- 1Department of Psychiatry and Behavioral Sciences and Center for Dissemination and Implementation Science, Northwestern University Feinberg School of Medicine, Chicago, IL, United States
- 2Institute of Behavioral Science, Feinstein Institutes for Medical Research, Northwell Health, Manhasset, NY, United States
- 3Departments of Psychiatry and of Molecular Medicine, The Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY, United States
- 4Northwestern University Feinberg School of Medicine, Chicago, IL, United States
- 5Center for Health Information Partnerships, Northwestern University Feinberg School of Medicine, Chicago, IL, United States
- 6Department of Medicine and Center for Health Information Partnerships, Northwestern University Feinberg School of Medicine, Chicago, IL, United States
Introduction: Long-acting injectable (LAI) antipsychotic medications and clozapine are effective yet underutilized medical therapies in early intervention services. The purpose of this study was to conduct a pre-implementation evaluation of contextual determinants of early intervention programs to implement innovations optimizing LAI antipsychotic and clozapine use within a shared decision-making model.
Methods: Semi-structured interviews explored barriers and facilitators to implementing LAI antipsychotics and clozapine in early intervention services. Participants were: prescribers (n = 2), non-prescribing clinicians (n = 5), administrators (n = 3), clients (n = 3), and caregivers (n = 3). Interviews were structured and analyzed using the Consolidated Framework for Implementation Research (CFIR 2.0).
Results: Participants were supportive of using LAI antipsychotics, despite barriers (e.g., transportation, insurance coverage), while most were unfamiliar with clozapine (Innovation). Critical incidents (e.g., COVID-19) did not interfere with implementation, while barriers included lack of performance measures; stigma affecting willingness to take medication; and clozapine considered to be a “last resort” (Outer Setting). Treatment culture was described as client-centered and collaborative, and most participants indicated LAI antipsychotic use was compatible with clinic workflows, but some were in need of resources (e.g., individuals trained to administer LAI antipsychotics; Inner Setting). Participants on the healthcare team expressed confidence in their roles. Family education and collaborative decision-making were recommended to improve client/family engagement (Individuals). Participants related the importance of tracking medication compliance, addressing client concerns, and providing prescribers with updated guidelines on evidence-based treatment (Implementation Process).
Discussion: Results may guide implementation strategy selection for future programs seeking to optimize the use of LAI antipsychotics and clozapine for early-phase schizophrenia, when appropriate.
1 Introduction
Early intervention services (i.e., coordinated specialty care; CSC) for early-phase schizophrenia (i.e., within the first 5 years after first episode) improves positive and negative psychosis symptoms, increases treatment engagement, decreases the likelihood of psychiatric hospitalization, increases involvement in meaningful activities, and improves overall symptom severity (1, 2). A key component of early intervention programs includes selecting the psychopharmacological interventions that are tailored to the needs of each patient. Unfortunately, patients in the early stages of illness are often reluctant to take medication or take it sporadically. As a result, relapse and rehospitalization rates are quite high. Early relapses can be particularly impactful and efforts should be made to reduce risk (3).
Long-acting injectable (LAI) forms of antipsychotic medications have the same ingredients as a daily oral pill, but they are slowly released in the body over time (typically 3–6 months). Several widely used antipsychotics are available in LAI formulations, including risperidone, paliperidone, aripiprazole and olanzapine. LAI formulations are typically indicated to enhance adherence, reduce the risk of relapse, and/or ensure patients who appear to be unresponsive are receiving the medication (3). Use of LAI, compared to oral, antipsychotics is associated with greater medication adherence and reduced rates of psychiatric hospitalization (4–6). Clinical trials that emphasized staff training and patient education found nearly 90% acceptance rates of LAI antipsychotics by patients (7) yet prescription of LAI antipsychotics in real-world settings remain low (9%–15%) (8, 9).
For patients with treatment-resistant schizophrenia (i.e., patients who show lack of response to treatment with two antipsychotic medications in either oral or LAI formulation), clozapine is the only medication that has demonstrated efficacy and has regulatory approval (3, 10)—including for those with first-episode or early-phase schizophrenia (11, 12). However, clozapine is also underutilized, especially for early-phase schizophrenia (13–15).
A number of prior investigations have sought to understand how the knowledge, beliefs, attitudes, and experiences of patients, family members, and healthcare providers contribute to underutilization of these medications (14, 16–21). For example, behavioral health providers under-estimate the level of acceptance of LAI antipsychotics among their patients, anticipating that their patients will have negative attitudes, lack of education, and issues with access (e.g., transportation) (16). Regarding clozapine, many psychiatrists are reluctant to prescribe clozapine, and believe that their patients who are treated with clozapine are less satisfied with their treatment than patients treated with other antipsychotics (20, 21).
Considerably less attention has been paid to the non-individual-level barriers to implementing these effective medications in clinical practice. One systematic review of barriers to LAI antipsychotic use identified poor coverage by insurance plans; administrative costs associated with the medication itself, storage, and training; and lack of infrastructure to administer LAI antipsychotic injections outside of a usual setting (e.g., while on vacation, in primary care clinics). Administrative and structural barriers to clozapine use include the burden of blood monitoring (for both patients and clinicians), limited resources in the healthcare system (e.g., trained staff, transportation services), and lack of infrastructure for monitoring clozapine use in community settings (22).
