- 1Department of Public Health, Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia
- 2School of Public Health, Adama Hospital Medical College, Adama, Ethiopia
Background: Person-centered care practice has not yet been fully adopted in low- and middle-income nations such as Ethiopia. It focuses on improving several areas of patient-physician interaction. Despite Ethiopia's rapid growth in healthcare facilities, there is insufficient data available on care practices.
Method: A facility-based comparative cross-sectional study was conducted in selected public and private general hospitals in Addis Ababa from May 26 to July 26, 2023. A multistage sampling technique was employed to select the study participants. The data were collected using an interviewer-administered structured questionnaire, entered into Epi Info-7, and exported to SPSS version 27 for analysis. Bivariate and multivariate logistic regression analyses were performed to identify significant factors associated with care practices.
Results: A total of 848 patients were involved, with a response rate of 99.5%. The overall magnitude of good care practice was 52.8%, with 34.8% in public hospitals and 70.9% in private hospitals. Factors associated with good care practices in private hospitals included hospital attractiveness (AOR: 3.2; 95% CI: 1.6–6.5), ease of access to services (AOR: 12.1; 95% CI: 6.2–23.3), and privacy of access and care (AOR: 10.89; 95% CI: 5.60–21.19). In contrast, factors associated with good healthcare practices in public hospitals were perceived intimacy with the provider (AOR: 8.85; 95% CI: 4.50–17.43), privacy in accessing care (AOR: 12.1; 95% CI: 6.62–22.16), and the provision of medication information (AOR: 4.39; 95% CI: 2.40–8.03).
Conclusion: Overall, 52.8% of participants rated person-centered care practices as good, with private hospitals in Addis Ababa (70.9%) demonstrating a higher prevalence of person-centered care practices compared to public hospitals (34.8%). The factors associated with healthcare practices in both public and private hospitals include hospital type, hospital attractiveness, ease of access to services, privacy in accessing care, perceived intimacy with the provider, and the provision of medication information. We recommend targeted improvements in public hospitals to enhance the quality of PCC.
Introduction
The Institute of Medicine (IOM) defines person-centered care (PCC) as care that respects and responds to individual patient preferences, needs, and values, ensuring that these values guide all clinical decisions, and it is identified as one of six essential goals for healthcare improvement (1). Person-centered care is holistic and empowering, recognizing and prioritizing the unique needs and preferences of each patient (2). The Picker Institute further explained that PCC has eight dimensions: (1) respect, (2) coordination and integration of care, (3) information, communication, and education, (4) physical comfort, (5) emotional support, (6) family and friends' involvement, (7) transition and continuity, and (8) access to care (3). Carl Rogers introduced person-centered care in the 1940s, leading to the development of advanced models and their application in various fields of practice (4). The World Health Organization (WHO) has emphasized the importance of the "PCC" in providing quality care for patients with chronic diseases, with patients and healthcare professionals as key components (4).
Despite its advantages, care encounters significant global implementation challenges, with inconsistent integration into clinical practice, even in developed countries (2). Studies indicate that barriers to implementing person-centered care include time constraints, heavy workloads, resistance to change, lack of organizational support, limited involvement of front-line staff, and inadequate resources (5). Similarly, evidence suggested that the barriers to care practice include time constraints, patient characteristics, providers' reluctance to relinquish control, and poor communication skills (6). A study found that poor PCC implementation in sub-Saharan Africa is due to provider issues, health system structure, and the broader socioeconomic environment (2).
Ethiopian healthcare tends to be more biological than biopsychosocial, with 71% of healthcare professionals lacking compassion and respect, leading to 30% of patients expressing dissatisfaction with the services (3). A study in Addis Ababa revealed that 49% of patients viewed the care as person-centered, with private hospitals showing a higher rate of 70.2% (7). This study aimed to assess and compare healthcare practices among public and private general hospitals in Addis Ababa, addressing research gaps in Ethiopia.
Methods
Study area and period
The study was conducted in general hospitals in Addis Ababa, Ethiopia, from May 26 to July 26, 2023. The city has a total of 52 hospitals, including three nongovernmental organizations (NGOs), three owned by the defense forces and the police, and 35 private hospitals. According to the Central Statistical Agency of Ethiopia (CSA) population forecast for 2022, Addis Ababa has a total population of 3,859,999, with 1,882,000 males.
Study design
A facility-based cross-sectional study design was conducted.
Source population
All admitted inpatients in public and private general hospitals in Addis Ababa during the study period were included in the study.
Study population
Randomly selected admitted inpatients from the chosen general hospitals between May 26 and July 26 were included in the study.
Inclusion criteria
Patients over 18 years of age, admitted to selected public and private hospital wards for 24 h or more, and mentally capable of providing informed responses, were included in the study.
Exclusion criteria
In this study, unconscious patients, those with impaired cognitive or communication abilities, and ICU patients were excluded from the analysis.
