- 1Department of Community Health and Health Behavior, School of Public Health and Health Professions, University at Buffalo, Buffalo, NY, United States
- 2Department of Anthropology, College of Arts and Sciences, University at Buffalo, Buffalo, NY, United States
- 3Department of Family Medicine, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, NY, United States
- 4Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
Objectives: The Veggie Van model is a mobile market model that is efficacious in increasing fruit and vegetable consumption for lower-income participants. The model is currently being evaluated for its effectiveness in a multi-state trial. Preliminary implementation data, collected through process measures surveys and implementation interviews, indicate that there are several barriers to implementation among partner organizations and implementation fidelity to the Veggie Van model was low. Consideration and planning for implementation ought to occur early and often throughout the research process order to ensure Veggie Van model effectiveness. This paper describes the step-by-step process for creating strategies to enhance implementation of Veggie Van model components.
Methods: Implementation mapping is a systematic process to develop implementation strategies through engagement with key stakeholders. We conducted a series of interviews (n = 31 representatives) with partner organizations (n = 8) to identify facilitators and barriers to Veggie Van model implementation. We then applied interview findings to an Implementation Mapping process to develop theory and practice-driven strategies to be integrated into existing implementation tools and technical assistance.
Results: We identified implementation outcomes (e.g., staff implement the Veggie Van model component of nutrition education with fidelity) and performance objectives (e.g., offer nutrition education, in the form of food lessons and/or food demonstrations, at least bi-weekly) to achieve them. We conducted a secondary qualitative analysis of the findings from implementation interviews with partner organizations to identify behavioral determinants (e.g., attitudinal beliefs, social support) which were combined with the performance objectives to generate change objectives (e.g., view the Veggie Van model as advantageous to an organization and communities served). To achieve the change objectives, we developed implementation strategies that would be integrated into existing Veggie Van training resources including an online toolkit, webinars and trainings, an annual mobile market conference, and technical assistance.
Conclusion: The development of theory and practice-driven implementation strategies will enable us to improve our implementation tools, thereby improving fidelity to the Veggie Van model among organizations and increasing the likelihood of its effectiveness. Detailing the design of a multifaceted implementation strategy using Implementation Mapping also provides a model to design similar strategies for other community-based interventions.
1 Introduction
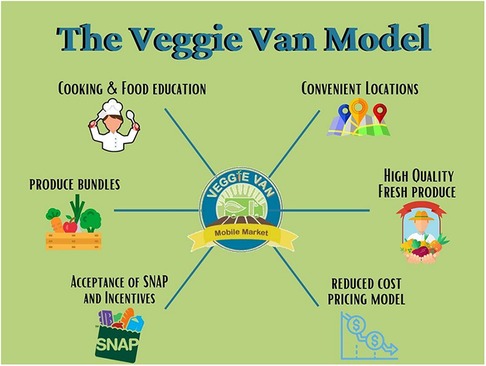
Veggie Van is an evidence-based model for mobile produce markets informed by Social Cognitive Theory and designed to address the multiple dimensions of access to fresh fruits and vegetables (F&V) for lower-income and underserved communities: acceptability, availability, affordability, accessibility, and accommodation (1). The Veggie Van intervention (mobile market following. the Veggie Van model) was tested in a 12-site cluster randomized controlled trial and found to be efficacious in increasing F&V consumption for lower-income participants over a 6-month period. Compared to study participants living in control communities, participants in communities that received access to the Veggie Van experienced a .95 cups/day greater change (p = 0.005) in F&V consumption at follow-up (2). Intervention participants also reported increases in self-efficacy for preparing and incorporating fresh F&V into meals and snacks (2). Figure 1 illustrates the six core components of the Veggie Van model, which include: (1) operating the mobile market at convenient locations that are selected based on strong partnerships with community-based organizations already working with the intended population of low-income families, (2) operate the mobile market regularly (e.g., weekly visits to the same location), (3) selling reduced cost fresh F&V through a combination of locally competitive pricing and participation in F&V incentive programs, (4) offering a variety of fresh, high quality F&V (e.g., prioritizing local produce), (5) encouraging F&V purchasing by offering and incentivizing bundles of produce (multiple items for a set price), and (6) offering regular nutrition education (e.g., cooking demonstrations, nutrition lessons) (1, 2). Although not a core component of the model, organizations that implement a Veggie Van intervention are encouraged to maintain consistent access for customers by operating at least 10–12 months out of the year.
An ongoing hybrid effectiveness-implementation study seeks to determine if the Veggie Van intervention impact F&V intake and other health-related outcomes in underserved communities when implemented by community organizations in multiple contexts. This 7-year study, known as the Veggie Van Study, also aims to understand how easy or hard it is for organizations to implement the Veggie Van model. Nine study partner organizations across several states in the Eastern U.S. were identified through a request-for-partners (RFP) process; details regarding the recruitment process and effectiveness study methods are reported elsewhere (3, 4). Briefly, partner organizations were provided funding to start or expand mobile market operations following the Veggie Van model for 12 months (4). Partner organizations were asked to partner with community sites serving lower-income areas to help host their mobile market and facilitate recruitment for the study (4). Representatives from each organization had access to a web-based Veggie Van toolkit and regular contact (i.e., email, web conference) with the study team to receive ongoing support for study activities and implementation of the Veggie Van model. Preliminary implementation data, collected through process measures surveys and implementation interviews, indicate that implementation fidelity to the Veggie Van model components among initial study partner organizations is low and there are persistent barriers to implementation (5). For example, although organizations successfully launched or expanded their mobile market operations, partners often did not implement all of the key components of the model (e.g., produce bundles) or at the recommended intensity (e.g., weekly). Therefore, there is a need to develop strategies to enhance implementation of the Veggie Van model components. Implementation strategies are approaches to enhance the adoption and implementation of evidence-based practices (6–8), but available implementation strategies to enhance healthy eating interventions have mainly been employed and tested in school and childcare settings. Furthermore, there is a lack of rigorous and theory-driven design of these strategies (9). Implementation mapping is a form of intervention mapping that guides planners through a systematic process to develop implementation strategies through engagement with key stakeholders (e.g., adopters, implementers) (9, 10). Implementation mapping has been used by several studies, but there is a recognized lack of description, justification, and use of theory in designing implementation strategies for public health interventions (6, 9–11). The goal of this paper is to add to the literature by describing our process of utilizing Implementation Mapping to design new implementation strategies for the Veggie Van intervention. Illustrating the step-by-step process of designing a multifaceted implementation strategy will provide a template for others to similarly design strategies for implementation of community-based evidence-based interventions. Strategies developed from this process will also be used to facilitate implementation of Veggie Van interventions among current and future study partners as well as prepare the model to go to scale and be implemented by practitioners more broadly. These strategies will also be used by the Veggie Van Training Center, a service center based at the University at Buffalo that supports community-based organizations to start mobile produce markets and related food access programs. The Veggie Van Training Center currently employs several implementation methods including the Veggie Van toolkit, a cohort-style course known as Mobile Market 101 (MM101), a webinar series on special topics, ongoing technical assistance, and individualized consulting. Therefore, the strategies developed from the Implementation Mapping process are intended to inform updates to these existing tools.
