- 1School of Nursing, Johns Hopkins University, Baltimore, MD, United States
- 2Health Policy and Management, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, United States
- 3Mothers Against Medical Error, Columbia, SC, United States
- 4Community Advisory Panel, New England Precision Medicine Consortium, All of Us Research Program, Boston, MA, United States
- 5Department of Family Medicine and Community Health, University of Wisconsin-Madison, Madison, WI, United States
Introduction: Despite the prevalence and devastating consequences of diagnostic breakdowns, there have been minimal efforts to systematically collect patient insight into diagnostic problems and mistakes. Collaborating with patient advocates to guide how patient-derived insights are interpreted and used is a critical, yet often overlooked, approach to identifying actionable solutions that speak to patients' priorities.
Objective: We collaborated with patient advocate co-authors to guide our understanding of findings from a mixed methods survey on diagnostic problems and mistakes, and report implications for patient engagement at three levels of action: (1) individual level before, during, after encounters (micro); (2) within health service delivery systems (meso); and (3) policy advocacy (macro).
Methods: Our research team applied narrative elicitation methods to conduct a novel survey about Americans' diagnostic experiences in a national, population-based survey. We shared early results with patient co-authors who highlighted the importance of further exploring how health systems and clinicians address the aftermath of diagnostic mishaps. Based on their input, we summarized the quantitative and qualitative survey results about the aftermath and worked with our patient co-authors to explore how findings might inform actionable next steps, including efforts to catalyze patient action, quality improvement efforts, and policy reform.
Results: Of the 3,684 survey respondents, about a third (33.0%, 1,216/3,684) of screened households reported diagnostic problems and mistakes in the past four years involving either themselves (18.9%, 697/3,684) or someone close to them (14.1%, 519/3,684). In the aftermath of a diagnostic mishap, over a third reported that someone in the healthcare setting where the mistake occurred acknowledged the mistake (35.9%, 432/1,204). In qualitative findings, reports that the health system “did nothing” surfacing as the most common response. Patient co-authors confirmed the results resonated with their experiences and emphasized the need for health systems to take accountability when a mishap occurs and to take follow-up actions to prevent future mishaps.
Discussion: Patients and care partners not only want and deserve acknowledgement of diagnostic problems or mistakes in their own care, they also want assurance that steps are being taken to prevent similar events from happening to others. Across micro-, meso-, and macro-levels of action, working with patients to understand and act on contributors to diagnostic breakdowns is aligned with high-reliability organizing principles.
Introduction
The need to improve diagnosis is urgent: diagnostic mistakes are the most deadly and costly of medical errors (1). Patient and care partner, a family or friend who partners in a patient's care, (hereon referred to as “patients”) engagement is essential to healthcare transformation (2), including diagnostic quality improvement efforts (3). However, the invaluable insights patients can offer about breakdowns in the diagnostic process (4) and about other factors that adversely impact their diagnostic experiences (5–7) are not regularly collected or used for quality improvement and high reliability organizing (8–10). The latter paradigm, emerging from studies of high levels of safety in high hazard industries (including healthcare delivery), recognizes the importance of deference to expertise, defined as appreciating that the people closest to the work are often the most knowledgeable about that work (10). In healthcare delivery, there is no question that patients are among the people closest to the work.
Many in the healthcare community recognize the need to engage patients and care partners in the design and conduct of research and quality improvement efforts to drive improved care and high reliability performance in the healthcare system. While patient engagement in programs of research focused on treating or managing a specific health condition is increasingly common (11), patient engagement in diagnostic improvement efforts is less common and not yet applied as a critical and natural source of expertise for high reliability organizing for diagnostic safety. The nature of diagnosis adds to the challenge of patient engagement in improvement efforts: diagnosis often occurs over time across multiple settings with multiple clinicians, and reasons for diagnostic mistakes are often multifactorial. The complex nature of diagnosis makes identifying a main cause difficult even for expert clinicians and is aligned with high reliability organizing principles which eschew main cause thinking (e.g., an error occurred because of one clinician's mistake) in lieu of a systems approach (e.g., an error occurred because of a host of factors). However, these same characteristics of diagnosis and its variegated contexts make patient input even more essential: only patients know their full diagnostic trajectory, and this knowledge is critical for understanding where breakdowns may have occurred and informing individual, system-level, and policy-level efforts to improve quality of care.
