- 1Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States
- 2Sparkman Center for Global Health, University of Alabama at Birmingham, Birmingham, AL, United States
Introduction: There is limited guidance on strategies for delivering complex global health programs. We synthesized available evidence on implementation strategies and outcomes utilized in the global polio eradication initiative (GPEI) across low and middle-income country (LMIC) settings.
Methods: We nested our scoping review into a literature review conducted as part of a parent study, STRIPE. This review systematically searched PubMed for articles between 1 January 1988 and 25 April 2018 using polio search terms. Strategies from included studies were organized according to the Expert Recommendations for Implementing Change (ERIC) framework, specified using Proctor's framework, and linked to various outcomes (implementation, services delivery, impact).
Results: 152 unique articles fulfilled our inclusion criteria (from 1,885 articles included in the parent study). Only 43 out of the 152 articles described a suitable quantitative study design for evaluating outcomes. We extracted 66 outcomes from the 43 unique studies. Study publication dates ranged from 1989 to 2018 and represented diverse country settings. The most common implementation strategies were developing mechanisms for feedback, monitoring, and evaluation (n = 69); increasing awareness among the population (n = 58); involving stakeholders, workers, and consumers in the implementation efforts (n = 46); conducting workshops (n = 33); using mass media (n = 31); and building robust record systems to capture outcomes (n = 31). Coverage (n = 13) and morbidity (n = 12) were the most frequently identified outcomes, followed by effectiveness (n = 9) and fidelity (n = 6). Feasibility and sustainability were rarely evaluated.
Conclusions: This review provides a catalogue of implementation strategies and outcomes relevant for advancing global health services delivery in LMICs drawing from the GPEI. Implementation strategies reviewed were poorly described and not adequately linked to outcomes. It calls for additional implementation research to unravel the mechanisms of implementation strategies and their effectiveness, and adaptation of the ERIC framework in LMICs.
Background
It can be challenging for public health practitioners to identify implementation strategies that will be the most effective for achieving desired health outcomes, and to determine which strategies may be the most relevant given the characteristics of both the intervention and implementation context. This challenge is exacerbated by a lack of adequate, comparable descriptions of implementation strategies within implementation science literature, and of the contextual barriers and outcomes that these strategies address (1, 2). Many studies fail to elaborate who delivers the implementation strategy, how the strategy is deployed, i.e., the processes or steps involved, the target of the strategy, and the frequency and intensity required for the strategy to be effective (3). Without a clear understanding of these features, practitioners may struggle to appropriately select and evaluate implementation strategies for addressing barriers to and facilitators of change, prioritize empirical evidence on implementation strategies from other contexts, and learn from and adapt evidence-supported implementation strategies to their prioritized issue and context. Researchers and practitioners alike will struggle to translate findings from ongoing disease control efforts into real-world applications. This gap is especially important in low- and middle-income countries where resources may be lacking to conduct locally based large-scale effectiveness studies around implementation strategies, and where actors may benefit from drawing on and adapting evidence from other settings. A synthesis of available evidence on implementation strategies, which seeks to describe how, when, and to what effect implementation strategies may be used is therefore needed.
The Expert Recommendations for Implementing Change (ERIC) framework provides a taxonomy for classifying implementation strategies, covering domains including management and problem-solving, monitoring and evaluation, engagement and capacity building, and communications and advocacy (3). By systematically gathering input on implementation strategies, the ERIC taxonomy provides consensus definitions on implementation strategies relevant to health services delivery. Given the lack of clarity on implementation strategies in the literature, the ERIC framework provides a useful conceptual home for understanding the breadth of implementation strategies utilized in a global program. Still, as the authors acknowledge, because ERIC was developed by and for stakeholders in North America, and drawn largely from high-income country settings, its transferability across contexts and applicability to low and middle-income settings may be limited. In this paper we have leveraged the ERIC framework to systematically describe the implementation strategies deployed for implementing the global polio eradication initiative (GPEI) while reflecting on its fit for global programs.
The GPEI provides a rich landscape for this assessment for several reasons. First, both the longevity and intensity of the initiative have contributed to a proliferation of research focused on the implementation of eradication activities, including the enactment of different implementation strategies, and polio-related health outcomes. Second, as a truly global initiative and one of the largest of its kind (4), the GPEI adopted a global strategy which was applied, and necessarily adapted and refined, across diverse low- and middle-income countries (LMIC) and regional contexts. While the programmatic strategies for the GPEI (i.e., surveillance, routine immunization, supplementary immunization activities, and mop-up campaigns) are conceptually distinct from the implementation strategies utilized to enable them, the global nature of the initiative facilitated multi-country application of implementation strategies, both through the efforts of implementing partners [e.g., WHO, United Nations Children's Fund (UNICEF), Rotary International, the U.S. Centers for Disease Control (CDC), the Bill and Melinda Gates Foundation (BMGF), the CORE group], and through national ministries of health and frontline health workers working in concert with global guidelines, procedures, and tools (5, 6). Thus, the GPEI provides a useful opportunity for assessing and synthesizing empirical evidence on various implementation strategies across diverse contexts, and the factors which may have led to variation in the effectiveness of select strategies, to facilitate the translation of these implementation strategies to other programs and settings.
For our study, implementation strategies are defined as “methods or techniques used to enhance the adoption, implementation, and sustainability of a clinical program or practice” (7, 8) [though, as per Peters et al. (9), we define clinical program or practice to include population-based public health interventions as well as individual clinical interventions]. The goal of this study is to describe the implementation strategies used throughout the Global Polio Eradication Initiative, including the challenges selected strategies were aimed to address and how they were operationalized, and to reflect on the strengths and limitations of available evidence. In the results that follow, we have aimed to synthesize this evidence by categorizing and describing implementation strategies utilized throughout the initiative from 1988-present according to the ERIC framework, the different types of outcomes they influenced, and their impact in diverse LMIC settings.
Methods
Our methodology followed the PRISMA Extension for Scoping Reviews (PRISMA-ScR) (as specified in Supplementary File S1) (10).
Search strategy
We nested our scoping review into a broader literature review of the GPEI conducted as part of a parent study, the Synthesis and Translation of Research and Innovations from Polio Eradication (STRIPE) (6). This review searched the electronic database PubMed for articles between 1 January 1988 (to align with the year the GPEI began) and 25 April 2018, using search terms for polio, and the search strategy and methods are described elsewhere (5). (Supplementary File S2 specifies the search terms used). Given the breadth of peer-reviewed literature on polio eradication implementation activities included in this initial review, we decided to pursue a secondary analysis focused on synthesizing implementation strategies utilized in the effort, and outcomes measured. We retained those articles included in the full text review of the scoping review (i.e., relevant to implementation of the GPEI in low and middle-income countries), and which were categorized as original/research articles or review articles (5). While the review was inclusive only up until 2018, we expect the review to still enclose sufficient data to generate a comprehensive synthesis given that the included 30 years period is when GPEI activities were at their peak.
Inclusion and exclusion criteria
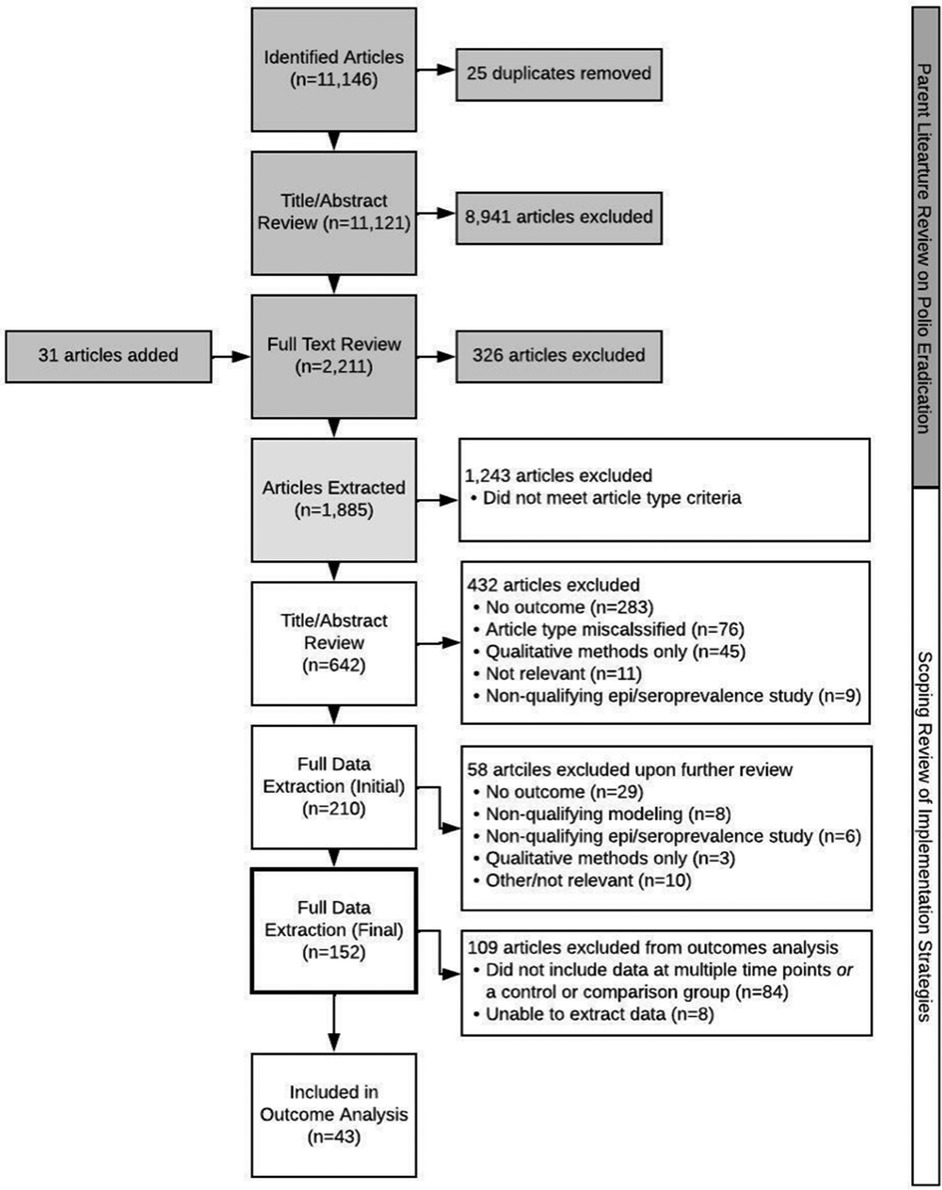
Since relevance to GPEI implementation was established a priori along with time, geography, and language restrictions (5), we focused on developing exclusion criteria to remove any articles not directly related to our aim of quantitatively assessing the effectiveness of implementation strategies utilized in polio eradication. These criteria are described in full in Supplementary File S3, but in short, articles were excluded if they (1) utilized only qualitative methods; (2) did not measure implementation, service delivery, or impact-level outcomes; (3) reported on epidemiological or seroprevalence studies that did not include at least two time points or a comparison district; (4) were modeling studies assessing non-programmatic features, or (5) did not meet article type criteria (e.g., an original/research or review article). Conversely, articles were included if they met inclusion criteria for the GPEI scoping review, were categorized as an original/research or review article, and included quantitative measurement of one or more implementation, service delivery, or impact-level outcomes. While valuable and included in the parent study, grey literature was excluded from this analysis as we sought to assess how published literature reported on and measured outcomes related to implementation. Two analysts independently reviewed titles and abstracts for inclusion in full text review. Conflicts were clarified at the midpoint, and final resolutions were completed at the endpoint by a third researcher. While we aimed to be comprehensive in our review, we may have missed some relevant data by excluding non-English language articles, as well as articles that were not deemed original/research or review articles. For the outcomes analysis only studies that included data collected at multiple timepoints and/or control or comparison groups (n = 43) were included (see Figure 1).