Limitations of prior studies include lack of structured theories or frameworks to guide the work and a shortage of integration of multilevel perspectives. The use of appropriate frameworks significantly improves the efficiency and effectiveness of implementation of evidence-based practices (23). Frameworks put forth specific constructs to guide the implementation plan, assist in the interpretation of results, and provide a shared language between researchers, practitioners, and those with lived experience. The Consolidated Framework for Implementation Research (CFIR), and the updated CFIR 2.0 (24), is a widely used determinants framework that is used to identify and explain how barriers and facilitators of the context may affect implementation of an evidence-based practice (24, 25). This information can then be used to select strategies to overcome barriers and leverage facilitators for successful implementation.
The purpose of this study was to conduct a pre-implementation evaluation of the contextual determinants of LAI antipsychotics and clozapine use in early intervention programs. We used the CFIR 2.0 (24) to elucidate barriers and facilitators to implementing an algorithm to support shared decision-making around prescribing of LAI antipsychotics and clozapine, from the perspective of individuals representing multiple levels of implementation. These results will guide implementation strategy selection for future studies and programs seeking to optimize the presentation of LAI antipsychotics and clozapine for early-phase schizophrenia in a shared decision-making approach to implement these medications, when appropriate.
2 Materials and methods
2.1 Study overview
This study was based in the Early Psychosis Intervention Network (EPINET), which includes 8 regional “hubs” and over 100 clinics providing CSC to early-phase schizophrenia patients across 17 states. EPINET is a national learning health system that seeks to improve early psychosis care by conducting large-scale, practice-based research. This study was conducted to identify implementation determinants (barriers and facilitators) and strategies to implementing an algorithm and training to increase the reach and adoption of appropriate LAI antipsychotics and clozapine use for early-phase schizophrenia. Initial interviews were conducted in March-May 2023 and analysis was conducted from May-June 2023. We then added client interviews, conducted in September 2023 and analyzed in October 2023. All procedures were approved by Northwestern University's Institutional Review Board.
2.2 Participants and recruitment
We recruited five groups of constituents associated with early psychosis clinics: (1) Prescribing healthcare professionals (Prescribers), including psychiatrists, family medicine physicians, advanced nurse practitioners, family nurse practitioners; (2) Non-prescribing healthcare professionals (Non-prescribing clinicians), including mental health therapists, clinical social workers, and occupational therapists; (3) Organizational leaders and administrative staff (Administrators), including executive leadership, principal investigators, and program directors; (4) Individuals diagnosed with early-phase schizophrenia who received or were offered an LAI antipsychotic and/or clozapine (Clients); and (5) Relatives or partners of Clients (Caregivers). We aimed to recruit at least 2 and up to 5 participants per constituent group to ensure variability and reach saturation, which has been shown to be achieved with 9–17 interviews (26). Due to difficulty recruiting clients from EPINET clinics, we expanded recruitment efforts to include clients and caregivers from the Recovery from Early Psychosis Program (REPP) at Northwestern Medicine.
Study team members circulated a study announcement and flyer via email to EPINET hubs and the REPP clinic. A member of the research team joined clinic team meetings to provide study information and answer questions. Interested individuals then self-referred to the study. Participants provided verbal informed consent prior to initiating study activities and were given a $50 giftcard for participating. Our final sample included 2 prescribers, 5 non-prescribing clinicians, 3 administrators, 3 caregivers, and 3 clients who were recruited from sites in Michigan (3), Oregon (2), Oklahoma (2), Florida (5), and Illinois (4). No further demographics were collected to preserve the anonymity of participants.
2.3 Interviews
Interview guides were constructed using the CFIR 2.0 (24); the interview guides are available as Supplementary Material. Two to six questions were selected for each of the five CFIR domains (Innovation, Outer Setting, Inner Setting, Individuals, and Implementation Process), focusing on constructs that members of the research team (two implementation scientists and two psychiatrists/schizophrenia researchers) identified as the most representative of the barriers frequently seen in the treatment of schizophrenia (Table 1). Each interview guide was tailored for the constituent role and comprised 12–16 questions. Interviews were conducted using the Zoom videoconferencing platform, lasted approximately 45 min, and were audio/video recorded for analysis.
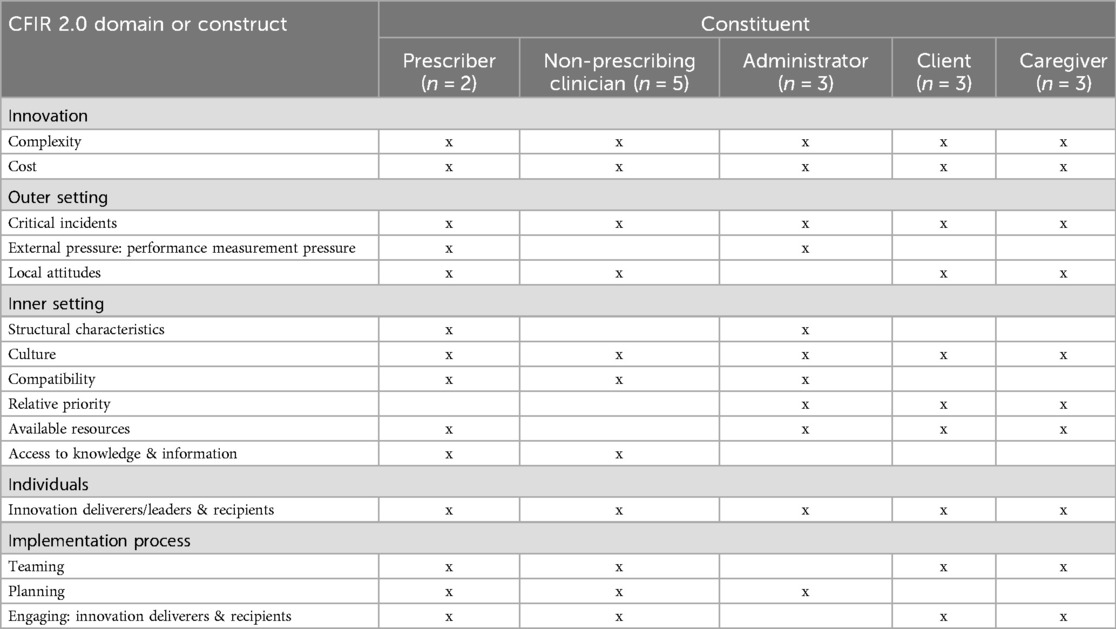
Table 1. Consolidated framework for Implementation Research (CFIR), version 2, domains and constructs asked of the included constituents.
