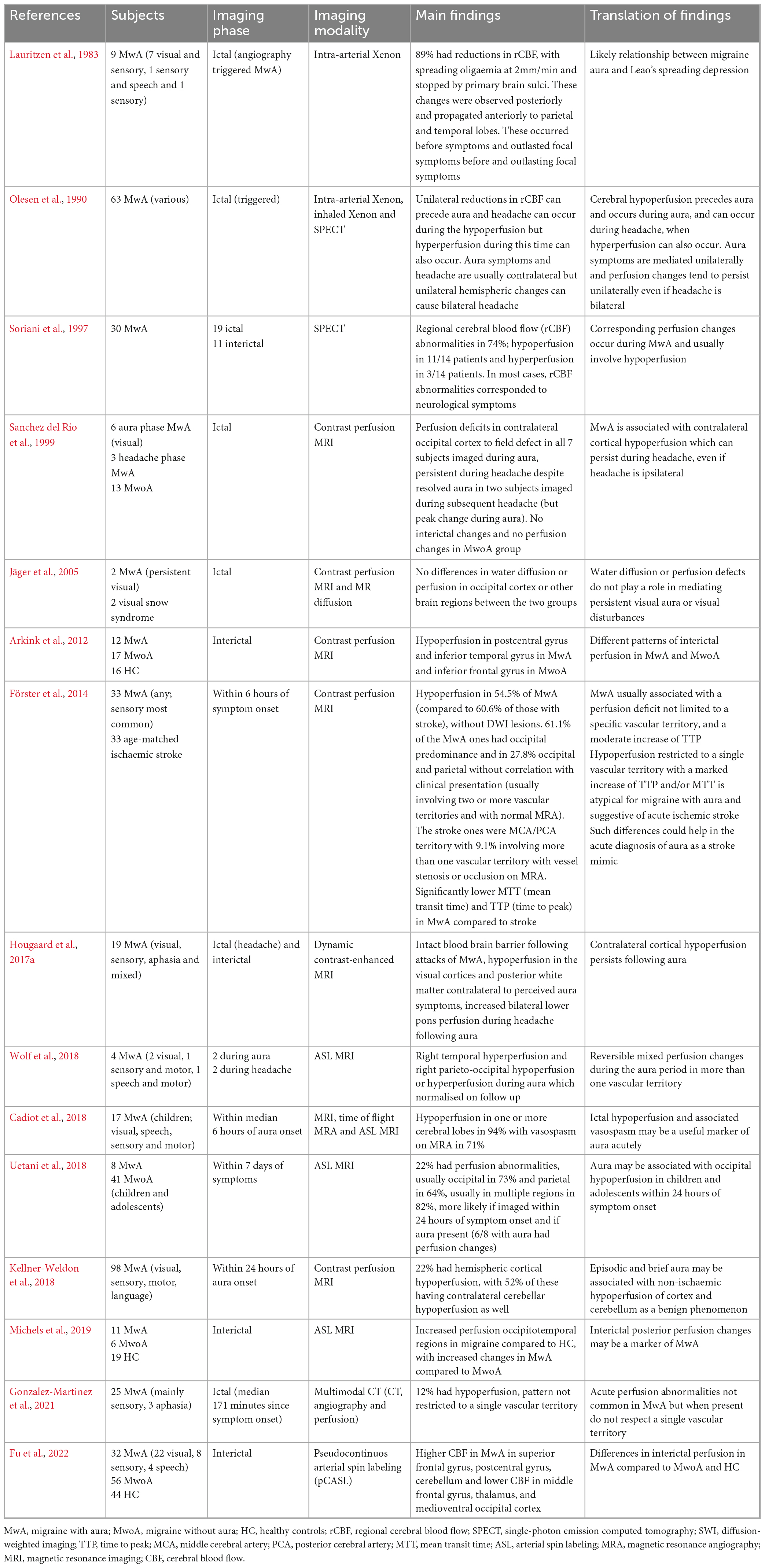
Perfusion studies
Several perfusion imaging modalities have been used for research purposes to evaluate migraine with aura. Most are not available for wide scale clinical use. This is an obvious choice of imaging methodology in aura, given the vascular and perfusion changes likely to occur with CSD and alterations in neurovascular coupling, which can be exploited using perfusion imaging methods. The potential utility of such techniques if available in clinical settings for differentiating migraine aura from stroke, is also attractive. These techniques have included historical intra-arterial Xenon and have evolved to include single photon emission computed tomography (SPECT) and advanced forms of perfusion MRI.
Ictal or peri-ictal imaging
Initial intra-arterial Xenon techniques used by Lauritzen et al. (1983), Olesen et al. (1990) were the first to show objective alterations in regional cerebral blood flow (rCBF) in migraine aura during triggered attacks occurring posteriorly, and propagating at a rate compatible with CSD. These studies provided evidence for CSD likely mediating aura in human subjects. Since then, more advanced non-invasive MR options have become available as a means of assessing cerebral perfusion without the need for ionizing radiation and contrast material. MR perfusion-weighted imaging or arterial spin labeling (ASL) (Sanchez del Rio et al., 1999; Jäger et al., 2005; Arkink et al., 2012; Förster et al., 2014; Cadiot et al., 2018; Kellner-Weldon et al., 2018; Uetani et al., 2018; Wolf et al., 2018; Michels et al., 2019; Fu et al., 2022), or indeed CT perfusion techniques (Gonzalez-Martinez et al., 2021) (this may be more likely to be available clinically), may show transient regional cerebral perfusion changes in aura, reflecting the hemodynamic variations occurring. Typically, such changes affect more than one vascular territory, can be bilateral, and tend to predominate posteriorly, but a variety of ictal and interictal perfusion changes have been demonstrated in migraine with aura using different imaging modalities and are summarized in Table 2.
In general, it seems that cerebral hypoperfusion in one or more vascular territories occurs mainly unilaterally early during aura in the ictal phase and persists throughout the duration of the aura and sometimes as headache starts, before hyperperfusion occurs. Headache can occur from the same hemisphere as the one mediating aura, even if headache is bilateral, suggesting that bihemispheric brain involvement is not needed for the perception of bilateral head pain. These perfusion changes are thought to be the imaging correlate for CSD in these subjects, as the affected brain region with perfusion change tends to correlate in terms of both laterality and anatomical location with the clinical aura phenotype. The hypoperfusion may be associated with radiological vasospasm on imaging. Imaging as close as possible to the time of onset of aura symptoms tends to yield the most positive results. The pattern of ictal perfusion change can help distinguish aura from stroke in terms of number of vascular territories involved, and ictal abnormalities on MRA can occur in migraine aura [vasoconstriction (Förster et al., 2014; Cadiot et al., 2018) or mild dilation (Förster et al., 2014)].
Interictal imaging
Interictal perfusion differences may exist between migraine with and without aura and involve a combination of hypo and hyperperfusion of different brain regions. These are also summarised in Table 2.
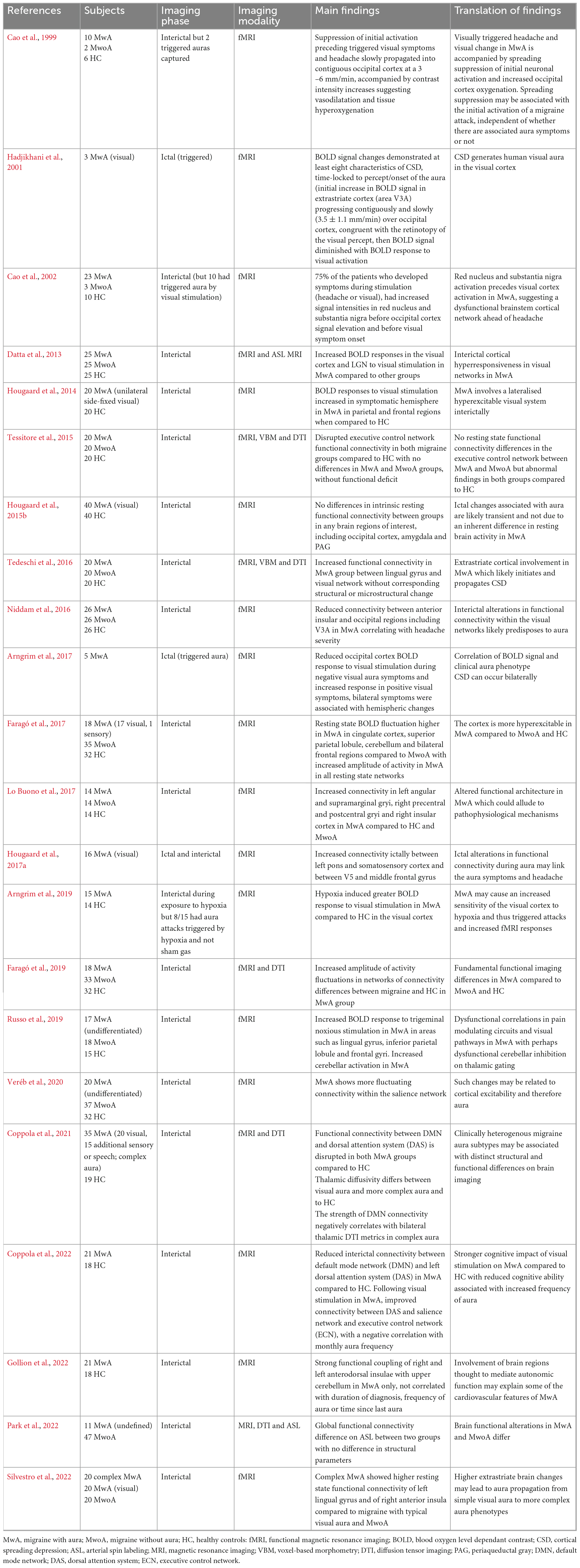
Functional imaging
Functional imaging studies have provided contributory evidence to the perfusion literature and have suggested ictal and interictal alterations in functional connectivity within visual and extrastriate cortex (Cao et al., 1999, 2002; Datta et al., 2013; Hougaard et al., 2014; Niddam et al., 2016; Tedeschi et al., 2016; Arngrim et al., 2017, 2019; Russo et al., 2019; Silvestro et al., 2022), as well as in other areas such as limbic regions (Faragó et al., 2017), and sensory (Hougaard et al., 2017b) and executive cortical areas (Coppola et al., 2022), amongst other alterations in migraine with aura. These studies are summarized in Table 3.