Data extraction strategy
A data extraction tool was developed and used to collect information on study design, implementation strategies, and outcomes. The data extraction tool asked analysts to determine inclusion/exclusion of the material, identify implementation strategies applied in the study, identify the outcome type, and assess elements of the study design, including methods, data sources, study type (e.g., randomized control trial, stepped wedge, etc.), frequency of data collection, and whether control or comparison groups were used. Following a pilot test of six articles and subsequent revisions to the data extraction tool, four analysts were randomly assigned a batch of articles for full text review. Ten percent of articles included were reviewed by all four analysts. The overall percent agreement across all 392 variables in our extraction tool was 86% (Benchmark Interval: 80%–100%), implying almost perfect agreement among raters based on the benchmark scale without accounting for agreement due to chance. A full analysis of inter-rater reliability conducted in Stata (14.2) on selected variables is available in Supplementary File S4 (11).
Data was collected on three key areas: study design, implementation strategies, and outcomes. We assessed characteristics of the study design as they are related to the level of inference (12), including sample size, study methods, data sources, data collection timepoints, and use of control and comparison groups. Implementation strategies were extracted as part of the original GPEI scoping review according to an adapted ERIC taxonomy (13). We also assessed the socioecological level at which the strategy was deployed, e.g., individual, household, community, organizational, system-wide. Outcome types were defined according to pre-existing typologies (9, 14) and categorized as implementation, service delivery, or impact (morbidity, mortality) outcomes. Implementation outcomes were defined as “effects of deliberate and purposive actions to implement new treatments, practices, and services” and service delivery outcomes derived from the Institute of Medicine (IOM) (8). In addition, the value, statistical significance, and direction of effect measures were extracted where available. To assure the quality of the included articles, the outcome analysis examining the effect or impact of implementation strategies was restricted only to studies with a comparison group for the implementation strategy, and/or outcome data collected over at least two timepoints.
Data synthesis and presentation
To standardize our results, we have drawn from a number of existing implementation science theories to describe the strategies in detail, including the ERIC framework which provides definitions for common implementation strategies (3), the Consolidated Framework on Implementation Research (CFIR) which provides a menu of constructs associated with effective implementation and contextual variables that may be the target of implementation strategies (15) what we have described here as “action targets”, as well as Proctor et al.'s guidance for specifying and reporting implementation strategies (8).
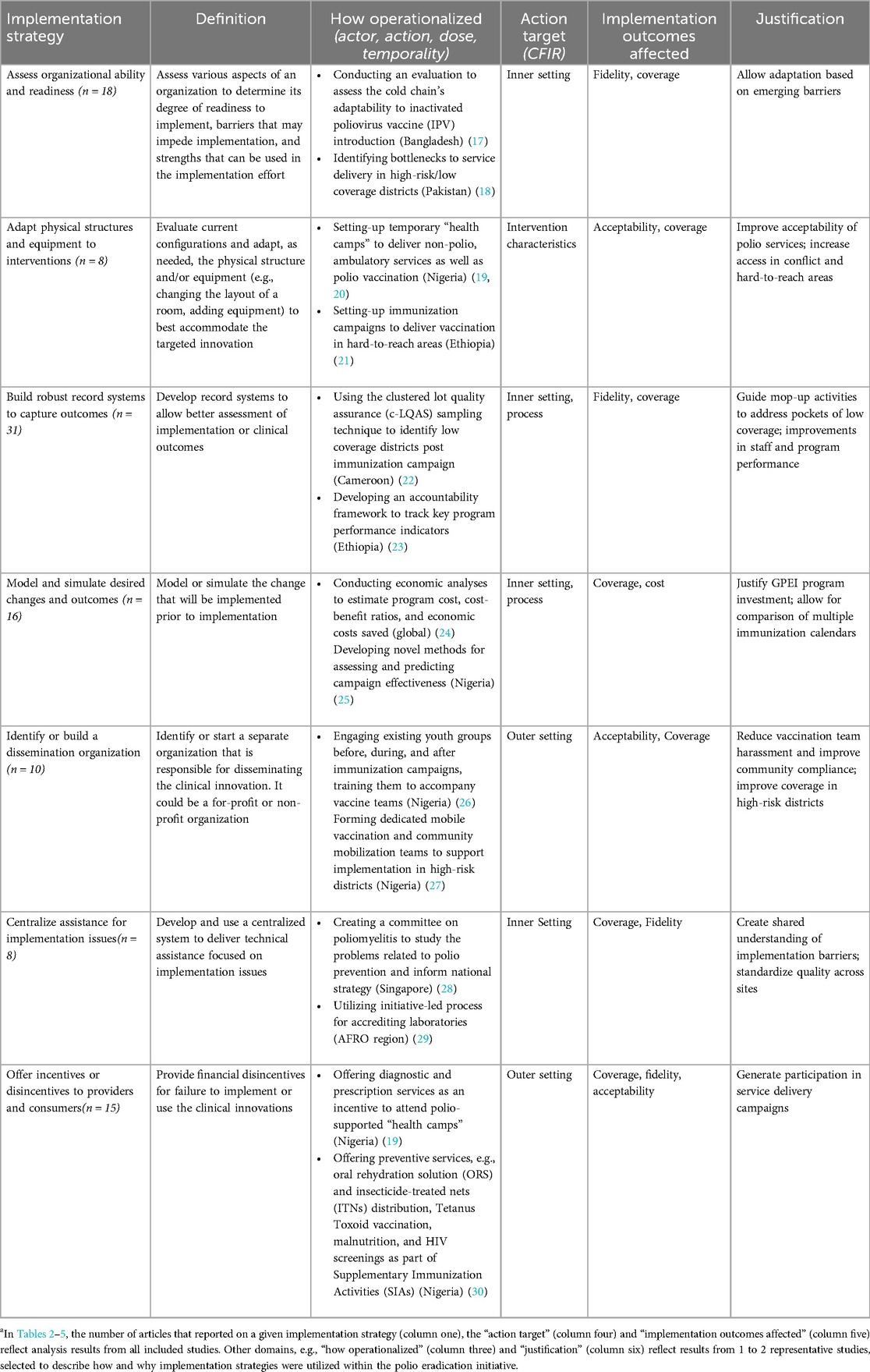
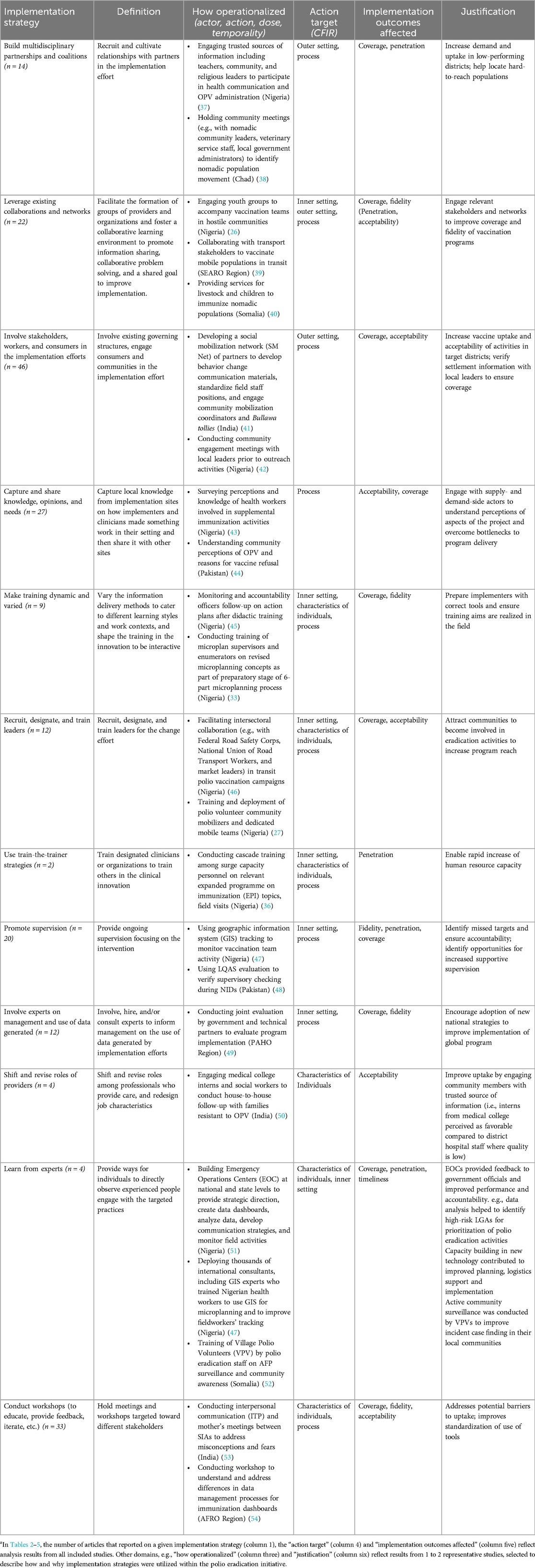
Proctor et al.'s guidance suggests that to fully describe implementation strategies they must be named, defined, and operationalized (8). We used the Expert Recommendations for Implementing Change (ERIC) catalog of implementation strategies (3) to name and define the implementation strategies used in included studies; this was part of the initial STRIPE study, whose methodology has been described more fully elsewhere (5, 6), but we used ERIC in order to have a standardized set of implementation strategies that would enable comparison across initiatives. We then described how these strategies were operationalized by describing the actor, action, dose, temporality and justification using 1–2 representative studies, selected to describe how and why implementation strategies were utilized within the polio eradication initiative. To standardize how we described the action targets of these strategies, we leveraged the CFIR framework, which also guided the STRIPE project and includes a series of domains within which implementation strategies may be levied (15). Finally, based on review of the included studies, we identified the implementation outcomes which were most often targeted by the implementation strategies deployed.
