
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Hum. Dyn. , 29 January 2025
Sec. Digital Impacts
Volume 6 - 2024 | https://doi.org/10.3389/fhumd.2024.1502432
This article is part of the Research Topic Ethical Dilemmas of Digitalisation of Mental Health View all 4 articles
Introduction: Digital mental health care system includes the interventions delivered via digital technologies, such as mobile apps, websites, or virtual reality (VR). A recent upsurge in the digital mental healthcare care services has been observed in the last 5 years. With its core advantage of reaching the unreached, wider coverage, cost and time effectivity, all eyes are on the digital mental health care system. It is definitely a mechanism to cater rising prevalence of mental health concern, stigma towards mental health, accessibility and cost and uplift the psychological wellbeing. Success of the digital mental health care system has been researched world-wide. However, the same is not unaffected by the ethical concerns.
Methods: This study aims to perform a comprehensive bibliometric analysis of scholarly articles on ethical concerns and dilemmas of digital mental health care by utilizing data extracted from the Scopus database from 2000 to 2024 by analysing 123 research articles. Statistical descriptive analysis in combination with performance analysis and co-word analysis was used to understand the research trends, leading countries and country collaborations studying ethical concerns related to digital mental healthcare.
Result and discussion: The first publication appeared in 2000 with zero research till the year 2005. In this decade till 2010 we can observe only 4 publications. Consistent publishing started trending upward through 2018, observing the largest increase during pandemic in 2020 and onwards constituting 100 publications. The United States of America is the leading country studying ethical dilemmas in Digital Mental healthcare, with 42 papers followed by United Kingdom with 23 publications. The most influential peace of research with 490 citations is article co-authored by Barak et al. (2009), which is defining internet-supported therapeutic interventions and related concerns. BMJ Open is noted as the leading journal which is publishing issues concerning Digital Mental Healthcare with 18 publications, followed by Frontiers in Psychiatry and JMIR Mental Health. Analyses reflects that the top cited articles on Digital Mental healthcare are specifically directed on bringing out some of the key concerns of data privacy, emergency response, therapist competency and consent which requires appropriate handling Otherwise they may be cause of distress to client and question the trustworthiness of the Digital Mental Health Care system.
Conclusion: The concerns brought out through this bibliometric analysis could be important guiding principles for online mental health services. Alongside, mental health professionals operating online must have orientation on the ethical concerns surrounding online mental healthcare.
India’s enormous population and diversified demographics provide a significant mental health burden that requires immediate treatment (Sagar et al., 2020; Sagar et al., 2020). Mental diseases affect people of all ages, socioeconomic backgrounds, and geographic areas. The consequences of these disorders include human pain, reduced everyday functioning, and significant social expenses (Sagar et al., 2020; Chokshi et al., 2016; Sagar et al., 2020; Chokshi et al., 2016). The frequency of mental health illnesses in India has gradually increased in recent years, adding to the growing public health concern (Chandra et al., 2018; Chokshi et al., 2016; Chandra et al., 2018; Chokshi et al., 2016). According to estimates, almost 15% of India’s population suffers from some sort of mental illness. This number represents a wide range of diseases, including anxiety disorders, depression, bipolar disorder, schizophrenia, drug use disorders, and neurodevelopmental problems (Hossain and Purohit, 2019; Sagar and Singh, 2022). The increasing incidence of mental health conditions in India and their complex effects call for a thorough comprehension of the difficulties.
These mental health issues have far-reaching effects for the entire society. For starters, people suffering from mental illnesses experience a great deal of psychological sorrow and misery since their afflictions frequently prevent them from leading fulfilled lives. They may have difficulty establishing relationships, pursuing school or work prospects, and engaging in social activities. Furthermore, mental health issues have a significant impact on the general functioning of communities and nations. Reduced productivity, both in the workplace and in homes, has a substantial economic impact. Mental health disorders frequently result in absenteeism, decreased job efficiency, and long-term incapacity, reducing worker productivity and economic growth(Mental Health, Brain Health and Substance Use, n.d.; McDaid et al., 2008).
Addressing mental health concerns is critical not just for the well-being of those afflicted, but also for the general advancement and development of the country.
Digital mental health technologies (DMHTs) are the application of digital technologies in the mental health field and have offered promising solutions to address challenges in mental health care (Wies et al., 2021). These technologies may encompass digital screening, assessment tools, digital interventions, artificial intelligence applications (e.g., chatbots), and virtual reality treatments (Hirschtritt and Insel, 2018), many others. DMHTs have been rapidly embraced due to their improved availability, real-time monitoring via digital phenotyping, and adaptability to blended care approaches which integrates digital and face-to-face interventions. Digital technologies aid in the optimisation of traditional services driven by user needs, data-informed “personalised services” for therapists, and digital mental health interventions (De Vos, 2021). The possibility of delivering mental health care remotely was seen during the COVID-19 pandemic which reinforced the need and development of scalable mental health interventions (Torous et al., 2020). In current scenario the role of DMHTs has extended beyond accessibility and enabled personalized and data driven services to cater the user needs. The real time adjustments to various interventions based on ongoing data collections have opened new avenues (Meyerhoff et al., 2023). For instance, digital phenotyping approaches utilizes smartphone built-in sensors and wearable devices to monitor various behavioural patterns, providing therapists with critical insights on ongoing improvements for patients’ mental health (Cornet and Holden, 2018).
This paper focusses solely on how digital technology is used in the field of mental health care. Mental health disorders are a major global concern, affecting 450 million people worldwide (Chaudhary et al., 2024; Cleary et al., 2019). According to many studies, the COVID-19 pandemic has exacerbated mental health issues, with an estimated global prevalence of 28.0% for depression, 26.9% for anxiety, and 36.5% for stress, raising further concerns (Nochaiwong et al., 2021). Mental disorders were the eighth most common health concern in Asia in 2019, with depressive and anxiety disorders accounting for the majority of cases (Chen et al., 2024). This implies that mental health issues now account for 16% of global disability-adjusted life years (DALYs), which is a threefold increase from previous assessments (Arias et al., 2022). Additionally, mental health issues due to the growing number, carry enormous societal and economic implications, with global economic losses estimated to exceed US$16 trillion over the next two decades (Tomlinson, 2013; Cleary et al., 2019). Despite the well-documented significant impact, mental health services receive very little funding and attention, with low-income countries allocating only 0.5% of their health budget to mental health, resulting in a stark disparity in need and demand (Tomlinson, 2013). Globally, mental health budgets remain inadequate, accounting for only 2% of total health expenditure (Cleary et al., 2019).
