- 1Department of Applied Health Sciences, College of Medicine and Health, University of Birmingham, Birmingham, United Kingdom
- 2Health Services Management Centre, College of Social Sciences, University of Birmingham, Birmingham, United Kingdom
- 3Eve Hill Surgery, Dudley, United Kingdom
- 4School of Psychology, University of Coventry, Coventry, United Kingdom
Access to UK general practice is complicated by the need to provide equitable and universal care within a system adapting to workforce challenges, digital innovation, and unprecedented demand. Despite the importance of accessing primary care in meeting the overall aim of delivering equitable care, this is the first time the direct and indirect influence of policies intended to facilitate access have been systematically explored. Further consideration by policymakers is needed to accommodate the difference between what patients need and what patients want when accessing primary care, and the differences in their ability to utilise digital options. The designation of care was hindered by long-standing issues of reliable data and variations in the interpretation of local and national protocols and guidelines.
1 Introduction
Although health care systems worldwide possess different financial motivations, staffing models, clinical capability, and capacity, they are all predicated on facilitating timely and appropriate access to care (1–4). In high income countries this access tends to begin with primary care, more specifically general or family practice where it is facilitated by a range of facilities, localities, clinical disciplines, and digital components (5). However, despite the best efforts of policymakers, funders and senior decision-makers, delays and inequities in access persist across multiple health systems (6). These are exacerbated by a lack of evidence that contextualises the implementation and interaction of central health care policies with the localised influences of individual primary care organisations, health care providers, and patients (7).
In the United Kingdom (UK) issues around access to healthcare, in particular access to primary care, have risen to national prominence, garnering the interest of the mainstream media and becoming the focus of political debate (8). The Royal College of General Practitioners (RCGP), has expressed concern that there has been no systematic attempt to explore the failings and strengths in securing access to primary care (9). This includes the contextual influences of patient needs and preferences, staff attitudes, training, and experience, and the various characteristics of primary care organisations (10).
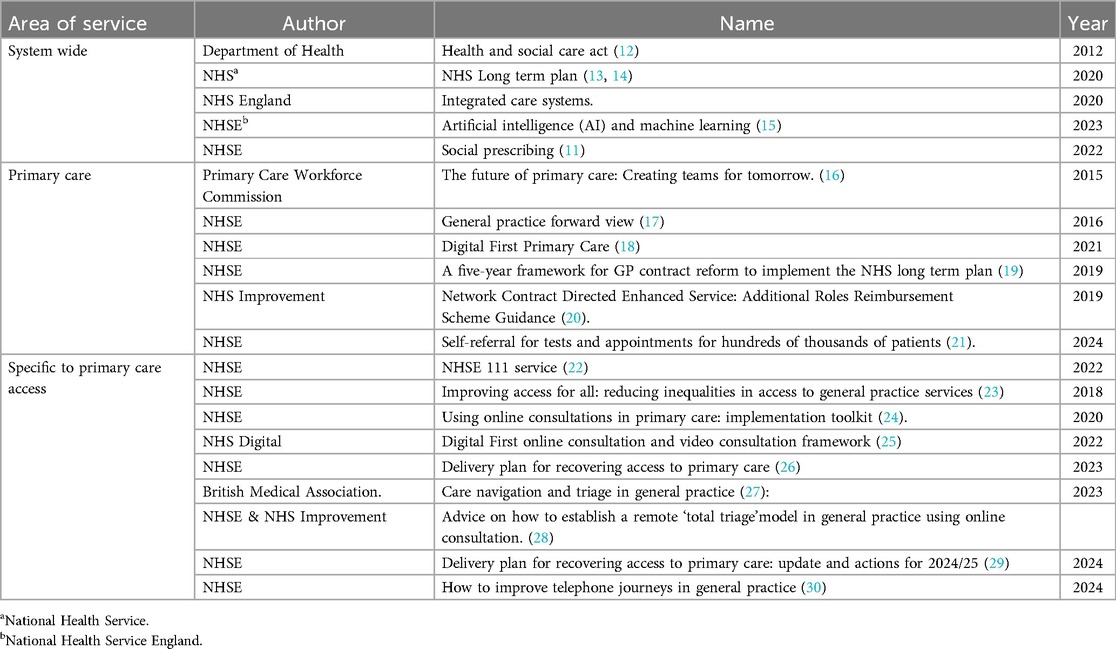
Over the last decade the National Health Service England (11) has introduced multiple policies and various funding streams in an attempt to improve primary care access; these include those directly aimed at a specific elements of access such as improving telephone systems, or increasing the use of digital first appointment booking; those more broadly aimed at the scope and delivery of primary care, such as the inclusion of additional non-clinical roles into the practice team, and finally the broader delivery of the health service such as the move to integrated health and care systems as described in Table 1. In all cases, their implementation as it affects primary care has been complicated by the growing demands of an ageing population, increasingly complex options for treatment and care, the challenges of reduced GP recruitment and retention (31, 32) and an evidence base limited in focus to discrete patient groups defined by condition or age (33–35). The work presented here uses process visualisation, namely a Service Blueprint, to unpick the process of primary care access and in turn the influences of individual and collective policies, ultimately providing a series of recommendations for future policy development applicable both to the NHSE and elsewhere.
1.1 Process visualisation
In the absence of any previous depiction of the process of accessing primary care we created a Service Blueprint (36, 37), a tool widely used in designing, delivering, or understanding new and established (health) service offerings (38–40). They have been used in a range of contexts that involve multiple people, processes, and channels of communication (40). They have been successfully applied to a range of healthcare environments and processes including the exploration of digital healthcare (41, 42), shared provider-patient decision making (43, 44), and delivering patient centred care (45, 46).
The service blueprint was developed using a secondary descriptive qualitative analysis relating to the procedural aspects of accessing care drawn from the lived experience of 52 staff (including GPs, nurses, practice managers, and receptionists) and 27 patients from five practices within the English Midlands (47). This was.corroborated by documental evidence drawn from practice protocols, independent reports, and existing academic literature (48). The resulting blueprint describes the individuals involved, their roles, actions, and support systems within two phases, the first is Patient Assessment, consisting of the initiation of contact by patients and the subsequent contact with service providers, including provider information gathering and patient negotiation; the second is Care Designation, describing the allocation of care whether within the practice or external settings or sources of support (49, 50). See Figure 1 for the blueprint describing access to primary care.
2 Policy options and implications
2.1 Patient assessment phase
2.1.1 Patient/frontstage actions
2.1.1.1 In-person/telephone request
Access typically begins with patients’ synchronous in-person or telephone contact with practice staff (51). Traditionally patients in the UK would be expected to access practices as a walk-in patient reflecting the history of general practice where single-handed practices serving smaller numbers of patients were the norm (52). In the last two decades the growth in size, and reduction in number of practices has meant their boundaries have been extended and such walk-in appointments are becoming rarer, with a marked increase in telephone contact (53). However, this is not universal and, in areas of high-deprivation, frustration with remote access and in some cases individual practice organisation protocols, means that attending in-person remains a preferred, or only viable option (54).
Currently patient attempts to access general practice in NHSE begin with contacting the practice via telephone (51). The ease of telephone access has been under closer scrutiny since the pandemic when what were already sometimes significant waits have become significantly longer (55–57). The additional burden of these waits can discourage some from seeking care entirely (57–61). In response in 2023 NHSE introduced ring-fenced funding to improve call management systems though their impact is as yet unexplored (62).