Ictal or peri-ictal studies
A key functional MRI (fMRI) study managed to image exertion-provoked migraine visual aura and the interictal period using an on/off visual stimulation paradigm. This study demonstrated fMRI signal in the occipital cortex (starting in V3a), correlating with the time of onset of the visual aura and the propagation correlating with the retinotopy of the visual percept (Hadjikhani et al., 2001). There was also a suggestion on the blood oxygen level dependent contrast (BOLD) of vasodilation followed by vasoconstriction, akin to that observed in CSD. This study for the first time used fMRI to visualize the aura itself, as well as the interictal phase in 3 subjects, and provided supportive imaging evidence for CSD mediating visual aura in the occipital cortex in this subject, and the propagation of this correlating with clinical symptoms. Similar findings had been previously observed using fMRI by Cao et al. (1999), with two captured auras (Cao et al., 1999).
Arngrim et al. (2017) were able to demonstrate differences in BOLD response over the visual cortex between positive and negative aura symptoms, suggesting a correlation between BOLD signal and clinical aura phenotype, and also suggested that occipital changes could occur bilaterally in bilateral aura. Hougaard et al. (2017a) imaged 16 migraine with visual aura ictally and demonstrated increased ictal connectivity between the left pons and somatosensory cortex, as well as between V5 and the middle frontal gyrus, providing possible links between brain areas involved in aura and those involved in headache. A further study by Arngrim et al. (2019) managed to capture 8 triggered aura attacks (using interictal exposure to hypoxia or sham gas) and image these with fMRI. The authors showed that hypoxia induced a larger BOLD response in the visual cortex of migraine with aura subjects compared to healthy controls in response to visual stimulation, and stipulated that migraine with aura may involve an inherent susceptibility of the visual cortex to hypoxia, triggered attacks and subsequent fMRI responses (Arngrim et al., 2019).
Interictal studies
A few studies have managed to use imaging to differentiate changes associated with different aura subtypes (pure visual aura compared to visual plus sensory or speech aura symptoms) (Coppola et al., 2018; Silvestro et al., 2022), and one has tried to distinguish positive and negative visual aura symptoms and correlate these with the BOLD response over the visual cortex (Arngrim et al., 2017). Coppola et al. (2021) suggested different degrees of altered thalamocortical cortical connectivity (thalamus and default mode network (DMN)) in migraine with visual aura compared to more complex aura (both being different to healthy controls interictally) and Silvestro et al. (2022) suggested that the insula is more involved in complex aura and is perhaps a cortical area of CSD propagation following visual cortex involvement. The insula region has also been suggested as being involved in mediating some of the cardiovascular autonomic features of migraine with aura (Gollion et al., 2022). Only one study has failed to demonstrate any interictal connectivity differences between migraine with aura and healthy controls in areas of interest including the occipital cortex (Hougaard et al., 2015b), however this study was a resting state study which did not involve any stimulation within the imaging paradigm. It is feasible that the abnormalities in brain function in migraine with aura are due to inherent network differences and/or altered neuronal excitability to sensory stimulation.
The use of these functional imaging techniques with different stimulation paradigms has in general suggested ictal and interictal differences between migraine with and without aura and healthy controls in brain function, and unsurprisingly changes involving areas like visual and somatosensory cortices. Additional cortical, thalamic and insular involvement suggests that aura involves or causes more widespread brain dysfunction in areas involved in sensory, executive and limbic processing. The differences in imaging methodologies and acquisition parameters, paradigms, subject selection, image processing and analyses make the reproducibility of fMRI studies a challenge in any field. The clinical heterogeneity of migraine contributes to the variance in imaging data and difficulties with producing consistent findings. There is however suggestion of alterations in ictal and interictal brain function in key cortical and subcortical regions in migraine with aura. Use of more advanced imaging methodologies and paradigms may enable further characterization of different aura types with such imaging, as a means to producing ictal and interictal biomarkers for different aura subtypes.
Other imaging modalities
In addition to perfusion and fMRI approaches, the use of other imaging methodologies has been increasing in migraine research as availability and expertise has advanced in the field. These have included MR spectroscopy (MRS), magnetoencephalography (MEG) and combination approaches using positron emission tomography (PET) and MR together.
Ligand-based PET and MR approaches interictally have suggested glial activation in patients with migraine and recent aura attacks in the visual cortex and Broca’s area. Changes have also been reported in somatosensory cortex and thalamus, and frontal and orbitofrontal cortex, with a positive association between the signal strength and baseline aura frequency (Albrecht et al., 2019). Occipital meningeal and bone involvement (Hadjikhani et al., 2020) has been observed, with suggestions of possible links between CSD and trigeminal pain. These studies have again suggested wider cortical involvement beyond the visual cortex and involvement of the thalamus in aura mechanisms. The role for the meninges and the possibility of an altered blood brain barrier in migraine with (Hougaard et al., 2017a; Hadjikhani et al., 2020) and without aura (Amin et al., 2017) has been disputed between different studies.
Spectroscopy studies have suggested a possible contribution of mitochondrial dysfunction in migraine, possibly secondary to the brain cortical excitability change as a mechanism of predisposition to CSD (Barbiroli et al., 1992; Sarchielli et al., 2005; Sándor et al., 2005; Arngrim et al., 2016; Zielman et al., 2017). Whilst the studies have produced heterogeneous findings, it has been postulated that identified energy disturbances may be related to the clinical phenotype, and alterations have more frequently been demonstrated in migraine with aura patients compared to those without aura (Sarchielli et al., 2005; Sándor et al., 2005). In migraine with aura, an elevated lactate peak is present before and after visual stimulation in migraine with visual aura, but only peaks during visual stimulation in more complex aura, suggesting that pure visual aura may involve more lactate transporter system dysfunction compared to other aura subtypes (Sándor et al., 2005). During photic stimulation in patients with migraine with aura, the decrease in N-acetylaspartate (NAA), as a marker of mitochondrial dysfunction, suggests a less efficient mitochondrial functioning state in these patients (Sarchielli et al., 2005). Increased glutamate levels in the visual cortex interictally have also been demonstrated in migraine with aura patients (Zielman et al., 2017), and an abnormal reduction of response from the occipital cortex to interventions that change cortical excitability (transcranial direct current stimulation) has also been reported (Siniatchkin et al., 2012).
These advanced imaging modalities have supported wider cortical involvement in aura beyond the visual cortex and raised the possibility of interictal altered mitochondrial function and increased cortical excitability (without a change in inhibitory mechanisms) in migraine with aura. Larger studies are required to evaluate these findings and their reproducibility and clinical translation more systematically in the future. Some of these studies are summarized in Table 4.