Despite the concerns raised aforementioned, digital interventions have the potential to help reduce the global mental health treatment gap (Rebello et al., 2014) and enable prevention, prediction, and personalised care (Terra et al., 2023). Digital mental health care is a useful tool for inpatient treatment and follow-up, particularly for patients with eating disorders, mood disorders, psychotic episodes, and patient groups with multiple diseases. In addition to in-person therapy, digital mental health care technologies can be utilized for aftercare or in situations when in-person treatment is not accessible (Diel et al. 2024). Some of the example of these technologies include secure social networking tools, AI-powered assistants that employ cognitive behavioural therapy techniques, and mobile mindfulness meditation apps (Ackerman et al., 2017; Ahmed et al., 2021). DMHTs if provided with evidence basis treatments like internet based cognitive behavioural therapy (iCBT), mobile mindfulness applications and online peer counselling, can have a significant impact on improving the mental health of individuals and societies (Apolinário-Hagen et al., 2020; Andersson et al., 2019; Fiske et al., 2019). DMHTs encompass a wide range of technologies, which in traditional set up is not possible. For example, mood tracking devices through mobile phone provide continuous and data driven support, reducing relapses (Torous et al., 2020). Additionally, some advanced tools like immersive technologies like virtual realities are being used successfully in exposure therapy for treating phobias and PTSDs (Maples-Keller et al., 2017). From simple internet-based interventions to smartphone applications and advanced technologies (immersive technology) such as virtual reality (Balcombe and De Leo, 2021; Bell et al., 2024). DMHT services enable the integration of these digital tools into primary care-based mental health services, potentially improving access to evidence-based care (Bucci et al., 2019). Beyond these treatments, DHMTs even have proven effective in improving mental health literacy, various stigmas, and increasing access to these services for marginalized groups (Naslund et al., 2017; Schueller et al., 2019). Therefore, DHMTs have the potential to predict the onset of various mental health issues, indicating a positive outlook for the future.
Despite the promises, integrating technology into mental healthcare presents both opportunities and ethical challenges. If the challenges are not identified and addressed, these can be extremely terrifying. These issues have become especially apparent in recent months, with several public cases of misuse of digitally available personal data (Isaak and Hanna, 2018). The current article presents an analysis of reported and addressed ethical issues related to DMHTs. There are several ethical concerns reported like user autonomy, transparency, privacy, informed consent, data security, and potential bias (Wykes et al., 2019; Martinez-Martin et al., 2020; Terra et al., 2023). Some research in the field of ihealth (AI-based) on algorithmic and data-driven technologies shows challenges due to limited user involvement and insufficient strategies to handle algorithmic accountability (Gooding and Kariotis, 2021). Other significant challenges reported include an agency’s safety monitoring, a lack of regulatory guidelines, and the exclusion of specific groups such as low and middle-income individuals (Rebello et al., 2014). DHMTs, despite their growth, are not still well presented with evidence-based results, adding another challenge in perceiving them as independent services or accepting their integration into traditional models. Many mental health professionals also lack of adequate training in technology use and underprepared, cannot observe the complex challenges (Sabin et al., 2017). A significant challenge lies in identifying who bears the responsibility for ethical practices and its distribution, whether it is creators, end users, and providers of DMHTs (Wykes et al., 2019). In the absence of well-defined ethical framework, the potential benefits of DMHTs could be overshadowed by these ethical challenges.
Considering the review of various studies and gap analysis following study objectives and methodologies are formed to operationalise current bibliometric analysis.
Prior to commencing the analysis process, it is critical to determine the purpose and scope of the proposed bibliometric analysis (Donthu et al., 2021). Utilizing data retrieved from the Scopus database from 2000 to 2024, the authors of the current bibliometric analysis sought to investigate and consider the prominent research contributors, trends, and ethical issues and quandaries surrounding digital mental health care.
The authors conducted the bibliometric study using the Scopus database. Data for this study were obtained on September 20th, 2024, from the Vellore Institute of Technology’s institutional access to the Scopus database. Since this is a relatively new topic, the search was not limited by a certain year. The analysis began with data extraction from the initial publication, which was published in 2000. The Scopus database for ethical concerns in digital mental health care comprised highly renowned worldwide scientific publications, guaranteeing that the stringent peer-review system maintained the papers’ calibre. Given the rigor of the SCOPUS-indexed articles, the information utilized was trustworthy. In 2004, Elsevier introduced its Scopus abstract and citation database, which is the largest academic database in the world and is used as a published reference in several countries. The bibliometric analysis conducted in this study only included articles that were indexed by Scopus.
Since digital mental health is a relatively new phenomena, there were no restrictions on the time range. The first academic papers came in the year 2000; hence, from 2000 to 2024, research articles were incorporated to have a deeper grasp of the issue under investigation. The most highly referenced works on “ethical concerns and dilemmas of digital mental health care” were located by utilizing the Scopus database’s advanced search tools.
The search terms (“Dilemmas” OR “ethical dilemmas” OR “Ethical concerns” OR “Ethics” or “ethical issues” AND “Digital Mental health” OR “online counselling” OR “online therapy “or “online mental health support “or “digital counselling “or “digital therapy” OR “Online Mental Health Care” OR “Tele mental health” OR “Digital Mental health Interventions “OR “Telepsychiatry” OR “Telepsychology” OR “digital psychotherapy” OR “Mental Health Application”) in topics (title, abstract, keywords) were used to find the articles published between the year 2000 and 2024. The search methodologies were chosen based on the investigators’ preliminary searches. We also eliminated articles that did not directly address digital mental health treatment and ethical issues (ex: articles which talked about digital therapy for pulmonary arterial hypertension, etc.).
The data is exported in CSV format once the research focus has been chosen by locating relevant keywords. MS Excel and RStudio were used to assess the CSV data. All of the data were entered into Microsoft Excel for rectification, classification, and selection. The results were presented using graphs, tables, and photographs. RStudio was used to create the visualization maps (Figure 1; Table 1).
