- 1MacDonald Franklin OSI Research and Innovation Centre, Lawson Health Research Institute, London, ON, Canada
- 2Department of Psychiatry, Western University, London, ON, Canada
- 3Department of Psychology, Toronto Metropolitan University, Toronto, ON, Canada
- 4Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
- 5Department of Psychiatry and Behavioural Neurosciences, McMaster University, Hamilton, ON, Canada
- 6St. Joseph’s OSI Clinic, St. Joseph’s Health Care London, London, ON, Canada
Introduction: Transitioning to civilian life after military service can be challenging for both Veterans and their families. Accessible mental health services are crucial during this period to provide support. The objective of this review was to conduct a rapid review to capture the barriers and identify facilitators that influence access to mental health services for Veterans and their families during the post-service transition period.
Methods: This review was conducted using the Cochrane Handbook for Systematic Reviews of Interventions as a methodological framework and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses - Rapid Review (PRISMA-RR).
Results: A total of 60 articles and 67 independent samples were included in the final data analyses. Across the included articles, this review identified 23 barriers and 14 facilitator themes. Issues navigating the mental health care system was identified as the main challenge among Veterans and their families, and those who received support navigating the system identified this as a significant facilitator. Applying the Theoretical Domains Framework, most of the identified barriers and facilitators were categorized into environmental context and resources domain.
Discussion: The heterogeneity in Veterans' and Veteran families' experiences with mental health care-seeking may suggest that access to mental health care for Veterans and Veteran families cannot be solved by addressing one type of barrier alone. Instead, coordinated efforts to address prioritized systemic, logistical, social, and inter-/intrapersonal obstacles are essential for improving access and optimizing mental health care outcomes. These insights underscore the complexity of considerations for Veterans and families accessing mental health care.
Introduction
For some Veterans, the post-service period is characterized by complex challenges (1, 2). Indeed, over one-third of Canadian Armed Forces (CAF) Veterans report a moderate or very difficult transition to civilian life (3). The reintegration experience involves significant changes to one's physical environment (e.g., work, housing) and identity (e.g., role within the family, relationships), which impose new duties, expectations, and stressors. A difficult transition to civilian life has been associated with poor mental health outcomes (2), including an increased risk of mental disorders and suicide (4, 5). Importantly, these changes are embedded within larger socio-ecological contexts and are amplified by existing health disparities and inequities.
While the perceived need for mental health care increases following the transition from the military to civilian life, St. Cyr et al. (6) found that a similar percentage of active members of the CAF and Canadian Veterans report accessing mental health care in the previous year. However, Veterans may experience different barriers to mental health care than actively serving military personnel, including geographical barriers to care (vs. having health care services readily available on base) and a lack of resources or knowledge of available support for Veterans [e.g., (7–9)]. Further, certain aspects of military culture, such as a strong emphasis on self-reliance, may be integrated into Veterans' core beliefs (10, 11) and deter help seeking. Additionally, the interpersonal, psychological, and behavioural difficulties that may be experienced during the post-service transition may also serve as barriers to treatment-seeking in this population (9, 12). Finally, it is important to note that following the transition to civilian life, access to certain services and supports (e.g., unit support, military-specific mental health care) may become more limited or stop (13, 14). Importantly, research has found a positive relation between mental health care access and health status among Veteran population [see (15)], which may also extend to the families of transitioning Veterans given the experiential link between Veterans and their family members [e.g., (9)]. Indeed, Schwartz et al. (9) note that many of the aforementioned barriers also impact Veteran family members, although the severity of their impact may vary with respect to various individual and environmental factors (9). Further, Maguire et al. (16) found that many health and wellbeing needs of Veteran families are amplified during the transition from military service to civilian life, and these families often face challenges navigating civilian systems of care. Indeed, Veterans and their families may encounter additional difficulties relative to active duty military personnel, especially related to continuity of care following release from the military when sources of health care and benefits change as a result of Veteran status [e.g., from the Department of Defense to Veterans Affairs; (17)]. It is therefore critical to elucidate existing barriers and facilitators to mental health care among Veterans and Veteran families to understand gaps in service access or experiences [including across demographic characteristics, such as gender; see Cornish et al., (12)].
To inform health care planning and policies within Canada, it is necessary to explore contemporary literature which describes experiences among similar populations of Veterans and families. As such, examining literature from across the Five Eyes nations (i.e., Australia, Canada, New Zealand, United Kingdom, United States), which are all Westernized countries sharing important similarities such as governmental structure and historical and military alliances [as noted in (18)], broadens the scope of available information when considering experiences of miliary personnel and families. Further, a representative sample across these countries allows for examinations of certain between-country nuances (e.g., health care delivery systems) in a review context [e.g., (19)]. For example, one report [see (20)] noted high discrepancies in budgets for expenditures, and the number of case managers and staff available to Veterans across various allied nations, among other findings.
Given the complexity of barriers and facilitators affecting mental health service access for Veterans and their families, there is a need for a structured, theory-based approach to identify and address these critical factors effectively. The Theoretical Domains Framework [TDF; (21, 22)] offers a particularly effective method for this purpose. The TDF an integrative framework used to support implementation objectives by providing a sound theoretical basis for assessing behavioural influences and promoting behavioural change to improve outcomes in various clinical contexts. The TDF outlines 14 domains (e.g., knowledge, skills, optimism, beliefs about consequences, goals, etc.) which include 84 component constructs that further specify aspects of each domain [e.g., within the domain of knowledge: procedural knowledge, knowledge of task environment, and other relevant knowledge; (22)]. These domains, in turn, influence physical, psychological, social, automatic, and reflective sources of behaviours that contribute to one's capability, opportunity, and motivation, which interact to produce behaviour (21). Notably, the TDF can be applied both deductively (e.g., as a preliminary framework for content analysis) and inductively [e.g., to generate themes relative to domains; (21)]. In the present review, the inductive utility of TDF was applied to identify barriers and facilitators which might influence treatment-seeking behaviours among Veterans and their families. The TDF has been successfully used to assess barriers and facilitators across different areas of health care [e.g., (23, 24)]; this review extends its use to specifically address the empirical literature concerning mental health service access by Veterans and families, providing a novel insight into this context.
Existing systematic reviews examining health-related behaviours among Veterans either focus exclusively on quantitative research (25) or were specific to help-seeking behaviours (26) which are distinct from actual access to care. Further, existing reviews do not contextualize findings within a validated framework. Taken together, the aim of this review is to identify barriers and facilitators to mental health care by examining the lived experiences (via qualitative and quantitative data) of Veterans and their families accessing mental health care during the post-service period, through the lens of the TDF. Findings from this review can be used to highlight considerations or inform actionable recommendations related to health policy for Canadian Veterans. Specifically, this review aimed to address the following research questions: (1) How do Veterans and family members articulate barriers and facilitators to access to and reception of mental health services during the post-service period?; (2) What factors may optimize access to and reception of mental health services for Veterans and families during the post-service period?; (3) What considerations may need to be in place at the policy level to facilitate changes to better promote mental health access and care for Veterans and their families during the post-service period?; and (4) How does mental health interact with other domains of wellbeing (as represented in the TDF)?
Methods
This review was conducted using the Cochrane Handbook for Systematic Reviews of Interventions as a methodological framework (27). Cochrane guidelines were chosen as they are internationally regarded for their transparency, standardized and replicable methodologies, and methodological rigour across a variety of health and health related disciplines synthesizing both quantitative and qualitative data [e.g., (28–30)]. Indeed, one survey of Moseley et al. (31) found that reviews implementing Cochrane Collaboration procedures demonstrated higher rigour and overall quality. The review process included deploying a search strategy across multiple databases, two levels of screening (title and abstract and full text) against inclusion and exclusion criteria, resolving conflicts at each level, as well as data extraction, data analyses, and data synthesis. This review followed the Preferred Reporting Items for Systematic Review and Meta-Analysis - Rapid Review (PRISMA-RR) guidelines for standards of reporting findings (32).