Sample size and sampling procedure
The sample size was determined using the double population proportion formula, with the following statistical assumptions: a 95% confidence interval (CI) and a proportion of person-centered care (PCC) practice in public hospitals (P1 = 60.9%) based on a study conducted in Wollo (8), and the proportion of PCC practice at private hospitals (P2 = 70.2%) from the study conducted in Addis Ababa (7) [Alpha (α) type 1 error; β is a type 2 error; power = 80%; confidence level = 1.96. Where Zα/2 is the critical value of the normal distribution at α/2 (for a 95% confidence level, for example, α is 0.05 and the critical value is 1.96) and Zβ is the critical value of the normal distribution at β (for example, β is 0.2 for 80% power) and the critical value is 0.84), and p1 and p2 are the expected sampling proportions of the two groups.
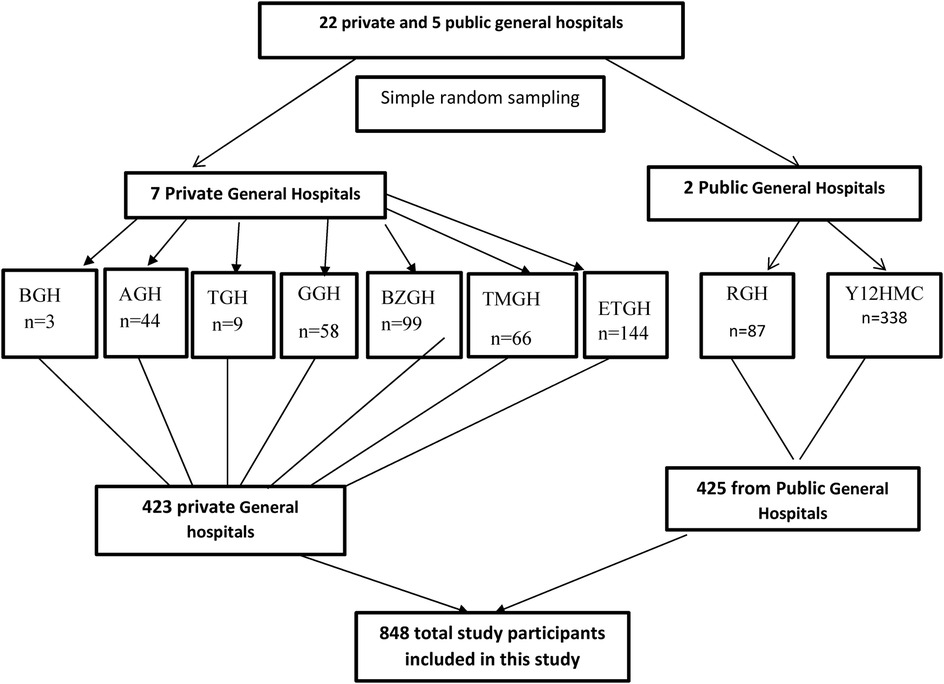
After accounting for a 5% nonresponse rate, the final sample size was set at 852, with 426 patients from private hospitals and 426 from public hospitals. Out of 27 general hospitals in the city (5 public and 22 private), two public hospitals (Ras-Desta Hospital and Yekatit 12 Hospital Medical College) and seven private hospitals (Betel General Hospital (BGH), Amen General Hospital (AGH), Tezena General Hospital (TGH), Grum General Hospital (GGH), Betezata General Hospital (BZGH), Teklehymtnot General Hospital (TMGH), and Ethio-Tebib General Hospital (ETGH)) were selected (30% of each group) using a lottery method. The sample size was proportionally allocated based on the monthly average of hospitalized patients at each hospital, and systematic random sampling was employed to identify study participants (Figure 1).
Study variables and measurements
In this study, the dependent variable was person-centered healthcare practices. The independent variables included sociodemographic factors (age, gender, educational status, marital status, income, and insurance status), organizational characteristics (hospital type, welcoming environment, ease of service access, noise levels, aesthetic appeal, privacy, and information on care plans, safety alerts, and diet), and healthcare provider factors (perceived intimacy, physician competency, and self-assessed clinical knowledge).
Data collection method and tool
Person-centered climate questionnaire-patient
The Patient-Centered climate questionnaire (PCQ-P), originally developed in Swedish, assesses patients' perspectives on the care environment within healthcare facilities. It comprises 17 items across three dimensions of person-centered care: safety, everydayness, and hospitality. The Swedish study reported satisfactory Cronbach's alpha values for the total scale (0.93) and its subscales safety (0.94), everydayness (0.80), and hospitality (0.64). Overall, the person-centered climate questionnaire is a valid and reliable tool for evaluating the extent of person-centeredness in hospital environments (8). The English version of the PCQ-P was also validated in an Australian study (9).
Since no Amharic version was available, the English version was translated into Amharic using the forward-backward translation method. The Amharic version demonstrated high reliability, with Cronbach's alpha values of 0.96 for the total scale and 0.88, 0.89, and 0.91 for the subscales of safety, everydayness, and hospitality, respectively. A pretest was conducted on 5% of the sample at St. Peter's Specialized Hospital to ensure the translation's accuracy and reliability.