Results of the bibliometric analysis are presented in form of tables and graphs as per the objectives and research questions formulised to understand the research trends and major contributors in the field of research studying “Ethical Concerns in the digital mental health care.” The results are displayed alongside the research questions which were explored in this analysis.
RQ1: What are the publication trends and metrics of performance analysis in the field of Ethical Concerns and Mental Health Care?
The publishing trend of research in field of Ethical Concerns and Digital Mental Healthcare is depicted in Table 2 by analysing the total number of publications published against the year of publication. As Table 2 shows, Ethical Concerns and Digital Mental healthcare has been the subject of research since only 2000 as it’s a relatively new field. 2021 (33 articles), 2022 (28 articles), 2020 (15 articles), 2023 (12 articles) and 2024 (11 articles) were the most prolific years. With 99 papers out of the 123 articles produced between 2020 and 2024, this growing tendency is predicted to continue beyond 2024. Figure 2 depicts the average citations per year and a pronounced peak observed in 2009 suggested it as a year of significant scholarly impact, where research within the field likely contributed pivotal insights or breakthroughs, leading to a high citation rate.
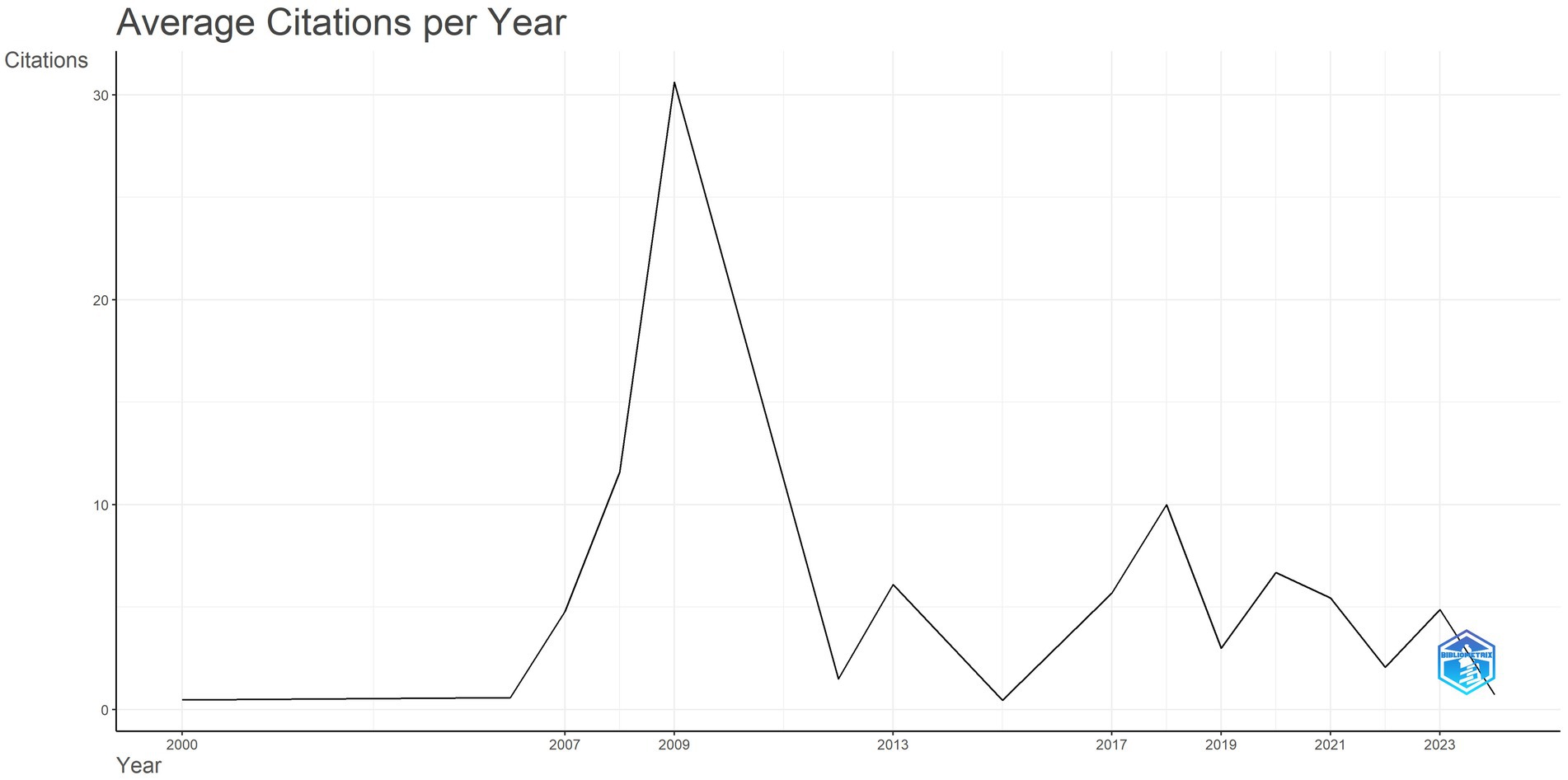
Figure 2. Performance analysis in the field of ethical concerns and mental health care in terms of citations.
Table 2 illustrates the distribution of articles on Ethical Concerns and Digital Mental healthcare, which shows the evolution of the range of publications. There are three main phases of evolution that may be identified. A few noteworthy publications were produced during the first period, which ran from 2000 to 2009. In comparison to the previous stage, there was an average of over four times as many papers generated during the second period, which spanned from 2010 to 2019. The most productive trajectory of current research on Ethical Concerns and Digital Mental healthcare may be seen in the third period, which spans 2020 to 2024. With 99 papers published, this time period saw the highest number of submissions to yet.
RQ 2: Which country and institution contribute the most to the publication of Ethical Concerns and Digital Mental Health Care?
Table 3 provides a thorough examination and unique display of the prevailing trend that is developing in the top 20 countries that contribute to publications on Ethical Concerns and Digital Mental Health Care. The United States (n = 22 with a total citation of 677), the United Kingdom (n = 14 with a total citation of 202), Canada (n = 11 with a total citation of 71), Australia (n = 9 with a total citation of 156), India (n = 9 with a total citation of 216), Germany (n = 6 with a total citation of 23), Israel (n = 5 with a total citation of 519), South Africa (n = 5 with a total citation of 59), France (n = 4 with a total citation of 21), Switzerland (n = 4 with a total citation of 272), China (n = 3 with a total citation of 29), Denmark (n = 3 with a total citation of 38), Ireland (n = 3 with a total citation of 183), Italy (n = 3 with a total citation of 339), Belgium (n = 1 with a total citation of 0), Brazil (n = 1 with a total citation of 3), Hong Kong (n = 1 with a total citation of 1), Iran (n = 1 with a total citation of 3), Kenya (n = 1 with a total citation of 6) and Lebanon (n = 1 with a total citation of 12) are among the top 20 countries.