Results
Overview of selected studies
Figure 1 presents the PRISMA flow diagram of the study selection process (16), bifurcated to illustrate the initial GPEI scoping review conducted as part of the STRIPE project and the nested implementation strategies and outcomes analyses reported in this paper. We retained 642 articles for title-abstract review after removing articles that were included in the scoping review but did not meet our requirements for article type (n = 1,243), i.e., were not an original/research or review article. A total of 432 articles were subsequently excluded during the abstract screening, most commonly because the article did not include an effectiveness measure of implementation strategies deployed for polio eradication (51.79%). Two-hundred and ten articles were identified for data extraction (see Supplementary File S5 for an overview of these 210 articles). An additional 58 articles were excluded from full data extraction upon further review: 29 did not have an outcome, 8 were modeling studies that did not model relevant outcomes, 6 were seroprevalence studies without an implementation strategy, 3 employed qualitative methods only, and 12 were excluded for a variety of other reasons. Ultimately, 152 articles were included in full text extraction (Tables 1–5). A subset of these articles (n = 68) included data at multiple timepoints (n = 51) and/or utilized control or comparison groups in their measurement of implementation, service delivery, or impact outcomes (n = 17), and were thus assessed to be of higher quality, were included for consideration in the outcome analysis (Tables 6–8). An additional 8 articles were excluded from inclusion in Tables 6–8 upon analysis as analysts were unable to extract data or access the full text articles.
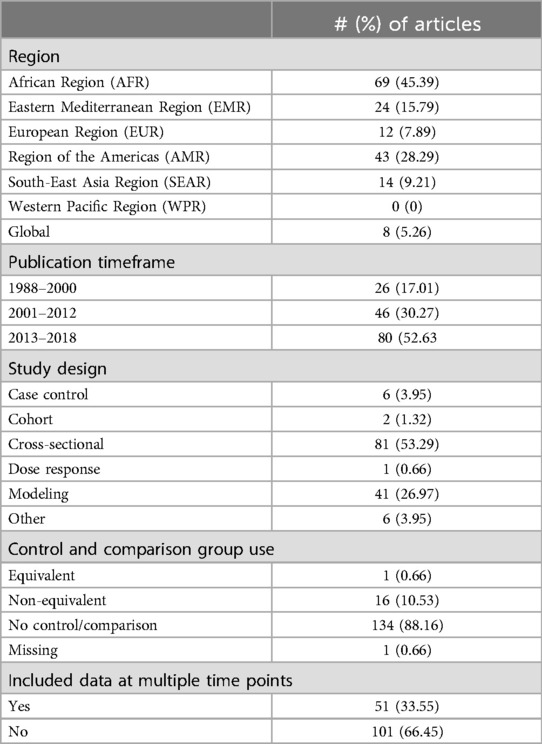
Study publication dates ranged from 1989 to 2018, but the majority (n = 80, 52.98%) were published between 2014 and 2018, coinciding with the fifth GPEI Strategic Plan (2013–2018) (83). Articles were relevant to multiple WHO regions covering a large swath of LMICs, especially the African (AFR), Americas (AMR), Eastern Mediterranean (EMR), and South-East Asia (SEAR) regions, though there was a clustering of articles in countries that remained polio endemic in 2020 or were focus LMICs for the GPEI [e.g., Nigeria (n = 50), India (n = 45), Pakistan (n = 22), Ethiopia (n = 12), and Democratic Republic of Congo (n = 8)]. The lack of articles from the WPR region likely reflect that the region was declared polio free in 2000 (84). Because the studies assessed a wide array of implementation strategies and their outcomes relevant to polio eradication, study samples were varied, however, most were focused on children 0–59 months, which is the target age range for three doses of poliovirus immunization. Of the included studies (n = 152), most (n = 135) utilized only quantitative methods, drawing heavily from surveys (n = 82, including both household and other surveys) and health management information system (HMIS) data (n = 49). We also included 17 studies which used a mixed methods approach and included qualitative methods such as focus group discussions and key informant interviews. Notably, the majority of studies reviewed utilized an adequacy design, that is, were cross-sectional in nature and did not include equivalent or non-equivalent comparison groups. Characteristics of the included studies are described further in Table 1.
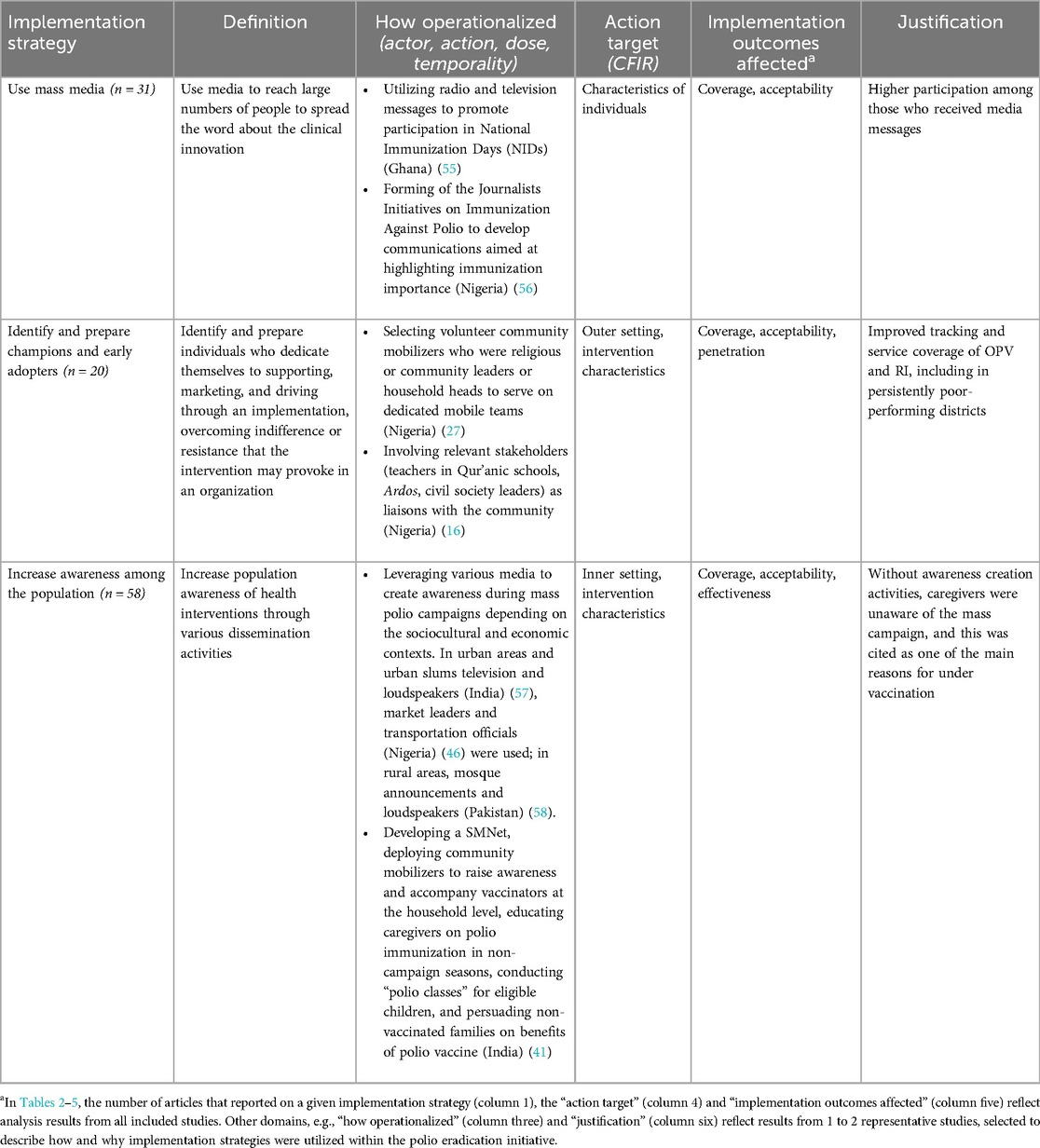
Implementation strategies
Tables 2–5 describe the implementation strategies utilized in the global polio eradication initiative from 1988 to 2018 following four themes identified from the broader STRIPE scoping review: management and problem solving (7 strategies referenced 106 times out of 496 total strategy references); monitoring and evaluation (4 strategies referenced 75 times out of 496 total references); engagement and capacity building (12 strategies referenced 206 times out of 496 total references); and communications and advocacy (3 strategies referenced 109 times out of 496 total references). A majority of included articles (n = 127, 83.6%) reported mostly multifaceted (i.e., combined multiple strategies or components), with an average of four implementation strategies (95% CI: 3.6, 4.7) reported on, and only 25 articles (16.4%) reported a single strategy. Across all themes, the most frequently documented implementation strategies were developing mechanisms for feedback, monitoring, and evaluation (69 out of 152 articles, 45.4%); increasing awareness among the population (58 out of 152 articles, 38.2%); involving stakeholders, workers, and consumers in the implementation efforts (46 out of 152 articles, 30.3%); conducting workshops (33 out of 152 articles, 21.7%); using mass media (31 out of 152 articles, 20.4%); and building robust record systems to capture outcomes (31 out of 152 articles, 20.4%). The most common implementation outcomes affected by these strategies were coverage (81% of strategies), acceptability (50% of strategies) and fidelity (46% of strategies). Conceptual definitions and operational examples for each of the implementation strategies are provided, along with explanations for how each strategy was used in the GPEI in Tables 2–5.
