- 1Division of Healthcare Engineering, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 2Division of Acute Care Surgery, Department of Surgery, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 3Department of Surgery, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 4Department of Radiation Oncology, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 5UNC Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 6School of Information and Library Science, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
Given the persistent safety incidents in operating rooms (ORs) nationwide (approx. 4,000 preventable harmful surgical errors per year), there is a need to better analyze and understand reported patient safety events. This study describes the results of applying the Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) supported by the Teamwork Evaluation of Non-Technical Skills (TENTS) instrument to analyze patient safety event reports at one large academic medical center. Results suggest that suboptimal behaviors stemming from poor communication, lack of situation monitoring, and inappropriate task prioritization and execution were implicated in most reported events. Our proposed methodology offers an effective way of programmatically sorting and prioritizing patient safety improvement efforts.
1 Introduction
Adverse events in operating rooms (ORs) can cause physical, emotional, and financial harm. The OR is a highly complex and variable environment, and errors may arise via systems, individuals, equipment, or any combination of these factors (1). Hospital-wide voluntary patient safety event reporting systems have been developed and implemented to document and learn from these events and are essential tools for error and harm reduction (2). These systems are useful for ascertaining root causes and contributing factors associated with near-misses, unsafe work conditions, and actual patient harm (2).
Non-technical skills such as communication, leadership, situation monitoring, and mutual support are needed in successful clinical interactions and, when neglected or improperly used, can contribute to patient safety events (3, 4). Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) is a robust framework for evaluating such skills. TeamSTEPPS is supported by the Teamwork Evaluation of Non-Technical Skills (TENTS) instrument for analyzing corresponding safety behaviors (5).
This study describes the results of an innovative study applying the TeamSTEPPS framework and TENTS instrument analysis to patient safety event reports at one large academic medical center to identify potential contributing behavioral factors.
2 Methods
Our academic medical center has an internal event reporting system available to all employees. It can be accessed via a web-based portal on all hospital computers or a link within our electronic health record. Employees are encouraged to report all patient safety events (e.g., harm events, near misses, unsafe work conditions). 873 reports submitted from 6 to 1-22 to 11-30-22 were reviewed. Among these, 296 reports related to the OR or perioperative areas were de-identified for further review. Discrete data extracted from each report included (i) date of the event, (ii) location within the hospital, (iii) operating service, and (iv) pre-established event type (i.e., process issues, anesthesia/pharmacy complication, count discrepancy, etc.).
Two independent reviewers received rigorous TeamSTEPPS training and a guided instruction for using the TENTS instrument (Table 1) with clinical examples. Both reviewers read each report, established frequencies for each pre-established event category in the risk management database and identified suboptimal behaviors associated with the analyzed event. Once completed, reviewers discussed and reconciled any discrepancies. If conflicts persisted, a third reviewer evaluated the data and made a final decision for the TENTS instrument analysis. The collected data was grouped and sorted based on the frequency, event category, and TENTS behaviors, with associated descriptive statistics. A data visualization chart was constructed to better understand the relationship between report category frequency and the number of contributing unique TENTS behaviors. Axes were divided in half so that each point could be grouped and studied for patterns.

Table 1. TENTS Instrument behaviors with numbering, grouped by broad behavior category based on the TeamSTEPPS framework.
3 Results
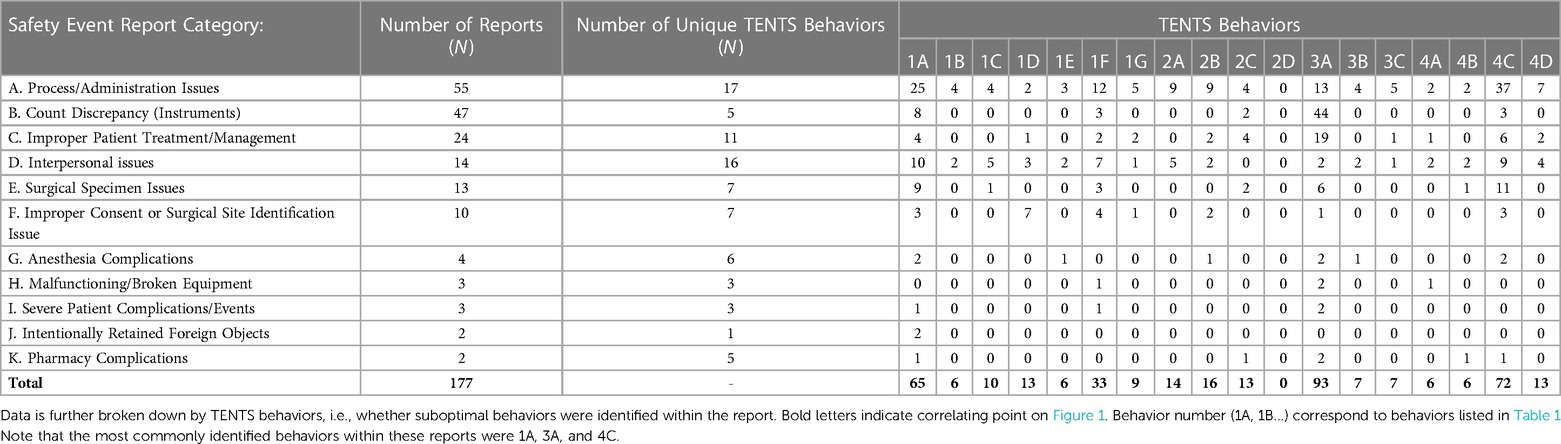
Of the 296 events related to the OR and perioperative areas, 177 had clearly described suboptimal behaviors identified within the report. Table 2 provides a breakdown based on adverse event category and unique TENTS behaviors. Figure 1 provides the data visualization chart summarizing the data into four quadrants, as shown.