2.4 Data analysis
Analysis of the interview data was performed using Rapid Turnaround Qualitative Analysis (27, 28). One extensively trained primary coder (AJC) conducted content analysis coding from the Zoom transcripts, which had been corrected and confirmed from the video recordings. A structured summary template was developed based on CFIR 2.0 (24). The results were then reviewed and confirmed with another member of the research team (AK) who had watched all of the interview recordings.
3 Results
The results are organized by the CFIR 2.0 domains and constructs. Due to a lack of familiarity with clozapine among many of the participants, most barriers and facilitators described herein relate primarily to LAI antipsychotics. Where applicable, disagreement between constituent groups is noted. See Table 2 for a summary and exemplar quotes.
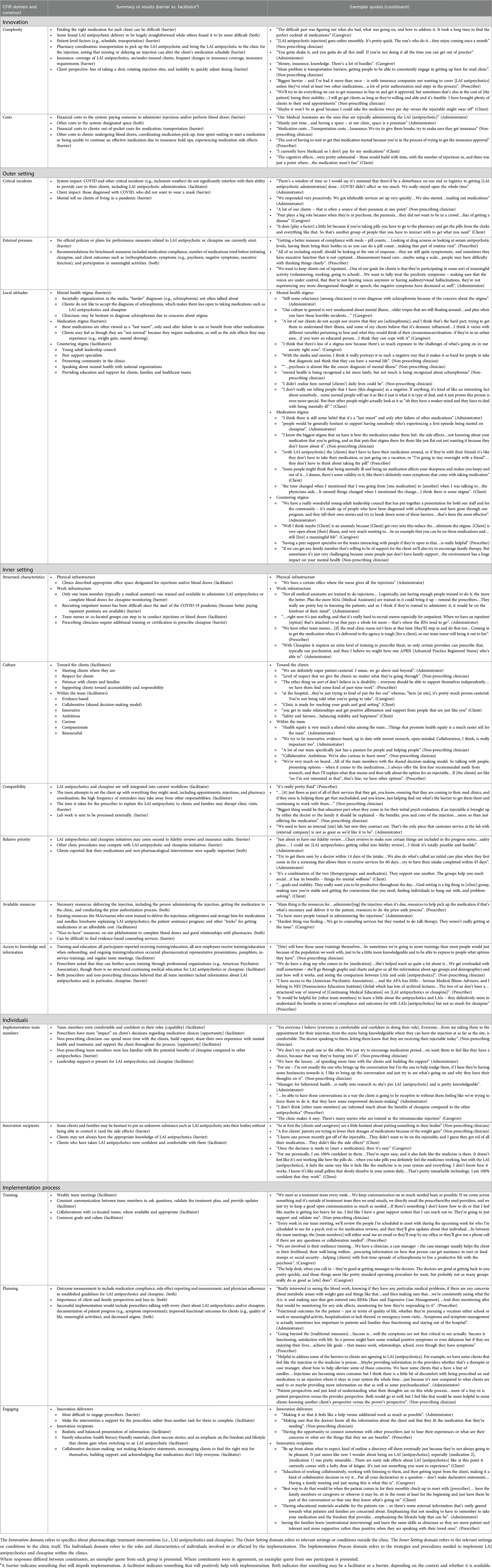
Table 2. Summary of qualitative results by consolidated framework for implementation research (CFIR), version 2, domain and construct.
3.1 General perceptions
All participants were supportive of using LAI antipsychotics; prescribers spoke to the literature recommending second-generation LAI antipsychotics as first-line treatment. Some participants noted that the LAI antipsychotics were underutilized. LAI antipsychotics (compared to oral medications) reportedly removed clients' daily reminder of illness and a potential method for suicide, however, clients expressed initial concerns about putting something foreign in their body. The importance of having the family involved and on-board with medication decisions was emphasized. Several participants described clozapine as a “last resort” largely due to side effects. Several participants described participating in prior research studies which increased use of these medications, but this effect atrophied after study completion.
3.2 Innovation
The Innovation domain refers to specifics about the pharmacologic treatment interventions (i.e., LAI antipsychotics and clozapine).