Patients can also contact NHS urgent care without needing a GP referral via the NHS 111 clinical assessment service system (63), a service designed to provide advice and signposting for people with urgent health-care problems. However, latest evidence suggests it has done little to reduce the pressure on direct contact with practices as it is seldom used by older or less well-educated patients i.e., the population groups most frequently in contact with general practice (64–66).
2.1.1.2 Online access
The NHSE have attempted to relieve some of the acknowledged pressure on front-line administrators by providing patients with the opportunity to independently book routine appointments on-line via patient portals and the multi-purpose NHS App (67, 68). In an attempt to broaden its use NHSE have issued detailed guidance to help practices with their implementation and integration of online booking (24). The latest iterations of these booking portals are growing in sophistication to include online symptom checkers, mechanisms for self-referral, and closer interaction with the NHS 111 system (63, 66, 69–71). All are available through the NHS App (68).
Take up of online booking is growing more slowly than anticipated, and used disproportionately by those that are younger and more affluent (57, 70, 72, 73), highlighting the discrepancies between UK policymakers move to digitalisation and the reality of it exacerbating existing health inequalities (74).
The use of online portals and their associated symptom checkers offers the potential of a streamlined automated booking service that can use algorithms to direct patients to the most appropriate care, but to function as expected they must be fed reliable data which currently does not exist, a precept for the expected use of AI in the role (26). Currently the efficacy of these systems means that the benefit of longitudinal contextual understanding of individual patients is lost, alongside that of in-person contact when assessing patients’ clinical need (75–79).
2.1.1.3 Access negotiation
For patients contacting the practice in person, the member of the practice team that typically processes patient requests is the receptionist (51), a role requiring no formal training or qualifications (75). In performing this role, receptionists assimilate formally described medical data from the patient's electronic health record (EHR), GP notes and recommendations, alongside patient descriptions of their symptoms and other contextual information, though not all patients are willing to disclose medical information to non- medically trained receptionists (51, 80).
Subsequent negotiations can be complicated, not every patient wants the same outcome, for example some might want the earliest available appointment but others a consultation with their usual or preferred clinician (51). It is also important that socio-cultural influences are accommodated, for example those from black and minority ethnic backgrounds prefer to wait for a clinician of the same gender (23, 81, 82) or the elderly may prefer in person appointments instead of teleconsultations (55).
This highlights the importance of understanding the discrepancy between what patients want from that initial contact and what commissioners and policymakers consider a successful outcome (83). Though waiting times for GP appointments are seen as the key metric, meeting patients’ expectations for seeing their preferred GP is currently not routinely recorded (84–87).
2.2 Care designation phase
2.2.1 Patient/frontstage actions
Various options are available when allocating care for patients including in-person, telephone or virtual appointments. Though traditionally this appointment would be with a GP they are increasingly conducted with an alternative member of the practice's clinical team or signposted to a source of care and support external to the practice (27, 88).
2.2.1.1 Teleconsultations
In 2019 NHSE declared that all GP practices should promote and offer remote i.e., telephone, online, or video consultations to their patients as an option for consulting with busy clinicians (19). This Digital First model offers patients a face-to-face consultation only when deemed necessary (26, 89, 90). Since COVID, teleconsultations have become the most frequently offered option in UK general practice (91). The use of digital routes is intended to make access easier; however, failure to account for the lack of connectivity and digital literacy in underserved populations is leading to an exacerbation of health disparities through the “digital divide” (92).
2.2.1.2 In-person practice appointments
Decisions on directing patients to in-person practice appointments are informed by capacity and clinical need, including whether they should be seen by the GP. However, recent NHSE initiatives have intended to ease the burden on busy GPs by filtering patients towards alternative members of a more multi-disciplinary practice team (67, 93–96). To further support this the NHS introduced the Additional Roles Reimbursement Scheme, consisting of 17 new roles intending to improve access for patients. This includes clinical roles such as Advanced Nurse Practitioners (97), and practice-based physiotherapists (98), or pharmacists (67, 99, 100) as well as new non-clinical roles such as social prescribers (101) and health and well-being coaches (102). It is understood that for these to become an accepted option patients need education as to their value and role in supporting health (9). Physician Associates are being increasingly used in general practice, although they remain controversial with the British Medical Association asserting that they pose a risk to patient safety due to their lack of clinical training (103). The most recent evidence suggests that these initiatives have broadened expertise but failed to reduce GP burden, with issues around the scope and expectations of those in additional roles, their management and support infrastructure, and ultimately their sustained integration and career progression (104).
2.2.1.3 Signposted externally
In recognition that people's health and wellbeing are determined predominantly by a range of social, economic and environmental factors, the NHS Long-Term Plan includes a commitment to offer more effective navigation across the health and social care system in an attempt to address these social determinants of health (67, 105, 106). The NHS is also placing a growing emphasis on the use of third sector organisations (e.g., charities, social enterprises and community groups) (107), facilitated by the growing role of social prescribers (108) and other lay health workers who provide synthetic forms of social support in the community (109). These individuals have basic training and are responsible for referring patients to a range of public, voluntary and community sector organisations with a focus on improving their health and well-being (108, 110). Despite their proliferation there is little evidence of their efficacy (111).
Patients might be signposted to community-based resources associated with, or contracted by, the NHS including local pharmacies (112). These have long been considered a useful opportunity to relieve the pressure on access to primary care and in 2023 the Department of Health's policy directive Recovering Access to Primary Care included funding and training to support patients attending pharmacies for the prescription of antibiotics and a range of other care solutions (62, 113–115).
2.3 Patient assessment and care designation
2.3.1 Backstage actions
These ‘backstage’ actions performed by front line service providers happen beyond the eye of the patient and include staff accessing clinical management systems, consultation with colleagues, and referral to practice protocols.
2.3.2 The clinical management system
In designating care, staff are required to locate the relevant patient information from within their practice's software based clinical management system (CMS) which incorporates the electronic health record, booking facilities, notes from GPs, reminders, referral letters and other patient-related information (116, 117). The patient data stored on the CMS is fragmented and not always current with longstanding issues around governance and interoperability with similar clinical systems in secondary care (118–121). Though a widely acknowledged concern, progress on linking data sets across NHS settings has been slow (67, 122, 123), despite NHS Supply Chain publishing open standards that technology suppliers must now comply with (67, 124).
2.3.3 Consulting with practice colleagues
The BMA has recently released guidance on triage and signposting in general practice recognising the previous absence of formal recommendations (27). Prior to this general practice receptionists typically relied on formal and informal advice, and shared responsibility and accountability with clinical and non-clinical members of the practice team (93, 125). The level and consistency of the support they receive from their colleagues is dependent upon the culture of individual practice organisations and the experience of those approached (126).
The success of such inter-professional connection relies on non-judgmental channels of communication and a working culture that flattens organisational hierarchies (127–129). With the scope and scale of primary care organisations expanding, informal and formal communication has been supported by the successful introduction of micro-teams consisting of GP, administrator, and a nurse or health care assistant (93, 130–132).
2.3.4 Reference to practice protocols
In the UK individual general practices develop their own protocols to support patient access, often informed by the interpretation and implementation of national and local policies and priorities (27, 133). Although there is some lattitude the overall performance of practices is regulated by the Clinical Care Commission (134). The protocols relating to access can incorporate a number of different elements according to whether usual care or urgent cases and the criteria for same-day access (35, 54, 135).