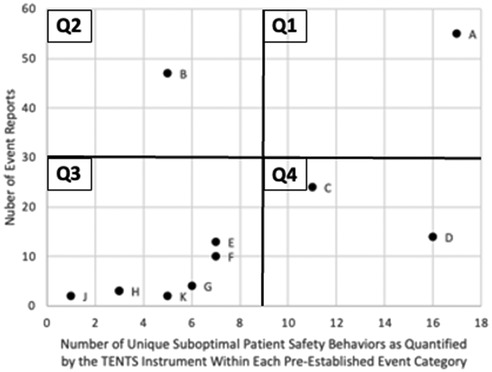
Figure 1. Data visualization chart. Each point represents one category of safety event reports (Table 2). Quadrants were created to compare categories based on volume of reports within the category and frequency of TENTS behaviors identified. For our analyses, axes were arbitrarily cut in half based on final charting of the data.
The three most common suboptimal behaviors contributing to adverse patient safety events among all reports were (i) “communicates and receives information appropriately” (1A: N = 65), (ii) “pays attention to surroundings/environment” (3A: N = 93), and (iii) “accomplishes and prioritizes tasks appropriately” (4C: N = 92), and the least common suboptimal behavior was “instructs as appropriate to the situation” (2D: N = 0). The most common adverse patient safety event categories were (i) Process/Administration Issues (N = 55) and (ii) Count Discrepancy (N = 47), and the least common patient safety events were (i) Intentionally Retained Foreign Objects (N = 2), and (ii) Pharmacy Complication (N = 2) (see Table 2 for breakdown by each category and TENTS behavior).
The most frequent type of event with coupled (many identified, N = 17) suboptimal behaviors was Process/Administration issues (Q1: top-right quadrant in Figure 1). The most frequent type of event with isolated (few identified, N = 5) suboptimal behaviors was Count Discrepancy (Instruments) (Q2: top-left quadrant in Figure 1). The least frequent type of event with isolated (N = 1) suboptimal behaviors was intentionally retained Foreign Objects (Q3: bottom-left quadrant in Figure 1). The least frequent type of event with coupled (N = 16) suboptimal behaviors was Interpersonal Issues (Q4: bottom-right quadrant in Figure 1).
4 Discussion
Results suggest that the TeamSTEPPS framework and TENTS instrument can be effectively used to analyze potential contributing behavioral factors to reported patient safety events. We constructed and visually displayed four quadrants that can aid healthcare leaders and patient safety improvement professionals in learning from our proposed analysis. The three dominant suboptimal behaviors contributing to patient safety events were (i) suboptimal communication, (ii) lack of situation awareness, and (iii) inappropriate task prioritization and execution. Below, we discuss possible learnings from each quadrant in Figure 1.
4.1 Q1: coupled suboptimal behavior(s) responsible for high-frequency safety events
Q1 in Figure 1 represents administrative based events that are primarily based on behaviors that are highly coupled (e.g., influence each other) and occur at a high frequency. While most of these events in our data set did not lead to patient harm, they could prove to be challenging to address as they involve many procedural tasks that require many operations and behaviors to go as planned (e.g., scheduling, cleaning and prepping ORs between cases, receiving prior authorizations for procedures). Thus, given the complexity of such operational issues, hospital leaders and improvement professionals could invest in programmatic systems and process improvement efforts to eliminate such inefficiencies and waste (e.g., optimization of handovers, projects to continuously eliminate waste from the system). Examples of such improvement efforts can be found in the works by Breuer (6) and Meretoja (7).
