- 1Department of Internal Medicine, University of Maryland Medical Center Midtown Campus, Baltimore, MD, United States
- 2Department of Internal Medicine, Hamad Medical Corporation, Doha, Qatar
- 3Department of Pharmacy and Practice, College of Pharmacy, Qatar University (QU) Health, Qatar University (QU), Doha, Qatar
- 4Department of Nursing Research, Hamad Medical Corporation, Doha, Qatar
- 5Department of Medical Oncology/Hematology, National Center for Cancer Care and Research, Hamad Medical Corporation, Doha, Qatar
Sickle cell disease (SCD) is a hemoglobin disorder inherited in an autosomal recessive pattern. Pain from vaso-occlusive crises (VOCs) is the most common symptom experienced by patients with SCD; thus, pain management constitutes a significant role in this patient population. We hypothesized that physicians with less favorable attitudes toward SCD patients are less likely to follow pain management guidelines. In this cross-sectional convenience sample survey, we aimed to assess the adherence of physicians in our institute to guidelines for the management of SCD pain crises and study the factors that are associated with non-adherence to these guidelines. Most surveyed physicians were early in their career and were found to adhere to the recommendations of using opioids and NSAIDs as a first-line therapy and avoiding using meperidine. On the other hand, some analgesic practices deviated from the recommendations, including less frequent assessment and reassessment of pain and response to pain medications and less frequent use of opioid patient-controlled analgesia (PCA). It is noteworthy that the frequency and severity of untreated pain in patients with SCD are associated with higher mortality, thus appropriate comprehensive care for such a vulnerable population should be prioritized and optimized. Although we did not find an association between the providers’ attitudes toward SCD patients and their pain management practices, improving these attitudes will promote the provider–patient relationship and its therapeutic outcomes. We conclude that the physicians taking care of SCD patients in our institute adhere to some of the guidelines in the field more than others. We also conclude that they have negative attitudes toward SCD patients; nevertheless, these did not affect their pain management practices.
1 Introduction
Sickle cell disease (SCD) is an autosomal recessive hemoglobin disorder affecting millions worldwide. It is prevalent among those with roots in South and Central America, Africa, the Caribbean, India, and Mediterranean countries such as Turkey, Greece, and Qatar (1, 2). The State of Qatar has a significant prevalence of homozygous SCD patients, with a prevalence of 0.71% of homozygous Hb-S disease among Qatari individuals (3). The history of malaria endemicity, large family size, and high rate of consanguinity in conjunction with tribe/clan endogamy made the Arabs unique from the point of view of genetic analysis. Therefore, this increased the prevalence of SCD in the Arabian Gulf region (4, 5).
Pain in patients with SCD is a prominent symptom that is classified as acute pain syndromes, including acute chest syndrome, hand-foot syndrome, and vaso-occlusive crises (VOCs); chronic pain syndromes, including arthralgia/arthritis and leg ulcers; and mixed pain syndromes where an acute pain is superimposed on chronic pain (6, 7).
Acute pain from VOCs can start as early as 6 months of age, recur unpredictably over a lifetime, and require treatment with strong analgesics, including opioids. Episodes of VOCs are the most common symptom experienced by SCD patients and the leading cause of emergency department (ED) visits. Common triggers for these episodes are infection, cold, dehydration, stress, and menses; nevertheless, most have no identifiable causes (8, 9). Pain management guidelines by the National Heart, Lung, and Blood Institute (NHLBI) (9) and the American Society of Hematology (ASH) (10) focus on the early and frequent reassessment of pain control and endorse using opioids as first-line analgesics. Previous studies (11) showed that negative attitudes in emergency physicians toward patients with SCD were associated with less adherence to these guidelines.
This study’s primary goal was to determine participating physicians’ self-reported adherence to the published guidelines for treating SCD patients presenting with VOCs. We hypothesized that physicians with negative attitudes toward SCD patients are less likely to adhere to the guidelines. We also hypothesized that specific clinical and demographic characteristics are associated with non-adherence to the guidelines. A secondary goal was to identify risk factors for guideline non-adherence.
Identifying provider-related risk factors associated with non-adherence to the guidelines will provide grounds for focused strategies to improve patients’ care.