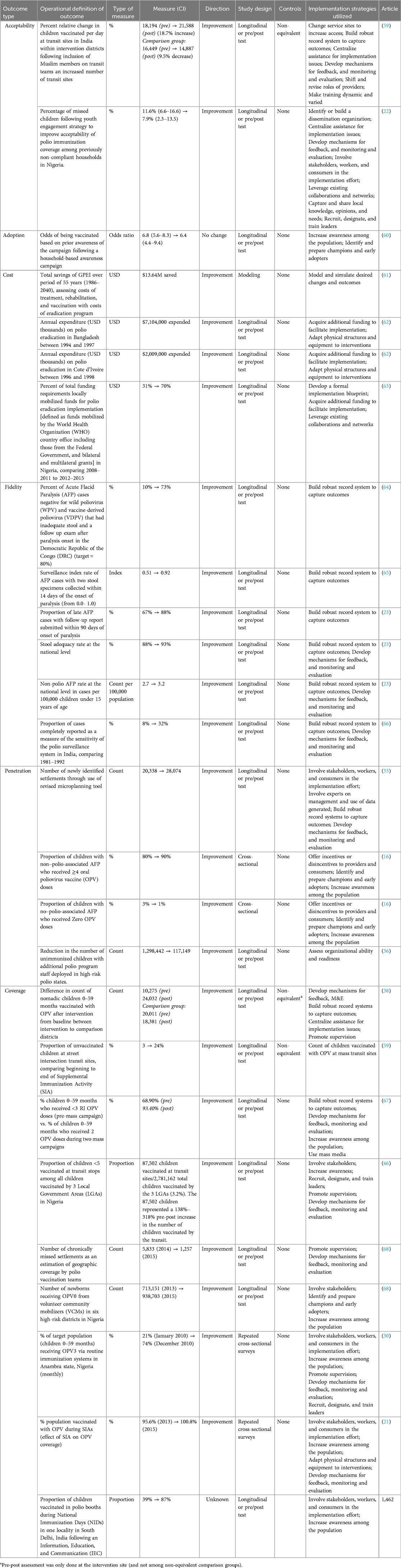
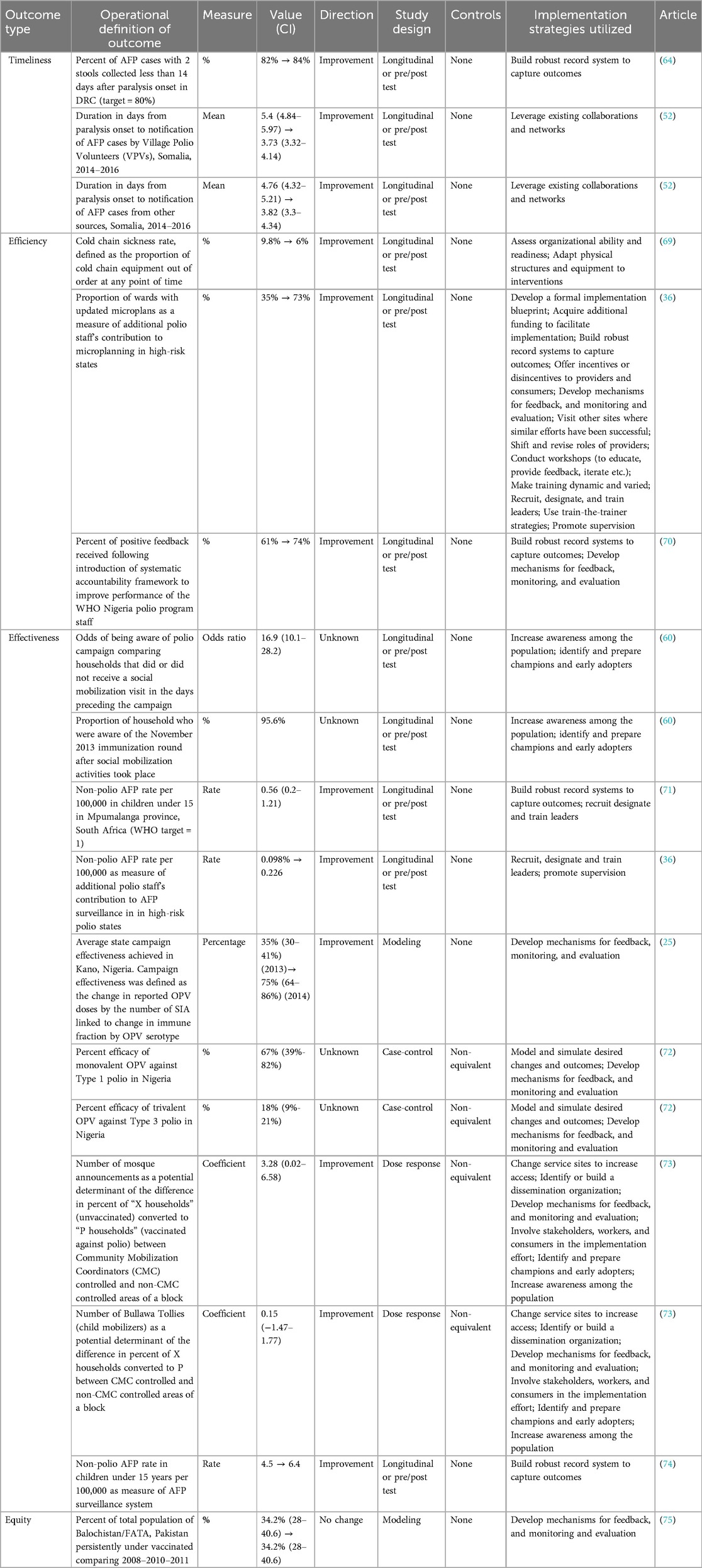
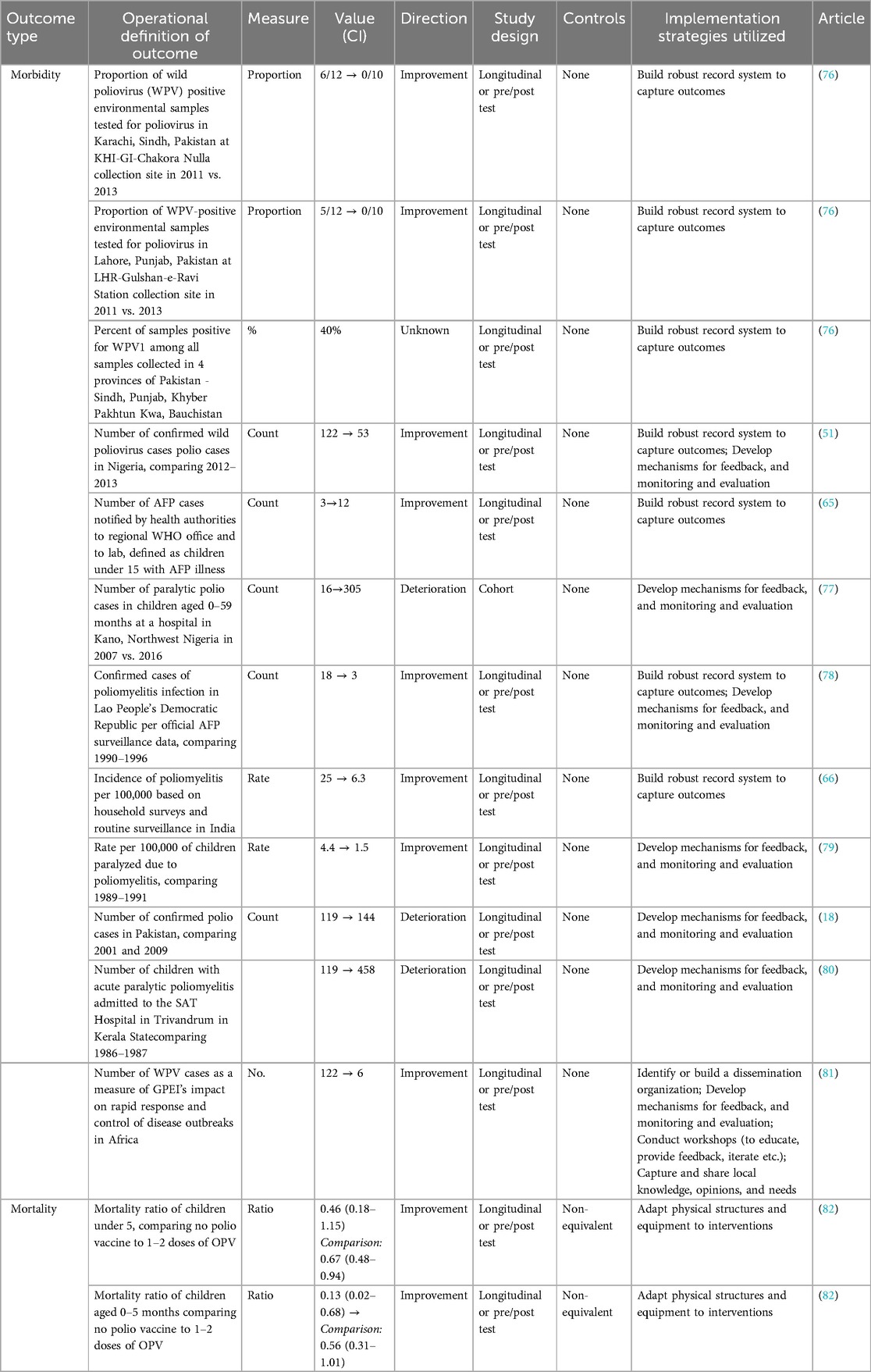
Implementation, service delivery, and impact outcomes
Tables 6–8 describe the implementation, service delivery, and impact outcomes that were described in the 43 unique studies included in the outcome analyses (see Figure 1: PRISMA flow diagram), that is studies that included data collected at multiple timepoints and/or control or comparison groups. There were 66 outcomes extracted from these 43 unique studies. Out of the 66 outcomes, coverage (n = 13) and morbidity (n = 12) were the most frequently identified outcomes, followed by effectiveness (n = 9) and fidelity (n = 6). Longitudinal or pre/post studies were the most frequently employed study design for assessing the influence of implementation strategies on the outcomes (n = 46) followed by cross-sectional data collection (n = 11). For the majority of outcomes (n = 57), there was no comparison group. Most studies reported changes in outcomes over time. Improvement in outcomes were reported in most cases (n = 44), whereas only 5 outcomes were reported as worse than expected over the course of the study.