The value of engaging patients in programs of research for diagnostic quality is clear. Best practice consensus is that patients should be engaged across the continuum of the research process, from project inception through dissemination (11). In practice, however, engagement activities have been typically concentrated in the bookends of the research endeavor, including the beginning (in which patients are engaged in the formative work that informs data collection efforts) and the end (in which patients are engaged in helping to translate and disseminate findings). A stage that often goes overlooked is engaging patients in the analysis of data, despite increasing recognition that patient partners lead to more comprehensive interpretation of findings, and more community-aligned solutions (2, 12). Recent patient-driven efforts, including the citizen scientist community for long COVID (12) and the Quantified Self Community (13), illustrate how meaningful patient engagement and leadership throughout the research process can lead to more comprehensive solutions. The principles of the citizen science community have yet to be robustly applied in improvement initiatives to address diagnostic errors, problems, and mistakes.
Drawing from our narrative elicitation project and recently fielded national survey on patient-reported diagnostic problems and mistakes, we report analytic findings for a key domain of patient experiences with diagnostic failures chosen by our patient advocate co-authors, and together derive learnings and potential actions from these findings. This paper aims to report implications for patient engagement driven by our patient-informed analysis summarized at three levels of potential action: (1) individual level before, during, after encounters (micro); (2) within health service delivery systems (meso); and (3) policy advocacy (macro).
Materials and methods
Research team reflexivity
The authors include two patient advocates (HH, MA), two clinician-researchers (KG, JE), and two organizational researchers (CY, KM). All authors report personally experiencing diagnostic problems and mistakes (also abbreviated as diagnostic mishaps and inclusive of diagnostic errors) as patients and/or care partners.
The authors adopt a patient-centered, whole-person approach to research and hold the beliefs that patients are experts in their health experiences, and that care partners often have a close-in view of their loved one's health experiences. The authors hold the contextual constructivist perspective that meaning is constructed through participants' understandings, the co-authors' interpretations (typically referred to as the researchers' interpretations), the sociocultural context and the interpretations of the scientific community (14). Thus, we recognize that our identities and experiences play a role in shaping our research and reporting.
Background of diagnostic problems and mistakes survey
We conducted a population-based survey drawing on the NORC AmeriSpeak® Panel, nationally representative sample in 2023. The survey was designed in part through work with a technical expert panel (TEP). Patient and care partner representatives, including co-authors, contributed to the TEP. We first pilot tested the survey on a sample of 671 respondents, using the open-ended descriptions of diagnostic experiences to verify characterization of diagnostic problems and mistakes. The survey is included in the Supplementary Material. The NORC AmeriSpeak® panel is a probability-based panel that provides sample coverage of approximately 97% of the U.S. household population. The study was approved by the institutional ethics boards at collaborating universities. Eligible participants were patients or care partners ages 18 or older with proficiency in English. Demographic data was collected from each participant: age, gender, race/ethnicity, and education. Of 3,684 individuals screened, those who had experienced diagnostic problems answered questions about one or more diagnostic experiences over the last four years in three iterations of the survey and in interviews with a subset. Participants who reported experiencing multiple problems and/or mistakes were guided to select a single problem and/or mistake for the survey responses. The resulting survey response rate was 26.5%, with 95.4% completing the entire set of questions. Rich data from more than 1,200 cases of lived experiences with diagnostic problems are available from this data source.
Collaboration with patient co-authors to identify domain for further analysis
After fielding the survey, the research team met with our patient co-authors and presented early results from five key domains of experience where the patient (care partner) is an essential source of information including: (1) how well providers communicated throughout the diagnostic process, (2) how any personal attributes of the patient, such as background, culture, identity or health needs, made diagnostic experiences better or worse, (3) whether a clinician or other person was a reliable source of guidance and support during the diagnostic process, (4) types and duration of harms associated with diagnostic problems that persist and affect patient or family well-being, and (5) what happens in terms of remediation, compensation, or other efforts from the health system/clinical team to address the diagnostic problem or mistake. The patient co-authors were most interested in deeper analysis of the fifth domain, focused on what we termed as the “diagnostic aftermath”, and particularly emphasized current gaps in how clinicians and the health system learn from and address problems and mistakes.