2 Methods
We carried out an Implementation Mapping process to design implementation strategies; our process was modeled after the methods of Fernandez and colleagues (9). Implementation mapping involves five tasks: (1) conduct an implementation needs assessment, (2) identify adoption and implementation outcomes, performance objectives, determinants, and change objectives, (3) select theoretical methods and design implementation strategies, (4) produce implementation protocols and materials, and (5) evaluate implementation outcomes. Each task we conducted is outlined in the results section; briefly, for task one, we conducted implementation interviews with representatives from organizations participating in the Veggie Van effectiveness-implementation study. Task two involved a brainstorm session among key members of the Veggie Van research team. The lead and second authors conducted a literature review and engaged in several brainstorm sessions, with input from the Veggie Van Training Center team, for the third task. Tasks four and five are forthcoming. The interviews conducted as part of task one were approved as exempt research by the University at Buffalo Institutional Review Board Study.
2.1 Theoretical framework
The Consolidated Framework for Implementation Research (CFIR) informed both the data collection and analysis processes used to identify contextual factors that impact implementation of the Veggie Van model. CFIR is an implementation determinants framework developed in 2009 by Damschroder and colleagues in response to a call for a greater use of theory to guide implementation research (12, 13). CFIR is comprised of 39 constructs within five major domains that interact to influence implementation of programs and interventions and their eventual effectiveness (12).
3 Results
3.1 Task 1: Conduct an implementation needs assessment
Qualitative data collected through implementation interviews were used for an implementation needs assessment. Interviews were conducted with representatives from eight Veggie Van study partner organizations who were implementing the Veggie Van intervention. Each organization was asked to identify the individuals who most closely engage in the implementation of Veggie Van to participate in two 90-minute semi-structured interviews. Up to four representatives from each organization were invited to participate in implementation interviews at baseline (shortly before or after market launch) and follow-up (9–12 months post market launch), to understand their experience implementing the Veggie Van intervention.
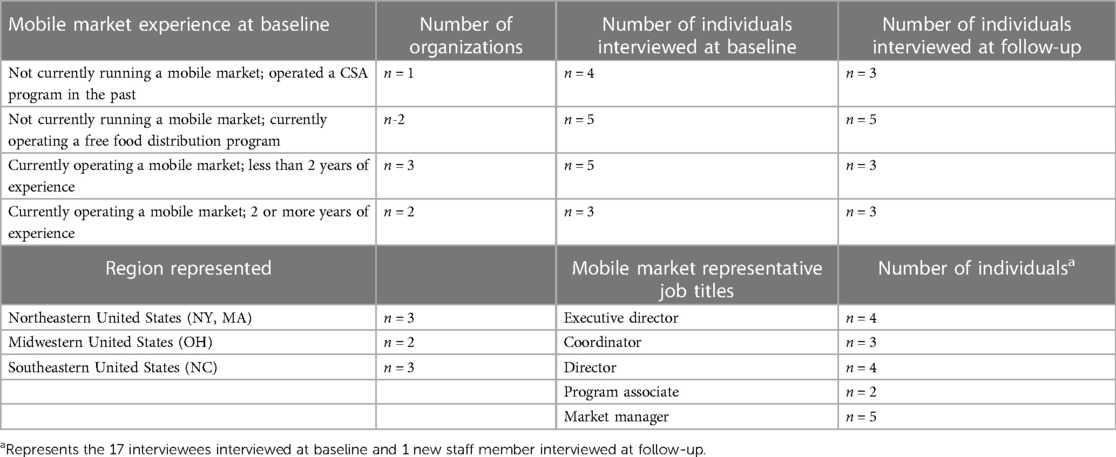
Seventeen representatives from eight study partner organizations completed baseline implementation interviews and fourteen representatives from six organizations completed follow-up interviews. Due to staff turnover, thirteen individuals were interviewed at both timepoints, and one new staff member was interviewed at follow-up. Table 1 presents the experience level of participating organizations and the number and characteristics of interviewees at baseline and follow-up. Each partner organization received compensation for participating in the larger RCT study. Interviews were completed as a part of interviewees' job function; thus, they did not receive additional compensation. Representatives that participated in a baseline interview but left the partner organization prior to follow-up and were still willing to participate in the follow-up interview were compensated with a $50 gift card for each hour they were interviewed.