Operational definition
A climate of safety is indicated by accessible and competent staff who respond quickly and a clean and well-organized physical environment (10).
Everyday climate refers to experiences of a deinstitutionalized environment that contains aspects of familiarity and everydayness and being home-like (10).
Hospitality refers to the reception and friendliness of local people, who both make you feel welcome and receive the best treatment and care (8).
Welcoming space to patient and family, Sound and noise, Ease to access services within the institution, Beauty and external appearance, Privacy to access care, Communication on the plan of care, Medication, Diet and Safety, Perceived intimacy with the provider, for the above factors Patients were classified as having a “good” perception if they responded very good and good and a “poor” perception if they responded either neutrally, poorly or very poorly (11).
Person-centered care practices: were measured with a 17-item structured questionnaire with responses structured on a five-point scale. Respondents were categorized as experiencing “good” person-centered care practices (PCC) if they scored above or equal to the mean score of 3.46, while those who scored below the mean were categorized as experiencing “poor” PCC.
Data analysis
Descriptive statistics such as frequencies and percentages were used for qualitative variables. The internal consistency of the PCQ-P was calculated using Cronbach's α coefficient. Bivariate and multiple binary logistic regression analyses were used to determine the associations between independent and dependent variables. The crude odds ratio (COR) and adjusted odds ratio (AOR) were calculated. To determine the factors significantly associated with the PCC, the odds ratio (OR) at the 95% CI was determined using multivariable logistic regression analysis. The Hosmer and Lemeshow tests were used to test the goodness of fit. Multicollinearity was determined using a VIF cutoff point >10. An adjusted odds ratio with a p-value < 0.05 was used to report the significant factors associated with PCC. All analyses were performed using the Statistical Package for Social Science (SPSS version 25).
Results
Sociodemographic characteristics of the participants
This study included 848 participants from public and private hospitals, with a response rate of 99.5%. Most participants were female (58%) in private hospitals and male (54.1%) in public hospitals. The average age was 44.6 ± 14.3 years for private hospital patients and 47 ± 13.8 years for public hospital patients. Regarding marital status, 52% of participants in private hospitals and 70.8% in public hospitals were married. Monthly incomes ranged from none to 27,000 ETB (Table 1).
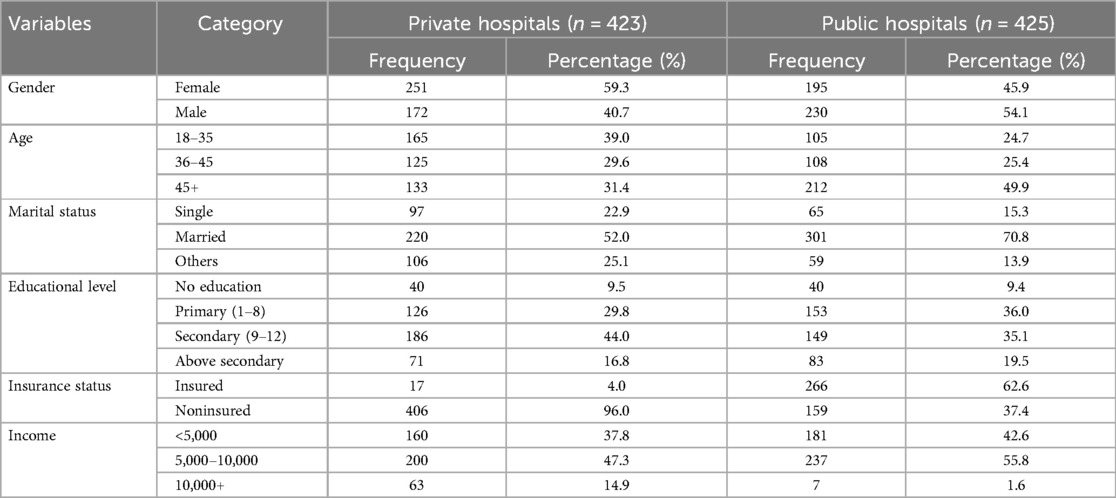
Table 1. Sociodemographic characteristics of the respondents at the public and private general hospitals of Addis Ababa, Ethiopia, 2023 (N = 848).
Organizational related factors
A majority of participants from private hospitals (71.4%) and public hospitals (63.8%) perceived the hospital environment as friendly. Accessibility of services was reported as easy by only 34.8% of participants from public hospitals, compared to 76.1% from private hospitals. Most clients from both public (79.7%) and private hospitals (71.3%) reported that there was no disruptive noise on the hospital premises.
Most participants from private hospitals, 302 (71.4%) felt that the hospital had a welcoming environment, compared to 271 (63.8%) of those from public hospitals. Additionally, 322 (76.1%) participants from private hospitals reported easy access to services, while only 34.8% of public hospital participants felt the same.
