
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Health Serv. , 14 May 2024
Sec. Mental Health Services
Volume 4 - 2024 | https://doi.org/10.3389/frhs.2024.1365785
This article is part of the Research Topic Women in Mental Health Services: Volume 2 View all articles
Introduction: During the COVID-19 pandemic individuals with mental illnesses faced challenges accessing psychiatric care. Our study aimed to describe patient characteristics and compare admissions and length of stay (LOS) for psychiatric-related hospitalizations before and during the COVID-19 pandemic.
Methods: We conducted a retrospective analysis using health administrative data comparing individuals with an acute psychiatric admission between two time periods: 1st March 2019 to 31st December 2019 (pre-COVID) and 1st March 2020 to 31st December 2020 (during-COVID). Multivariable negative binomial regression was used to model the association between most responsible diagnosis type and the two-time periods to hospital LOS, reporting the Rate Ratio (RR) as the measure of effect.
Results: The cohort comprised 939 individuals who were predominately male (60.3%) with a severe mental illness (schizophrenia or mood-affective disorder) (72.7%) and a median age of 38 (IQR: 28.0, 52.0) years. In the multivariable analysis, anxiety disorders (RR: 0.63, CI: 0.4, 0.99) and personality disorders (RR: 0.52, CI: 0.32, 0.85) were significantly associated with a shorter LOS when compared to individuals without those disorders. Additionally, when compared to hospital admissions for non-substance related disorders the LOS for patients with substance-related disorders were significantly shorter during the COVID period (RR: 0.45, CI: 0.30, 0.67) and pre-COVID period (RR: 0.31, CI: 0.21, 0.46).
Conclusions: We observed a significant difference in the type and length of admissions for various psychiatric disorders during the COVID-19 period. These findings can support systems of care in adapting to utilization changes during pandemics or other global health events.
The COVID-19 pandemic placed unprecedented stress on both individuals and healthcare systems worldwide. Social isolation, financial stress and fear contributed to exacerbation of existing psychiatric conditions (1) and increased incidence of mental disorders (2, 3). Vulnerable groups, including individuals with pre-existing mental disorders, were disproportionally impacted by societal restrictions and mandated public health measures (4). Faced with escalating COVID-19 transmission rates, many jurisdictions required patient and health care provider isolation, resulting in a shift towards virtual healthcare and telemedicine to promote continuity of care while maintaining the safety of patients and providers (5–7). Despite rapid implementation of virtual services, reports of decreased availability and potential inadequacies of mental health treatment during the pandemic were a major concern and may have impacted access to those seeking psychiatric care (8).
There is emerging international evidence of variation in healthcare utilization patterns for individuals with mental illness during the COVID-19 pandemic. Italy and Portugal reported a decrease in psychiatric hospitalizations (9, 10), yet indicators of psychological distress such as suicidal ideation were notably increased in some jurisdictions (11). Similar trends of reduced utilization were observed across emergency department presentations in Germany (12) and Switzerland (13), but post-lockdown periods were associated with increased presentations and more severe clinical conditions (14). Moreover, observational research demonstrates varying hospitalization trends across diagnostic groups and population subgroups. In the United States (US) population-level research identified a significant increase in the number of admissions and longer length of inpatient hospitalizations for individuals with eating disorders during the pandemic (15). In addition, US youth and pediatric populations were linked to increased severity of symptoms (16) and higher rates of hospital admissions during the pandemic when compared to pre-pandemic periods (17).
Across Canada, mental health and substance use service utilization during the pandemic has mostly suggested a decline in emergency department and hospital visits (18, 19) with hospitalization rates returning to pre-pandemic levels by March 2021 (20). Evidence from Ontario, Canada using population-level administrative data found psychiatric-related hospital admissions did not return to pre-restriction rates (21) and while overall volumes may have decreased, monthly increases were observed for specific mental disorders post pandemic (22, 23). In British Columbia (BC), Canada COVID-19 mental-health related service use rose sharply during 2020, but quickly stabilized; however, other types of mental health service use and drug dispensation continued to rise significantly into 2021 (24). The impact of the pandemic on mental health hospital admissions within Canada exhibited considerable variability across geography and disorder type and research examining changes to hospital LOS for psychiatric patients during COVID-19 in Canada remains scare. Despite what appears to be a stabilization of psychiatric hospitalization trends, it remains critical to evaluate the impact of changes to acute care (i.e., hospital-based care and treatment for a disease or severe episode of illness on a time limited basis) (25) and explore other health system indicators including length of stay (LOS) during the COIVD-19 period. Hospital LOS, among other indicators is commonly used to measure aspects of hospital quality and efficiency (26, 27) and is a standard metric in many health systems to understand operational needs including flow of patients through hospital services (28). While commonly used, hospital LOS is complex and can be affected by several factors including illness severity, treatment complexity and individual patient characteristics (29, 30) which makes calculating and predicting an optimal LOS challenging (31). Average LOS for psychiatric inpatients generally exceeds other medical specialities (32–34), with shorter LOS potentially signalling treatment disparities or perpetuating a “revolving door” phenomenon (35, 36). Nevertheless, it is generally accepted that reducing LOS for patients is desirable as longer than average LOS is also associated with increased risk of hospital acquired harms (e.g., falls, infection, other adverse events) and healthcare resources utilization (37, 38).
In BC, as in numerous other regions, the pandemic was associated with significant unmet health needs and worsening mental health and substance use outcomes (39). Regrettably, health system capacity remains strained since the pandemic (40, 41) and health services planning has failed to examine how to address changes in demand for health services following COVID-19 (42, 43). Moreover, such planning needs to be informed by service utilization data that are representative of local contexts and populations. To address this gap we conducted a retrospective cohort study using health administrative data comparing acute psychiatric admissions and LOS before and during the COVID-19 pandemic in Vancouver, BC, Canada.