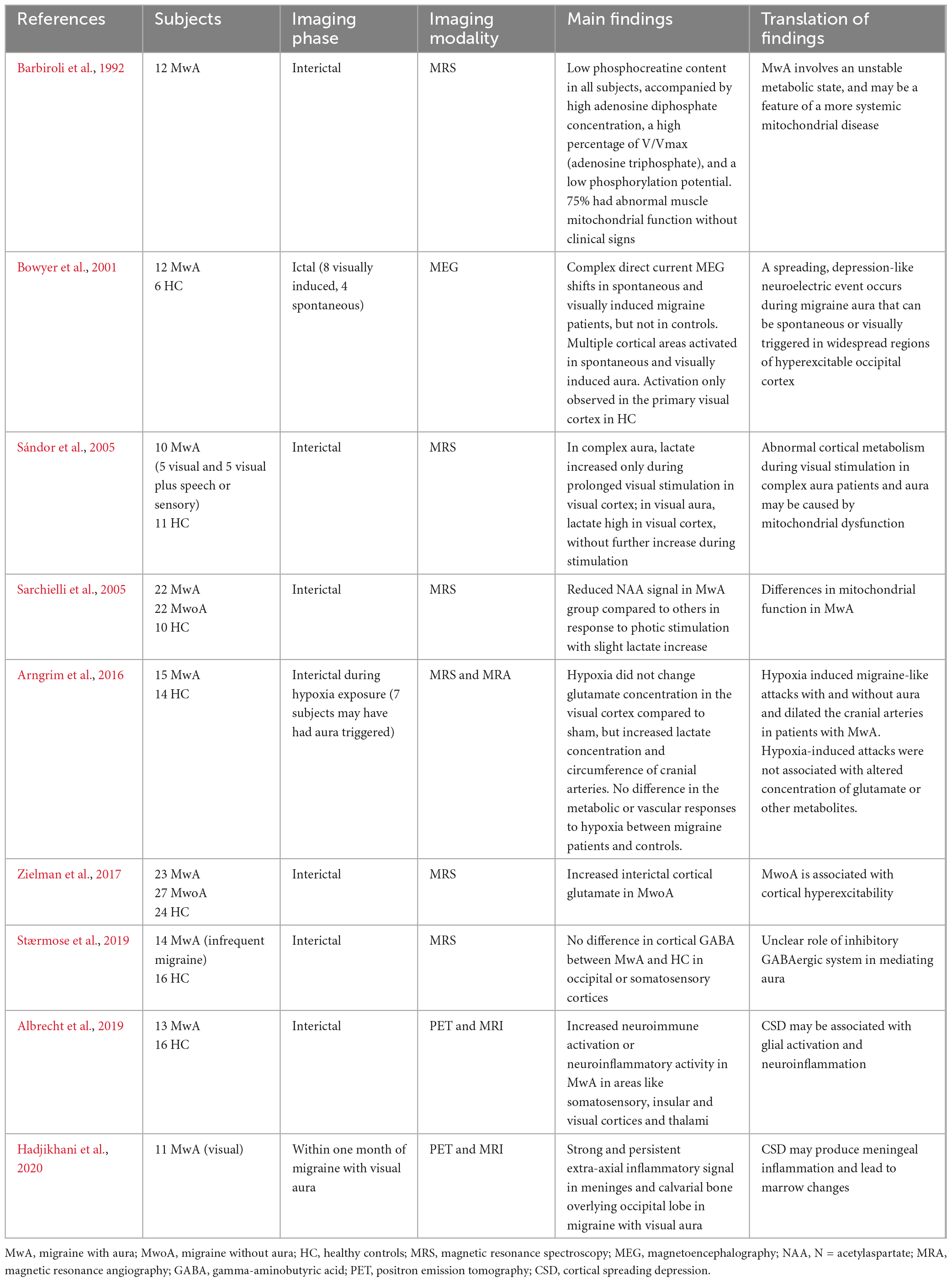
Table 4. A summary of studies using other advanced imaging techniques in migraine with typical aura.
Discussion
The use of increasingly advanced structural and functional imaging techniques has allowed the study of migraine in humans in ways that were not possible before. In particular, the ictal imaging of aura both clinically and using functional imaging methods, has provided a feasible imaging correlate for CSD mechanisms observed in preclinical models. The increasing use of perfusion-based imaging modalities in clinical practice, largely through stroke services, may provide a unique opportunity to capture aura ictally more frequently than we have been able to in the past, and provide a means of diagnostic differentiation, as well as potential mechanistic insights into aura mediation.
The imaging studies using different structural and functional imaging modalities have compared both migraine with and without aura to each other, and at times have evaluated migraine with aura alone or in comparison to healthy controls. Clearly, there are limitations to studies in which there is no comparison group, and in those that do not include a migraine without aura group. It can be difficult to make inferences about the biology of aura from such studies, but they can provide supportive evidence of differences between the migraine with aura brain in general, and in comparison to healthy controls.
Overall, the studies seem to suggest that aura is likely mediated by widespread brain dysfunction in areas involving, but not limited to, visual cortex, other cortical areas and thalamus, therefore suggesting altered cortical hyperexcitability and sensory sensitivity. The interictal predisposition to aura among sufferers, and differences in cortical excitability in response to sensory stimulation compared to healthy controls and migraine without aura, are a likely result of genetic influences and interictal alterations in resting brain structure and function. Pure visual aura and visual aura with other sensory or speech symptoms may involve different functional reorganization of brain networks and mitochondrial dysfunction.
The differences in study size, subject recruitment and screening, imaging modalities, scanner strength and analysis methods, are challenges in the study of any condition. In migraine, baseline headache frequency, disease duration, medication use, clinical heterogeneity, genetics and phase of the migraine cycle and comorbid psychological and psychiatric disorders, are just some of the additional factors that contribute to variance amongst imaging data sets. The definition of aura and which subjects are diagnosed with migraine with aura is another area which may not be as clear as one may think in clinical practice. The difficulties with studying aura ictally contribute to these challenges. The general lack of consistent ability to provoke aura in experimental settings, using natural trigger factors (Hougaard et al., 2013) and using pharmacological migraine provocation agents such as nitroglycerin (NTG) (Christiansen et al., 1999), calcitonin gene-related peptide (CGRP) (Hansen et al., 2008, 2010) and sildenafil (Butt et al., 2022), despite these being potent experimental triggers for migraine headache and other associated migraine symptoms, suggest that aura and headache mechanisms are perhaps distinct in migraine. The majority of imaging studies conducted to evaluate aura, or the differences between migraine with and without aura, have been performed interictally in the absence of symptoms.
The differences in baseline stroke risk, heritability of migraine, treatment response to acute and preventive migraine medication and possible changes in structural and functional imaging, support fundamental biological differences between migraine with and without aura (Hansen and Charles, 2019). The heterogeneity in aura phenotype, timing and duration between and within patients with migraine with aura (Viana et al., 2017) is also interesting and supports the theory that migraine is a heterogenous umbrella disorder, likely involving various neurobiological mechanisms, not all of which are unanimously implicated in all sufferers. Whilst migraine aura with visual components is the most common phenotype, the individuals that also experience speech and sensory symptoms may have different genetic and neurobiological mechanisms contributing to the additional aura phenotype. Such differences amongst migraineurs may also explain the differences in treatment efficacy amongst different migraine preventive medications in patients with migraine, where even with the newly emerged CGRP antibodies, a significant proportion of sufferers will not respond to therapy (Cullum et al., 2022). This disease and treatment-related heterogeneity is poorly understood and makes the individualization of therapy challenging for physicians. At present, owing to lack of systematic and large randomized clinical trials in this area, management options for migraine with and without aura are shared. Agents such as ketamine (Kaube et al., 2000; Afridi et al., 2013), aspirin (Anoaica et al., 2014; Turk et al., 2017), amiloride (Holland et al., 2012) and levetiracetam (Brighina et al., 2006) have been used in clinical case series or unblinded studies of aura with some suggestions of efficacy, but not enough evidence to support their wide scale clinical use. There is a suggestion that triptans are less useful acutely in migraine with aura attacks compared to those without aura (Hansen et al., 2015), and that single pulse transcranial magnetic stimulation is more useful in treating migraine with aura compared to migraine without aura (Lipton et al., 2010; Lan et al., 2017). Migraine preventive drugs tend to lower the threshold for CSD (and CSD has been used as a preclinical model to test drug efficacy) or lower the frequency of CSD’s, suggesting there may be a link between CSD and trigeminal nociception (Ayata et al., 2006), but it is important to remember that many traditionally used migraine drugs have broad mechanisms of action unspecific for migraine, so may alter CSD thresholds in ways unrelated to their anti-migraine effect. In clinical practice, the use of commonly used migraine preventives is rarely sufficient for the management of problematic aura symptoms in our experience.
There are several other questions and challenges that aura poses. The possible mediation of asymptomatic aura (although this would clearly not meet clinical criteria for an aura diagnosis) within the brain in some individuals, perhaps propagating in silent or less eloquent areas of cortex (Karsan et al., 2018; Hadjikhani and Vincent, 2021), how and why aura starts in visual cortex and can spread to other cortical areas, why some attacks are not associated with aura symptoms despite the presumed same cortical areas being involved across attacks, and the potential links between CSD and trigeminal nociception, are just some of these. Several associated migraine symptoms distinct from aura are also mediated via cerebral cortex and there is a lack of clinical or radiological means of differentiating these clinically and neurobiologically from aura. These include reversible alterations in speech (Schwedt et al., 2019) and cognition (Vincent and Hadjikhani, 2007), which can occur in the premonitory phase in the lead up to a migraine attack (Karsan and Goadsby, 2018), as can aura. In our practice, we would not usually classify transient non-specific visual blurring or non-aphasic or non-dysarthric speech symptoms associated with a migraine attack as typical aura symptoms, but more as premonitory or premonitory-like symptoms if occurring preceding or during pain respectively, or postdrome symptoms if occurring after headache resolution. This is largely because they are not necessarily localizable to one area of cortex, lack anatomical lateralisability do not necessarily spread in the same way other aura symptoms do, and could not be classified as ‘positive’. These are all characteristics ICHD3 defines as being consistent with aura and some of which have to be met to make the diagnosis (Headache Classification Committee of the International Headache Society [IHS], 2018). However, it is feasible that in some studies, these symptoms could be included in imaging studies, and the potential symptomatic differences between such symptoms and true aura is an area that should be explored in further iterations of the International Classification of Headache Disorders. As well as contributing to data variance in imaging studies, such symptoms may pose diagnostic and classification challenges for clinicians when occurring before or during headache and may prompt investigations for secondary causes. Systematic and classification-based distinction of these from aura, is in our opinion, an important area going forwards.