Of the respondents, 295 (69.4%) from public hospitals and 332 (78.3%) from private hospitals felt the facilities were well-maintained. Privacy was considered adequate by 74.7% of private hospital patients and 46.4% of public hospital patients. Most participants shared their views on care quality, with 352 (83.2%) from private hospitals and 332 (78.3%) from public hospitals providing feedback. Additionally, 331 private hospital patients (78.3%) and 259 public hospital patients (60.9%) felt they received sufficient information about safety alerts (Table 2).
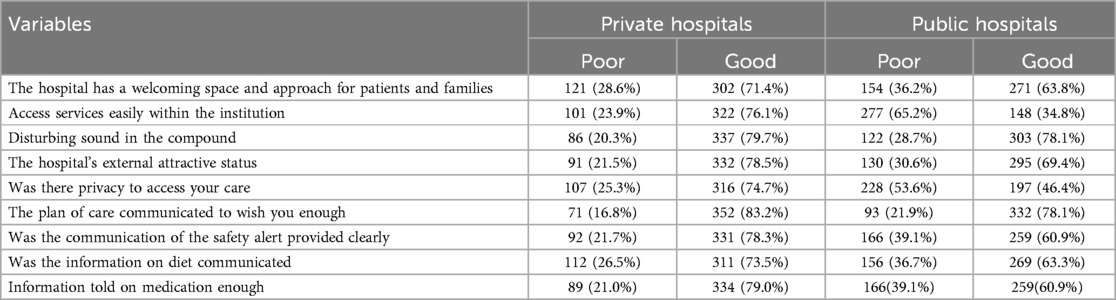
Table 2. Perceived organizational factors affecting person-centered care practices at public and private general hospitals in Addis Ababa, Ethiopia, in 2023 (N = 848).
Self- and physician-related factors
Approximately 61.4% of public hospital clients and 80% of private hospital clients were aware of their healthcare providers. Knowledge of their condition was reported by 284 (66.8%) public hospital participants and 348 (82.3%) private hospital participants. Three-foruth (75.4%) of private hospital participants and 71.1% of public hospital participants were aware of the available treatment options. Most participants felt well-informed about their illness, with 406 (96%) in private hospitals and 393 (92.5%) in public hospitals showing strong knowledge of their condition (Table 3).
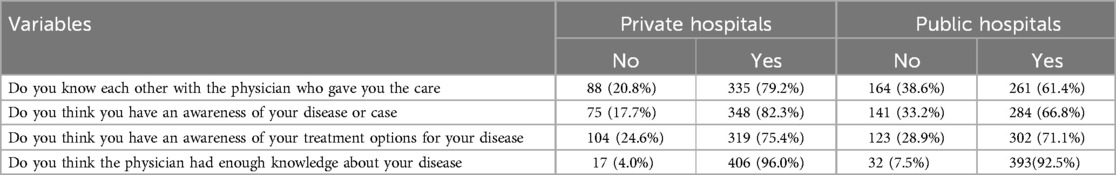
Table 3. Perceived self- and provider-related factors that might affect person-centered care practices at public and private general hospitals in Addis Ababa, Ethiopia, in 2023 (N = 848).
Person-centered care at public and private hospitals
The magnitude of good person-centered care (PCC) in public general hospitals in Addis Ababa was 34.8% (95% CI: 30.3%–39.3%), compared to 70.9% (95% CI: 66.6%–75.2%) in private hospitals. Overall, 52.8% (95% CI: 49.6%–56.1%) of respondents rated the PCC practice as good (Figure 2).
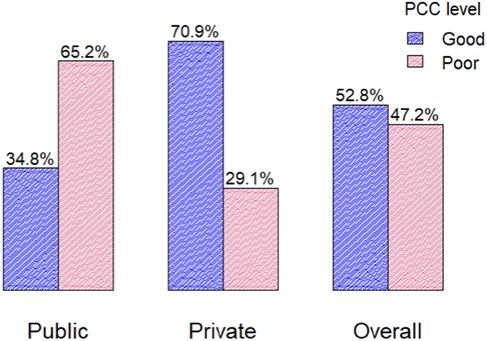
Figure 2. The overall PCC in public, private, and general hospitals in Addis Ababa city, Ethiopia, in 2023 (n = 848).
Factors associated with PCC in private hospitals
Multivariable logistic regression analysis revealed that hospital attractiveness, ease of access to services, and privacy during care were significantly associated with person-centered care (PCC) practices in private hospitals. Patients who perceived the hospital as unattractive were three times more likely to rate its PCC as poor (AOR: 3.4; 95% CI: 1.70–6.77). Those who found accessing services difficult were 13.12 times more likely to consider PCC poor (AOR: 13.12; 95% CI: 6.70–25.72) compared to those who found access easy. Additionally, patients who perceived poor privacy during care were approximately eleven times more likely to rate PCC as poor (AOR: 11.01; 95% CI: 5.70–21.27) than their counterparts (Table 4).