Semi-structured interview guides, informed by CFIR, were used for data collection. Relevant CFIR constructs were selected from the 39 measures in the 5 domains of CFIR (characteristics of intervention, outer setting, inner setting, characteristics of individuals, and process). Identification of the most salient constructs for inclusion in the interview guide was guided by our past research with 21 key informants representing established mobile market organizations across the US; findings from that formative work highlighted persistent operational challenges faced by organizations across the US that may undermine implementation of an evidence-based intervention (e.g., the Veggie Van model) (14). The final interview guides focused on the following CFIR constructs: relative advantage, adaptability, complexity, design quality and packaging, cost, external policy and incentives, customer needs and resources, cosmopolitanism, peer pressure, structural characteristics, implementation climate, readiness for implementation, knowledge and beliefs about the intervention, self-efficacy, planning, engaging, and executing. Both interview guides were designed to understand the factors in each organization that either enhance or impede implementation of Veggie Van model components.
Interviews were recorded and transcribed; transcripts were data cleaned for errors and inconsistencies. Qualitative data analysis was completed using the software ATLAS.ti version 8.0. Baseline and follow-up interview data were coded by two independent coders (CK & AC). Each coder analyzed all interview transcripts separately. The first phase of coding involved an inductive organization of data utilizing open coding to identify barriers and facilitators to implementation (15). A second phase of coding involved a deductive organization of interview data (baseline and follow-up) into the 5 domains of CFIR (e.g., inner setting) (12, 15). The creation and iterative refinement of a codebook throughout the coding process allowed for themes across codes to be combined into inductive subcategories (e.g., funding and resources) (15). Regular meetings between coders involved discussion and updates to the codebook throughout the coding process. Coding of baseline interviews was completed first and the codebook generated from that coding process was utilized for subsequent coding of the follow-up interviews, but continual updating and refinements occurred during the coding of follow-up data. Baseline and follow-up data were coded with the same analytical approach, but we iteratively updated the codebook to reflect additional CFIR constructs that were added to the follow-up interview guide. All coded baseline and follow-up data were ultimately merged into one project bundle and the coders met to reconcile coding differences. Reports and queries were generated for facilitators and barriers, for each CFIR construct, across all partner organizations. Memos were written to summarize each code report and query.
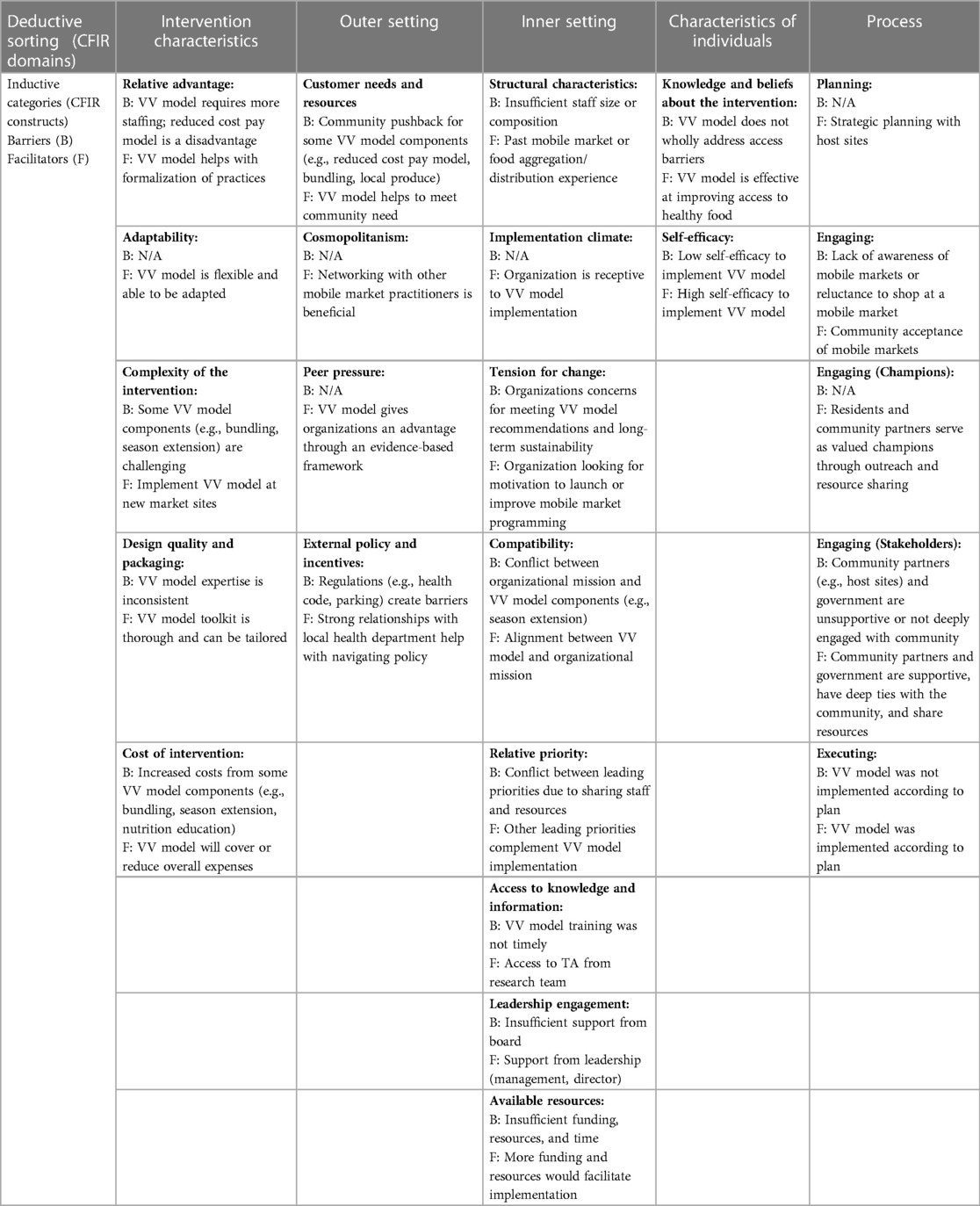
In our analysis, we identified barrier and facilitators to implementation that fall under the following CFIR constructs and sub-constructs: intervention characteristics (subconstructs: relative advantage, adaptability, complexity, design quality and packaging, and cost), outer setting (subconstructs: customer needs and resources, cosmopolitanism, peer pressure, and external policy and incentives), inner setting (subconstructs: structural characteristics, implementation climate, and readiness for implementation), and characteristics of individuals (subconstructs: knowledge and beliefs about the intervention and self-efficacy), and process (subconstructs: planning, engaging, and executing). Facilitators and barriers are presented in Table 2 according to CFIR construct. Our findings indicated that there were perceptions of complexity for implementing the Veggie Van model components, particularly offering produce bundles and extending the season. Perceptions that implementing model components requires more staffing, funding, and organizational capacity were also cited barriers, while advantages such as the Veggie Van model being adaptable and providing an evidence base were identified as facilitators to implementation. Concerns surrounding costs related to implementation was a perceived barrier; conversely, understanding that the Veggie Van model is a more a financially sustainable model than a free food distribution market models was a facilitator. Other barriers included: a perceived conflict between organizational mission and/or community preferences and implementing certain Veggie Van model components (e.g., the Veggie Van interventions is a paid model in contrast with one organization that had been previously implementing a free food distribution model), challenges with navigating external barriers (e.g., restrictive policies, unsupportive partners), lack of planning for implementation, and low or worsening self-efficacy to implement the model and its individual components. Networking with other practitioners implementing the model and specialized training in the Veggie Van model components were identified as facilitators to implementation.