Search strategy
We conducted a preliminary search for ten relevant articles that should be included in a systematic literature search. These articles served as “benchmark articles” to ensure our search strategy was accurate and comprehensive across a number of indexing databases (33). Our team then consulted with an academic librarian at Western University to confirm the following search strategy. In light of optimizing databases across the benchmarking articles and meeting the minimum number of searched databases required for systematic reviews [e.g., (34, 35)], we selected three databases to perform our search: Scopus, Medline (OVID), and PsycINFO (ProQuest). The following keywords were identified: military, “armed forces”, soldier, RCMP, Veteran*, transiti*, retir*, resources, “mental health care”, programs, “mental health service use”, “mental health services use”, “mental health care”, “mental health support”, “mental health treatment”, “mental health use”, “psychiatr* service use”, “utili*ation”, “help-seeking”, and “mental health” (see Supplementary Material for string terms). We imposed a date restriction of 10 years from the search date (i.e., 2013–2023), which was conducted on December 18, 2023, in order to focus on contemporary barriers and facilitators of mental health care. In addition, the Veterans Affairs Canada (VAC) Research Directorate webpage was scanned to identify any potentially relevant grey literature.
Inclusion and exclusion criteria
Articles were included if they:
(1) focused on military Veterans who have been released from service for any reason,
(2) focused on families of Veterans,
(3) reported on post-service experiences and mental health service use, and
(4) described barriers and/or facilitators to accessing and/or using mental health services.
Articles were excluded if they:
(1) did not differentiate between active duty and Veteran populations,
(2) reported the occurrence of a barrier or facilitator without any context of any specific barrier or facilitator,
(3) exclusively focused on medical services, including chronic pain,
(4) were non-study papers (e.g., books, news articles),
(5) not available in English or French,
(6) were not from the Five Eyes Countries [Canada, United States, United Kingdom (UK), Australia, New Zealand], and
(7) were published before 2013.
With respect to exclusion criterion (7), the goal of this review was to be able to provide actionable policy recommendations related to mental health service use by Veterans and their families. As such, this review will focus on capturing relatively contemporary barriers and facilitators to mental health care. Further, given that rapid reviews are often conducted to support policy-focused work [e.g., (36)], a 10-year search restriction allowed for the requisite timely execution of this style of review in consideration of the scope of available literature.
Study selection
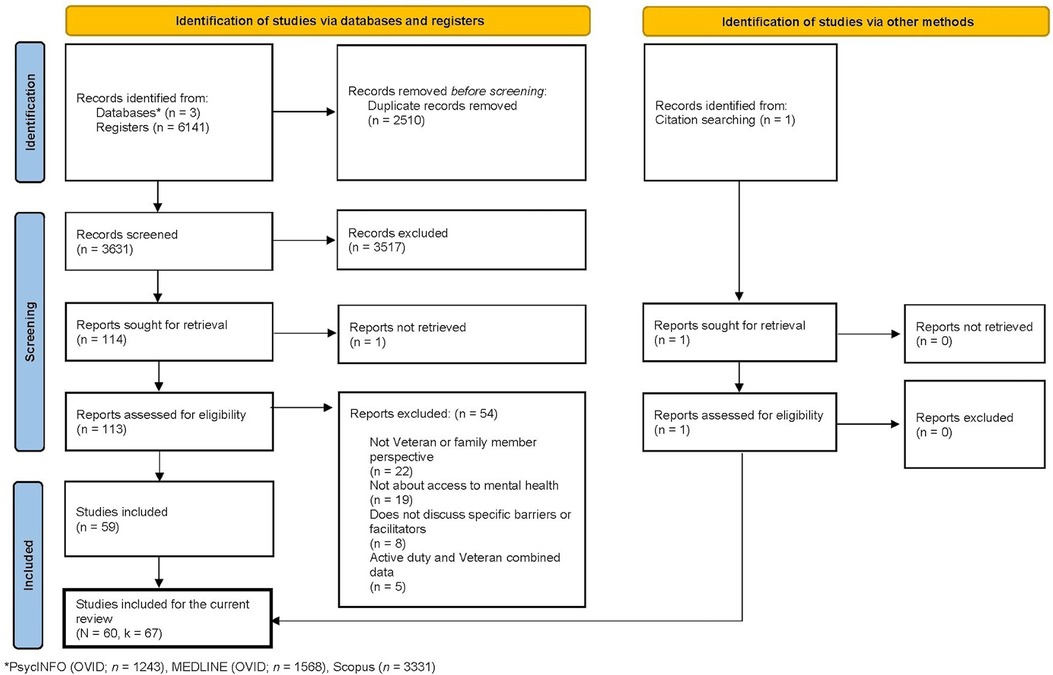
Following the deduplication of database outputs, two screeners independently reviewed each article against the inclusion and exclusion criteria for title and abstract review and full-text review. Across the entire body of citations, seven screeners participated in the screening process. Interrater reliability was good for title and abstract review [using percent agreement (97.2%), and Kappa (Fleiss and Conger; 0.742)] and full-text review [using percent agreement (90.4%), and Kappa (Fleiss and Conger; 0.705)]. At the data extraction stage, two raters extracted relevant information from included articles. Conflicts were resolved at each level of screening by study authors until a consensus was reached (see Figure 1). SWIFT-Active Screener, a web-based, collaborative review software that accelerates the screening processes, was used for the title and abstract and full-text review stages. SWIFT enlists a proprietary machine-learning algorithm to prioritize relevant articles for screening with a high degree of accuracy (37). Using this approach, our review and screening times were reduced without risk or loss of accuracy.
Data extraction
The following information was extracted from each article (1): article and demographic information, and (2) barriers and facilitators to mental health service use reported by Veterans or their family members. For article and demographic information, the following data were extracted: type of article (i.e., empirical article or dissertation/theses, further broken down by qualitative, quantitative or mixed data), country of study (i.e., Canada, United Kingdom, United States, New Zealand, Australia), age, gender/sex (i.e., mixed, women/female, men/male, transgender, not specified), race (i.e., White/European, Black/African/Caribbean, East Asian, Southeast Asian, Hawaiian/Pacific Islander, Indigenous Peoples, Latin American/Hispanic, Multiracial/Multiethnic, other, mixed, not specified), income (i.e., less than $40,000, $40,000–$59,999, $60,000–$79,999, $80,000–$99,999, $100,000–$119,999, $120,000 or more, mixed, not specified), education (i.e., less than high school, high school, college, undergraduate, graduate/professional degree, mixed, not specified), length of service, type of release (i.e., honourably discharged, dishonourably discharged, not specified), number of years since release, and Veteran vs. family perspective (i.e., Veteran, family, both).
Barrier and facilitator information associated with mental health service use (as reported by Veteran or their family members) was extracted from each article. To be considered a barrier, the results of the study must have explicitly stated an obstacle, difficulty, or challenge Veterans and/or their family members experienced during access to mental health service use. To be considered a facilitator, the results of the study must have explicitly stated a factor that eased the access to mental health service use for Veterans and/or their family members. As such, two independent reviewers extracted the data in the following stages:
○ Step 1. Extracted direct quotes or empirical outcome data from the article and categorized as being experienced by a Veteran or family member.
○ Step 2. Examined the raw data and identified common, repeated themes from a policy informed lens and categorized into barriers or facilitators within the dataset.
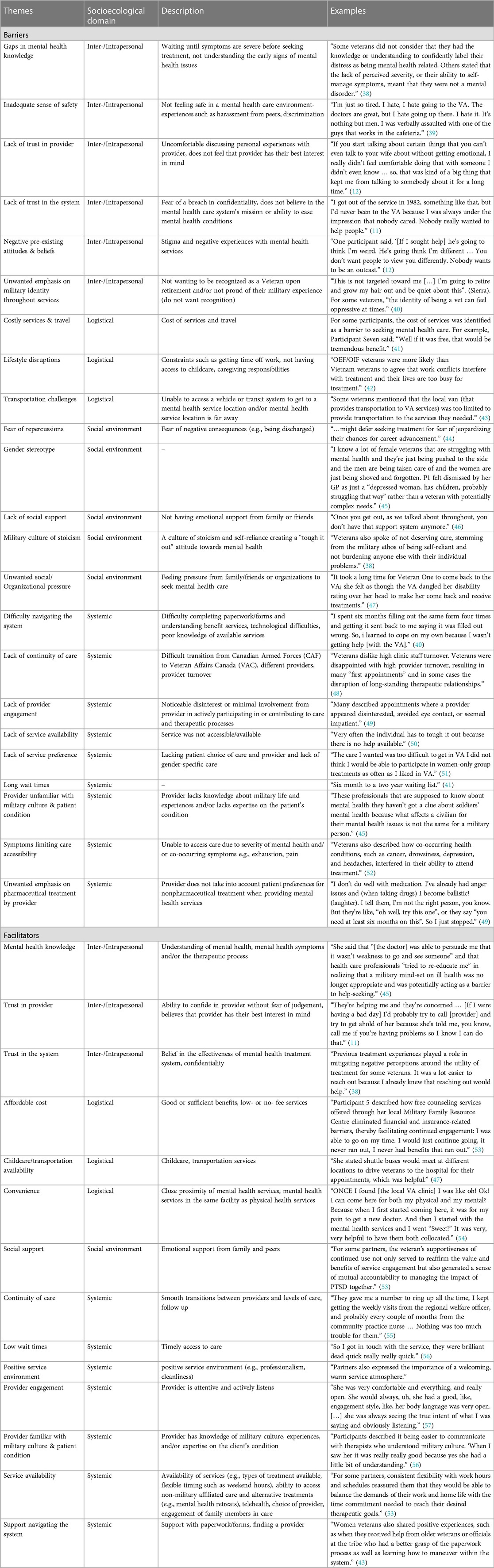
○ Step 3. Systematically grouped the emerging themes and subsequently organized them into relevant categories (e.g., Barriers–Veterans; Barriers–family members; Facilitators–Veterans; Facilitators–family members; see Table 1 for descriptive information about the emerging themes). For the primary analysis, a thematically-driven approach was used to classify barriers and facilitators to mental health care, rather than a pre-existing theoretical framework, to ensure a good fit of the data. For the secondary analysis, we mapped barriers and facilitators onto the domains of the TDF.