In BC, Canada the local government declared a provincial state of emergency on 17 March 2020, to support the provincewide response to the COVID-19 pandemic. Schools, playgrounds and non-essential businesses were closed, and social distance requirements were broadly implemented (44). Concurrently, healthcare organizations limited visitation and implemented new safety protocols while also postponing or delaying nonessential care (45). Despite a brief disruption in healthcare services (40), by May 2020 local hospitals (including the study site) adapted services in response to provincial COVID-19 policies and implemented site specific screening, testing and infection control precautions. Additionally, a coordinated response was developed and implemented to manage COVID-19 infections among psychiatric patients who required hospital admission. Our study site created designated psychiatric units for suspected and confirmed COVID-19 patients to receive psychiatric care while minimizing the risk of transmission and disruptions to treatment.
This retrospective cohort study used health administrative data for adults with a psychiatric admission to a single urban hospital in Vancouver, BC. Admission rates and LOS were compared between two time periods: 1st March 2019 to 31st December 2019 (pre-COVID) and 1st March to 31st December 2020 (during-COVID). Our study site provides inpatient and emergency services to a catchment area that includes Vancouver's Downtown Eastside, a region with high rates of mental illness, substance use, and communicable disease (46). The patient's first discharge during that time period determined the index admission (first hospital admission during observation period). Hospital LOS (number of days a patient was admitted to hospital) was measured for each hospital admission during the study period. Patients were excluded from the study if they had an invalid personal health number, invalid age, were younger than 17 years of age, died during the psychiatric hospitalization or transferred to another hospital at the time of discharge. Sociodemographic variables (age, sex, and homelessness) were obtained from electronic medical records. Hospitalization data were obtained from the Ministry of Health's Discharge Abstract Database, which includes information related to each acute hospital separation. The study was reviewed and approved by the University of British Columbia—Providence Health Care (UBC-PHC) Research Ethics Board–H21-00462. Because of the retrospective nature of this study, patient informed consent for inclusion was waived by the institutional review board of UBC-PHC Research Ethics Board.
Our primary outcome was any psychiatric hospital admission and hospital LOS. LOS is a continuous variable indicating the number of days a patient was admitted to hospital (total number of days from admission date to discharge date). All hospitalization records included diagnostic codes representing the most responsible diagnosis for each psychiatric hospitalization. The present study used International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Canada (ICD-10-CA) to determine the most responsible diagnosis, a modified version of ICD-10, developed by Canadian Institute for Health Information and used across Canada. The following ICD-10-CA codes were used to determine the most responsible diagnoses for hospitalizations associated with: schizophrenia, delusional and non organic psychotic disorders F20 (excluding F20.4) to F25, F28, F29, F53.1; mood/affective disorders (F30–F34, F38, F39, F53.0); anxiety disorders (F40–F43, F48.8, F48.9); personality disorders (F60–F62, F69, F21); and substance use disorders (F55, F10–F19).
Patient demographic variables were summarized and compared using percentages and Chi-square tests for categorical variables (sex, homelessness) and median (IQR) and Kruskal–Wallis tests for continuous variables (age and LOS), stratified by the pre-COVID and during-COVID periods. Given the observed overdispersion, we selected the Negative Binomial model to evaluate the impact of diagnosis type on LOS. The negative binomial model was adjusted for age, sex, homelessness and pre-during COVID, where interactions between diagnoses type (yes vs. no) and the two time periods (pre-COVID vs. during COVID) on hospital LOS were tested. Significance for the interaction was determined with a p-value of <0.1. We used Rate Ratios and 95% CIs to estimate the association of predictor variables on the outcome. Analyses were completed used SAS, version 9.4.
The cohort comprised 939 patients who were predominately male (60.3%) with a severe mental illness (schizophrenia or mood-affective disorder) (72.7%) and a mean age of 38 (IQR: 28.0, 52.0) years. There were 472 acute psychiatric admissions during the pre-COVID period and 467 acute psychiatric admissions during the COVID period. After adjusting for the population size, the pre-COVID admission rate was 11.1 per 100,000 individuals and the during-COVID admission rate was 10.9 per 100,000 individuals. In the during-COVID period, admissions related to schizophrenia and psychotic disorders were significantly higher (49.7% vs. 40.9%; p = 0.007) and admissions related to substance disorders were significantly lower (15.4% vs. 21.6%; p = 0.015) when compared to the pre-COVID period (Figure 1). Additional details characterizing the sample during the pre and during COVID periods are reported in Table 1.
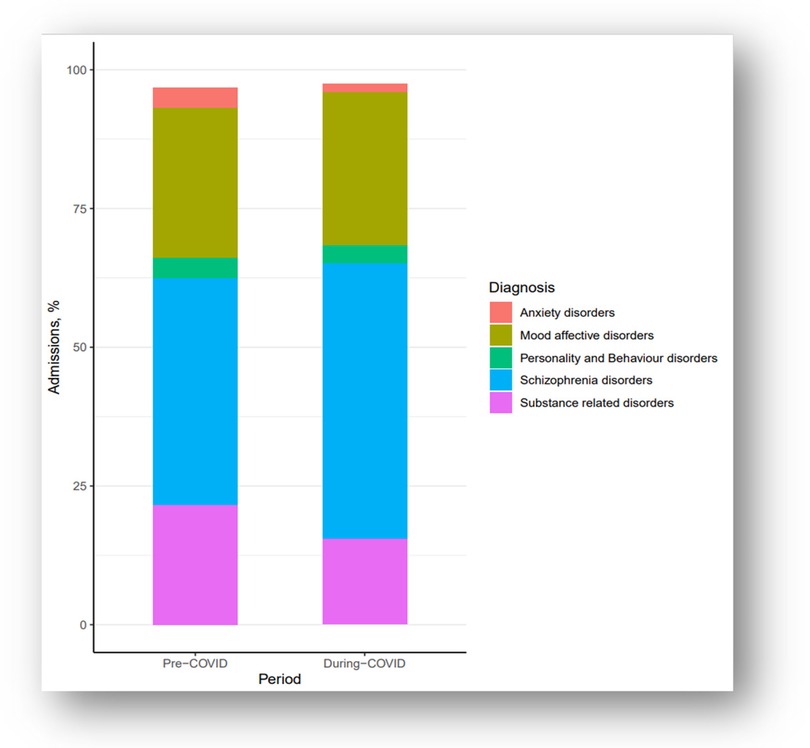
Figure 1. Proportion of hospital admissions by diagnosis type for the pre-COVID period (2019; n = 472) and during-COVID period (2020; n = 467) from an urban hospital in Vancouver, BC (n = 939).