The research also looked at the degree of international collaboration between nations; the results showed that United Kingdom had the highest rates of collaboration, as shown by the significant number of multiple-country publications (MCP) they had which was seven this was followed by USA with an MCP of four. However, the study also revealed that there is little international collaboration in this field, since the number of single-country publications (SCP) among the top 10 most prolific nations significantly outweighs the number of MCPs as seen in Figure 3. Figure 4 shows the international network of collaboration between nations. The thickness of the lines indicating the degree of collaboration between countries/regions indicates the cooperative links between them. USA turned out to be the most active member of this network, interacting with the Canada, Germany and United Kingdom at very high levels.
As depicted in Table 3, the five most extensive contributor affiliations in this study are the Queen’s University (n = 42), Washington University School of Medicine in Saint Louis (n = 21), University Health Network (n = 16), University of Alberta (n = 16), and the Post Graduate Institute of Medical Education and Research (n = 13).
RQ 3: Which journals are productively publishing in the field of Ethical Concerns and Digital Mental Health Care?
Table 4 reveals that a majority of publications are published in medical journals, especially journals related to psychology. With 18 publications altogether, BMJ Open holds the first place with around 62 citations and a h-index of 4. Since 2015, the magazine has been publishing continuously. JMIR Mental Health (TC:266; h-index: 6) and Frontiers In Psychiatry (TC: 229; h-index: 5) comes next with nine articles followed by JMIR Research Protocols with around eight articles (TC:46; h-index: 4). Annals Of Behavioral Medicine is a renowned, higher-quality journal that will hold the first position if citation count becomes a criteria (TC:490; h-index: 1; TP: 1). With a well-regarded publication list, JMIR Mental Health (TC:266; h-index: 6; TP: 9) is the second-ranked journal. Each journal shown in the table has an index in both Scopus and Web of Science. This shows how much focus has recently been placed on researching Ethical Concerns and Digital Mental Healthcare. Subsequent research endeavours have to consider a publication that will disseminate their study on Ethical Concerns and Digital Mental Healthcare (Figure 5).
Bradford’s Law is a bibliometric principle that describes the distribution of scholarly publications on a specific topic across different journals. It suggests that a small number of journals publish a disproportionate number of articles on a given subject. Bradford’s Law divides journals into zones of decreasing productivity. The first zone contains a small number of journals with the most influential articles, the second zone, a larger number of journals with fewer articles each, and so on. Observing how many journals fall into each zone can help in understanding the concentration or dispersion of research in the field. Table 5 reveals that the core area or Zone 1 consists of four journals which are: BMJ Open, Frontiers in Psychiatry, JMIR Mental Health and JMIR Research Protocols. It could be hence understood that these journals are the most significant and impactful journals in the current scenario (Figure 6).
RQ 4: Which are the most influential articles and authors in this domain?
Together with the overall count of publications and citations, Table 6 lists the leading authors in the domains of Digital Mental Health and Ethical Concerns. Grover S is the most productive author in terms of publications, having published four times. This could be due to the availability of good research infrastructure and funding in premier institutes. Alavi N. is the second most productive author in the field of Digital Mental healthcare (Figure 7).
The most often referenced works on Digital Mental Health and Ethical Concerns research are included in Table 7. Barak et al.’s (2009) work has received the greatest number of citations in Scopus (490), followed by Gorini et al., 2008 paper with 197 citations. Other impactful and influential areas of research, as indicated by the list of top-cited publications, include Ethical Issues in Online Psychotherapy (Stoll et al., 2020), Best Practices in Videoconferencing-Based Telemental Health (Shore et al., 2018), Online Counseling (Richards and Viganó, 2013).
RQ 5: How are the keywords in the field of Ethical Concerns and Mental Health Care clustered?
A key component of this work is the examination of publishing themes, which enables researchers to explore novel approaches to integrating two seemingly unrelated disciplines of study: Ethical Concerns and Digital Mental Healthcare. By examining keyword networks, researchers will be able to get relevant study themes and objects, offer clear distinctiveness, and enhance scientific knowledge. Figure 8 displays a TreeMap Visualization that provides a concise summary of the keywords that were identified throughout the research.
The TreeMap visualization from the bibliometric analysis presents a comprehensive overview of key terms related to the fields of digital mental health and ethical concerns. Each block represents a specific term, with its size indicating the frequency of its occurrence in the literature and the percentage indicating its proportion relative to other terms. Some of the key themes which emerged are described below: -.
Human (7%), Humans (5%). and Mental Health (7%) are the most prominent terms, indicating a strong focus on human-centric studies and mental health as primary subjects of research. Article (5%) suggest a broad engagement with these topics across various research articles, emphasizing an academic focus.
Telemedicine (4%) and Telepsychiatry (3%) highlight the growing relevance of remote treatment methods in mental health, reflecting increased attention to how these technologies meet the needs of patients. Videoconferencing (1%) and Telehealth (1%) further underscore the importance of technology in facilitating health care delivery and its ethical implications.
The terms Pandemic (3%), Coronavirus Disease 2019 (2%), and Covid-19 (2%) show the significant impact of the global health crisis on digital mental health research, guiding new ethical questions and research directions.
Medical Ethics (2%), Ethics (2%), and Privacy (1%) indicate crucial concerns in maintaining ethical standards and protecting patient privacy amid expanding digital health practices. Quality of Life (2%) reflects the outcome focus of many studies, measuring how digital health interventions affect overall well-being.
Adult (4%) and Adolescent (2%) suggest targeted research towards these age groups, possibly addressing different ethical concerns and digital health applications suitable for each.
Terms like Controlled Study (2%), Review (2%), and Major Clinical Study (1%) point to the methodologies employed to investigate these topics, indicating robust research efforts to evaluate and synthesize findings rigorously.