3.2 Task 2: Identify adoption and implementation outcomes, performance objectives, determinants, and change objectives
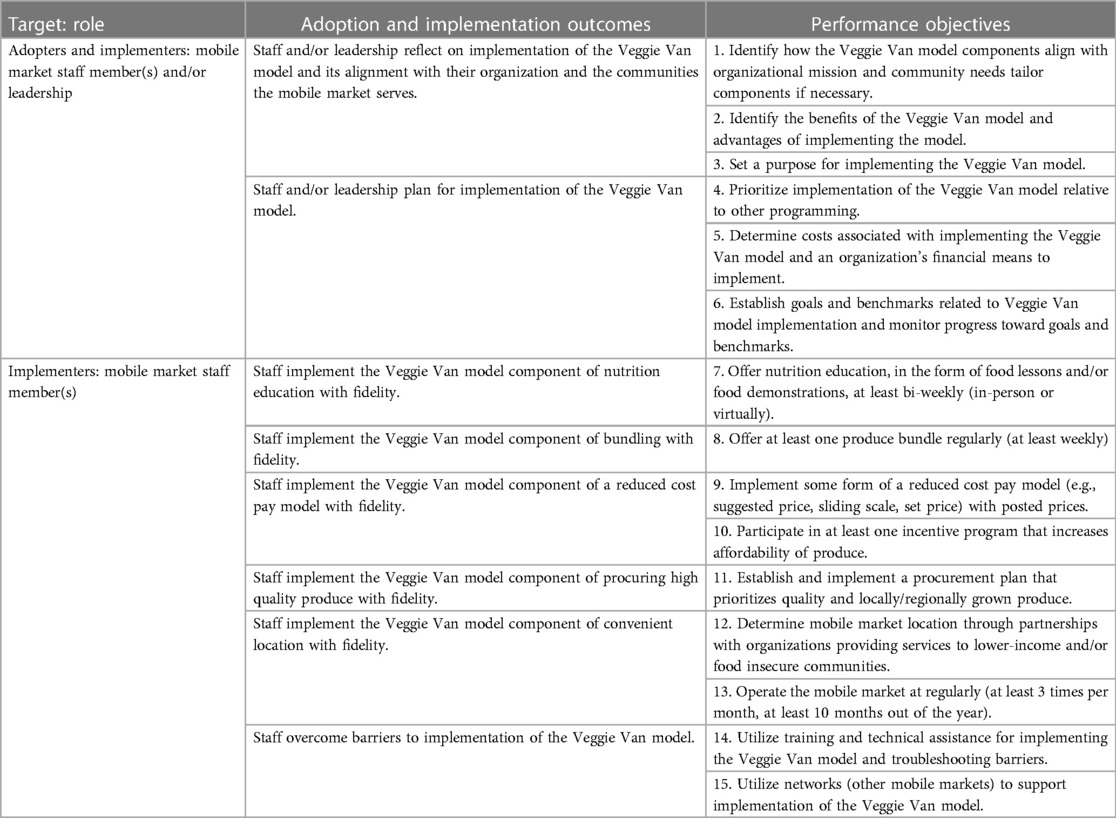
For task two, individuals from the Veggie Van study research team and Veggie Van Training Center that had in-depth knowledge of the Veggie Van model and experience with understanding of mobile market operations participated in a brainstorm session. Drawing on the collective experiences from both research and practice and our findings from the needs assessment (task 1), the planning team drafted adoption outcomes, implementation outcomes, and performance objectives for the implementation of the Veggie Van model. Adoption and implementation outcomes were guided by broader goals of what is considered necessary to achieve prior to implementation (adoption) and during implementation to achieve optimal implementation of the Veggie Van model. Discussion of the specific tasks required to achieve those outcomes guided the selection of performance objectives. Performance objectives answer the question, “What do program [implementers] need to do to deliver the essential program components?” (9). Organizations participating in the Veggie Van Study completed monthly process measures surveys for the study period which assess implementation of each of the Veggie Van model components. Preliminary process measures data indicate that fidelity to the model, including the dose or intensity (e.g., frequency of nutrition education lessons), greatly varies between and within organizations for individual model components; therefore, the granular nature of our performance objectives reflects this variability in implementation. Implementation outcomes and performance objectives were subsequently refined through follow-up email correspondence between group members. Table 3 outlines the final implementation outcomes and performance objectives.