3.2.1 Complexity
LAI antipsychotics and the day-to-day procedures (e.g., try an oral form first, ensure team member availability for injection) were viewed as relatively straightforward. The complexity of LAI antipsychotics lays in the coordination between the pharmacy and the clinic to obtain the medication and with insurance companies. Insurance coverage of these medications (especially LAI antipsychotics) varies widely; clients' insurance coverage changes; or complex insurance requirements (e.g., using a medical pharmacy). A prescriber stated, “Biggest barrier – and I’ve had it more than once – is with insurance companies not wanting to cover [LAI antipsychotics] unless they’ve tried at least two other medications…a lot of prior authorization and steps in the process”. Participants reported that the programs strive to manage these complexities where possible (e.g., procedures and personnel dedicated to prior authorizations, providing transportation), but high barriers to access persist (e.g., repeating paperwork).
3.2.2 Cost
Financial costs to the system included employing trained personnel to deliver injections and/or perform blood draws—though, it was also noted that having a nurse or other team member in that role saved the prescribing clinician time. Additionally, injections and blood draws require designated clinic space. To clients, the financial costs included the medications itself (if un/der covered by insurance) and transportation. Non-financial costs to clients included time (e.g., coordinating with pharmacy, attending the clinic, waiting for insurance) and the physical consequences (e.g., pain of injections, blood draws, side effects). One client described their experience as, “The cognitive effects…were pretty substantial – these would build with time, with the number of injections in, and there was just a point where…the medication wasn't fun”.
3.3 Outer setting
The Outer Setting domain refers to relevant settings or conditions outside the clinic.
3.3.1 Critical incidents
Largely, COVID and other critical incidents (e.g., inclement weather) do not significantly interfere with a program's ability to provide care to their clients, including LAI antipsychotic administration. COVID did impact clients individually where they could not visit the clinic if they were diagnosed with COVID or did not want to wear a mask when receiving services, as well as the mental toll of living in a pandemic.
3.3.2 External pressure: performance measurement pressure
Per the administrators and prescribing clinicians, no official policies or plans for performance measures related to LAI antipsychotic or clozapine use currently exist. Rather, they recommended relevant benchmark measures [e.g., medication compliance, (re)hospitalization, and participation in meaningful activities]: “We want to keep clients out of inpatient…One of our goals for clients is that they’re participating in some sort of meaningful activity (volunteering, working, going to school)” (Administrator).
3.3.3 Local attitudes
Clients described experiencing stigma associated with schizophrenia, the medications, and the side effects of the medications (e.g., weight gain, mental slowing), such as: “the tone changed when I mentioned that I was going from [one medication] to [another] when I was talking to…the physicians aide…I think there is some stigma”. Healthcare participants described the negative impact of stigma on the mental health and wellbeing of clients, resulting in clients having greater difficulty accepting a diagnosis of psychosis. Some also described a hesitance on the part of clinicians to diagnosis schizophrenia due to concerns about stigmatization. Regarding the medications themselves, healthcare participants described these medications (especially clozapine) as a “last resort”. In contrast, they noted LAI antipsychotics may reduce stigma by removing the daily reminder (when taking a pill) of mental health problems. Participants also described examples of countering stigma, such as asking clients to share their stories and by employing peer support specialists. As a prescriber noted, “having a peer support specialist on the teams interacting with people if they’re open to that…is really helpful”.
3.4 Inner setting
The Inner Setting domain refers to the relevant settings or conditions in the clinic itself.
3.4.1 Structural characteristics
Per administrators and prescribing clinicians, physical infrastructure factors were not barriers to LAI antipsychotics or clozapine administration. The primary work infrastructure barrier was limited availability of trained personnel to administer LAI antipsychotics, complete blood draws for clozapine monitoring, and prescribe clozapine. One participant noted difficulty hiring outpatient nurses with appropriate skills. However, several participants described how team nurses or co-located groups provided assistance when needed: “We have other team nurses…[if] the med clinic nurse isn't here at that time, [they’ll] step in and do that too” (Prescriber).
3.4.2 Culture
Several participants spontaneously described their teams as “patient-centered” with some specific examples including respect for clients while also guiding clients toward accountability and responsibility. Within their teams, participants described their culture with words such as collaborative (consistent with a shared-decision making model), compassionate, and resourceful.
3.4.3 Compatibility
Most participants (administrators, non-prescribing clinicians, prescribing clinicians) expressed that LAI antipsychotic and clozapine use were already well integrated with the clinic workflows: “it's really pretty fluid” (Prescriber). The team assists clients with everything needed to facilitate LAI antipsychotic injections, including scheduling appointments, performing injections, and coordinating with pharmacies. Some barriers to compatibility included the time for prescribers to explain LAI antipsychotics to clients/families, sending frequent reminders for clients and their families, and sending lab work to be processed externally. As an administrator described, “We used to have an internal [site] lab, but now they contract out. That's the only piece that customer service at the lab with [external company] is not as great as we’d like it to be”.
3.4.4 Relative priority
Administrators identified some potential competing initiatives in the clinics. For example, they identified regular fidelity reviews and insurance audits that occur a few times per year. They also described regular clinic procedures that may be prioritized, such as seeing the client within 14 days of intake or smoothly transitioning clients from hospitalization to outpatient. Clients reported that the program and clinicians focused equally on medications and non-pharmacological interventions (e.g., therapy, making connections, setting goals): “It's a combination of the two [therapy/groups and medication]. They support one another. The groups help you reach social…it has its benefits – things for mental wellness” (Client).