Of the 32 implementation outcomes extracted, the most frequently described outcomes were related to coverage (Table 8). Although the operational definition for coverage varied, these studies generally reported on the proportion of children that were vaccinated within a geographic area. The operational definitions for other implementation outcomes captured elements of other GPEI program components. For example, fidelity outcomes largely reported on the processes related to AFP surveillance systems, acceptability outcomes tracked the impact of community engagement strategies, while cost outcomes reflected on overall program expenditures. For most implementation outcomes, it was difficult to identify influential implementation strategies because of the multifaceted nature of most of the strategies and limited description on how they were specified. However, all 6 of the fidelity outcomes were influenced by strategies that build robust record systems to capture outcomes. Notably, there were no included studies that reported on outcomes related to appropriateness, feasibility, or sustainability.
Among the service delivery outcomes, effectiveness was the most frequently reported outcome (Table 7). Effectiveness outcomes focused on a range of issues, from the effectiveness of social mobilization campaigns to the efficacy of various polio vaccinations, and to the overall effectiveness of GPEI programming in geographic areas. Most of the timeliness outcomes related to the speed at which the AFP surveillance system found and reported suspect cases of polio. An example of an efficiency outcome is the proportion of wards (sub-districts) using updated microplans in high-risk states. Equity concerns were only directly addressed by two modeling studies. There were no included studies that reported on patient safety, or the level of patient-centered care provided by GPEI programs.
Outcome measures of morbidity were reported more frequently than mortality (Table 8). Morbidity outcome measures largely captured the incidence or prevalence of polio within a population. Across the 12 morbidity outcomes recorded, 6 assessed for implementation strategy on building robust record systems, 4 were assessed for developing mechanisms for feedback, and monitoring and evaluation, and 2 outcomes were assessed for both implementation strategies. Only one study examined the polio mortality over time and found a beneficial impact of supplementary immunization activities (e.g., house-to-house, mobile posts, and hotspots vaccination campaigns) on mortality ratios in children even during conflict.
Discussion
Synthesis
The global polio eradication initiative is one of the largest public health initiatives in the world (4)—and provides important lessons in implementation research and practice for improving delivery of health programs and services globally (6). In this paper, we examined implementation strategies and outcomes that were used for facilitating polio vaccination at different socioecological levels and diverse settings using a theory-based and systematic approach drawing heavily from theories, models, and frameworks in implementation science. We found that most implementation strategies deployed under GPEI in LMICs were multifaceted, focusing on stakeholder engagement and capacity building, and addressing management and problem solving in real time. These strategies were only weakly associated with implementation outcomes, especially coverage and fidelity, and service delivery and impact outcomes.
Whereas the ERIC framework (3) was helpful to initially organize the implementation strategies described as part of the GPEI, we had to adapt it to accommodate other strategies which were salient for the LMIC settings, but not described in any categories of the ERIC framework. For example, strategies focused on setting up and adapting infrastructure for services delivery, developing community partnership and community-led engagement activities (Tables 2–5) featured prominently and were relevant across different LMIC settings reviewed. This fact may point to the limitation of the ERIC framework in that it was originally designed for categorizing implementation strategies for supporting clinical interventions (and not population-based, public health interventions), from a high income country perspective, and lacks sufficient coverage of health systems strengthening strategies which are often necessary in resource-limited settings, especially in LMICs, to facilitate effective implementation and impact of evidence-supported interventions.
Indeed, implementation strategies deployed in low-resource settings need to be coupled with other strategies and efforts to build and strengthen health systems. For instance, some of the most frequently applied implementation strategies described for supporting the delivery of the polio vaccines in this review (e.g., developing mechanisms for feedback, increasing health awareness among population, building robust record systems to capture outcomes) were coupled with additional health system strengthening strategies (e.g., building advanced laboratory systems and community-based surveillance) that were critical for providing essential health services more broadly in LMIC settings (84).
The findings from this review are consistent with the priorities of the polio eradication initiative and its operational emphases over time, reflecting priorities to engage communities and individuals, reach hard-to-reach and hard-to-vaccinate populations, and improve program operations (17–21, 84). Consistent with other studies, strategies to build partnership and coalitions (20, 84), co-deliver other interventions and provide other health services beyond polio vaccination (17), develop mechanisms for feedback and accountability (84), engage local community and gain trust (21), conduct monitoring and evaluation including setting up robust data system (84) were all identified in this review.
What this study adds that has not been explicitly considered in the other studies is the influence of these implementation strategies on implementation, service delivery, and impact outcomes which can facilitate an evaluation of the likelihood of these strategies to achieve their expected results when applied to other programs (Tables 6–8)—thus, facilitating decision-making and prioritization efforts around these implementation strategies. Coverage of polio vaccination was predictably the central measure of the global polio eradication initiative. Hence, most of the implementation strategies reviewed were positively linked to these implementation outcomes. Two other implementation outcomes—acceptability and fidelity—also emerged from the data as significant for driving global health services delivery as demonstrated by the influence of strategies to build robust record system and develop mechanisms for feedback on these outcomes. The emphasis on fidelity was strong throughout the initiative, reflecting the top-down and central-command approach of the GPEI, and a response to limited health infrastructure and capacities in many of the implementing environments. The top-down and central-command approach was also reflected in the initiative's data-driven approach to planning and implementation, which leveraged strategies geared toward health information systems (e.g., building robust record systems to capture outcomes, developing mechanisms for feedback, monitoring, and evaluation).
Studies examining fidelity as an outcome of interest also described the initiative's investment in deploying human resources for health for polio-related activities (e.g., recruiting health workers, making training dynamic and varied, promoting supervision). Over time, acceptability became an increasing concern for the GPEI as implementer's struggled to penetrate pockets of low coverage and faced resistance from communities who were fatigued or mistrustful of the campaign (85). As has been well documented, the polio eradication initiative was compelled to address these issues through numerous engagement and communications strategies (e.g., identifying and preparing champions and early adopters, leveraging existing networks and collaborations), often tailored to meet highly localized needs. The polio eradication experience suggests that achieving coverage of health interventions is dually dependent on implementation processes that enable both precision and modification, and attention to demand-side factors that affect uptake and satisfaction.
Given the unique nature of the GPEI (a well-described evidence-based intervention in the polio vaccine, an ambitious eradication goal which drove the perception that an urgent response was warranted, a massive influx of resources, and an expectation of a discrete timeline), it is not altogether surprising that appropriateness, feasibility, and sustainability were rarely studied implementation outcomes. However, the absence of attention to sustainability has borne out over time to be an issue as implementers continue to struggle with how to integrate polio activities with other service delivery priorities and integrate programmatic assets into the broader health infrastructure and health system (86). Future efforts would benefit from developing and evaluating strategies to improve sustainability of health interventions. With regards to services delivery outcomes, the focus of reported studies on timeliness and speed of program delivery, and lack of attention to equity, are noteworthy given the ongoing and intractable challenges to reach marginalized populations under the GPEI. This provides important lessons for global vaccine delivery programs aimed at addressing pandemics and adequately responding to changing infectious disease dynamics. Speed and equity are not mutually exclusive goals.
Our synthesis revealed a few significant gaps in the literature which warrant commentary. First, throughout the literature implementation strategies were poorly described and, importantly, were not explicitly tied to implementation, service delivery, or impact outcomes. Indeed, there seemed to be a division in the literature between manuscripts which described polio eradication strategies in-depth, and those that measured polio-relevant outcomes, but which were only loosely connected to specific eradication strategies. This may partially reflect an operational reality that implementation strategies are pursued simultaneously, and researchers may have struggled to describe and measure the relationship between implementation strategies. Programmatic information systems and internal reports may better capture these dynamics, however, the utility of those findings for assessing implementation strategy effectiveness is limited if they are not cogently shared with a wider audience. Second, as was noted, a very limited set of articles included in the review demonstrated no change or a deterioration in the outcome of interest. As a result, the literature provides limited insights into those implementation strategies that were attempted and failed. This may reflect a larger trend in public health literature to focus publications on proven solutions (87), and in this context, a need to disseminate learnings which may have wider applicability. Efforts to document failures may have a critical role to play in building learning health systems that can refine programs and policies in real time as they adapt to changing conditions.
Strengths and limitations
Our study presents a comprehensive examination of implementation strategies leveraged throughout the polio eradication effort, drawing from a large sample of peer-reviewed articles. While there have been many efforts to document program strategies (88–90) few studies have described implementation strategies with the operational detail we present here. By utilizing standardized definitions for implementation strategies (3) and following operational guidelines for elaborating on them (8) we have tried to make our results interpretable and enable their practical use, while also contributing to the relevant theories, models and frameworks from the field of implementation science. For example, we realized the need to further organize implementation strategies around a context/domain-specific strategy taxonomy to complement the ERIC framework as shown in Tables 2–5 (i.e., framing implementation strategies around broader implementation objectives that they aim to accomplish, e.g., management and problem-solving, monitoring and evaluation, engagement and capacity building, communication and advocacy) to guide readers in understanding the context surrounding the deployment of specific strategy in different countries. This additional framework may be useful for guiding the choice of implementation strategies, especially in settings where a strategy may not necessarily be named and formulated as described by the ERIC framework—and enhance the contextual generalizability of strategies in implementation analysis (e.g., while two strategies may have different names in different settings, the lessons surrounding their implementation may be generalizable given any similarities of implementation objectives in the different settings). Hence, we recommend that this additional framework be used for naming strategies alongside the ERIC framework where feasible. In our analysis, we have taken an iterative, theory-based approach, ensuring high inter-rater reliability among our analysts. As far as we know, the combining of the ERIC and CFIR frameworks as operationalized for analyzing implementation strategies may be novel to this study.