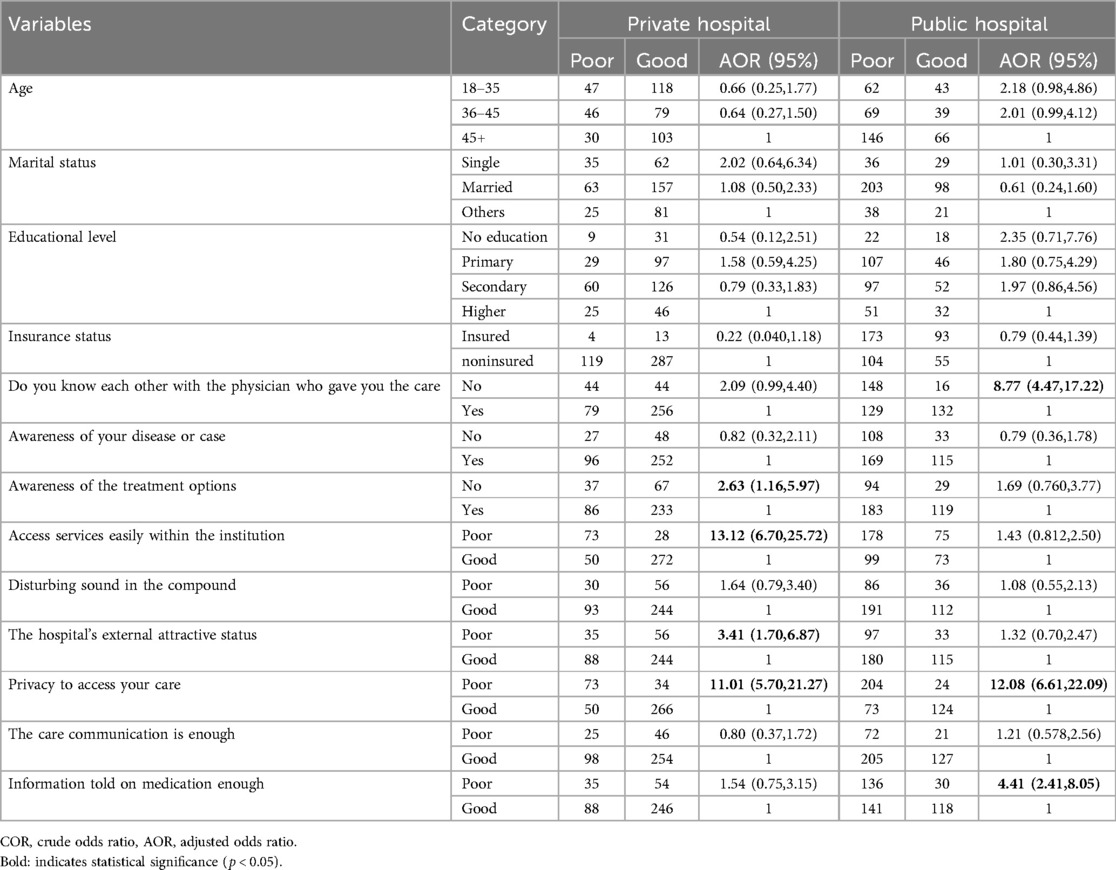
Table 4. Factors associated with person-centered care practices in private and public general hospitals (n = 848).
Factors associated with PCC in public hospitals
Similarly, in the multivariable binary logistic regression analysis for public hospitals, perceived intimacy with the provider, privacy during care, and information about medication were significantly associated with person-centered care (PCC) practices. Patients who did not know their healthcare provider were eight times more likely to rate the care as poor (AOR: 8.77; 95% CI: 4.47–17.22) compared to their counterparts. Those who perceived poor privacy in the hospital were twelve-fold more likely to rate PCC as poor (AOR: 12.08; 95% CI: 6.61–22.09) than those who perceived good privacy. Similarly, patients who felt they received inadequate information about their medication were 4.4 times more likely to rate the care as poor (AOR: 4.41; 95% CI: 2.41–8.05) compared to those who felt adequately informed (Table 4).
Factors associated with PCC in the overall hospital
In the overall adjusted model, hospital type, perceived intimacy with the provider, ease of accessing services, hospital attractiveness, privacy during care, and medication information were significantly associated with person-centered care practices. Patients from private hospitals were 56% more likely to perceive the care they received as good for person-centered care (PCC) than those from public hospitals (AOR: 0.44; 95% CI: 0.26–0.75). Patients who did not know their healthcare provider were 4.8 times more likely to rate the PCC interaction as poor (AOR: 4.80; 95% CI: 3.07–7.50) compared to those who knew their provider. Patients who found it difficult to access services were 3.4 times more likely to rate the care as poor for PCC than those who found it easy to access services (AOR: 3.36; 95% CI: 2.24–5.03). Patients who perceived the hospital as unattractive were 1.65 times more likely to rate the care as poor for PCC (AOR: 1.65; 95% CI: 1.05–2.59) compared to those who found the hospital appealing. Patients who believed the hospital had poor privacy were 11.21 times more likely to perceive the care as poor for PCC (AOR: 11.21; 95% CI: 7.38–17.04). Patients who felt they did not receive adequate education on medication were 2.5 times more likely to rate the care as poor for PCC than those who felt adequately informed (AOR: 2.25; 95% CI: 1.67–3.90) (Table 5).