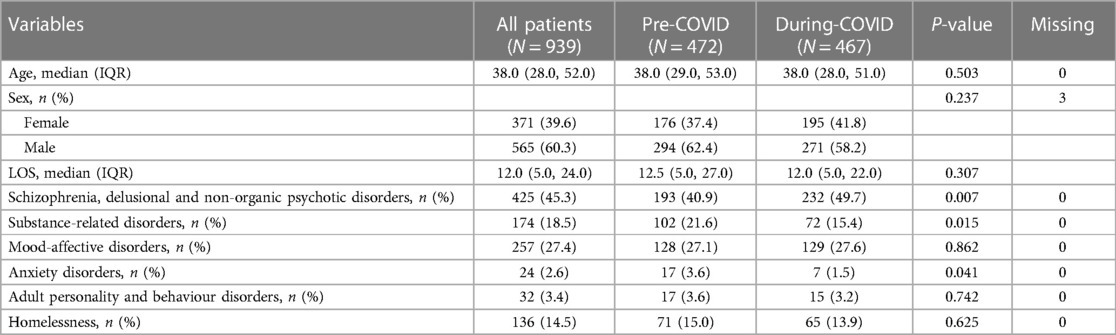
Table 1. Characteristics of included patients at the pre-COVID period (2019) and during-COVID period (2020), from an urban hospital in Vancouver, BC (n = 939).
The median pre-COVID and during-COVID hospital LOS was 12 days. As shown in Table 2, female patients had a longer LOS than male patients (p = 0.022) and LOS increased with age (p ≤ 0.001). When compared to individuals without each disorder type, individuals with schizophrenia-related disorders and mood-affective disorders had longer lengths of stay and individuals with substance-related disorders, anxiety disorders, or personality and behaviour disorders had shorter lengths of stay (Table 2). Comparisons of hospital LOS for each disorder are provided in (Supplementary Material Figures S1–S5).
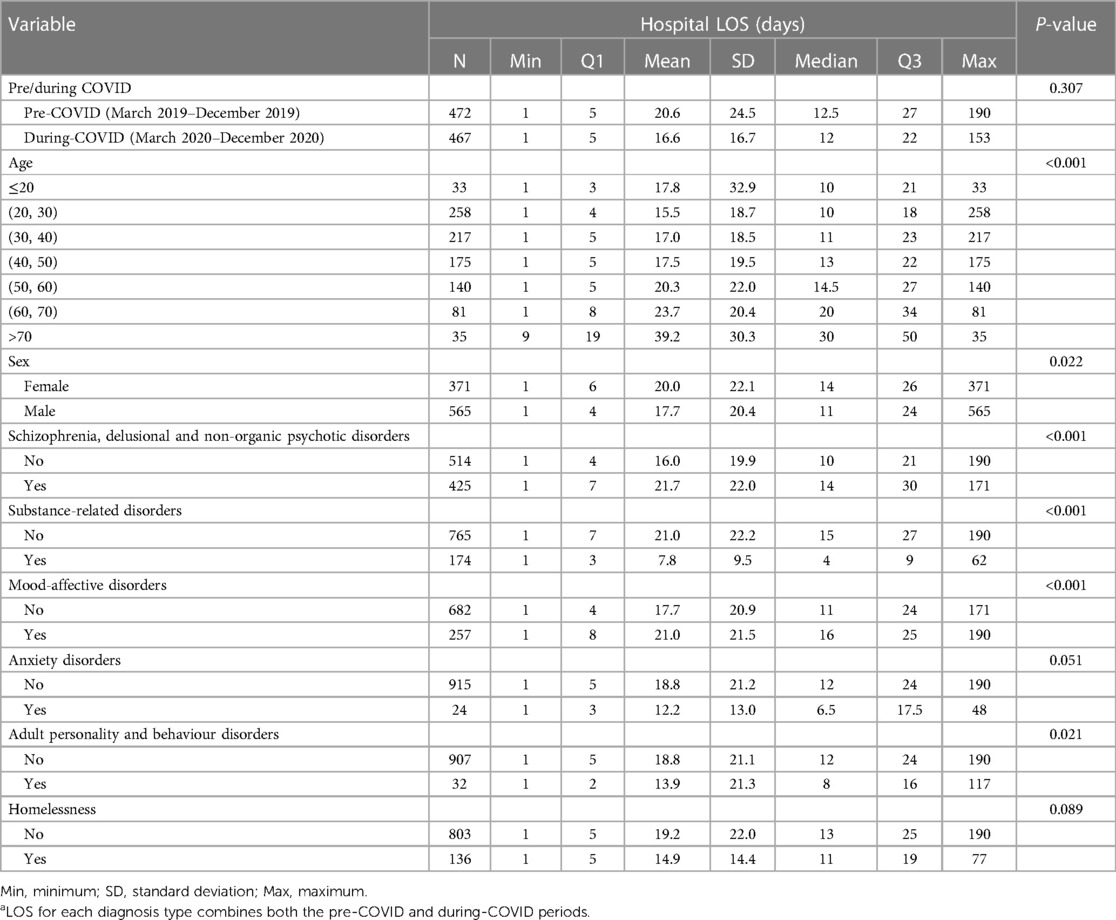
Table 2. Distribution of hospital LOSa for the pre-COVID period (2019) and during-COVID period (2020), from an urban hospital in Vancouver, BC (n = 939).