Following the guidance from our patient co-authors, we conducted further exploration of the quantitative and qualitative data related to how the health system and providers addressed the aftermath of diagnostic mishaps. We examined responses to quantitative questions using summary statistics on whether the diagnostic problem or mistake was acknowledged by the healthcare team, whether the healthcare team apologized if an apology was necessary, and, if the patient (care partner) did not report the diagnostic problem or mistake to the healthcare team, why they did not report it (Table 1). We also preliminarily examined the qualitative responses to three open-ended survey questions related to what patients (care partners) perceived could have been done differently. We categorized the responses using a qualitative descriptive approach (15, 16) paired with inductive content analysis (17).
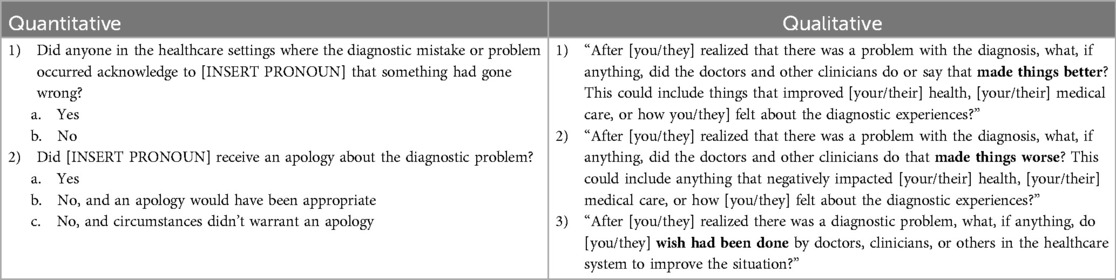
Table 1. Quantitative and qualitative survey questions examined to explore post-event response and resolution.
The patient co-author insights were chiefly gathered based on 3 h of live interaction (a one-hour meeting with both co-authors together and then one hour-long meeting with both patient co-authors separately). The co-authors were sent the findings in advance to review, and the sessions were focused on ascertaining their interpretation of the findings, and their initial ideas around patient-level, healthcare system-level, and policy level solutions. Asynchronous communication occurred throughout for revisions to and confirmation of the insights included.
Results
Of the 3,684 survey respondents, about a third (33.0%, 1,216/3,684) of screened households reported a diagnostic mishap in the past four years involving either themselves (18.9%, 697/3,684) or someone close to them (14.1%, 519/3,684). Of the 3,684 survey respondents, half were female (50.6%, 1,865/3,684) and the majority (62.6%, 2,307/3,684) identified as white, 12.8% identified as Black, and 17.9% as Hispanic. The majority of respondents reported that the healthcare delivery site where the mishap occurred did not acknowledge the mishap or offer an apology. For the engagement of patient co-authors in interpreting these emerging findings, we selected two preliminary categories from the qualitative analysis to focus our discussions, including: (1) post-event response experiences, and (2) post-event resolution experiences.
Prevalence estimates of patient and clinician actions in the diagnostic aftermath shared with patient co-authors
Over a third of survey respondents reported that someone in the healthcare setting where the mistake occurred acknowledged the mistake (35.9%, 432/1,204). Excluding those who reported that an apology was not necessary (n = 377), about one-third of respondents reported receiving an apology (33.0%, 275/839). Those who did not report the diagnostic problem (n = 530) identified the following reasons for not reporting: (1) they did not think it would do any good (43.8%, 232/530), (2) there was no way to do so anonymously (21.5%, 114/530), and (3) because they did not want to get anyone in trouble (17.4%, 92/530). Only one-tenth reported that someone on the care team offered information about a formal review or investigation to determine what caused the problem (10.9%, 135/1,216); more reported that they received an explanation of actions they were taking to prevent similar diagnostic problems (18.8%, 220/1,216). About a third reported that someone on the care team spoke openly and truthfully about the problems (426/1,216, 34.5%).
In the open-ended comments, “did nothing” was the most commonly noted post-event action by providers in the qualitative responses and was identified 325 times. Respondents were most likely to report that they wished the providers had done testing (identified 192 times) or that providers had tried hard and did not give up (identified 170 times).
Illustrative quotes about the diagnostic aftermath shared with patient co-authors
In open-ended comments, survey respondents described post-event response experiences, experiences of diagnostic problems that were not acknowledged, validated, or followed up on in their own care or for future patients. As an example, we shared the following verbatim quote with patient co-authors for discussion:
Well, initially, on the initial phone call, after I called, and then later, when it went through other channels there, less so. They tried to invalidate what I said and invalidate what their own people said on the phone with me, and that's what led to the back and forth emails, until I finally got them to relent and – I mean, all I got out of it was from a financial standpoint, but whether they did anything on that end to correct anything, highly doubtful.
