
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Hum. Dyn. , 10 June 2022
Sec. Migration and Society
Volume 4 - 2022 | https://doi.org/10.3389/fhumd.2022.778592
This article is part of the Research Topic Women's Empowerment, Migration and Health View all 9 articles
 Brian D. Earp1,2,3*
Brian D. Earp1,2,3*The World Health Organization (WHO) condemns all medically unnecessary female genital cutting (FGC) that is primarily associated with people of color and the Global South, claiming that such FGC violates the human right to bodily integrity regardless of harm-level, degree of medicalization, or consent. However, the WHO does not condemn medically unnecessary FGC that is primarily associated with Western culture, such as elective labiaplasty or genital piercing, even when performed by non-medical practitioners (e.g., body artists) or on adolescent girls. Nor does it campaign against any form of medically unnecessary intersex genital cutting (IGC) or male genital cutting (MGC), including forms that are non-consensual or comparably harmful to some types of FGC. These and other apparent inconsistencies risk undermining the perceived authority of the WHO to pronounce on human rights. This paper considers whether the WHO could justify its selective condemnation of non-Western-associated FGC by appealing to the distinctive role of such practices in upholding patriarchal gender systems and furthering sex-based discrimination against women and girls. The paper argues that such a justification would not succeed. To the contrary, dismantling patriarchal power structures and reducing sex-based discrimination in FGC-practicing societies requires principled opposition to medically unnecessary, non-consensual genital cutting of all vulnerable persons, including insufficiently autonomous children, irrespective of their sex traits or socially assigned gender. This conclusion is based, in part, on an assessment of the overlapping and often mutually reinforcing roles of different types of child genital cutting—FGC, MGC, and IGC—in reproducing oppressive gender systems. These systems, in turn, tend to subordinate women and girls as well as non-dominant males and sexual and gender minorities. The selective efforts of the WHO to eliminate only non-Western-associated FGC exposes the organization to credible accusations of racism and cultural imperialism and paradoxically undermines its own stated goals: namely, securing the long-term interests and equal rights of women and girls in FGC-practicing societies.
Female, male, and intersex forms of non-therapeutic child genital cutting—so-called “gendered genital modifications” (Fusaschi, 2022)—tend to be discussed and evaluated separately, both in scholarly and popular discourses. It is increasingly recognized, however, that despite various differences between them, the practices also share certain features that render this tendency toward discursive separation questionable on several grounds. Scientifically, the tendency is questionable because in many countries at least two, and sometimes all three, forms of cutting are carried out together within the same cultural contexts or institutions; in these cases, the practices are often tightly symbolically linked, serving complementary or mutually reinforcing social functions. These functions—for example, maintaining gendered social divisions and associated power hierarchies—cannot adequately be understood, much less appropriately addressed, by studying each practice in isolation (Caldwell et al., 1997; Junos, 1998; Toubia, 1999; Lightfoot-Klein et al., 2000; Abu-Sahlieh, 2001; Knight, 2001; Robertson and James, 2002; Boddy, 2007; Merli, 2008, 2010; Fox and Thomson, 2009; Androus, 2013; Reis, 2013; Svoboda, 2013; Ahmadu, 2016a; Prazak, 2017; Johnsdotter, 2018; Earp, 2020a).
Legally, the tendency is questionable because it may lead to discriminatory treatment of different persons or groups based on constitutionally forbidden criteria, such as sex, gender, race, religion, ethnicity, or national origin (Coleman, 1998; Bond, 1999; Price, 1999; Davis, 2001; Mason, 2001; Somerville, 2004; Dustin, 2010; Johnsdotter and Essén, 2010; Askola, 2011; Adler, 2012; Merkel and Putzke, 2013; Fusaschi, 2015; Arora and Jacobs, 2016; Rogers, 2016, 2022; Svoboda et al., 2016; Earp et al., 2017; La Barbera, 2017; Shahvisi, 2017; Munzer, 2018; Notini and Earp, 2018; Pardy et al., 2019; Möller, 2020; Carpenter, 2021; Ahmadu and Kamau, 2022; Bootwala, 2022; Earp, 2022a; Rosman, 2022; Shweder, 2022b). And ethically, the tendency is questionable because, in practice, it privileges the customs of more powerful stakeholders (Gunning, 1991; Lewis, 1995; Obiora, 1996; Tangwa, 1999, 2004; Toubia, 1999; Androus, 2004, 2013; Chambers, 2004; Njambi, 2004; Bell, 2005; Ehrenreich and Barr, 2005; Shweder, 2005; Oba, 2008; Boddy, 2016, 2020; Ahmadu, 2017; Onsongo, 2017; Coene, 2018; Kart, 2020; MacNamara et al., 2020; Shahvisi, 2021), while also occluding overlapping moral concerns about the different forms of child genital cutting (Davis, 2003; Hellsten, 2004; Svoboda and Darby, 2008; van den Brink and Tigchelaar, 2012; Antinuk, 2013; Shweder, 2013; Svoboda, 2013; Earp, 2015b, 2020b; Shahvisi, 2016; Jones, 2017; Carpenter, 2018a; O'Donnell and Hodes, 2018; Lunde et al., 2020; O'Neill et al., 2020; Sarajlic, 2020; Townsend, 2020, 2022; Reis-Dennis and Reis, 2021). This moral occlusion leads to incoherent, unjust, and often ineffective or harmful social policies, which may further disadvantage the very groups that are meant to be helped (Coleman, 1998; Gruenbaum, 2001; Manderson, 2004; Berer, 2010, 2015; Johnson, 2010; Evans, 2011; Abdulcadir et al., 2012; Aktor, 2016; Latham, 2016; Johnsdotter, 2019; Karlsen et al., 2019, 2020, 2022; Sandland, 2019; Earp and Johnsdotter, 2021; Hehir, 2022; Johnsdotter and Wendel, 2022).
In response to these concerns, scholars of genital cutting have increasingly undertaken a more comprehensive, cross-cultural and cross-sex comparative approach, particularly in the last several years. For example, in a recent publication, a large group of scholars from diverse countries, cultures, and disciplinary backgrounds highlighted the following shared aspects of non-therapeutic female, male, and intersex child genital cutting (FGC, MGC, and IGC, respectively), that seemed to them to be morally—and perhaps also legally—relevant:
they are all (1) medically unnecessary acts of (2) genital cutting that are (3) overwhelmingly performed on young children (4) on behalf of norms, beliefs, or values that may not be the child's own and which the child may not adopt when of age. Indeed, such norms, beliefs, or values are often controversial in the wider society and hence prone to reevaluation upon later reflection or exposure to other points of view (e.g., the belief that a child's body must conform to a strict gender binary; that surgery is an appropriate means of pursuing hygiene; that one's genitals must be symbolically purified before one can be fully accepted; and so on). In this, they constitute painful intrusions into the “private parts” of the most vulnerable members of society, despite being [of] contested value overall (BCBI, 2019) (p. 21).
Nevertheless, despite such similarities, there has been considerable resistance among policymakers, legislators, international health agencies, and other key actors—especially those situated in or led from within the Global North—to evaluate these practices together. This resistance has been strongest in response to proposals to treat FGC and MGC together, so it is this comparison, along with common objections to it, that will serve as the primary focus of this paper.1
Why has there been such resistance to comparing female and male forms of child genital cutting? There are several potential explanations. As I discuss near the end of the paper, a partial explanation stems from sociological factors having to do with which countries or cultures predominately practice each form of genital cutting, and which of these countries or cultures have more “bargaining power”—for example, in determining what counts as a human rights violation—in the relevant spheres of influence (Tangwa, 1999; Njambi, 2004; Shweder, 2005; Oba, 2008; Carpenter, 2014; Latham, 2016; Onsongo, 2017). As Nahid Toubia has argued, at least one important difference between FGC and MGC is that “the female procedure is primarily carried out in Africa, which is currently the least dominant culture in the world. The male procedure is also common in the same countries, but it is also common in the United States, which is currently the most dominant culture in the world through its far-reaching media machine. This historical situation has made it easier to vilify and condemn what is common in Africa and sanctify what is popular in America” (Toubia, 1999) (p. 5).
This would suggest that reasons having to do with geopolitics and power are key to understanding what medical historian Robert Darby has described as “our habit of placing male and female genital cutting in separate ethical boxes” (Darby, 2016) (p. 155). However, there may also be principled reasons for treating the practices differently that could justify such separation. In this vein, there have been two main strategies for rejecting any moral comparison between FGC and MGC of children. The first has been to argue that the practices are highly distinct from one another in terms of typical health outcomes, whether considering physical or psychosexual harms or benefits. For example, according to the World Health Organization (WHO), in contrast to FGC, which “has no known health benefits [but] is known to be harmful to girls and women in many ways,” MGC, in the form of penile circumcision, “has significant health benefits that outweigh the very low risk of complications when performed by adequately-equipped and well-trained providers in hygienic settings” (WHO, 2008) (p. 1 and 11).
The second main strategy has been to argue that, even if the health outcomes were similar in certain respects, there would still be an important moral difference between the practices in terms of their underlying intent, social functions, cultural associations, or symbolic meanings. According to the WHO, again: “Communities that practice female genital mutilation report a variety of social and religious reasons for continuing with it.” However, “as seen from a human rights perspective, the practice reflects deep-rooted inequality between the sexes, and constitutes an extreme form of discrimination against women” (WHO, 2008) (p. 1). MGC, by contrast, is generally not thought to constitute sex-based discrimination, whether against women and girls or indeed against men and boys. It is therefore not seen as conflicting with human rights (here, the right not to be discriminated against on account of one's sex or gender).
In the first part of this paper, I respond to the “health outcomes” argument of the WHO, showing that the alleged or purported differences in health benefits vs. harms—even if they are simply granted—cannot justify the current, categorically different treatment of the two types of genital cutting, especially as performed on non-consenting minors. This part of the paper will be comparatively brief, however, as I have previously addressed the health-based argument elsewhere (most recently in Earp, 2021a).
In the second part of the paper, I respond to the argument that, while FGC discriminates against women and girls, reflecting their lower status in society, MGC does not share these objectionable features. Instead, it is often said, MGC actually reflects the higher status of boys and men, practically and symbolically elevating them into positions of power (Dorkenoo, 1994).
I first raise some empirical concerns about the scope or generalizability of these claims, arguing that, while they may apply in some cases or along certain dimensions, they do not apply universally. Instead, it is necessary to take a more culture-relative and context-sensitive approach to understanding these ritual practices (Leonard, 2000a; Wade, 2012). Then, simply granting the claimed difference between MGC and FGC in relation to status or power, I reflect on the moral and political implications of this claim. I argue that, even if it is granted that the primary function of MGC in some communities is to “elevate” boys into powerful men, this would not, from the perspective of disrupting gendered socialization processes that oppress and subordinate women and girls, constitute a reason to ignore the male rite while seeking only to eliminate the female rite. It would, instead, constitute a compelling reason to (also) oppose the male rite.
As I aim to demonstrate, boys in many cultures are only “elevated” in the above-described sense if they successfully prove their masculinity in accordance with overtly patriarchal standards: in other words, the power that they may gain through these rites is typically power over women and girls (Junos, 1998). Insofar as that is a common effect or purpose of MGC, this should make the rite more concerning, not less concerning, from the perspective of seeking to promote women's and girls' flourishing and equal rights.
However, in patriarchal cultures, MGC and associated norms do not only contribute to the ongoing subordination of women and girls. As I argue, they also subordinate males who are perceived to be insufficiently masculine, including gay men and non-circumcised boys. These boys often face severe social mistreatment including ostracization unless they submit to a risky and painful genital cutting procedure (WHO, 2009).2 Moreover, in societies where MGC, but not FGC, is practiced and regarded as legal, boys face distinctive challenges. Although almost every society that practices FGC also practices MGC in tandem—meaning that girls are not singled out for genital cutting—the inverse is not true. Instead, there are many societies that ritually cut the genitals only of boys, precisely on account of their gender (Cohen, 1997, 2022; DeMeo, 1997; Abdulcadir et al., 2012). Insofar as being subjected to a medically unnecessary, non-consensual act of genital cutting is a moral violation in its own right, boys in these societies are discriminated against in the sense that, due to their gender, only they lack legal protection from such cutting (Möller, 2020).
Of course, there need not be a choice between opposing either FGC or MGC. Rather, a focus on children's rights could motivate campaigns against all non-consensual, medically unnecessary genital cutting of minors—female, male, or intersex—aimed at protecting the most vulnerable members of society on a non-discriminatory basis from adult interference with their sexual anatomy (Junos, 1998; Svoboda, 2013; Earp and Steinfeld, 2017; Townsend, 2022). In fact, given the symbolic and functional linkages between FGC and MGC in societies that practice both together—sometimes also alongside IGC; see Box 1—such a conjoined effort may be necessary for the successful abandonment of either (Abu-Sahlieh, 1994; Martí, 2010; Prazak, 2017; Šaffa et al., 2022).
Box 1. The role of intersex genital cutting in upholding patriarchal gender systems
How does intersex genital cutting (IGC) relate to patriarchal gender systems? On classic models, patriarchy requires socialization of persons into dichotomous gender roles, with a clear distinction between (dominant) men and (subordinated) women, and thus between male and female bodies. Because IGC attempts to surgically remove signs of sexual ambiguity, it is, on this view, strongly implicated in patriarchal social formations, laying the “physical” groundwork for an oppressive gender binary (Hird, 2000; Ehrenreich and Barr, 2005; Reis, 2009). This may have policy implications. As this paper suggests, the WHO opposes “FGM,” not only on the grounds that it involves medically unnecessary genital cutting, typically of a pre-autonomous minor, but also because it upholds oppressive gender norms that disadvantage women and girls. If that is correct, then, for the sake of consistency in promoting its own aims, the WHO should also campaign against IGC (i.e., as a means of resisting gender oppression). IGC does not only indirectly contribute to gender-based oppression of women and girls, however. According to advocates for intersex rights, it also directly, indeed violently, oppresses persons with intersex traits, including intersex males, intersex females, and persons whose bodies or identities confound such binary classification altogether (Chase, 1998; Dreger, 1999; Reis, 2009, 2019; Carpenter, 2016, 2018b; Viloria, 2017).
The take-home message of the paper is this: regardless of one's position on the role of FGC in socially subordinating women and girls, MGC rites in the same and other societies (also) uphold patriarchal power structures. Indeed, as I will argue, in many contexts, the genital cutting of boys and associated rituals are in fact central cultural mechanisms by which female-oppressive gender norms are reinforced in each generation. Thus, if a desire to contest such norms is at the heart of global campaigns to eliminate FGC, then, insofar as these campaigns are justified, it may be equally important, if not more important, for them to target MGC as well.
I proceed as follows. I first map out, in more detail, the various moral and conceptual inconsistencies that have been identified within the WHO's policies on genital cutting. I then address possible justifications of these inconsistencies, based on allegedly different health-related outcomes as well as divergent social functions or symbolic meanings. I then describe how MGC in many societies socializes boys to become “real men” (Dembroff, 2022) in accordance with patriarchal ideology. For the purposes of this paper, patriarchy refers to a social system within which males, in particular those who are interpreted as fulfilling locally normative expectations of masculinity—so-called “real men”—disproportionately occupy positions of power and privilege across multiple domains. Moreover, these men maintain their dominant status through structural oppression of females as well as non-dominant males (e.g., males who are subordinately racialized, disabled, or perceived to be of a lower class; young or effeminate boys, and so on) and likewise gender and sexual minorities (e.g., gay or transgender persons): all “not real men” according to this ideology (Dembroff, 2022). I conclude by discussing the work of Egyptian feminist Seham Abd el Salam, who argues that selective condemnation of FGC—while ignoring or promoting MGC—represents a political “bargain” with conservative patriarchal forces, given that, in her view, MGC is a distinctly powerful means of upholding men's dominance in society (Abd el Salam, 1999).
For decades, scholars have called attention to troubling inconsistencies in the WHO's policies on medically unnecessary3 genital cutting practices, especially those imposed on children (Junos, 1998; Toubia, 1999; Lightfoot-Klein et al., 2000; Ehrenreich and Barr, 2005; Oba, 2008; Svoboda and Darby, 2008; DeLaet, 2009; Askola, 2011; van den Brink and Tigchelaar, 2012; Svoboda, 2013; Coene, 2018; Johnsdotter, 2018; Sandland, 2019). The WHO conceptualizes “female genital mutilation” (FGM) as all non-therapeutic cutting, however slight, of the external genitalia of (non-intersex)4 females—irrespective of the individual's consent—and categorically condemns such cutting as a violation of the human right to bodily integrity. However, the WHO has exclusively sought to eliminate medically unnecessary female genital cutting (FGC) practices that are customary in parts of the Global South, while ignoring comparable practices that are common in the Global North, such as elective labiaplasty (see Table 1) which is increasingly performed on adolescent girls (Liao et al., 2012; Runacres and Wood, 2016; Boddy, 2020).