Adherence to these protocols varies some of which is due to vague definitions and poor understanding of protocols and processes (86, 87, 136, 137). Some of the variation is due to the discretion of individual staff members, a discretion given implicit legitimacy by senior practice colleagues who acknowledge that receptionists must be flexible in their approach to accommodate limited resources (54, 126). Such discretionary decision-making, and its impacts on the delivery and outcomes of broader policies has been witnessed in front line providers in other public sector services, where it has been earned the term street-level bureaucracy (126, 138, 139).
2.4 Support processes
The processes and policies that underlie primary care access include those that facilitate an extended primary care network, the impact of nationally implemented clinical guidelines, and the policy driven initiatives for training and qualifications of those facilitating access to care.
2.4.1 Extended clinical networks
The UK Health and Social Care Act of 2022 has seen the integration of health and social care in new bodies called Integrated Care Systems (ICS) designed to unite NHS organisations, social care providers, and local authorities in planning and delivering locally relevant services (140). These are run by Integrated Care Boards with their stakeholders drawn from across care settings and communities (141). It is expected that ICSs will reinforce previously incoherent links between primary, secondary, and social care though there have been calls for the Department of Health and Social Care to remodel existing funding frameworks to incentivise greater integration and shared responsibility (87, 142).
The latest evidence suggests that primary care leaders and managers remain unclear about the role of general practice within these integrated models (143). There are also concerns that GPs’ priorities will be overshadowed by the larger funding and political influence afforded acute trusts (141). This is problematic in the context of expectations that primary care's management of chronic conditions and provision of preventative care will alleviate much of the pressure on secondary care (144, 145).
2.4.2 Evidence-based clinical guidance
The delivery of evidence-based medicine in general practice is directed by national guidance intended to support equitable and consistent care (146, 147). These guidelines are expected to underpin consistent, high quality care, through their local implementation and integration with existing protocols and processes (148). They include elements of access and signposting yet these guidelines are not always followed despite the introduction of financial incentives (149). A number of reasons for this have been identified including uncertainty surrounding their relevance to patients, inadequate remuneration, or technical support, and an underlying lack of resource necessary to deliver them (150). Subsequently there have been calls for greater engagement of those creating these guidelines with representatives of the various organisational, social, cultural, and community contexts in which they will be implemented (150, 151).
2.4.3 Training and qualifications for access
As described elsewhere, in UK primary care those most frequently charged with facilitating access are receptionists, unqualified but expected to fulfil a range of functions including making consequential decisions on patient priority and access, and including acting on red flags if patients present potentially serious symptoms (51, 54, 148). Recently, this aspect of their role has been acknowledged as distinct and worthy of NHSE policymakers as recategorization as care navigators and specialised training to signpost patients to various sources of help, advocacy and support (87, 96, 137, 152–154).
The growing role of remote triaging or otherwise processing patient requests remotely is made more difficult by the loss of visual cues (51, 54, 137, 155–157). Its growing prominence has been recognised as deserving of specific training both for clinical and non-clinical members of the practice team (9, 62).
3 Actionable recommendations
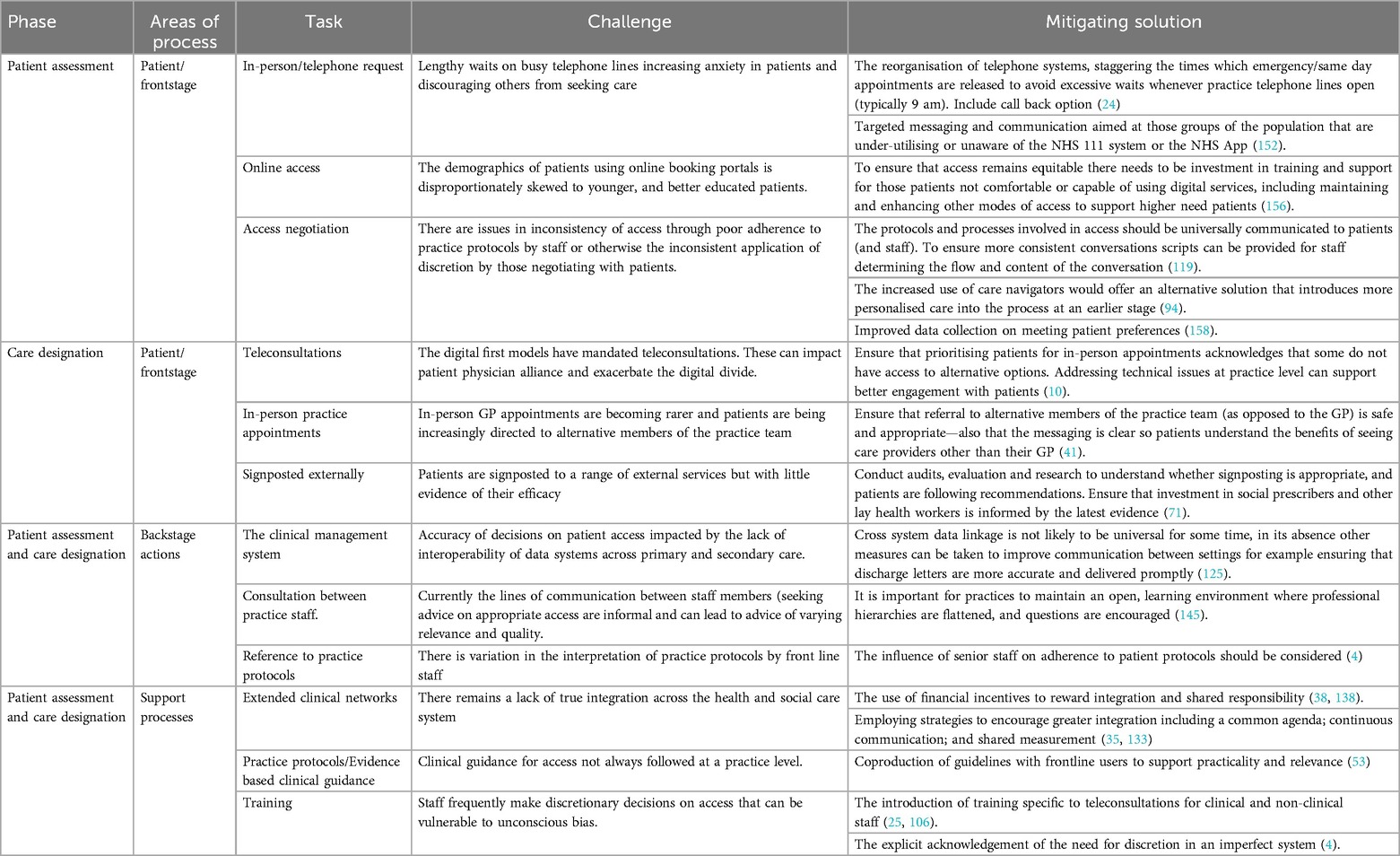
We have summarised the issues uncovered despite or because of existing policy initiatives and suggested practicable mitigations in Table 2.