Conclusion
Migraine with aura is a complex heterogenous condition, likely mediated by widespread brain dysfunction ictally and interictally in areas involving but not limited to visual cortex, and also involving other cortical areas and thalamus. Neuroimaging, with increasingly advanced clinically available techniques being used largely due to advances in hyperacute stroke management, and novel and emerging research methodologies, have greatly contributed to our understanding of the neurobiological bases of migraine and migraine aura. However, differences in scanner strengths and imaging acquisition, imaging modalities, patient recruitment methods, sample sizes, aura diagnosis and analysis methods, among other issues make reproducibility of imaging findings across studies and centers challenging. Outside of the scope of this review, there have also been several case reports and case series reporting of imaging changes associated with aura. The brain changes discussed in this review in general suggest that there are distinct changes in migraine with aura compared to migraine without aura and healthy controls both ictally and interictally and allude to a state of cortical hyperexcitability and altered sensory processing in migraine with aura, likely mediated by a combination of structural and functional brain changes. These findings support neurophysiological literature in this area. The interictal predisposition to aura and differences in cortical excitability in response to sensory stimulation are probably a result of genetic influences and interictal alterations in resting brain structure and function. Pure visual aura and visual aura with other sensory or speech symptoms may involve different functional reorganization of brain networks and mitochondrial dysfunction. Larger more systematic population-based imaging studies with larger cohorts of subjects with different aura subgroup analyses are required to characterize these findings further and shed further light on the possible neurobiological differences in different aura presentations. Given the visual predominance in aura symptoms even in those that also develop other symptoms, a genetic basis to predisposition to occipital CSD via altered cortical excitability and perhaps mitochondrial mechanisms seem most likely, but the reasons that the majority of attacks do not involve aura, the links between CSD and trigeminal pain and how CSD propagates to different cortical areas from occipital cortex and why are questions that remain unanswered. Going forwards, developing provocation models of aura to allow ictal imaging, and advances in routine clinical imaging methodologies for the acute imaging of aura, will be key ways to develop such understandings and contribute to the development of imaging biomarkers for aura, increase the use of diagnostic imaging acutely, and allow personalization of migraine therapeutics. This is an area that all clinicians that treat migraine would find attractive, as despite many therapeutic advances in the field, prediction of treatment response and specific treatment of problematic and disabling aura are areas that need further work.
Author contributions
NK and ES wrote the manuscript following review of the literature. NK made the tables. PG was involved in senior review of the manuscript. All authors have reviewed the manuscript prior to final submission.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Afridi, S., Giffin, N., Kaube, H., and Goadsby, P. J. (2013). A randomized controlled trial of intranasal ketamine in migraine with prolonged aura. Neurology 80, 642–647. doi: 10.1212/WNL.0b013e3182824e66
Albrecht, D., Mainero, C., Ichijo, E., Ward, N., Granziera, C., Zürcher, N., et al. (2019). Imaging of neuroinflammation in migraine with aura: A [11C]PBR28 PET/MRI study. Neurology 92, e2038–e2050. doi: 10.1212/WNL.0000000000007371
Amin, F., Hougaard, A., Cramer, S., Christensen, C., Wolfram, F., Larsson, H., et al. (2017). Intact blood-brain barrier during spontaneous attacks of migraine without aura: A 3T DCE-MRI study. Eur. J. Neurol. 24, 1116–1124. doi: 10.1111/ene.13341
Anoaica, M., Anoaica, P., and Popescu, F. (2014). Acetylsalicylic acid in migraine with aura prevention—a retrospective study. Curr. Health Sci. J. 40, 126–128. doi: 10.12865/CHSJ.40.02.08
Arkink, E., Bleeker, E., Schmitz, N., Schoonman, G., Wu, O., Ferrari, M., et al. (2012). Cerebral perfusion changes in migraineurs: A voxelwise comparison of interictal dynamic susceptibility contrast MRI measurements. Cephalalgia 32, 279–288. doi: 10.1177/0333102411435985
Arngrim, N., Hougaard, A., Ahmadi, K., Vestergaard, M., Schytz, H., Amin, F., et al. (2017). Heterogenous migraine aura symptoms correlate with visual cortex functional magnetic resonance imaging responses. Ann. Neurol. 82, 925–939. doi: 10.1002/ana.25096
Arngrim, N., Hougaard, A., Schytz, H., Vestergaard, M., Britze, J., Amin, F., et al. (2019). Effect of hypoxia on BOLD fMRI response and total cerebral blood flow in migraine with aura patients. J. Cereb. Blood Flow Metab. 39, 680–689. doi: 10.1177/0271678X17719430
Arngrim, N., Schytz, H., Britze, J., Amin, F., Vestergaard, M., Hougaard, A., et al. (2016). Migraine induced by hypoxia: An MRI spectroscopy and angiography study. Brain 139, 723–737. doi: 10.1093/brain/awv359
Ayata, C., Jin, H., Kudo, C., Dalkara, T., and Moskowitz, M. (2006). Suppression of cortical spreading depression in migraine prophylaxis. Ann. Neurol. 59, 652–661. doi: 10.1002/ana.20778
Barbanti, P., Aurilia, C., Dall’Armi, V., Egeo, G., Fofi, L., and Bonassi, S. (2016). The phenotype of migraine with unilateral cranial autonomic symptoms documents increased peripheral and central trigeminal sensitization. A case series of 757 patients. Cephalalgia 36, 1334–1340. doi: 10.1177/0333102416630579
Barbiroli, B., Montagna, P., Cortelli, P., Funicello, R., Iotti, S., Monari, L., et al. (1992). Abnormal brain and muscle energy metabolism shown by 31P magnetic resonance spectroscopy in patients affected by migraine with aura. Neurology 42, 1209–1214. doi: 10.1212/wnl.42.6.1209
Bashir, A., Lipton, R., Ashina, S., and Ashina, M. (2013). Migraine and structural changes in the brain: A systematic review and meta-analysis. Neurology 81, 1260–1268. doi: 10.1212/WNL.0b013e3182a6cb32
Bereczki, D., Kollár, J., Kozák, N., Viszokay, K., Barta, Z., Sikula, J., et al. (2008). Cortical spreading edema in persistent visual migraine aura. Headache 48, 1226–1229. doi: 10.1111/j.1526-4610.2008.01183.x
Bonanno, L., Lo Buono, V., De Salvo, S., Ruvolo, C., Torre, V., Bramanti, P., et al. (2020). Brain morphologic abnormalities in migraine patients: An observational study. J. Headache Pain 21:39. doi: 10.1186/s10194-020-01109-2
Borgdorff, P. (2018). Arguments against the role of cortical spreading depression in migraine. Neurol. Res. 40, 173–181. doi: 10.1080/01616412.2018.1428406
Bowyer, S., Aurora, K., Moran, J., Tepley, N., and Welch, K. (2001). Magnetoencephalographic fields from patients with spontaneous and induced migraine aura. Ann. Neurol. 50, 582–587. doi: 10.1002/ana.1293
Breiding, P., Kellner-Weldon, F., Grunder, L., Scutelnic, A., Fischer, U., Meinel, T., et al. (2020). Quantification of cerebral veins in patients with acute migraine with aura: A fully automated quantification algorithm using susceptibility-weighted imaging. PLoS One 15:e0233992. doi: 10.1371/journal.pone.0233992
Brighina, F., Palermo, A., Aloisio, A., Francolini, M., Giglia, G., and Fierro, B. (2006). Levetiracetam in the prophylaxis of migraine with aura: A 6-month open-label study. Clin. Neuropharmacol. 29, 338–342. doi: 10.1097/01.WNF.0000236766.08409.03
Butt, J., S Eddelien, H., and Kruuse, C. (2022). The headache and aura-inducing effects of sildenafil in patients with migraine with aura. Cephalalgia 42, 984–992. doi: 10.1177/03331024221088998
Cadiot, D., Longuet, R., Bruneau, B., Treguier, C., Carsin-Vu, A., Corouge, I., et al. (2018). Magnetic resonance imaging in children presenting migraine with aura: Association of hypoperfusion detected by arterial spin labelling and vasospasm on MR angiography findings. Cephalalgia 38, 949–958. doi: 10.1177/0333102417723570
Cao, Y., Aurora, S., Nagesh, V., Patel, S., and Welch, K. (2002). Functional MRI-BOLD of brainstem structures during visually triggered migraine. Neurology 59, 72–78. doi: 10.1212/wnl.59.1.72
Cao, Y., Welch, K., Aurora, S., and Vikingstad, E. (1999). Functional MRI-BOLD of visually triggered headache in patients with migraine. Arch. Neurol. 56, 548–554. doi: 10.1001/archneur.56.5.548