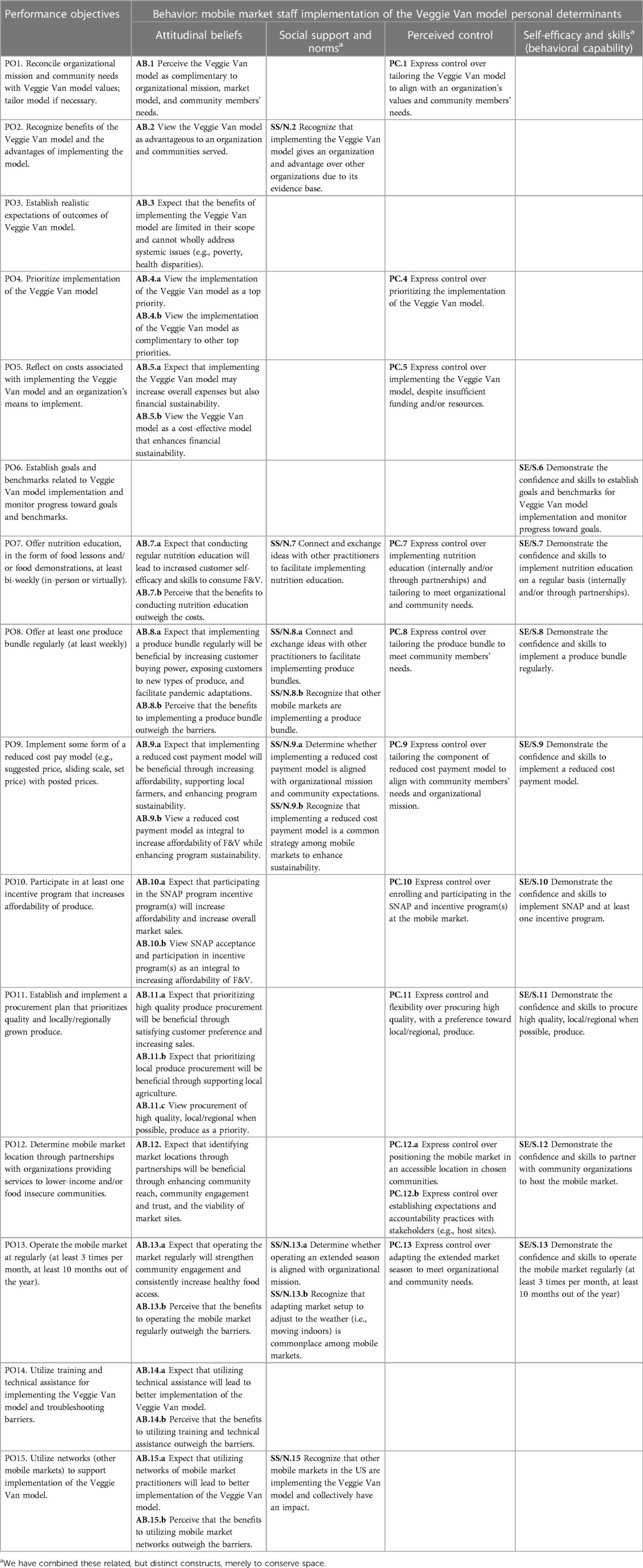
Next, the lead and second authors conducted a secondary qualitative analysis of the findings from the formative work on barriers and facilitators to implementation (needs assessment) to identify determinants. Determinants answer the question, “Why does an individual choose to, or choose not to, implement Veggie Van model components?” (9). The use of health behavior theories such as the social cognitive theory and theory of planned behavior is an accepted practice for intervention mapping, including Implementation Mapping (6, 9, 16). These theories are widely used, psychometrically valid, and reliable in predicting and influencing health behaviors (e.g., cigarette smoking, exercise) through individual-level determinants (16). Constructs and determinants from individual-level theories including social cognitive theory, health belief model theory, and theory of planned behavior were incorporated into a codebook (17–19). Memos were then deductively coded by each author to identify individual level determinants among interviewees (implementers) that were relevant to implementation. The authors met to discuss and reconcile codes; final theories (social cognitive theory, theory of planned behavior, and health belief model) were chosen based on the frequency of determinants represented and some determinants were collapsed into overarching concepts. Many of our aforementioned findings corresponded to the constructs perceived benefits and barriers (health belief model), attitudes (theory of planned behavior), and outcome expectations/expectancies (social cognitive theory). We consolidated these constructs into the overarching determinant of “attitudinal beliefs”. Other constructs that are represented by the findings included social support and norms (theory of planned behavior, social cognitive theory), self-efficacy and skills (social cognitive theory), and perceived control (health belief model) (17–19). Next, a matrix of change was created in which performance objectives are combined with the personal determinants in order to produce change objectives. Change objectives are discrete changes that are required for each relevant determinant that will ideally lead to achieving performance objectives (9). Table 4 is the final matrix of change outlining performance objectives, identified determinants, and change objectives.