In exploring post-event resolution experiences, survey respondents explained how they perceived the liability culture of medicine and clinician orientation to protect one another undermined efforts to respond to mishaps. For discussion of this preliminary finding, we shared the following passage for co-authors' consideration:
When no one answered my letter about what happened, it made me reluctant to use this practice. Since they are the only one of this type in this area (urogynecology) and I have ongoing issues, I did eventually go back to them. However, I missed annual checkups because I was upset at the way I was treated at the time [and] so what they did, they had one of the administrators of the hospital, she said she was going to file a complaint and I never heard anything. I never heard the results of the complaint. I think it was just a smoke screen, you know, just trying to I guess placate me and not really do anything. So they didn't really do anything. And you know, doctors, they will look out for each other, because they know that something like that could happen to them. It's easy to make a mistake and your career could be ruined. So I think they wanted to protect themselves and that's pretty much what happened.
Patient co-author insight on mixed-methods results
Table 2 describes the insights patient co-authors offered in responding to the quantitative and qualitative findings, including additional insights not described in the text. The finding of the mishap not being acknowledged by the health system was unsurprising to the patient co-authors, and resonated with their own experiences and those they knew about from their patient and family networks. They noted that there is a perceived pressure for clinicians not to admit responsibility for a mishap, and that this perceived pressure was highly correlated with the significance of the mishap (i.e., more serious mishap, less likelihood to admit responsibility). It was also noted that while there are mandates in place that require acknowledgement of medical errors, application of these mandates in practice may be inconsistent given the complexity of diagnostic errors. That the majority of the respondents who wanted an apology did not receive one was also unsurprising to patient co-authors, who also emphasized the value of a sincere apology.
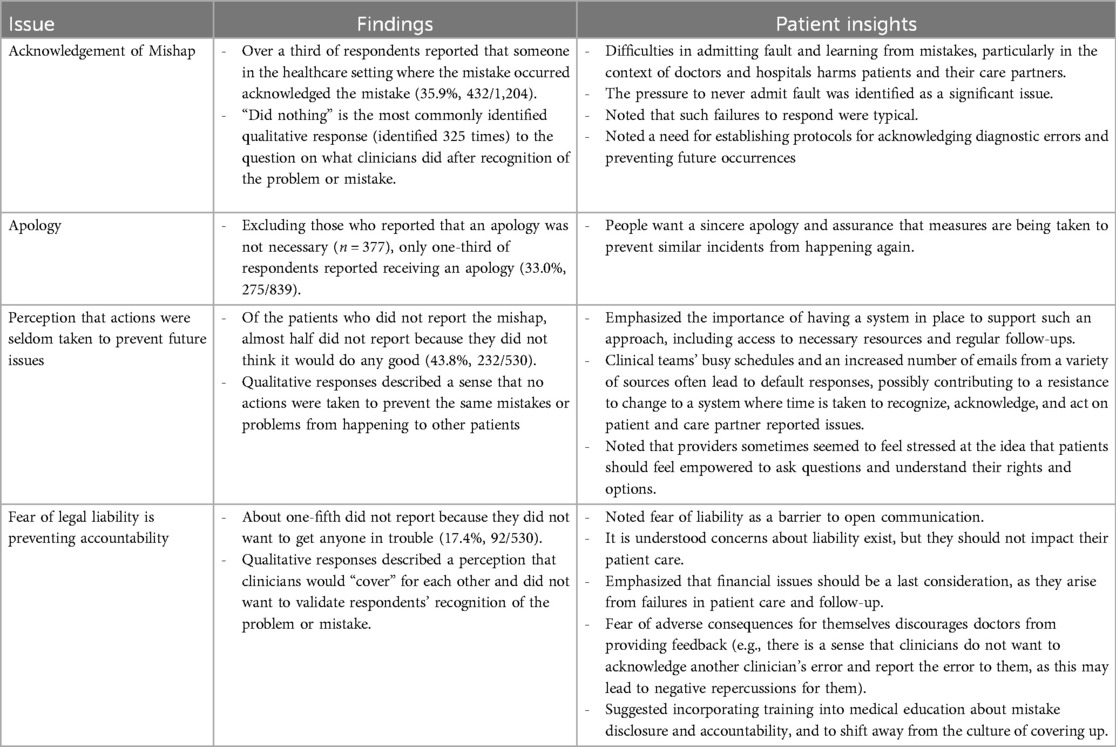
Table 2. Quantitative and qualitative emerging findings on post-event response and resolution experiences, and patient Co-authors insights.