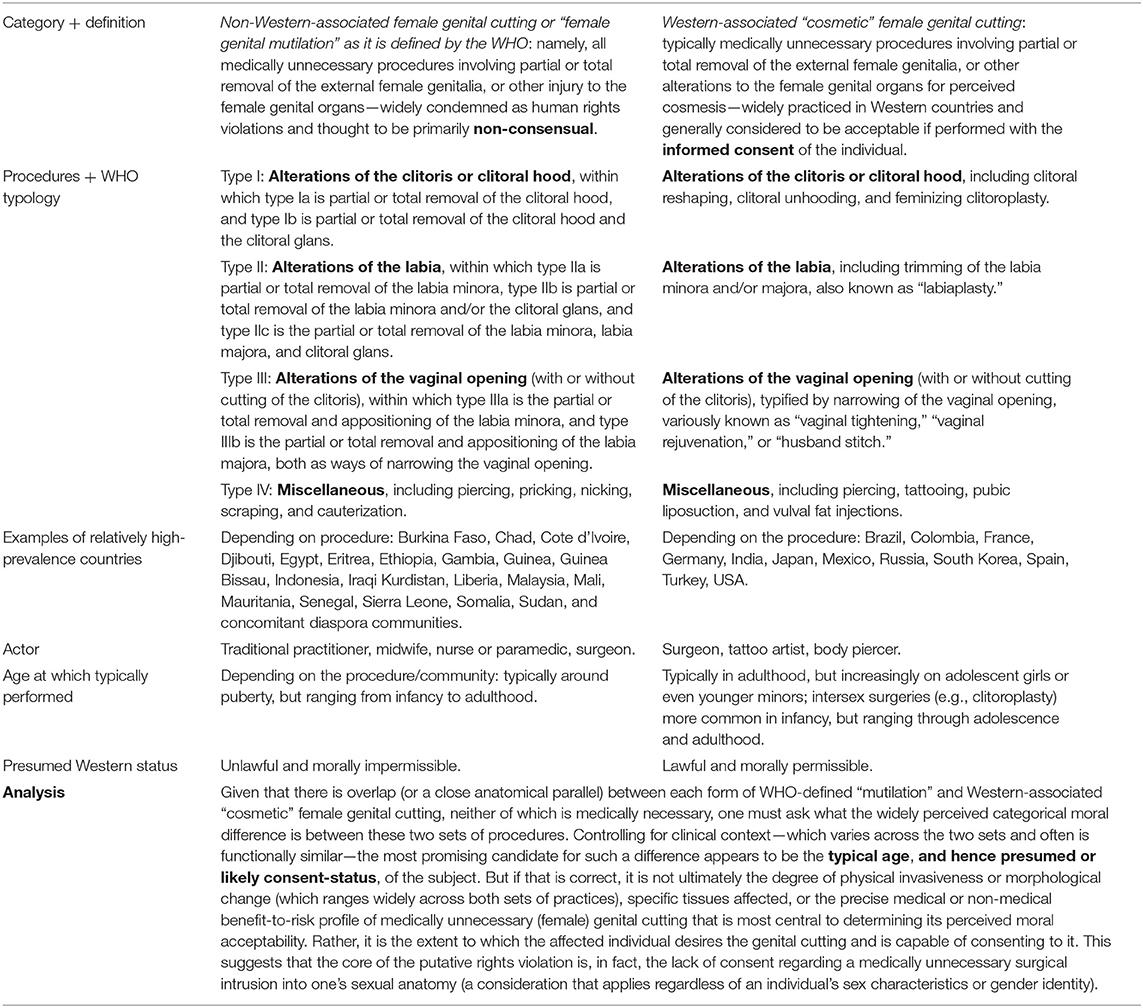
Table 1. Non-Western-associated female genital “mutilation” (Global South) vs. Western-associated “cosmetic” female genital cutting (Global North); adapted from BCBI (2019) and Shahvisi and Earp (2019); internal references ommitted.
Numerous scholars have argued that this selective focus reflects moral double standards rooted in racism and cultural imperialism (Gunning, 1991; Obiora, 1996; Tangwa, 1999; Ahmadu, 2000, 2007, 2016b; Mason, 2001; Shweder, 2002, 2013; Njambi, 2004; Ehrenreich and Barr, 2005; Oba, 2008; Dustin, 2010; Smith, 2011; Kelly and Foster, 2012; Boddy, 2016, 2020; Onsongo, 2017; Shahvisi, 2017, 2021; Shahvisi and Earp, 2019). Some have therefore called on the WHO to revise its policy: either by including Western-associated5 so-called “cosmetic” female genital surgeries in the campaign against “FGM” (Esho, 2022), or by establishing an age limit or consent criterion for FGC to be applied without discrimination or favor (Dustin, 2010; Shahvisi, 2021). According to this latter approach, self-affecting FGC requested by legally competent adult women or sufficiently mature (e.g., Gillick-competent)6 minors would in principle be allowed (assuming certain conditions are met regarding, e.g., safety and informed consent), while medically unnecessary genital cutting of non-consenting girls would be uniformly forbidden. That is, it would be forbidden regardless of whether the cutting is characterized (by some) as being “cosmetic” or “cultural” in nature7 and without distinction as to the girl's race, ethnicity, immigration status, parental religion, or other such features.
If the WHO were to take this approach, it might neutralize accusations of racism, cultural imperialism, and moral double standards, at least with regard to FGC. But it would not address concerns about other vulnerable persons who also face non-consensual genital cutting. These include children who may be categorized as either female or male at birth who have certain intersex traits, sometimes called differences of sex development or variations of sex characteristics (Monro et al., 2017; Carpenter, 2018a), and children who, at birth, do not appear to have such traits and are categorized as male.8 A growing number of scholars argue that an age limit or consent criterion should be applied to these children too (Tangwa, 1999; Toubia, 1999; Lightfoot-Klein et al., 2000; Mason, 2001; Ehrenreich and Barr, 2005; Darby, 2013; Svoboda, 2013; Ungar-Sargon, 2015; Earp, 2016b; Svoboda et al., 2016; Steinfeld and Earp, 2017; Chambers, 2018, 2022; BCBI, 2019; Reis, 2019; Townsend, 2020, 2022; Bootwala, 2022).
In fact, the WHO has, in at least one published report, referred to medically unnecessary intersex genital cutting (IGC) as a form of “abuse” if performed on minors without their consent, thus appearing to recognize the moral importance of consent in evaluating the permissibility of non-therapeutic genital modifications in children (WHO, 2015). However, despite the extraordinary oppression faced by intersex people in many countries, the WHO has not led a concerted effort to eliminate such non-consensual IGC (Ehrenreich and Barr, 2005; Jones, 2017; Earp et al., 2021). Regarding male genital cutting (MGC), although the WHO firmly opposes all non-Western-associated FGC (Table 1), including non-tissue-removing forms (e.g., sanitized “nicking” of the clitoral foreskin or prepuce undertaken for religious purposes) (Bootwala, 2019; Shweder, 2022b, 2023), it does not condemn any form of medically unnecessary MGC, including relatively severe and unhygienic forms, irrespective of how much healthy genital tissue is damaged or removed.
This latter inconsistency is particularly striking given that, wherever non-Western-associated FGC is performed, MGC is virtually always performed within the same communities, typically on children of a similar age under comparable conditions (DeMeo, 1997; Abdulcadir et al., 2012; Johnsdotter, 2018; Šaffa et al., 2022). In other words, wherever girls are cut for cultural or religious reasons, whether in a modern clinic or a rural homestead, their brothers are cut as well (but not vice versa). It has been estimated that 13.3 million boys and 2 million girls are “circumcised” every year (Denniston et al., 2007). The motivations for cutting overlap between the sexes and the rites often serve complementary social functions as I detail below.
Regarding physical outcomes or harms, depending on the community and the subtypes of cutting that are customary within it, either the male or female version of the ritual may be more physically severe, damaging to sexual experience, or have a higher risk of medical complications. As Debra DeLaet (2009) argues,
there are sharp differences between infibulation, the most extreme form of female genital mutilation, and the less invasive form of male circumcision that is most widely practiced. However, that comparison is not necessarily the most appropriate comparison that can be made … there are extremely invasive forms of male circumcision that are as harsh as infibulation [and while it is true] that these extreme forms [are relatively rare] it is also the case that infibulation is much less common than the less invasive variants of female circumcision. (pp. 406-407)
Indeed, according to DeLaet, “female circumcision as it is commonly practiced can be as limited in terms of the procedures that are performed and their effects as the most widespread type of male circumcision” (DeLaet, 2009) (p. 407). Taking a similar view, Nahid Toubia, the pioneering Sudanese surgeon, women's health advocate, and longtime campaigner against FGC, has stated that in many cases, “female circumcision actually results in less functional impairment and fewer physical complications than male circumcision” (Toubia, 1999) (p. 4). This appears to be the case, for example, in many Muslim communities throughout South and Southeast Asia, where religiously-inspired circumcision (i.e., cutting of the genital prepuce; see Box 2) is a gender-inclusive rite, where both forms have been largely medicalized, and where the female form is often less physically substantial than the male form (Rashid et al., 2010; Rogers, 2016; Bhalla, 2017; DBWRF, 2017; Bootwala, 2019; Rashid and Iguchi, 2019; Wahlberg et al., 2019; Dawson et al., 2020; O'Neill et al., 2020; Shweder, 2022a,b, 2023).9
Box 2. Overview of the human prepuce. Box adapted from Myers and Earp (2020) and Earp (2022a).
The term “circumcision” can refer to cutting or removing part or all of either the male or female prepuce. The genital prepuce or foreskin is a shared anatomical feature of both male and female members of all human and non-human primate species (Cold and Taylor, 1999). In humans, the penile and clitoral prepuces are undifferentiated in early fetal development, emerging from an ambisexual genital tubercle that is capable either of penile or clitoral development regardless of genotype (Baskin et al., 2018). Even at birth—and thereafter—the clitoral and penile prepuces may remain effectively indistinguishable in persons who have certain intersex traits or differences of sex development (Pippi Salle et al., 2007; Hodson et al., 2019; Grimstad et al., 2021). The penile prepuce has a mean reported surface area of between 30 and 50 square centimeters in adults (Werker et al., 1998; Kigozi et al., 2009) and it is the most sensitive part of the penis, both to light touch stimulation and to sensations of warmth (Sorrells et al., 2007; Bossio et al., 2016). The clitoral prepuce, while smaller in absolute terms, is continuous with the sexually-sensitive labia minora; it is also an important sensory platform in its own right, and one through which the clitoral glans can be stimulated without direct contact (which can be unpleasant or even painful) (O'Connell et al., 2008). Regardless of a person's sex, the prepuce is “a specialized, junctional mucocutaneous tissue which marks the boundary between mucosa and skin [similar to] the eyelids, labia minora, anus and lips … The unique innervation of the prepuce establishes its function as an erogenous tissue” (Cold and Taylor, 1999) (p. 34). It has been argued that, insofar as one assigns a positive value to the prepuce, or to the ability to decide for oneself whether such delicate genital tissue should be cut or removed, circumcision, whether of boys or of girls, necessarily harms the child to that extent, irrespective of medical risks or complications (Svoboda, 2017).
In short, the harms of genital cutting vary widely, both within and between cultures, and they do so in a way that is not reliably predicted by the sex of the affected child (Androus, 2013). That FGC in Global South settings can be medically dangerous, and sometimes deadly, is well-documented and commonly known (Obermeyer, 1999, 2003, 2005; WHO, 2008; Berg and Denison, 2012; Berg and Underland, 2013; Berg et al., 2014). As the case of Egypt shows, even in countries where most girls are cut by doctors with sterile instruments, deaths associated with FGC—due to shock, infection, sudden loss of blood pressure, or even an overdose of anesthesia—are known to occur. At least four such cases have captured the attention of national and international media in recent years (Meleigy, 2007; Al Arabiya, 2013; Al Sherbini, 2016; BBC, 2020).
By contrast, the fact that MGC within Global South settings can also be, and often is, comparably or even more dangerous has not been as widely discussed (nor, for that matter, have the risks associated with female genital “cosmetic” surgeries, intersex genital cutting, or routine penile circumcision in the Global North, although these, too, can be substantial) (Beh and Diamond, 2000; Creighton, 2001; Diamond and Garland, 2014; Darby, 2015; Earp et al., 2018; Fahmy, 2019; Learner et al., 2020; Gress, 2021; Kalampalikis and Michala, 2021; Schröder et al., 2021). To illustrate, health department records from the Eastern Cape region of South Africa show that more than five thousand Xhosa boys required hospitalization due to their traditional circumcisions between 2006 and 2013; there were 453 recorded deaths among initiates within this time period and 214 circumcision-related penile amputations (Meissner and Buso, 2007; Meel, 2010; Douglas and Nyembezi, 2015). These amputations, which ensue from circumcision nearly every cutting season, are sufficiently common that there is now an established literature debating the ethics of using government resources to pay for attempted penile transplantations (Moodley and Rennie, 2018; van der Merwe, 2020; van der Merwe et al., 2021).10
This is not to suggest that comparative harm judgments could ever suffice for a moral or political analysis of these practices; rather, it is to dispel a common empirical misunderstanding, namely, that FGC and MGC can be clearly distinguished on the basis of the respective damage they cause to health or sexuality. Indeed, from a human rights perspective, the perspective ostensibly adopted by the WHO, the relative harmfulness of genital cutting under various conditions does not determine its moral permissibility. Instead, a focus on rights might suggest that non-consenting persons (per se), including insufficiently autonomous children, have a moral—and in many countries also a legal—right against having their sexual anatomy interfered with, to any extent, whether surgically or otherwise, unless it is medically necessary11 to do so (Archard, 2007; Bruce, 2020; Bruce et al., 2022). If that is correct, a child is automatically wronged—that is, their rights are violated—by any and all such genital interference, irrespective of how harmful or even beneficial (e.g., physically, psychosocially, or spiritually) a third party intends or expects the cutting to be.
That is the position I take in my own work, at least with regard to the cultures with whose political histories, social institutions, and ethicolegal norms I am most familiar, primarily in North America, Australasia, and Europe.12 However, I argue that the right in question, insofar as it is recognized, must apply to all non-consenting persons irrespective of their sexual anatomy or socially assigned gender role (Earp, 2021b, 2022a,b). According to this approach, one cannot determine the moral acceptability of genital cutting based on an individual's sex or gender, nor can it be determined by making an empirical prediction about how harmful the cutting is likely to be. In addition to inherent problems with trying to “measure” harm-levels associated with genital cutting, whether physical or psychological, there is also the problem of coming to a principled agreement as to how much harm, or risk of harm, should be considered “too much” for a child to suffer as a result of a medically non-indicated surgery (i.e., before the operation is regarded as unacceptable).
But there is a deeper problem. And that is that one and the same type of cutting, under the same conditions (whether clinical or non-clinical), can have radically different implications for well-being depending on the affected person's attitudes, beliefs, and values (Einstein, 2008; Earp and Darby, 2017; Earp and Steinfeld, 2018; Connor et al., 2019; Abdulcadir, 2021; Johnson-Agbakwu and Manin, 2021; Tye and Sardi, 2022). Put differently, the level of harm a person experiences by virtue of having their sexual anatomy non-consensually cut or altered is not simply a function of how physically severe the cutting was, or whether there were surgical complications. Rather, for many persons subjected to medically unnecessary genital cutting, even supposedly minor forms, it is the mere fact of having been judged “imperfect,” “impure,” or “incomplete” as a child, and (therefore) unwillingly subjected to a surgical operation—targeting a part of the body that is culturally constructed as being especially intimate or personal—that engenders feelings of harm and even sexual violation (Dreger, 1999; Hammond and Carmack, 2017; Taher, 2017). How much harm the person feels, or will feel, on such a basis, cannot be predicted in advance, as it depends on culturally and individually variable interpretive frameworks (Johnsdotter, 2013).
In its policies and materials on FGC, the WHO gives a cluster of reasons for opposing the practice, without clarifying which of the reasons, or combination of reasons, is necessary or sufficient to make it a rights violation. Nevertheless, it stresses that the practice—regardless of type—is condemnable due to the following: it involves the cutting or removal of healthy, functional tissue from the sexual anatomy of a vulnerable individual; it is medically unnecessary; it is usually very painful; it risks various complications, both physical and psychological; and it is typically performed on pre-autonomous minors, making it (presumably in conjunction with one or more of the other factors) “a violation of the rights of children” (WHO, 2020b). As Hope Lewis writes, this reasoning is common among human rights advocates primarily situated in the Global North: “From the perspectives of non-practicing cultures, the primary ethical basis of universal concern about [FGC] is that it involves the infliction of great physical pain and the risk of life-threatening complications for infants and children, whose well-being is of special legal and moral concern in both practicing and non-practicing cultures” (Lewis, 1995) (p. 19, emphasis added).
As demonstrated in Box 3, each of these concerns applies with equal force to MGC in the same societies where FGC is carried out, as well as to MGC in other societies, where only boys are cut. Moreover, the WHO is aware of this fact, as the information presented in Box 3 is derived from its own 2009 report on “Traditional Male Circumcision Among Young People” (WHO, 2009).
Box 3. What the WHO knows about the harms and circumstances of “traditional” MGC.
In its report on “traditional” MGC, the WHO acknowledges that, as with FGC, “complications associated with male circumcision, including long-term morbidity and death … have not been systematically assessed.” Nevertheless, it cites a 35% complication rate for traditional male circumcision, with wound infection and delayed wound-healing (more than 60 days) being common (WHO, 2009) (p. 4). Other “serious sequelae in the traditional groups were persistent swelling, extensive scarring, and loss of erectile function” (WHO, 2009) (p. 27).
More generally, the WHO is aware of “reports of appalling complications after male circumcision,” “forced male circumcision through the abduction of boys” in multiple African countries, “reactive depression” of boys following circumcision, homophobia associated with male circumcision rites, and “reporting of suicide in some cases” (p. 13). The WHO states that in some communities, boys “face ritual circumcision without any encouragement or social support” (ibid.).
In the same report, the WHO affirms that boys are “expected to tolerate” the pain of circumcision “without showing any weakness” and that participation is rarely voluntary: as with FGC, circumcision is “usually not an optional procedure to be decided about on an individual basis” (p. 12). Indeed, “the social pressure to undergo circumcision puts uncircumcised boys at risk of ostracism,” which, in the relevant circumstances, can be a life-endangering proposition (p. 14). Moreover, “women are reported as actively influencing” adolescents boys' decisions to be circumcised (p. 14), with one of the “main” reasons cited being the belief that circumcised men will give them more sexual pleasure. In many African communities, “no self-respecting” girl would marry an “uncircumcised” male, leaving few options for boys who would refuse the rite (ibid).
Finally, the WHO reports that in some contexts, boys experience “bullying and beatings” until they agree to be circumcised; however, hospital circumcisions are considered to be ritually inadequate: “particularly because of the use of anesthesia and the avoidance of pain, which is considered [a] central aspect of the traditional ritual” (p. 21). The WHO concludes that severe stigmatization of boys who do not want to be circumcised “limits the freedom of choice regarding circumcision” (ibid.).