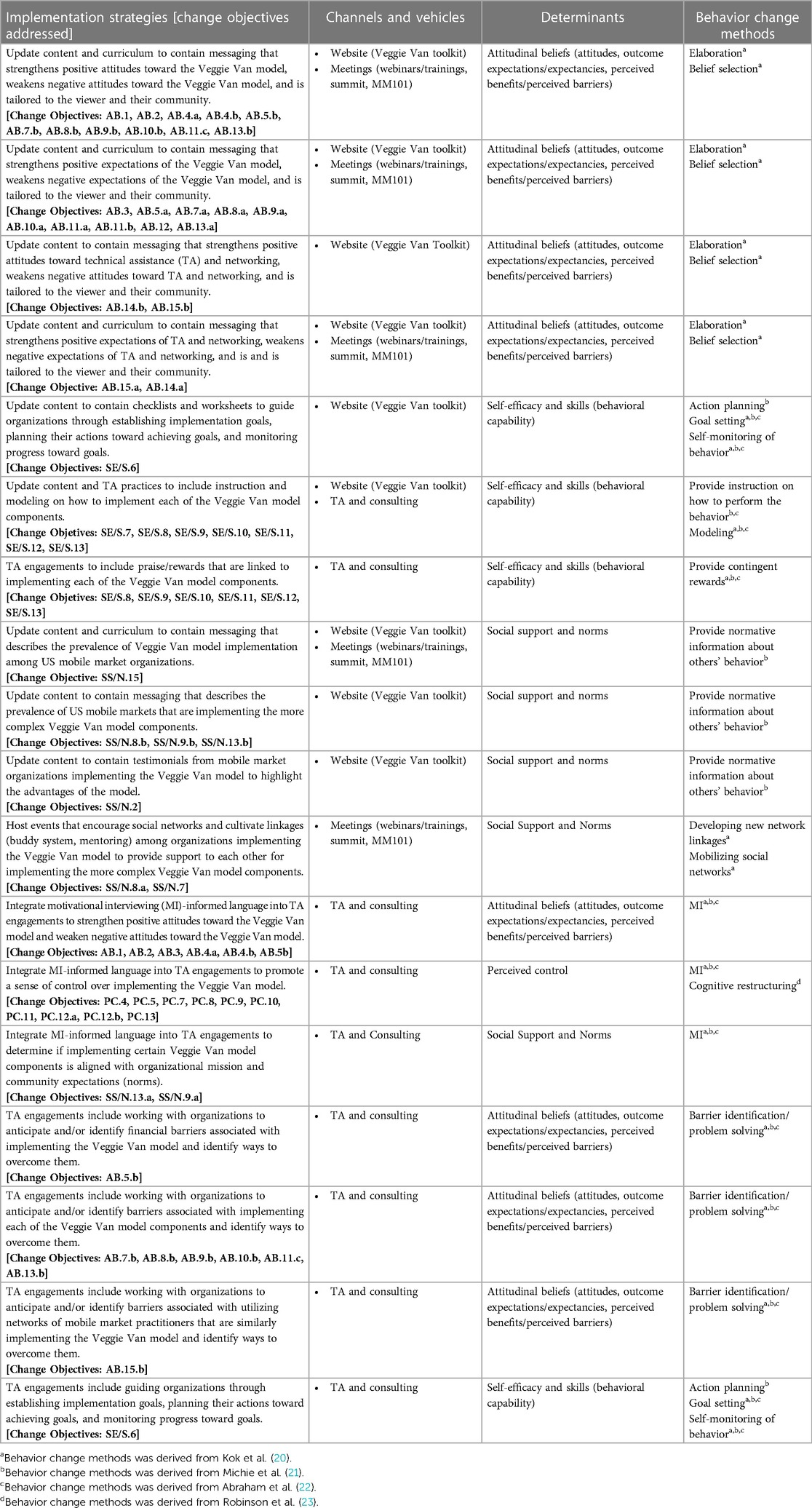
3.3 Task 3: Select theoretical methods and design implementation strategies
A literature review identified taxonomies of theory-based behavior change techniques from Michie et al., Kok et al., and Abraham et al. (20–22). The determinant of perceived control was not represented in these taxonomies, but we identified a textbook on perceived control and behavior change (23). The techniques from this literature were synthesized in a master spreadsheet that outlined each method, definition, and parameters (i.e., conditions necessary for a particular change to be effective); techniques were also organized based on which individual determinant they target. Through discussion among the first and second authors, techniques were primarily chosen based on relevance to the individual determinants that were identified in our needs assessment. For example, the behavior change technique of modeling involves demonstrating a desired action or behavior (e.g., implementing the produce bundle components of the Veggie Van model) and could be employed to target self-efficacy and skills. The choice of behavior change techniques was also guided by practical considerations of what can feasibly be integrated into existing implementation resources and relevance to program implementers. For example, the technique of fear arousal involving presentation of mortality information is not relevant to the context of implementing the Veggie Van model. Furthermore, providing normative information about others' behavior (implementation of the Veggie Van model) is more feasible to incorporate into existing tools compared to mass media role modeling which involves enforcing norms through mass media.
The chosen behavior change techniques informed the design of more tangible implementation strategies. Implementation strategies were drafted by the lead and second author and were finalized after receiving feedback from the planning team. For example, one strategy for the online toolkit is to include instruction on how to implement the Veggie Van model component of a produce bundle which is intended to increase self-efficacy and behavioral capability. Determinants are targeted through multiple methods (i.e., toolkit, training) and many of the strategies target multiple determinants. Table 5 presents the final implementation plan with chosen behavior change methods and corresponding individual determinants that are targeted.
4 Discussion
This research contributes to the field of implementation science through demonstrating our process of using Implementation Mapping to design strategies that can enhance implementation of a food access intervention known as the Veggie Van Model. To our knowledge, this is the first published Implementation Mapping process for a community-based intervention addressing food access and F&V consumption. Implementation Mapping has been conducted overwhelmingly for evidence-based interventions intended for clinical settings; the few examples of Implementation Mapping for community-based interventions have been in fields such as rehabilitation science (24), cancer prevention (25), and physical activity (26). Needs assessments from these Implementation Mapping processes involved quantitative data collection or informal discussion (24, 25); though, one process similarly conducted extensive formative work identifying facilitators and barriers to implementation (26). A strength of this research is that we conducted our needs assessment with 31 representatives from organizations that were actively implementing the Veggie Van model across eight cities that were having mixed success with implementation. The scope of our needs assessment provided a breadth of data with rich detail on facilitators and barriers of implementing the model across unique organizations and communities. Another strength of this research is the usage of the implementation framework CFIR, that has been recommended for the Implementation Mapping process (9). The benefit of utilizing CFIR is that it organized our qualitative findings in a way that allowed us to fully understand the many dimensions of implementation. For example, the benefits of networking among practitioners (CFIR construct: cosmopolitanism) and its impact on implementation of the Veggie Van model were not immediately apparent to our research team until we conducted interviews that were guided by this framework. This research is unique in that implementation tools and resources (i.e., TA, toolkit) were already in place which allowed us to focus on how to augment these existing resources through refining the content and messaging conveyed through these channels. We hope that this approach inspires others to systematically improve their implementation resources in non-clinical settings.