Risk of bias assessment
The Mixed Method Appraisal Tool [MMAT; (58)] was used to evaluate the risk of bias among articles. The MMAT is a valid and efficient quality assessment tool that allows for simultaneous appraisal of qualitative, quantitative, and mixed methods studies. Each article was categorized by study type (i.e., qualitative, quantitative, or mixed methods). Studies were then rated based on the MMAT criteria corresponding to the respective study type. Criteria included five specific appraisal questions assessing methodological characteristics (e.g., appropriate and effectively executed methodological approach) relative to the type of study conducted. Criteria were evaluated with “yes”, “no”, and “can’t tell” answer options.
Data analysis
Smartsheet and Microsoft Excel were used for data analyses. Demographic information was examined using descriptive statistics (i.e., frequencies; means and standard deviations). The themes emerged through deductive analysis based on our own binning process. Initially, themes were identified and categorized as either barriers or facilitators. These themes were then thematically organized into socio-ecological domains. This organization was based on the structural, environmental, or individual level at which these barriers and facilitators were described as relevant: (1) Systemic which refers to the obstacles or benefits that are embedded within the structure, policies, or practices of a system that impacts one's access to mental health services, (2) Inter-/Intrapersonal which refers to obstacles or benefits arising from interactions between individuals or within an individual's own thoughts, beliefs, or behaviors which influence help-seeking for mental health care, (3) Logistical which refers to obstacles or benefits that arise from practical considerations such as transportation, scheduling, or infrastructure limitations related to accessing mental health services, and (4) Social Environment which refers to obstacles or benefits originating from an individual's physical surroundings, social interactions, or external influences, which influence help-seeking for mental health care. While an emerging theme may recur throughout an article, our results are focused on the identification of unique themes within each article, rather than the frequency with which themes are repeated within an article.
Barriers and facilitators were then thematically organized across the 14 domains of the TDF: (1) Knowledge which refers to being aware of the existence of something, (2) Skills which refer to abilities or proficiencies acquired through practice, (3) Social/Professional Role and Identity which refers to the behaviours and qualities that individuals display in social or work settings, (4) Beliefs about Capabilities which refers to the level of acceptance of an ability that a person can put to use, (5) Optimism which refers to the level of belief that a goal can be attained or that something will happen for the best, (6) Beliefs about Consequences which refers to the level of acceptance for the outcomes of a behaviour in a particular setting, (7) Reinforcement which refers to the arrangement of a dependent relationship or contingency between a stimulus and response which increases the odds of that given response, (8) Intentions which refers to the decision that one makes to perform a behaviour in a certain manner, (9) Goals which refers to a mental representation of an end-state that an individual seeks to achieve, (10) Memory, Attention, and Decision Processes which refers to the ability to focus selectively, retain information, or make a choice between alternatives, (11) Environmental Context and Resource which refers to circumstances of an individual's environment or situation that either promote or discourage the development of abilities, independence, or adaptive behaviours, (12) Social Influences which refers to interpersonal processes that can lead individuals to change their behaviours, thoughts, or feelings, (13) Emotion which refers to reactionary patterns involving experiential, behavioural, and physiological elements to deal with a significant matter or event, and (14) Behavioural Regulation which refers to anything that is aimed at changing or managing measured or observed actions.
MMAT scoring to assess the risk of bias was calculated based on the percentage of MMAT criteria met (i.e., number of “yes” responses). Hong et al. (58) noted that calculating an overall score is not advisable. As such, studies were rated based on the percentage of criteria met [i.e., 20, 40, 60, 80, 100; per (58)].
Results
Study characteristics
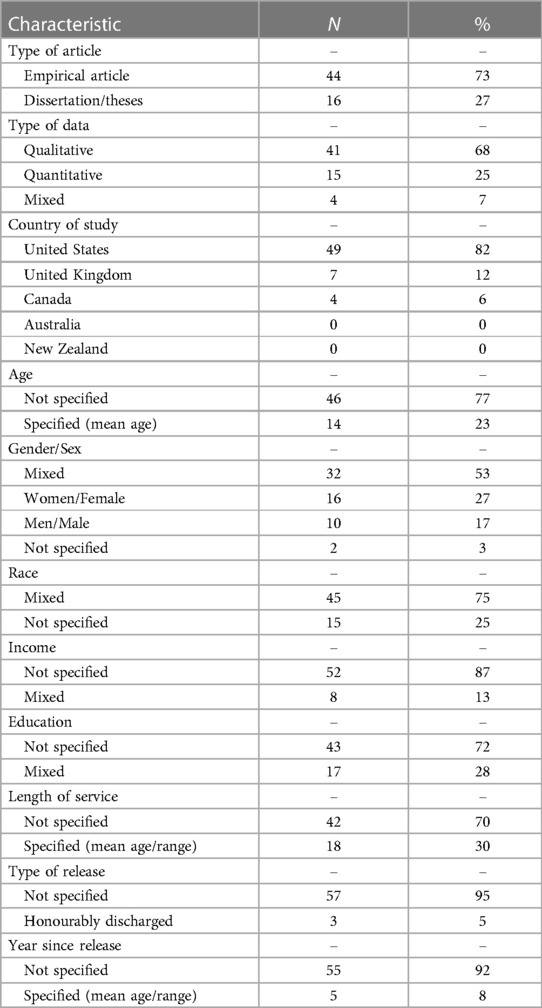
The final sample consisted of 60 articles (denoted with N) with 67 independent samples (denoted with k; Figure 1; see Supplementary Material for raw data and reference list of included articles). The samples mostly included Veteran (k = 58) perspectives, with a few from family perspectives (k = 9). Across all included articles, this review identified 23 barriers and 14 facilitator themes. It is important to note that the demographic characteristics reported in Table 2 do not fully represent the participants across samples due to inconsistencies in the information reported across the included samples (see Table 2 for characteristic information). Notably, across all samples, 11 articles discussed topics related to military sexual trauma.