So, what has been the WHO's policy in this area? In the case of “traditional” MGC, the WHO advises that it should preferably be done in a clinical setting or with sterilized equipment to make it safer, taking a harm-reduction approach. Indeed, the WHO has published its own training manual for healthcare providers on how to successfully medicalize the practice. The manual gives explicit, step-by-step instructions with accompanying photographs, showing how to perform medically unnecessary penile circumcisions on non-consenting boys, while touting a new surgical device for doing so invented and patented by an author of the manual (WHO, 2010).13
At the same time, the WHO categorically opposes medicalization of any type of FGC, including forms that are less physically substantial than the penile circumcisions performed in certain cases within the same families, as illustrated earlier with the gender-inclusive Islamic ritual common in parts of South and Southeast Asia (Rashid and Iguchi, 2019; Dawson et al., 2020; Rashid et al., 2020). The WHO fears that medicalizing even such “minor” FGC (e.g., nicking, pricking, or partial removal of the female foreskin or labia without clitoral glans modification) might “legitimize” the practice (WHO, 2020b):
In many settings, health care providers perform FGM due to the belief that the procedure is safer when medicalized. WHO strongly urges health care providers not to perform FGM. FGM is recognized internationally as a violation of the human rights of girls and women.
Thus, the WHO argues that medicalizing FGC risks “legitimizing” a ritual practice that is internationally recognized to violate human rights—perhaps most saliently, the right to bodily integrity—irrespective of cutting severity or any health-related outcomes. This suggests that it is not the medical risk level, degree of harmfulness, anticipated adverse effects on health or sexuality, or any other such contingent empirical feature that grounds the status of medically unnecessary FGC as being a violation of this purported human right. Instead, according to the WHO, or at least implicit within its statements and claims, it is the simple fact of cutting into a vulnerable person's sexual anatomy, when there is no relevant medical emergency, that makes FGC a rights violation (perhaps especially when the person cannot consent).
Given its widely noted commitment to the principle of non-discrimination on the basis of sex, it might seem that the WHO should therefore regard any act of genital cutting that shares these features to be a violation of the human right to bodily integrity. Both MGC and FGC, to quote now directly from the WHO policy on the latter, involve “[t]he removal of or damage to healthy, normal genital tissue [risking] several immediate and long-term health consequences,” can be “painful and traumatic,” and are “nearly always carried out on minors,” often within the same communities (WHO, 2008) (p. 1). A puzzle is therefore raised as to why the WHO treats one of these practices as a fundamental human rights violation in all its forms, while the other type is not treated as a human rights violation in any of its forms. The situation is puzzling because human rights, by definition, apply to all humans; that is, they apply regardless of sex.14
Instead, paradoxically, as the anthropologist Kirsten Bell has noted, the WHO seeks “to medicalize male circumcision on the one hand, oppose the medicalization of female circumcision on the other, while simultaneously basing their opposition to the female operations on grounds that could legitimately be used to condemn the male operations” (Bell, 2005) (p. 131).
These and other inconsistencies threaten to damage the credibility of the WHO and undermine its perceived authority to pronounce on human rights. This, in turn, may have implications for the global campaign against FGC, given that the campaign increasingly relies on human rights-based arguments rather than solely, or even mainly, on health-based arguments (Shell-Duncan, 2008). As the WHO acknowledges, the latter type of argument may tend to foster medicalization of FGC, or a transition to its less severe forms, rather than the wholesale abandonment of the practice as the WHO prefers (Askew et al., 2016). In short, whatever one thinks of the legitimacy of the WHO's policy goals in this area, if the organization is to be taken seriously on matters of genital cutting, whether scientifically, politically, or morally, these inconsistencies must be addressed.
One way the WHO might seek to address the aforementioned inconsistencies would be to deny that they are based on double standards. A common way to do this has been to suggest that FGC, either typically or on balance, is far more harmful than MGC, often by making appeals to Western stereotypes of the practices that are based on very different exemplars. Plausibly, these contrasting stereotypes stem, in part, from greater cultural familiarity with MGC in Western countries, especially in the United States, where MGC—but not FGC—is a medicalized birth custom associated with concepts of hygiene (Wallerstein, 1985; Gollaher, 1994; Hodges, 1997; Darby, 2016). In addition, Jewish religious MGC has also been familiar to Western culture for many centuries.15 By contrast, since the 1970s, FGC has been linked in Western discourse to “African” culture, which is widely portrayed as being “primitive” or “barbaric” (Bader, 2019; Abdulcadir et al., 2020; Bader and Mottier, 2020). A major aspect of this “othering” portrayal has been a disproportionate focus on the most drastic forms of FGC done in “traditional” settings, while ignoring both (1) the less drastic, medicalized forms of FGC that are common in many Global South countries, and (2) the comparatively dangerous, “traditional” forms of MGC that co-occur with their female counterparts.16 As we have seen, however, when the full range of practices across cultures is taken into account, and relevantly similar cases compared, a harm-based analysis of health outcomes cannot justify the WHO's categorically differential treatment of the two types of cutting.
What about health-related benefits, then? According to this approach, the WHO could appeal to potential health benefits associated with MGC, while maintaining that FGC has “no health benefits, only harm” (WHO, 2020b). As noted previously, the WHO has indeed relied on this argument to distinguish its apparently conflicting policies on genital cutting, so it merits some comment here.
Recall that, according to the WHO, MGC, in the form of penile circumcision, “has significant health benefits that outweigh the very low risk of complications when performed by adequately-equipped and well-trained providers in hygienic settings” (WHO, 2008) (p. 11). The WHO goes on to cite evidence of a reduced risk for circumcised males, but not their partners, of acquiring heterosexually transmitted HIV in settings where transmission of this kind is epidemic (the trial looking at male-to-female transmission was stopped early for futility, as the female partners of circumcised males were contracting HIV at a higher rate; the WHO does not mention this trial).17
Note the multiple qualifiers, in the previous paragraph, in the quote from the WHO after “when.” In trying to establish a categorical difference between FGC and MGC, the WHO picks out a very specific type of MGC, namely the type that is culturally familiar to Western countries, primarily through exposure to the medicalized version of the practice that is customary in the United States. When it illustrates “FGM,” by contrast, it highlights the least sanitary forms of the practice, done in the most coercive ways, with the most disabling physical outcomes, while simultaneously urging that these forms not be medicalized (Gruenbaum, 2005). According to Dr. Tatu Kamau, a Kenyan physician who advocates for equal legal treatment of male and female genital cutting, such an approach “absurdly prevents women from accessing quality health services and then blames them for risking their lives. This asymmetry [is] all the more questionable considering that during circumcision, both males and females run the same immediate surgical risks of uncontrolled bleeding, shock and sepsis yet males are privileged to have these risks mitigated but females are not” (Ahmadu and Kamau, 2022) (p. 32).
As for the claim that the health benefits of male circumcision outweigh the risks, that is, in part, a value judgment (Savulescu, 2015; Frisch and Earp, 2018), and it is not a judgment that is universally shared among relevant authorities. In fact, it is the minority position among national-level medical societies to have formally considered the question: only U.S.-based bodies have joined the WHO in attributing net health benefits to (especially newborn) MGC (FMA, 2008; KNMG, 2010; RACP, 2010; AAP, 2012; Frisch et al., 2013; CPS, 2015; Earp, 2015a; Earp and Shaw, 2017; DMA, 2020; Deacon and Muir, 2022). But suppose the claim is simply granted. The alleged net health improvement the WHO ascribes to medicalized MGC under ideal clinical conditions obviously does not apply to so-called “traditional” MGC, which, by contrast, has an extremely high rate of morbidity and mortality that would more than nullify any claimed health benefit (see Box 3). However, the WHO does not condemn any type of MGC as a rights violation, including its most dangerous and unhygienic forms, even when these are carried out on non-consenting children. Instead, it urges that the more dangerous forms be medicalized, as noted previously. By contrast, as we saw, the WHO opposes medicalization of FGC, arguing that such attempts at harm-reduction would be unethical: the practice is, in its view, inherently a human rights violation, irrespective of medical outcome or even the affected person's own consent (Shell-Duncan, 2001; WHO, 2008, 2020b; Askew et al., 2016). It stands to reason, then, that, even if “FGM” did have statistical health benefits similar to those that have been attributed to MGC, the WHO would not switch to supporting it.
This can be seen by drawing an analogy, taking MGC first. The data regarding HIV-related health benefits for MGC come from studies of adult men in sub-Saharan Africa who, ostensibly, gave their free and informed consent to undergo penile circumcision, hoping this would reduce their risk of acquiring HIV. The population-level effectiveness of such circumcision as a form of prophylaxis against HIV remains contested (Garenne et al., 2013; Rosenberg et al., 2018; Garenne and Matthews, 2019; Loevinsohn et al., 2020; Luseno et al., 2021; Garenne, 2022), perhaps because one's risk of contracting a sexually transmitted virus has more to do with behavioral and social-structural considerations than with anatomical factors such as the presence or absence of healthy genital tissues (Aggleton, 2007; Norton, 2013, 2017; Parker et al., 2015; Earp and Darby, 2019; Fish et al., 2021).
Nevertheless, the WHO has cited these HIV-related data to justify not only the voluntary circumcision of adult men, as might be expected, but also the circumcision of young boys—including infants in the U.S. American style—in populations that do not traditionally practice genital cutting (WHO, 2010). In fact, a “large proportion” of the now more than 25 million medicalized circumcisions that have taken place in Africa since 2007, promoted as prophylaxis by the WHO and substantially funded by the U.S. government, have been carried out, not on consenting adults, but on underage boys between the ages of 10 and 14 (WHO, 2020a).18
To complete the analogy, let us now turn to FGC. Suppose there were equivalent data suggesting an HIV-protective effect of adult, consensual FGC—labiaplasty, say—in women. It is inconceivable that the WHO would cite these data as a justification for surgically removing non-diseased labial tissues from healthy newborns or even 10–14 year-old adolescent girls. Instead, as I have suggested elsewhere, the WHO would likely argue as follows: “healthy, nerve-laden genital tissue (a description that applies as much to the penile foreskin as it does to the labia) is valuable in its own right, so that removing it without urgent medical need is itself a harm; [it] would stress that all more conservative means of addressing potential infection should be exhausted before surgery is employed; and [it] would insist that girls have an inviolable moral right against any medically unnecessary interference with their private, sexual anatomy to which they themselves do not consent when of age” (Earp, 2021a) (p. 6).
To summarize, the health benefits attributed to “medicalized” MGC—even if they are simply granted—do not apply to so-called “traditional” MGC, which the WHO does not condemn regardless of risk-level or consent. In any case, the data that are cited in support of these benefits come from studies of consensual adult surgeries, not non-consensual surgeries performed on minors: the data cannot, whether scientifically or ethically, simply be transposed to children. Finally, the benefits themselves can be realized more effectively in alternative ways that do not require genital surgery (such as regular condom use), making this a morally inappropriate option for pre-autonomous minors. This can be seen, I have suggested, by imagining that WHO-defined “FGM” did have health benefits comparable to the ones that have been attributed to medicalized MGC. If that were so, would the WHO conclude that the practice no longer counted as an instance of genital mutilation, nor violated human rights, even if it were imposed on pre-autonomous girls? It does not seem likely.
Empirical questions, therefore, concerning health benefits or harms will not be the focus of the rest of this paper. Instead, I will now consider whether the WHO can defend its selective opposition to non-Western-associated FGC by appealing to a distinctive role for such FGC in upholding patriarchal gender systems and furthering sex-based discrimination.
According to the WHO, all non-Western-associated FGC “reflects deep-rooted inequality between the sexes, and constitutes an extreme form of discrimination against women” (WHO, 2008) (p. 1). The implied corollary is that MGC does not reflect deep-rooted inequality between the sexes nor constitute sex-based discrimination. In other words, FGC might be thought to symbolize or even actively reinforce the subordinated status of women and girls, making it a highly objectionable practice, whereas boys on this view are not similarly demeaned or disadvantaged by MGC, so it is less of a problem (if a problem at all). In fact, MGC is sometimes said to benefit boys by elevating them into positions of power, thereby granting them access to special social privileges (Dorkenoo, 1994). It is therefore entirely appropriate, according to this perspective, that global campaigns against genital cutting should aim to help women and girls but not boys.
I argue that this view is mistaken, not only empirically and conceptually, but also politically and morally.
The empirical and conceptual flaws can be summarized as follows. First, with respect to the claim that non-Western-associated FGC constitutes an extreme form of discrimination against women, one must rehearse the point that, as far as anthropologists are aware, women and girls are rarely if ever19 exclusively targeted for genital cutting, whereas, by contrast, boys in many cultures are so targeted (Abdulcadir et al., 2012; Šaffa et al., 2022; see also Gruenbaum et al., in press). In such “MGC-only” cultures, moreover, while boys may be advantaged along some dimensions, they are specifically disadvantaged by genital cutting, specifically because they are boys. In other words, because they were designated male at birth and raised as boys, rather than as female and raised as girls, they (and only they) must submit to a physically risky and often intentionally painful intervention into their sexual anatomy, or else face potentially severe social sanction (Schlegel and Barry, 2017).
Of course, girls in such societies may be significantly disadvantaged in various other ways. And it can readily be agreed that, wherever girls are disadvantaged along some dimension simply because they are girls, this should be a matter for serious concern and needs to be addressed. Here, however, we are evaluating the claim that women and girls are discriminated against by virtue of having their genitals cut, thus potentially justifying the WHO's selective condemnation of non-Western-associated FGC. That claim appears not to be true.
Nevertheless, it might still be argued that, even if girls are not singled out for genital cutting, whereas boys often are; and even if, because of their gender, boys in some cultures are significantly disadvantaged by genital cutting in particular (whereas girls in those same cultures are spared that particular disadvantage), FGC is still uniquely problematic on other grounds having to do with gender inequality. For example, it could be argued that FGC, and only FGC, reflects and reinforces a lower status for women and girls in the societies where it is practiced, despite being practiced alongside MGC.
Efua Dorkenoo, the great Ghanaian-British campaigner against FGC, is one of many prominent voices to have advanced such a claim. In her classic book Cutting the Rose, she begins by acknowledging that there are at least some similarities between, in her terms, “FGM and male circumcision,” and also between “the rites of passage” into adulthood for girls and boys in many African communities. She writes: “Certainly the two procedures are related. Both are widely practiced without medical necessity and in both cases children go through a traumatic experience. Both are performed on children without their consent.” But, she continues, “there the parallel ends.” With respect to symbolic meanings, she stresses that
the content of male rites of passage is geared toward training young boys to develop skills associated with power and control, not to reinforce their submissiveness and to make them feel they are second-class citizens as is done in the female initiation (Dorkenoo, 1994) (p. 52).
Therefore, Dorkenoo seems to suggest, it is not so important to criticize the boys' “traumatic” rite.
Such a conclusion, however, does not follow. As LeYoni Junos argued more than 20 years ago, where FGC and MGC are practiced together as parallel rites of initiation, “the initiation of both boys and girls have a codependency. The males in the community cannot have power and control unless there is someone to be controlled. Equally, female submissiveness can only be reinforced if there is someone to be submissive to; i.e., someone (male) exerting power and control” (Junos, 1998) (p. 11, emphasis in original). To break this codependency, she argues, both male and female genital cutting of children must be opposed.
The key word here is “both,” not one or the other. From the perspective of gender equality, it would be no more appropriate to selectively condemn MGC than it is to selectively condemn FGC, simply as a matter of principle. However, more than abstract principles are at stake. In fact, as I will now argue, women and girls may be actively harmed by the WHO's “single sex” approach to addressing medically unnecessary child genital cutting. This harm is based, in part, on a failure to understand the multiple meanings, motivations, intentions, and functions of FGC in the diverse societies where it is practiced (Thomas, 1996; Yoder et al., 1999; Shell-Duncan and Hernlund, 2000; Baumeister and Twenge, 2002; Robertson and James, 2002; Dellenborg, 2007; Kratz, 2010), not least because, by ignoring the concurrent rite for boys, FGC is inaccurately and misleadingly reduced to “discrimination” (WHO, 2008).
The reality is not so simple. Not all of the social meanings and functions of FGC are straightforwardly bad for women and girls—at least not under the arguably non-ideal conditions in which boys are also cut—and nor do they necessarily reflect a subordinated status. Instead, where deliberately harsh MGC rites enable men to form politically powerful bonds amongst themselves, created in part through their shared experience of genital cutting20 (Schlegel and Barry, 2017), FGC appears to have arisen in some cultures as a parallel rite that is then invariably led by women. And like its male counterpart, the female rite serves to promote within-sex bonding, communal network-building, and power consolidation, thereby weakening other-sex domination in various spheres (Grande, 2009; Ahmadu, 2010, 2016a; Prazak, 2017).
In fact, some scholars suggest that FGC may have culturally evolved in reaction to, or in conjunction with, male-oriented rites in certain gender systems, as an offsetting force or power-neutralizer (Caldwell et al., 1997; Leonard, 2000b; Knight, 2001; Silverman, 2004; Moxon, 2017). According to a recent global phylogenetic analysis conducted by Gabriel Šaffa and colleagues, over the course of human history, FGC has almost exclusively emerged in societies that were already practicing MGC. The result has often been a co-equal platform for girls, like boys, to gain social status through displays of courage, maturity, and the ability to withstand pain, while showing respect for authority and communal institutions (Šaffa et al., 2022). Indeed, even the potential exceptions to this pattern (i.e., of FGC emerging or persisting only alongside MGC) may end up proving the rule. Support for this possibility comes from the Hadza of Tanzania, a primarily hunting and foraging people. Ironically, the Hadza may be one of the few—perhaps the only—society on record in which FGC, but not MGC, is traditionally practiced. Far from being patriarchal, however, the Hadza are “famously egalitarian” (Power, 2015) (p. 339). If FGC serves primarily to subordinate women and girls, how could that be so? The answer is revealing. The Hadza practice a linked pair of gender rituals, one male-oriented and the other female-oriented, in which members of both sexes engage in “costly signaling”—including genital cutting in the case of women—to demonstrate their commitment to the group. The male ritual, epeme, confers certain sacred privileges, however, which is seen as “discordant” in a society where men have very little authority over women in daily life. To explain how such ritual male privilege could co-exist with a deep-rooted lack of male control over women, Camilla Power posits that the female rite, maitoko, acts as a “counterbalance: women-as-a-group contesting and answering men's ritual claims” (Power, 2015) (p. 353). In particular, she argues that the women's intense, painful, and emotionally transformative rite is a vital source of female bonding and solidarity formation that operates to counteract male power and thus “maintain egalitarianism” (Power, 2015) (p. 354).