Caputi, L., D’Amico, D., Usai, S., Grazzi, L., Parati, E., and Bussone, G. (2009). Prevalence and characteristics of right-to-left shunt in migraine with aura: A survey on 120 Italian patients. Neurol. Sci. 30(Suppl. 1), S109–S111. doi: 10.1007/s10072-009-0064-4
Christiansen, I., Thomsen, L., Daugaard, D., Ulrich, V., and Olesen, J. (1999). Glyceryl trinitrate induces attacks of migraine without aura in sufferers of migraine with aura. Cephalalgia 19, 660–7. doi: 10.1046/j.1468-2982.1999.019007660.x
Coppola, G., Corbelli, I., Di Renzo, A., Chiappiniello, A., Chiarini, P., Parisi, V., et al. (2022). Visual stimulation and frequency of focal neurological symptoms engage distinctive neurocognitive resources in migraine with aura patients: A study of resting-state functional networks. J. Headache Pain 23:80. doi: 10.1186/s10194-022-01446-4
Coppola, G., Di Lorenzo, C., Parisi, V., Lisicki, M., Serrao, M., and Pierelli, F. (2019). Clinical neurophysiology of migraine with aura. J. Headache Pain 20:42. doi: 10.1186/s10194-019-0997-9
Coppola, G., Di Renzo, A., Tinelli, E., Di Lorenzo, C., Scapeccia, M., Parisi, V., et al. (2018). Resting state connectivity between default mode network and insula encodes acute migraine headache. Cephalalgia 38, 846–854. doi: 10.1177/0333102417715230
Coppola, G., Di Renzo, A., Tinelli, E., Petolicchio, B., Parisi, V., Serrao, M., et al. (2021). Thalamo-cortical networks in subtypes of migraine with aura patients. J. Headache Pain 22:58. doi: 10.1186/s10194-021-01272-0
Cucchiara, B., Datta, R., Aguirre, G., Idoko, K., and Detre, J. (2015). Measurement of visual sensitivity in migraine: Validation of two scales and correlation with visual cortex activation. Cephalalgia 35, 585–592. doi: 10.1177/0333102414547782
Cucchiara, B., Wolf, R., Nagae, L., Zhang, Q., Kasner, S., Datta, R., et al. (2013). Migraine with aura is associated with an incomplete circle of Willis: Results of a prospective observational study. PLoS One 8:e71007. doi: 10.1371/journal.pone.0071007
Cullum, C., Do, T., Ashina, M., Bendtsen, L., Hugger, S., Iljazi, A., et al. (2022). Real-world long-term efficacy and safety of erenumab in adults with chronic migraine: A 52-week, single-center, prospective, observational study. J. Headache Pain 23:61. doi: 10.1186/s10194-022-01433-9
Danno, D., Wolf, J., Ishizaki, K., Kikui, S., Yoshikawa, H., and Takeshima, T. (2020). Cranial autonomic symptoms of migraine in Japan: Prospective study of 373 migraine patients at a tertiary headache center. Headache 60, 1592–1600. doi: 10.1111/head.13888
DaSilva, A., Granziera, C., Snyder, J., and Hadjikhani, N. (2007a). Thickening in the somatosensory cortex of patients with migraine. Neurology 69, 1990–1995. doi: 10.1212/01.wnl.0000291618.32247.2d
DaSilva, A., Granziera, C., Tuch, D., Snyder, J., Vincent, M., and Hadjikhani, N. (2007b). Interictal alterations of the trigeminal somatosensory pathway and periaqueductal gray matter in migraine. Neuroreport 18, 301–305. doi: 10.1097/WNR.0b013e32801776bb
Datta, R., Aguirre, G., Hu, S., Detre, J., and Cucchiara, B. (2013). Interictal cortical hyperresponsiveness in migraine is directly related to the presence of aura. Cephalalgia 33, 365–374. doi: 10.1177/0333102412474503
Datta, R., Detre, J., Aguirre, G., and Cucchiara, B. (2011). Absence of changes in cortical thickness in patients with migraine. Cephalalgia 31, 1452–1458. doi: 10.1177/0333102411421025
Demarquay, G., and Mauguière, F. (2016). Central nervous system underpinnings of sensory hypersensitivity in migraine: Insights from neuroimaging and electrophysiological studie s. Headache 56, 1418–1438. doi: 10.1111/head.12651
Faragó, P., Tóth, E., Kocsis, K., Kincses, B., Veréb, D., Király, A., et al. (2019). Altered resting state functional activity and microstructure of the white matter in migraine with aura. Front. Neurol. 10:1039. doi: 10.3389/fneur.2019.01039
Faragó, P., Tuka, B., Tóth, E., Szabó, N., Király, A., Csete, G., et al. (2017). Interictal brain activity differs in migraine with and without aura: Resting state fMRI study. J. Headache Pain 18:8. doi: 10.1186/s10194-016-0716-8
Förster, A., Wenz, H., Kerl, H., Brockmann, M., and Groden, C. (2014). Perfusion patterns in migraine with aura. Cephalalgia 34, 870–876. doi: 10.1177/0333102414523339
Fu, T., Liu, L., Huang, X., Zhang, D., Gao, Y., Yin, X., et al. (2022). Cerebral blood flow alterations in migraine patients with and without aura: An arterial spin labeling study. J. Headache Pain 23:131. doi: 10.1186/s10194-022-01501-0
Gaist, D., Hougaard, A., Garde, E., Reislev, N., Wiwie, R., Iversen, P., et al. (2018). Migraine with visual aura associated with thicker visual cortex. Brain 141, 776–785. doi: 10.1093/brain/awx382
Gelfand, A. (2015). Episodic syndromes that may be associated with migraine: A.K.A. &the childhood periodic syndromes". Headache 55, 1358–1364. doi: 10.1111/head.12624
Gelfand, A., Reider, A., and Goadsby, P. (2013). Cranial autonomic symptoms in pediatric migraine are the rule, not the exception. Neurology 81, 431–436. doi: 10.1212/WNL.0b013e31829d872a
Gollion, C., Lerebours, F., Nemmi, F., Arribarat, G., Bonneville, F., Larrue, V., et al. (2022). Insular functional connectivity in migraine with aura. J. Headache Pain 23:106. doi: 10.1186/s10194-022-01473-1
Gonzalez-Martinez, A., Trillo Senín, S., Benavides Bernaldo de Queirós, C., Casado Fernández, L., Barbosa Del Olmo, A., Manzanares López, R., et al. (2021). Clinical characteristics and perfusion-computed tomography alterations in a series of patients with migraine with aura attended as stroke code. Headache 61, 1568–1574. doi: 10.1111/head.14243
Granziera, C., Daducci, A., Romascano, D., Roche, A., Helms, G., Krueger, G., et al. (2014). Structural abnormalities in the thalamus of migraineurs with aura: A multiparametric study at 3 T. Hum. Brain Mapp. 35, 1461–1468. doi: 10.1002/hbm.22266
Granziera, C., DaSilva, A., Snyder, J., Tuch, D., and Hadjikhani, N. (2006). Anatomical alterations of the visual motion processing network in migraine with and without aura. PLoS Med. 3:e402. doi: 10.1371/journal.pmed.0030402
Gupta, R., and Bhatia, M. (2007). A report of cranial autonomic symptoms in migraineurs. Cephalalgia 27, 22–28. doi: 10.1111/j.1468-2982.2006.01237.x
Guven, H., Çilliler, A., and Çomoğlu, S. (2013). Unilateral cranial autonomic symptoms in patients with migraine. Acta Neurol. Belg. 113, 237–242. doi: 10.1007/s13760-012-0164-4
Hadjikhani, N., Albrecht, D., Mainero, C., Ichijo, E., Ward, N., Granziera, C., et al. (2020). Extra-axial inflammatory signal in parameninges in migraine with visual aura. Ann. Neurol. 87, 939–949. doi: 10.1002/ana.25731
Hadjikhani, N., and Vincent, M. (2021). Can you have a migraine aura without knowing it? Curr. Opin. Neurol. 34, 350–355. doi: 10.1097/WCO.0000000000000924
Hadjikhani, N., Sanchez Del Rio, M., Wu, O., Schwartz, D., Bakker, D., Fischl, B., et al. (2001). Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc. Natl. Acad. Sci. U.S.A. 98, 4687–4692. doi: 10.1073/pnas.071582498
Hansen, J., and Charles, A. (2019). Differences in treatment response between migraine with aura and migraine without aura: Lessons from clinical practice and RCTs. J. Headache Pain 20:96. doi: 10.1186/s10194-019-1046-4
Hansen, J., Goadsby, P., and Charles, A. (2015). Reduced efficacy of sumatriptan in migraine with aura vs without aura. Neurology 84, 1880–1885. doi: 10.1212/WNL.0000000000001535
Hansen, J., Hauge, A., Olesen, J., and Ashina, M. (2010). Calcitonin gene-related peptide triggers migraine-like attacks in patients with migraine with aura. Cephalalgia 30, 1179–1186. doi: 10.1177/0333102410368444
Hansen, J., Thomsen, L., Olesen, J., and Ashina, M. (2008). Calcitonin gene-related peptide does not cause the familial hemiplegic migraine phenotype. Neurology 71, 841–847. doi: 10.1212/01.wnl.0000325482.64106.3f
Harriott, A., Takizawa, T., Chung, D., and Chen, S. (2019). Spreading depression as a preclinical model of migraine. J. Headache Pain 20:45. doi: 10.1186/s10194-019-1001-4
Headache Classification Committee of the International Headache Society [IHS] (2013). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33, 629–808. doi: 10.1177/0333102413485658
Headache Classification Subcommittee of the International Headache Society (2004). The international classification of headache disorders: 2nd edition. Cephalalgia 24(Suppl. 1), 9–160. doi: 10.1111/j.1468-2982.2003.00824.x
Headache Classification Committee of the International Headache Society [IHS] (2018). The international classification of headache disorders, 3rd edition. Cephalalgia 1–211, doi: 10.1177/0333102417738202
Headache Classification Committee of the International Headache Society (1988). Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 8(Suppl. 7), 1–96.