2 Materials and methods
Our study is a cross-sectional convenience sample survey. Instrument design and validation are described below. The authors administered anonymous surveys during February and March 2022 in two hospitals in Hamad Medical Corporation in Qatar: one was a general hospital and the other was a hematology and oncology center. Both hospitals are staffed with attending physicians, fellows, and residents and mainly treat adult patients on site. The study was approved by the Hamad Medical Corporation Institutional Review Board and granted a waiver for informed consent (protocol code: MRC-01-21-211).
Physicians in the two hospitals’ internal medicine, hematology, and emergency departments were approached to participate in a self-administered survey. Based on a maximum number of target physicians (N=350), a margin error of 5%, a confidence level of 95%, and a response distribution of 50%, the estimated sample size required was 184. They were approached during breaks, before and after educational conferences, and after rounds. Surveys were distributed and collected by the investigators, who ensured every participant had privacy while completing the survey.
Respondents filled out paper questionnaires, the data were scanned and entered by the co-authors in accordance with a set protocol, and 15% of questionnaires were double-entered and checked for interrater agreement, with a mandatory cut-off of 98.5% agreement. All variables were checked for outliers (below the fifth and above the 95th percentile), and all implausible values were corrected. We administered a 32-item instrument containing items developed or adapted from the extant literature (Appendix A1).
The entire survey was grouped into three sections: demographics (nine items), provider practice patterns (six items), and provider attitudes (17 items). To measure attitudes, we administered the previously validated 17-item General Perceptions About Sickle Cell Patients Scale (12, 13). Subscales of the attitudes survey are reliable (Cronbach’s α 0.76 to 0.89).
The previously validated survey (11) was used to measure practice patterns; six new items were developed based on a literature review of analgesic practices for SCD patients. Eight recommendations for the management of SCD pain were identified from the NHLBI and American Pain Society guidelines. Provider practice pattern items were generated with these guidelines to explore analgesic practice patterns, including pharmacologic approaches (choice of agent, route, dose, and frequency of selection) and non-pharmacologic approaches.