The patient co-authors were interested in the quantitative finding of patients not reporting mishaps because patients did not think it would do any good, and they resonated with the qualitative findings of patients reporting a mishap and perceiving that the health system did nothing to address the root causes of their mishap to prevent future harm to other patients. The importance of actions being taken to prevent future mishaps was viewed as particularly significant. Patient co-authors discussed how acting on patient-reported mishaps appropriately, so root causes could be identified and addressed, requires a health system to devote dedicated resources. They emphasized that having a person to respond to patient feedback and take phone calls meant little if that person did not also have resources to act upon what they heard. Patient co-authors viewed this exchange as a shared endeavor – when a patient reports a mishap, that patient should also be capacitated to request what changes they believe would be helpful to prevent future mishaps.
The fear of malpractice lawsuits was discussed as a barrier to openly communicating with patients when a mishap occurs. One patient co-author emphasized they consider a malpractice lawsuit to mean that the health system failed at taking steps to openly communicate and act on a patient-reported mishap; the malpractice lawsuit is a patient's last resort when they feel the mishap will not otherwise be recognized, including with actions taken to prevent mishaps happening to other patients. The other patient co-author pointed out that malpractice lawsuits are heavily emphasized in medical education training and practice, yet malpractice lawsuits themselves are relatively rare, and that training on mishap disclosure and accountability would not only do more to gain patients' trust and improve outcomes and patient safety, but also potentially prevent both mishaps and lawsuits from occurring. Both patient co-authors emphasized the need for accountability over issue avoidance when fears of a malpractice lawsuit override reality. Patient co-authors felt financial consequences to health systems arise from inaction, rather than from addressing patient concerns: the health systems having to manage financial issues resulting from a problem or mistake were seen as something that would only occur if health systems had not taken the appropriate actions to acknowledge and act on the identified problem.
Future-facing recommendations on micro-, meso-, and macro-level
Together as an authorship team, we discussed future-facing recommendations at the micro-, meso-, and macro-levels. On a patient-level (referred to as the micro level for individual actions), there is a need to raise patient awareness of their rights to report mishaps in care. To our knowledge, most United States' health systems have an office specific to patient experience, where problems can be reported and, when possible, addressed, and the existence of this office and its role should be known by every patient. When patients report a problem, they should be prepared to articulate their desired resolution from the health system, including actions to be taken to prevent future problems. Individual clinicians and clinical teams can also consider the value of openly communicating with patients, and acknowledging when they perceive that there may have been a mishap in their care.
On a meso level, health systems should take steps to build cultures of accountability in their processes for error remediation. Adequate resources are essential for gathering patient feedback on diagnostic process breakdowns and implementing solutions at all levels within the healthcare delivery system. In particular, guidelines are needed on how to respond when a mistake or breakdown happens that is not necessarily attributable to any one person or action, but nonetheless impacted patient care; not acknowledging these issues to the patient leads to diminished trust.
On a macro level (meaning external influences on meso and micro levels), the patient co-authors noted that the Centers for Medicare and Medicaid Services (CMS) require healthcare systems to have mechanisms for patients to report mistakes. However, the fact that issues around diagnosis, often occur over time and across settings without a clear “problem owner” was identified as a potential reason why healthcare systems may be less likely to receive and manage reports of diagnostic mistakes. They noted that healthcare systems could benefit from better guidance on how best to enable reporting, and what actions to take on a problem or mistake, including the important step of closing the loop with the patient.
Discussion
We present our learnings from working with patient co-authors to interpret quantitative and qualitative findings from a nationally representative survey on diagnostic problems and mistakes. These results suggest a path for “what to do next” on the patient, health system, and policy levels (also known as the micro, meso and macro levels) in response to insights from the experiences of many survey respondents. By employing the quantitative weight of these national estimates with accompanying qualitative illustrative quotes as motivators for changes to improve diagnosis in alignment with principles of high reliability organizing, the paper concludes with potential actions at multiple levels which were informed by patient advocate co-authors.