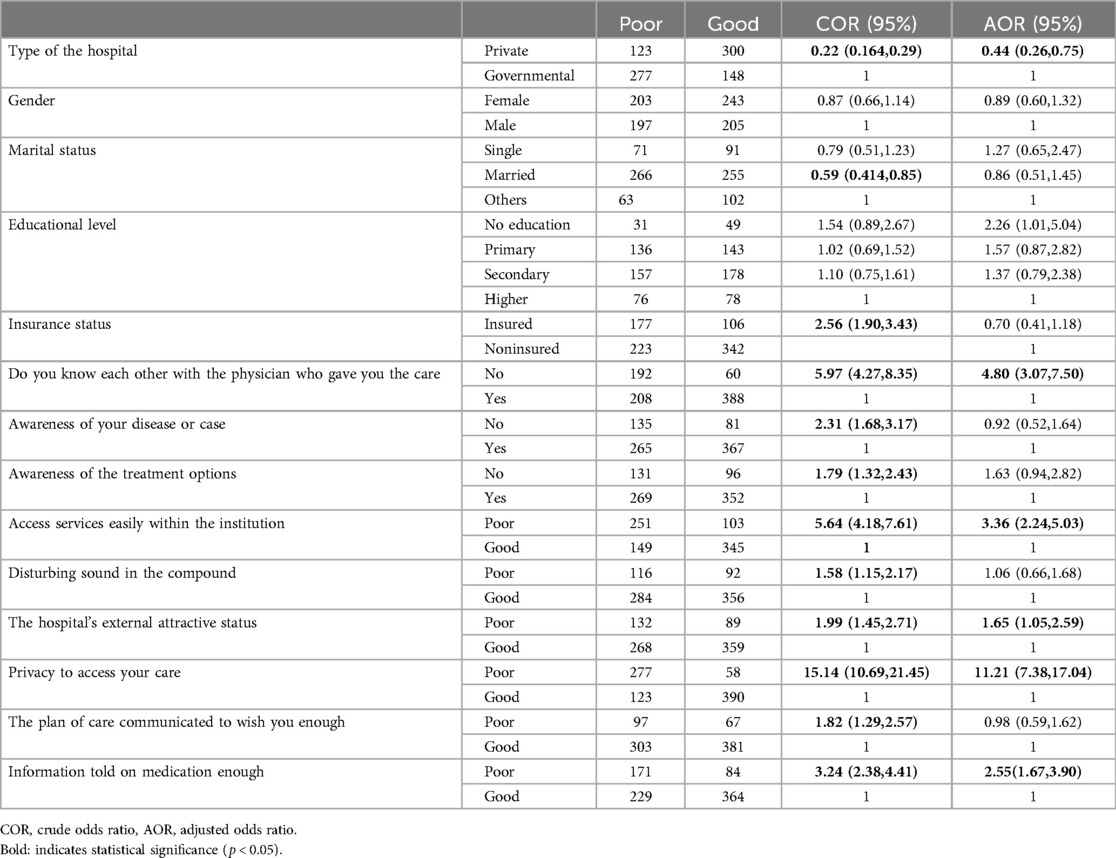
Table 5. Overall factors associated with person-centered care practices in public and private general hospitals.
Discussions
This study assessed medical practices in Addis Ababa, Ethiopia, with a focus on aligning care with patient preferences and involving patients in decision-making. It included consultations with both patients and healthcare providers, ensuring that dignity and compassion were maintained throughout the treatment process, including in medication choices.
Overall, 52.8% of respondents rated healthcare practices (PCC) as good, aligning with findings from previous studies in Tigray and Addis Ababa, Ethiopia (6, 12). However, this finding is lower than those reported in previous studies conducted in Norway (86.5%), China (59.7%), and Saudi Arabia (73%) (7, 13–15). The disparity may be attributed to variations in socioeconomic levels, differences in study design and timing, and variations in healthcare systems. Socioeconomic factors can influence both patient expectations and access to care. Differences in study design and timing may affect how data is collected and interpreted. Additionally, variations in healthcare systems across regions can impact the implementation and effectiveness of care practices.