The producers of the referenced paper and survey developed a set of practice pattern questions and assessed content validity, specifically face and utility validity, from a panel of five experts in emergency medicine and SCD (B.L., VT, LDR), a sickle cell hematologist (M.R.D.), and a patient perspective (CH) (Appendix A1). Expert reviews of the survey resulted in 100% agreement that the instrument covered the construct and content validity indices for each domain.
Data were inputted and managed by the statistical package SPSS v29 (Armonk, NY: IBM Corp). Continuous data were checked for normality using the Kolmogorov–Smirnov test. Descriptive statistics, i.e., mean ( ± SD), median (IQR), and frequency (%), were used to describe the data. Inferential statistics were used for analysis, i.e., Mann–Whitney U, Kruskal–Wallis, chi-square, and Fisher’s exact tests. A priori alpha level was set at 0.05.
3 Results
3.1 Characteristics of study subjects
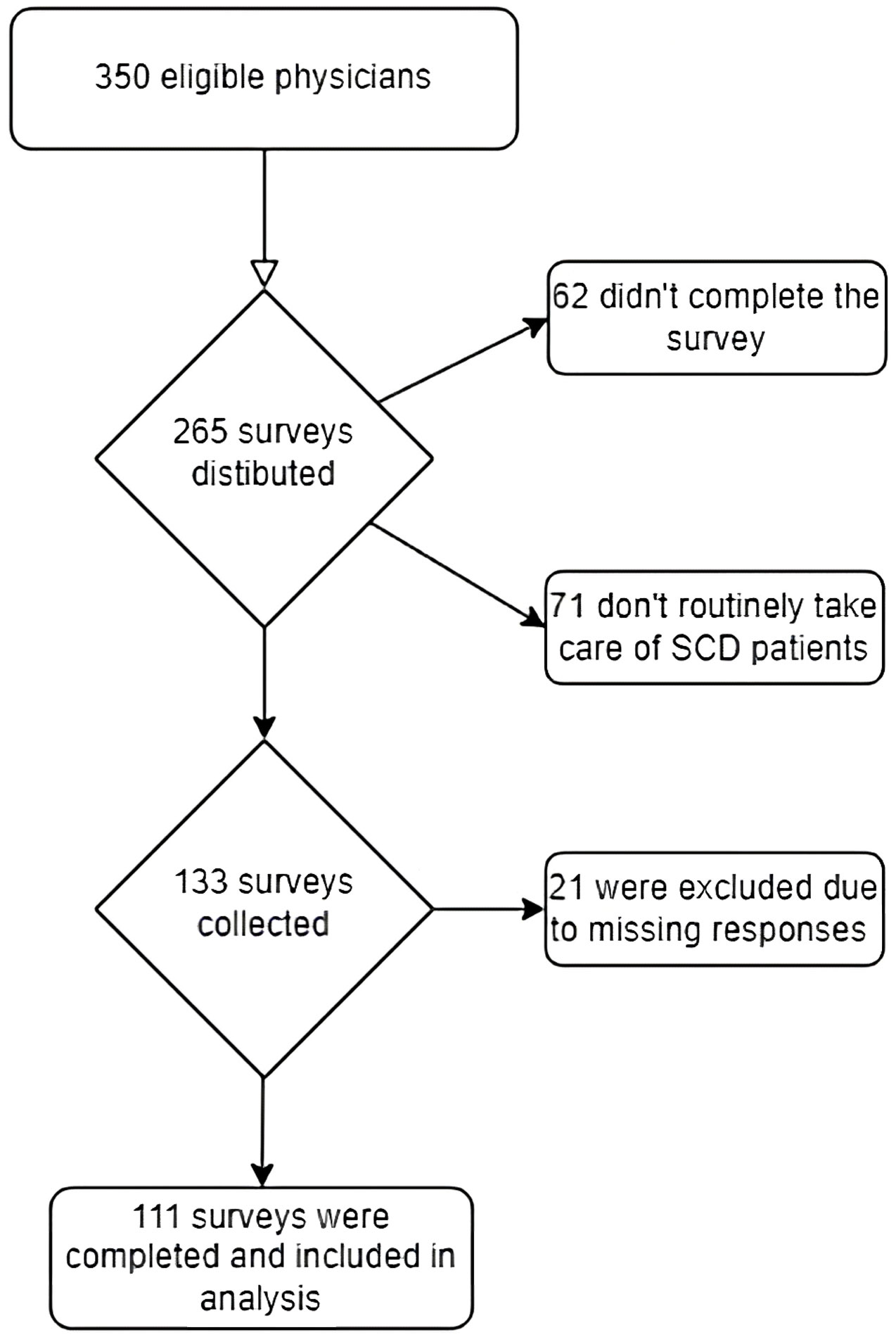
As described in the flow diagram in Figure 1, we distributed 265 surveys to eligible physicians in the two hospitals. Two hundred and three surveys were completed; 132 respondents indicated that they care for patients with SCD, and 111 responded entirely to the survey questions and were included in the analysis. All respondents practiced in urban teaching settings in the state of Qatar. The survey response rate was 77%, and the survey completion rate was 42%.
3.2 Demographics
Seventy-two percent of respondents were younger than 30 years of age, and 94% of the respondents were in training (residency and fellowship), while the rest were attending physicians. The male to female ratio is 4.5:1. Three-quarters of respondents reported treating one patient with SCD per week; the rest reported treating more than one patient with SCD per week.
The attitudes component of the survey was separated into three factors with good psychometric properties. Six items were grouped to form a negative attitudes scale (mean: 14; SD: 5.13; potential range 0 to 100). Higher scores on this scale indicated more negative views about SCD patients. Four items were grouped in a positive attitudes scale (mean: 11.97; SD: 4.10; potential range 0 to 100). Higher scores indicated more positive views about SCD patients. Finally, seven items were grouped to form the red-flag behaviors scale (mean: 14.46; SD: 5.12; potential range 0 to 100). Higher scores indicate a greater belief that certain SCD patient behaviors raise concern that the patient is inappropriately drug-seeking.
The attitudinal level of physicians regarding pain management in patients with SCD is shown in Table 1.
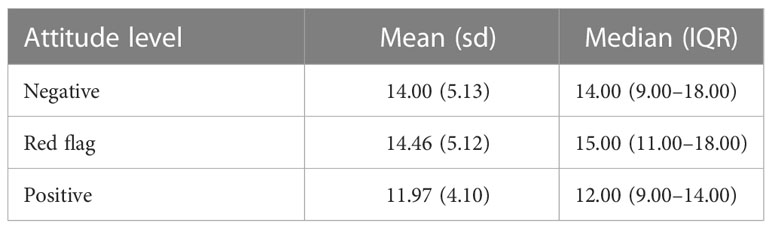
Table 1 The attitudinal level of physicians regarding pain management in patients with sickle cell disease.