4 Conclusions
To the best of our knowledge this is the first time anywhere, but certainly in the UK, the complex processes of accessing primary care have been isolated, visualised, and described in the context of the impact of policy. Unpicking the various interlinked components via a Service Blueprint has allowed a more precise description of the impact of various policies and service initiatives on a range of established and novel health service processes and interventions (40, 159). The blueprint we created was based on the largest purposely collected qualitive data set yet to explore access to primary care in the UK, and corroborated with a range of policy and peer-reviewed literature (48, 141, 142, 160). We acknowledge that work has only focussed on the UK and that although comprehensive in the range of health policies discussed primary care organisations do not sit in isolation. There may be broader societal and cultural influences on the way in which patients are able, or prefer to, access care. However, it remains a useful demonstration of how a process visualisation can support commissioners and policymakers understanding of the impact of their decisions on patient and staff experience (158, 161, 162).
Safe and consistent access to general practice is an integral element of the equitable and personalised future of NHSE care provision. However, the growing reliance on remote and digital solutions risks leaving large parts of the population disadvantaged and reinforcing existing health inequalities. This brief has provided yet further evidence of how future policy design would benefit from closer attention to the experiences of patients and front-line providers and we recommend in particular that greater efforts are made to consult marginalized communities.
Author contributions
IL: Conceptualization, Formal Analysis, Funding acquisition, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing. NG: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing. SG: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing. DS: Writing – review & editing. MB: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The work was funded by the Health Foundation Grant number: 7452.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kringos DS, Boerma WG, Hutchinson A, Saltman RB. Building Primary Care in a Changing Europe, World Health Organization. Geneva: Regional Office for Europe (2015).
2. Ford JA, Gkiouleka A, Kuhn I, Sowden S, Head F, Siersbaek R, et al. Reducing health inequalities through general practice: protocol for a realist review (EQUALISE). BMJ Open. (2021) 11(6):e052746. doi: 10.1136/bmjopen-2021-052746
3. Saunders CL, Flynn S, Massou E, Lyratzopoulos G, Abel G, Burt J. Sociodemographic inequalities in patients’ experiences of primary care: an analysis of the general practice patient survey in England between 2011 and 2017. J Health Serv Res Policy. (2021) 26(3):198–207. doi: 10.1177/1355819620986814
4. Pratt C, Taylor R, Smith SD. Health equity and access to health care as a social determinant of health: the role of the primary care provider. Prim Care. (2023) 50(4):549–59. doi: 10.1016/j.pop.2023.04.006
5. Porter J, Boyd C, Skandari MR, Laiteerapong N. Revisiting the time needed to provide adult primary care. J Gen Intern Med. (2023) 38(1):147–55. doi: 10.1007/s11606-022-07707-x
6. Organization, W. H. Tracking Universal Health Coverage: 2023 Global Monitoring Report. Geneva: World Health Organization (2023).
7. Kuhlmann E, Groenewegen PP, Bond C, Burau V, Hunter DJ. Primary care workforce development in Europe: an overview of health system responses and stakeholder views. Health Policy. (2018) 122(10):1055–62. doi: 10.1016/j.healthpol.2018.07.021
8. Gregory A. Millions of Patients a Month Wait Longer Than a Fortnight to see GP in England. Manchester: The Guardian (2024).
9. Royal College of General Practitioners. (2021). The future role of remote consultations & patient ‘triage’: general practice COVID-19 recovery. (2021).
10. Ward B, Lane R, McDonald J, Powell-Davies G, Fuller J, Dennis S, et al. Context matters for primary health care access: a multi-method comparative study of contextual influences on health service access arrangements across models of primary health care. Int J Equity Health. (2018) 17:1–12. doi: 10.1186/s12939-018-0788-y
11. NHSE. Social prescribing. Available online at: https://www.england.nhs.uk/personalisedcare/social-prescribing/ (Accessed May 02, 2024).
12. Department of Health and Social Care. Health and Social Care Act 2012. (2012) (Accessed May 02, 2024).
13. NHS. NHS Long term plan (2020) Available online at: https://www.longtermplan.nhs.uk/ (Accessed May 02, 2024).
14. NHS England. Integrated Care Systems. London: NHS (2020). Available online at: https://www.england.nhs.uk/integratedcare/integrated-care-systems (Accessed 2020).
15. NHSE. Artificial Intelligence (AI) and Machine Learning. London: National Health Service UK (2023). Available online at: https://www.england.nhs.uk/long-read/artificial-intelligence-ai-and-machine-learning/#:∼:text=Symptom%20checkers%20such%20as%20NHS,data%20scientists%20and%20product%20designers
16. Roland M, Barber N, Howe A, Imison C, Rubin G, Storey K. The Future of Primary Health Care: Creating Teams for Tomorrow: Report by the Primary Care Workforce Commission. London: Health Education England (2015).
17. NHS England. General Practice Forward View. (2016). Available online at: https://webarchive.nationalarchives.gov.uk/ukgwa/20240703092032/https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-collections/general-practice-forward-view-gpfv (Accessed June 06, 2024).
18. NHS England. Digital First Primary Care (2021). Available online at: https://www.england.nhs.uk/gp/digital-first-primary-care/ (Accessed June 06, 2024).
19. England N. A Five-year Framework for GP Contract Reform to Implement the NHS Long Term Plan. London: NHS England (2019).
20. England N, Improvement N. Network Contract Directed Enhanced Service: Additional Roles Reimbursement Scheme Guidance. London: NHS (2019).
21. National Health Service England. NHS Self-referral for Tests and Appointments for Hundreds of Thousands of Patients. London: National Health Service England (2024). Available online at: https://www.england.nhs.uk/2024/04/nhs-self-referral-for-tests-and-appointments-for-hundreds-of-thousands-of-patients/
22. NHS. NHS 111 (2022). Available online at: https://111.nhs.uk/ (Accessed June 06, 2024).
23. NHS England. Improving access for all: reducing inequalities in access to general practice services. (2018).
24. England N. Using Online Consultations in Primary Care: Implementation Toolkit. London: NHS England (2020).
25. Digital N. Digital First Online Consultation and Video Consultation Framework. London: National Health Service UK (2022). Available online at: https://digital.nhs.uk/services/digital-care-services-catalogue/digital-first-online-consultation-and-video-consultation-framework
27. British Medical Association. Care Navigation and Triage in General Practice. London: BMA (2023). Available online at: https://www.bma.org.uk/advice-and-support/gp-practices/managing-workload/care-navigation-and-triage-in-general-practice#:∼:text=Clinical%20triage%20is%20a%20clinical,within%20the%20practice%20or%20elsewhere
28. England N, Improvement N. Advice on how to Establish a Remote ‘total Triage’model in General Practice Using Online Consultations. London: NHS England (2020).
29. NHSE. Delivery Plan for Recovering Access to Primary Care: Update and Actions for 2024/25. London: National Health Service England (2024). Available online at: https://www.england.nhs.uk/long-read/delivery-plan-for-recovering-access-to-primary-care-update-and-actions-for-2024-25/
30. NHSE. How to Improve Telephone Journeys in General Practice. London: National Health Service England (2024). Available online at: https://www.england.nhs.uk/long-read/how-to-improve-telephone-journeys-in-general-practice/.
31. Macdonald N, Clements C, Sobti A, Rossiter D, Unnithan A, Bosanquet N. Tackling the elective case backlog generated by COVID-19: the scale of the problem and solutions. J Public Health. (2020) 42(4):712–6. doi: 10.1093/pubmed/fdaa155
32. Henley J, Connolly K, Jones S, Giuffrida A. A ticking time bomb’: healthcare under threat across Western Europe. The Guardian. (2022) 14.