Examination of barrier and facilitator themes across socio-ecological domains
Veteran perspective
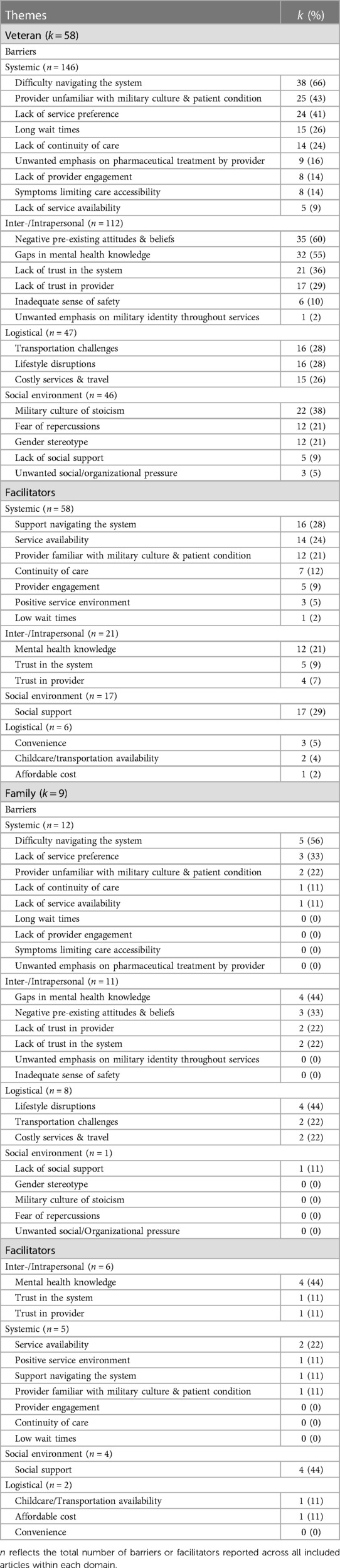
Across all samples that captured the Veteran's perspective (k = 58), the most common type of barrier experienced was systemic in nature (n = 146; in this section, n denotes the total number of barriers or facilitators reported across all included articles within a respective domain as per Table 3). Within this domain, the most commonly identified theme was difficulty navigating the system (e.g., difficulty completing forms; k = 38; 66%), followed by health care provider (i.e., physician, clinical psychologist, or psychotherapist) unfamiliar with military culture and patient condition (e.g., provider lacks knowledge about military life; k = 25; 43%), and lack of service preference (e.g., lacking patient choice of care; k = 24; 41%). The second most common domain was inter-/intrapersonal (n = 112). The most common theme identified within this domain was negative preexisting attitudes and beliefs towards mental health (e.g., stigma; k = 35; 60%), followed by gaps in mental health knowledge (e.g., not understanding the early signs of mental health issues; k = 32; 55%), and lack of trust in the system (e.g., belief that the mental health care system cannot ease mental health conditions; k = 21; 36%). The third most common domain was logistical (n = 47). In this domain, the identified themes exhibited relatively equal prevalence: transportation challenges (e.g., location of mental health service is too far away; k = 16; 28%), lifestyle disruptions (e.g., not able to take time off from work; k = 16; 28%) and costly services and travel (e.g., cost of service is too expensive; k = 15; 26%). Social environment was the least identified domain (n = 46). Within this domain, the most common theme was a military culture of stoicism (e.g., a culture creating a “tough it out” attitude; k = 22; 38%), followed by fear of repercussions (e.g., fear of negative consequences such as losing out of job opportunities; k = 12; 21%), and gender stereotypes (k = 12; 21%).
As for facilitators reported by Veterans, similarly, the most common domain was systemic (n = 58). Specifically, support navigating the system was the most prominent theme (k = 16; 28%), followed by service availability (k = 14; 24%), and health care provider familiarity with military culture and patient condition (k = 12; 21%). The second common domain was inter-/intrapersonal (n = 21). In particular, the most common themes were mental health knowledge (k = 12; 21%), followed by trust in the system (k = 5; 9%), and trust in provider (e.g., feeling the provider has their best interest in mind; k = 4; 7%). The third most common domain was social environment, with social support being the only emerging theme (k = 17; 29%). Lastly, logistical was the least prevalent domain (n = 6). Within this domain, the reported themes included convenience (e.g., mental health service is close; k = 3; 5%), childcare/transportation availability (k = 2; 4%), and affordable cost (k = 1; 2%; see Table 3 for reported themes within each domain across barriers and facilitators, as experienced by Veterans).
Family perspective
Similarly, across all samples that captured the Veteran family's perspective (k = 9), the most common barrier was systemic (n = 12). Specifically, difficulty navigating the system was reported as the most prominent theme (k = 5; 56%), followed by lack of service preference (k = 3; 33%) and provider unfamiliar with military culture and patient condition (k = 2; 22%). The inter-/intrapersonal domain was reported with almost equal frequency (n = 11). Within this domain, gaps in mental health knowledge was the most prominent barrier (k = 4; 44%), while negative preexisting attitudes and beliefs (k = 3; 33%), trust in provider (k = 2; 22%), and trust in the system (k = 2; 22%) were equally common. The third most common domain was logistical (n = 8). In particular, lifestyle disruptions were most common (k = 4; 44%), followed by transportation challenges (k = 2; 22%) and costly service and travel (k = 2; 22%) reported as equally common. The final domain, social environment, was not a prominent domain within the family literature (n = 1).
With regards to facilitators, the most prominent domain was inter-/intrapersonal (n = 6). Within this domain, the only repeated theme was mental health knowledge (k = 4; 44%). The next most common domain was systemic (n = 5), with service availability (k = 2; 22%) being the only repeatedly reported theme. Importantly, the social environment domain found social support was the only theme reported (k = 4; 44%). Lastly, the logistical domain was not prominent (n = 2; see Table 3 for reported themes within each domain across barriers and facilitators, as experienced by families).
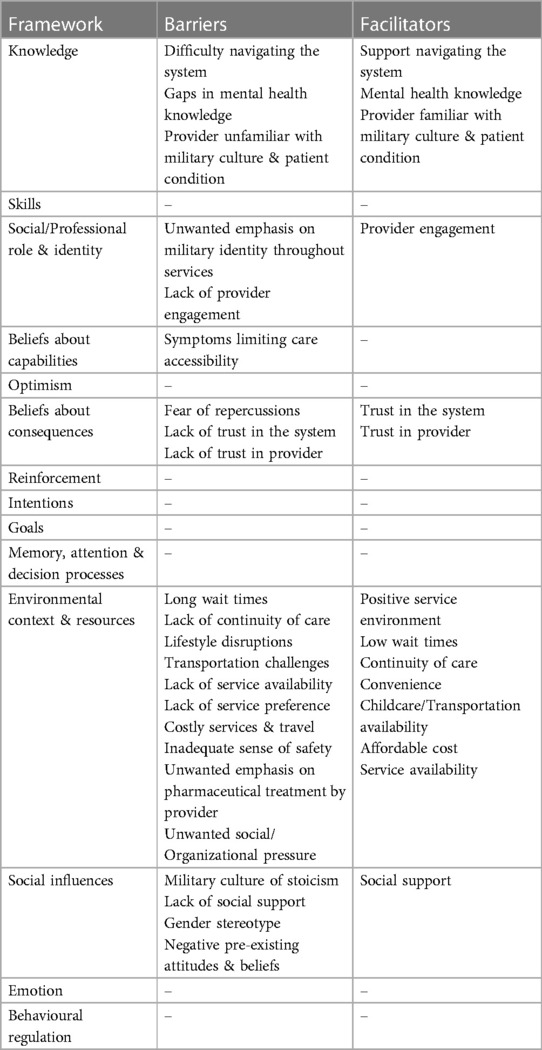
Examination of the barriers and facilitators within the Theoretical Domains Framework
When examining the themes within the TDF framework, six of the domains were captured by the data in this review: knowledge, social/professional role and identity, beliefs about capabilities, beliefs about consequences, environmental context and resources, and social influences. Most of the 23 identified barriers were categorized into environmental context and resources (n = 10; 43%; in this section, n denotes the number of barrier or facilitator themes across TDF domains per Table 4), followed by social influences (n = 4; 17%), knowledge (n = 3; 13%) and beliefs about consequences (n = 3; 13%), social/professional role and identity (n = 2; 9%), and beliefs about capabilities (n = 1; 4%). As for facilitators, most of the 14 identified facilitators were embedded into the environmental context and resources (n = 7; 50%), followed by knowledge (n = 3; 21%), beliefs about consequences (n = 2; 14%), social/professional role and identity (n = 1; 7%) and social influences (n = 1; 7%).
Risk of bias (Mixed Method Appraisal Tool)
Overall, the methodological quality of the included articles (N = 60) varied: 52% of the articles met ≤60% of MMAT criteria (31/60; 20% [n = 3], 40% [n = 12], 60% [n = 16]), while 48% of the articles met >60% of MMAT criteria (29/60; 80% [n = 28], 100% [n = 1]). Notably, the most common criterion was a quality threshold of 80% (see Supplementary Material for MMAT scores of all included articles).
Discussion
Emerging barrier and facilitator themes within the socio-ecological domains
Veterans and Veteran family members identified a number of common barriers and facilitators across systemic, interpersonal/intrapersonal, logistical, and social environmental domains.