3.3 Main results
The participating physicians in our institute scored higher on the red-flag behaviors scale (mean: 14.46; SD: 5.12; potential range 0 to 100) and negative attitudes scale (mean: 14; SD: 5.13; potential range 0 to 100) than on the positive attitudes scale (mean: 11.97; SD: 4.10; potential range 0 to 100). These findings indicate a substantial inclination to express negative attitudes toward SCD patients. It is concerning that the majority of young physicians in the study tended to demonstrate predominantly unfavorable attitudes toward this population of patients.
3.3.1 Association between demographics and attitude
We studied the association between the demographic and practice profiles of the surveyed physicians and their attitudes toward SCD patients as determined by the three attitude scores mentioned earlier.
The following factors were associated with significant differences in attitude scores: level of practice and frequency of use of the word “sicklers” to refer to SCD patients. Compared to attending physicians, fellows and residents had statistically significantly higher scores for negative and positive attitudes, whereas red-flags behavior scores did not have statistically significant differences between these groups. For the frequency of use of the word “sicklers,” statistically significant differences were found on the red-flag behavior score; those who reported that they “always” or “frequently” used the word “sicklers” had higher scores on the red-flag behavior score. On the other hand, no statistically significant differences were found in the positive or negative attitude scores between these groups.
We did not find significant differences in positive attitude, negative attitude, or red-flag behavior scores between different age and gender groups. Likewise, no statistically significant differences were found between physicians from different departments (internal medicine, hematology, and emergency medicine) or between physicians who treated a high volume of SCD patients, defined as more than one patient weekly, and those who treated a low volume of SCD patients.
3.3.2 Adherence to guidelines
Analgesic practices among our surveyed physicians that were consistent with current recommendations for pain management during VOCs included using parenteral morphine and NSAIDs and avoiding using meperidine.
Ninety-one percent of respondents reported prescribing morphine routinely to patients with VOCs, making it the analgesic agent most commonly prescribed in our study. Fifty-four percent of the respondents administered morphine via the subcutaneous route, whereas intravenous and oral morphine was administered by 37% and 12% of the respondents, respectively. None of the respondents reported routine use of intramuscular morphine.
NSAIDs were prescribed by 60% of the respondents, and acetaminophen was prescribed by 77% of them. On the other hand, some analgesic practices deviated from the recommendations, including less frequent assessment and reassessment of pain and response to pain medications and less frequent use of opioid patient-controlled analgesia (PCA). Only 21% of the respondents reported being comfortable with delivering a second or third dose of opioids within 30 min, while 22% reported being comfortable with delivering a second or third dose of opioids within 30–60 min for inadequate analgesia. Over 50% of the respondents reported reassessing the pain and the response to analgesics in longer intervals (>60 min). Opioid PCA was routinely prescribed by only 20% of respondents.
3.3.3 Association between demographics and adherence to guidelines
Demographic factors, including age, gender, level of practice (resident, attending), and different departments, had no significant association with adherence to analgesic guidelines. However, the frequency of use of the term “sicklers” to describe SCD patients was associated with a significant change in practice; those who rarely used that word were more likely to avoid using meperidine in pain management correctly. Furthermore, the volume of SCD patients treated per week had no significant relationship with adherence to analgesics guidelines.
3.3.4 Association between attitude and adherence to guidelines
We also studied the association between positive, negative, and red-flag behavior scores and adherence to the recommendations for pain management during VOCs.
3.3.4.1 Opioids as first-line analgesics
The hypothesis we studied was that physicians with poor attitudes toward SCD patients were less likely to use opioids as first-line analgesics. However, our findings deviated from that.
We discovered that higher scores for negative attitude and red-flag behavior were associated with a more frequent prescription of morphine. Conversely, higher scores for positive attitude were associated with a less frequent prescription.
It is important to acknowledge that pain management behaviors are complex and multifaceted. Other unmeasured factors, such as individual preferences, social support, or past treatment outcomes, could have influenced participants’ practices and led to an underestimation of the impact of attitudes on these practices. These unexpected contradictory findings warrant further investigation.