Patient co-authors identification of priority area for further analysis, and then leading our interpretation of the data, widened our understanding of the findings and contributed to a more comprehensive set of potential early solutions. Not only did the patient co-authors have their own firsthand experiences with diagnostic mishaps, they also regularly counsel others through their experiences with medical errors, and thus had wide knowledge of typical patient experiences in the aftermath of problems and mistakes. The patient co-authors' interpretation of analyses described in this paper will lay the foundation for future research by our study team focused on better understanding current practices in the aftermath, and how to improve.
High reliability organizing emphasizes deference to those closest to the process (10). There is no one closer to the diagnostic process than the patient (18). Yet, patients remain largely excluded from health care governance, including how mishaps are identified and managed (19). This exclusion not only further allows unacceptable practices, including not acknowledging a mishap once it has occurred, but also causes health systems to lose out on the substantial learnings enabled by patient inclusion. For example, it was continually emphasized that the very basics of patient communication - sincerely listening to the patient and acknowledging what they perceived as a mishap in their care, seem to have been lost by many healthcare sites. Future research that examines best practices in acknowledging a diagnostic mishap to the patient may benefit diagnostic quality overall.
Limitations
This work is not without limitations. Two patient co-author insights were chiefly gathered over 2 one-hour meetings (one hour-long meeting with both patient co-authors, and a subsequent one-hour meeting with each patient co-author separately). The findings of our study are complex and further time could have been spent with a larger number of patient advocates to gather a broader range of perspectives. Both the quantitative and qualitative analysis conducted of the patient-reported aftermath were preliminary, and we thus may be missing other important findings.
Conclusion
In conclusion, the urgent need for improved diagnosis in healthcare underscores the critical role of patient engagement. Patients possess invaluable insights into diagnostic breakdowns and adverse experiences that are often overlooked in traditional quality improvement efforts. By embracing patient engagement as a cornerstone of high reliability organizing, healthcare systems can harness the expertise of those closest to the work, fostering a culture of safety and driving meaningful improvements in diagnostic accuracy and patient outcomes.
Data availability statement
The datasets presented in this article are available upon reasonable request to the corresponding author. Requests to access the datasets should be directed to Kelly Gleason, a2dsZWFzbzJAamh1LmVkdQ==.
Ethics statement
The studies involving humans were approved by Yale Human Research Protection Program, Institutional Review Boards, FWA00002571. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KG: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. CY: Conceptualization, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. HH: Conceptualization, Validation, Writing – original draft, Writing – review & editing. MA: Conceptualization, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. JE: Conceptualization, Data curation, Validation, Writing – original draft, Writing – review & editing. KM: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. AHRQ R18HS029350 (PIs Newman-Toker & McDonald), AHRQ R01HS029789 (PI Schlesinger), Gordon and Betty Moore Foundation Grant number 10781 (PI Schlesinger).
Acknowledgments
We acknowledge M. Schlesinger, R. Grob, E. Warne, and I. Darne for their role in acquiring funding to support this work, question creation, and in the qualitative coding of patients' and care partners' free-text responses.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2024.1474073/full#supplementary-material
References
1. Newman-Toker DE, Nassery N, Schaffer AC, Yu-Moe CW, Clemens GD, Wang Z, et al. Burden of serious harms from diagnostic error in the USA. BMJ Qual Saf. (2024) 33(2):109–20. doi: 10.1136/bmjqs-2021-014130
2. Riggare S. Patient researchers—the missing link? Nat Med. (2020) 26:1507. doi: 10.1038/s41591-020-1080-4