Systemic
Systemic barriers were the most cited barriers to accessing mental health care with issues navigating the system reported by over half of the Veteran samples. Upon retirement, Veterans move from a military-specific health care system to the provincial or territorial health care system in their province or territory of residence, with additional VAC health care benefits being available for Veterans who have service-related injuries (59). This change can pose new difficulties such as not completing the necessary paperwork to access the benefits available to them [see (10, 60)], which may prohibit Veterans from initiating or continuing mental health care in the post-service period. Additionally, Veteran samples noted a lack of military cultural competence and/or unfamiliarity with treating mental health conditions among providers. Veterans represent a distinct cultural group which may have different health care needs relative to non-Veterans. Tam-Seto et al. (61) notes that a lack of cultural awareness, sensitivity, knowledge, and skills required to meet the unique mental health needs of Veterans can diminish the quality of the therapeutic relationship and impact wellbeing. This finding highlights the importance of the therapeutic alliance in this group [see (62)]. A lack of service preferences (e.g., requests for a female mental health service provider or individual therapy vs. group therapy) was also identified as a prominent barrier by Veterans. Distinct from barriers which impede access to services, service preferences may be equally as important in determining Veteran engagement (63).
Findings also revealed that when these barriers are rectified, these themes can function as significant facilitators. For example, while difficulties navigating the system were the most common barriers, support navigating the system was the most common facilitator. In this sample, Veterans noted the importance of receiving assistance from fellow Veterans, health care providers, and staff members. Similarly, service availability and having health care providers with military cultural competence were other prominent facilitators of receiving mental health care. Indeed, having a variety of mental health services and treatment modalities available is important in addressing individual differences in needs [especially among minority groups such as women Veterans; (49)]. Further, access to providers educated in the unique occupational stressors that are associated with a military career can help to facilitate the transition to the civilian health care system and ensures access to relevant resources (61, 64).
Families of Veterans identified having difficulty navigating the system as the most common systemic barrier to care. Schwartz et al. (9) found that family members of Veterans are often unaware of the formal mental health resources available to them and are unclear on the administrative processes required to access these supports. Service availability was the most reported systemic facilitator; however, the representation of samples is too small to reliably interpret.
Interpersonal/intrapersonal
Negative pre-existing attitudes and beliefs were reported among many of the Veteran samples in the review. One review exploring the association between mental health beliefs and service use in military populations found that personal beliefs (about mental health, including stigma) are an important predictor of mental health service use [see (65)]. Veterans also frequently reported gaps in mental health knowledge related to mental health symptoms and the potential treatments available to address them [see (66)]. Increasing mental health knowledge may increase help-seeking and service use by minimizing the impact of other barriers. For example, a study of female Veterans in the U.S. found that increasing mental health knowledge reduced stigma and, thus, indirectly increased mental health treatment-seeking behaviours (67). Veterans also reported a lack of trust in the system, including but not limited to federally operated Veterans Affairs health organizations. One qualitative study found that lack of trust in the U.S. Veterans Affairs (VA) health care system acted as a significant barrier to mental health care-seeking, because of concerns it would be “nonresponsive, ineffective, and uncaring” [see (11)]. Concerns over confidentiality or the ability to provide high-quality services in a timely manner also contribute to a lack of trust in Veteran health organizations (22). Relatedly, a lack of trust in their mental health care provider was also reported as a barrier among some samples. Consistent with the previous themes, mental health knowledge was identified as the most common facilitator among the Veteran samples. This aligns with previous research suggesting that increased mental health knowledge is inversely associated with negative attitudes towards mental health and mental health treatment (68). As in the Veteran samples, gaps in mental health knowledge were the most commonly reported intra-/interpersonal barrier among Veteran family samples while having mental health knowledge was the most frequently reported facilitator. Family members who are more aware of the impact that living with a Veteran experiencing mental health issues can have on their own mental health may be more inclined to seek mental health treatment themselves.
Logistical
Transportation challenges were identified as the most prominent logistical barrier in Veteran samples. This encompasses the distance to the closest mental health care provider (i.e., too far to travel) or a lack of a reliable mode of transportation to reach these services. This may be a particular concern for Veterans residing in rural areas, where there are fewer mental health care providers and resources available (11). Lifestyle disruptions, such as needing to request time off work or finding a childcare provider to attend treatment (69), were also reported as barriers to mental health care in this review. It is important to note that these barriers may carry additional costs that render mental health care unaffordable, particularly for Veterans who may not have additional benefits or health care coverage. Convenience was the most reported logistical facilitator in this sample. Convenience may encompass living near mental health services, accessing services remotely, or being able to receive mental health services in the same location as physical health services. Previous research indicates that logistical barriers are frequently reported barriers to health care among military spouses (70). Among the samples of Veteran families included in this review, lifestyle disruptions–such as needing to take time off work or finding childcare–was the most reported barrier. Indeed, Maguire et al. (16), notes that care coordination can be particularly challenging among Veteran families with complex mental health needs (i.e., those impacting more than one domain of functioning), as may be the case during the post-service period. Logistical facilitators to mental health care were not widely commented on by the Veteran families included in the review.
Social environmental
The stereotypical military characteristics of stoicism and self-reliance were the most commonly reported social environmental barriers to seeking mental health care among the Veteran samples included in this review. One study exploring barriers to mental health care among U.S. Veterans found that self-reliance and stoicism were the most common attitudinal barriers to mental health care, with many Veterans reported enduring their mental health systems without complaint until the need for mental health treatment became undeniable (11). Indeed, another study found that Veterans delayed seeking mental health care for almost twelve years following their release from the military [see (71)]. Concerns about the potential consequences mental health care-seeking might have on their military careers were also identified as a common barrier. Some of these concerns may include being treated differently by military leadership (72) or adverse military career implications (73). Additionally, gender stereotypes were identified as a barrier to mental health care in some studies. Previous research shows that men and women Veterans experience different barriers to mental health care, with women being more likely to indicate that their gender itself, as well as gender-based discrimination experienced during their military service, act as barriers to seeking mental health services (74). Female Veterans may also feel uncomfortable in male- dominated health service environments, such as VA mental health clinics (75).
Social support was the only social environmental facilitator cited in the Veteran samples included in this review. Positive social support (from partners, civilian communities, peers, etc.) has been identified as a motivator for seeking mental health care in a number of studies involving military Veterans [e.g., (11, 25, 55)]. Further, research suggests that mentor/mentee-like relationships with other Veterans who have experienced and successfully sought help for a mental health concern may be a particularly valuable source of social support for Veterans contemplating mental health treatment initiation (11).
Few Veteran family members identified any social environmental barriers to mental health care: only lack of social support was identified in one of the Veteran family samples as a barrier to mental health care. Previous research has identified lack of social support as a generalized barrier to mental health care (16); however, it may be possible that this is significantly less of a concern for Veteran family members than it appears to be for Veterans themselves.
Positive social support was the only social environmental facilitator of mental health care identified in the Veteran family samples. Recent research suggests that family involvement in treatment for military-related posttraumatic stress disorder is, for some, motivated by social relationships [e.g., improving family life; protecting familial relationships; (52)]. This may be a unique form of social support that motivates Veteran family members to engage in mental health care.
Mapping barrier and facilitator themes onto the Theoretical Domains Framework
The barriers and facilitators to mental health care identified in this review mapped on to 6 out of 14 TDF constructs: knowledge, social/professional role and identity, beliefs about capabilities, beliefs about consequences, environmental context and resources, and social influences (see Table 4).
Most of the barriers identified in this review reflected the environmental context and resources, and social influences related to mental health care experiences. According to the TDF Behaviour Change Wheel [see (21)], environmental context and resources and social influences jointly contribute to opportunity. Barriers within these domains limit opportunity and influence both physical and social sources of behaviour. In the context of this review, Veterans and Veteran families reported how their engagement in mental health care services are limited by numerous barriers affecting access and availability (e.g., cost, service preferences), and the social contexts they are embedded within (e.g., military culture of stoicism, gender stereotypes). Per the TDF these barriers are inhibiting both physical and social components of treatment-seeking behaviours. These findings highlight specific areas (i.e., enhancing opportunity via environmental and social strategies) for policy recommendations or interventions aimed at engendering behavioural change related to help-seeking in these populations.
Notably, the environmental context and resources domain also emerged as an important facilitator of mental health care experiences. As previously noted, these facilitators often reflect the inverse of barriers (e.g., service availability vs. lack of service availability), highlighting the importance of rectifying prominent barriers to optimize experience and outcomes. Further, this finding serves to help refine our examination of gaps in services and supports with respect to the TDF. While environmental factors detract from opportunity, most facilitators also fell into this category, while facilitators with respect to social influences were very limited (i.e., social support only). Taken together, it may be that social influences are disproportionately detracting from opportunity relative to environmental factors; however, the representation of facilitators was relatively limited, and this review did not determine the magnitude of the effect of these barriers and facilitators beyond reported frequency. The knowledge domain also emerged as an important factor in facilitating experiences of Veterans and Veteran families' experiences with mental health care services. With respect to the TDF Behaviour Change Wheel, knowledge (e.g., mental health knowledge, and support navigating the system) bolsters capability and positively influences psychological sources of help-seeking behaviours.