3.4.5 Available resources
Existing resources that facilitated LAI antipsychotics and clozapine use included the MAs/nurses who were trained to deliver injections and complete blood draws; refrigerators and storage bins for medications and needles; brochures explaining LAI antipsychotics; patient assistance program; and “tricks” for getting medications at affordable cost. A prescriber stated, “Main thing is the resources for…administer[ing] the injection when it's due, resources to help pick up the medication if that's what's necessary and deliver it to the patient, resources to do the prior auth process”. One caregiver noted it was difficult to find evidence-based screening and counseling services to receive an accurate diagnosis and effective, holistic treatment.
3.4.6 Access to knowledge and information
All healthcare participants reported baseline and ongoing training and education about pharmacologic treatment interventions. Many described receiving updated data and research results about LAI antipsychotics via pamphlets, in-service trainings, and team meetings. Prescribers noted they have access to training for both LAI antipsychotics and clozapine through professional organizations (e.g., American Psychiatric Association). Participants indicated that team members would benefit from further education: “It would be helpful for [other team members] to learn a little about the antipsychotics and LAIs–they definitively seem to understand the benefits in terms of compliance and outcomes for with LAIs [antipsychotics] but not so much for clozapine” (Prescriber).
3.5 Individuals
The Individuals domain refers to the roles and characteristics of individuals involved in or affected by the implementation.
3.5.1 Implementation team members
Participants agreed that healthcare team members are comfortable and confident in their roles and have positive views of LAI antipsychotics. For example, prescribers have more influence on a client's decision about medication, while non-prescribing clinicians build rapport with clients via time spent and shared experiences. Several participants indicated that they respect their clients' autonomy, such as a non-prescribing clinician who said, “We don't try to push one or the other. We just try to encourage medication period…we want them to feel like they have a choice, because that way they're buying into it”. Non-prescribing team members were less familiar with the potential benefits of clozapine. Prescribers suggested further training and education would increase non-prescribers' capability and motivation to recommend and support clients on clozapine. Finally, participants indicated they had strong leadership support for LAI antipsychotics and clozapine, as well as new research to developed further evidence for their use.
3.5.2 Innovation recipients
Non-client participants described hesitation among clients and their families about putting [medication] into their bodies, especially in the injectable form. Others noted that, oftentimes, clients were not aware of LAI antipsychotics as an option. Another consideration was that clients and their families occasionally try to use lower doses of medications due to side effects (e.g., weight gain), which is more difficult with an LAI antipsychotic compared to a daily pill. In contrast, caregivers and clients were agreeable to LAI antipsychotics: “I am 100% confident in them…They’re super easy, and it also feels like the medicine is there. It doesn't feel like it's not working like how the pills do…” (Client).
3.6 Implementation process
The Implementation process domain refers to the strategies and procedures needed to implement LAI antipsychotics and clozapine within the clinics.
3.6.1 Teaming
Nearly all healthcare participants mentioned weekly team meetings as collaborative and helpful for team members to align expectations and present a united front to clients. They also noted that team members are in regular communication outside of team meetings, as needed. A non-prescribing clinician stated: “If there's something I don't know how to do or that I feel like maybe is getting too heavy for me, I feel like I have a great support system that I can reach out to. They’re going to just support and validate me”. One team noted they collaborate with the co-located integrated primary care team to share resources. Participants described common goals among members within their teams. Caregivers also described good collaboration with the healthcare team: “We are involved in their resilience training…We have a clinician, a case manager [who] helps the client in their livelihood…procuring information on how that person can get assistance in rent or food stamps or social security…helping [clients] with first-time episode of schizophrenia to live a productive life with the psychosis”.
3.6.2 Planning
Relevant outcomes of LAI antipsychotic and clozapine use among participants included medication compliance, prescribers’ adherence to guidelines, and medication side effects. Successful implementation would be demonstrated by prescribers talking with every client about LAI antipsychotics/clozapine; documentation of client progress (e.g., symptom improvement); wellbeing outcomes for clients (e.g., quality of life, meaningful activities); and stigma. One administrator noted the importance of “Functional outcomes for the patient – just in terms of quality of life, whether they’re pursuing a vocation either school or work or meaningful activity, hospitalization or lack thereof, or emergency room visits…Symptoms and symptom management is actually sometimes less important to patients and families than functioning and staying out of the hospital”. It was noted that tracking these outcomes can increase use of LAI antipsychotics and clozapine. Many participants also described the importance of gathering client and family perspectives about LAI antipsychotics and clozapine to gauge their understanding, concerns, and buy-in.
3.6.3 Engaging
To engage innovation deliverers, participants noted that it can be difficult to get prescribers on-board because they are overbooked and do not spend as much time with clients. Thus, any intervention implemented would need to support prescribers rather than adding to their workload: “Making it so that it feels like a help vs. additional work as much as possible” (Administrator; e.g., proactively providing the necessary information for prescribing). Recommendations to engage innovation recipients included family education (e.g., client success stories), collaborative decision-making (e.g., presenting a balanced perspective), and applying evidence-based counseling approaches (e.g., motivational interviewing, cognitive behavioral therapy). As stated by a client, “Be up front about what to expect, kind of outline a directory off them eventually just because they’re not always going to be pleasant.”