Still, our study is not without limitations. The data itself presented numerous challenges which limited the depth of quantitative analysis we were able to conduct. Many studies were missing sample size information, while others did not provide denominators for outcomes measured. This made it challenging to evaluate the effectiveness of various strategies and prohibited conducting a meta-analysis. Additionally, this study centers on research evaluating quantitative measures; there is, however, qualitative work evaluating implementation strategies in this space—and the synthesis of these works could be the focus of future studies. Despite these limitations, our review of quantitative analyses provides a unique synthesis of how, when, and to what effect implementation strategies have been deployed throughout the course of the GPEI and have also pointed to clear gaps in how implementation outcomes are measured and reported. Notably, because our review was part of a larger study, it only includes articles through 2018. The included articles reflect a period of high intensity for the GPEI and are thus rich for understanding the implementation strategies used, however, future studies may wish to update these findings to explore any new innovations that have come in the final periods of the GPEI, particularly as the GPEI has turned to focus on integration into essential health systems (91). Finally, our analysis focused on peer-reviewed literature published in English; this provided helpful insights into how implementation strategies and outcomes are reported but may have led to the exclusion of some findings only available in the grey literature or published in other languages.
Implications for future research and practice
Within global health service delivery, more can and should be done to link the measurement of implementation strategies utilized in programs like the polio eradication effort to implementation, service delivery, and impact outcomes, and to evaluate those pathways in depth. These strategies should be evidentially or theoretically linked to specific implementation barriers or facilitation levers to define their objectives. While we were unable to conduct a full meta-analysis, our study did identify specific implementation strategies (Tables 6–8) that demonstrated a positive effect on implementation outcomes such as acceptability, fidelity, and coverage. By describing these in full, implementers can assess the appropriateness of these strategies (for example, changing service sites to increase access and acceptability, and involving stakeholders in the implementation effort to improve penetration) to their initiatives, and better drive outcomes.
As these implementation strategies are taken up in future initiatives, they should be coupled with embedded implementation research efforts to answer critical questions in real-time which can inform program adaptation and provide further insights into strategy effectiveness and contribute to broader health systems resilience (92). These studies should consider methodological instruments which enable the evaluation of both individual and combined implementation strategies, and their mechanisms of action. They should also emphasize the measurement of implementation outcomes which provide valuable information as to implementation strengths and weaknesses across numerous dimensions affecting delivery, uptake, and sustained use of health interventions.
Critically, implementation strategies and outcomes must be measured in a linked way, and in consideration of influencing variables which impact implementation over time, and lead to programmatic and systemic adaptations. Multiple and mixed methods research, which were not commonly reported in this review, are one avenue for advancing our understanding in this regard. As others have previously demonstrated, mixed method designs allow for hypothesis testing, while also providing a deeper understanding of implementation mechanisms (9, 93). Advancing theory can also help address the gaps identified in this study. While many of the implementation strategies described by the ERIC framework were relevant to polio eradication, there were health system strengthening strategies (e.g., human resources for health innovations) that did not fit under the framework, and the orientation of this framework to high-income countries was a significant limitation as described in the discussion above. Research to validate the appropriateness of the implementation strategies included in the ERIC framework for low and middle-income settings, and to describe missing implementation strategies relevant to ongoing public health initiatives (e.g., disease control, primary health care) should be considered. Organizing these strategies according to specific implementation outcomes can also support the development of theoretically grounded monitoring and evaluation platforms to better assess the effectiveness of implementation strategies for achieving relevant health outcomes.
Finally, published evaluations of this nature should not shy away from presenting failures to improve public health outcomes. Instead, these studies should endeavor to explain why targets were unmet to facilitate understanding and inform future implementation. Neglecting to address these gaps risks the repeated selection of inappropriate, ineffective strategies which may be predicated on potentially incorrect assumptions and inconclusive evidence. Practitioners would benefit most from research that helps them to reliably determine the potential effectiveness of strategies, and to assess necessary adaptations for programmatic and contextual specificities.
Conclusion
This review provides a catalogue of implementation strategies and outcomes relevant for global health services delivery drawing from the global polio eradication initiative through a systematic and theory-driven synthesis. Implementation strategies to develop mechanisms for feedback, increase awareness among population, engage communities and other stakeholders, and build robust record system to capture outcomes were found to be frequently applied across diverse settings with loose evidence on their positive influence on implementation, service, and impact outcomes. It is important to carefully consider the context in which these strategies and to consider coupling them with health system strengthening strategies (e.g., building health infrastructure) in resource-limited settings to maximize impact. This review advances theories in implementation science through the application of models and frameworks for operationalizing implementation strategies and outcomes, demonstrating the utility and gaps in using these models and frameworks for specifying strategies applied in LMIC settings. It demonstrates the gaps in the literature around the effectiveness and impact of implementation strategies relevant for global health services delivery and describes important lessons and guidance for achieving the goals of the GPEI and similar global health services delivery programs.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
AN: Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. AO: Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. MP: Data curation, Formal Analysis, Investigation, Methodology, Writing – review & editing. MS: Data curation, Investigation, Methodology, Writing – review & editing. OA: Conceptualization, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
Funding for the STRIPE project was provided by the Bill and Melinda Gates Foundation. The funder did not play any role in writing the protocol, interpreting the data, or in writing this manuscript.
Acknowledgments
The authors would like to acknowledge Dr. Anna Kalbarczyk for her role as the STRIPE program manager at the Johns Hopkins University, Dr. Rasheedat Oke and the late Ms. Oluwatamilore Areola for their contributions to the data collection for the scoping review, and Dr. Svea Closser for her contribution to the project activities. The authors would also like to acknowledge team members and academic institutions included under the broader STRIPE consortium: Drs. Ahmad Shah Salehi, Ahmad Omid Rahimi, and Tawab Saljuqi of Global Innovation Consultancy Services Afghanistan, Professor Malabika Sarker, Drs. Humayra Binte Anwar and Yameen Mazumder of BRAC University Bangladesh, Professor Wakgari Deressa and Dr. Assefa Seme of Addis Ababa University Ethiopia, late Professor Patrick Kayembe and Dr. Eric Mafuta of the Kinshasa School of Public Health Democratic Republic of Congo, Professor SD Gupta, Drs. Piyusha Majumdar, D.K. Magnal, and Neeraj Sharma of the IIHMR University India, Professor Yodi Mahendradhata and Dr. Riris Andono Ahmad of Universitas Gadjah Mada Indonesia, and Professor Eme Owoaje and Dr. Oluwaseun Akinyemi of the University of Ibadan Nigeria. Finally, the authors acknowledge the support Dr. Sue Gerber on the project activities and Bill Melinda Gates Foundation for the funding support to the project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2024.1287554/full#supplementary-material
Supplementary File S1 | Scoping Review PubMed Search Terms.
Supplementary File S2 | Inclusion/Exclusion Criteria.
Supplementary File S3 | Results of inter-rater reliability statistics.
Supplementary File S4 | PRISMA checklist.
Supplementary File S5 | Bibliography of articles identified for data extraction.
Abbreviations
AFP, acute flaccid paralysis; AFRO, African region; CFIR, consolidated framework for implementation research; CMC, community mobilization coordinators; EMRO, Eastern Mediterranean region; ERIC, expert recommendations for implementing change; GPEI, global polio eradication initiative; HMIS, health management information system; LMICs, Low And Middle-Income Countries; PAHO, Pan-American Health Organization; PRISMA, preferred reporting items for systematic reviews and meta-analyses; SEARO, Southeast Asian region; SIA, supplementary immunization activities; STRIPE, synthesis and translation of research and innovations for polio eradication; UNICEF, United Nations Children's Fund; WHO, World Health Organization.