4.2 Q2: isolated suboptimal behavior(s) responsible for high-frequency safety events
Q2 in Figure 1 represents patient safety events primarily based on isolated behaviors that occur at a high frequency. In our data set these events are represented by errors related to the surgical count of instruments and soft goods, with the most frequent contributing behavior being the lack of situational awareness. Therefore, a targeted effort to establish and implement a safety barrier, which by high reliability standards is highly standardized, robust, and effective, for instruments and soft good count could be spearheaded. Examples of such improvement efforts can be noted in the works by Mullins (8), Duggan (9) and Loftus (10).
4.3 Q3: isolated suboptimal behavior(s) responsible for low-frequency safety events
Patient safety events within Q3 are rare and have few suboptimal behaviors implicated. The low frequency of these events might cause organizations to place little urgency on addressing such issues. However, most events in this quadrant are unfortunately associated with patient harm and, as such, are often the most severe and undergo official root-cause analysis (RCA) procedures. Interestingly, our data suggest that these events are driven mainly by the same three dominant behaviors (suboptimal communications, lack of situational awareness, and inappropriate task prioritization) and are often rooted in the lack of psychological safety to speak up when complications arise. Thus, efforts to improve soft skills (e.g., teamwork, communication, and psychological safety) could be the most relevant to deal with such events. Our recommendations are in alignment with the prior research of Mishra (11) and Gillespie (12).
4.4 Q4: coupled suboptimal behaviors responsible for low-frequency safety events
Patient safety events within Q4 are rare but have many suboptimal behaviors implicated. Most events in this quadrant are based on interpersonal conflicts and improper patient treatment and management and point to interpersonal issues that are more nuanced than suboptimal behaviors alone, thus often requiring the assistance of executive leadership and human resources professionals to intervene. Focus on organizational values (e.g., trust, culture, accountability) and corrective actions seems most relevant as means to deal with such cases. Examples of such improvement efforts can be found in works by Brenner (13) and Bleakley (14).
We recognize that all patient safety events are important and require organizational attention. When deciding which events to address first, a decision-making process is needed. Our proposed methodology offers one possible way of sorting and prioritizing patient safety efforts programmatically. One potential complication of utilizing our proposed methodology is the underreporting of patient safety events, which is a known drawback of event reporting systems (15–17). It is also crucial to employ practical categorization of reports, which would offer insight based on event type frequency and coupling of suboptimal behaviors. There is also potential for bias in interpreting patient safety behaviors while applying the TENTS instrument. Our study offset this possibility by using two independent reviewers for each report and a third reviewer to resolve conflicts.
Patient safety event reporting systems can be analyzed to determine the role of suboptimal behaviors in safety events. At one large academic medical institution, suboptimal behaviors stemming from poor communication, lack of situation monitoring, and inappropriate task prioritization and execution were implicated in most reported events. Strategic and targeted interventions can be designed to reduce the frequency of specific suboptimal behaviors and events, and it is vital to consider the effort of implementing an intervention and the impact of selected interventions on reducing patient harm and improving the culture of patient safety.
Data availability statement
The dataset will not be available as it includes sensitive safety event reporting information that cannot be anonymized with regard to the institution. Requests to access the datasets should be directed tobHVrYXN6X21henVyQG1lZC51bmMuZWR1.
Ethics statement
The studies involving humans were approved by University of North Carolina at Chapel Hill Institutional Review Board (IRB). The studies were conducted in accordance with the local legislation and institutional requirements. The Ethics Committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because Participants gave verbal consent prior to participation, as required by IRB approval.
Author contributions
CM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. LB: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Writing – review & editing. AH: Conceptualization, Data curation, Writing – review & editing. JR: Conceptualization, Supervision, Writing – review & editing. KA: Writing – review & editing. CG: Writing – review & editing. LM: Writing – review & editing. TI: Writing – review & editing. LM: Conceptualization, Formal Analysis, Funding acquisition, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article.
Funding provided by Innovate Carolina.
Acknowledgments
We would like to thank the UNC Office of Quality Excellence and the UNC Health Well-Being Program for their support in this effort.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Krizek TJ. Surgical error: ethical issues of adverse events. Arch Surg. (2000) 135(11):1359–66. doi: 10.1001/archsurg.135.11.1359
2. Howe JL, Hettinger AZ, Ratwani RM. Using patient safety-event report data to assess health-IT safety: benefits and challenges. Lancet Digit Health. (2019) 1(3):e104–5. doi: 10.1016/S2589-7500(19)30060-3
3. Keebler JR, Dietz AS, Lazzara EH, Benishek LE, Almeida SA, Toor PA, et al. Validation of a teamwork perceptions measure to increase patient safety. BMJ Qual Saf. (2014) 23(9):718–26. doi: 10.1136/bmjqs-2013-001942
4. TeamSTEPPS 3.0 | Agency for Healthcare Research and Quality. Available online at: https://www.ahrq.gov/teamstepps-program/index.html (cited August 28, 2023).