Taking a broader view, anthropologists have argued that FGC rites in some societies, whether functioning as rites of passage or so-called instituting rites,21 may thus serve to undermine gender inequality (Leonard, 2000b; Shweder, 2002; Grande, 2009; Ahmadu, 2010; Abdulcadir et al., 2012; Prazak, 2017; Dellenborg and Malmström, 2020). Elisabetta Grande, for example, argues that in many cases, the women-led FGC rites are such crucial sources of “group solidarity, mutual aid, exchange and companionship, that [they may act as] the primary and most important form of resistance against male dominance” (Grande, 2009) (p. 15).22
Thus, rather than simply being a means of oppressing girls, as implied by the WHO, FGC rites in some societies appear to serve as politically important sources of power for women—just as the MGC rites often do for men. Ironically, then, the WHO's selective targeting of the female rites may actually “weaken female power centers within society and bring women's bodies and lives under the hegemonic control and management of local male religious or political leaders” (Abdulcadir et al., 2012) (p. 23). Meanwhile, as MGC is not targeted for condemnation, the men are free to continue their own initiations, training up the next generation of boys to assume the aforementioned leadership positions, often through stoical displays of patriarchal masculinity (as I describe next).
To summarize, it may be the WHO's selective opposition to FGC rituals in societies that initiate girls and boys together, more so than the rituals themselves, that discriminate(s) on the basis of sex (women, but not men, exposed to legal sanction for carrying out their valued traditions; girls, but not boys, protected from genital cutting) while simultaneously weakening female power centers (Grande, 2009; Abdulcadir et al., 2012) and diverting resources away from more pressing material needs—such as access to medicines, nutritious food, or clean water—thereby leaving women worse off overall (Gruenbaum, 2001).23
Strikingly, a more appropriate target of condemnation, from the perspective of promoting women's and girls' rights in FGC-practicing cultures, may in fact be the male-centered genital cutting rituals that occur in the same societies.
In these rituals, young boys are typically separated from their mothers and sisters, isolated from female friends and playmates, and socialized—often by means of an explicitly gendered trial of violence—to become “real men” (see Dembroff, 2022), where this is characteristically defined in terms of patriarchal norms of masculinity that promote the subordination of women and girls (Leonard, 2000a; Silverman, 2004; Schlegel and Barry, 2017; Mashabane and Henderson, 2020). Therefore, opposition to these male initiations and other MGC rites may be crucial for disrupting gendered socialization processes by which patriarchal hierarchies are reproduced (Kimmel, 2001; Prazak, 2017; Steinfeld and Earp, 2017; Meoded Danon, 2021).
Using the Xhosa of South Africa as an example, it has been argued that the prevailing patriarchal belief system embedded in Xhosa culture “contributes to the widespread gender-based violence in South Africa” (Mashabane and Henderson, 2020) (p. 163). Tellingly, these authors claim that the initiation rite for boys “explicitly instills norms of hegemonic masculinity” (ibid.). According to Alice Schlegel and Herbert Barry III, adolescent impressionability “facilitates intensive teaching of cultural beliefs and ideology, including the ideology of masculinity. If the ideal man is aggressive, subjecting boys to aggressive behavior by men is a vivid demonstration of that ideal” (Schlegel and Barry, 2017) (p. 15).
Domineering behavior is a common feature of such rites; similar observations have been made of the male initiation practices among the Kikuyu of Kenya (Njoroge et al., 2022), for example, or among various ethnic groups in Papua New Guinea (Kelly et al., 2012). In these and other MGC-practicing societies, young boys who fail to live up to the demands of “real man” masculinity often face bullying and harassment from older males to prove their manliness—a necessary component of which is surviving the MGC ritual (see Box 3). In fact, in many such societies, males are not considered men unless they have been circumcised in the ritually prescribed way; a non-circumcised male remains a “boy” regardless of age or maturity, and thus cannot marry or receive other social goods (Mavundla et al., 2010).
Accordingly, non-circumcised boys, along with other males who are perceived to violate “real man” standards (gay, disabled, or poor men, for example) are stigmatized, ridiculed, and marginalized—both by circumcised men and by women and girls24—unless and until they comply with their prescribed socialization (Weiss, 1966; Rowanchilde, 1996; Martí, 2010; Mavundla et al., 2010; Kelly et al., 2012; Mashabane and Henderson, 2020). Under such a regime, the only way to escape from this subordinated position (apart from suicide, which is not uncommon in the relevant contexts) is to undergo a painful genital cutting rite without flinching or showing signs of “weakness” (WHO, 2009). As a part of this, the initiate is forced to reject and repudiate any “feminine” aspects of his personality, character, or body (the foreskin is considered “feminine,” being soft and sensitive; this is part of why it must be cut off).25
According to research summarized by Schlegel and Barry III, such harrowing male rituals, and the teachings that accompany them,
force a cognitive reorganization, from attachment to and dependence on mothers and other women to denigration of them. [Boys may be] forcefully taken from the nurturing environment of their mothers' dwellings to the community men's house in which men spend most of their non-working time and may also sleep. In addition to the abrupt transition and the pain and fear they experience, boys are taught that women are dangerous. The initiation ceremony, emphasizing women's pollution [and] the need to remove it, prepares the boys to denigrate women, particularly women of reproductive age … By learning that women are polluting and dangerous, they come to fear women and feel revulsion at female bodies and to realign their attachment from mothers and sisters to males (Schlegel and Barry, 2017) (p. 16).
As a part of this transformation, boys must learn to assume a dominant gender role, which means domination over women and girls—as well as non-circumcised boys, gay men, and other perceived failures of masculinity (Junos, 1998; Mashabane and Henderson, 2020). And so the cycle continues. Thus, I conclude, the MGC ritual in many FGC-practicing societies (as well as in some societies where FGC is not practiced) is a major cultural mechanism through which female-subordinating gender hierarchies and associated ideologies are reproduced. Accordingly, insofar as the WHO is concerned about genital cutting practices that “reflect deep-rooted inequality between the sexes”—one of the main reasons for its condemnation of non-Western-associated FGC—it should similarly oppose and condemn ritual MGC in the same (and other) societies.
Much of what I have synthesized here has been said, in one way or another, by many other scholars before me. Indeed, there is a large and longstanding body of research—within anthropology, gender studies, post-colonial feminism, and other areas—that has highlighted the WHO's inaccurate, sensationalized, and essentializing characterizations of non-Western-associated FGC. All of this research is well-known to scholars of genital cutting and is readily available to the WHO. Yet as Michela Fusaschi writes:
Ignoring much of this research, the WHO has persisted in cordoning off and defining only non-Western-associated female-only genital modification as a grave human rights abuse, except when performed for ‘medical reasons.' Much of the academic literature, journalistic coverage of the topic, and international policy and law approaches to genital modification have taken their cue from the WHO (Fusaschi, 2022) (p. 2).
This has led to an unfortunate situation whereby “common knowledge” of non-Western-associated FGC, especially in relation to MGC, does not constitute knowledge at all, but rather highly skewed impressions and incorrect inferences based on stereotypes and selective examples. Moreover, this “common knowledge” is not merely mistaken, or randomly erroneous; rather, it is systematically biased in a way that preserves the status quo of unequal power relations between certain countries and cultures in the arena of global health and human rights governance (Shweder, 2002; Njambi, 2004; Boddy, 2007; Earp, 2016a; Shahvisi, 2021).
This is not an abstract or theoretical point. Rather, there has been fine-grained sociological research into the relevant decision-making processes of human rights “gatekeepers” at the WHO and other Global North agencies. Charli Carpenter (2014), who has conducted such research, notes that the perceived acceptability of different genital cutting practices tracks the personal or familial commitments/customs of the decision-makers themselves.
Notably, MGC of non-consenting minors, specifically non-therapeutic penile circumcision, is a majority birth custom in the United States, the country with the greatest influence on the WHO. This influence extends to the personnel who are directly involved in setting the global human rights agenda, a disproportionate number of whom are U.S. Americans. As such, “the practice [of MGC] is prevalent in their own social networks” (p. 138). Carpenter reports that, “unlike many other practices human rights professionals condemn but do not participate in, the practice of circumcision was widespread” among her interview subjects. Confronting this fact “evoked defensiveness from those who had circumcised their own [male] children and were loath to think of themselves as human rights abusers” (p. 139).
Hope Lewis has drawn a similar connection: “Because male circumcision is a far more accepted practice among Western groups—whose cultural norms have significantly shaped human rights instruments and norms—it is rarely considered an appropriate subject of human rights concern” (Lewis, 1995) (p. 6). Ditto Zachary Androus: “The normalization of male circumcision in Anglophone society was a necessary condition for the emergence of the paradigmatic gender distinction that characterizes [Western] cultural, social, and political responses to African genital modification practices” (Androus, 2013) (p. 277).
These sorts of analyses suggest that U.S.-based human rights campaigners may suffer from a cultural illusion, simply failing to connect the dots between, on the one hand, their cited reasons for opposing all non-Western-associated FGC, regardless of severity, and, on the other hand, the practice of MGC that is happening in their own back yard. However, the Egyptian feminist Seham Abd el Salam (1999) (all quoted material from section III.C.a) has argued that such selective opposition to FGC is not due to simple ignorance or a failure to have considered the connections to MGC. Rather, she suggests that such “pragmatic” or inconsistent proponents of the human right to bodily integrity have made an “unwritten deal with … conservative social forces” to allow MGC to go unquestioned:
The terms of this unspoken deal imply that pro-bodily integrity activists accept some conservative practices, such as [MGC] that provides symbolic carving of traditional masculinity, in exchange [for] letting the activists oppose [FGC], which is a traditional … symbolic carving of femininity.
The bargain thus rests on a certain logic that takes for granted patriarchal gender asymmetries, with MGC as the immovable foundation. The logic, according to Abd el Salam, rests on the heightened status or worth of male children within patriarchal social systems. She writes: “given that male children are particularly valued by patriarchal family systems, [MGC] is significant to replicate the terms of the patriarchal hierarchy, which requires submission of lower to higher rank groups.” This includes not only rankings based on gender (men dominating women) but also based on age (men dominating boys and women dominating girls). Thus, the practice of involuntary MGC of young boys acts as a type of “age discrimination” with more powerful adults asserting their control over the bodies of the next generation. This serves to uphold social hierarchies because it “socializes people into submission to hurting their own children.” Moreover, Abd el Salam maintains, it is a particularly effective means of doing so because of the special value of boys in patriarchal systems.
For such patriarchal systems to persist, the role of MGC in normalizing such top-down violence—that is, painful genital cutting inflicted on the most valuable members of society when they are simultaneously at their most vulnerable—must not be questioned. It is, according to one theory of the socio-functional origins of the practice, a dangerous and costly signaling device that proves one's willingness to submit to the norms (and rankings or authority structure) of the wider community, which would have been necessary for group survival under certain challenging conditions (Schlegel and Barry, 2017). FGC also serves this purpose, but to a lesser extent: “getting people to tolerate mutilation of their sons' bodies as a price for conditioned social acceptance is a stronger tool to ensure their submission to authorities than getting them to tolerate [FGC]” (Abd el Salam, 1999).
According to Abd el Salam, there is at least an implicit recognition of this fact among “pragmatic” defenders of the right to bodily integrity: that is, those campaigners who, like the WHO, selectively apply the principle and oppose only FGC. Such campaigners seem to know, at least on some level, that raising MGC as an issue “may break the terms of their unwritten political bargain” with the conservative patriarchal forces. This, in turn, “explains the panic of pragmatists from raising the issue [and their] attack of anyone who dares to raise it.”26 According to this way of thinking, it is better to allow men to continue to dominate boys within the logic of the patriarchal power system—for example, by testing them with painful rites until they prove they are capable of assuming a dominant position themselves—than to disturb the status quo while seeking an allowance to end FGC of girls.
The strategy may seem sensible, but Abd el Salam proposes that it cannot work in the long run, if the aim is to undermine the patriarchal system. She writes: “the pragmatists are right in that … hegemonic social authorities at all levels are likely to stand against any efforts to liberate people from the suffering of hurting their own sons. Nonetheless, they are not right in neglecting the potential impact of such efforts on bringing about a social change for the benefit of the more vulnerable social groups,” including women and girls and sexual and gender minorities. MGC, she suggests, serves as a lynchpin of patriarchy in those various human societies that have, at some point in their history, discovered its usefulness for that very purpose. To undermine the patriarchal order of gender relations, the lynchpin must be pulled.
This analysis by Abd el Salam appears to be borne out by the recent global phylogenetic study conducted by Šaffa and colleagues, mentioned earlier. Not only did they find that FGC has almost always come about, historically, in societies already practicing MGC; they also found that the abandonment of MGC in certain societies has reliably been followed by a “rapid loss” of FGC as well (Šaffa et al., 2022). Given, therefore, the apparently greater socio-structural dependence of FGC on MGC than vice versa, Šaffa and colleagues suggest that “it may be more difficult to eliminate [FGC] while treating male circumcision as a separate issue.” Instead, “efforts to eradicate [genital cutting] may benefit from greater gender neutrality” in dominant approaches to social reform.
If this line of analysis is correct, it might be necessary for the long-term achievement of gender equality in societies that practice FGC—and thus also MGC—for international advocates of children's rights to bodily integrity to join forces across lines of sex and gender. This should involve collaboration with local dissenters and reformers to condemn and campaign against, not only FGC, but also MGC and IGC: that is, all medically unnecessary genital cutting of vulnerable children by adults in positions of power. All such practices can be seen as normalizing the infliction of bodily injuries on relatively defenseless persons and thus as a form of violent domination, thereby reinforcing the patriarchal status quo. By contrast, a human rights approach, consistently applied, may break the cycle of violence once and for all.
The author confirms being the sole contributor of this work and has approved it for publication.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Thank you to Clare Chambers, Manon Garcia, Ellen Gruenbaum, Sara Johnsdotter, Saarrah Ray, Arianne Shahvisi, and the peer reviewers for valuable feedback on earlier drafts. Thank you also to Enrico Ripamonti for his extraordinary patience with the revisions.
1. ^I discuss intersex practices throughout the paper; however, most of that discussion is in the notes or Box 1. This is not to suggest that IGC is any less important than FGC or MGC. Rather, it is to simplify the flow of ideas by focusing on the numerically more prevalent practices—and the heightened controversy surrounding attempts to compare them—so as to improve readability. Moreover, comparisons between FGC and IGC (Ehrenreich and Barr, 2005) and between IGC and MGC (Antinuk, 2013) have been thoughtfully explored by others.
2. ^Note that “non-circumcised” girls face similar mistreatment in societies that widely practice FGC (UNICEF Innocenti Research Centre, 2010).
3. ^For the purposes of this paper, an intervention to alter a bodily state is medically necessary “when (1) the bodily state poses a serious, time-sensitive threat to the person's well-being, typically due to a functional impairment in an associated somatic process, and (2) the intervention, as performed without delay, is the least harmful feasible means of changing the bodily state to one that alleviates the threat” (BCBI, 2019) (p. 18). Of course, the social and political processes by which some practices come to be considered medically necessary—whether in the above sense or otherwise—while other similar practices do not, are complex and require careful interrogation. For a recent discussion, see Hegarty et al. (2021).
4. ^Also termed “endosex” (Carpenter et al., 2022). Endosex, in contrast to intersex, refers to the state of being “born with physical sex characteristics that match what is considered usual for binary female or male bodies by the medical field” (Monro et al., 2021) (p. 437). Although the WHO definition of “FGM” does not explicitly refer to endosex females as the population of interest, in practice, intersex females (that is, persons with intersex traits or differences of sex development who have been categorized as female at birth) have not been included within the ambit of the term, nor have they been protected by associated child-safeguarding laws or policies (Lightfoot-Klein et al., 2000). Neither have intersex males been so included or protected. Thus, the “assignment” of children with intersex traits to one binary sex category or another continues to be accompanied by, or effectuated with, medically unnecessary so-called “normalizing” surgeries to try to conform their genitalia to an endosex appearance (Carpenter, 2018b; Reis, 2019).
5. ^Following Shahvisi (2021), I use “Western” to refer to the countries of Europe, North America, and Australasia, and “non-Western” to refer to all other contexts, with a particular emphasis on Africa, South and Southeast Asia, and the Middle East. As Shahvisi emphasizes, this is a “troubling dichotomy,” but such labeling tracks the morally suspect distinction between “the West” and “the rest” that she and others have argued underlies the perceived categorical difference between some forms of FGC compared to others (see Table 1); critiquing this dichotomy requires the use of language that captures the relevant distinction.
6. ^Gillick competence is a standard set by UK law regarding the criteria that must be fulfilled by under-16-year-olds if they are to be deemed capable of giving their own morally valid consent to a proposed procedure. These criteria involve adequately understanding the nature of the procedure (including its long-term potential consequences) and making a rational decision based on sufficiently supportive reasons. For discussion, see Larcher and Hutchinson (2010).
7. ^According to Shahvisi (2021), both types of cutting “have significant overlap in terms of their physical details, both practices are also risky, often performed on minors, and are motivated by [powerful] cultural pressures, some of which are unambiguously patriarchal” (p. 3). Framing the practices as morally incomparable despite these similarities, she suggests, reflects prejudicial thinking: white women are painted as rational agents in a supposedly culture-free environment (“the West”) whereas women of color are seen as “victims of their cultures and their menfolk, unable to make choices about their bodies” (“the rest”) (ibid.).
8. ^That is, non-intersex or “endosex” males; see footnote 4. Note that some children who, at birth, outwardly appear to have male-typical anatomy may discover later in life (often around puberty, accompanying hormonal changes, or when facing certain unexplained health problems) that some of their internal reproductive features or chromosomes are more typical for females (Reis, 2009; Majzoub et al., 2017).