Hirtz, C., Adam, G., Raposo, N., Fabre, N., Ducros, A., Calviere, L., et al. (2022). Diagnostic utility of T2*-weighted GRE in migraine with aura attack. The cortical veins sign. Cephalalgia 42, 730–738. doi: 10.1177/03331024221076484
Holland, P., Akerman, S., Andreou, A., Karsan, N., Wemmie, J., and Goadsby, P. (2012). Acid-sensing ion channel 1: A novel therapeutic target for migraine with aura. Ann. Neurol. 72, 559–563. doi: 10.1002/ana.23653
Hougaard, A., Amin, F., Arngrim, N., Vlachou, M., Larsen, V., Larsson, H., et al. (2016). Sensory migraine aura is not associated with structural grey matter abnormalities. Neuroimage Clin. 11, 322–327. doi: 10.1016/j.nicl.2016.02.007
Hougaard, A., Amin, F., Christensen, C., Younis, S., Wolfram, F., Cramer, S., et al. (2017a). Increased brainstem perfusion, but no blood-brain barrier disruption, during attacks of migraine with aura. Brain 140, 1633–1642. doi: 10.1093/brain/awx089
Hougaard, A., Amin, F., Hauge, A., Ashina, M., and Olesen, J. (2013). Provocation of migraine with aura using natural trigger factors. Neurology 80, 428–431. doi: 10.1212/WNL.0b013e31827f0f10
Hougaard, A., Amin, F., Hoffmann, M., Larsson, H., Magon, S., Sprenger, T., et al. (2015a). Structural gray matter abnormalities in migraine relate to headache lateralization, but not aura. Cephalalgia 35, 3–9. doi: 10.1177/0333102414532378
Hougaard, A., Amin, F., Hoffmann, M., Rostrup, E., Larsson, H., Asghar, M., et al. (2014). Interhemispheric differences of fMRI responses to visual stimuli in patients with side-fixed migraine aura. Hum. Brain Mapp. 35, 2714–2723. doi: 10.1002/hbm.22361
Hougaard, A., Amin, F., Larsson, H., Rostrup, E., and Ashina, M. (2017b). Increased intrinsic brain connectivity between pons and somatosensory cortex during attacks of migraine with aura. Hum. Brain Mapp. 38, 2635–2642. doi: 10.1002/hbm.23548
Hougaard, A., Amin, F., Magon, S., Sprenger, T., Rostrup, E., and Ashina, M. (2015b). No abnormalities of intrinsic brain connectivity in the interictal phase of migraine with aura. Eur. J. Neurol. 22, 702–e46. doi: 10.1111/ene.12636
Hougaard, A., Nielsen, S., Gaist, D., Puonti, O., Garde, E., Reislev, N., et al. (2020). Migraine with aura in women is not associated with structural thalamic abnormalities. Neuroimage Clin. 28:102361. doi: 10.1016/j.nicl.2020.102361
Igarashi, H., Sakai, F., Kan, S., Okada, J., and Tazaki, Y. (1991). Magnetic resonance imaging of the brain in patients with migraine. Cephalalgia 11, 69–74. doi: 10.1046/j.1468-2982.1991.1102069.x
Jäger, H., Giffin, N., and Goadsby, P. (2005). Diffusion- and perfusion-weighted MR imaging in persistent migrainous visual disturbances. Cephalalgia 25, 323–332. doi: 10.1111/j.1468-2982.2004.00858.x
Karsan, N., and Goadsby, P. (2018). Biological insights from the premonitory symptoms of migraine. Nat. Rev. Neurol. 14, 699–710. doi: 10.1038/s41582-018-0098-4
Karsan, N., Bose, P., Zelaya, F., and Goadsby, P. (2018). Alterations in cerebral blood flow associated with the premonitory phase of migraine. Cephalalgia 38:36.
Karsan, N., Nagaraj, K., and Goadsby, P. (2022). Cranial autonomic symptoms: Prevalence, phenotype and laterality in migraine and two potentially new symptoms. J. Headache Pain 23:18. doi: 10.1186/s10194-022-01389-w
Kaube, H., Herzog, J., Käufer, T., Dichgans, M., and Diener, H. (2000). Aura in some patients with familial hemiplegic migraine can be stopped by intranasal ketamine. Neurology 55, 139–141. doi: 10.1212/wnl.55.1.139
Kellner-Weldon, F., El-Koussy, M., Jung, S., Jossen, M., Klinger-Gratz, P., and Wiest, R. (2018). Cerebellar hypoperfusion in migraine attack: Incidence and significance. AJNR Am. J. Neuroradiol. 39, 435–440. doi: 10.3174/ajnr.A5508
Kellner-Weldon, F., Jossen, M., Breiding, P., Grunder, L., Schankin, C., Scutelnic, A., et al. (2021). Imaging neurovascular uncoupling in acute migraine with aura with susceptibility weighted imaging. Clin. Neuroradiol. 31, 581–588. doi: 10.1007/s00062-020-00962-7
Kellner-Weldon, F., Lehmann, V., Breiding, P., Grunder, L., Muri, R., Pastore-Wapp, M., et al. (2020). Findings in susceptibility weighted imaging in pediatric patients with migraine with aura. Eur. J. Paediatr. Neurol. 28, 221–227. doi: 10.1016/j.ejpn.2020.05.008
Khouri Chalouhi, K., Squarza, S., Pisani Mainini, A., Di Fiore, P., Cariati, M., Frediani, F., et al. (2018). Brain MRI in patients affected by migraine with aura: Is there any cortical lesion? Neurol. Sci. 39(Suppl. 1), 65–66. doi: 10.1007/s10072-018-3349-7
Kruit, M., Launer, L., Ferrari, M., and van Buchem, M. (2005). Infarcts in the posterior circulation territory in migraine. The population-based MRI CAMERA study. Brain 128, 2068–2077. doi: 10.1093/brain/awh542
Kruit, M., van Buchem, M., Hofman, P., Bakkers, J., Terwindt, G., Ferrari, M., et al. (2004). Migraine as a risk factor for subclinical brain lesions. JAMA 291, 427–434. doi: 10.1001/jama.291.4.427
Kruit, M., van Buchem, M., Launer, L., Terwindt, G., and Ferrari, M. (2010). Migraine is associated with an increased risk of deep white matter lesions, subclinical posterior circulation infarcts and brain iron accumulation: The population-based MRI CAMERA study. Cephalalgia 30, 129–136. doi: 10.1111/j.1468-2982.2009.01904.x
Lai, T., Fuh, J., and Wang, S. (2009). Cranial autonomic symptoms in migraine: Characteristics and comparison with cluster headache. J. Neurol. Neurosurg. Psychiatry 80, 1116–1119. doi: 10.1136/jnnp.2008.157743
Lan, L., Zhang, X., Li, X., Rong, X., and Peng, Y. (2017). The efficacy of transcranial magnetic stimulation on migraine: A meta-analysis of randomized controlled trails. J. Headache Pain 18:86. doi: 10.1186/s10194-017-0792-4
Lauritzen, M., and Olesen, J. (1984). Regional cerebral blood flow during migraine attacks by xenon-133 inhalation and emission tomography. Brain 107(Pt 2), 447–461. doi: 10.1093/brain/107.2.447
Lauritzen, M., Jørgensen, M., Diemer, N., Gjedde, A., and Hansen, A. (1982). Persistent oligemia of rat cerebral cortex in the wake of spreading depression. Ann. Neurol. 12, 469–474. doi: 10.1002/ana.410120510
Lauritzen, M., Skyhøj Olsen, T., Lassen, N., and Paulson, O. (1983). Changes in regional cerebral blood flow during the course of classic migraine attacks. Ann. Neurol. 13, 633–641. doi: 10.1002/ana.410130609
Leao, A. (1944). Spreading depression of activity in the cerebral cortex. J. Neurophysiol. 7, 359–390.