Implications for research and policy
The findings of this review of qualitative and quantitative research align well with a rapid review conducted by Randles & Finnegan (26), as well as Hitch et al.'s (25) systematic review of quantitative research exploring barriers and facilitators to health care-seeking. Despite differences in the types of studies included across all three reviews, the consistency of findings increases confidence in the reliability and accuracy of our findings.
The heterogeneity in reported experiences observed across barriers and facilitators included in this review suggests that perhaps access to the system is not standardized or is based on other factors, such as reason for release from the military or familiarity with the system. Additionally, variability in structure, availability, and cost of mental health services between and within countries (e.g., state to state) may account for some of the variability with respect to thematic valence. However, these variations (i.e., experiencing a systemic factor as a barrier or facilitator) can be used to identify opportunities to create equitable policies that increase access to mental health services. The use of objective measures of barriers to mental health care (e.g., wait time from referral to support) may help to disentangle some of the heterogeneity observed in this review.
Findings of this review may also be used to inform relevant policy recommendations at the federal and provincial/community level. Concerted efforts to address the systemic, logistical, social environmental, and intra-/interpersonal barriers to mental health care should occur conjointly in order to maximize their benefit. For example, this might include building upon recent efforts by the CAF to increase mental health awareness and reduce stigma. Reducing stigma around service-related mental health concerns may promote help-seeking behaviours in military (and subsequently Veteran) populations. Federal agencies should aim to ensure the availability of culturally competent providers within their networks while also exploring avenues to decrease logistical and demand barriers to mental health care, such as providing childcare support and offering women-only hours in their mental health clinics. Nevertheless, access to mental health care for Veterans and Veteran families cannot be solved through addressing one type of barrier alone. For example, efforts to decrease stigma will not get more Veterans into treatment if supply issues are not addressed or the system remains difficult to navigate.
Similar steps could be taken at the provincial health care level. The civilian health care system is not always well equipped to treat the mental health needs of Veterans, particularly in areas without a large military or Veteran population. Efforts to identify the root cause(s) of insufficient military cultural competency, such as lack of training, could help address the paucity of community-based mental health providers with military cultural competence, while targeted recruitment efforts could be used to increase the number of mental health care providers in rural regions.
Limitations and strengths
The findings of this review should be interpreted in consideration of a few limitations. First, we were unable to conduct subgroup analyses. As such, the overall findings of this review disproportionately reflect experiences of mental health care for an American Veteran population via qualitative experiential accounts relative to mixed methods designs and do not adequately reflect the experiences of Veterans from other Five Eyes nations, and Veterans with intersectional identities. While these countries share important similarities, the inclusion of samples from Australia and New Zealand in addition to a more robust representation of Canadian and UK samples in this review may have allowed us to capture meaningful trends in access across various types of health care delivery systems (e.g., public vs. private), which would have provided important contextual nuance with respect to these experiential findings especially as they related to barriers associated with cost. Further efforts to disentangle whether the systemic barriers and facilitators to mental health care vary across nations and health care systems would help solidify our understanding of the specific barriers and facilitators faced by Canadian Veterans and families. Second, most studies did not provide information about the amount of time between data collection and end of participants' military service. The military to civilian transition period, which can be a period of increased need for mental health services, may have different barriers or facilitators to mental health care than in the years following this transitional period. Finally, our review contained only a few samples of Veteran families. This review adds to a growing body of literature attempting to elucidate and contextualize experiences of mental health care for Veteran families and calling for additional research within this population.
This review also had several strengths. First, this review provides a much-needed synthesis of literature in this area and summarizes available information on barriers and facilitators to mental health care for both Veterans and Veteran families. Importantly, this review highlighted that when Veteran health organizations address barriers to mental health care, these barriers became facilitators, enabling access to mental health services. Second, the quality of the studies included in the review were adequate, as measured by the MMAT, indicating that information included in this review was collected and analyzed with rigour. Finally, the findings of this review, in conjunction with the context provided by the TDF, highlight opportunities for future research, intervention approaches, and policy changes.
Considerations for future directions
Future studies in this field should aim to pinpoint specific behavioural determinants of health-seeking via primary data collection with Veterans and Veteran families. Using a structured framework such as the TDF would provide a more comprehensive context-specific understanding, and capture data that is reflective of current policies and community attitudes. Second, studies should implement conjoint analyses to empirically examine the relative importance of specific barriers and facilitators to treatment-seeking. Similarly, given that these results are based on mostly qualitative studies, future studies should seek to understand how themes related to help-seeking and service use among these populations are represented in both qualitative and quantitative data. For example, if themes related to stigma are more commonly captured in qualitative research, then it becomes important to identify the best way to capture these themes in a quantitative capacity as well. Third, studies should aim to capture the unique barriers and facilitators to mental health care for Veterans' and their families in a Canadian context. Relatedly, future studies should attempt to better understand help-seeking behaviours with respect to individual differences and across social identities (e.g., gender, age, sexual orientation, etc.). Finally, families represent a broad group, and future research should consider the barriers and facilitators for different kinds of family members and dynamics (e.g., spouses, children).
Conclusion
This review identified several barriers and facilitators to mental health care for Veterans and Veteran families. While systemic barriers, such as difficulty navigating systems were commonly reported by Veterans and Veteran families, these factors were also identified as facilitators to mental health care when addressed. These findings highlight the heterogeneity in Veterans' and Veteran families' experiences with mental health care-seeking, and the need to understand the effects of barriers on help-seeking behaviours and experiences to implement the appropriate modifications to remove them. In doing so, Veteran health and well-being organizations can provide relevant and accessible mental health care and, subsequently, improve mental health outcomes for Veterans and Veteran families.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
NE: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. JG: Formal Analysis, Investigation, Writing – original draft, Writing – review & editing. KS: Writing – original draft, Writing – review & editing. JL: Conceptualization, Funding acquisition, Methodology, Resources, Visualization, Writing – review & editing. CB: Data curation, Investigation, Writing – original draft, Writing – review & editing. AN: Writing – review & editing. JR: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This work was supported by the Atlas Institute for Veterans and Families.
Acknowledgments
The authors would like to thank the following individuals who contributed to the screening and data extraction stages of this rapid review: Michelle Birch, Vanessa Soares, Ilyana Kocha, Akshitha Ereddy, Rishika Bhogadi, William Younger, and Jieun Jung. We would also like to thank Dominic Gargala for data analytic support.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2024.1426202/full#supplementary-material
References
1. Elnitsky CA, Fisher MP, Blevins CL. Military service member and Veteran reintegration: a conceptual analysis, unified definition, and key domains. Front Psychol. (2017) 8:369. doi: 10.3389/fpsyg.2017.00369
2. VanTil DV, Sweet J, Poirier A, McKinnon K, Pedlar D, Sudom K, et al. Well-being of Canadian Regular Force Veterans, Findings from LASS 2016 Survey. Charlottetown (PE): Veterans Affairs Canada (2017).
3. Statistics Canada. Life After Service Survey. Ottawa, ON: The Daily (2019). Available online at: https://www150.statcan.gc.ca/n1/en/daily-quotidien/200116/dq200116a-eng.pdf?st=d7Fq8R8T. Published 2020
4. Ravindran C, Morley SW, Stephens BM, Stanley IH, Reger MA. Association of suicide risk with transition to civilian life among US military service members. JAMA Netw Open. (2020) 3(9):e2016261. doi: 10.1001/jamanetworkopen.2020.16261
5. Taylor S, Miller BL, Tallapragada M, Vogel M. Veterans’ transition out of the military and knowledge of mental health disorders. Faculty/Researcher Works.