References
1. McKibbon KA, Lokker C, Wilczynski NL, Ciliska D, Dobbins M, Davis DA, et al. A cross-sectional study of the number and frequency of terms used to refer to knowledge translation in a body of health literature in 2006: a tower of Babel? Implement Sci. (2010) 5(1):16. doi: 10.1186/1748-5908-5-16
2. Michie S, Fixsen D, Grimshaw JM, Eccles MP. Specifying and reporting complex behaviour change interventions: the need for a scientific method. Implement Sci. (2009) 4(1):40. doi: 10.1186/1748-5908-4-40
3. Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci. (2015) 10(1):21. doi: 10.1186/s13012-015-0209-1
4. Alonge O. What can over 30 years of efforts to eradicate polio teach US about global health? BMC Public Health. (2020) 20(Suppl 2):1177. doi: 10.1186/s12889-020-09198-z
5. Schleiff M, Olateju A, Decker E, Neel AH, Oke R, Peters MA, et al. A multi-pronged scoping review approach to understanding the evolving implementation of the smallpox and polio eradication programs: what can other global health initiatives learn? BMC Public Health. (2020) 20(Suppl 4):1698. doi: 10.1186/s12889-020-09439-1
6. Alonge O, Neel AH, Kalbarczyk A, Peters MA, Mahendradhata Y, Sarker M, et al. Synthesis and translation of research and innovations from polio eradication (STRIPE): initial findings from a global mixed methods study. BMC Public Health. (2020) 20(Suppl 2):1176. doi: 10.1186/s12889-020-09156-9
7. Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs. Med Care. (2012) 50(3):217–26. doi: 10.1097/MLR.0b013e3182408812
8. Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. (2013) 8(1):139–139. doi: 10.1186/1748-5908-8-139
9. Peters DH, Adam T, Alonge O, Agyepong IA, Tran N. Implementation research: what it is and how to do it. BMJ Br Medical J. (2013) 347(8):f6753. doi: 10.1136/bmj.f6753
10. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169(7):467–73. doi: 10.7326/M18-0850
12. Habicht JP, Victora CG, Vaughan JP. Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. Int J Epidemiol. (1999) 28(1):10–8. doi: 10.1093/ije/28.1.10
13. Waltz TJ, Powell BJ, Chinman MJ, Smith JL, Matthieu MM, Proctor EK, et al. Expert recommendations for implementing change (ERIC): protocol for a mixed methods study. Implement Sci. (2014) 9(1):39. doi: 10.1186/1748-5908-9-39
14. Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. (2011) 38(2):65–76. doi: 10.1007/s10488-010-0319-7
15. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. (2009) 4(1):50. doi: 10.1186/1748-5908-4-50
16. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Br Med J. (2009) 339:b2700. doi: 10.1136/bmj.b2700
17. Billah MM, Zaman K, Estivariz CF, Snider CJ, Anand A, Hampton LM, et al. Cold-chain adaptability during introduction of inactivated polio vaccine in Bangladesh, 2015. J Infect Dis. (2017) 216(Suppl 1):S114–21. doi: 10.1093/infdis/jiw591
18. Shah M, Khan MK, Shakeel S, Mahmood F, Sher Z, Sarwar MB, et al. Resistance of polio to its eradication in Pakistan. Virol J. (2011) 8(1):457. doi: 10.1186/1743-422X-8-457
19. Birukila G, Babale SM, Epstein H, Gugong V, Anger R, Corkum M, et al. Reducing resistance to polio immunisation with free health camps and bluetooth messaging: an update from Kaduna, Northern, Nigeria. Glob Public Health. (2016) 12(1):1–12. doi: 10.1080/17441692.2016.1152283
20. Shuaibu FM, Birukila G, Usman S, Mohammed A, Galway M, Corkum M, et al. Mass immunization with inactivated polio vaccine in conflict zones—experience from Borno and Yobe States, North-Eastern Nigeria. J Public Health Policy. (2016) 37(1):36–50. doi: 10.1057/jphp.2015.34
21. Tafesse B, Tekle E, Wondwossen L, Bogale M, Fiona B, Nsubuga P, et al. Effects of polio eradication activities on routine immunization: lessons from the 2013 outbreak response in Somali region of Ethiopia. Pan Afr Med J. (2017) 27(Suppl 2):4. doi: 10.11604/pamj.supp.2017.27.2.10569
22. Pezzoli L, Tchio R, Dzossa AD, Ndjomo S, Takeu A, Anya B, et al. Clustered lot quality assurance sampling: a tool to monitor immunization coverage rapidly during a national yellow fever and polio vaccination campaign in Cameroon, May 2009. Epidemiol Infect. (2012) 140(1):14–26. doi: 10.1017/S0950268811000331
23. Kassahun A, Braka F, Gallagher K, Gebriel AW, Nsubuga P, M’pele-Kilebou P. Introducing an accountability framework for polio eradication in Ethiopia: results from the first year of implementation 2014–2015. Pan Afr Med J. (2017) 27(Suppl 2):12. doi: 10.11604/pamj.supp.2017.27.2.10939
24. Tebbens RJD, Pallansch MA, Cochi SL, Wassilak SGF, Linkins J, Sutter RW, et al. Economic analysis of the global polio eradication initiative. Vaccine. (2010) 29(2):334–43. doi: 10.1016/j.vaccine.2010.10.026
25. Upfill-Brown AM, Voorman A, Chabot-Couture G, Shuaib F, Lyons HM. Analysis of vaccination campaign effectiveness and population immunity to support and sustain polio elimination in Nigeria. BMC Med. (2016) 14(1):60. doi: 10.1186/s12916-016-0600-z
26. Musa A, Mkanda P, Manneh F, Korir C, Warigon C, Gali E, et al. Youth group engagement in noncompliant communities during supplemental immunization activities in Kaduna, Nigeria, in 2014. J Infect Dis. (2016) 213(Suppl 3):S91–5. doi: 10.1093/infdis/jiv510
27. Ongwae KM, Bawa SB, Shuaib F, Braka F, Corkum M, Isa HK. Use of dedicated mobile teams and polio volunteer community mobilizers to increase access to zero-dose oral poliovirus vaccine and routine childhood immunizations in settlements at high risk for polio transmission in Northern Nigeria. J Infect Dis. (2017) 216(Suppl 1):S267–72. doi: 10.1093/infdis/jiw520
28. Lee HC, Tay J, Kwok CYH, Wee MJ, Ang LW, Kita Y, et al. Certification of poliomyelitis eradication in Singapore and the challenges ahead. Ann Acad Med Singap. (2012) 41(11):518–28. doi: 10.47102/annals-acadmedsg.V41N11p518
29. Gumede N, Coulibaly SO, Yahaya AA, Ndihokubwayo JB, Nsubuga P, Okeibunor J, et al. Polio eradication initiative (PEI) contribution in strengthening public health laboratories systems in the African region. Vaccine. (2016) 34(43):5164–9. doi: 10.1016/j.vaccine.2016.05.055
30. Onyeka I, Onyibe R, Okoye C, Diden G, Onubogu C, Ilika A, et al. Experiences from polio supplementary immunization activities in Anambra State, Nigeria. Niger J Clin Pract. (2014) 17(6):808. doi: 10.4103/1119-3077.144406
31. Kazi A, Murtaza A, Khoja S, Zaidi A, Ali S. Monitoring polio supplementary immunization activities using an automated short text messaging system in Karachi, Pakistan. Bull World Health Organ. (2013) 92(3):220–5. doi: 10.2471/BLT.13.122564
32. Farrell M, Hampton LM, Shendale S, Menning L, Gonzalez AR, Garon J, et al. Monitoring and validation of the global replacement of tOPV with bOPV, April–May 2016. J Infect Dis. (2017) 216(Suppl 1):S193–201. doi: 10.1093/infdis/jiw558
33. Gali E, Mkanda P, Banda R, Korir C, Bawa S, Warigon C, et al. Revised household-based microplanning in polio supplemental immunization activities in Kano State, Nigeria. 2013–2014. J Infect Dis. (2016) 213(suppl_3):S73–8. doi: 10.1093/infdis/jiv589
34. Banerjee K, Suresh K. Repeat process evaluation of pulse polio immunization. Indian Pediatr. (1997) 34(4):357–65. Available online at: https://pubmed.ncbi.nlm.nih.gov/9332108/9332108
35. Okeibunor J, Nshimirimana D, Nsubuga P, Mutabaruka E, Tapsoba L, Ghali E, et al. Documentation of polio eradication initiative best practices: experience from WHO African region. Vaccine. (2016) 34(43):5144–9. doi: 10.1016/j.vaccine.2016.05.058
36. Yehualashet YG, Mkanda P, Gasasira A, Erbeto T, Onimisi A, Horton J, et al. Strategic engagement of technical surge capacity for intensified polio eradication initiative in Nigeria, 2012–2015. J Infect Dis. (2016) 213(suppl_3):S116–23. doi: 10.1093/infdis/jiv494
37. Warigon C, Mkanda P, Muhammed A, Etsano A, Korir C, Bawa S, et al. Demand creation for polio vaccine in persistently poor-performing communities of Northern Nigeria: 2013–2014. J Infect Dis. (2016) 213(Suppl 3):S79–85. doi: 10.1093/infdis/jiv511
38. Ndiaye SM, Ahmed MA, Denson M, Craig AS, Kretsinger K, Cherif B, et al. Polio outbreak among Nomads in Chad: outbreak response and lessons learned. J Infect Dis. (2014) 210(suppl_1):S74–84. doi: 10.1093/infdis/jit564
39. Maurice J. Polio eradication effort sees progress, but problems remain. Lancet. (2014) 383(9921):939–40. doi: 10.1016/S0140-6736(14)60452-9
40. Kamadjeu R, Mulugeta A, Gupta D, Hirsi AA, Belayneh A, Clark-Hattingh M, et al. Immunizing nomadic children and livestock—experience in North East zone of Somalia. Hum Vaccin Immunother. (2015) 11(11):2637–9. doi: 10.1080/21645515.2015.1038682
41. Weiss WM, Rahman M, Solomon R, Singh V, Ward D. Outcomes of polio eradication activities in Uttar Pradesh, India: the social mobilization network (SM net) and core group polio project (CGPP). BMC Infect Dis. (2011) 11(1):117. doi: 10.1186/1471-2334-11-117
42. Gidado SO, Ohuabunwo C, Nguku PM, Ogbuanu IU, Waziri NE, Biya O, et al. Outreach to underserved communities in Northern Nigeria, 2012–2013. J Infect Dis. (2014) 210(suppl_1):S118–24. doi: 10.1093/infdis/jiu197
43. Arulogun OS, Obute JA. Health workers’ perception about the supplemental immunization activities in Gombe local government area, Gombe State. Afr J Med Med Sci. (2007) 1:65–70. Available online at: https://pubmed.ncbi.nlm.nih.gov/17874492/17874492
44. Murakami H, Kobayashi M, Hachiya M, Khan ZS, Hassan SQ, Sakurada S. Refusal of oral polio vaccine in Northwestern Pakistan: a qualitative and quantitative study. Vaccine. (2014) 32(12):1382–7. doi: 10.1016/j.vaccine.2014.01.018
45. Adamu US, Archer WR, Braka F, Damisa E, Siddique A, Baig S, et al. Progress toward poliomyelitis eradication—Nigeria, January 2018–May 2019. Morbidity Mortal Wkly Rep. (2019) 68(29):642–6. doi: 10.15585/mmwr.mm6829a3
46. Musa A, Abba B, Ningi AMI, Gali E, Bawa S, Manneh F, et al. Enhancing transit polio vaccination in collaboration with targeted stakeholders in Kaduna State, Nigeria: lessons learnt: 2014–2015. Vaccine. (2016) 34(43):5159–63. doi: 10.1016/j.vaccine.2016.05.064