In unadjusted analysis the mean LOS decreased by 20% during-COVID when compared to the pre-COVID period (RR: 0.80, CI: 0.71, 0.91) (Table 3). Except for adult personality and behaviour disorders, all the other diagnosis types are significantly associated to LOS (p ≤ 0.05). Results for the multivariable negative binomial model are shown in Table 4. Anxiety disorders (RR: 0.63, CI: 0.40, 0.99) and adult personality (RR: 0.52, CI: 0.32, 0.85) disorders were significantly associated with a shorter LOS when compared to individuals without those disorders at the pre- and during-COVID periods. Additionally, having a substance use disorder was significantly associated with a shorter LOS. There was a significant interaction between substance-related disorders and pre-during COVID period (p-value = 0.057) (See Supplementary Material Table S1). The ratio of LOS among patients with and without substance-related disorders increased from RR: 0.31, CI: 0.21, 0.46 in the pre-COVID period to RR: 0.45, CI: 0.30, 0.67 in the during COVID period (Table 4). There were no significant associations between LOS and schizophrenia-related disorders or mood and affective disorders.
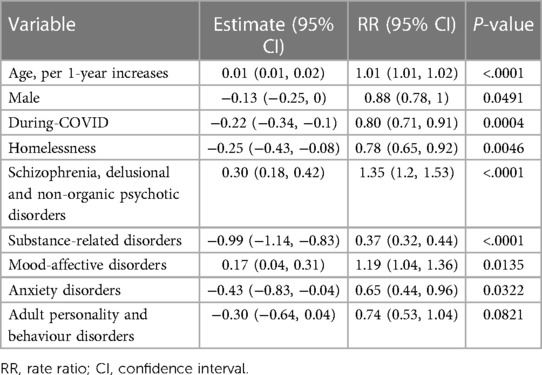
Table 3. Univariate associations between diagnosis type and hospital LOS (days) from an urban hospital in Vancouver, BC, 2019–2020.
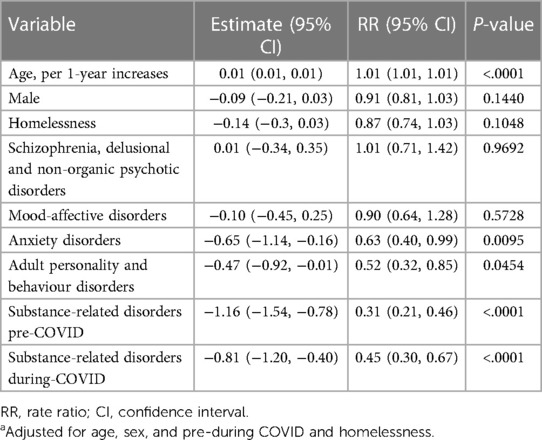
Table 4. Multivariable negative binomial model estimating the association between diagnosis type and hospital LOSa (days) from an urban hospital in Vancouver, BC, 2019–2020.
We observed statistically significant changes in hospital admissions and hospital LOS for several mental and substance use disorders during the COVID-19 period. When compared to pre-pandemic psychiatric hospital admissions by diagnoses, admissions for schizophrenia and psychotic disorders were significantly increased while admissions for substance disorders were significantly decreased. With respect to hospital LOS, anxiety disorders, personality disorder and substance use disorder were associated with significantly shorter LOS when compared to individuals without those disorders. To our knowledge, this is the first study to examine changes to acute psychiatric admissions and hospital LOS during the COVID-19 pandemic using clinical and administrative data from a large urban hospital in Vancouver, BC.
The pandemic had a disproportionate impact on individuals with severe mental illness and related vulnerabilities (e.g., homelessness, substance use), exacerbating symptoms and worsening clinical outcomes (1). Despite this trend, our study revealed an overall reduction in acute psychiatric hospitalizations during the pandemic when compared to the same time period in 2019. Possible explanations for this decrease in hospitalizations may be linked to public health restrictions limiting movement and deterring people from seeking help for non-COVID related illnesses during the pandemic (47). While our overall hospitalization rates declined, we observed a 10% increase in admissions related to psychotic disorders during the COVID-19 period. This rise in admissions may be attributed to the limited availability of community supports and the potentially heightened severity of individual needs requiring urgent or involuntary admissions (12) and psychotropic medications (24). Conversely, when compared to the pre-COVID period, we observed a decrease in substance-related admissions. While several factors such as restricted access to substances, disruptions in treatment services, or changes in substance use patterns during the pandemic (48, 49) provide context to the change in hospital admission rates in our study, mortality from drug-related deaths rose sharply during this period in BC (50). In 2020, the BC Coroners Service reported a staggering 80% rise in drug-related deaths in comparison to the preceding year, with a notable increase observed within the Vancouver Coastal Health (VCH) region—an area encompassing our study site (51). Fentanyl, a powerful synthetic opioid, was present in 84% of unregulated drug deaths in the VCH region in 2020, a slight increase from 81% in 2019 (51). The rise in fentanyl or fentanyl analogues involved deaths is growing and is currently the leading cause of opioid related deaths in BC and Canada (52). Continued assessment is crucial to understand the effects on individuals who may have received inadequate support during the pandemic, considering the ongoing challenges posed by the opioid crisis in British Columbia.
Risk factors for hospital LOS serve as important indicators for health system planning, resources allocation and costs. Healthcare delivery has undergone significant shifts and challenges in the wake of the COVID-19 pandemic, with the pandemic introducing unique variables and considerations that may influence LOS patterns. For example, our study site's adjustments to hospital policies regarding COVID-19 screening and quarantine for psychiatric patients reduced the need to transfer or prematurely discontinue care. This was achieved by setting up specialized psychiatric units specifically for patients who were suspected of having, or who tested positive for, COVID-19. Our findings highlight a 20% decrease in mean LOS during-COVID when compared to the pre-COVID period and demonstrate significant associations between important demographic factors and increased LOS. Consistent with prior research reporting gender disparities in LOS (53), we found that female patients had longer LOS compared to male patients, with a mean difference of 2.3 days. While propensity for help-seeking (54) and pre-existing rates of depression and anxiety are heightened among females (55, 56), rates of psychological distress during the pandemic were significantly higher for females (57) when compared to males. These sex differences may offer potential explanation to the increased hospital LOS for females in our study. Additionally, our results demonstrated that increasing age was associated with a longer LOS, with a small but statistically significant increase. This finding aligns with existing research reporting a robust association between older age and increased LOS in both general and psychiatric populations (29, 58). Extensive research on hospital LOS in psychiatric inpatients reveals a body of evidence indicating that longer stays are consistently linked to more adverse outcomes (e.g., suicidality and reduced social functioning, employment and housing) and escalating costs (59–61). Conversely, shorter than average hospital LOS might be indicative of lower quality care and associated with risk for early readmission (36, 62); however, this conclusion is not supported by current evidence (63). While determining an optimal LOS is complex, stabilization and coordinated discharge remains the goal of inpatient psychiatric care. Our study contributes to the growing body of evidence examining risk factors for LOS and provide insights into healthcare resource management while underscoring the importance of targeted interventions to address demographic disparities and promote equitable patient care.