33. Monteny M, Berger MY, van der Wouden JC, Broekman BJ, Koes BW. Triage of febrile children at a GP cooperative: determinants of a consultation. Br J Gen Pract. (2008) 58(549):242–7. doi: 10.3399/bjgp08X279643
34. Moffat J, Hinchliffe R, Ironmonger L, Osborne K. Identifying anticipated barriers to help-seeking to promote earlier diagnosis of cancer in Great Britain. Public Health. (2016) 141:120–5. doi: 10.1016/j.puhe.2016.08.012
35. Wilson A, Coleby D, Regen E, Phelps K, Windridge K, Willars J, et al. Service factors causing delay in specialist assessment for TIA and minor stroke: a qualitative study of GP and patient perspectives. BMJ Open. (2016) 6(5):e011654. doi: 10.1136/bmjopen-2016-011654
36. Stanley M. Qualitative Descriptive: A Very Good Place to Start. Qualitative Research Methodologies for Occupational Science and Therapy. London: Routledge (2014). p. 21–36.
37. Litchfield I, Gale N, Burrows M, Greenfield S. Protocol for using mixed methods and process improvement methodologies to explore primary care receptionist work. BMJ Open. (2016) 6(11):e013240. doi: 10.1136/bmjopen-2016-013240
39. Holdford DA. Using service blueprints to visualize pharmacy innovations. Pharmacy (Basel). (2019) 7(2). doi: 10.3390/pharmacy7020043
40. Joseph AL, Kushniruk AW, Borycki EM. Patient journey mapping: current practices, challenges and future opportunities in healthcare. Knowledge Manag E-Learning. (2020) 12(4):387–404. doi: 10.34105/j.kmel.2020.12.021
41. Weir NM, Newham R, Corcoran ED, Al-Gethami AAA, Abd Alridha AM, Bowie P, et al. Application of process mapping to understand integration of high risk medicine care bundles within community pharmacy practice. Res Social Adm Pharm. (2018) 14(10):944–50. doi: 10.1016/j.sapharm.2017.11.009
42. Alkandari M, Ryan K, Hollywood A. The experiences of people living with peripheral neuropathy in Kuwait—a process map of the patient journey. Pharmacy. (2019) 7(3):127. doi: 10.3390/pharmacy7030127
43. Selwood A, Senthuran S, Blakely B, Lane P, North J, Clay-Williams R. Improving outcomes from high-risk surgery: a multimethod evaluation of a patient-centred advanced care planning intervention. BMJ Open. (2017) 7(2):e014906. doi: 10.1136/bmjopen-2016-014906
44. Peng K, Liu H, Zhang J, Yang M, Liu Y, Tian M, et al. Applying normalization process theory and process mapping to understand implementation of a co-management program for older hip fracture patients in China: a qualitative study. Arch Osteoporos. (2020) 15(1):1–10. doi: 10.1007/s11657-020-00760-1
45. Philpot LM, Khokhar BA, DeZutter MA, Loftus CG, Stehr HI, Ramar P, et al. Creation of a patient-centered journey map to improve the patient experience: a mixed methods approach. Mayo Clin Proc Innov Qual Outcomes. (2019) 3(4):466–75. doi: 10.1016/j.mayocpiqo.2019.07.004
46. Tran V-T, Diard E, Ravaud P. Priorities to improve the care for chronic conditions and multimorbidity: a survey of patients and stakeholders nested within the ComPaRe e-cohort. BMJ Qual Saf. (2021) 30(7):577–87. doi: 10.1136/bmjqs-2020-011219
47. Burrows MJ. The Use of Process Improvement Methodologies to Equip Receptionists for Their Clinical Roles in General Practice. Birmingham: University of Birmingham (2020).
48. Young WB, Ryu H. Secondary data for policy studies: benefits and challenges. Policy Politics Nurs Pract. (2000) 1(4):302–7. doi: 10.1177/152715440000100408
49. Odland ML, Whitaker J, Nepogodiev D, Aling CA, Bagahirwa I, Dushime T, et al. Identifying, prioritizing and visually mapping barriers to injury care in Rwanda: a multi-disciplinary stakeholder exercise. World J Surg. (2020) 44(9):2903–18. doi: 10.1007/s00268-020-05571-6
50. Sijm-Eeken M, Zheng J, Peute L. Towards a lean process for patient journey mapping - A case study in a large academic setting. Stud Health Technol Inform. (2020) 270:1071–5. doi: 10.3233/SHTI200326
51. Litchfield L, Burrows M, Gale N, Greenfield S. Understanding the invisible workforce: lessons for general practice from a survey of receptionists. BMC Prim Care. (2021) 23(1):230. doi: 10.1186/s12875-022-01842-4
53. Tan S, Mays N. Impact of initiatives to improve access to, and choice of, primary and urgent care in England: a systematic review. Health Policy. (2014) 118(3):304–15. doi: 10.1016/j.healthpol.2014.07.011
54. Burrows M, Gale N, Greenfield S, Litchfield I. A quantitative assessment of the parameters of the role of receptionists in modern primary care using the work design framework. BMC Fam Pract. (2020) 21(1):1–10. doi: 10.1186/s12875-020-01204-y
55. Murphy M, Scott LJ, Salisbury C, Turner A, Scott A, Denholm R, et al. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br J Gen Pract. (2021) 71(704):e166–77. doi: 10.3399/BJGP.2020.0948
57. IPSOS. (2022). GP Survey. Available online at: https://www.gp-patient.co.uk/ (Accessed June 06, 2024).
58. Mair FS, May CR. Thinking about the burden of treatment. Br Med J. (2014) 349:349. doi: 10.1136/bmj.g6680
59. Litchfield I, Bentham L, Hill A, McManus RJ, Lilford R, Greenfield S. Routine failures in the process for blood testing and the communication of results to patients in primary care in the UK: a qualitative exploration of patient and provider perspectives. BMJ Qual Saf. (2015) 24(11):681–90. doi: 10.1136/bmjqs-2014-003690
61. Opticall. (2022). Your patients aren't that patient (and its costing you). Available online at: https://www.opticall.com/patients-are-not-patient/ (Accessed July 13, 2024).
62. NHSE. (2023). Artificial intelligence (AI) and machine learning. Available online at: https://www.england.nhs.uk/long-read/artificial-intelligence-ai-and-machine-learning/#:∼:text=Symptom%20checkers%20such%20as%20NHS,data%20scientists%20and%20product%20designers (Accessed July 13, 2024).
63. NHS. (2022). NHS 111. Available online at: https://111.nhs.uk/ (Accessed July 13, 2024).
64. Pope C, Turnbull J, Jones J, Prichard J, Rowsell A, Halford S. Has the NHS 111 urgent care telephone service been a success? Case study and secondary data analysis in England. BMJ Open. (2017) 7(5):e014815. doi: 10.1136/bmjopen-2016-014815
65. Steventon A. (2018). NHS 111: Understanding the impact on urgent and emergency care. Available online at: https://www.health.org.uk/blogs/nhs-111-understanding-the-impact-on-urgent-and-emergency-care#:∼:text=NHS%20111%20was%20set%20up,over%2015%20million%20every%20year (Accessed July 13, 2024).