Artificial Intelligence (1%), Health Care Access (1%), and Social Media (1%) are indicative of newer areas of interest that are gaining traction within the broader theme of digital mental health.
The figure effectively illustrates the diverse yet interconnected aspects of research within digital mental health and ethical concerns, showing both broad thematic engagements and specific, targeted research areas. It also underscores the dynamic nature of this field, influenced heavily by technological advancements and societal shifts such as the COVID-19 pandemic.
This study examined publications about Ethical Concerns and Digital Mental Healthcare from 2000 to 2024 using bibliometric analysis. Considering the importance of maximising digital health care system efficacy to improve mental health (Lu et al., 2014) and uplift the psychological wellbeing (Taher et al., 2023; Neguț et al., 2016; Aboujaoude et al., 2020; Voinescu et al., 2023). The research to understand the potent ethical dilemmas and concerns faced across globe in digital healthcare is much needed. Present bibliometric study results revealed that the United States contributed considerably more than other nations or regions, as seen by the total publication and the total citations obtained by the countries which was followed by United Kingdom. The same could be understood from various research studies indicating introduction and free use of digital mental health services in the USA during pandemic. One of the studies conducted among American citizens revealed that an increased use of digital mental health applications was observed during the COVID-19 Pandemic in US (Sorkin et al., 2021). Also, in cities like New York City technologies supporting mental health were made freely available to their residents for their use, feedback and recommendations (NYCL Health). Alongside, Kaiser company created a digital mental health ecosystem contributing to the data generated on people’s satisfaction and concerns towards digital services (Mordecai et al., 2021). Queen’s University in USA is the core institution which is contributing for the field of Ethical Concerns and Digital Mental Health. Trend shows that there are more collaboration networks formed by developed nations than the developing or underdeveloped nations. Such as frequency of USA collaborating with India and Africa is more than India collaborating with USA. This shows lack of funds or resources in the developing or developed nations dedicated to the research in this field (Tomlinson, 2013; Cleary et al., 2019). Evidences show that collaborative research, especially in health, is often more efficient and impactful. To give an example during pandemic due to collaboration the process of vaccine development and delivery was expedited (Saenz et al., 2024).
The research focus has been changing from 2000 to 2024, with 2020–2024 being the peak time -period of researches done in this particular field. This trend is overall increasing in almost all field because of the introduction of advanced technologies which could help in research formulation, data collection and data analysis and report writing. This points to the rising importance of this certain field in the current era. The most cited paper was by Barak et al. (2009) which acted as foundation on which other papers have started their research. The paper talks about how the area of Internet-based therapeutic treatments has seen a dearth of coherence and uniformity (Taylor et al., 2021). The paper discusses that currently this sector is described as being scattered and unorganized due to a lack of professional leadership and recognized regulating concepts, vocabulary, professional standards, and procedures. This paper, thus presented guiding definitions and associated terminology for further study and development in this sector. In a similar way, the second most cited paper by Gorini A. titled “A Second life for eHealth: Prospects for the use of 3-D virtual worlds in clinical psychology” talks about the ethical considerations which should be kept in mind while implementing various digital health apps. These include intricate and interconnected issues pertaining to security, privacy, and confidentiality as well as licensure requirements, competency, standards of care, and reimbursement that practitioners, researchers, patients, healthcare organizations and state and federal legislators must be considered. Stoll et al. (2020) in his article talks about 24 ethical arguments in favor of online psychotherapy and 32 against the online therapies. The ethical arguments regarding the negative side of online therapies as extracted from multiple articles in which few include Privacy, Confidentiality, and Security Issues, Therapist Competence and Training, Communication Issues, Informed Consent Issues, Technological Competence, Absent or Incomplete Guidelines, Legal Issues, Payment and Insurance Issues, Therapeutic Relationship Issues, Identity and Verification Issues, Misuse and Harm, Increased Liability and Litigation, Negative Influence of Technology Use, Loss of Therapeutic Control, Patient Dependence and Loss of Control, Dehumanization and Stigmatization. With similar concern raised in several other researches (Wykes et al., 2019; Martinez-Martin et al., 2020; Terra et al., 2023).
Analysis involved using keywords to understand the trends following this area of research and it was seen that humans and mental health were the most prominent terms which indicates that a strong focus is placed on human-centric studies in the current scenario. Telemedicine, telepsychiatry, Videoconferencing and telehealth were also focused through these researches. There is overall spike in the use of distant mode health services world-wide (American Medical Association, 2019; Busch et al., 2021; Sugarman and Busch, 2023; Wosik et al., 2020). A noteworthy observation which should be made here is regarding the mention of pandemic which indicates the influence of pandemic in the development of the field of digital mental health though it was present before pandemic but its prevalence increased during pandemic with current rising trends (Barnett et al., 2021). Within the larger issue of digital mental health, Artificial Intelligence and Social Media. In terms of study methods, researches were mainly done using the methods of controlled study, review and clinical studies.
The ever-increasing demand for mental health support (Chaudhary et al., 2024; Cleary et al., 2019) is indicative of bright and convincing future of digital Mental healthcare services. However, this also brings out the pertinent ethical concerns discussed in the notable publications brought into light through this bibliometric analysis. Therefore, these scientific discourse across nations opens up the diverse scope of enlisting ethical concerns and guidelines to make wise judgments for operating in the best interests of the people accessing digital mental health support. The authors anticipate that through this study, a conversation might be stimulated among researchers and mental health professional on ethical concerns involving Digital Mental healthcare.
The findings of this study have significant implications for research, policy, and practice in digital mental health care. The underrepresentation of LMICs, including India, in the global discourse underscores the need for scalable, affordable, and contextually relevant digital mental health solutions tailored to socio-economic and cultural realities. Consistent with the ICMR Guidelines on AI and Digital Health, future research must emphasize inclusivity, exploring innovative, low-cost technologies that bridge existing gaps in accessibility and equity. Existing Guidelines like the ICMR Guidelines on AI and Digital Health and The IPS Telepsychiatry Operational Guidelines provide a foundational framework; however, their scope must be expanded to incorporate AI-driven interventions such as chatbots, digital phenotyping, and virtual reality therapies. Addressing ethical concerns, including data ownership, cross-border data sharing, and emergency response protocols, is imperative and should align with ICMR’s principles of ethical and secure data use. Furthermore, the absence of standardized metrics to evaluate the clinical and ethical efficacy of digital mental health tools necessitates the development of robust benchmarks in future research endeavors. Aligning national guidelines with global standards, such as the WHO Guidelines on Digital Health Interventions, is crucial to fostering international collaboration and ensuring consistency in ethical practices. Successful global models, such as New York City’s free mental health initiatives during the COVID-19 pandemic, provide actionable frameworks that can be adapted for LMICs, including India, while respecting local socio-cultural contexts.