In addition to socio-demographic factors, we found a disproportionate impact on hospital LOS for certain diagnostic subgroups. Specifically, individuals with anxiety disorders and adult personality disorders had significantly shorter hospital LOS compared to those without these disorders during the COVID-19 period. These findings align with prior evidence reporting shorter hospital stays for patients due to infection control and changes to treatment approaches, including the increased use of tele-psychiatry (64, 65). Despite reductions in acute care capacity, outpatient mental health services rapidly adapted to support patients using virtual health solutions and were associated with improved visit adherence over time and have emerged as a promising model for improving the efficiency of mental health care delivery (66, 67). Moreover, substance use disorders were significantly associated with a shorter LOS which is consistent with findings from prior research examining psychiatric hospitalizations (58, 68, 69). Specifically, hospital LOS in the pre-COVID and during-COVID periods was 69% and 55% shorter, respectively, for patients with substance-related disorders compared to those without substance-related disorders. The reduced hospital LOS may be attributed to various factors, including altered discharge planning processes, or modifications/reductions in the overall healthcare system capacity (e.g., when demand is not met with additional capacity, this can translate into shorter hospital stays) (70); however, it is important to consider that the observed decrease in LOS may also reflect changes in case mix or individual care needs during the pandemic. While substance use has been linked to shorter hospital LOS, further evaluation and examination of the impact of shorter LOS for people with a substance use disorder are warranted in the context of documented unmet treatment needs (71). These findings contribute to the existing body of literature on psychiatric disorders and LOS, emphasizing the importance of providing evidence-based care that addresses the specific needs of individuals with psychiatric and substance use disorders.
While our study has several strengths including a large sample and use of administrative data, there are some limitations to consider. Firstly, our results may not be generalizable to other settings or populations, as they are based on data from a single site. Given the location of the study site, our sample may not be representative of the broader population, leading to potential selection biases and limited external validity. Secondly, administrative data primarily captures information that is routinely collected for billing purposes, which may not capture all relevant clinical variables or detailed patient characteristics. Data describing race/ethnicity were not reliably collected as part of routine care and therefore excluded from our analysis. This can result in incomplete or limited data on potential confounding variables, making it challenging to fully account for all factors that could influence the outcome of interest. Thirdly, the use of administrative data is subject to potential data quality issues, including inaccuracies, missing data, and coding errors. These issues can introduce measurement biases and affect the validity of the study findings. Fourthly, we could not examine the circumstance surrounding admission such as whether pandemic related restrictions contributed and our data does not capture all relevant parameters contributing to LOS such as community services and social or family supports which may have impacted LOS. Researchers should consider these limitations when interpreting both the magnitude and direction of the effect size, and generalize the findings cautiously to other populations or settings. Future research would benefit from additional analysis to account for social context, changes during the early pandemic period and the inclusion of multiple study sites.
We observed a significant difference in length of stay for mental and substance use disorders during the COVID-19 period. These findings underscore the need for further evaluation of the healthcare system to effectively plan and adapt to evolving utilization patterns during pandemics and public health emergencies, particularly for psychiatric populations. Our results provide knowledge about determinants of LOS which could lead to improvements in the quality of psychiatric hospital care for people with mental and substance use disorders. Future research is needed to understand the long-term implications of pandemic-related changes in mental illness and related healthcare utilization.
The data analyzed in this study is subject to the following licenses/restrictions: The datasets analyzed during the current study are not publicly available due to privacy reasons. Requests to access these datasets should be directed toYXJ1c3NvbGlsbG8xQHByb3ZpZGVuY2VoZWFsdGguYmMuY2E=.
The studies involving humans were approved by the University of British Columbia—Providence Health Care (UBC-PHC) Research Ethics Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
AR: Conceptualization, Data curation, Methodology, Project administration, Writing – original draft, Writing – review & editing. MC: Writing – review & editing. MG: Formal Analysis, Writing – review & editing. PS: Writing – review & editing. DK: Writing – review & editing. JR: Writing – review & editing.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2024.1365785/full#supplementary-material
1. Murphy L, Markey K, Donnell CO, Moloney M, Doody O. The impact of the COVID-19 pandemic and its related restrictions on people with pre-existent mental health conditions: a scoping review. Arch Psychiatr Nurs. (2021) 35(4):375–94. doi: 10.1016/j.apnu.2021.05.002
2. Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. (2021) 281:91–8. doi: 10.1016/j.jad.2020.11.117
3. Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, et al. Epidemiology of mental health problems in COVID-19: a review. F1000Res. (2020) 9:636. doi: 10.12688/f1000research.24457.1
4. Hong S, Walton B, Kim HW, Kaboi M, Moynihan S, Rhee TG. Exploring disparities in behavioral health service use in the early stages of the COVID-19 pandemic. Int J Behav Med. (2023):1–14. doi: 10.1007/s12529-023-10192-z. [Epub ahead of print].