Our implementation interviews (step 1: needs assessment) yielded important factors that help or hinder implementation at levels of the socioecological model beyond the individual. As such, we recognize that even well designed and executed strategies that target the individual implementer may still be limited by these organizational, community, and policy-level constraints. Many of these challenges further validate our past formative work identifying common operational challenges among mobile market organizations (14) and justify the need for further exploration of the interplay between individual and environmental factors. Technical assistance is an effective strategy aimed at building organizational capacity to support implementation (27, 28) and could be viewed as a way of helping organizations overcome barriers at multiple levels including the environment. However, there is opportunity to identify additional strategies to more directly influence the outer spheres of the socioecological model to improve implementation.
This research is not without its limitations. Utilizing active study partner organizations for our needs assessment may bias our findings because these organizations are likely more committed to implementing the Veggie Van model given that it was a requirement of participation in a research study and have greater means to implement due to receiving research funding and technical assistance. However, evaluating implementation among highly invested partners has forged strong relationships between the research team and mobile market organizations which in turn facilitates in-depth and long-term implementation data collection. Conducting future implementation interviews with organizations that are not implementing the Veggie Van model as a requirement of an intervention study would provide context on implementing the model with less support. Finally, a more community-engaged approach could have been employed in this process which could have involved inviting representatives outside of our research lab, namely those that participated in interviews, to contribute to the design of these strategies.
We are currently conducting tasks four and five of the Implementation Mapping process. Task four entails updating all of our implementation tools and protocols based on the strategies outlined here. We have created an implementation intervention protocol for the Veggie Van Training Center, fidelity checklists for technical assistance engagements, and have begun making content edits to the online toolkit. Task five will involve evaluating the impact of our strategies on implementation of the Veggie Van model through interviews and monthly process measures surveys with new cohorts of organizations enrolled in MM101. Outcomes of interest will include adoption and fidelity to the Veggie Van model but also psychosocial determinants. Despite the common use of behavior change techniques in Implementation Mapping, it is unclear whether the application of these techniques and purported mechanisms of action (i.e., individual determinants and constructs) are applicable to implementing behaviors given that the evidence base is rooted in health intentions and behaviors. We hope to help elucidate the role of these determinants among implementers over time and in relation to our implementation strategies through this impending evaluation work. Finally, interviews were mostly conducted with implementers, rather than adopters, and the interview guide was focused on implementation of the Veggie Van model. We recognize that adoption is a distinct but related process to implementation, and we hope to expand our understanding of the factors that influence the decision to initially adopt the Veggie Van model and the progression from adoption to implementation in future research.
5 Conclusion
There is a dearth of evidence-based implementation strategies to enhance the implementation of community-based interventions. Researchers and practitioners that are interested in improving fidelity to similar food access interventions, particularly those with existing implementation tools in place, may benefit from modeling after our process.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This trial is registered under clinicaltrials.gov (NCT04246593). Registered on January 29, 2020.
Ethics statement
The requirement of ethical approval was waived by University at Buffalo Institutional Review Board Study for the studies involving humans because this study was deemed exempt from IRB requiring IRB approval due to minimal to no risk to human subjects. The studies were conducted in accordance with the local legislation and institutional requirements. The Ethics Committee/institutional review board also waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because This study was deemed exempt from IRB requiring IRB approval, including written informed consent, due to minimal to no risk to human subjects.
Author contributions
CK: Writing – original draft, Writing – review & editing, Conceptualization, Methodology, Project administration, Visualization, Formal Analysis. AC: Visualization, Writing – original draft, Writing – review & editing, Formal Analysis. AM: Conceptualization, Methodology, Project administration, Writing – original draft, Writing – review & editing. JT: Writing – original draft, Writing – review & editing. LV: Conceptualization, Writing – original draft, Writing – review & editing. SL: Writing – original draft, Writing – review & editing. AA: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. LL: Conceptualization, Funding acquisition, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This research was funded by National Cancer Institute, grant number 1R37CA215232-01A1. The APC was funded by National Cancer Institute, grant number 1R37CA215232-01A1.
Acknowledgments
The authors want to thank the community partner organizations that have participated thus far in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2024.1288160/full#supplementary-material
References
1. Leone LA, Tripicchio GL, Haynes-Maslow L, McGuirt J, Grady Smith JS, Armstrong-Brown J, et al. A cluster-randomized trial of a mobile produce market program in 12 communities in North Carolina: program development, methods, and baseline characteristics. J Acad Nutr Diet. (2019) 119(1):57–68. doi: 10.1016/j.jand.2018.04.010
2. Leone LA, Tripicchio GL, Haynes-Maslow L, McGuirt J, Grady Smith JS, Armstrong-Brown J, et al. Cluster randomized controlled trial of a mobile market intervention to increase fruit and vegetable intake among adults in lower-income communities in North Carolina. Int J Behav Nutr Phys Act. (2018) 15(1):2. doi: 10.1186/s12966-017-0637-1
3. Leone LA, Kasprzak C, Lally A, Haynes-Maslow L, Vermont LN, Horrigan-Maurer C, et al. A novel process to recruit and select community partners for a hybrid implementation-effectiveness study. Prog Community Health Partnersh. (2023) 17(1):159–71. doi: 10.1353/cpr.2023.0021
4. Vermont LN, Kasprzak C, Lally A, Claudio A, Tumiel-Berhalter L, Haynes-Maslow L, Ammerman A, et al. A randomized controlled trial of a research-tested mobile produce market model designed to improve diet in under-resourced communities: rationale and design for the veggie van study. Int J Environ Res Public Health. (2022) 19(16):9832. doi: 10.3390/ijerph19169832
5. Kasprzak CM. Evaluation of Pre-implementation Capacity and Implementation Effectiveness of an Evidence-Based-Intervention for Mobile Produce Markets (Ph.D.). State University of New York at Buffalo, United States, New York (2022).
6. Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. (2013) 8:139. doi: 10.1186/1748-5908-8-139
7. Powell BJ, Fernandez ME, Williams NJ, Aarons GA, Beidas RS, Lewis CC, et al. Enhancing the impact of implementation strategies in healthcare: a research agenda. Front Public Health. (2019) 7:3. doi: 10.3389/fpubh.2019.00003
8. Powell BJ, McMillen JC, Proctor EK, Carpenter CR, Griffey RT, Bunger AC, et al. A compilation of strategies for implementing clinical innovations in health and mental health. Med Care Res Rev. (2012) 69(2):123–57. doi: 10.1177/1077558711430690
9. Fernandez ME, Ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, et al. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. (2019) 7:158. doi: 10.3389/fpubh.2019.00158
10. Fernandez ME, Ruiter RAC, Markham CM, Kok G. Intervention mapping: theory- and evidence-based health promotion program planning: perspective and examples. Front Public Health. (2019) 7:209. doi: 10.3389/fpubh.2019.00209
11. Davies P, Walker AE, Grimshaw JM. A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations. Implement Sci. (2010) 5(1):14. doi: 10.1186/1748-5908-5-14
12. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. (2009) 4:50. doi: 10.1186/1748-5908-4-50
13. Kirk MA, Kelley C, Yankey N, Birken SA, Abadie B, Damschroder L. A systematic review of the use of the consolidated framework for implementation research. Implement Sci. (2016) 11:72. doi: 10.1186/s13012-016-0437-z
14. Kasprzak CM, Lally A, Schoonover JJ, Gallicchio DR, Haynes-Maslow L, Vermont LN, et al. Operational challenges that may affect implementation of evidence-based mobile market interventions. BMC Public Health. (2022) 22(1):776. doi: 10.1186/s12889-022-13207-8
15. Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs. (2008) 62(1):107–15. doi: 10.1111/j.1365-2648.2007.04569.x
16. Bartholomew Eldredge LK, Markham CM, Ruiter RAC, Fernández ME, Kok G, Parcel GS. Planning Health Promotion Programs: An Intervention Mapping Approach. Hoboken: John Wiley & Sons (2016).
17. Bandura A. Health promotion by social cognitive means. Health Educ Behav. (2004) 31(2):143–64. doi: 10.1177/1090198104263660
18. Ajzen I. The theory of planned behaviour: reactions and reflections. Psychol Health. (2011) 26(9):1113–27. doi: 10.1080/08870446.2011.613995
19. Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. (1988) 15(2):175–83. doi: 10.1177/109019818801500203
20. Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. (2011) 26(11):1479–98. doi: 10.1080/08870446.2010.540664
21. Kok G, Gottlieb NH, Peters GJ, Mullen PD, Parcel GS, Ruiter RA, et al. A taxonomy of behaviour change methods: an intervention mapping approach. Health Psychol Rev. (2016) 10(3):297–312. doi: 10.1080/17437199.2015.1077155
22. Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. (2008) 27(3):379–87. doi: 10.1037/0278-6133.27.3.379
23. Robinson SA, Lachman ME. Perceived control and behavior change: a personalized approach. In: Reich JW, Infurna FJ, editors. Perceived Control: Theory, Research, and Practice in the First 50 Years. New York: Oxford University Press (2016). p. 0.
24. Kang E, Foster ER. Use of implementation mapping with community-based participatory research: development of implementation strategies of a new goal setting and goal management intervention system. Front Public Health. (2022) 10:834473. doi: 10.3389/fpubh.2022.834473
25. Ibekwe LN, Walker TJ, Ebunlomo E, Ricks KB, Prasad S, Savas LS, et al. Using implementation mapping to develop implementation strategies for the delivery of a cancer prevention and control phone navigation program: a collaboration with 2-1-1. Health Promot Pract. (2020) 23(1):86–97. doi: 10.1177/1524839920957979
26. Walker TJ, Kohl HW, Bartholomew JB, Green C, Fernández ME. Using implementation mapping to develop and test an implementation strategy for active learning to promote physical activity in children: a feasibility study using a hybrid type 2 design. Implement Sci Commun. (2022) 3(1):26. doi: 10.1186/s43058-022-00271-9
27. Scott VC, Jillani Z, Malpert A, Kolodny-Goetz J, Wandersman A. A scoping review of the evaluation and effectiveness of technical assistance. Implement Sci Commun. (2022) 3(1):70. doi: 10.1186/s43058-022-00314-1
Keywords: implementation mapping, implementation strategies, dietary intake, mobile produce market, fruits and vegetables, food access
Citation: Kasprzak CM, Canizares A, Lally A, Tirabassi JN, Vermont LN, Lev S, Ammerman AS and Leone LA (2024) Using implementation mapping to refine strategies to improve implementation of an evidence-based mobile market intervention: a study protocol. Front. Health Serv. 4:1288160. doi: 10.3389/frhs.2024.1288160
Received: 4 September 2023; Accepted: 22 January 2024;
Published: 13 February 2024.
Edited by:
Serena Ann Rodriguez, University of Texas Health Science Center at Houston, United StatesReviewed by:
Alexandre Morais Nunes, University of Lisbon, PortugalEunyoung Kang, University of Texas Health Science Center at Houston, United States
© 2024 Kasprzak, Canizares, Lally, Tirabassi, Vermont, Lev, Ammerman and Leone. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christina M. Kasprzak Y21rMjdAYnVmZmFsby5lZHU=
 Christina M. Kasprzak
Christina M. Kasprzak Andy Canizares1
Andy Canizares1 Jill N. Tirabassi
Jill N. Tirabassi Leah N. Vermont
Leah N. Vermont Alice S. Ammerman
Alice S. Ammerman