Lewis, R., Ruiz, A., and Monteith, T. (2020). Reversible lesion of the corpus callosum in a patient with migraine with aura: A case study. Headache 60, 791–792. doi: 10.1111/head.13768
Lin, F., and Yang, C. (2011). Reversible splenial lesion of the corpus callosum in migraine with aura. Neurologist 17, 157–159. doi: 10.1097/NRL.0b013e31821733c2
Lipton, R., Dodick, D., Silberstein, S., Saper, J., Aurora, S., Pearlman, S., et al. (2010). Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: A randomised, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. 9, 373–380. doi: 10.1016/S1474-4422(10)70054-5
Liu, K., Wang, B., Hao, Y., Song, S., and Pan, M. (2020). The correlation between migraine and patent foramen ovale. Front. Neurol. 11:543485. doi: 10.3389/fneur.2020.543485
Lo Buono, V., Bonanno, L., Corallo, F., Pisani, L., Lo Presti, R., Grugno, R., et al. (2017). Functional connectivity and cognitive impairment in migraine with and without aura. J. Headache Pain 18:72. doi: 10.1186/s10194-017-0782-6
Magon, S., May, A., Stankewitz, A., Goadsby, P., Schankin, C., Ashina, M., et al. (2019). Cortical abnormalities in episodic migraine: A multi-center 3T MRI study. Cephalalgia 39, 665–673. doi: 10.1177/0333102418795163
Maller, J., Anderson, R., Thomson, R., Daskalakis, Z., Rosenfeld, J., and Fitzgerald, P. (2017). Occipital bending in schizophrenia. Aust. N. Z. J. Psychiatry 51, 32–41. doi: 10.1177/0004867416642023
Maller, J., Anderson, R., Thomson, R., Rosenfeld, J., Daskalakis, Z., and Fitzgerald, P. (2015). Occipital bending (yakovlevian torque) in bipolar depression. Psychiatry Res. 231, 8–14. doi: 10.1016/j.pscychresns.2014.11.008
Maller, J., Thomson, R., Rosenfeld, J., Anderson, R., Daskalakis, Z., and Fitzgerald, P. (2014). Occipital bending in depression. Brain 137(Pt 6), 1830–1837. doi: 10.1093/brain/awu072
Masson, R., Demarquay, G., Meunier, D., Lévêque, Y., Hannoun, S., Bidet-Caulet, A., et al. (2021). Is migraine associated to brain anatomical alterations? New data and coordinate-based meta-analysis. Brain Topogr. 34, 384–401. doi: 10.1007/s10548-021-00824-6
Matharu, M., Good, C., May, A., Bahra, A., and Goadsby, P. (2003). No change in the structure of the brain in migraine: A voxel-based morphometric study. Eur. J. Neurol. 10, 53–57. doi: 10.1046/j.1468-1331.2003.00510.x
Mehnert, J., Schulte, L., and May, A. (2020). No grey matter alterations in longitudinal data of migraine patients. Brain 143:e93. doi: 10.1093/brain/awaa300
Messina, R., Rocca, M., Colombo, B., Valsasina, P., Horsfield, M., Copetti, M., et al. (2013). Cortical abnormalities in patients with migraine: A surface-based analysis. Radiology 268, 170–180. doi: 10.1148/radiol.13122004
Michels, L., Villanueva, J., O’Gorman, R., Muthuraman, M., Koirala, N., Büchler, R., et al. (2019). Interictal hyperperfusion in the higher visual cortex in patients with episodic migraine. Headache 59, 1808–1820. doi: 10.1111/head.13646
Niddam, D., Lai, K., Fuh, J., Chuang, C., Chen, W., and Wang, S. (2016). Reduced functional connectivity between salience and visual networks in migraine with aura. Cephalalgia 36, 53–66. doi: 10.1177/0333102415583144
Ogunyemi, A. (1995). Migraine with prolonged aura: Correlation of clinical and EEG features. Behav. Neurol. 8, 109–114. doi: 10.3233/BEN-1995-8206
Olesen, J., Friberg, L., Olsen, T., Iversen, H., Lassen, N., Andersen, A., et al. (1990). Timing and topography of cerebral blood flow, aura, and headache during migraine attacks. Ann. Neurol. 28, 791–798. doi: 10.1002/ana.410280610
Olesen, J., Larsen, B., and Lauritzen, M. (1981). Focal hyperemia followed by spreading oligemia and impaired activation of rCBF in classic migraine. Ann. Neurol. 9, 344–352. doi: 10.1002/ana.410090406
Özkan, E., and Gürsoy-Özdemir, Y. (2021). Occipital bending in migraine with visual aura. Headache 61, 1562–1567. doi: 10.1111/head.14240
Palm-Meinders, I., Koppen, H., Terwindt, G., Launer, L., Konishi, J., Moonen, J., et al. (2012). Structural brain changes in migraine. JAMA 308, 1889–1897. doi: 10.1001/jama.2012.14276
Park, S., Lee, D., Lee, H., Shin, K., and Park, K. (2022). Brain networks in migraine with and without aura: An exploratory arterial spin labeling MRI study. Acta Neurol. Scand. 145, 208–214. doi: 10.1111/ane.13536
Parks, N., Rigby, H., Gubitz, G., Shankar, J., and Purdy, R. (2014). Dysmetropsia and Cotard’s syndrome due to migrainous infarction—or not? Cephalalgia 34, 717–720. doi: 10.1177/0333102414520765
Petrusic, I., Dakovic, M., and Zidverc-Trajkovic, J. (2019a). Subcortical volume changes in migraine with aura. J. Clin. Neurol. 15, 448–453. doi: 10.3988/jcn.2019.15.4.448
Petrusic, I., Dakovic, M., and Zidverc-Trajkovic, J. (2019b). Volume alterations of brainstem subregions in migraine with aura. Neuroimage Clin. 22:101714. doi: 10.1016/j.nicl.2019.101714
Petrusic, I., Dakovic, M., Kacar, K., and Zidverc-Trajkovic, J. (2018). Migraine with aura: Surface-based analysis of the cerebral cortex with magnetic resonance imaging. Korean J. Radiol. 19, 767–776. doi: 10.3348/kjr.2018.19.4.767
Raieli, V., Giordano, G., Spitaleri, C., Consolo, F., Buffa, D., Santangelo, G., et al. (2015). Migraine and cranial autonomic symptoms in children and adolescents: A clinical study. J. Child Neurol. 30, 182–186. doi: 10.1177/0883073814535494
Ridolfi, M., Granato, A., Polverino, P., Furlanis, G., Ukmar, M., Zorzenon, I., et al. (2018). Migrainous aura as stroke-mimic: The role of perfusion-computed tomography. Clin. Neurol. Neurosurg. 166, 131–135.