5. Baum A, Kaboli PJ, Schwartz MD. Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med. (2020) 174(1):M20–3026. doi: 10.7326/M20-3026
6. Mishkind MC, Shore JH, Bishop K, D’Amato K, Brame A, Thomas M, et al. Rapid conversion to telemental health services in response to COVID-19: experiences of two outpatient mental health clinics. Telemed e-Heal. (2021) 27(7):778–84. doi: 10.1089/tmj.2020.0304
7. Shore JH, Schneck CD, Mishkind MC. Telepsychiatry and the coronavirus disease 2019 pandemic—current and future outcomes of the rapid virtualization of psychiatric care. JAMA Psychiatry. (2020) 77(12):1211–2. doi: 10.1001/jamapsychiatry.2020.1643
8. Rains LS, Johnson S, Barnett P, Steare T, Needle JJ, Carr S, et al. Early impacts of the COVID-19 pandemic on mental health care and on people with mental health conditions: framework synthesis of international experiences and responses. Soc Psychiatry Psychiatr Epidemiol. (2021) 56(1):13–24. doi: 10.1007/s00127-020-01924-7
9. Rodrigues CA, Rodrigues N, Nascimento M, Oliveira-Silva J. Patterns of adult and youth inpatient admissions before and after the COVID-19 pandemic in a psychiatric ward: an observational study. BMC Heal Serv Res. (2022) 22(1):1048. doi: 10.1186/s12913-022-08374-8
10. Clerici M, Durbano F, Spinogatti F, Vita A, de Girolamo G, Micciolo R. Psychiatric hospitalization rates in Italy before and during COVID-19: did they change? An analysis of register data. Ir J Psychol Med. (2020) 37(4):283–90. doi: 10.1017/ipm.2020.29
11. Boldrini T, Girardi P, Clerici M, Conca A, Creati C, Cicilia GD, et al. Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in Italy: reduced psychiatric hospitalizations and increased suicidality. Prog Neuro-Psychopharmacol Biol Psychiatry. (2021) 110:110304. doi: 10.1016/j.pnpbp.2021.110304
12. Fasshauer JM, Bollmann A, Hohenstein S, Hindricks G, Meier-Hellmann A, Kuhlen R, et al. Emergency hospital admissions for psychiatric disorders in a German-wide hospital network during the COVID-19 outbreak. Soc Psychiatry Psychiatr Epidemiology. (2021) 56(8):1469–75. doi: 10.1007/s00127-021-02091-z
13. Ambrosetti J, Macheret L, Folliet A, Wullschleger A, Amerio A, Aguglia A, et al. Impact of the COVID-19 pandemic on psychiatric admissions to a large Swiss emergency department: an observational study. Int J Environ Res Public Heal. (2021) 18(3):1174. doi: 10.3390/ijerph18031174
14. Ambrosetti J, Macheret L, Folliet A, Wullschleger A, Amerio A, Aguglia A, et al. Psychiatric emergency admissions during and after COVID-19 lockdown: short-term impact and long-term implications on mental health. BMC Psychiatry. (2021) 21(1):465. doi: 10.1186/s12888-021-03469-8
15. Asch DA, Buresh J, Allison KC, Islam N, Sheils NE, Doshi JA, et al. Trends in US patients receiving care for eating disorders and other common behavioral health conditions before and during the COVID-19 pandemic. JAMA Netw Open. (2021) 4(11):e2134913. doi: 10.1001/jamanetworkopen.2021.34913
16. Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19. JAMA Pediatr. (2021) 175(11):1142–50. doi: 10.1001/jamapediatrics.2021.2482
17. Gutiérrez-Sacristán A, Serret-Larmande A, Hutch MR, Sáez C, Aronow BJ, Bhatnagar S, et al. Hospitalizations associated with mental health conditions among adolescents in the US and France during the COVID-19 pandemic. JAMA Netw Open. (2022) 5(12):e2246548. doi: 10.1001/jamanetworkopen.2022.46548
18. Kim HK, Carvalho AF, Gratzer D, Wong AHC, Gutzin S, Husain MI, et al. The impact of COVID-19 on psychiatric emergency and inpatient services in the first month of the pandemic in a large urban mental health hospital in Ontario, Canada. Front Psychiatry. (2021) 12:563906. doi: 10.3389/fpsyt.2021.563906
19. Kim S, Rajack N, Mondoux SE, Tardelli VS, Kolla NJ, Foll BL. The COVID-19 impact and characterization on substance use-related emergency department visits for adolescents and young adults in Canada: practical implications. J Eval Clin Pr. (2023) 29(3):447–58. doi: 10.1111/jep.13817
20. Saunders NR, Toulany A, Deb B, Strauss R, Vigod SN, Guttmann A, et al. Acute mental health service use following onset of the COVID-19 pandemic in Ontario, Canada: a trend analysis. Can Méd Assoc Open Access J. (2021) 9(4):E988–97. doi: 10.9778/cmajo.20210100
21. Ham E, Hilton NZ, Crawford J, Kim S. Psychiatric inpatient services in Ontario, 2019–2021: a cross-sectional comparison of admissions, diagnoses and acuity during the COVID-19 prerestriction, restriction and postrestriction periods. Can Méd Assoc Open Access J. (2023) 11(5):E988–94. doi: 10.9778/cmajo.20220158
22. Tanner B, Kurdyak P, de Oliveira C. Adult psychiatric hospitalizations in Ontario, Canada before and during the COVID-19 pandemic. Can J Psychiatry. (2023) 68(12):925–32. doi: 10.1177/07067437231167386
23. Patten SB, Dimitropoulos G, Williams JVA, Rao S, Fahim M, Sharifi V, et al. Hospital admissions for personality disorders increased during the COVID-19 pandemic. Can J Psychiatry. (2023) 68(6):470–2. doi: 10.1177/07067437231155999
24. Zandy M, Kurdi SE, Samji H, McKee G, Gustafson R, Smolina K. Mental health-related healthcare service utilisation and psychotropic drug dispensation trends in British Columbia during COVID-19 pandemic: a population-based study. Gen Psychiatry. (2023) 36(1):e100941. doi: 10.1136/gpsych-2022-100941
25. Canadian Institute for Health Information (CIHI). Acute care. Available online at: https://www.cihi.ca/en/topics/acute-care (cited March 6, 2024).