3.3.4.2 Frequent reassessment of pain
Our data analysis shows that more frequent redosing (<30 min) of opioids in patients with inadequate pain management was associated with the highest scores for negative attitude and red-flag behavior: medians of 18 (IQR: 5.5) and 17 (IQR: 3), respectively. It was also associated with a positive attitude score of 12 (IQR: 4) (min: 9; max: 16).
On the other hand, less frequent redosing of opioids (>120 min) was associated with lower scores for negative attitude and red-flag behavior: medians of 12 (IQR: 9.5) and 14 (IQR: 10), respectively. It was also associated with the highest score for positive attitude: median of 16 (IQR: 8).
3.3.4.3 Use of non-steroidal anti-inflammatory drugs (represented by ibuprofen)
There was no statistically significant difference in the three attitude scores between physicians prescribing non-steroidal anti-inflammatory drugs (NSAIDs) more frequently versus those prescribing them less frequently.
Further details and the association between the rest of the pain management recommendations and attitude scores are depicted in Appendix A2.
4 Discussion
Our study aimed to assess the adherence to SCD VOC pain management guidelines by the physicians in our institute. Most physicians adhered to the routine prescription of opioids but were less adherent to the frequent reassessment of pain and response to analgesics. Patients presenting with acute pain in the ED were given priority for treatment. There are around 3,000 SCD patients in Qatar, among whom 500 have severe phenotypes, requiring hospitalization between 2 and 10 times annually.
Pain management recommendations by NHLBI (2014) and ASH (2020) (9, 10) focus on rapid assessment of pain and analgesic requirements in patients presenting with VOCs and rapid reassessment of response to analgesics (in intervals shorter than 30 min). They also endorse the use of parenteral opioids and NSAIDs during these episodes. As described above, analgesic practices of our surveyed physicians were consistent with the recommendations, including using parenteral morphine and NSAIDs and avoiding using meperidine. However, frequent reassessment and redosing of opioids and using PCA opioids were less adhered to, which might have resulted from fears of opioid overdosing and fears of inducing opioid dependence. Meperidine used to be the most frequently used opioid analgesic in SCD pain management (14); however, due to its neurotoxic adverse effects, such as seizures, its use is no longer recommended (9).
Most of the factors we studied were not associated with statistically significant effects on pain management practices in patients with SCD and adherence to the published guidelines. Referring to patients with SCD as “sicklers” has been previously postulated to be associated with poorer attitudes and management of these patients (15). In our study, those who rarely used that word were more likely to avoid using meperidine in pain management, which aligns with the guidelines. Furthermore, those who reported that they “always” or “frequently” used that word had higher scores on the red-flag behavior score.
Attitudes toward patients with SCD, as determined by the attitude scores (positive, negative, and red flag), did not have a significant association with adherence to pain management guidelines. Our study showed that many physicians taking care of patients with SCD presenting with VOCs could have negative attitudes toward these patients. Although data analysis did not show any significant impact of this attitude on pain management, other studies did. For example, Glassberg et al. (11) concluded that negative attitudes in emergency physicians toward patients with SCD were associated with less adherence to pain management guidelines. Identifying the patterns of negative attitudes toward this patient population in various institutes is a step toward improving their care.
Significant barriers to effective VOC management are inadequate pain assessment, limited knowledge of SCD, and misinformation or bias against opioid use. Such biases result from ignorance about opioid tolerance and physical dependence, and confusion about addiction. Fear of addiction is common among patients, families, and healthcare workers; however, it is usually unwarranted and contributes to undertreating patients with VOCs and unnecessary increases in their suffering.
Wright et al. (16) reported that concerns regarding opioid dependence and addiction were major factors impacting the provision of adequate pain management to patients with SCD. Our results showed that the surveyed physicians were highly concerned about drug-seeking behavior in patients with SCD (median of 15). Patients with SCD are presumed to be opioid dependent because they frequently need analgesics and are sometimes kept on a chronic pain regimen. However, previous studies suggest the opposite. For example, a study by Ruta et al. (17) in 2016 used Center for Disease Control (CDC) data covering deaths from 1999 until 2013. It followed the trend of people dying from opioid pain reliever (OPR) overdose. It reported that in 2013, 16,225 people died due to OPR overdose, while only 10 patients with SCD died due to OPR overdose. This trend was maintained over all these years, with a mean number of deaths of 11,664 ± 4,701 in non-SCD patients and 6.3 ± 2.58 in SCD patients (P <.001). It also showed that the percentage of SCD patients who died from OPR overdose was less than that seen in non-cancer pain conditions, including fibromyalgia and back pain.