5. Lin W-T, Lee B-O, Mayer C. Validity and reliability of the teamwork evaluation of non-technical skills tool. Aust J Adv Nurs. (2019) 36(3):29–38.
6. Breuer RK, Taicher B, Turner DA, Cheifetz IM, Rehder KJ. Standardizing postoperative PICU handovers improves handover metrics and patient outcomes. Pediatr Crit Care Med. (2015) 16(3):256–63. doi: 10.1097/PCC.0000000000000343
7. Meretoja A, Strbian D, Mustanoja S, Tatlisumak T, Lindsberg PJ, Kaste M. Reducing in-hospital delay to 20 min in stroke thrombolysis. Neurology. (2012) 79(4):306–13. doi: 10.1212/WNL.0b013e31825d6011
8. Mullins BT, McGurk R, McLeod RW, Lindsay D, Amos A, Gu D, et al. Human error bowtie analysis to enhance patient safety in radiation oncology. Pract Radiat Oncol. (2019) 9(6):465–78. doi: 10.1016/j.prro.2019.06.022
9. Duggan EG, Fernandez J, Saulan MM, Mayers DL, Nikolaj M, Strah TM, et al. 1,300 Days and counting: a risk model approach to preventing retained foreign objects (rfos). Jt Comm J Qual Patient Saf. (2018) 44(5):260–9. doi: 10.1016/j.jcjq.2017.11.006
10. Loftus T, Dahl D, OHare B, Power K, Toledo-Katsenes Y, Hutchison R, et al. Implementing a standardized safe surgery program reduces serious reportable events. J Am Coll Surg. (2015) 220(1):12–17.e3. doi: 10.1016/j.jamcollsurg.2014.09.018
11. Mishra A, Catchpole K, Dale T, McCulloch P. The influence of non-technical performance on technical outcome in laparoscopic cholecystectomy. Surg Endosc. (2008) 22(1):68–73. doi: 10.1007/s00464-007-9346-1
12. Gillespie BM, Chaboyer W, Longbottom P, Wallis M. The impact of organisational and individual factors on team communication in surgery: a qualitative study. Int J Nurs Stud. (2010) 47(6):732–41. doi: 10.1016/j.ijnurstu.2009.11.001
13. Brenner MJ, Boothman RC, Rushton CH, Bradford CR, Hickson GB. Honesty and transparency, indispensable to the clinical mission-part I: how tiered professionalism interventions support teamwork and prevent adverse events. Otolaryngol Clin North Am. (2022) 55(1):43–61. doi: 10.1016/j.otc.2021.07.016
14. Bleakley A, Allard J, Hobbs A. Towards culture change in the operating theatre: embedding a complex educational intervention to improve teamwork climate. Med Teach. (2012) 34(9):e635–40. doi: 10.3109/0142159X.2012.687484
15. Shojania KG, Thomas EJ. Trends in adverse events over time: why are we not improving? BMJ Qual Saf. (2013) 22(4):273–7. doi: 10.1136/bmjqs-2013-001935
16. Chamberlain CJ, Koniaris LG, Wu AW, Pawlik TM. Disclosure of “nonharmful” medical errors and other events: duty to disclose. Arch Surg. (2012 Mar) 147(3):282–6. doi: 10.1001/archsurg.2011.1005
Keywords: patient safety, safety event, event reporting, TeamSTEPPPS, operating room, surgical error, communication, TENTS
Citation: Mitchell C, Butler L, Holloway AD, Ra JH, Adapa K, Greenberg C, Marks LB, Ivester T and Mazur L (2024) Analysis of patient safety event report categories at one large academic hospital. Front. Health Serv. 4:1337840. doi: 10.3389/frhs.2024.1337840
Received: 13 November 2023; Accepted: 26 February 2024;
Published: 2 April 2024.
Edited by:
Helen Higham, University of Oxford, United KingdomReviewed by:
Hilde Valen Waehle, Haukeland University Hospital, NorwayJanet C. Long, Macquarie University, Australia
© 2024 Mitchell, Butler, Holloway, Ra, Adapa, Greenberg, Marks, Ivester and Mazur. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lukasz Mazur bHVrYXN6X21henVyQG1lZC51bmMuZWR1
 Cody Mitchell
Cody Mitchell Logan Butler1
Logan Butler1 Karthik Adapa
Karthik Adapa Lawrence B. Marks
Lawrence B. Marks