The study relies on Scopus database for data collection, which may have excluded few of the relevant articles published in other repositories or non-indexed journals. Only articles published in English were analyzed, potentially overlooking significant research in other languages. Since, Bibliometric analysis emphasizes quantitative aspects, qualitative nuances of these issues would not be completely captured. Also, researches from LMICs, including India, may be underrepresented due to limited publication in indexed journals or disparities in research funding and infrastructure. Ethical concerns and dilemmas vary across regions and cultures, and the global scope of the analysis may not fully account for localized ethical challenges or priorities.
With first publication appearing in the year 2000, United States of America stands as the leading country followed by United Kingdom publishing in the field of Ethical concerns and mental health from 2000 to 2024. BMJ Open is noted as the foremost journal with 18 publications, followed by Frontiers in Psychiatry and JMIR Mental Health. Analyses reflects that the top cited articles on Digital Mental healthcare are specifically directed on bringing out some of the key concerns of data privacy, emergency response, therapist competency and consent. The ever-increasing demand for Online Mental healthcare specifies on making wise judgments and operating in patients’ best interests. Psychologists from various professional backgrounds need to be well aware on the ethical concerns surrounding online mental healthcare systems. The authors anticipate that through this study, a conversation might be stimulated among researchers on ethical concerns involving Digital Mental healthcare.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
PS: Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis, Investigation, Methodology, Software, Visualization. RW: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. MV: Data curation, Formal analysis, Investigation, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that Generative AI was used in the creation of this manuscript. AI is used to have simplified understanding of the various concepts related to bibliometric analysis and understand the related steps. To get concise summary of some articles for building up the introduction section AI is used.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fhumd.2024.1502432/full#supplementary-material
Aboujaoude, E., Gega, L., Parish, M. B., and Hilty, D. M. (2020). Editorial: digital interventions in mental health: current status and future directions. Front. Psychol. 11:111. doi: 10.3389/fpsyt.2020.00111
Ackerman, M. L., Virani, T., and Billings, B. (2017). Digital mental health - innovations in consumer driven care. Nurs. Leadersh. (Tor. Ont) 30, 63–72. doi: 10.12927/CJNL.2018.25384
Ahmed, A., Ali, N., Aziz, S., Abd-alrazaq, A. A., Hassan, A., Khalifa, M., et al. (2021). A review of Mobile Chatbot apps for anxiety and depression and their self-care features. Comp. Methods Prog. Biomed. Update 1:100012. doi: 10.1016/j.cmpbup.2021.100012
American Medical Association (2019). Telehealth implementation playbook. Available at: https://www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.(Accessed September 25, 2020).
Andersson, G., Titov, N., Dear, B. F., Rozental, A., and Carlbring, P. (2019). Internet-delivered psychological treatments: from innovation to implementation. World Psychiatry 18, 20–28. doi: 10.1002/wps.20610
Apolinário-Hagen, J., Drüge, M., and Fritsche, L. (2020). Cognitive Behavioral therapy, mindfulness-based cognitive therapy and acceptance commitment therapy for anxiety disorders: integrating traditional with digital treatment approaches. Adv. Exp. Med. Biol. 1191, 291–329. doi: 10.1007/978-981-32-9705-0_17
Arias, D., Saxena, S., and Verguet, S. (2022). Quantifying the global burden of mental disorders and their economic value. EClinicalMedicine 54:101675. doi: 10.1016/J.ECLINM.2022.101675
Balcombe, L., and De Leo, D. (2021). Digital mental health challenges and the horizon ahead for solutions. JMIR Mental Health 8:e26811. doi: 10.2196/26811
Barak, A., Klein, B., and Proudfoot, J. G. (2009). Defining internet-supported therapeutic interventions. Ann. Behav. Med. 38, 4–17. doi: 10.1007/s12160-009-9130-7
Barnett, M. L., Huskamp, H. A., Busch, A. B., Uscher-Pines, L., Chaiyachati, K. H., and Mehrotra, A. (2021). Trends in outpatient telemedicine utilization among rural Medicare beneficiaries, 2010 to 2019. JAMA Health Forum 2:e213282. doi: 10.1001/jamahealthforum.2021.3282
Bell, I. H., Pot-Kolder, R., Rizzo, A., Rus-Calafell, M., Cardi, V., Cella, M., et al. (2024). Advances in the use of virtual reality to treat mental health conditions. Nat. Rev. Psychol. 3, 552–567. doi: 10.1038/s44159-024-00334-9