6. St. Cyr K, Liu A, Plouffe RA, Nouri MS, Forchuk CA, Wanklyn SG, et al. Mental health services use among Canadian armed forces members and Veterans: data from the 2018 Canadian armed forces members and Veterans mental health follow-up survey (CAFMVHS). Front Health Serv. (2022) 2:954914. doi: 10.3389/frhs.2022.954914
7. Possemato K, Wray LO, Johnson E, Webster B, Beehler GP. Facilitators and barriers to seeking mental health care among primary care Veterans with posttraumatic stress disorder. J Trauma Stress. (2018) 31(5):742–52. doi: 10.1002/jts.22327
8. Thompson JM, VanTil LD, Zamorski MA, Garber B, Dursun S, Fikretoglu D, et al. Mental health of Canadian armed forces Veterans: review of population studies. J Mil Vet Fam Health. (2016) 2(1):70–86. doi: 10.3138/jmvfh.3258
9. Schwartz KD, Norris D, Cramm H, Tam-Seto L, Mahar A. Family members of Veterans with mental health problems: seeking, finding, and accessing informal and formal supports during the military-to-civilian transition. J Mil Vet Fam Health. (2021) 7(1):21–34. doi: 10.3138/jmvfh-2019-0023
10. Cheney AM, Koenig CJ, Miller CJ, Zamora K, Wright P, Stanley R, et al. Veteran-centered barriers to VA mental healthcare services use. BMC Health Serv Res. (2018) 18(1):591. doi: 10.1186/s12913-018-3346-9
11. Fischer EP, McSweeney JC, Wright P, Cheney A, Curran GM, Henderson K, et al. Overcoming barriers to sustained engagement in mental health care: perspectives of rural Veterans and providers. J Rural Health. (2016) 32(4):429–38. doi: 10.1111/jrh.12203
12. Cornish MA, Thys A, Vogel DL, Wade NG. Post-deployment difficulties and help-seeking barriers among military Veterans: insights and intervention strategies. Prof Psychol: Res Pract. (2014) 45(6):405. doi: 10.1037/a0037986
13. Derefinko KJ, Hallsell TA, Isaacs MB, Colvin LW, Salgado Garcia FI, Bursac Z. Perceived needs of Veterans transitioning from the military to civilian life. J Behav Health Serv Res. (2018) 46:384–98. doi: 10.1007/s11414-018-9633-8
14. Morissette SB, Ryan-Gonzalez C, Yufik T, DeBeer BB, Kimbrel NA, Sorrells AM, et al. The effects of posttraumatic stress disorder symptoms on educational functioning in student Veterans. Psychol Serv. (2021) 18(1):124–33. doi: 10.1037/ser0000356
15. Drapalski AL, Milford J, Goldberg RW, Brown CH, Dixon LB. Perceived barriers to medical care and mental health care among Veterans with serious mental illness. Psychiatr Serv. (2008) 59(8):921–4. doi: 10.1176/ps.2008.59.8.921
16. Maguire AM, Keyser J, Brown K, Kivlahan D, Romaniuk M, Gardner IR, et al. Veteran families with complex needs: a qualitative study of the Veterans’ support system. BMC Health Serv Res. (2022) 22(1):1–15. doi: 10.1186/s12913-021-07368-2
17. Institute of Medicine (US). Returning Home from Iraq and Afghanistan: Assessment of Readjustment Needs of Veterans, Service Members, and Their Families. Washington, DC: National Academies Press (2013).
18. Dodge J, Kale C, Keeling M, Gribble R, Taylor-Beirne S, Maher S, et al. Families transition, too! military families transition out of service: a scoping review of research from the five eyes nations. J Fam Soc Work. (2022) 25(4-5):128–52. doi: 10.1080/10522158.2023.2167896
19. Armour C, Spikol E, McGlinchey E, Gribble R, Fear NT, Murphy D. Identifying psychological outcomes in families of five eyes alliance armed forces Veterans: a systematic review. J Mil Veteran Fam Health. (2022) 8(1):7–27. doi: 10.3138/jmvfh-2021-0025
20. Ellis NR. Comparative Study of Services to Veterans in Other Jurisdictions: Report of the Standing Committee on Veteran Affairs. Ottawa, ON: House of Commons Canada (2017).
21. Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci. (2017) 12:1–18. doi: 10.1186/s13012-016-0533-0
22. Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. (2012) 7:1–17. doi: 10.1186/1748-5908-7-37
23. Amemori M, Michie S, Korhonen T, Murtomaa H, Kinnunen TH. Assessing implementation difficulties in tobacco use prevention and cessation counselling among dental providers. Implement Sci. (2011) 6:1–10. doi: 10.1186/1748-5908-6-1
24. Yamada J, Kouri A, Simard SN, Segovia SA, Gupta S. Barriers and enablers to using a patient-facing electronic questionnaire: a qualitative theoretical domains framework analysis. J Med Internet Res. (2020) 22(10):e19474. doi: 10.2196/19474
25. Hitch C, Toner P, Armour C. Enablers and barriers to military Veterans seeking help for mental health and alcohol difficulties: a systematic review of the quantitative evidence. J Health Serv Res Policy. (2023) 28(3):197–211. doi: 10.1177/13558196221149930
26. Randles R, Finnegan A. Veteran help-seeking behaviour for mental health issues: a systematic review. BMJ Mil Health. (2022) 168(1):99–104. doi: 10.1136/bmjmilitary-2021-001903
27. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions (Version 6.3, updated February 2022). (2022). Available online at: www.training.cochrane.org/handbook
28. Ahmad N, Boutron I, Dechartres A, Durieux P, Ravaud P. Applicability and generalisability of the results of systematic reviews to public health practice and policy: A systematic review. Trials. (2010) 11:1–9.20059766
29. Jørgensen L, Paludan-Müller AS, Laursen DR, Savovic J, Boutron I, Sterne JA, et al. Evaluation of the Cochrane tool for assessing risk of bias in randomized clinical trials: overview of published comments and analysis of user practice in Cochrane and non-Cochrane reviews. Syst Rev. (2016) 5:1–3.27160280
30. Jørgensen AW, Hilden J, Gøtzsche PC. Cochrane reviews compared with industry supported meta-analyses and other meta-analyses of the same drugs: systematic review. BMJ. (2006) 333(7572):782.17028106
31. Moseley AM, Elkins MR, Herbert RD, Maher CG, Sherrington C. Cochrane reviews used more rigorous methods than non-Cochrane reviews: survey of systematic reviews in physiotherapy. J Clin Epidemiol. (2009) 62(10):1021–30.19282144
32. Stevens A, Garritty C, Hersi M, Moher D. Developing PRISMA-RR, a Reporting Guideline for Rapid Reviews of Primary Studies (Protocol). Equator Network (2018).
33. Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. (2017) 6(1):245. doi: 10.1186/s13643-017-0644-y
34. Charrois TL. Systematic reviews: what do you need to know to get started? Can J Hosp Pharm. (2015) 68(2):144. doi: 10.4212/cjhp.v68i2.1440
35. Ewald H, Klerings I, Wagner G, Heise TL, Stratil JM, Lhachimi SK, et al. Searching two or more databases decreased the risk of missing relevant studies: a meta research study. J Clin Epidemiol. (2022) 149:154–64. doi: 10.1016/j.jclinepi.2022.05.022
36. O'Leary DF, Casey M, O'Connor L, Stokes D, Fealy GM, O'Brien D, et al. Using rapid reviews: an example from a study conducted to inform policy-making. J Adv Nurs. (2017) 73(3):742–52.27943377
37. Howard BE, Phillips J, Tandon A, Maharana A, Elmore R, Mav D, et al. SWIFT-active screener: accelerated document screening through active learning and integrated recall estimation. Environ Int. (2020) 138:105623. doi: 10.1016/j.envint.2020.105623
38. Rafferty LA, Wessely S, Stevelink SAM, Greenberg N. The journey to professional mental health support: a qualitative exploration of the barriers and facilitators impacting military Veterans’ engagement with mental health treatment. Eur J Psychotraumatol. (2019) 10(1700613). doi: 10.1080/20008198.2019.1700613
39. Williams L. Women Veterans’ perceptions of mental health outpatient services. [dissertation]. University of California (2015). ProQuest Dissertations Publishing.
40. Harris MPJ, Palmedo PC, Fleary SA. “What gets people in the door”: an integrative model of student Veteran mental health service use and opportunities for communication. J Am Coll Health. (2022):1–11. doi: 10.1080/07448481.2022.2129977
41. Drummelsmith J. Understanding the mental health needs and perceptions of incarcerated Canadian Veterans. [dissertation]. The Chicago School of Professional Psychology (2020). ProQuest Dissertations Publishing. Publication No. 13898583.