66. Chambers D, Cantrell AJ, Johnson M, Preston L, Baxter SK, Booth A, et al. Digital and online symptom checkers and health assessment/triage services for urgent health problems: systematic review. BMJ open. (2019) 9(8):e027743. doi: 10.1136/bmjopen-2018-027743
67. Alderwick H, Dixon J. The NHS Long Term Plan. London: British Medical Journal Publishing Group (2019). p. 364.
68. Sukriti K, Tewolde S, Laverty AA, Costelloe C, Papoutsi C, Reidy C, et al. Uptake and adoption of the NHS app in England: an observational study. Br J Gen Pract. (2023) 73(737):e932–40. doi: 10.3399/BJGP.2022.0150
69. Tidy SJC. (2019). Refer Yourself for NHS Talking Therapy. Available online at: https://patient.info/treatment-medication/self-referral/refer-yourself-for-nhs-talking-therapy-counselling (Accessed July 13, 2024).
70. Gomez-Cano M, Atherton H, Campbell J, Eccles A, Dale J, Poltawski L, et al. Awareness and use of online appointment booking in general practice: analysis of GP patient survey data. Br J Gen Pract. (2020) 70(suppl 1). doi: 10.3399/bjgp20X711365
71. National Health Service England. (2024). NHS self-referral for tests and appointments for hundreds of thousands of patients. Available online at: https://www.england.nhs.uk/2024/04/nhs-self-referral-for-tests-and-appointments-for-hundreds-of-thousands-of-patients/ (Accessed August 10, 2024).
72. Baldwin JL, Singh H, Sittig DF, Giardina TD. Patient portals and health apps: pitfalls, promises, and what one might learn from the other. Healthcare. (2017) 5(3):81–5. doi: 10.1016/j.hjdsi.2016.08.004
74. Sheikh A, Anderson M, Albala S, Casadei B, Franklin BD, Richards M, et al. Health information technology and digital innovation for national learning health and care systems. Lancet Digit Health. (2021) 3(6):e383–96. doi: 10.1016/S2589-7500(21)00005-4
75. Burrows M, Greenfield S, Gale N, Walsh F, Litchfield I. General practice receptionists. Visible but invisible: the forgotten workforce. BMC Fam Pract. (2019) 21:138. doi: 10.1186/s12875-020-01204-y
76. Jongsma KR, Bekker MN, Haitjema S, Bredenoord AL. How digital health affects the patient-physician relationship: an empirical-ethics study into the perspectives and experiences in obstetric care. Pregnancy Hypertens. (2021) 25:81–6. doi: 10.1016/j.preghy.2021.05.017
77. Nilsson E, Sverker A, Bendtsen P, Eldh AC. A human, organization, and technology perspective on Patients’ experiences of a chat-based and automated medical history–taking service in primary health care: interview study among primary care patients. J Med Internet Res. (2021) 23(10):e29868. doi: 10.2196/29868
78. Darley S, Coulson T, Peek N, Moschogianis S, Van Der Veer SN, Wong DC, et al. Understanding how the design and implementation of online consultations affect primary care quality: systematic review of evidence with recommendations for designers, providers, and researchers. J Med Internet Res. (2022) 24(10):e37436. doi: 10.2196/37436
79. Eggleton K, Bui N, Goodyear-Smith F. Disruption to the doctor–patient relationship in primary care: a qualitative study. BJGP Open. (2022) 6(4):BJGPO.2022.0039. doi: 10.3399/BJGPO.2022.0039
80. Brant HD, Atherton H, Bikker A, Porqueddu T, Salisbury C, McKinstry B, et al. Receptionists’ role in new approaches to consultations in primary care: a focused ethnographic study. Br J Gen Pract. (2018) 68(672):e478–86. doi: 10.3399/bjgp18X697505
81. Hancock D. GP Patient survey 2020: making use of the data. Pract Manag. (2021) 31(1):22–30. doi: 10.12968/prma.2021.31.1.22
82. Rassa N, McCarthy M, Casalotti S, Zhang C, Wurie F, Brown C, et al. The impact of NHS charging regulations on healthcare access and utilisation among migrants in England: a systematic review. BMC Public Health. (2023) 23(1):1–12. doi: 10.1186/s12889-023-15230-9
83. Agrawal D, Pang G, Kumara S. Preference based scheduling in a healthcare provider network. Eur J Oper Res. (2023) 307(3):1318–35. doi: 10.1016/j.ejor.2022.09.027
84. Steel N, Abdelhamid A, Stokes T, Edwards H, Fleetcroft R, Howe A, et al. A review of clinical practice guidelines found that they were often based on evidence of uncertain relevance to primary care patients. J Clin Epidemiol. (2014) 67(11):1251–7. doi: 10.1016/j.jclinepi.2014.05.020
85. Bostock N. GPS Demand Government Review into Unprecedented Demand on General Practice. London: GP online (2019).
86. Marshall M. Long Waiting Times for GP Appointments are Unacceptable, Says College, as it Calls on Government to Prioritise General Practice Which has Been ‘running on Empty for too Long’, Royal College of General Practitioners. London: Royal College of General Practitioners (2020).
88. British Medical Association. Care Navigation and Triage in General Practice. 2024. London: British Medical Association (2023). Available online at: https://www.bma.org.uk/advice-and-support/gp-practices/managing-workload/care-navigation-and-triage-in-general-practice#:∼:text=Clinical%20triage%20is%20a%20clinical,within%20the%20practice%20or%20elsewhere
89. Salisbury C, Murphy M, Duncan P. The impact of digital-first consultations on workload in general practice: modeling study. J Med Internet Res. (2020) 22(6):e18203. doi: 10.2196/18203
90. NHS England. (2021). Digital First Primary Care. Available online at: https://www.england.nhs.uk/gp/digital-first-primary-care/ (Accessed August 10, 2024).
91. Clarke G, Pariza P, Wolters A. How are Total Triage and Remote Consultation Changing the use of Emergency Care? London: The Health Foundation 3 (2020).
92. Ueno A, Dennis C, Dafoulas GA. Digital exclusion and relative digital deprivation: exploring factors and moderators of internet non-use in the UK. Technol Forecast Soc Change. (2023) 197:122935. doi: 10.1016/j.techfore.2023.122935
93. Baird B, Reeve H, Ross S, Honeyman M, Nosa-Ehima M, Sahib B, et al. Innovative Models of General Practice. London: King’s Fund (2018).
94. Thorlby R, Tallack C, Finch D, Idriss O, Rocks S, Kraindler J, et al. Spending Review 2020: Priorities for the NHS, Social Care and the Nation’s Health. London: The Health Foundation (2020).
95. Imison C, Castle-Clarke S, Watson R. Reshaping the Workforce to Deliver the Care Patients Need. London: Nuffield Trust London (2016).
96. Brunton L, Tazzyman A, Ferguson J, Hodgson D, Nelson PA. The challenges of integrating signposting into general practice: qualitative stakeholder perspectives on care navigation and social prescribing in primary care. BMC Prim Care. (2022) 23(1):1–12. doi: 10.1186/s12875-022-01669-z
97. Reynolds J, Mortimore G. Advanced nurse practitioners: the NHS England framework. Gastrointestinal Nurs. (2018) 16(2):14–7. doi: 10.12968/gasn.2018.16.2.14
98. Goodwin R, Moffatt F, Hendrick P, Stynes S, Bishop A, Logan P. Evaluation of the first contact physiotherapy (FCP) model of primary care: a qualitative insight. Physiotherapy. (2021) 113:209–16. doi: 10.1016/j.physio.2021.08.003
99. England, N, N. Improvement. Network Contract Directed Enhanced Service: Additional Roles Reimbursement Scheme Guidance. London: NHS (2019).