Bucci, S., Schwannauer, M., and Berry, N. (2019). The digital revolution and its impact on mental health care. Psychol. Psychother. Theory Res. Pract. 92, 277–297. doi: 10.1111/papt.12222
Busch, A. B., Sugarman, D. E., Horvitz, L. E., and Greenfield, S. F. (2021). Telemedicine for treating mental health and substance use disorders: reflections since the pandemic. Neuropsychopharmacology 46, 1068–1070. doi: 10.1038/s41386-021-00960-4
Carlo, F. D., Antonella, S., Elena, P., Mauro, P., Federica, V., Valeria, V, et al. (2021). Telepsychiatry and Other Cutting-Edge Technologies in COVID-19 Pandemic: Bridging the Distance in Mental Health Assistance. Int. J. Clin. Pract. 75. doi: 10.1111/IJCP.13716
Chandra, P. S., Shiva, L., and Nanjundaswamy, M. H. (2018). The impact of urbanization on mental health in India. Curr. Opin. Psychiatry 31, 276–281. doi: 10.1097/YCO.0000000000000408
Chaudhary, S., Hoffmann, J. A., Pulcini, C. D., Zamani, M., Hall, M., Jeffries, K. N., et al. (2024). Youth suicide and preceding mental health diagnosis. JAMA Netw. Open 7:e2423996. doi: 10.1001/jamanetworkopen.2024.23996
Chen, Q., Huang, S., Xu, H., Peng, J., Wang, P., Li, S., et al. (2024). The burden of mental disorders in Asian countries, 1990–2019: an analysis for the global burden of disease study 2019. Transl. Psychiatry 14, 1–11. doi: 10.1038/s41398-024-02864-5
Chokshi, M., Patil, B., Khanna, R., Neogi, S. B., Sharma, J., Paul, V. K., et al. (2016). Health Systems in India. J. Perinatol. 36, S9–S12. doi: 10.1038/JP.2016.184
Cleary, M., PhD,, West, S. RN, PhD,, Arthur, D. RN, PhD,, et al. (2019). Change Management in Health Care and Mental Health Nursing. Issues Ment. Health Nurs. 40, 966–972. doi: 10.1080/01612840.2019.1609633
Cornet, V. P., and Holden, R. J. (2018). Systematic review of smartphone-based passive sensing for health and wellbeing. J. Biomed. Inform. 77, 120–132. doi: 10.1016/J.JBI.2017.12.008
Diel, A., Schröter, I. C., Frewer, A.-L., Jansen, C., Robitzsch, A., Gradl-Dietsch, G., et al. (2024). A systematic review and meta analysis on digital mental health interventions in inpatient settings. Digit. Med. 7, 1–9. doi: 10.1038/s41746-024-01252-z
Donthu, N., Kumar, S., Mukherjee, D., Pandey, N., and Lim, W. M. (2021). How to conduct a bibliometric analysis: an overview and guidelines. J. Bus. Res. 133, 285–296. doi: 10.1016/j.jbusres.2021.04.070
Fiske, A., Peter, H., and Alena, B. (2019). Your Robot Therapist Will See You Now: Ethical Implications of Embodied Artificial Intelligence in Psychiatry, Psychology, and Psychotherapy. J. Med. Internet Res. 21: e13216. doi: 10.2196/13216
Gooding, P., and Kariotis, T. (2021). Ethics and law in research on algorithmic and data-driven Technology in Mental Health Care: scoping review. JMIR Mental Health 8:e24668. doi: 10.2196/24668
Gorini, A., Gaggioli, A., Vigna, C., and Riva, G. (2008). A second life for EHealth: prospects for the use of 3-D virtual worlds in clinical psychology. J. Med. Internet Res. 10:e21. doi: 10.2196/jmir.1029
Hirschtritt, M. E., and Insel, T. R. (2018). Digital Technologies in Psychiatry: present and future. Focus 16, 251–258. doi: 10.1176/appi.focus.20180001
Hossain, M., and Purohit, N. (2019). Improving child and adolescent mental health in India: status, services, policies, and way forward. Indian J. Psychiatry 61, 415–419. doi: 10.4103/psychiatry.IndianJPsychiatry_217_18
Isaak, J., and Hanna, M. J. (2018). User data privacy: Facebook, Cambridge Analytica, and privacy protection. Computer 51, 56–59. doi: 10.1109/MC.2018.3191268
Lu, S. H., Titov, N., Dear, B. F., Johnston, L., and Wootton, B. (2014). An internet survey of emotional health, treatment seeking and barriers to accessing mental health treatment among Chinese-speaking international students in Australia. Couns. Psychol. Q. 27, 96–108. doi: 10.1080/09515070.2013.824408
Maples-Keller, J. L., Yasinski, C., Manjin, N., and Rothbaum, B. O. (2017). Virtual reality-enhanced extinction of phobias and post-traumatic stress. Neurotherapeutics 14, 554–563. doi: 10.1007/s13311-017-0534-y
Martinez-Martin, N., Dasgupta, I., Carter, A., Chandler, J. A., Kellmeyer, P., Kreitmair, K., et al. (2020). Ethics of digital mental health during COVID-19: crisis and opportunities. JMIR Mental Health 7:e23776. doi: 10.2196/23776
Martinez-Martin, N., and Karola, K. (2018). Ethical Issues for Direct-to-Consumer Digital Psychotherapy Apps: Addressing Accountability, Data Protection, and Consent. JMIR Mental Health. 5. doi: 10.2196/MENTAL.9423
McDaid, D., Knapp, M., and Raja, S. (2008). Barriers in the mind: promoting an economic case for mental health in low- and middle-income countries. World Psychiatry 7, 79–86. doi: 10.1002/j.2051-5545.2008.tb00160.x
Mental Health, Brain Health and Substance Use (n.d.). Available at: https://www.who.int/teams/mental-health-and-substance-use/promotion-prevention/mental-health-in-the-workplace (Accessed December 14, 2024).