9. ^It may also be the case in certain African communities, as argued by Ayaan Hirsi Ali, the Somali-born author and activist against FGC, to which she herself was subjected as a child: “I think male circumcision is worse than an incision of the girl. With boys, a lot of skin is removed. Depending on how that's done, [in] countries, for instance, where there's poor hygiene, and where the people who carry it out don't possess the necessary skills, the consequences can be worse for [the] boy than for [the] girl. With girls, a sharp object is pricked into the clitoris. It bleeds a little. And the whole family is satisfied, and she is declared ‘pure.' Strictly speaking, that procedure is less dramatic than male circumcision” (Hirsi Ali, 2012; see also Bodenner, 2015). Needless to say, other procedures to which girls are subjected in certain contexts, such as excision of the external clitoris and labia and/or infibulation, can be far more dramatic, in terms of likely medical complications, degree of anatomical change, risk of sexual impairment, and so on, than a typical penile circumcision (holding all else equal).
10. ^Although Xhosa girls are also initiated into adulthood, they do not traditionally undergo genital cutting as a part of this process, and no initiation-related deaths have been reported in recent years. More generally, according to a comprehensive overview of FGC in Population, “infant and childhood mortality linked to [FGC] is poorly measured and is invisible in mortality statistics for the affected countries” (Andro et al., 2016) (p. 262).
11. ^See footnote 3 for a definition. For example: to treat a disease, perform a required health exam, or, for a parent or other appropriate caregiver, help a child wash who cannot yet do so on their own. By contrast, a doctor who performed an unnecessary medical exam on a non-autonomous person's sexual anatomy (as in the case of Larry Nassar; see Barr and Murphy, 2018), or a parent who continued to wash their child's genitals when the child was capable of doing so on their own, would likely be crossing an ethical, and in many jurisdictions, a legal, boundary (BCBI, 2019).
12. ^I believe these arguments may also be appropriate for other cultural contexts, but I do not take a stand on that here.
13. ^The WHO's erstwhile “chief expert on circumcision” (Hennessy-Fiske, 2011), David Tomlinson, an author of the manual, has apparently received generous royalty payments relating to a WHO-recommended infant circumcision device called AccuCirc for which he owns the patent: https://openpaymentsdata.cms.gov/physician/775085.
14. ^The WHO must be sincere in assuming that it is truly human rights that are at stake in its policy—as opposed to sex-discriminatory claims or merely conflicting cultural preferences: that is, “the universalization of one particular culture-bound perspective” (Androus, 2013) (p. 267). Otherwise, the organization would lack an appropriate justification for striving to “eliminate” FGC over the objections of long-practicing communities who regard both FGC and MGC as virtuous. Of course, this is precisely the argument of defenders of FGC (and MGC) who claim that the WHO's appeals to “human rights” are, far from being principled, a hypocritical means of asserting Western cultural dominance (Shweder, 2002, 2005, 2006; Oba, 2008).
15. ^In fact, the American form of the practice—complete removal of the penile foreskin as opposed to only the most distal tip, and performed on newborns rather than on older boys—is historically based on the Jewish style (Glick, 2005).
16. ^As Nahid Toubia has noted, FGC is associated in Western media with “widely publicized, widely-circulated, and [often] exaggerated accounts of the physical complications of infibulation [the most invasive form of FGC] performed under adverse conditions in rural Africa,” while at the same time, “there is little mention in the popular media of the immediate and long-term complications of male circumcision” under similar “rural” conditions, “despite extensive documentation in the medical literature” (Toubia, 1999) (p. 4). Another potential cause of the asymmetry in Western perceptions of male versus female genital cutting is the widespread gender-segregation among researchers working on genital cutting: because it is primarily women who study FGC (and only FGC) and men who study MGC (and only MGC), neither group tends to explore the intracultural connections between male and female genital cutting within a given society (Merli, 2008, 2010).
17. ^See Wawer et al. (2009). Marge Berer, the founding editor of Reproductive Health Matters, has raised numerous concerns about the failure to account for this trial, which she suggests puts African women at risk who are already more vulnerable to HIV and AIDS (Berer, 2007, 2008, 2009). Additional gender-related, ethical, and public health concerns about the WHO campaign to circumcise millions of African boys and men have been raised by others (Rudrum et al., 2017; Gilbertson et al., 2019; Luseno et al., 2019, 2021; Rudrum, 2020; Fish et al., 2021; Rennie et al., 2021).
18. ^Going forward, the WHO plans to continue targeting teenagers, as “uptake of [circumcision] among adult men has been limited” in various settings (WHO, 2020a) (p.xi).
19. ^There is one possible exception of which I am aware, namely the Hadza, who live, hunt, and forage around Lake Eyasi in Tanzania. I will say more about the Hadza later on.
20. ^According to Power (2015), ritually induced trauma recruits cognitive and emotional mechanisms that convert painful or frightening experiences shared with others into a lasting bond. Those who survive the ordeal “engage in reflection, creating rich representations of the episode's significance” (p. 338). Doing so reinforces “the impression that only those who have experienced the same thing can possibly understand how it feels and what it means,” thereby producing a “robust and enduring state of psychological kinship among coparticipants” (Whitehouse and Lanmann, 2014) (p. 680).
21. ^According to Pierre Bourdieu (2005), there are limitations to the concept of a rite of passage as applied to certain social practices; the example of newborn circumcision in Judaism is a key example, as it is not a ritual through which the child deliberately passes on his way to—or as a way of attaining—adult status. Nevertheless, it is an important social ritual that draws a line around one type of person (the circumcised male) and imbues him with a status that is not attainable by those who have not undergone the ritual. In fact, what Bourdieu calls an “instituting” rite is one whose purpose is even more essential: “to clearly separate those who have undergone it not from those who have not yet undergone it, but from those who will under no circumstances undergo it, and thus to institute a lasting difference between those whom the rite concerns and those whom it does not concern” (p. 80). To speak of rites of institution, therefore, “is to point to the fact that every rite leads toward the consecration or legitimization of an arbitrary boundary; that is to say, it misrepresents the arbitrariness and presents the boundary as legitimate and natural” (p. 81)—for example, the boundary line of gender by which males and females are treated differently in the social sphere in accordance with a culture's dominant gender ideology. Thus, within Judaism, the rite of circumcision institutes a separation, not only between circumcised and not-yet-circumcised boys, but between “the set of those who can be subjected to circumcision (boys and men, regardless of whether they are children or adults) and those who cannot (girls and women)” (p. 81). As Shaye Cohen (1997) argues, it is precisely this exclusion of females from the rite of genital cutting that reflects their lower status within the patriarchal social structure of rabbinical Judaism (see also Kimmel, 2001; Glick, 2005; Benatar, 2008). The fact that, in FGC-practicing societies, the rite of genital cutting does not exclude females is therefore significant. Instead of assigning them to a lower status on account of their sex, it rather places them in a complementary relationship to males—i.e., “different but equal” —which may reflect a relatively non-hierarchical gender structure within the “cultural DNA” of at least some such societies (Ahmadu, 2000; Ahmadu and Kamau, 2022).
22. ^Due in part to Western intervention and criminalization, the ability of the rituals in question to serve their social function as sites of bonding is increasingly disrupted, with the practices being driven underground and stripped of their symbolic significance. This is a relatively recent development, but there are still places where the rites are considered “women's business” and are supported by women on the basis of the relationships that are formed through them (Dellenborg and Malmström, 2020). Insofar as the counter-patriarchal bonding functions of the rites have been diluted due to Western intervention, such that, increasingly, the rites are simply painful genital cutting experiences carried out underground to avoid criminal sanction, this would be a highly unfortunate and in some ways deeply ironic consequence of Western intervention which is, in fact, premised on the idea that the rites serve no valid social function and are simply painful interventions into girls' genitals.
23. ^According to Lewis (1995) (p. 33), Marie-Angelique Savane, the Senegalese sociologist and feminist, has questioned the focus of Western efforts to eliminate primarily African FGC, arguing that “Western apprehensions about the health of African women did not appear to extend to the detrimental effects of neo-colonialism and inequitable development.”
24. ^According to bell hooks (2004), it is important to “highlight the role women play in perpetuating and sustaining patriarchal culture so that we will recognize patriarchy as a system women and men support equally, even if men receive more rewards from that system. Dismantling and changing patriarchal culture is work that men and women must do together” (p. 24).
25. ^According to Fox and Thomson (2009), this is just one of the ways in which “circumcision has functioned as a marker of masculine belonging. By literally inscribing particular [identities on a boy's] body, circumcision can be understood as a normalizing technology which validates particular forms of body modification; in this case the removal of tissue which comes to be coded as excessive, redundant, polluted or feminine” (p. 196).
26. ^According to the Canadian bioethicist Margaret Sommerville (Somerville, 2004), “When I spoke out against infant male circumcision, one response that I encountered was an angry reaction from some feminists. They accused me of detracting from the horror of female genital mutilation and weakening the case against it by speaking about it and infant male circumcision in the same context” (p. 241).
Abd el Salam, S. (1999). Male Genital Mutilation (Circumcision): Feminist Study of a Muted Gender Issue [American University in Cairo]. Available online at: http://www.noharmm.org/muted5.htm (accessed April 2, 2022).
Abdulcadir, J. (2021). “Female genital mutilation/cutting,” in The EBCOG Postgraduate Textbook of Obstetrics & Gynaecology, eds T. Mahmood, C. Savona-Ventura, I. Messinis, and S. Mukhopadhyay (Cambridge: Cambridge University Press), 473–482. doi: 10.1017/9781108582322.057
Abdulcadir, J., Ahmadu, F. S., Essén, B., Gruenbaum, E., Johnsdotter, S., Johnson, M. C., et al. (2012). Seven things to know about female genital surgeries in Africa. Hastings Center Rep. 42, 19–27. doi: 10.1002/hast.81
Abdulcadir, O., Bader, D., Abdulcadir, J., and Catania, L. (2020). Different cultures but similar requests: adolescents' demands for non-therapeutic genital modifications. Curr. Sexual Health Rep. 12, 289–291. doi: 10.1007/s11930-020-00279-z
Abu-Sahlieh, S. A. A. (1994). To mutilate in the name of Jehovah or Allah: legitimization of male and female circumcision. Med. Law 13, 575–622.
Abu-Sahlieh, S. A. A. (2001). Male and Female Circumcision: Religious, Medical, Social and Legal Debate. Warren Center, PA: Marco Polo Monographs, Shangri-La Publications. Available online at: http://sami-aldeeb.com/livres/Circumcision.pdf (accessed April 2, 2022).
Aggleton, P. (2007). “Just a snip”? A social history of male circumcision. Reprod. Health Matters 15, 15–21. doi: 10.1016/S0968-8080(07)29303-6
Ahmadu, F. S. (2000). “Rites and wrongs: an insider/outsider reflects on power and excision,” in Female “Circumcision” in Africa: Culture, Controversy, and Change, eds B. Shell-Duncan and Y. Hernlund (Boulder, CO: Lynne Rienner Publishers), 283–315.
Ahmadu, F. S. (2007). “Ain't I a woman too? Challenging myths of sexual dysfunction in circumcised women,” in Transcultural Bodies: Female Genital Cutting in Global Context, eds Y. Hernlund and B. Shell-Duncan (New Brunswick, NJ: Rutgers University Press), 278–310. doi: 10.36019/9780813541389-014
Ahmadu, F. S. (2010). Empowering girls in Sierra Leone: initiation into the Bondo society. J. Dev. Behav. Pediatrics 31, 172–173. doi: 10.1097/DBP.0b013e3181d55a5d
Ahmadu, F. S. (2016a). Male and Female Circumcision Among the Mandinka of the Gambia: Understanding the Dynamics of Traditional Dual-Sex Systems in a Contemporary African Society. Saarbrücken: LAP LAMBERT Academic Publishing.
Ahmadu, F. S. (2016b). Why the term female genital mutilation (FGM) is ethnocentric, racist and sexist – let's get rid of it! Hysteria. Available online at: http://www.hystericalfeminisms.com/voices1/2016/10/16/why-the-term-female-genital-mutilation-fgm-is-ethnocentric-racist-and-sexist-lets-get-rid-of-it (accessed April 2, 2022).
Ahmadu, F. S. (2017). “Equality, not special protection: multiculturalism, feminism, and female circumcision in Western liberal democracies,” in Universalism Without Uniformity: Explorations in Mind and Culture, eds J. Cassaniti and U. Menon (Chicago, IL: University of Chicago Press), 214–236. doi: 10.7208/chicago/9780226501710.003.0013
Ahmadu, F. S., and Kamau, T. (2022). Dr Tatu Kamau vs The Attorney General and Others: Problems and prospects in Kenya's 2021 High Court ruling to uphold the Prohibition of Female Genital Mutilation Act 2011. Glob. Discourse 12, 29–46. doi: 10.1332/204378921X16388161357195
Aktor, M. (2016). “Whose rights? The Danish debate on ritual infant male circumcision as a human rights issue,” in Contemporary Views on Comparative Religion, eds P. Antes, A. W. Geertz, and M. Rothstein (Sheffield: Equinox), 311–324.
Al Arabiya (2013, June 10). Egyptian girl dies undergoing circumcision. Al Arabiya English. Available online at: https://english.alarabiya.net/News/middle-east/2013/06/10/Egyptian-girl-dies-while-being-circumcised
Al Sherbini, R. (2016, May 31). Egypt in shock as girl dies from Female Genital Mutilation (FGM). Al Bawaba. Available online at: https://www.albawaba.com/news/egypt-shock-girl-dies-female-genital-mutilation-fgm-846416
Andro, A., Lesclingand, M., Grieve, M., and Reeve, P. (2016). Female genital mutilation. Overview and current knowledge. Population 71, 215–296.
Androus, Z. T. (2004). The United States, FGM, and Global Rights to Bodily Integrity. The United States and Global Human Rights Conference (University of Oxford), 1–7. Available online at: http://www.zacharyandrous.com/The%20US%20FGM%20and%20Global%20HR.pdf (accessed April 2, 2022).
Androus, Z. T. (2013). Critiquing circumcision: in search of a new paradigm for conceptualizing genital modification. Glob. Discourse 3, 266–280. doi: 10.1080/23269995.2013.813282
Antinuk, K. (2013). Forced genital cutting in North America: feminist theory and nursing considerations. Nurs. Ethics 20, 723–728. doi: 10.1177/0969733013496361
Arora, K. S., and Jacobs, A. J. (2016). Female genital alteration: a compromise solution. J. Med. Ethics 42, 148–154. doi: 10.1136/medethics-2014-102375
Askew, I., Chaiban, T., Kalasa, B., and Sen, P. (2016). A repeat call for complete abandonment of FGM. J. Med. Ethics 42, 619–620. doi: 10.1136/medethics-2016-103553
Askola, H. (2011). Cut-off point? Regulating male circumcision in Finland. Int. J. Law Policy Family 25, 100–119. doi: 10.1093/lawfam/ebq018
Bader, D. (2019). Picturing female circumcision and female genital cosmetic surgery: a visual framing analysis of Swiss newspapers, 1983–2015. Feminist Media Stud. 19, 1159–1177. doi: 10.1080/14680777.2018.1560348
Bader, D., and Mottier, V. (2020). Femonationalism and populist politics: the case of the Swiss ban on female genital mutilation. Nations Nationalism 26, 807–825. doi: 10.1111/nana.12615
Barr, J., and Murphy, D. (2018, January 22). Nassar surrounded by adults who enabled his predatory behavior. ABC News. Available online at https://abcnews.go.com/Sports/nassar-surrounded-adults-enabled-predatory-behavior/story?id=52533983
Baskin, L. S., Shen, J., Sinclair, A. W., Cao, M., Liu, X., Liu, G. Y. Y., et al. (2018). Development of the human penis and clitoris. Differentiation 103, 74–85. doi: 10.1016/j.diff.2018.08.001
Baumeister, R. F., and Twenge, J. M. (2002). Cultural suppression of female sexuality. Rev. General Psychol. 6, 166–203. doi: 10.1037/1089-2680.6.2.166
BBC (2020, January 31). Female genital mutilation: Parents arrested after death of girl in Egypt. BBC News. Available online at: https://www.bbc.com/news/world-middle-east-51332011
BCBI. (2019). Medically unnecessary genital cutting and the rights of the child: moving toward consensus. Am. J. Bioethics 19, 17–28. doi: 10.1080/15265161.2019.1643945
Beh, H. G., and Diamond, M. (2000). An emerging ethical and medical dilemma: Should physicians perform sex assignment surgery on infants with ambiguous genitalia? Michigan J. Gender Law 7, 1–63.
Bell, K. (2005). Genital cutting and Western discourses on sexuality. Med. Anthropol. Q. 19, 125–148. doi: 10.1525/maq.2005.19.2.125
Berer, M. (2007). Male circumcision for HIV prevention: perspectives on gender and sexuality. Reprod. Health Matters 15, 45–48. doi: 10.1016/S0968-8080(07)29304-8
Berer, M. (2008). Male circumcision for HIV prevention: What about protecting men's partners? Reprod. Health Matters 16, 171–175. doi: 10.1016/S0968-8080(08)32418-5
Berer, M. (2009). Male circumcision and risk of HIV in women. Lancet 374, 1497–1498. doi: 10.1016/S0140-6736(09)61898-5
Berer, M. (2010). Labia reduction for non-therapeutic reasons vs. female genital mutilation: contradictions in law and practice in Britain. Reprod. Health Matters 18, 106–110. doi: 10.1016/S0968-8080(10)35506-6
Berer, M. (2015). The history and role of the criminal law in anti-FGM campaigns: Is the criminal law what is needed, at least in countries like Great Britain? Reprod. Health Matters 23, 145–157. doi: 10.1016/j.rhm.2015.10.001
Berg, R. C., and Denison, E. (2012). Does female genital mutilation/cutting (FGM/C) affect women's sexual functioning? A systematic review of the sexual consequences of FGM/C. Sexuality Res. Soc. Policy 9, 41–56. doi: 10.1007/s13178-011-0048-z
Berg, R. C., and Underland, V. (2013). The obstetric consequences of female genital mutilation/cutting: a systematic review and meta-analysis. Obstet. Gynecol. Int. 2013, 1–15. doi: 10.1155/2013/496564
Berg, R. C., Underland, V., Odgaard-Jensen, J., Fretheim, A., and Vist, G. E. (2014). Effects of female genital cutting on physical health outcomes: a systematic review and meta-analysis. BMJ Open 4, e006316. doi: 10.1136/bmjopen-2014-006316
Bhalla, N. (2017, November 28). Female circumcision in Sri Lanka is “just a nick,” not mutilation: supporters. Jakarta Globe. Available online at: https://jakartaglobe.id/news/female-circumcision-sri-lanka-just-nick-not-mutilation-supporters
Boddy, J. (2007). Civilizing Women: British Crusades in Colonial Sudan. Princeton, NJ: Princeton University Press. doi: 10.1515/9780691186511
Boddy, J. (2016). The normal and the aberrant in female genital cutting: shifting paradigms. HAU J. Ethnographic Theory 6, 41–69. doi: 10.14318/hau6.2.008
Boddy, J. (2020). Re-thinking the zero tolerance approach to FGM/C: the debate around female genital cosmetic surgery. Curr. Sexual Health Rep. 12, 302–313. doi: 10.1007/s11930-020-00293-1
Bodenner, C. (2015, May 13). How similar is FGM male circumcision? The Atlantic. Available online at: https://www.theatlantic.com/health/archive/2015/05/malecircumcision-vs-female-circumcision/392732/
Bond, S. L. (1999). State laws criminalizing female circumcision: a violation of the equal protection clause of the fourteenth amendment? John Marshall Law Rev. 32, 353–380.