42. Garcia HA, Finley EP, Ketchum N, Jakupcak M, Dassori A, Reyes SC. A survey of perceived barriers and attitudes toward mental health care among OEF/OIF Veterans at VA outpatient mental health clinics. Mil Med. (2014) 179(3):273–8. doi: 10.7205/milmed-d-13-00076
43. AlMasarweh L, Ward C. Barriers to health care access and utilization: a study of native American women Veterans in two Montana reservations. Res Sociol Health Care. (2016) 34:33–60. doi: 10.1108/s0275-495920160000034003
44. True G, Rigg KK, Butler A. Understanding barriers to mental health care for recent war Veterans through photovoice. Qual Health Res. (2015) 25(10):1443–55. doi: 10.1177/1049732314562894
45. Campbell GM, Williamson V, Murphy D. “A hidden community”: the experiences of help-seeking and receiving mental health treatment in U.K. women Veterans. A qualitative study. Armed Forces Soc. (2023). doi: 10.1177/0095327(231182140
46. Clary KL, Pena S, Smith DC. Masculinity and stigma among emerging adult military members and Veterans: implications for encouraging help-seeking. Curr Psychol. (2021) 42:4422–38. doi: 10.1007/s12144-021-01768-7
47. Gayles A. Understanding the mental healthcare needs of female Veterans and access to mental health care services within a Veterans health care facility: a phenomenological case study. [dissertation]. Baylor University (2021). ProQuest Dissertations Publishing. Publication No. 28776688.
48. Koenig CJ, Abraham T, Zamora KA, Hill C, Kelly PA, Uddo M, et al. Pre-implementation strategies to adapt and implement a Veteran peer coaching intervention to improve mental health treatment engagement among rural Veterans. J Rural Health. (2016) 32(4):418–28. doi: 10.1111/jrh.12201
49. Koblinsky SA, Schroeder AL, Leslie LA. “Give US respect, support and understanding”: women Veterans of Iraq and Afghanistan recommend strategies for improving their mental health care. Soc Work Ment Health. (2017) 15(2):121–42. doi: 10.1080/15332985.2016.1186134
50. Rosado JC. Interventions to reduce perceived stigma for mental health treatment in a Veteran population: do peer contact, psychoeducation, and empathy make a difference? [dissertation]. Fielding Graduate University (2017). ProQuest Dissertations Publishing. Publication No. 10607939.
51. Kimerling R, Pavao J, Greene L, Karpenko J, Rodriguez A, Saweikis M, et al. Access to mental health care among women Veterans. Med Care. (2015) 53:S97–104. doi: 10.1097/mlr.0000000000000272
52. Shepherd-Banigan M, Shapiro A, Sheahan KL, Ackland PE, Meis LA, Thompson-Hollands J, et al. Mental health therapy for Veterans with PTSD as a family affair: a qualitative inquiry into how family support and social norms influence Veteran engagement in care. Psychol Serv. (2023) 20(4):839–48. doi: 10.1037/ser0000742
53. Beks TA, Cairns SL. Factors that influence mental health service use among female partners of posttraumatic stress disorder-affected Veterans. Traumatology. (2020). doi: 10.1037/trm0000240
54. Bovin MJ, Miller CJ, Koenig CJ, Lipschitz JM, Zamora KA, Wright PB, et al. Veterans’ experiences initiating VA-based mental health care. Psychol Serv. (2019) 16(4):612–20. doi: 10.1037/ser0000233
55. Mellotte H, Murphy D, Rafferty L, Greenberg N. Pathways into mental health care for UK Veterans: a qualitative study. Eur J Psychotraumatol. (2017) 8:1389207. doi: 10.1080/20008198.2017.1389207
56. Skellon N. Factors that impact on military personnel and military Veterans accessing mental health services. [dissertation]. The University of Liverpool (United Kingdom) (2016). ProQuest Dissertations Publishing. Publication No. 28782520.
57. Doughty Shaine MJ, Cor DN, Campbell AJ, McAlister AL. Mental health care experiences of trans service members and Veterans: a mixed-methods study. J Couns Dev. (2021) 99(3):273–88. doi: 10.1002/jcad.12374
58. Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. (2018) 34(4):285–91. doi: 10.3233/EFI-180221
59. Government of Canada. Military families’ Access to Health Care. (2023). Available online at: www.canada.ca, https://www.canada.ca/en/ombudsman-national-defence-forces/education-information/military-families/access-health-care.html (Accessed April 23, 2024).
60. Ramalingam NS, Barnes C, Patzel M, Kenzie ES, Ono SS, Davis MM. “It’s like finding your way through the labyrinth”: a qualitative study of Veterans’ experiences accessing healthcare. J Gen Intern Med. (2023):1–7.37904070
61. Tam-Seto L, Williams A, Cramm H. Exploring Veteran cultural competency in Canadian health care services. J Mil Vet Fam Health. (2023) 9(4):100–10. doi: 10.3138/jmvfh-2022-0073
62. Turchik JA, Bucossi MM, Kimerling R. Perceived barriers to care and gender preferences among Veteran women who experienced military sexual trauma: a qualitative analysis. Mil Behav Health. (2014) 2(2):180–8. doi: 10.1080/21635781.2014.892410
63. Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. (2004) 19(2):69–79. doi: 10.1093/heapol/czh009
64. Meyer EG, Writer BW, Brim W. The importance of military cultural competence. Curr Psychiatry Rep. (2016) 18:26. doi: 10.1007/s11920-016-0662-9
65. Vogt D. Mental health-related beliefs as a barrier to service use for military personnel and Veterans: a review. Psychiatr Serv. (2011) 62(2):135–42. doi: 10.1176/ps.62.2.pss6202_0135
66. Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. “Mental health literacy”: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust. (1997) 166(4):182–6. doi: 10.5694/j.1326-5377.1997.tb140071.x
67. Williston SK, Bramande EA, Vogt DS, Iverson KM, Fox AB. An examination of the roles of mental health literacy, treatment-seeking stigma, and perceived need for care in female Veterans’ service use. Psychiatr Serv. (2020) 71(2):144–50. doi: 10.1176/appi.ps.20180040
68. Williston SK, Vogt DS. Mental health literacy in Veterans: what do U.S. Military Veterans know about PTSD and its treatment? Psychol Serv. (2022) 19(2):327–34. doi: 10.1037/ser0000501
69. Gorman LA, Blow AJ, Ames BD, Reed PL. National guard families after combat: mental health, use of mental health services, and perceived treatment barriers. Psychiatr Serv. (2011) 62(1):28–34. doi: 10.1176/ps.62.1.pss6201_0028
70. Schvey NA, Burke D, Pearlman AT, Britt TW, Riggs DS, Carballo C, et al. Perceived barriers to mental healthcare among spouses of military service members. Psychol Serv. (2022) 19(2):396. doi: 10.1037/ser0000523
71. Murphy D, Busuttil W. Exploring outcome predictors in UK Veterans treated for PTSD. Psychol Res. (2015) 5(8):441–51. doi: 10.17265/2159-5542/2015.08.001
72. Gould M, Adler A, Zamorski M, Castro C, Hanily N, Steele N, et al. Do stigma and other perceived barriers to mental health care differ across armed forces? J R Soc Med. (2010) 103(4):148–56. doi: 10.1258/jrsm.2010.090426
73. Clary KL, Pena S, Smith DC. Masculinity and stigma among emerging adult military members and Veterans: implications for encouraging help-seeking. Curr Psychol. (2023) 42(6):4422–38. doi: 10.1007/s12144-021-01768-7
74. Godier-McBard LR, Gillin N, Fossey MJ. “Treat everyone like they're a man”: stakeholder perspectives on the provision of health and social care support for female Veterans in the UK. Health Soc Care Community. (2022) 30(6):e3966–76. doi: 10.1111/hsc.13790
Keywords: mental health services, Veterans, Veteran families, wellbeing, mental health
Citation: Ein N, Gervasio J, St. Cyr K, Liu JJW, Baker C, Nazarov A and Richardson JD (2024) A rapid review of the barriers and facilitators of mental health service access among Veterans and their families. Front. Health Serv. 4: 1426202. doi: 10.3389/frhs.2024.1426202
Received: 30 April 2024; Accepted: 25 June 2024;
Published: 22 July 2024.
Edited by:
Warren Ponder, One Tribe Foundation, United StatesReviewed by:
Richard Adams, Kent State University, United StatesCraig Rosen, National Center for PTSD, VA Palo Alto Healthcare System, United States
© 2024 Ein, Gervasio, St. Cyr, Liu, Baker, Nazarov and Richardson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Natalie Ein, bmF0YWxpZS5laW5Ac2poYy5sb25kb24ub24uY2E=
 Natalie Ein
Natalie Ein Julia Gervasio1,3
Julia Gervasio1,3 Kate St. Cyr
Kate St. Cyr Anthony Nazarov
Anthony Nazarov J. Don Richardson
J. Don Richardson