26. Agency for Healthcare Research and Quality. Measuring the quality of hospital care. Measuring the quality of hospital care. Available online at: https://www.ahrq.gov/talkingquality/measures/setting/hospitals/index.html (cited Mar 26, 2024).
27. Organisation for Economic Cooperation and Development (OECD). Length of hospital stay (indicator). (cited April 1, 2024). doi: 10.1787/8dda6b7a-en
28. Manning L, Islam MS. A systematic review to identify the challenges to achieving effective patient flow in public hospitals. Int J Heal Plan Manag. (2023) 38(3):805–28. doi: 10.1002/hpm.3626
29. Eskandari M, Bahmani AHA, Mardani-Fard HA, Karimzadeh I, Omidifar N, Peymani P. Evaluation of factors that influenced the length of hospital stay using data mining techniques. BMC Méd Inform Decis Mak. (2022) 22(1):280. doi: 10.1186/s12911-022-02027-w
30. Buttigieg SC, Abela L, Pace A. Variables affecting hospital length of stay: a scoping review. J Heal Organ Manag. (2018) 32(3):463–93. doi: 10.1108/JHOM-10-2017-0275
31. Stone K, Zwiggelaar R, Jones P, Parthaláin NM. A systematic review of the prediction of hospital length of stay: towards a unified framework. PLOS Digit Heal. (2022) 1(4):e0000017. doi: 10.1371/journal.pdig.0000017
32. Lee S, Rothbard AB, Noll EL. Length of inpatient stay of persons with serious mental illness: effects of hospital and regional characteristics. Psychiatr Serv. (2012) 63(9):889–95. doi: 10.1176/appi.ps.201100412
33. Simko L, Birgisson NE, Pirrotta EA, Wang E. Waiting for care: length of stay for ED mental health patients by disposition, diagnosis, and region (2009–2015). Cureus. (2022) 14(6):e25604. doi: 10.7759/cureus.25604
34. Adepoju OE, Kim LH, Starks SM. Hospital length of stay in patients with and without serious and persistent mental illness: evidence of racial and ethnic differences. Healthcare. (2022) 10(6):1128. doi: 10.3390/healthcare10061128
35. Glick ID, Sharfstein SS, Schwartz HI. Inpatient psychiatric care in the 21st century: the need for reform. Psychiatr Serv. (2011) 62(2):206–9. doi: 10.1176/ps.62.2.pss6202_0206
36. Figueroa R, Harman J, Engberg J. Use of claims data to examine the impact of length of inpatient psychiatric stay on readmission rate. Psychiatr Serv. (2004) 55(5):560–5. doi: 10.1176/appi.ps.55.5.560
37. Adler L, Yi D, Li M, McBroom B, Hauck L, Sammer C, et al. Impact of inpatient harms on hospital finances and patient clinical outcomes. J Patient Saf. (2018) 14(2):67–73. doi: 10.1097/PTS.0000000000000171
38. Canadian Institute for Health Information (CIHI). Understanding Variability in the Cost of a Standard Hospital Stay. Ottawa, ON: CIHI (2017). Available online at: https://secure.cihi.ca/free_products/cshs-variability-study-2017-en.pdf (cited March 6, 2024).
39. British Columbia Centre for Disease Control [BCCDC]. BC COVID-19 SPEAK survey round 2. Available online at: https://public.tableau.com/app/profile/bccdc/viz/BCCOVID-19SPEAKSurveyRound2/BCCOVID-19SPEAKresults (cited October 6, 2023).
40. Canadian Institute for Health Information (CIHI). Impact of COVID-19 on Canada’s health care systems. Available online at: https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems (cited March 6, 2024).
41. Canadian Institute for Health Information (CIHI). Wait times for community mental health counselling. Available online at: https://www.cihi.ca/en/indicators/wait-times-for-community-mental-health-counselling (cited October 6, 2023).
42. Pujolar G, Oliver-Anglès A, Vargas I, Vázquez ML. Changes in access to health services during the COVID-19 pandemic: a scoping review. Int J Environ Res Public Heal. (2022) 19(3):1749. doi: 10.3390/ijerph19031749
43. Isasi F, Naylor MD, Skorton D, Grabowski D, Hernández S, Rice VM. Patients, families, and communities COVID-19 impact assessment: lessons learned and compelling needs. NAM Perspect. (2021):11. doi: 10.31478/202111c
44. Detsky AS, Bogoch II. COVID-19 in Canada. JAMA. (2020) 324(8):743–4. doi: 10.1001/jama.2020.14033
45. British Columbia Centre for Disease Control (BCCDC). Examining the societal consequences of the COVID-19 pandemic. Available online at: http://www.bccdc.ca/health-professionals/data-reports/societal-consequences-covid-19/health-care-services (cited March 1, 2024).
46. Linden IA, Mar MY, Werker GR, Jang K, Krausz M. Research on a vulnerable neighborhood—the Vancouver downtown eastside from 2001 to 2011. J Urban Heal. (2013) 90(3):559–73. doi: 10.1007/s11524-012-9771-x
47. Filip R, Puscaselu RG, Anchidin-Norocel L, Dimian M, Savage WK. Global challenges to public health care systems during the COVID-19 pandemic: a review of pandemic measures and problems. J Pers Med. (2022) 12(8):1295. doi: 10.3390/jpm12081295
48. Chacon NC, Walia N, Allen A, Sciancalepore A, Tiong J, Quick R, et al. Substance use during COVID-19 pandemic: impact on the underserved communities. Discoveries (Craiova). (2021) 9(4):e141. doi: 10.15190/d.2021.20
49. McNeil R, Fleming T, Mayer S, Barker A, Mansoor M, Betsos A, et al. Implementation of safe supply alternatives during intersecting COVID-19 and overdose health emergencies in British Columbia, Canada, 2021. Am J Public Heal. (2022) 112(S2):S151–8. doi: 10.2105/AJPH.2021.306692
50. Palis H, Bélair M, Hu K, Tu A, Buxton J, Slaunwhite A. Overdose deaths and the COVID-19 pandemic in British Columbia, Canada. Drug Alcohol Rev. (2022) 41(4):912–7. doi: 10.1111/dar.13424
51. British Columbia Coroner Service. Statistical reports on deaths in British Columbia: unregulated drug deaths—summary. Available online at: https://www2.gov.bc.ca/gov/content/life-events/death/coroners-service/statistical-reports (cited January 1, 2024).