Another study (18) assessed the impacts of the opioid epidemic on pain management in SCD patients. Fifteen patients were interviewed and reported that their access to opioid analgesics had become more restricted, and that they were facing increasing difficulties in filling out their prescriptions at pharmacies. They also described increased stigmatization about opioid use and that their medical care was affected by the physicians’ exclusive focus on reducing pain medication use.
That being said, we want to highlight that the frequency and severity of untreated pain in patients with SCD are associated with higher mortality. In a paper published in the New England Journal of Medicine by O S Platt et al. (19) on life expectancy and circumstances of death in patients with SCD, 33% of deaths occurred in relatively healthy SCD patients during SCD sickle crises. Seventy-eight percent of these patients died during an acute painful episode or acute chest syndrome. Given the frequency of their occurrence and their vast impact on the quality of life and survival of SCD patients, prompt and proper management of VOCs should be an important goal for every healthcare professional (9).
Our study had limitations. We distributed 265 surveys to eligible physicians: 203 surveys were completed, 132 respondents indicated that they take care of patients with SCD, and 111 responded entirely to the survey questions and were included in the analyses. Since those who completed the survey were more likely to be more aware of and adhere to the published guidelines, this could be a source of response bias. On the other hand, most respondents were young and still in training as residents and fellows, which may implicate reduced awareness and adherence to existing pain management guidelines. In addition, while the male-to-female ratio of physicians in the three departments was close to 2:1, the ratio of respondents was 4.5:1. Lastly, three-quarters of respondents report treating one patient with SCD per week. However, we found no association between the number of SCD patients treated weekly and attitudes on the one hand and between the number of SCD patients treated weekly and analgesic practices on the other. This reflects that the majority of the surveyed physicians, being early-career physicians, have a low volume of SCD patients and thus lack expertise in this field.
Our hospital guidelines were adapted from the ASH guidelines and treatment recommendations. SCD patients in Qatar are followed up in hematology clinics per ASH guidelines in a multidisciplinary and comprehensive care manner. Each patient is evaluated and followed up to improve his/her quality of life and to prevent end-organ damage, including echocardiogram, renal function tests, and evaluation from various medical specialists.
New challenges are arising nowadays in Qatar due to the expansion of the hospital system, which now includes more than 14 hospitals. Our doctors come from different backgrounds and have different levels of training. This further highlights the need for more robust education and awareness about SCD management. As for the cultural factors, SCD patients in the state of Qatar come from large families and tribes. As a result, they usually get good socioeconomic support, which helps promote their mental health and general well-being.
SCD patients remain particularly vulnerable, as a large percentage belong to a poorly represented racial group in healthcare settings and a large percentage are children and adolescents. Appropriate comprehensive care for such a vulnerable population should be prioritized and optimized. Conducting similar studies to assess adherence to guidelines and prepare grounds for changes in local healthcare providers’ practices can be significantly valuable. Moreover, participation in similar studies might lead to participants’ reflection on their deficiencies that pertain to SCD pain management guidelines, which should also improve the care provided to SCD patients.
Although we did not find an association between the providers’ attitudes toward SCD patients and their pain management practices, improving these attitudes will promote the provider–patient relationship and its therapeutic outcomes.
To address the discussed challenges, comprehensive studies need to be conducted on a larger scale to explore areas requiring improvement within this complex patient population. Future surveys should incorporate specific questions pertaining to knowledge of published guidelines in SCD pain management. Understanding the reasons for negative attitudes and non-adherence to guidelines should also be a focus of future studies, and these inquiries should be incorporated into the survey methodology. Furthermore, it would be beneficial for scientific societies such as ASH, the American College of Physicians (ACP), and the American Academy of Pediatrics (AAP) to issue practice statements endorsing adherence to guidelines and supporting appropriate behaviors, thus promoting constructive changes.