The subgroup analysis found that 70.9% of private hospital patients and 34.8% of public hospital patients rated person-centered care practices (PCC) as good. This aligns with a previous cross-sectional study conducted in Addis Ababa (6), which reported that 70.2% of private patients and 27.8% of public patients rated person-centered care practices (PCCP) positively. This difference likely stems from several factors. Private hospitals typically have better resources, higher staffing levels, and more personalized care due to greater funding, leading to higher patient satisfaction. In contrast, public hospitals face budget constraints, higher patient volumes, and limited resources, which can affect the quality of person-centered care (PCC) (16). Additionally, patients in private hospitals may have higher expectations, while those in public hospitals, dealing with more complex health issues, may rate their care differently.
Hospital ownership type (public or private) was identified as a significant factor influencing patient-centered healthcare practices, as supported by a previous study (7, 9, 17–20). This disparity may be due to private hospitals generally offering more advanced medical facilities and technology, shorter wait times, and better access to internal services compared to public hospitals (16). A statistically significant association was found between healthcare practices and hospital attractiveness, consistent with studies conducted in Addis Ababa (7). Patients likely feel more comfortable and have a better healthcare experience in hospitals with a welcoming atmosphere, which can lead to increased patient involvement and a better healthcare system.
The study found a statistically significant association between healthcare practices and privacy in accessing care, consistent with findings from a study conducted in Addis Ababa (6, 7). Patients may feel more comfortable sharing concerns when provided with privacy, such as private examination rooms or confidential communication, which enhances trust and open communication with healthcare professionals and supports care.
Information on the medication is a critical factor in healthcare practices, as supported by previous studies (6, 7, 21). Clear communication about medications enables patients to take an active role in their care. When informed about the purpose, correct usage, side effects, and interactions of their medications (22), patients can make better decisions, leading to improved adherence and outcomes. This approach respects patients' preferences, a core element of person-centered care, and fosters trust between patients and healthcare providers, promoting a collaborative treatment approach that prioritizes patient well-being and autonomy.
Personal and professional factors play a significant role. Research in Addis Ababa and central Ethiopia found that patients who felt familiar with their healthcare provider were 60% less likely to rate their interaction negatively (2, 3, 6). Additionally, a study in central Ethiopia showed that these patients were twice as likely to receive empathic care (7). The study also found a statistically significant association between perceived closeness to physicians and healthcare practices.
The limitation of the study
This cross-sectional study assessed person-centered care practices, but factors such as participants' moods or personal issues during data collection may have influenced their responses, potentially affecting the accuracy of the findings. Additionally, the study was conducted in Addis Ababa, the capital city of Ethiopia, and its findings may not be easily generalized to other regions. Significant differences in infrastructure and the availability of skilled healthcare professionals across regions may limit the applicability of the results.
Conclusion
Overall, 52.8% of respondents rated healthcare practices as good, with private hospitals in Addis Ababa (70.9%) showing a higher percentage of person-centered care practices compared to public hospitals (34.8%). Key factors influencing PCCs include hospital type, perceived intimacy with providers, ease of access, privacy, and medication information. We recommend targeted improvements in public hospitals to enhance the quality of PCC. Additionally, the findings should be considered in the context of hospitals in less urbanized areas of Ethiopia, where challenges in infrastructure and resources may affect PCC implementation.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://figshare.com/articles/dataset/The_data_for_Personcentered_care_practice_between_public_and_private_General_Hospitals_in_Addis_Ababa_Ethiopia/28001708?file=51086549.
Ethics statement
The studies involving humans were approved by The studies involving human participants were reviewed and approved by the ethical review committee of Yikatit 12 Hospital Medical College, Ethiopia. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
TGC: Formal Analysis, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors wish to acknowledge the participants and data collectors who contributed to this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Handley SC, Bell S, Nembhard IM. A Systematic Review of Surveys for Measuring Patient-centered Care in the Hospital Setting. Vol. 59, Medical Care. Philadelphia, PA: Lippincott Williams and Wilkins (2021). p. 228–37.
2. Tamiru B, Beharu M, Tesfaye T, Belay Y. Scope of patient centered care practice in public hospitals of benishangul gumuze regional state. Qual Prim Care. (2017) 26(2017):31–7.