5 Discussion
The purpose of this study was to evaluate the contextual determinants of implementing an algorithm to optimize appropriate use of LAI antipsychotics and clozapine within a CSC program for early-phase schizophrenia. Results from these interviews with multilevel constituents will form the basis of a matrix used to select the most relevant implementation strategies to address the prevalent barriers and leverage the key facilitators in the implementation of LAI antipsychotics and clozapine.
The identified strengths of CSC programs that support the use of LAI antipsychotics and clozapine may be leveraged by these and other programs. First, nearly all participants described a collaborative culture with common goals and respect for client autonomy. Second, several participants confirmed high compatibility of medication procedures with current workflows. Third, healthcare team members, clients, and caregivers described healthy communication and engagement between all constituent groups.
Barriers reported across participants included the costs of these medications (financial and other), lack of external pressure (e.g., benchmarks) to encourage use and mark fidelity, and pervasive stigma about psychosis and treatment. Administrators, providers, and clients/caregivers alike described competing demands that kept them from prioritizing medications. Participants noted limited knowledge among non-prescribing clinicians, staff, and clients/families about LAI antipsychotics and clozapine, which is a known barrier to use of these medications (29, 30). Interestingly, several healthcare team participants overestimated the frequency of LAI antipsychotic and clozapine use. The predominant belief that everyone in the clinic supports the use of LAI antipsychotic use is at odds with the data that LAI antipsychotics are under-prescribed (8, 9). In fact, one administrator noted that a review of program data found they were not prescribing LAI antipsychotics as much as they thought. Additionally, most of the non-prescribing participants viewed clozapine as a “last resort”, despite research indicating that the majority of clients and their caregivers are more satisfied, stable, and adherent after clozapine is initiated (18, 19).
Several evidence-based implementation strategies may be employed to address these barriers. First, it is clear that appropriate training and education of healthcare teams, clients, and caregivers is needed. For example, virtual training holds great promise for cost-effective, scalable, and effective training for working with individuals with severe mental illness (31–33). Second, audit and feedback strategies, in which a systematic review of prescribing behaviors may be shared back to clinicians, may inform healthcare providers about their actual use (and missed opportunities) of LAI antipsychotics and clozapine and encourage greater adherence to guideline recommendations (34, 35). Finally, practice facilitation is a multi-level strategy designed to increase the uptake of effective clinical innovations and build organizational capacity through activities such as training and education, workflow review, practice reports and discussion, and developing tailored program materials (36, 37). Practice facilitation has been shown to be effective across healthcare settings to manage a range of clinical conditions (38, 39).
These results should be considered within the context of their limitations. First, we did not collect demographic information about our participants to preserve their anonymity. Second, the EPINET and REPP clinics represent a particular type of clinic. Thus, the identified determinants and proposed strategies may not be applicable to more general mental health clinics. Moreover, the selection of clinics was not random and may not be representative. Nonetheless, using the framework of the five CFIR 2.0 domains across multiple clinics likely allowed us to identify broader patterns that influence treatment of early-phase schizophrenia in similar settings.
This study identified determinants of implementing LAI antipsychotics and clozapine to treat early-phase schizophrenia in early intervention services clinics. These results expand prior work examining individual perspectives and opinions about these treatments to identify outer and inner setting confounders, as well as potential strategies to leverage facilitators and overcome barriers to optimize appropriate use of these evidence-based treatments.
Data availability statement
The datasets presented in this article are not readily available because we wish to protect the privacy and confidentiality of our participants given the sensitive and personal nature of the contents of the qualitative data. Requests to access the datasets should be directed to Dr. Allison Carroll,YWxsaXNvbi5jYXJyb2xsQG5vcnRod2VzdGVybi5lZHU=.
Ethics statement
The studies involving humans were approved by Northwestern University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AJC: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. DGR: Conceptualization, Resources, Writing – review & editing. JMK: Conceptualization, Resources, Writing – review & editing. AK: Data curation, Investigation, Writing – review & editing. JB: Writing – review & editing. TLW: Writing – review & editing. CHB: Conceptualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