From our perspective, the proposed solutions entail physicians familiarizing themselves with pain management guidelines and actively working to improve their attitudes and behaviors toward SCD patients. Additionally, institutions can contribute by providing local practice guidelines to their physicians and promoting adherence through quality assessment and improvement projects. By implementing these strategies collectively, we can strive toward addressing the identified challenges and improving the care provided to individuals with SCD.
5 Conclusion
Physicians who participated in our study exhibited a tendency to utilize opioids and NSAIDs routinely in the management of VOCs. However, there was a lack of frequent reassessment of pain levels or response to analgesics. Our study did not find any correlation between physicians’ attitudes toward patients with SCD and their approach to pain management; however, it revealed a notable association between the frequency of using the term “sicklers” and a higher score for red-flag behavior, which could indicate concerning conduct. We also noted that the majority of our younger physician sample tended to have negative attitudes toward SCD patients, which is alarming and needs to be addressed. It is imperative to tackle negative attitudes and their underlying causes, especially among young physicians, through anti-stigma education and policies for patients seeking pain relief. Initiatives should be undertaken to enhance healthcare providers’ comprehension of established guidelines in the domain of SCD management to improve patient satisfaction and reduce morbidity and mortality rates. Emphasis on this aspect of SCD management is paramount for improving patient outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The study was approved by Hamad Medical Corporation Institutional Review Board and granted a waiver from informed consent (protocol code: MRC-01-21-211).
Author contributions
Conceptualization, AI and MY; Data curation, MY; Formal analysis, MI and KS; Funding acquisition, MY; Investigation, A I, AA, MAb, MS, and MAr; Methodology, AI, MI, and MY; Project administration, AI and MY; Resources, MY; Software, MI; Supervision, MY; Writing—original draft, AI, AA, MAb, MS, and MA; Writing—review and editing, A I, AA, MAb, MS, MAr, MI, and MY. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the Qatar National Library. Open Access funding provided by the Qatar National Library.
Conflict of interest
Authors AI, AA, MAb, MS, MAr KS, and MY were employed by Hamad Medical Corporation.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author MY declared that they were an editorial board member of Frontiers at the time of submission. This had no impact on the peer review process and the final decision.
The authors declare that this study will receive funding from Academic Health System, Hamad Medical Corporation. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhem.2023.1214902/full#supplementary-material
References
1. El-Hazmi MAF, Al-Hazmi AM, Warsy AS. Sickle cell disease in Middle East Arab countries. Indian J. Med. Res. (2011) 134(5):597–610. doi: 10.4103/0971-5916.90984
2. Khamees I, Ata F, Choudry H, Soliman AT, De Sanctis V, Yassin MA. Manifestations of HbSE sickle cell disease: a systematic review. J. Transl. Med. (2021) 19(1):262. doi: 10.1186/s12967-021-02931-1
3. Fawzi ZO, Al Hilali A, Fakhroo N, Al Bin Ali A, Al Mansour S. Distribution of hemoglobinopathies and thalassemias in Qatari nationals seen at Hamad hospital in Qatar. Qatar Med. J. (2003) 2003:11. doi: 10.5339/qmj.2003.1.11
4. Wali Y, Kini V, Yassin MA. Distribution of sickle cell disease and assessment of risk factors based on transcranial Doppler values in the Gulf region. Hematology (2020) 25(1):55–62. doi: 10.1080/16078454.2020.1714113
5. Ata F, Rahhal A, Malkawi L, Iqbal P, Khamees I, Alhiyari M, et al. Genotypic and phenotypic composition of sickle cell disease in the Arab population-a systematic review. Pharmacogenomics Pers Med. (2023) 31:133–44. doi: 10.2147/PGPM.S391394