Meyerhoff, J., Kruzan, K. P., Kim, K.-Y., Van Orden, K., and Mohr, D. C. (2023). Exploring the safety of a general digital mental health intervention to effect symptom reduction among individuals with and without suicidal ideation: a secondary analysis. Arch. Suicide Res. 27, 966–983. doi: 10.1080/13811118.2022.2096520
Mordecai, D., Histon, T., Neuwirth, E., Heisler, W. S., Kraft, A., Bang, Y., et al. (2021). How Kaiser Permanente created a mental health and wellness digital ecosystem. NEJM Catalyst 2:1. doi: 10.1056/CAT.20.0295
Naslund, J. A., Aschbrenner, K. A., Araya, R., Marsch, L. A., Unützer, J., Patel, V., et al. (2017). Digital Technology for Treating and Preventing Mental Disorders in low-income and middle-income countries: a narrative review of the literature. Lancet Psychiatry 4, 486–500. doi: 10.1016/S2215-0366(17)30096-2
Neguț, A., Matu, S. A., Sava, F. A., and David, D. (2016). Virtual reality measures in neuropsychological assessment: a meta-analytic review. Neuropsychol. Dev. Cogn. Sectio. D Clin. Neuropsychol. 30, 165–184. doi: 10.1080/13854046.2016.1144793
Nochaiwong, S., Ruengorn, C., Thavorn, K., Hutton, B., Awiphan, R., Phosuya, C., et al. (2021). Global prevalence of mental health issues among the general population during the coronavirus Disease-2019 pandemic: a systematic review and meta-analysis. Sci. Rep. 11:10173. doi: 10.1038/S41598-021-89700-8
Rebello, T. J., Marques, A., Gureje, O., and Pike, K. M. (2014). Innovative strategies for closing the mental health treatment gap globally. Curr. Opin. Psychiatry 27, 308–314. doi: 10.1097/YCO.0000000000000068
Richards, D., and Viganó, N. (2013). Online Counseling: a narrative and critical review of the literature. J. Clin. Psychol. 69, 994–1011. doi: 10.1002/jclp.21974
Sabin, J. E., and Jonathan, C. H. (2017). Professional Ethics for Digital Age Psychiatry: Boundaries, Privacy, and Communication. Curr. Psychiatry Rep. 19: 1–7. doi: 10.1007/S11920-017-0815-5/METRICS
Saenz, C., Krahn, T. M., Smith, M. J., Haby, M. M., Carracedo, S., and Reveiz, L. (2024). Advancing collaborative research for health: why does collaboration matter? BMJ Glob. Health 9:e014971. doi: 10.1136/bmjgh-2024-014971
Sagar, R., Dandona, R., Gopalkrishna Gururaj, R. S., Dhaliwal, A. S., Ferrari, A., Dua, T., et al. (2020). The burden of mental disorders across the states of India: the global burden of disease study 1990–2017. Lancet Psychiatry 7, 148–161. doi: 10.1016/S2215-0366(19)30475-4
Sagar, R., and Singh, S. (2022). National Tele-Mental Health Program in India: a step towards mental health Care for all? Indian J. Psychiatry 64, 117–119. doi: 10.4103/indianjpsychiatry.indianjpsychiatry_145_22
Schueller, S. M., Glover, A. C., Rufa, A. K., Dowdle, C. L., Gross, G. D., Karnik, N. S., et al. (2019). A mobile phone–based intervention to improve mental health among homeless young adults: pilot feasibility trial. JMIR Mhealth Uhealth 7:e12347. doi: 10.2196/12347
Shore, J. H., Hilty, D. M., and Yellowlees, P. (2007). Emergency management guidelines for telepsychiatry. Gen. Hosp. Psychiatry 29, 199–206. doi: 10.1016/j.genhosppsych.2007.01.013
Shore, J. H., Yellowlees, P., Caudill, R., Johnston, B., Turvey, C., Mishkind, M., et al. (2018). Best practices in videoconferencing-based Telemental health April 2018. Telemed. E-Health 24, 827–832. doi: 10.1089/tmj.2018.0237
Sorkin, D. H., Janio, E. A., Eikey, E. V., Schneider, M., Davis, K., Schueller, S. M., et al. (2021). Rise in use of digital mental health tools and Technologies in the United States during the COVID-19 pandemic: survey study. J. Med. Internet Res. 23:e26994. doi: 10.2196/26994
Sousa, A. D., Mohandas, E., and Afzal, J. (2020). Psychological Interventions during COVID-19: Challenges for Low and Middle Income Countries. Asian J Psychiatr 51. doi: 10.1016/J.AJP.2020.102128
Stoll, J., Müller, J. A., and Trachsel, M. (2020). Ethical issues in online psychotherapy: a narrative review. Front. Psychol. 10:993. doi: 10.3389/fpsyt.2019.00993
Sugarman, D. E., and Busch, A. B. (2023). Telemental health for clinical assessment and treatment. BMJ 380:e072398. doi: 10.1136/bmj-2022-072398
Taher, R., Hsu, C. W., Hampshire, C., Fialho, C., Heaysman, C., Stahl, D., et al. (2023). The safety of digital mental health interventions: systematic review and recommendations. JMIR Mental Health 10:e47433. doi: 10.2196/47433
Taylor, C. B. R., Graham, A. K., Flatt, R. E., Waldherr, K., and Fitzsimmons-Craft, E. E. (2021). Current state of scientific evidence on internet-based interventions for the treatment of depression, anxiety, eating disorders, and substance abuse: an overview of systematic reviews and meta-analyses. Eur. J. Pub. Health 31, i3–i10. doi: 10.1093/eurpub/ckz208
Terra, M., Baklola, M., Ali, S., and El-Bastawisy, K. (2023). Opportunities, applications, challenges and ethical implications of artificial intelligence in psychiatry: a narrative review. Egyp. J. Neurol. Psychiatry Neurosurg. 59, 1–10. doi: 10.1186/S41983-023-00681-Z/TABLES/5
Tomlinson, M. (2013). Global mental health: a sustainable post millennium development goal? Int. Health 5, 1–3. doi: 10.1093/inthealth/iht001
Torous, J., Myrick, K. J., Rauseo-Ricupero, N., and Firth, J. (2020). Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Mental Health 7:e18848:e18848. doi: 10.2196/18848
Voinescu, A., Petrini, K., Stanton Fraser, D., Lazarovicz, R. A., Papavă, I., and Fodor, L. A. (2023). The effectiveness of a virtual reality attention task to predict depression and anxiety in comparison with current clinical measures. Virtual Reality 27, 119–140. doi: 10.1007/s10055-021-00520-7
De Vos, J. (2021). A Critique of Digital Mental Health via Assessing the Psychodigitalisation of the COVID-19 Crisis. Psychotherapy and Politics International. 19:e1582. doi: 10.1002/PPI.1582
Wies, B., Landers, C., and Ienca, M. (2021). Digital mental health for young people: a scoping review of ethical promises and challenges. Front. Digit. Health 3:697072. doi: 10.3389/fdgth.2021.697072
Wosik, J., Fudim, M., Cameron, B., Gellad, Z. F., Cho, A., Phinney, D., et al. (2020). Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 27, 957–962. doi: 10.1093/jamia/ocaa067
Keywords: digital mental healthcare, ethical dilemmas, bibliometric analysis, online psychotherapy and counselling, Telemental health
Citation: Sharma P, Wagani R and Varghese MA (2025) Bibliometric analysis of research in ethical concerns and dilemmas of digital mental health care in the last two decades. Front. Hum. Dyn. 6:1502432. doi: 10.3389/fhumd.2024.1502432
Received: 26 September 2024; Accepted: 24 December 2024;
Published: 29 January 2025.
Edited by:
Apurvakumar Pandya, Indian Institute of Public Health Gandhinagar (IIPHG), IndiaReviewed by:
Nongzaimayum Tawfeeq Alee, Gandhi Institute of Technology and Management (GITAM), IndiaCopyright © 2025 Sharma, Wagani and Varghese. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Poonam Sharma, ZHJwb29uYW1zaGFybWExODlAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.