52. Belzak L, Halverson J. The opioid crisis in Canada: a national perspective. Heal Promot Chronic Dis Prev Can Res Policy Pract. (2018) 38(6):224–33. doi: 10.24095/hpcdp.38.6.02
53. Tulloch AD, Fearon P, David AS. Length of stay of general psychiatric inpatients in the United States: systematic review. Adm Polic Ment Heal Ment Heal Serv Res. (2011) 38(3):155–68. doi: 10.1007/s10488-010-0310-3
54. Mackenzie CS, Gekoski WL, Knox VJ. Age, gender, and the underutilization of mental health services: the influence of help-seeking attitudes. Aging Ment Heal. (2006) 10(6):574–82. doi: 10.1080/13607860600641200
55. McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. (2011) 45(8):1027–35. doi: 10.1016/j.jpsychires.2011.03.006
56. Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci. (2015) 40(4):219–21. doi: 10.1503/jpn.150205
57. Pongou R, Ahinkorah BO, Maltais S, Mabeu MC, Agarwal A, Yaya S. Psychological distress during the COVID-19 pandemic in Canada. PLoS One. (2022) 17(11):e0277238. doi: 10.1371/journal.pone.0277238
58. Chen S, Collins A, Anderson K, McKenzie K, Kidd S. Patient characteristics, length of stay, and functional improvement for schizophrenia spectrum disorders: a population study of inpatient care in Ontario 2005–2015. Can J Psychiatry. (2017) 62(12):854–63. doi: 10.1177/0706743716680167
59. Xu Z, Müller M, Lay B, Oexle N, Drack T, Bleiker M, et al. Involuntary hospitalization, stigma stress and suicidality: a longitudinal study. Soc Psychiatry Psychiatr Epidemiol. (2018) 53(3):309–12. doi: 10.1007/s00127-018-1489-y
60. Tseng MCM, Chang CH, Liao SC, Yeh YC. Length of stay in relation to the risk of inpatient and post-discharge suicides: a national health insurance claim data study. J Affect Disord. (2020) 266:528–33. doi: 10.1016/j.jad.2020.02.014
61. Smith P, Nicaise P, Giacco D, Bird VJ, Bauer M, Ruggeri M, et al. Use of psychiatric hospitals and social integration of patients with psychiatric disorders: a prospective cohort study in five European countries. Soc Psychiatry Psychiatr Epidemiol. (2020) 55(11):1425–38. doi: 10.1007/s00127-020-01881-1
62. Thomas JW, Guire KE, Horvat GG. Is patient length of stay related to quality of care? Hosp Heal Serv Adm. (1997) 42(4):489–507.
63. Babalola O, Gormez V, Alwan NA, Johnstone P, Sampson S. Length of hospitalisation for people with severe mental illness. Cochrane Database Syst Rev. (2014) 2014(1):CD000384. doi: 10.1002/14651858.cd000384
64. Gude J, Subhedar RV, Zhang MH, Jain P, Bhela J, Bangash F, et al. Emerging needs and viability of telepsychiatry during and post COVID-19 era: a literature review. Cureus. (2021) 13(8):e16974. doi: 10.7759/cureus.16974
65. Andersen JA, Rowland B, Gloster E, McElfish PA. Telehealth utilization during COVID-19 among people with diagnosed mental health conditions. Telemed e-Heal. (2022) 28(5):743–6. doi: 10.1089/tmj.2021.0356
66. Eyllon M, Barnes JB, Daukas K, Fair M, Nordberg SS. The impact of the COVID-19-related transition to telehealth on visit adherence in mental health care: an interrupted time series study. Adm Polic Ment Heal Ment Heal Serv Res. (2022) 49(3):453–62. doi: 10.1007/s10488-021-01175-x
67. Abraham A, Jithesh A, Doraiswamy S, Al-Khawaga N, Mamtani R, Cheema S. Telemental health use in the COVID-19 pandemic: a scoping review and evidence gap mapping. Front Psychiatry. (2021) 12:748069. doi: 10.3389/fpsyt.2021.748069
68. Miller KA, Hitschfeld MJ, Lineberry TW, Palmer BA. How does active substance use at psychiatric admission impact suicide risk and hospital length-of-stay? J Addict Dis. (2016) 35(4):291–7. doi: 10.1080/10550887.2016.1177808
69. Gopalakrishna G, Ithman M, Malwitz K. Predictors of length of stay in a psychiatric hospital. Int J Psychiatry Clin Pr. (2015) 19(4):238–44. doi: 10.3109/13651501.2015.1062522
70. Duden GS, Gersdorf S, Stengler K. Global impact of the COVID-19 pandemic on mental health services: a systematic review. J Psychiatr Res. (2022) 154:354–77. doi: 10.1016/j.jpsychires.2022.08.013
Keywords: COVID-19, hospitalizations, health services, mental health, substance use, length of stay
Citation: Russolillo A, Carter M, Guan M, Singh P, Kealy D and Raudzus J (2024) Adult psychiatric inpatient admissions and length of stay before and during the COVID-19 pandemic in a large urban hospital setting in Vancouver, British Columbia. Front. Health Serv. 4:1365785. doi: 10.3389/frhs.2024.1365785
Received: 4 January 2024; Accepted: 1 May 2024;
Published: 14 May 2024.
Edited by:
Fraser Gaspar, Mitre, United StatesReviewed by:
Alex Wu, Mitre, United States© 2024 Russolillo, Carter, Guan, Singh, Kealy and Raudzus. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Angela Russolillo, YXJ1c3NvbGlsbG8xQHByb3ZpZGVuY2VoZWFsdGguYmMuY2E=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.