3. McDonald KM, Gleason KT, Jojodia A, Haskell H, Dukhanin V. Achieving diagnostic excellence: roadmaps to develop and use patient-reported measures with an equity Lens. Int J Health Policy Manag. (2024) 13:8048. doi: 10.34172/IJHPM.8048
4. Bell SK, Bourgeois F, DesRoches CM, Dong J, Harcourt K, Liu SK, et al. Filling a gap in safety metrics: development of a patient-centred framework to identify and categorise patient-reported breakdowns related to the diagnostic process in ambulatory care. BMJ Qual Saf. (2022) 31(7):526–40. doi: 10.1136/bmjqs-2021-013672
5. Gleason KT, Peterson S, Dennison Himmelfarb CR, Villanueva M, Wynn T, Bondal P, et al. Feasibility of patient-reported diagnostic errors following emergency department discharge: a pilot study. Diagnosis (Berl). (2021) 8(2):187–92. doi: 10.1515/dx-2020-0014
6. Gleason K, Dahm MR. How patients describe their diagnosis compared to clinical documentation. Diagnosis (Berl). (2021) 9(2):250–4. doi: 10.1515/dx-2021-0070
7. Bell SK, Dong J, Ngo L, McGaffigan P, Thomas EJ, Bourgeois F. Diagnostic error experiences of patients and families with limited English-language health literacy or disadvantaged socioeconomic position in a cross-sectional US population-based survey. BMJ Qual Saf. (2023) 32(11):644–54. doi: 10.1136/bmjqs-2021-013937
8. Gomes R, Nederveld A, Glasgow RE, Studts JL, Holtrop JS. Lung cancer screening in rural primary care practices in Colorado: time for a more team-based approach? BMC Prim Care. (2023) 24(1):62. doi: 10.1186/s12875-023-02003-x
9. Godde K, Gough Courtney M, Roberts J. Health insurance coverage as a social determinant of osteoporosis diagnosis in a population-based cohort study of older American adults. J Appl Gerontol. (2023) 42(2):302–12. doi: 10.1177/07334648221132792
10. Yousef EA, Sutcliffe KM, McDonald KM, Newman-Toker DE. Crossing academic boundaries for diagnostic safety: 10 complex challenges and potential solutions from clinical perspectives and high-reliability organizing principles. Hum Factors. (2022) 64(1):6–20. doi: 10.1177/0018720821996187
11. Greenhalgh T, Hinton L, Finlay T, Macfarlane A, Fahy N, Clyde B, et al. Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot. Health Expect. (2019) 22(4):785–801. doi: 10.1111/hex.12888
12. Ziegler S, Raineri A, Nittas V, Rangelov N, Vollrath F, Britt C, et al. Long COVID citizen scientists: developing a needs-based research agenda by persons affected by long COVID. Patient. (2022) 15(5):565–76. doi: 10.1007/s40271-022-00579-7
13. Zhang X, Gao P, Snyder MP. The exposome in the era of the quantified self. Annu Rev Biomed Data Sci. (2021) 4:255–77. doi: 10.1146/annurev-biodatasci-012721-122807
14. Madill A, Jordan A, Shirley C. Objectivity and reliability in qualitative analysis: realist, contextualist and radical constructionist epistemologies. Br J Psychol. (2000) 91(Pt 1):1–20. doi: 10.1348/000712600161646
15. Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. (2000) 23(4):334–40. doi: 10.1002/1098-240X(200008)23:4%3C334::AID-NUR9%3E3.0.CO;2-G
16. Sandelowski M. What’s in a name? Qualitative description revisited. Res Nurs Health. (2010) 33(1):77–84. doi: 10.1002/nur.20362
17. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15(9):1277–88. doi: 10.1177/1049732305276687
18. McDonald KM, Bryce CL, Graber ML. The patient is in: patient involvement strategies for diagnostic error mitigation. BMJ Qual Saf. (2013) 22 Suppl 2:ii33–9. doi: 10.1136/bmjqs-2012-001623
Keywords: diagnostic safety, patient safety, patient engagement, family engagement, quality improvement
Citation: Gleason KT, Yuan CT, Haskell H, Anderson MA, Evered JA and McDonald KM (2024) Patient-informed exploration of the aftermath of a diagnostic problem or mistake based on results of a national survey. Front. Health Serv. 4:1474073. doi: 10.3389/frhs.2024.1474073
Received: 1 August 2024; Accepted: 15 November 2024;
Published: 28 November 2024.
Edited by:
Charles Vincent, University of Oxford, United KingdomReviewed by:
Esther Van Poel, Ghent University, BelgiumCarmel Crock, The Royal Victorian Eye & Ear Hospital, Australia
Copyright: © 2024 Gleason, Yuan, Haskell, Anderson, Evered and McDonald. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kelly T. Gleason, a2dsZWFzbzJAamhtaS5lZHU=
 Kelly T. Gleason
Kelly T. Gleason Christina T. Yuan
Christina T. Yuan Helen Haskell3
Helen Haskell3 Kathryn M. McDonald
Kathryn M. McDonald