Bootwala (2019). A review of female genital cutting (FGC) in the Dawoodi Bohra community: parts 1, 2, and 3. Curr. Sexual Health Rep. 11, 212–235. doi: 10.1007/s11930-019-00212-z
Bootwala, Y. (2022). Exploring opposition to ritual female genital cutting since the first U.S. federal prosecution: the 2017 Detroit case. Int. J. Impotence Res. doi: 10.1038/s41443-022-00532-0. [Epub ahead of print].
Bossio, J. A., Pukall, C. F., and Steele, S. S. (2016). Examining penile sensitivity in neonatally circumcised and intact men using quantitative sensory testing. J. Urol. 195, 1848–1853. doi: 10.1016/j.juro.2015.12.080
Bourdieu, P. (2005). “Rites as acts of institution,” in Honor and Grace in Anthropology, eds J. G. Peristiany, J. G. Peristiany, and J. Pitt-Rivers (Cambridge: Cambridge University Press), 79–89.
Bruce, L. (2020). A pot ignored boils on: sustained calls for explicit consent of intimate medical exams. HEC Forum 32, 125–145. doi: 10.1007/s10730-020-09399-4
Bruce, L., Hannikainen, I. R., and Earp, B. D. (2022). New findings on unconsented intimate exams suggest racial bias and gender parity. Hastings Center Rep. 52, 7–9. doi: 10.1002/hast.1349
Caldwell, J. C., Orubuloye, I. O., and Caldwell, P. (1997). Male and female circumcision in Africa from a regional to a specific Nigerian examination. Soc. Sci. Med. 44, 1181–1193. doi: 10.1016/S0277-9536(96)00253-5
Carpenter, C. (2014). “Lost” Causes: Agenda Vetting in Global Issue Networks and the Shaping of Human Security. Ithaca, NY: Cornell University Press.
Carpenter, M. (2016). The human rights of intersex people: addressing harmful practices and rhetoric of change. Reprod. Health Matters 24, 74–84. doi: 10.1016/j.rhm.2016.06.003
Carpenter, M. (2018a). Intersex variations, human rights, and the international classification of diseases. Health Hum. Rights 20, 205–214.
Carpenter, M. (2018b). The “normalization” of intersex bodies and “othering” of intersex identities in Australia. J. Bioeth. Inq. 15, 487–495. doi: 10.1007/s11673-018-9855-8
Carpenter, M. (2021). Intersex human rights, sexual orientation, gender identity, sex characteristics and the Yogyakarta Principles plus 10. Cult. Health Sex. 23, 516–532. doi: 10.1080/13691058.2020.1781262
Carpenter, M., Dalke, K. B., and Earp, B. D. (2022). Endosex. J. Med. Ethics. doi: 10.1136/medethics-2022-108317. [Epub ahead of print].
Chambers, C. (2004). Are breast implants better than female genital mutilation? Autonomy, gender equality and Nussbaum's political liberalism. Critic. Rev. Int. Soc. Politic. Philos. 7, 1–33. doi: 10.1080/1369823042000269366
Chambers, C. (2018). Reasonable disagreement and the neutralist dilemma: abortion and circumcision in Matthew Kramer's “Liberalism with Excellence.” Am. J. Jurisprudence 63, 9–32. doi: 10.1093/ajj/auy006
Chase, C. (1998). Hermaphrodites with attitude: mapping the emergence of intersex political activism. GLQ J. Lesbian Gay Stud. 4, 189–211. doi: 10.1215/10642684-4-2-189
Coene, G. (2018). “Male circumcision: the emergence of a harmful cultural practice in the West?,” in FGM/C: From Medicine to Critical Anthropology, eds M. Fusaschi and G. Cavatorta (Turin: Meti Edizioni), 133–150.
Cohen, S. J. D. (1997). Why aren't Jewish women circumcised? Gend. Hist. 9, 560–578. doi: 10.1111/1468-0424.00076
Cohen, S. J. D. (2022). Parity between men and women? Reflections on the circumcision of men and the circumcision of women. Glob. Discourse 12, 207–209. doi: 10.1332/204378921X16359777893946
Cold, C. J., and Taylor, J. R. (1999). The prepuce. BJU Int. 83, 34–44. doi: 10.1046/j.1464-410x.1999.0830s1034.x
Coleman, D. L. (1998). The Seattle compromise: multicultural sensitivity and Americanization. Duke Law J. 47, 717–783. doi: 10.2307/1372912
Connor, J. J., Brady, S. S., Chaisson, N., Sharif Mohamed, F., and Robinson, B. B. E. (2019). Understanding women's responses to sexual pain after female genital cutting: an integrative psychological pain response model. Arch. Sex. Behav. 50, 1859–1869. doi: 10.1007/s10508-019-1422-9
CPS (2015). Newborn male circumcision. Paediatr. Child Health 20, 311–320. doi: 10.1093/pch/20.6.311
Creighton, S. M. (2001). Surgery for intersex. J. R. Soc. Med. 94, 218–220. doi: 10.1177/014107680109400505
Darby, R. (2013). The child's right to an open future: Is the principle applicable to non-therapeutic circumcision? J. Med. Ethics 39, 463–468. doi: 10.1136/medethics-2012-101182
Darby, R. (2015). Risks, benefits, complications and harms: neglected factors in the current debate on non-therapeutic circumcision. Kennedy Inst. Ethics J. 25, 1–34. doi: 10.1353/ken.2015.0004
Darby, R. (2016). Moral hypocrisy or intellectual inconsistency? A historical perspective on our habit of placing male and female genital cutting in separate ethical boxes. Kennedy Inst. Ethics J. 26, 155–163. doi: 10.1353/ken.2016.0018
Davis, D. S. (2001). Male and female genital alteration: a collision course with the law. Health Matrix 11, 487–570.
Davis, D. S. (2003). Cultural bias in responses to male and female genital surgeries. Am. J. Bioethics 3, W15–W16. doi: 10.1162/152651603766436333
Dawson, A., Rashid, A. K., Shuib, R., Wickramage, K., Budiharsana, M., Hidayana, I. M., et al. (2020). Addressing female genital mutilation in the Asia Pacific: the neglected sustainable development target. Aust. N. Z. J. Public Health 44, 8–10. doi: 10.1111/1753-6405.12956
DBWRF (2017). Dawoodi Bohra Women's Association for Religious Freedom. Dawoodi Bohra Women's Association for Religious Freedom. Available online at: https://dbwrf.org/
Deacon, M., and Muir, G. (2022). What is the medical evidence on non-therapeutic child circumcision? Int. J. Impot. Res. doi: 10.1038/s41443-021-00502-y. [Epub ahead of print].
DeLaet, D. L. (2009). Framing male circumcision as a human rights issue? Contributions to the debate over the universality of human rights. J. Human Rights 8, 405–426. doi: 10.1080/14754830903324795
Dellenborg, L. (2007). Multiple Meanings of Female Initiation [Doctoral Dissertation, Göteborg University]. Available online at: http://www.gu.se/english/research/publication/?publicationId=5863 (accessed April 7, 2022).
Dellenborg, L., and Malmström, M. F. (2020). “Female circumcision/genital mutilation and human rights: ownership of personal change,” in Female Genital Cutting: The Global North and South, ed S. Johnsdotter (Mälmo: Centre for Sexology and Sexuality Studies), 159–183.
Dembroff, R. A. (2022). Real Men on Top: How Patriarchy Weaponizes Gender. Oxford: Oxford University Press.
DeMeo, J. (1997). “The geography of male and female genital mutilations,” in Sexual Mutilations: A Human Tragedy, eds G. C. Denniston and M. F. Milos (Boston, MA: Springer US), 1–15. doi: 10.1007/978-1-4757-2679-4_1
Denniston, G. C., Hodges, F. M., and Milos, M. F. (2007). Male and Female Circumcision: Medical, Legal, and Ethical Considerations in Pediatric Practice. New York, NY: Springer Science & Business Media.
Diamond, M., and Garland, J. (2014). Evidence regarding cosmetic and medically unnecessary surgery on infants. J. Pediatr. Urol. 10, 2–6. doi: 10.1016/j.jpurol.2013.10.021
DMA (2020). Lægeforeningens politik vedrørende omskæring af drengebørn uden medicinsk indikation. Danish Medical Association. Available online at: https://www.laeger.dk/omskaering-af-drenge-uden-medicinsk-indikation-er-etisk-uacceptabelt (accessed April 2, 2022).
Dorkenoo, E. (1994). Cutting the Rose: Female Genital Mutilation: The Practice and Its Prevention. London: Minority Rights Group.
Douglas, M., and Nyembezi, A. (2015). Challenges facing traditional male circumcision in the Eastern Cape. Human Sciences Research Council, 1–47. Available online at: http://www.hsrc.ac.za/uploads/pageContent/6391/Presentation%20-%20Challenges%20facing%20traditional%20male%20circumcision%20in%20the%20Eastern%20Cape.pdf (accessed April 2, 2022).
Dustin, M. (2010). Female genital mutilation/cutting in the UK: challenging the inconsistencies. Europ. J. Women's Stud. 17, 7–23. doi: 10.1177/1350506809350857
Earp, B. D. (2015a). Do the benefits of male circumcision outweigh the risks? A critique of the proposed CDC guidelines. Front. Pediatrics 3, 18. doi: 10.3389/fped.2015.00018
Earp, B. D. (2015b). Female genital mutilation and male circumcision: toward an autonomy-based ethical framework. Medicolegal Bioethics 5, 89–104. doi: 10.2147/MB.S63709
Earp, B. D. (2016a). Between moral relativism and moral hypocrisy: reframing the debate on “FGM.” Kennedy Inst. Ethics J. 26, 105–144. doi: 10.1353/ken.2016.0009
Earp, B. D. (2016b). In defence of genital autonomy for children. J. Med. Ethics 42, 158–163. doi: 10.1136/medethics-2015-103030
Earp, B. D. (2020a). Systems thinking in gender and medicine. J. Med. Ethics 46, 225–226. doi: 10.1136/medethics-2020-106206
Earp, B. D. (2020b). Zero tolerance for genital mutilation: a review of moral justifications. Curr. Sexual. Health Rep. 12, 276–288. doi: 10.1007/s11930-020-00286-0
Earp, B. D. (2021a). Male or female genital cutting: why ‘health benefits' are morally irrelevant. J. Med. Ethics 47, 1–10. doi: 10.1136/medethics-2020-106782
Earp, B. D. (2021b). Protecting children from medically unnecessary genital cutting without stigmatizing women's bodies: implications for sexual pleasure and pain. Arch. Sex. Behav. 50, 1875–1885. doi: 10.1007/s10508-020-01633-x
Earp, B. D. (2022a). Against legalising female ‘circumcision' of minors. Glob. Discourse 12, 47–76. doi: 10.1332/204378921X16347905414226
Earp, B. D. (2022b). “The ethics of circumcision,” in The Rowman & Littlefield Handbook of Bioethics, eds E. Di Nucci, J.-Y. Lee, and I. Wagner (Lanham, MD: Rowman & Littlefield).
Earp, B. D., Allareddy, V., Allareddy, V., and Rotta, A. T. (2018). Factors associated with early deaths following neonatal male circumcision in the United States, 2001- 2010. Clin. Pediatr. 57, 1532–1540. doi: 10.1177/0009922818790060
Earp, B. D., and Darby, R. (2017). Circumcision, sexual experience, and harm. Univ. Pennsylvania J. Int. Law 37, 1–57. Available online at: https://www.researchgate.net/publication/315763686
Earp, B. D., and Darby, R. (2019). Circumcision, autonomy and public health. Public Health Ethics 12, 64–81. doi: 10.1093/phe/phx024
Earp, B. D., Hendry, J., and Thomson, M. (2017). Reason and paradox in medical and family law: shaping children's bodies. Med. Law Rev. 25, 604–627. doi: 10.1093/medlaw/fwx027
Earp, B. D., and Johnsdotter, S. (2021). Current critiques of the WHO policy on female genital mutilation. Int. J. Impot. Res. 33, 196–209. doi: 10.1038/s41443-020-0302-0
Earp, B. D., Shahvisi, A., Reis-Dennis, S., and Reis, E. (2021). The need for a unified ethical stance on child genital cutting. Nurs. Ethics 28, 1294–1305. doi: 10.1177/0969733020983397
Earp, B. D., and Shaw, D. M. (2017). Cultural bias in American medicine: the case of infant male circumcision. J. Pediatr. Ethics 1, 8–26. Available online at: https://www.researchgate.net/publication/316527603
Earp, B. D., and Steinfeld, R. (2017). “Gender and genital cutting: a new paradigm,” in Gifted Women, Fragile Men, ed T. G. Barbat (Brussels: ALDE Group-EU Parliament).
Earp, B. D., and Steinfeld, R. (2018). Genital autonomy and sexual well-being. Curr. Sexual. Health Rep. 10, 7–17. doi: 10.1007/s11930-018-0141-x
Ehrenreich, N., and Barr, M. (2005). Intersex surgery, female genital cutting, and the selective condemnation of cultural practices. Harvard Civil Rights-Civil Liberties Law Rev. 40, 71–140. Available online at: https://www.researchgate.net/publication/294195994
Einstein, G. (2008). From body to brain: considering the neurobiological effects of female genital cutting. Perspect. Biol. Med. 51, 84–97. doi: 10.1353/pbm.2008.0012
Esho, T. (2022). “The future of female genital cutting: an evolution of its medicalization,” in African Futures, Vol. 27, eds C. Greiner, S. Van Wolputte, and M. Bollig (Leiden: Brill), 338–346. doi: 10.1163/9789004471641_029
Evans, M. (2011). Circumcision in boys and girls: why the double standard? BMJ 342, 442. doi: 10.1136/bmj.d978
Fish, M., Shahvisi, A., Gwaambuka, T., Tangwa, G. B., Ncayiyana, D., and Earp, B. D. (2021). A new Tuskegee? Unethical human experimentation and Western neocolonialism in the mass circumcision of African men. Dev. World Bioethics 21, 211–226. doi: 10.1111/dewb.12285
FMA. (2008). Finnish Medical Association opposes circumcisions in public health care. Yle Uutiset. Available online at: http://yle.fi/uutiset/finnish_medical_association_opposes_circumcisions_in_public_health_care/5142149 (accessed April 2, 2022).
Fox, M., and Thomson, M. (2009). Foreskin is a feminist issue. Austral. Feminist Stud. 24, 195–210. doi: 10.1080/08164640902852415
Frisch, M., Aigrain, Y., Barauskas, V., Bjarnason, R., Boddy, S.-A., Czauderna, P., et al. (2013). Cultural bias in the AAP's 2012 technical report and policy statement on male circumcision. Pediatrics 131, 796–800. doi: 10.1542/peds.2012-2896
Frisch, M., and Earp, B. D. (2018). Circumcision of male infants and children as a public health measure in developed countries: a critical assessment of recent evidence. Glob. Pub. Health 13, 626–641. doi: 10.1080/17441692.2016.1184292
Fusaschi, M. (2015). Humanitarian bodies: gender, moral economy and genital modifications in Italian immigration policy. Cahiers d'Études Africaines 217, 11–28. doi: 10.4000/etudesafricaines.17985
Fusaschi, M. (2022). Gendered genital modifications in critical anthropology: from discourses on FGM/C to new technologies in the sex/gender system. Int. J. Impot. Res. doi: 10.1038/s41443-022-00542-y. [Epub ahead of print].
Garenne, M. (2022). HIV prevention in Africa: is VMMC useful and acceptable? Int. J. Impot. Res. doi: 10.1038/s41443-022-00575-3. [Epub ahead of print].
Garenne, M., Giami, A., and Perrey, C. (2013). “Male circumcision and HIV control in Africa: questioning scientific evidence and the decision-making process,” in Global Health in Africa: Historical Perspectives on Disease Control, eds T. Giles-Vernik and J. Webb (Athens, OH: Ohio University Press), 185–210.
Garenne, M., and Matthews, A. (2019). Voluntary medical male circumcision and HIV in Zambia: expectations and observations. J. Biosoc. Sci. 52, 560–572. doi: 10.1017/S0021932019000634
Gilbertson, A., Ongili, B., Odongo, F. S., Hallfors, D. D., Rennie, S., Kwaro, D., et al. (2019). Voluntary medical male circumcision for HIV prevention among adolescents in Kenya: unintended consequences of pursuing service-delivery targets. PLoS ONE 14, e0224548. doi: 10.1371/journal.pone.0224548
Glick, L. B. (2005). Marked in Your Flesh: Circumcision from Ancient Judea to Modern America. Oxford: Oxford University Press. doi: 10.1093/019517674X.001.0001
Gollaher, D. L. (1994). From ritual to science: the medical transformation of circumcision in America. J. Soc. Hist. 28, 5–36. doi: 10.1353/jsh/28.1.5
Grande, E. (2009). Hegemonic human rights: the case of female circumcision. A call for taking multiculturalism seriously. Archivio Antropologico Mediterraneo 12, 11–27. Available online at: https://www.academia.edu/14381184
Gress, S. (2021). Labia minora repair. Aesthetic Plast. Surg. 45, 2447–2463. doi: 10.1007/s00266-021-02383-4
Grimstad, F., Boskey, E. R., Taghinia, A., Estrada, C. R., and Ganor, O. (2021). The role of androgens in clitorophallus development and possible applications to transgender patients. Andrology 9, 1719–1728. doi: 10.1111/andr.13016
Gruenbaum, E. (2001). The Female Circumcision Controversy: An Anthropological Perspective. Philadelphia, PA: University of Pennsylvania Press. doi: 10.9783/9780812292510
Gruenbaum, E. (2005). Socio-cultural dynamics of female genital cutting: research findings, gaps, and directions. Cult. Health Sex. 7, 429–441. doi: 10.1080/13691050500262953
Gruenbaum, E., Earp, B. D., and Shweder, R. A. (in press). Reconsidering the role of patriarchy in upholding female genital modifications: analysis of contemporary pre-industrial societies. Int. J. Impot. Res.