100. Karampatakis GD, Patel N, Stretch G, Ryan K. Community pharmacy teams’ experiences of general practice-based pharmacists: an exploratory qualitative study. BMC Health Serv Res. (2020) 20(1):431. doi: 10.1186/s12913-020-05245-y
101. Kiely B, Croke A, O’Shea M, Boland F, O’Shea E, Connolly D, et al. Effect of social prescribing link workers on health outcomes and costs for adults in primary care and community settings: a systematic review. BMJ open. (2022) 12(10):e062951. doi: 10.1136/bmjopen-2022-062951
102. Perlman AI, Abu Dabrh AM. Health and wellness coaching in serving the needs of today’s patients: a primer for healthcare professionals. Glob Adv Health Med. (2020) 9:2164956120959274. doi: 10.1177/2164956120959274
103. Rimmer A. Physician Associates: BMA Launches Legal Action Against GMC. London: British Medical Journal Publishing Group (2024).
104. Jones B, Anchors Z, Voss S, Walsh N. Challenges and enablers to implementation of the additional roles reimbursement scheme in primary care: a qualitative study. Br J Gen Pract. (2024) 74(742):e315–22. doi: 10.3399/BJGP.2023.0433
105. NHS. (2020). NHS Long term plan. Available online at: https://www.longtermplan.nhs.uk/ (Accessed August 10, 2024).
106. Bhat AA, Rashid I, Hassan SU, Kansra P. Social Determinants of Health and Health Outcomes: A Bibliographic Review of the Scientific Literature from 2000 to 2021. Global Knowledge, Leeds: Memory and Communication (2023).
107. Regmi K, Mudyarabikwa O. A systematic review of the factors-barriers and enablers-affecting the implementation of clinical commissioning policy to reduce health inequalities in the national health service (NHS), UK. Public Health. (2020) 186:271–82. doi: 10.1016/j.puhe.2020.07.027
108. Drinkwater C, Wildman J, Moffatt S. Social prescribing. Br Med J. (2019) 364. doi: 10.1136/bmj.l1285
109. Gale NK, Kenyon S, MacArthur C, Jolly K, Hope L. Synthetic social support: theorizing lay health worker interventions. Soc Sci Med. (2018) 196:96–105. doi: 10.1016/j.socscimed.2017.11.012
110. NHSE. (2023). Workforce development framework: social prescribing link workers. Available online at: https://www.england.nhs.uk/publication/workforce-development-framework-social-prescribing-link-workers/ (Accessed August 10, 2024).
111. Husk K, Elston J, Gradinger F, Callaghan L, Asthana S. Social prescribing: where is the evidence? Br J Gen Pract. (2019) 69(678):6–7. doi: 10.3399/bjgp19X700325
112. Anderson A, O'Connell SS, Thomas C, Chimmanamada R. Telehealth interventions to improve diabetes management among black and hispanic patients: a systematic review and meta-analysis. J Racial Ethn Health Disparities. (2022):1–12. doi: 10.1007/s40615-021-01174-6
113. Paudyal V, Watson MC, Sach T, Porteous T, Bond CM, Wright DJ, et al. Are pharmacy-based minor ailment schemes a substitute for other service providers? A systematic review. Br J Gen Pract. (2013) 63(612):e472–81. doi: 10.3399/bjgp13X669194
114. Bond C. Pharmacy: finally part of the team? Br J Gen Pract. (2015) 65(639):e638–9. doi: 10.3399/bjgp15X686797
115. Todd A, Copeland A, Husband A, Kasim A, Bambra C. Access all areas? An area-level analysis of accessibility to general practice and community pharmacy services in England by urbanity and social deprivation. BMJ Open. (2015) 5(5):e007328. doi: 10.1136/bmjopen-2014-007328
116. Litchfield I, Gale N, Burrows M, Greenfield S. The future role of receptionists in primary care. Br J Gen Pract. (2017) 67(664):523. doi: 10.3399/bjgp17X693401
117. Ethier JF, McGilchrist M, Barton A, Cloutier AM, Curcin V, Delaney BC, et al. The TRANSFoRm project: experience and lessons learned regarding functional and interoperability requirements to support primary care. Learn Health Syst. (2018) 2(2):e10037. doi: 10.1002/lrh2.10037
118. Standardization, I. O. f. Health informatics-Electronic health record-Definition, scope and context, na (2005).
119. Rothman B, Leonard JC, Vigoda MM. Future of electronic health records: implications for decision support. Mt Sinai J Med. (2012) 79(6):757–68. doi: 10.1002/msj.21351
120. Campion-Awwad O, Hayton A, Smith L, Vuaran M. The National Programme for IT in the NHS. A Case History. London: University of Cambridge (2014).
121. Li E, Clarke J, Neves AL, Ashrafian H, Darzi A. Protocol: electronic health records, interoperability and patient safety in health systems of high-income countries: a systematic review protocol. BMJ Open. (2021) 11(7):e044941. doi: 10.1136/bmjopen-2020-044941
122. Cresswell KM, Lee L, Mozaffar H, Williams R, Sheikh A, e N, et al. Sustained user engagement in health information technology: the long road from implementation to system optimization of computerized physician order entry and clinical decision support systems for prescribing in hospitals in England. Health Serv Res. (2017) 52(5):1928–57. doi: 10.1111/1475-6773.12581
123. Health DO, S Care. (2018). The future of healthcare: our vision for digital, data and technology in health and care.
124. Executive NH. (2019). How the new NHS Supply Chain is transforming the landscape. Available online at: https://www.nationalhealthexecutive.com/Health-Service-Focus/how-the-new-nhs-supply-chain-is-transforming-the-landscape (Accessed August 10, 2024).
125. West M. Developing Cultures of High Quality Care. London: Talk at the Kings Fund London (2013).
126. Litchfield I, Gale N, Burrows M, Greenfield S. You're only a receptionist, what do you want to know for?: street-level bureaucracy on the front line of primary care in the United Kingdom. Heliyon. (2023) 9:11. doi: 10.1016/j.heliyon.2023.e21298
127. Daker-White G, Hays R, McSharry J, Giles S, Cheraghi-Sohi S, Rhodes P, et al. Blame the patient, blame the doctor or blame the system? A meta-synthesis of qualitative studies of patient safety in primary care. PLoS One. (2015) 10(8):e0128329. doi: 10.1371/journal.pone.0128329
128. Primary Care Workforce Commission. The Future of Primary Care: Creating Teams for Tomorrow. London: Health Education England (2015).
129. Leadership FoM and Management. Leadership and Management Standards for Medical Professionals. London: Faculty of Medical Leadership and Management (2016).
130. Risi L, Bhatti N, Cockman P, Hall J, Ovink E, Macklin S, et al. Micro-teams for better continuity in tower hamlets: we have a problem but we’re working on a promising solution!. Br J Gen Pract. (2015) 65(639):536. doi: 10.3399/bjgp15X687025
131. Baird B, Boyle T, Chauhan K, Heller A, Proce C. How to Build Effective Teams in General Practice. London: The King’s Fund (2020).