Previous Presentation: Partial results from this paper were presented at the annual meeting for the American Psychiatric Association in May, 2024. Site/staff recruitment used sites from the ESPRITO project (the National Institute of Mental Health (NIMH), Bethesda, MD R01MH120594; PIs: Delbert Robinson, John Kane).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2024.1385398/full#supplementary-material
References
1. Correll CU, Galling B, Pawar A, Krivko A, Bonetto C, Ruggeri M, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry. (2018) 75(6):555–65. doi: 10.1001/jamapsychiatry.2018.0623
2. Nordentoft M, Rasmussen JØ, Melau M, Hjorthøj CR, Thorup AAE. How successful are first episode programs? A review of the evidence for specialized assertive early intervention. Curr Opin Psychiatry. (2014) 27(3):167–72. doi: 10.1097/YCO.0000000000000052
3. Keepers GA, Fochtmann LJ, Anzia JM, Benjamin S, Lyness JM, Mojtabai R, et al. The American psychiatric association practice guideline for the treatment of patients with Schizophrenia. Am J Psychiatry. (2020) 177(9):868–72. doi: 10.1176/appi.ajp.2020.177901
4. Kane JM, Schooler NR, Marcy P, Correll CU, Achtyes ED, Gibbons RD, et al. Effect of long-acting injectable antipsychotics vs usual care on time to first hospitalization in early-phase schizophrenia: a randomized clinical trial. JAMA Psychiatry. (2020) 77(12):1217–24. doi: 10.1001/jamapsychiatry.2020.2076
5. Kirson NY, Weiden PJ, Yermakov S, Huang W, Samuelson T, Offord SJ, et al. Efficacy and effectiveness of depot versus oral antipsychotics in schizophrenia: synthesizing results across different research designs. J Clin Psychiatry. (2013) 74(6):568–75. doi: 10.4088/JCP.12r08167
6. Lin D, Thompson-Leduc P, Ghelerter I, Nguyen H, Lafeuille M-H, Benson C, et al. Real-world evidence of the clinical and economic impact of long-acting injectable versus oral antipsychotics among patients with schizophrenia in the United States: a systematic review and meta-analysis. CNS Drugs. (2021) 35(5):469–81. doi: 10.1007/s40263-021-00815-y
7. Kane JM, Schooler NR, Marcy P, Achtyes ED, Correll CU, Robinson DG. Patients with early-phase schizophrenia will accept treatment with sustained-release medication (long-acting injectable antipsychotics): results from the recruitment phase of the PRELAPSE trial. J Clin Psychiatry. (2019) 80(3):18m12546. doi: 10.4088/JCP.18m12546
8. Bernardo M, San L, Olivares JM, Dilla T, Polavieja P, Gilaberte I, et al. Treatment patterns and health care resource utilization in a 1-year observational cohort study of outpatients with schizophrenia at risk of nonadherence treated with long-acting injectable antipsychotics. Patient Prefer Adherence. (2011) 5:601–10. doi: 10.2147/PPA.S26253
9. Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. (2015) 21(9):754–68. doi: 10.18553/jmcp.2015.21.9.754
10. Howes OD, McCutcheon R, Agid O, de Bartolomeis A, van Beveren NJ, Birnbaum ML, et al. Treatment-resistant schizophrenia: treatment response and resistance in psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am J Psychiatry. (2017) 174(3):216–29. doi: 10.1176/appi.ajp.2016.16050503
11. Thien K, Bowtell M, Eaton S, Bardell-Williams M, Downey L, Ratheesh A, et al. Clozapine use in early psychosis. Schizophr Res. (2018) 199:374–9. doi: 10.1016/j.schres.2018.02.054
12. Williams R, Malla A, Roy MA, Joober R, Manchanda R, Tibbo P, et al. What is the place of clozapine in the treatment of early psychosis in Canada? Can J Psychiatry. (2017) 62(2):109–14. doi: 10.1177/0706743716651049
13. Yi W, She S, Zhang J, Wu H, Zheng Y, Ning Y. Clozapine use in patients with early-stage schizophrenia in a Chinese psychiatric hospital. Neuropsychiatr Dis Treat. (2020) 16:2827–36. doi: 10.2147/NDT.S261503
14. Warnez S, Alessi-Severini S. Clozapine: a review of clinical practice guidelines and prescribing trends. BMC Psychiatry. (2014) 14:102. doi: 10.1186/1471-244X-14-102
15. Stokes I, Griffiths SL, Jones R, Everard L, Jones PB, Fowler D, et al. Prevalence of treatment resistance and clozapine use in early intervention services. BJPsych Open. (2020) 6(5):e107. doi: 10.1192/bjo.2020.89
16. Schwartz S, Carilli C, Mian T, Ruekert L, Kumar A. Attitudes and perceptions about the use of long-acting injectable antipsychotics among behavioral health practitioners. Ment Health Clin. (2022) 12(4):232–40. doi: 10.9740/mhc.2022.08.232
17. Kane JM, McEvoy JP, Correll CU, Llorca PM. Controversies surrounding the use of long-acting injectable antipsychotic medications for the treatment of patients with schizophrenia. CNS Drugs. (2021) 35(11):1189–205. doi: 10.1007/s40263-021-00861-6
18. Verma M, Grover S, Chakrabarti S, Dua D. Attitude towards and experience with clozapine of patients and their caregivers after three months of starting of clozapine. Nord J Psychiatry. (2021) 75(5):336–43. doi: 10.1080/08039488.2020.1857832
19. Parkes S, Mantell B, Oloyede E, Blackman G. Patients’ experiences of clozapine for treatment-resistant schizophrenia: a systematic review. Schizophr Bull Open. (2022) 3(1):sgac042. doi: 10.1093/schizbullopen/sgac042
20. Leung JG, Cusimano J, Gannon JM, Milgrom O, Valcourt SC, Stoklosa JB, et al. Addressing clozapine under-prescribing and barriers to initiation: a psychiatrist, advanced practice provider, and trainee survey. Int Clin Psychopharmacol. (2019) 34(5):247–56. doi: 10.1097/YIC.0000000000000269