3. Tamiru B. Facilitators and barriers of patient centered care practice in Public Hospitals of Benishangul Gumuze Regional State, South West Ethiopia. Rehabil Sci. (2021) 6(1):10. doi: 10.11648/j.rs.20210601.12
4. Kobrai-abkenar F, Pourghane P, Jafarzadeh-kenarsari F. Heliyon psychometric properties of the persian language person-centered climate questionnaire—patient version (PCQ-P) what does this paper contribute to the wider global clinical community? Heliyon. (2020) 6(October 2019):e05154. doi: 10.1016/j.heliyon.2020.e05154
5. Ryan BL, Brown JB, Tremblay PF, Stewart M. Measuring patients’ perceptions of health care encounters: examining the factor structure of the revised patient perception of patient-centeredness (PPPC-R) questionnaire. J Patient Cent Res Rev. (2019) 6(3):192–202. doi: 10.17294/2330-0698.1696
6. Birhanu F YK, Addis A, Alemayehu D, Shifera N. Patient-centered care and associated factors at public and private hospitals of Addis Ababa: patients’ perspective. Patient Relat Outcome Meas. (2021) 2:107–16. doi: 10.2147/PROM.S301771
7. Rahel GE, Biks GA, Worku N, Endalew B, Dellie E. Patient-centered care and associated factors among adult admitted patients in South Wollo Public Hospitals, Northeast Ethiopia. Patient Prefer Adherence. (2022) 16:333–42. doi: 10.2147/PPA.S346000
8. Kamimura A, Weaver S, Armenta B, Gull B, Ashby J. Patient centeredness: the perspectives of uninsured primary care patients in the United States. Int J Care Coord. (2019) 22(1):19–26. doi: 10.1177/2053434519836424
9. Kuipers SJ, Cramm JM, Nieboer AP. The importance of patient-centered care and co-creation of care for satisfaction with care and physical and social well-being of patients with multi-morbidity in the primary care setting. BMC Health Serv Res. (2019) 19(1):13. doi: 10.1186/s12913-018-3818-y
10. Nigusie A, Endehabtu BF, Angaw DA, Teklu A, Mekonnen ZA, Feletto M, et al. Status of compassionate, respectful, and caring health service delivery: scoping review. JMIR Hum Factors. (2022) 9(1):e30804. doi: 10.2196/30804
11. Yoon JY, Roberts T, Grau B, Edvardsson D. Person-centered climate questionnaire-patient in English: a psychometric evaluation study in long-term care settings. Arch Gerontol Geriatr. (2015) 61(1):81–7. doi: 10.1016/j.archger.2015.03.010
12. Berhe H BH, Bayray A, Godifay H, Gigar G, Beedemariam G. Status of caring, respectful and compassionate health care practice in tigrai regional state: patients’ perspective. Int J Caring Sci. (2017) 10(3):1118–28.
13. Bergland Å, Hofoss D, Kirkevold M, Vassbø T, Edvardsson D. Person-centred ward climate as experienced by mentally lucid residents in long-term care facilities. J Clin Nurs. (2015) 24(3–4):406–14. doi: 10.1111/jocn.12614
14. Yang Y, Li H, Xiao LD, Zhang W, Xia M, Feng H. Resident and staff perspectives of person-centered climate in nursing homes: a cross-sectional study. BMC Geriatr. (2019) 19(1):292. doi: 10.1186/s12877-019-1313-x
15. Al-Sahli B, Eldali A, Aljuaid M, Al-Surimi K. Person-centered care in a tertiary hospital through patient’s eyes: a cross-sectional study. Patient Prefer Adherence. (2021) 15:761–73. doi: 10.2147/PPA.S286237
16. Luxford K, Safran DG, Delbanco T. Promoting patient-centered care: a qualitative study of facilitators and barriers in healthcare organizations with a reputation for improving the patient experience. Int J Qual Health Care. (2011) 23(5):510–5. doi: 10.1093/intqhc/mzr024
17. Ethiopian Ministry of Health. Health sector transformation plan II 2020/2021–2024/2025. Ethiop Minist Heal. (2021) 25:1–128.
18. Arnetz JE, Zhdanova L, Arnetz BB. Patient involvement: a new source of stress in health care work? Health Commun. (2016) 31(12):1566–72. doi: 10.1080/10410236.2015.1052872
19. Adesanya T, Gbolahan O, Ghannam O, Miraldo M, Patel B, Verma R, et al. Exploring the responsiveness of public and private hospitals in Lagos, Nigeria. J Public Health Res. (2012) 1(1):2–6. doi: 10.4081/jphr.2012.e2
20. Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press (US) (2001).
21. Edvardsson D, Watt E, Pearce F. Patient experiences of caring and person-centredness are associated with perceived nursing care quality. J Adv Nurs. (2017) 73(1):217–27. doi: 10.1111/jan.13105
Keywords: healthcare, patient-physician interaction, magnitude, associated factors, Ethiopia
Citation: Ali M and Charkos TG (2024) A comparative study on person-centered care practice between public and private General Hospitals in Addis Ababa, Ethiopia. Front. Health Serv. 4:1482363. doi: 10.3389/frhs.2024.1482363
Received: 18 August 2024; Accepted: 9 December 2024;
Published: 18 December 2024.
Edited by:
Shashank Saurabh Sinha, King George's Medical University, IndiaReviewed by:
Naseem Akhtar Qureshi, Al-Falah University, IndiaNidhi Vadanere, Vardhman Mahavir Medical College & Safdarjung Hospital, India
Kushal Baidya, Andaman & Nicobar Islands Institute of Medical Sciences, India
Copyright: © 2024 Ali and Charkos. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tesfaye Getachew Charkos, dGVzZmF5ZWdjaEBnbWFpbC5jb20=
 Mierage Ali1
Mierage Ali1 Tesfaye Getachew Charkos
Tesfaye Getachew Charkos