Gunning, I. R. (1991). Arrogant perception, world-travelling and multicultural feminism: the case of female genital surgeries. Columbia Human Rights Law Rev. 23, 189–248.
Hammond, T., and Carmack, A. (2017). Long-term adverse outcomes from neonatal circumcision reported in a survey of 1,008 men: an overview of health and human rights implications. Int. J. Human Rights 21, 189–218. doi: 10.1080/13642987.2016.1260007
Hegarty, P., Prandelli, M., Lundberg, T., Liao, L. M., Creighton, S., and Roen, K. (2021). Drawing the line between essential and nonessential interventions on intersex characteristics with European health care professionals. Rev. Gen. Psychol. 25, 101–114.
Hehir, B. (2022). Why we should be concerned about UK female genital mutilation laws and associated monitoring and reporting systems. Glob. Discourse 12, 131–143. doi: 10.1332/204378921X16343302385556
Hellsten, S. K. (2004). Rationalising circumcision: from tradition to fashion, from public health to individual freedom—critical notes on cultural persistence of the practice of genital mutilation. J. Med. Ethics 30, 248–253. doi: 10.1136/jme.2004.008888
Hennessy-Fiske, M. (2011, September 26). Injuries linked to circumcision clamps. Los Angeles Times. Available online at: https://www.latimes.com/health/la-xpm-2011-sep-26-la-he-circumcision-20110926-story.html
Hird, M. J. (2000). Gender's nature: intersexuality, transsexualism and the ‘sex'/'gender' binary. Feminist Theory 1, 347–364. doi: 10.1177/146470010000100305
Hirsi Ali, A. (2012). “The consequences can be worse for the boy than the girl,” in Uncredited Interview. Available online at: https://www.youtube.com/watch?v=NaEoQVZnN8I (accessed April 2, 2022).
Hodges, F. (1997). “A short history of the institutionalization of involuntary sexual mutilation in the United States,” in Sexual Mutilations, eds G. C. Denniston and M. F. Milos (Boston, MA: Springer US), 17–40. doi: 10.1007/978-1-4757-2679-4_2
Hodson, N., Earp, B. D., Townley, L., and Bewley, S. (2019). Defining and regulating the boundaries of sex and sexuality. Med. Law Rev. 27, 541–552. doi: 10.1093/medlaw/fwz034
hooks, b. (2004). The Will to Change: Men, Masculinity, and Love (Reprint edition). New York, NY: Washington Square Press.
Johnsdotter, S. (2013). Discourses on sexual pleasure after genital modifications: the fallacy of genital determinism (a response to J. Steven Svoboda). Global Dis. 3, 256–265.
Johnsdotter, S. (2018). “Girls and boys as victims: asymmetries and dynamics in European public discourses on genital modifications in children,” in FGM/C: From Medicine to Critical Anthropology, eds M. Fusaschi and G. Cavatorta (Turin: Meti Edizioni), 31–50.
Johnsdotter, S. (2019). Meaning well while doing harm: compulsory genital examinations in Swedish African girls. Sex. Reprod. Health Matters 27, 1–13. doi: 10.1080/26410397.2019.1586817
Johnsdotter, S., and Essén, B. (2010). Genitals and ethnicity: the politics of genital modifications. Reprod. Health Matters 18, 29–37. doi: 10.1016/S0968-8080(10)35495-4
Johnsdotter, S., and Wendel, L. (2022). Cultural change demands proportionate societal response in the handling of suspected FGM/C cases. Int. J. Impot. Res. doi: 10.1038/s41443-022-00535-x. [Epub ahead of print].
Johnson, M. T. (2010). Male genital mutilation: beyond the tolerable? Ethnicities 10, 181–207. doi: 10.1177/1468796810361654
Johnson-Agbakwu, C. E., and Manin, E. (2021). Sculptors of African women's bodies: forces reshaping the embodiment of female genital cutting in the West. Arch. Sex. Behav. 50, 1949–1957. doi: 10.1007/s10508-020-01710-1
Jones, M. (2017). Intersex genital mutilation – a Western version of FGM. Int. J. Children's Rights 25, 396–411. doi: 10.1163/15718182-02502008
Junos, L. (1998). Bodily Integrity for Both: The Obligation of Amnesty International to Recognize All Forms of Genital Mutilation of Males as Human Rights Violations, 1–30. Amnesty International Bermuda. Available online at: http://circumcisionharm.org/images-circharm.org/1998%20AI%20Report-Bodily%20Integrity.pdf (accessed April 2, 2022).
Kalampalikis, A., and Michala, L. (2021). Cosmetic labiaplasty on minors: a review of current trends and evidence. Int. J. Impot. Res. doi: 10.1038/s41443-021-00480-1. [Epub ahead of print].
Karlsen, S., Carver, N., Mogilnicka, M., and Pantazis, C. (2020). ‘Putting salt on the wound': a qualitative study of the impact of FGM-safeguarding in healthcare settings on people with a British Somali heritage living in Bristol, UK. BMJ Open 10, e035039. doi: 10.1136/bmjopen-2019-035039
Karlsen, S., Howard, J., Carver, N., Mogilnicka, M., and Pantazis, C. (2022). Available evidence suggests that prevalence and risk of female genital cutting/mutilation in the UK is much lower than widely presumed—policies based on exaggerated estimates are harmful to girls and women from affected communities. Int. J. Impot. Res. doi: 10.1038/s41443-021-00526-4. [Epub ahead of print].
Karlsen, S., Mogilnicka, M., Carver, N., and Pantazis, C. (2019). Female genital mutilation: empirical evidence supports concerns about statistics and safeguarding. BMJ, 364, 1915. doi: 10.1136/bmj.l915
Kart, S. (2020). The missing women of Sande: a necessary exercise in museum decolonization. African Arts. 53, 72–83. doi: 10.1162/afar_a_00539
Kelly, A., Kupul, M., Nake Trumb, R., Aeno, H., Neo, J., Fitzgerald, L., et al. (2012). More than just a cut: a qualitative study of penile practices and their relationship to masculinity, sexuality and contagion and their implications for HIV prevention in Papua New Guinea. BMC Int. Health Hum. Rights 12, 1–18. doi: 10.1186/1472-698X-12-10
Kelly, B., and Foster, C. (2012). Should female genital cosmetic surgery and genital piercing be regarded ethically and legally as female genital mutilation? BJOG Int. J. Obstet. Gynaecol. 119, 389–392. doi: 10.1111/j.1471-0528.2011.03260.x
Kigozi, G., Wawer, M., Ssettuba, A., Kagaayi, J., Nalugoda, F., Watya, S., et al. (2009). Foreskin surface area and HIV acquisition in Rakai, Uganda (size matters). AIDS 23, 2209–2213. doi: 10.1097/QAD.0b013e328330eda8
Kimmel, M. S. (2001). The kindest un-cut: feminism, Judaism, and my son's foreskin. Tikkun 16, 43–48. Available online at: http://www.cirp.org/pages/cultural/kimmel1/
Knight, M. (2001). Curing cut or ritual mutilation? Some remarks on the practice of female and male circumcision in Graeco-Roman Egypt. Isis 92, 317–338. doi: 10.1086/385184
KNMG. (2010). Nontherapeutic Circumcision of Male Minors, 1–17. Royal Dutch Medical Association KNMG. Available onlline at: http://www.circumstitions.com/Docs/KNMG-policy.pdf (accessed April 2, 2022).
Kratz, C. A. (2010). Affecting Performance: Meaning, Movement, and Experience in Okiek Women's Initiation. New York, NY: Wheatmark.
La Barbera, M. C. (2017). Ban without prosecution, conviction without punishment, and circumcision without cutting: a critical appraisal of anti-FGM laws in Europe. Glob. Jurist 17, 20160012. doi: 10.1515/gj-2016-0012
Larcher, V., and Hutchinson, A. (2010). How should paediatricians assess Gillick competence? Arch. Dis. Child. 95, 307–311. doi: 10.1136/adc.2008.148676
Latham, S. (2016). The campaign against female genital cutting: empowering women or reinforcing global inequity? Ethics Soc. Welfare 10, 108–121. doi: 10.1080/17496535.2016.1167227
Learner, H. I., Rundell, C., Liao, L.-M., and Creighton, S. M. (2020). ‘Botched labiaplasty': a content analysis of online advertising for revision labiaplasty. J. Obstet. Gynaecol. 40, 1000–1005. doi: 10.1080/01443615.2019.1679732
Leonard, L. (2000a). Interpreting female genital cutting: moving beyond the impasse. Annu. Rev. Sex Res. 11, 158–190. doi: 10.1080/10532528.2000.10559787
Leonard, L. (2000b). “We did it for pleasure only.” Hearing alternative tales of female circumcision. Qualitative Inquiry 6, 212–228. doi: 10.1177/107780040000600203
Lewis, H. (1995). Between Irua and “female genital mutilation”: feminist human rights discourse and the cultural divide. Harvard Human Rights J. 8, 1–55.
Liao, L.-M., Taghinejadi, N., and Creighton, S. M. (2012). An analysis of the content and clinical implications of online advertisements for female genital cosmetic surgery. BMJ Open 2, e001908. doi: 10.1136/bmjopen-2012-001908
Lightfoot-Klein, H., Chase, C., Hammond, T., and Goldman, R. (2000). “Genital surgeries on children below an age of consent,” in Psychological Perspectives on Human Sexuality, eds L. T. Szuchman and F. Muscarella (New York, NY: John Wiley & Sons), 440–479.
Loevinsohn, G., Kigozi, G., Kagaayi, J., Wawer, M. J., Nalugoda, F., Chang, L. W., et al. (2020). Effectiveness of voluntary medical male circumcision for HIV prevention in Rakai, Uganda. Clin. Infect. Dis. 73, e1946–e1953. doi: 10.1093/cid/ciaa1533
Lunde, I. B., Hauge, M.-I., Johansen, R. E. B., and Sagbakken, M. (2020). ‘Why did I circumcise him?' Unexpected comparisons to male circumcision in a qualitative study on female genital cutting among Kurdish–Norwegians. Ethnicities. 20, 1003–1024. doi: 10.1177/1468796819896089
Luseno, W. K., Field, S. H., Iritani, B. J., Rennie, S., Gilbertson, A., Odongo, F. S., et al. (2019). Consent challenges and psychosocial distress in the scale-up of voluntary medical male circumcision among adolescents in western Kenya. AIDS Behav. 23, 3460–3470. doi: 10.1007/s10461-019-02620-7
Luseno, W. K., Rennie, S., and Gilbertson, A. (2021). A review of public health, social and ethical implications of voluntary medical male circumcision programs for HIV prevention in sub-Saharan Africa. Int. J. Impot. Res. doi: 10.1038/s41443-021-00484-x. [Epub ahead of print].
MacNamara, N., Mackle, D., Pierson, C., and Bloomer, F. (2020). Interrogating the politicization of female genital cutting (FGC) within conditions of asymmetrical cultural convergence. A case study of Northern Ireland. Women's Stud. Int. Forum 82, 102391. doi: 10.1016/j.wsif.2020.102391
Majzoub, A., Arafa, M., Starks, C., Elbardisi, H., Al Said, S., and Sabanegh, E. (2017). 46 XX karyotype during male fertility evaluation; case series and literature review. Asian J. Androl. 19, 168–172. doi: 10.4103/1008-682X.181224
Manderson, L. (2004). Local rites and body politics: tensions between cultural diversity and human rights. Int. Feminist J. Politics 6, 285–307. doi: 10.1080/1461674042000211272
Martí, J. (2010). Tradition and change in circumcision: practices in Equatorial Guinea. Zeitschrift Für Ethnol. 135, 59–75.
Mashabane, B., and Henderson, N. (2020). Ulwaluko: ‘rights' of passage of gay men in South Africa. J. GLBT Fam. Stud. 16, 1–13. doi: 10.1080/1550428X.2020.1739487
Mason, C. (2001). Exorcising excision: medico-legal issues arising from male and female genital surgery in Australia. J. Law Med. 9, 58–67. Available online at: http://www.cirp.org/library/legal/mason1/
Mavundla, T. R., Netswera, F. G., Toth, F., Bottoman, B., and Tenge, S. (2010). How boys become dogs: stigmatization and marginalization of uninitiated Xhosa males in East London, South Africa. Qual. Health Res. 20, 931–941. doi: 10.1177/1049732310363804
Meel, B. L. (2010). Traditional male circumcision-related fatalities in the Mthatha area of South Africa. Med. Sci. Law 50, 189–191. doi: 10.1258/msl.2010.010017
Meissner, O., and Buso, D. L. (2007). Traditional male circumcision in the Eastern Cape–scourge or blessing? South Afr. Med. J. 97, 371–373. Available online at: https://hdl.handle.net/10520/EJC68998
Meleigy, M. (2007). Egypt tightens ban on female genital mutilation after 12 year old girl dies. BMJ. 335, 15. doi: 10.1136/bmj.39266.425752.DB
Meoded Danon, L. (2021). The parental struggle with the Israeli genital socialization process. Qual. Health Res. 31, 898–912. doi: 10.1177/1049732320984420
Merkel, R., and Putzke, H. (2013). After Cologne: male circumcision and the law. Parental right, religious liberty or criminal assault? J. Med. Ethics 39, 444–449. doi: 10.1136/medethics-2012-101284
Merli, C. (2008). Sunat for girls in southern Thailand: its relation to traditional midwifery, male circumcision and other obstetrical practices. Finnish J. Ethnicity Migrat. 3, 32–41. Available online at: https://dro.dur.ac.uk/5302/1/5302.pdf?DDD5+xlls97
Merli, C. (2010). Male and female genital cutting among Southern Thailand's Muslims: rituals, biomedical practice and local discourses. Cult. Health Sex. 12, 725–738. doi: 10.1080/13691051003683109
Möller, K. (2020). Male and female genital cutting: between the best interest of the child and genital mutilation. Oxf. J. Leg. Stud. 40, 508–532. doi: 10.1093/ojls/gqaa001
Monro, S., Carpenter, M., Crocetti, D., Davis, G., Garland, F., Griffiths, D., et al. (2021). Intersex: cultural and social perspectives. Cult. Health Sex. 23, 431–440. doi: 10.1080/13691058.2021.1899529
Monro, S., Crocetti, D., Yeadon-Lee, T., Garland, F., and Travis, M. (2017). Intersex, Variations of Sex Characteristics and DSD: The Need for Change. University of Huddersfield. Available online at: http://eprints.hud.ac.uk/id/eprint/33535/ (accessed April 2, 2022).
Moodley, K., and Rennie, S. (2018). Penile transplantation as an appropriate response to botched traditional circumcisions in South Africa: an argument against. J. Med. Ethics. 44, 86–90. doi: 10.1136/medethics-2016-103515
Moxon, S. (2017). Only male genital modification is 'control'—the female form is competition by women. New Male Stud. 6, 126–166. Available online at: https://www.researchgate.net/publication/33046746
Munzer, S. R. (2018). Examining nontherapeutic circumcision. Health Matrix 28, 1–77. Available online at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3180209
Myers, A., and Earp, B. D. (2020). What is the best age to circumcise? A medical and ethical analysis. Bioethics 34, 645–663. doi: 10.1111/bioe.12714
Njambi, W. N. (2004). Dualisms and female bodies in representations of African female circumcision: a feminist critique. Feminist Theory 5, 281–303. doi: 10.1177/1464700104040811
Njoroge, K. M., Cattan, M., Chinouya, M., and Ahlberg, B. M. (2022). Women as agents of change: male circumcision and HIV prevention in Kenya. Sexual. Cult. doi: 10.1007/s12119-021-09932-8. [Epub ahead of print].
Norton, A. T. (2013). Surveying risk subjects: public health surveys as instruments of biomedicalization. Biosocieties 8, 265–288. doi: 10.1057/biosoc.2013.20
Norton, A. T. (2017). Foreskin and the molecular politics of risk. Soc. Stud. Sci. 47, 655–680. doi: 10.1177/0306312717707360
Notini, L., and Earp, B. D. (2018, April 22). Iceland's Proposed Circumcision Ban. Pursuit (University of Melbourne). Available online at: https://pursuit.unimelb.edu.au/articles/iceland-s-proposed-circumcision-ban (accessed April 2, 2022).
Oba, A. A. (2008). Female circumcision as female genital mutilation: human rights or cultural imperialism? Glob. Jurist 8, 1–38. doi: 10.2202/1934-2640.1286
Obermeyer, C. M. (1999). Female genital surgeries: the known, the unknown, and the unknowable. Med. Anthropol. Q. 13, 79–106. doi: 10.1525/maq.1999.13.1.79
Obermeyer, C. M. (2003). The health consequences of female circumcision: science, advocacy, and standards of evidence. Med. Anthropol. Q. 17, 394–412. doi: 10.1525/maq.2003.17.3.394
Obermeyer, C. M. (2005). The consequences of female circumcision for health and sexuality: an update on the evidence. Cult. Health Sex. 7, 443–461. doi: 10.1080/14789940500181495
Obiora, L. A. (1996). Bridges and barricades: rethinking polemics and intransigence in the campaign against female circumcision. Case Western Reserve Law Rev. 47, 275–378.