132. Coombs CRH, Cohen T, Duddy C, Mahtani KR, Roberts N, Saini A, et al. Primary care micro-teams: a protocol for an international systematic review to describe and examine the opportunities and challenges of implementation for patients and healthcare professionals. BMJ Open. (2022) 12(3):e052651. doi: 10.3399/BJGP.2022.0545
133. Young A, Beswick K. Protocols used by UK general practitioners, what is expected of them and what solutions are provided. Comput Methods Programs Biomed. (1995) 48(1-2):85–90. doi: 10.1016/0169-2607(95)01665-G
135. Mellor RM, Sheppard JP, Bates E, Bouliotis G, Jones J, Singh S, et al. Receptionist rECognition and rEferral of patients with stroke (RECEPTS): unannounced simulated patient telephone call study in primary care. Br J Gen Pract. (2015) 65(636):e421–7. doi: 10.3399/bjgp15X685621
136. Grant S, Mesman J, Guthrie B. Spatio-temporal elements of articulation work in the achievement of repeat prescribing safety in UK general practice. Sociol Health Illn. (2016) 38(2):306–24. doi: 10.1111/1467-9566.12308
137. Grant S, Guthrie B. Between demarcation and discretion: the medical-administrative boundary as a locus of safety in high-volume organisational routines. Soc Sci Med. (2018) 203:43–50. doi: 10.1016/j.socscimed.2018.03.005
138. Lipsky M. Street-level Bureaucracy: Dilemmas of the Individual in Public Service. Oxford: Russell Sage Foundation (2010).
139. Maynard-Moody S, Musheno M. Social equities and inequities in practice: street-level workers as agents and pragmatists. Public Adm Rev. (2012) 72(s1):S16–23. doi: 10.1111/j.1540-6210.2012.02633.x
140. NHS England. Integrated Care Systems. London: NHS (2020). Available online at: https://www.england.nhs.uk/integratedcare/integrated-care-systems (Accessed).
141. England N, N. Improvement. Integrated Care Systems. London: NHS (2021). Available online at: https://www.england.nhs.uk/integratedcare/integrated-care-systems (Accessed November).
142. NHS Confederation. The role of primary care in integrated care systems. London: NHS Confederation (2021).
143. Colivicchi A. GPS Asked to Submit ‘Quality Alerts’ to ICB When Experiencing Workload Dump. London: Cogora (2023). Available online at: https://www.pulsetoday.co.uk/news/workload/gps-asked-to-submit-quality-alerts-to-icb-when-experiencing-workload-dump/
144. Grafton-Clarke C, Chen KW, Wilcock J. Diagnosis and referral delays in primary care for oral squamous cell cancer: a systematic review. Br J Gen Pract. (2019) 69(679):e112–26. doi: 10.3399/bjgp18X700205
145. Williams P, Murchie P, Bond C. Patient and primary care delays in the diagnostic pathway of gynaecological cancers: a systematic review of influencing factors. Br J Gen Pract. (2019) 69(679):e106–11. doi: 10.3399/bjgp19X700781
146. Chidgey J, Leng G, Lacey T. Implementing NICE guidance. J R Soc Med. (2007) 100(10):448–52. doi: 10.1177/014107680710001012
147. NICE. (2024). National INstitute for Health and Care Excellence. Available online at: https://www.nice.org.uk/ (Accessed August 10, 2024).
148. Excellence, N. I. f. H. a. C. (2021). Red flag signs and symptoms. Available online at: https://cks.nice.org.uk/topics/chronic-pain/diagnosis/red-flag-signs-symptoms/ (Accessed August 10, 2024).
149. Starr OD. New guidance does not trump clinical judgment. Br Med J. (2019) 367. doi: 10.1136/bmj.l6112
150. Tao W, Jing-Yu T, Xian-Liang L, Isabella Z. Barriers and enablers to implementing clinical practice guidelines in primary care: an overview of systematic reviews. BMJ Open. (2023) 13(1):e062158. doi: 10.1136/bmjopen-2022-062158
151. Scullard P, Abdelhamid A, Steel N, Qureshi N. Does the evidence referenced in NICE guidelines reflect a primary care population? Br J Gen Pract. (2011) 61(584):e112–117. doi: 10.3399/bjgp11X561177
152. Health Education England. (2016). Care Navigation. Available online at: https://www.hee.nhs.uk/our-work/care-navigation (retrieved March, 2023).
153. Peart A, Lewis V, Brown T, Russell G. Patient navigators facilitating access to primary care: a scoping review. BMJ open. (2018) 8(3):e019252. doi: 10.1136/bmjopen-2017-019252
154. NHS England. (2022). Integrated care in action – primary care. Available online at: https://www.england.nhs.uk/integratedcare/resources/case-studies/integrated-care-in-action-primary-care/ (Accessed August 10, 2024).
155. Hammond J, Gravenhorst K, Funnell E, Beatty S, Hibbert D, Lamb J, et al. Slaying the dragon myth: an ethnographic study of receptionists in UK general practice. Br J Gen Pract. (2013) 63(608):E177–84. doi: 10.3399/bjgp13X664225
156. Vaona A, Pappas Y, Grewal RS, Ajaz M, Majeed A, Car J. Training interventions for improving telephone consultation skills in clinicians. Cochrane Database Syst Rev. (2017) (1). doi: 10.1002/14651858.CD010034.pub2
157. Leach B, Parkinson S, Gkousis E, Abel G, Atherton H, Campbell J, et al. Digital facilitation to support patient access to web-based primary care services: scoping literature review. J Med Internet Res. (2022) 24(7):e33911. doi: 10.2196/33911
158. Walker SC, Baquero B, Bekemeier B, Parnes M, Arora K. Strategies for enacting health policy codesign: a scoping review and direction for research. Implement Sci. (2023) 18(1):44. doi: 10.1186/s13012-023-01295-y
160. Trebble TM, Hansi N, Hydes T, Smith MA, Baker M. Process mapping the patient journey: an introduction. Br Med J. (2010) 341:c4078. doi: 10.1136/bmj.c4078
161. Dickson JM, Hilton A, Kelsall C, Cormack L. Primary care: the sleeping giant of research delivery. Br J Gen Pract. (2023) 73:198–9. doi: 10.3399/bjgp23X732573
Keywords: primary care, policy implementation and delivery, access and quality, process visualization, National Health Service England
Citation: Litchfield I, Gale NK, Greenfield S, Shukla D and Burrows M (2025) Enhancing access to primary care is critical to the future of an equitable health service: using process visualisation to understand the impact of national policy in the UK. Front. Health Serv. 4:1499847. doi: 10.3389/frhs.2024.1499847
Received: 21 September 2024; Accepted: 31 December 2024;
Published: 27 January 2025.
Edited by:
Shasha Yuan, Chinese Academy of Medical Sciences and Peking Union Medical College, ChinaReviewed by:
Ashley M. Hughes, Case Western Reserve University, United StatesJana Bartakova, University of Basel, Switzerland
Copyright: © 2025 Litchfield, Gale, Greenfield, Shukla and Burrows. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ian Litchfield, aS5saXRjaGZpZWxkQGJoYW0uYWMudWs=
 Ian Litchfield
Ian Litchfield Nicola Kay Gale
Nicola Kay Gale Sheila Greenfield
Sheila Greenfield David Shukla3
David Shukla3