6. Elenga N, Loko G, Etienne-Julan M, Al-Okka R, Adel AM, Yassin MA. Real-world data on efficacy of L- glutamine in preventing sickle cell disease-related complications in pediatric and adult patients. Front. Med. (Lausanne) (2022) 9:931925. doi: 10.3389/fmed.2022.931925
7. Adel AA, Abushanab D, Hamad A, Al-Badriyeh D, Yassin MA. L-glutamine and Crizanlizumab for adults with sickle cell disease (SCD) in Qatar: a cost effectiveness analysis. Blood (2021) 138(Supplement 1):4945. doi: 10.1182/blood-2021-144636
8. Soliman AT, Yasin M, El-Awwa A, Abdelrahman MO, De Sanctis V. Does blood transfusion affect pituitary gonadal axis and sperm parameters in young males with sickle cell disease? Indian J. Endocrinol. Metab. (2013) 17(6):962– 8. doi: 10.4103/2230-8210.122599
9. Cabana MD, Kanter J, Marsh AM, Treadwell MJ, Rowland M, Stemmler P, et alBarriers to pediatric sickle cell disease guideline recommendations. Glob Pediatr Health (2019) 6:2333794X19847026. doi: 10.1177/2333794X19847026
10. Brandow AM, Carroll CP, Creary S, Edwards-Elliott R, Glassberg J, Hurley RW, et al. American Society of Hematology 2020 guidelines for sickle cell disease: management of acute and chronic pain. Blood Adv (2020) 4(12):2656–701. doi: 10.1182/bloodadvances.2020001851
11. Glassberg JA, Tanabe P, Chow A, Harper K, Haywood C Jr., DeBaun MR, et al. Emergency provider analgesic practices and attitudes toward patients with sickle cell disease. Ann. Emerg. Med. (2013) 62(4):293–302.e10. doi: 10.1016/j.annemergmed.2013.02.004
12. Haywood C Jr., Lanzkron S, Hughes MT, Brown R, Massa M, Ratanawongsa N, et al. A video-intervention to improve clinician attitudes toward patients with sickle cell disease: the results of a randomized experiment. J. Gen. Intern. Med. (2011) 26(5):518–23. doi: 10.1007/s11606-010-1605-5
13. Christison GW, Haviland MG, Riggs ML. The medical condition regard scale: measuring reactions to diagnoses. Acad. Med. (2002) 77(3):257–62. doi: 10.1097/00001888-200203000-00017
14. Ballas SK. Meperidine for acute sickle cell pain in the emergency department: revisited controversy. Ann. Emerg. Med. (2008) 51(2):217. doi: 10.1016/j.annemergmed.2007.09.033
15. Glassberg J, Tanabe P, Richardson L, Debaun M. Among emergency physicians, use of the term “Sickler” is associated with negative attitudes toward people with sickle cell disease. Am. J. Hematol. (2013) 88(6):532–3. doi: 10.1002/ajh.23441
16. Wright K, Adeosum O. Barriers to effective pain management in sickle cell disease. Br. J. Nurs (2009) 18(3):158–61. doi: 10.12968/bjon.2009.18.3.39043
17. Ruta NS, Ballas SK. The opioid drug epidemic and sickle cell disease: guilt by association. Pain Med. (2016) 17(10):1793–8. doi: 10.1093/pm/pnw074
18. Sinha CB, Bakshi N, Ross D, Krishnamurti L. Management of chronic pain in adults living with sickle cell disease in the era of the opioid epidemic: a qualitative study. JAMA Netw. Open (2019) 2(5):e194410. doi: 10.1001/jamanetworkopen.2019.4410
Keywords: vaso-occlusive crisis, painful crisis, opioids, sickle-cell disease, sicklers, behaviors
Citation: Ismail A, Aqel A, Abumuhfouz M, Safieh M, Arabyat M, Ibrahim M, Singh K and Yassin MA (2023) Knowledge, attitude, and practice of physicians regarding pain management in patients with Sickle cell disease. Front. Hematol. 2:1214902. doi: 10.3389/frhem.2023.1214902
Received: 30 April 2023; Accepted: 26 June 2023;
Published: 04 August 2023.
Edited by:
Evangelia Yannaki, G. Papanikolaou General Hospitali, GreeceReviewed by:
Marina Economou, Aristotle University of Thessaloniki, GreeceSaliou Diop, Cheikh Anta Diop University, Senegal
Copyright © 2023 Ismail, Aqel, Abumuhfouz, Safieh, Arabyat, Ibrahim, Singh and Yassin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdellatif Ismail, YWJkb193YXFxYWRAeWFob28uY29t; Mohamed A. Yassin, eWFzc2lubW9oYUBnbWFpbC5jb20=
 Abdellatif Ismail
Abdellatif Ismail Ali Aqel2
Ali Aqel2 Ma’in Abumuhfouz
Ma’in Abumuhfouz Mohamed Ibrahim
Mohamed Ibrahim Mohamed A. Yassin
Mohamed A. Yassin