O'Connell, H. E., Eizenberg, N., Rahman, M., and Cleeve, J. (2008). The anatomy of the distal vagina: towards unity. J. Sex. Med. 5, 1883–1891. doi: 10.1111/j.1743-6109.2008.00875.x
O'Donnell, N. A., and Hodes, D. (2018). “Female genital mutilation,” in Justice for Children and Families: A Developmental Perspective, eds M. Shaw, and S. Bailey (Cambridge: Cambridge University Press), 101–109. doi: 10.1017/9781108619554.013
O'Neill, S., Bader, D., Kraus, C., Godin, I., Abdulcadir, J., and Alexander, S. (2020). Rethinking the anti-FGM zero-tolerance policy: from intellectual concerns to empirical challenges. Curr. Sexual Health Rep. 12, 266–275. doi: 10.1007/s11930-020-00299-9
Onsongo, N. (2017). Female genital cutting (FGC): who defines whose culture as unethical? Int. J. Fem. Approaches Bioeth. 10, 105–123. doi: 10.3138/ijfab.10.2.105
Pardy, M., Rogers, J., and Seuffert, N. (2019). Perversion and perpetration in female genital mutilation law: the unmaking of women as bearers of law. Soc. Leg. Stud. 29, 273–293. doi: 10.1177/0964663919856681
Parker, R., Aggleton, P., and Jr, K. R. de C. (2015). Circumcision and HIV prevention: emerging debates in science, policies and programmes. Glob. Public Health 10, 549–551. doi: 10.1080/17441692.2015.1015705
Pippi Salle, J. L., Braga, L. P., Macedo, N., Rosito, N., and Bagli, D. (2007). Corporeal sparing dismembered clitoroplasty: an alternative technique for feminizing genitoplasty. J. Urol. 178(4 Suppl), 1796–1801. doi: 10.1016/j.juro.2007.03.167
Power, C. (2015). Hadza gender rituals–epeme and maitoko–considered as counterparts. Hunt. Gatherer Res. 1, 333–359.
Prazak, M. (2017). Making the Mark: Gender, Identity, and Genital Cutting. Athens, OH: Ohio University Press. doi: 10.2307/j.ctv224txfv
Price, C. (1999). “Male non-therapeutic circumcision: legal and ethical issues,” in Male and Female Circumcision, eds G. C. Denniston, F. M. Hodges, and M. F. Milos (Boston, MA: Springer US), 425–454. doi: 10.1007/978-0-585-39937-9_37
RACP (2010). Circumcision of Infant Males. Royal Australasian College of Physicians, 1–28. Available online at: https://www.racp.edu.au/docs/default-source/advocacy-library/circumcision-of-infant-males.pdf (accessed April 2, 2022).
Rashid, A. K., and Iguchi, Y. (2019). Female genital cutting in Malaysia: a mixed-methods study. BMJ Open 9, e025078. doi: 10.1136/bmjopen-2018-025078
Rashid, A. K., Iguchi, Y., and Afiqah, S. N. (2020). Medicalization of female genital cutting in Malaysia: a mixed methods study. PLoS Med. 17, e1003303. doi: 10.1371/journal.pmed.1003303
Rashid, A. K., Patil, S. S., and Valimalar, A. S. (2010). The practice of female genital mutilation among the rural Malays in north Malaysia. Internet J. Third World Med. 9, 1–8. doi: 10.5580/a23
Reis, E. (2013). “Intersex surgeries, circumcision, and the making of 'normal,”' in Genital Cutting: Protecting Children from Medical, Cultural, and Religious Infringements, eds G. C. Denniston, F. M. Hodges, and M. F. Milos (Amsterdam: Springer Netherlands), 137–147. doi: 10.1007/978-94-007-6407-1_10
Reis, E. (2019). Did bioethics matter? A history of autonomy, consent, and intersex genital surgery. Med. Law Rev. 27, 658–674. doi: 10.1093/medlaw/fwz007
Reis-Dennis, S., and Reis, E. (2021). The irrelevance of data to the ethics of intersex surgery. J. Pediatr. Ethics 1, 162–164. Available online at: https://scholarsbank.uoregon.edu/xmlui/handle/1794/26931
Rennie, S., Gilbertson, A., Hallfors, D., and Luseno, W. K. (2021). Ethics of pursuing targets in public health: the case of voluntary medical male circumcision for HIV-prevention programs in Kenya. J. Med. Ethics. 47, e51–e51. doi: 10.1136/medethics-2020-106293
Robertson, C. C., and James, S. M. (2002). Genital Cutting and Transnational Sisterhood: Disputing U.S. Polemics. Champaign, IL: University of Illinois Press.
Rogers, J. (2016). The first case addressing female genital mutilation in Australia: Where is the harm? Alternative Law J. 41, 235–238. doi: 10.1177/1037969X1604100404
Rogers, J. (2022). Remnants of mutilation in anti-FGM law in Australia. Glob. Discourse 12, 145–157. doi: 10.1332/204378921X16349692612474
Rosenberg, M. S., Gómez-Oliv,é, F. X., Rohr, J. K., Kahn, K., and Bärnighausen, T. W. (2018). Are circumcised men safer sex partners? Findings from the HAALSI cohort in rural South Africa. PLoS ONE 13, e0201445. doi: 10.1371/journal.pone.0201445
Rosman, M. E. (2022). Federalism and female circumcision in the US. Glob. Discourse 12, 159–166. doi: 10.1332/204378921X16264509095737
Rowanchilde, R. (1996). Male genital modification: a sexual selection interpretation. Human Nat. 7, 189–215. doi: 10.1007/BF02692110
Rudrum, S. (2020). Promoting male circumcision as HIV prevention in sub-Saharan Africa: an evaluation of the ethical and pragmatic considerations of adopting a demand creation approach. Glob. Public Health 15, 1349–1363. doi: 10.1080/17441692.2020.1761423
Rudrum, S., Oliffe, J. L., and Benoit, C. (2017). Discourses of masculinity, femininity and sexuality in Uganda's Stand Proud, Get Circumcised campaign. Cult. Health Sex. 19, 225–239. doi: 10.1080/13691058.2016.1214748
Runacres, S. A., and Wood, P. L. (2016). Cosmetic labiaplasty in an adolescent population. J. Pediatr. Adolesc. Gynecol. 29, 218–222. doi: 10.1016/j.jpag.2015.09.010
Šaffa, G., Zrzavý, J., and Duda, P. (2022). Global phylogenetic analysis reveals multiple origins and correlates of genital mutilation/cutting. Nat. Hum. Behav. doi: 10.1038/s41562-022-01321-x. [Epub ahead of print].
Sandland, R. (2019). The construction of gender and sexuality in the approach of key international law actors to the circumcision of children. Human Rights Law Rev. 19, 617–647. doi: 10.1093/hrlr/ngz030
Sarajlic, E. (2020). Children, culture, and body modification. Kennedy Inst. Ethics J. 30, 167–190. doi: 10.1353/ken.2020.0005
Savulescu, J. (2015). Bioethics: why philosophy is essential for progress. J. Med. Ethics 41, 28–33. doi: 10.1136/medethics-2014-102284
Schlegel, A., and Barry, H. (2017). Pain, fear, and circumcision in boys' adolescent initiation ceremonies. Cross-Cult. Res. 1, 1–29. doi: 10.1177/1069397116685780
Schröder, A., Farhat, W. A., Chiasson, D., Wilson, G. J., and Koyle, M. A. (2021). Serious and fatal complications after neonatal circumcision. Eur. Urol. Focus. doi: 10.1016/j.euf.2021.12.005. [Epub ahead of print].
Shahvisi, A. (2016). Cutting slack and cutting corners: an ethical and pragmatic response to Arora and Jacobs' ‘Female genital alteration: a compromise solution.' J. Med. Ethics 42, 156–157. doi: 10.1136/medethics-2015-103206
Shahvisi, A. (2017). Why UK doctors should be troubled by female genital mutilation legislation. Clin. Ethics 12, 102–108. doi: 10.1177/1477750916682671
Shahvisi, A. (2021). “FGM” vs. female “cosmetic” surgeries: Why do they continue to be treated separately? Int. J. Impot. Res. doi: 10.1038/s41443-021-00514-8. [Epub ahead of print].
Shahvisi, A., and Earp, B. D. (2019). “The law and ethics of female genital cutting,” in Female Genital Cosmetic Surgery: Solution to What Problem?, eds S. M. Creighton and L.-M. Liao (Cambridge: Cambridge University Press), 58–71. doi: 10.1017/9781108394673.007
Shell-Duncan, B. (2001). The medicalization of female “circumcision”: harm reduction or promotion of a dangerous practice? Soc. Sci. Med. 52, 1013–1028. doi: 10.1016/S0277-9536(00)00208-2
Shell-Duncan, B. (2008). From health to human rights: female genital cutting and the politics of intervention. Am. Anthropol. 110, 225–236. doi: 10.1111/j.1548-1433.2008.00028.x
Shell-Duncan, B., and Hernlund, Y. (2000). Female “Circumcision” in Africa: Culture, Controversy, and Change. Boulder, CO: Lynne Rienner Publishers.
Shweder, R. A. (2002). “What about female genital mutilation?' and why understanding culture matters in the first place,” in Engaging Cultural Differences: The Multicultural Challenge in Liberal Democracies, eds R. A. Shweder, M. Minow, and H. R. Markus (New York, NY: Russell Sage Foundation Press), 216–251.
Shweder, R. A. (2005). “When cultures collide: Which rights? Whose tradition of values? A critique of the global anti-FGM campaign,” in Global Justice and the Bulwarks of Localism: Human Rights in Context, eds C. L. Eisgruber and A. Sajó (Leiden: Martinus Nijhoff Publishers), 181–199. doi: 10.1163/9789047416005_012
Shweder, R. A. (2006). Customs control: some anthropological reflections on human rights crusades. Va. J. Soc. Policy Law. 14, 1–38.
Shweder, R. A. (2013). The goose and the gander: the genital wars. Glob. Discourse 3, 348–366. doi: 10.1080/23269995.2013.811923
Shweder, R. A. (2022a). Permitting gender equality in Abrahamic circumcision: the central argument – in retrospect and reply. Glob. Discourse 12, 211–244. doi: 10.1332/204378921X16394338241091
Shweder, R. A. (2022b). The prosecution of Dawoodi Bohra women: some reasonable doubts. Glob. Discourse 12, 9–27. doi: 10.1332/204378921X16141809582432
Shweder, R. A. (2023). “The prosecution of gender equal Abrahamic circumcision: implications for Jews and Muslims,” in Non-Coercive Threats to Freedom, eds J. Cole and A. Bilgrami (New York, NY: Columbia University Press). [Forthcoming].
Silverman, E. K. (2004). Anthropology and circumcision. Annu. Rev. Anthropol. 33, 419–445. doi: 10.1146/annurev.anthro.33.070203.143706
Smith, C. (2011). Who defines “mutilation”? Challenging imperialism in the discourse of female genital cutting. Feminist Format. 23, 25–46. doi: 10.1353/ff.2011.0009
Somerville, M. (2004). The Ethical Canary: Science, Society, and the Human Spirit. Montreal: McGill-Queen's University Press.
Sorrells, M. L., Snyder, J. L., Reiss, M. D., Eden, C., Milos, M. F., Wilcox, N., et al. (2007). Fine-touch pressure thresholds in the adult penis. BJU Int. 99, 864–869. doi: 10.1111/j.1464-410X.2006.06685.x
Steinfeld, R., and Earp, B. D. (2017). Could efforts to eliminate female genital cutting be strengthened by extending protections to male and intersex children? Reprod. Health 14, 115–115. Available online at: https://www.academia.edu/31889024
Svoboda, J. S. (2013). Promoting genital autonomy by exploring commonalities between male, female, intersex, and cosmetic female genital cutting. Glob. Discourse 3, 237–255. doi: 10.1080/23269995.2013.804757
Svoboda, J. S. (2017). Nontherapeutic circumcision of minors as an ethically problematic form of iatrogenic injury. AMA J. Ethics 19, 815–824. doi: 10.1001/journalofethics.2017.19.8.msoc2-1708
Svoboda, J. S., Adler, P. W., and Van Howe, R. S. (2016). Circumcision is unethical and unlawful. J. Law, Med. Ethics 44, 263–282. doi: 10.1177/1073110516654120
Svoboda, J. S., and Darby, R. (2008). “A rose by any other name? Symmetry and asymmetry in male and female genital cutting,” in Fearful Symmetries: Essays and Testimonies around Excision and Circumcision, Vol. 37, ed C. Zabus (Amsterdam; New York, NY: Editions Rodopi), 251–297.
Taher, M. (2017). Understanding Female Genital Cutting in the Dawoodi Bohra Community: An Exploratory Survey. Sahiyo: United Against Female Genital Cutting, 1–82. Available online at: https://sahiyo.files.wordpress.com/2017/02/sahiyo_report_final-updatedbymt2.pdf (accessed April 2, 2022).
Tangwa, G. B. (1999). “Circumcision: an African point of view,” in Male and Female Circumcision, eds G. C. Denniston, F. M. Hodges, and M. F. Milos (Boston, MA: Springer), 183–193. doi: 10.1007/978-0-585-39937-9_12
Tangwa, G. B. (2004). Bioethics, biotechnology and culture: a voice from the margins. Dev. World Bioeth. 4, 125–138. doi: 10.1111/j.1471-8731.2004.00088.x
Thomas, L. M. (1996). “Ngaitana (I will circumcise myself)”: the gender and generational politics of the 1956 ban on clitoridectomy in Meru, Kenya. Gend. Hist. 8, 338–363. doi: 10.1111/j.1468-0424.1996.tb00062.x
Toubia, N. F. (1999). “Evolutionary cultural ethics and the circumcision of children,” in Male and Female Circumcision, eds G. C. Denniston, F. M. Hodges, and M. F. Milos (Boston, MA: Springer), 1–7. doi: 10.1007/978-0-585-39937-9_1
Townsend, K. G. (2020). The child's right to genital integrity. Philos. Soc. Criticism 46, 878–898. doi: 10.1177/0191453719854212
Townsend, K. G. (2022). Defending an inclusive right to genital and bodily integrity for children. Int. J. Impot. Res. doi: 10.1038/s41443-022-00545-9. [Epub ahead of print].
Tye, M. C., and Sardi, L. M. (2022). Psychological, psychosocial and psychosexual aspects of penile circumcision. Int. J. Impot. Res. doi: 10.1038/s41443-022-00553-9. [Epub ahead of print].
Ungar-Sargon, E. (2015). On the impermissibility of infant male circumcision: a response to Mazor (2013). J. Med. Ethics 41, 186–190. doi: 10.1136/medethics-2013-101598
UNICEF and Innocenti Research Centre (2010). The Dynamics of Social Change: Towards the Abandonment of Female Genital Mutilation/Cutting in Five African Countries. Florence: UNICEF, Innocenti Research Centre.
van den Brink, M., and Tigchelaar, J. (2012). Shaping genitals, shaping perceptions: a frame analysis of male and female circumcision. Netherlands Quart. Human Rights 30, 417–445. doi: 10.1177/016934411203000404
van der Merwe, A. (2020). In response to an argument against penile transplantation. J. Med. Ethics. 46, 63–64. doi: 10.1136/medethics-2018-104795
van der Merwe, A., Toefy, Y., Moosa, M. R., van Deventer, H., and Scott, C. J. (2021). Living with someone else's penis: the lived experiences of two South African penile allograft recipients: a descriptive phenomenological study. Ann. Med. Surg. 69, 102794. doi: 10.1016/j.amsu.2021.102794
Wade, L. (2012). Learning from “female genital mutilation”: lessons from 30 years of academic discourse. Ethnicities 12, 26–49. doi: 10.1177/1468796811419603
Wahlberg, A., Påfs, J., and Jordal, M. (2019). Pricking in the African diaspora: current evidence and recurrent debates. Curr. Sexual Health Rep. 11, 95–101. doi: 10.1007/s11930-019-00198-8
Wallerstein, E. J. (1985). Circumcision: the uniquely American medical enigma. Urol. Clin. North Am. 12, 123–132. doi: 10.1016/S0094-0143(21)00798-9
Wawer, M. J., Makumbi, F., Kigozi, G., Serwadda, D., Watya, S., Nalugoda, F., et al. (2009). Circumcision in HIV-infected men and its effect on HIV transmission to female partners in Rakai, Uganda: a randomised controlled trial. Lancet 374, 229–237. doi: 10.1016/S0140-6736(09)60998-3
Weiss, C. (1966). Motives for male circumcision among preliterate and literate peoples. J. Sex Res. 2, 69–88. doi: 10.1080/00224496609550503
Werker, P. M. N., Terng, A. S. C., and Kon, M. (1998). The prepuce free flap: dissection feasibility study and clinical application of a super-thin new flap. Plastic Reconst. Surg. 102, 1075–1082. doi: 10.1097/00006534-199809020-00024
Whitehouse, H., and Lanmann, J. (2014). The ties that bind us: ritual, fusion and identification. Curr. Anthropol. 55, 674–695. doi: 10.1086/678698
WHO (2008). Eliminating Female Genital Mutilation: An Interagency Statement. Geneva: World Health Organization.
WHO (2010). Manual for Early Infant Male Circumcision Under Local Anaesthesia. Geneva: World Health Organization.
WHO (2015). Ending Violence and Discrimination Against Lesbian, Gay, Bisexual, Transgender, and Intersex People. Geneva: World Health Organization.
WHO (2020a). Preventing HIV Through Safe Voluntary Medical Male Circumcision for Adolescent Boys and Men in Generalized HIV Epidemics: Recommendations and Key Considerations. Geneva: World Health Organization.
Keywords: female genital mutilation (cutting), circumcision—male, intersex genital cutting, Global South, sex discrimination, gender based violence, World Health Organization
Citation: Earp BD (2022) Genital Cutting as Gender Oppression: Time to Revisit the WHO Paradigm. Front. Hum. Dyn. 4:778592. doi: 10.3389/fhumd.2022.778592
Received: 17 September 2021; Accepted: 28 March 2022;
Published: 10 June 2022.
Edited by:
Enrico Ripamonti, University of Brescia, ItalyReviewed by:
Daniela Carrillo, University of Milano-Bicocca, ItalyCopyright © 2022 Earp. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brian D. Earp, YnJpYW4uZWFycEBwaGlsb3NvcGh5Lm94LmFjLnVr
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.