21. Nielsen J, Dahm M, Lublin H, Taylor D. Psychiatrists’ attitude towards and knowledge of clozapine treatment. J Psychopharmacol. (2010) 24(7):965–71. doi: 10.1177/0269881108100320
22. Oloyede E, Blackman G, Mantell B, Harris E, Williams J, Taylor D, et al. What are the barriers and facilitators of clozapine use in early psychosis? A survey of UK early intervention clinicians. Schizophrenia. (2023) 9(1):26. doi: 10.1038/s41537-023-00353-0
23. Moullin JC, Dickson KS, Stadnick NA, Albers B, Nilsen P, Broder-Fingert S, et al. Ten recommendations for using implementation frameworks in research and practice. Implement Sci Commun. (2020) 1(1):42. doi: 10.1186/s43058-020-00023-7
24. Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated consolidated framework for implementation research based on user feedback. Implement Sci. (2022) 17(1):75. doi: 10.1186/s13012-022-01245-0
25. Skolarus TA, Lehmann T, Tabak RG, Harris J, Lecy J, Sales AE. Assessing citation networks for dissemination and implementation research frameworks. Implement Sci. (2017) 12(1):97. doi: 10.1186/s13012-017-0628-2
26. Hennink M, Kaiser BN. Sample sizes for saturation in qualitative research: a systematic review of empirical tests. Soc Sci Med. (2022) 292:114523. doi: 10.1016/j.socscimed.2021.114523
27. Hamilton AB. Qualitative methods in rapid turn-around health services research. VA Womens Health Res Netw. (2013). Available online at: https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=780
28. Neal JW, Neal ZP, VanDyke E, Kornbluh M. Expediting the analysis of qualitative data in evaluation: a procedure for the rapid identification of themes from audio recordings (RITA). Am J Eval. (2015) 36(1):118–32. doi: 10.1177/1098214014536601
29. Oloyede E, Mantell B, Williams J, Lai S, Jauhar S, Taylor D, et al. Clozapine for treatment resistance in early psychosis: a survey of UK clinicians’ training, knowledge and confidence. Ther Adv Psychopharmacol. (2022) 12:20451253221141222. doi: 10.1177/20451253221141222
30. Farooq S, Choudry A, Cohen D, Naeem F, Ayub M. Barriers to using clozapine in treatment-resistant schizophrenia: systematic review. BJPsych Bull. (2019) 43(1):8–16. doi: 10.1192/bjb.2018.67
31. Rakofsky JJ, Talbot TB, Dunlop BW. A virtual standardized patient–based assessment tool to evaluate psychiatric Residents’ psychopharmacology proficiency. Acad Psychiatry. (2020) 44(6):693–700. doi: 10.1007/s40596-020-01286-x
32. Rizzo A, Thomas Koenig S, Talbot TB. Clinical results using virtual reality. J Technol Hum Serv. (2019) 37(1):51–74. doi: 10.1080/15228835.2019.1604292
33. Rizzo AS, Koenig ST, Talbot TB. Clinical virtual reality: emerging opportunities for psychiatry. FOCUS. (2018) 16(3):266–78. doi: 10.1176/appi.focus.20180011
34. Wheeler A, Humberstone V, Robinson E, Sheridan J, Joyce P. Impact of audit and feedback on antipsychotic prescribing in schizophrenia. J Eval Clin Pract. (2009) 15(3):441–50. doi: 10.1111/j.1365-2753.2008.01032.x
35. Snider MDH, Boyd MR, Walker MR, Powell BJ, Lewis CC. Using audit and feedback to guide tailored implementations of measurement-based care in community mental health: a multiple case study. Implement Sci Commun. (2023) 4(1):94. doi: 10.1186/s43058-023-00474-8
36. Kilbourne AM, Geng E, Eshun-Wilson I, Sweeney S, Shelley D, Cohen DJ, et al. How does facilitation in healthcare work? Using mechanism mapping to illuminate the black box of a meta-implementation strategy. Implement Sci Commun. (2023) 4(1):53. doi: 10.1186/s43058-023-00435-1
37. Agency for Healthcare Research and Quality. Practice Facilitation Rockville, MDContent last reviewed February 2023. Available online at: https://www.ahrq.gov/evidencenow/practice-facilitation/index.html (Accessed February 01, 2024).
38. Walunas TL, Ye J, Bannon J, Wang A, Kho AN, Smith JD, et al. Does coaching matter? Examining the impact of specific practice facilitation strategies on implementation of quality improvement interventions in the healthy hearts in the heartland study. Implement Sci. (2021) 16(1):33. doi: 10.1186/s13012-021-01100-8
Keywords: consolidated framework for implementation research, patient perspective, schizophrenia, coordinated specialty care, stakeholder engagement, implementation determinants, antipsychotic medication
Citation: Carroll AJ, Robinson DG, Kane JM, Kordon A, Bannon J, Walunas TL and Brown CH (2024) Multi-level barriers and facilitators to implementing evidence-based antipsychotics in the treatment of early-phase schizophrenia. Front. Health Serv. 4:1385398. doi: 10.3389/frhs.2024.1385398
Received: 12 February 2024; Accepted: 23 September 2024;
Published: 14 October 2024.
Edited by:
Obasanjo Bolarinwa, York St John University, United KingdomReviewed by:
Christos Theleritis, University General Hospital Attikon, GreeceJane Ellen Carland, St Vincent's Hospital Sydney, Australia
Copyright: © 2024 Carroll, Robinson, Kane, Kordon, Bannon, Walunas and Brown. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Allison J. Carroll, QWxsaXNvbi5jYXJyb2xsQG5vcnRod2VzdGVybi5lZHU=
 Allison J. Carroll
Allison J. Carroll Delbert G. Robinson2,3
Delbert G. Robinson2,3 Avram Kordon
Avram Kordon Theresa L. Walunas
Theresa L. Walunas C. Hendricks Brown
C. Hendricks Brown