Riesco, N., Pérez-Alvarez, A., Verano, L., García-Cabo, C., Martínez-Ramos, J., Sánchez-Lozano, P., et al. (2016). Prevalence of cranial autonomic parasympathetic symptoms in chronic migraine: Usefulness of a new scale. Cephalalgia 36, 346–350. doi: 10.1177/0333102415593087
Rocca, M., Pagani, E., Colombo, B., Tortorella, P., Falini, A., Comi, G., et al. (2008). Selective diffusion changes of the visual pathways in patients with migraine: A 3-T tractography study. Cephalalgia 28, 1061–1068. doi: 10.1111/j.1468-2982.2008.01655.x
Russell, M., and Olesen, J. (1996). A nosographic analysis of the migraine aura in a general population. Brain 119(Pt 2), 355–361. doi: 10.1093/brain/119.2.355
Russo, A., Tessitore, A., Silvestro, M., Di Nardo, F., Trojsi, F., Del Santo, T., et al. (2019). Advanced visual network and cerebellar hyperresponsiveness to trigeminal nociception in migraine with aura. J. Headache Pain 20:46. doi: 10.1186/s10194-019-1002-3
Sanchez del Rio, M., Bakker, D., Wu, O., Agosti, R., Mitsikostas, D., Ostergaard, L., et al. (1999). Perfusion weighted imaging during migraine: Spontaneous visual aura and headache. Cephalalgia 19, 701–707. doi: 10.1046/j.1468-2982.1999.019008701.x
Sándor, P., Dydak, U., Schoenen, J., Kollias, S., Hess, K., Boesiger, P., et al. (2005). MR-spectroscopic imaging during visual stimulation in subgroups of migraine with aura. Cephalalgia 25, 507–518. doi: 10.1111/j.1468-2982.2005.00900.x
Sarchielli, P., Tarducci, R., Presciutti, O., Gobbi, G., Pelliccioli, G., Stipa, G., et al. (2005). Functional 1H-MRS findings in migraine patients with and without aura assessed interictally. Neuroimage 24, 1025–1031. doi: 10.1016/j.neuroimage.2004.11.005
Schankin, C., Viana, M., and Goadsby, P. (2017). Persistent and repetitive visual disturbances in migraine: A review. Headache 57, 1–16. doi: 10.1111/head.12946
Schwedt, T., Peplinski, J., Garcia-Filion, P., and Berisha, V. (2019). Altered speech with migraine attacks: A prospective, longitudinal study of episodic migraine without aura. Cephalalgia 39, 722–731. doi: 10.1177/0333102418815505
Serrano, F., Arauz, A., Uribe, R., Becerra, L., Mantilla, K., and Zermeño, F. (2018). Long-term follow-up of patients with migrainous infarction. Clin. Neurol. Neurosurg. 165, 7–9. doi: 10.1016/j.clineuro.2017.12.008
Sheng, L., Ma, H., Shi, Y., Dai, Z., Zhong, J., Chen, F., et al. (2021). Cortical thickness in migraine: A coordinate-based meta-analysis. Front. Neurosci. 14:600423. doi: 10.3389/fnins.2020.600423
Sheng, L., Zhao, P., Ma, H., Yuan, C., Zhong, J., Dai, Z., et al. (2020). A lack of consistent brain grey matter alterations in migraine. Brain 143:e45. doi: 10.1093/brain/awaa123
Shin, Y., Park, H., Shim, J., Oh, M., and Kim, M. (2015). Seasonal variation, cranial autonomic symptoms, and functional disability in migraine: A questionnaire-based study in tertiary care. Headache 55, 1112–1123. doi: 10.1111/head.12613
Silvestro, M., Tessitore, A., Di Nardo, F., Scotto di Clemente, F., Trojsi, F., Cirillo, M., et al. (2022). Functional connectivity changes in complex migraine aura: Beyond the visual network. Eur. J. Neurol. 29, 295–304. doi: 10.1111/ene.15061
Siniatchkin, M., Sendacki, M., Moeller, F., Wolff, S., Jansen, O., Siebner, H., et al. (2012). Abnormal changes of synaptic excitability in migraine with aura. Cereb. Cortex 22, 2207–2216. doi: 10.1093/cercor/bhr248
Slavova, N., Denier, N., El-Koussy, M., Wiest, R., Kellner-Weldon, F., Fischer, U., et al. (2020). The index vein pointing to the origin of the migraine aura symptom: A case series. Neurology 94, e2577–e2580. doi: 10.1212/WNL.0000000000009493
Soriani, S., Feggi, L., Battistella, P., Arnaldi, C., De Carlo, L., and Stipa, S. (1997). Interictal and ictal phase study with Tc 99m HMPAO brain SPECT in juvenile migraine with aura. Headache 37, 31–36. doi: 10.1046/j.1526-4610.1997.3701031.x
Stærmose, T., Knudsen, M., Kasch, H., and Blicher, J. (2019). Cortical GABA in migraine with aura -an ultrashort echo magnetic resonance spectroscopy study. J. Headache Pain 20:110. doi: 10.1186/s10194-019-1059-z
Tantik Pak, A., Nacar Dogan, S., and Sengul, Y. (2022). Structural integrity of corpus callosum in patients with migraine: A diffusion tensor imaging study. Acta Neurol. Belg. [Epub ahead of print]. doi: 10.1007/s13760-021-01863-3
Tedeschi, G., Russo, A., Conte, F., Corbo, D., Caiazzo, G., Giordano, A., et al. (2016). Increased interictal visual network connectivity in patients with migraine with aura. Cephalalgia 36, 139–147. doi: 10.1177/0333102415584360
Tessitore, A., Russo, A., Conte, F., Giordano, A., De Stefano, M., Lavorgna, L., et al. (2015). Abnormal connectivity within executive resting-state network in migraine with aura. Headache 55, 794–805. doi: 10.1111/head.12587
Tolner, E., Houben, T., Terwindt, G., de Vries, B., Ferrari, M., and van den Maagdenberg, A. (2015). From migraine genes to mechanisms. Pain 156(Suppl. 1), S64–S74. doi: 10.1097/01.j.pain.0000460346.00213.16
Turk, W., Uiterwijk, A., Pasmans, R., Meys, V., Ayata, C., and Koehler, P. (2017). Aspirin prophylaxis for migraine with aura: An observational case series. Eur. Neurol. 78, 287–289. doi: 10.1159/000481252
Uetani, H., Kitajima, M., Sugahara, T., Kikuchi, H., Muto, Y., Hirahara, T., et al. (2018). Perfusion abnormality on three-dimensional arterial spin labeling with a 3T MR system in pediatric and adolescent patients with migraine. J. Neurol. Sci. 395, 41–46. doi: 10.1016/j.jns.2018.09.024
Veréb, D., Szabó, N., Tuka, B., Tajti, J., Király, A., Faragó, P., et al. (2020). Temporal instability of salience network activity in migraine with aura. Pain 161, 856–864. doi: 10.1097/j.pain.0000000000001770
Viana, M., Linde, M., Sances, G., Ghiotto, N., Guaschino, E., Allena, M., et al. (2016). Migraine aura symptoms: Duration, succession and temporal relationship to headache. Cephalalgia 36, 413–421. doi: 10.1177/0333102415593089
Viana, M., Sances, G., Linde, M., Ghiotto, N., Guaschino, E., Allena, M., et al. (2017). Clinical features of migraine aura: Results from a prospective diary-aided study. Cephalalgia 37, 979–989. doi: 10.1177/0333102416657147
Viana, M., Sances, G., Linde, M., Nappi, G., Khaliq, F., Goadsby, P., et al. (2018). Prolonged migraine aura: New insights from a prospective diary-aided study. J. Headache Pain 19:77. doi: 10.1186/s10194-018-0910-y
Vincent, M., and Hadjikhani, N. (2007). Migraine aura and related phenomena: Beyond scotomata and scintillations. Cephalalgia 27, 1368–1377. doi: 10.1111/j.1468-2982.2007.01388.x
Wolf, M., Okazaki, S., Eisele, P., Rossmanith, C., Gregori, J., Griebe, M., et al. (2018). Arterial spin labeling cerebral perfusion magnetic resonance imaging in migraine aura: An observational study. J. Stroke Cerebrovasc. Dis. 27, 1262–1266. doi: 10.1016/j.jstrokecerebrovasdis.2017.12.002
Yeo, J., Goh, C., Tan, Y., Sim, B., Chan, B., Syn, N., et al. (2022). Evaluating the relationship between right-to-left shunt and white matter hyperintensities in migraine patients: A systematic review and meta-analysis. Front. Neurol. 13:972336. doi: 10.3389/fneur.2022.972336
Yilmaz-Kusbeci, O., Gocmen-Mas, N., Yucel, A., Karabekir, H., Ertekin, T., and Yazici, A. (2010). Evaluation of cerebellar and cerebral volume in migraine with aura: A stereological study. Cerebellum 9, 345–351. doi: 10.1007/s12311-010-0167-8
Zhang, C., Detre, J., Kasner, S., and Cucchiara, B. (2018). Basilar artery lateral displacement may be associated with migraine with aura. Front. Neurol. 9:80. doi: 10.3389/fneur.2018.00080
Zhang, Q., Datta, R., Detre, J., and Cucchiara, B. (2017). White matter lesion burden in migraine with aura may be associated with reduced cerebral blood flow. Cephalalgia 37, 517–524. doi: 10.1177/0333102416649760
Zhang, X., Zhou, J., Guo, M., Cheng, S., Chen, Y., Jiang, N., et al. (2023). A systematic review and meta-analysis of voxel-based morphometric studies of migraine. J. Neurol. 270, 152–170. doi: 10.1007/s00415-022-11363-w
Keywords: migraine, aura, visual aura, sensory aura, dysphasic aura, neuroimaging, fMRI, MRI
Citation: Karsan N, Silva E and Goadsby PJ (2023) Evaluating migraine with typical aura with neuroimaging. Front. Hum. Neurosci. 17:1112790. doi: 10.3389/fnhum.2023.1112790
Received: 30 November 2022; Accepted: 01 March 2023;
Published: 21 March 2023.
Edited by:
Catherine D. Chong, Mayo Clinic Arizona, United StatesReviewed by:
Christoph Schankin, University Hospital of Bern, SwitzerlandRémy Masson, Institut de l’Audition, Institut Pasteur, France
Copyright © 2023 Karsan, Silva and Goadsby. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nazia Karsan, bmF6aWEua2Fyc2FuQGtjbC5hYy51aw==
 Nazia Karsan
Nazia Karsan Elisa Silva
Elisa Silva Peter J. Goadsby
Peter J. Goadsby