47. Barau I, Zubairu M, Mwanza MN, Seaman VY. Improving polio vaccination coverage in Nigeria through the use of geographic information system technology. J Infect Dis. (2014) 210(suppl_1):S102–10. doi: 10.1093/infdis/jiu010
48. Mushtaq MU, Majrooh MA, Ullah MZS, Akram J, Siddiqui AM, Shad MA, et al. Are we doing enough? Evaluation of the polio eradication initiative in a district of Pakistan’s Punjab province: a LQAS study. BMC Public Health. (2010) 10(1):60. doi: 10.1186/1471-2458-10-60
49. Carvalho LHF, Weckx LY. Universal use of inactivated polio vaccine. J Pediatr (Rio J). (2006) 82(7):75–82. doi: 10.2223/JPED.1493
50. Ansari MA, Khan Z, Khan IM. Reducing resistance against polio drops. J R Soc Promot Health. (2007) 127(6):276–9. doi: 10.1177/1466424007083705
51. Ado JM, Etsano A, Shuaib F, Damisa E, Mkanda P, Gasasira A, et al. Progress toward poliomyelitis eradication in Nigeria. J Infect Dis. (2014) 210(suppl_1):S40–9. doi: 10.1093/infdis/jiu318
52. Mbaeyi C, Mohamed A, Owino BO, Mengistu KF, Ehrhardt D, Elsayed EA. Strengthening acute flaccid paralysis surveillance through the village polio volunteers program in Somalia. Clin Infect Dis. (2018) 67(6):941–6. doi: 10.1093/cid/ciy180
53. Weiss WM, Choudhary M, Solomon R. Performance and determinants of routine immunization coverage within the context of intensive polio eradication activities in Uttar Pradesh, India: social mobilization network (SM net) and core group polio project (CGPP). BMC Int Health Hum Rights. (2013) 13(1):25. doi: 10.1186/1472-698X-13-25
54. Poy A, van den Ent MMVX, Sosler S, Hinman AR, Brown S, Sodha S, et al. Monitoring results in routine immunization: development of routine immunization dashboard in selected African countries in the context of the polio eradication endgame strategic plan. J Infect Dis. (2017) 216(suppl_1):S226–36. doi: 10.1093/infdis/jiw635
55. Browne ENL, Bonney AA, Agyapong FA, Essegbey IT. Factors influencing participation in national immunization days in Kumasi, Ghana. Ann Trop Med Parasitol. (2013) 96(1):93–104. doi: 10.1179/000349802125000556
56. Warigon C, Mkanda P, Banda R, Zakari F, Damisa E, Idowu A, et al. The journalists initiatives on immunisation against polio and improved acceptance of the polio vaccine in Northern Nigeria 2007–2015. J Infect Dis. (2016) 213(suppl_3):S86–90. doi: 10.1093/infdis/jiv545
57. Chudasama R. Evaluation of intensive pulse polio immunization in district Valsad during 2007. Indian Pediatr. (2008) 45(3):233–5. Available online at: https://pubmed.ncbi.nlm.nih.gov/18367772/18367772
58. Hennessey KA, Marx A, Hafiz R, Ashgar H, Hadler SC, Jafari H, et al. Widespread paralytic poliomyelitis in Pakistan: a case-control study to determine risk factors and implications for poliomyelitis eradication. J Infect Dis. (2000) 182(1):6–11. doi: 10.1086/315675
59. Shah NK, Talyan A, Jain V, Khaparde SD, Bahl S, Hutin Y, et al. Improving polio vaccination during supplementary campaigns at areas of mass transit in India. BMC Public Health. (2010) 10(1):243. doi: 10.1186/1471-2458-10-243
60. Haskew J, Kenyi V, William J, Alum R, Puri A, Mostafa Y, et al. Use of mobile information technology during planning, implementation and evaluation of a polio campaign in South Sudan. PLoS One. (2015) 10(8):e0135362. doi: 10.1371/journal.pone.0135362
61. Bart K, Foulds J, Patriarca P. Global eradication of poliomyelitis: benefit-cost analysis. Bull World Health Organ. (1996) 74(1):35–45. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2486843/?page=88653814
62. Levin A, Ram S, Kaddar M. The impact of the global polio eradication initiative on the financing of routine immunization: case studies in Bangladesh, C Te d’Ivoire, and Morocco. Bull World Health Organ. (2002) 80(10):822–8.12471404
63. Yehualashet YG, Horton J, Mkanda P, Vaz RG, Afolabi O, Gashu SG, et al. Intensified local resource mobilization for the polio eradication initiative: the experience of world health organization in Nigeria during 2008–2015. J Infect Dis. (2016) 213(Suppl 3):S101–7. doi: 10.1093/infdis/jiv535
64. Alleman MM, Meyer SA, Mulumba A, Nyembwe M, Riziki Y, Mbule A, et al. Improved acute flaccid paralysis surveillance performance in the democratic republic of the Congo, 2010–2012. J Infect Dis. (2014) 210(suppl_1):S50–61. doi: 10.1093/infdis/jit670
65. Fontana S, Buttinelli G, Fiore S, Mulaomerovic M, Aćimović J, Amato C, et al. Acute flaccid paralysis surveillance in Bosnia and Herzegovina: recent isolation of two sabin like type 2 poliovirus. J Med Virol. (2017) 89(9):1678–81. doi: 10.1002/jmv.24827
66. Singh J, Foster S. Sensitivity of poliomyelitis surveillance in India. Indian Pediatr. (1998) 35(4):311–5. doi: 10.1007/BF02752309
67. Andrianarivelo MR, Boisier P, Rabarijaona L, Ratsitorahina M, Migliani R, Zeller H. Mass vaccination campaigns to eradicate poliomyelitis in Madagascar: oral poliovirus vaccine increased immunity of children who missed routine programme. Trop Med Int Health. (2001) 6(12):1032–9. doi: 10.1046/j.1365-3156.2001.00812.x
68. Touray K, Mkanda P, Tegegn SG, Nsubuga P, Erbeto TB, Banda R, et al. Tracking vaccination teams during polio campaigns in northern Nigeria by use of geographic information system technology: 2013–2015. J Infect Dis. (2016) 213(suppl_3):S67–72. doi: 10.1093/infdis/jiv493
69. Goel N, Pathak R, Galhorta A, Dankal C, Swami H. Status of cold-chain maintenance in Chandigarh. Indian J Public Health. (2008) 52(1):37–9.18700720
70. Tegegne SG, MKanda P, Yehualashet YG, Erbeto TB, Touray K, Nsubuga P, et al. Implementation of a systematic accountability framework in 2014 to improve the performance of the Nigerian polio program. J Infect Dis. (2016) 213(Suppl 3):S96–100. doi: 10.1093/infdis/jiv492
71. Harris BN, Dürrheim DN, Ogunbanjo GA. Polio eradication—the validity of surveillance indicators. Trop Med Int Health. (2003) 8(5):386–91. doi: 10.1046/j.1365-3156.2003.01048.x
72. Jenkins HE, Aylward RB, Gasasira A, Donnelly CA, Abanida EA, Koleosho-Adelekan T, et al. Effectiveness of immunization against paralytic poliomyelitis in Nigeria. N Engl J Med. (2008) 359(16):1666–74. doi: 10.1056/NEJMoa0803259
73. Weiss WM, Rahman MH, Solomon R, Ward D. Determinants of performance of supplemental immunization activities for polio eradication in Uttar Pradesh, India: social mobilization activities of the social mobilization network (SM net) and core group polio project (CGPP). BMC Infect Dis. (2013) 13(1):17–17. doi: 10.1186/1471-2334-13-17
74. Bassey B, Gasasira A, Mitula P, Frankson U, Adeniji J. Surveillance of acute flaccid paralysis in Akwa Ibom State, Nigeria 2004–2009. Pan Afr Med J. (2011) 9(1):32. doi: 10.4314/pamj.v9i1.71208
75. O’Reilly KM, Cori A, Durry E, Wadood MZ, Bosan A, Aylward RB, et al. A new method for estimating the coverage of mass vaccination campaigns against poliomyelitis from surveillance data. Am J Epidemiol. (2015) 182(11):961–70. doi: 10.1093/aje/kwv199
76. Alam MM, Shaukat S, Sharif S, Angez M, Khurshid A, Malik F, et al. Detection of multiple cocirculating wild poliovirus type 1 lineages through environmental surveillance: impact and progress during 2011–2013 in Pakistan. J Infect Dis. (2014) 210(suppl_1):S324–32. doi: 10.1093/infdis/jiu160
77. Lamina S, Hanif S. Paralytic poliomyelitis during the pre-, peri- and post-suspension periods of a polio immunization campaign. Trop Doct. (2008) 38(3):173–5. doi: 10.1258/td.2007.070196
78. Kuroiwa C, CHose T, Murakami H, Duangmala S, Vongphrachanh P, Saito T, et al. Polio surveillance in Lao PDR: a two-year experience of active case search, 1994–1996. J Trop Pediatr. (1999) 45(3):185–90. doi: 10.1093/tropej/45.3.185
79. Srinivasa DK, Sahai A, Rotti SB, Soudarssanane MB, Danabalan M, Sahoo RN, et al. Poliomyelitis trends in pondicherry, South India, 1989–91 on JSTOR. J Epidemiol Community Health. (1997) 51(4):443–8. doi: 10.1136/jech.51.4.443
80. Sulekha C, Sujamol S, Bai NSS, Cherian T, John TJ. An epidemic of poliomyelitis in Southern Kerala. Int J Epidemiol. (1990) 19(1):177–81. doi: 10.1093/ije/19.1.177
81. Kouadio K, Okeibunor J, Nsubuga P, Mihigo R, Mkanda P. Polio infrastructure strengthened disease outbreak preparedness and response in the WHO African region. Vaccine. (2016) 34(43):5175–80. doi: 10.1016/j.vaccine.2016.05.070
82. Aaby P, Hedegaard K, Sodemann M, Nhante E, Veirum JE, Jakobsen M, et al. Childhood mortality after oral polio immunisation campaign in Guinea-Bissau. Vaccine. (2005) 23(14):1746–51. doi: 10.1016/j.vaccine.2004.02.054
84. Adams T. Farewell to polio in the western pacific. Bull World Health Organ. (2000) 12(78):1375.11196482
85. Neel AH, Closser S, Villanueva C, Majumdar P, Gupta SD, Krugman D, et al. 30 years of polio campaigns in Ethiopia, India and Nigeria: the impacts of campaign design on vaccine hesitancy and health worker motivation. BMJ Glob Health. (2021) 6(8):e006002. doi: 10.1136/bmjgh-2021-006002
86. Rodriguez DC, Neel AH, Mahendradhata Y, Deressa W, Owoaje E, Akinyemi O, et al. The effects of polio eradication efforts on health systems: a cross-country analysis using the develop–distort dilemma. Health Policy Plan. (2021) 36(5):czab044. doi: 10.1093/heapol/czab044
87. Rajkotia Y. Beware of the success cartel: a plea for rational progress in global health. BMJ Glob Health. (2018) 3(6):e001197. doi: 10.1136/bmjgh-2018-001197
88. Cochi SL, Hegg L, Kaur A, Pandak C, Jafari H. The global polio eradication initiative: progress, lessons learned, and polio legacy transition planning. Health Aff. (2017) 35(2):277–83. doi: 10.1377/hlthaff.2015.1104
89. Zipursky S, Vandelaer J, Brooks A, Dietz V, Kachra T, Farrell M, et al. Polio endgame: lessons learned from the immunization systems management group. J Infect Dis. (2017) 216(suppl_1):S9–14. doi: 10.1093/infdis/jiw592
90. Perry HB, Solomon R, Bisrat F, Hilmi L, Stamidis KV, Steinglass R, et al. Lessons learned from the CORE group polio project and their relevance for other global health priorities. Am J Trop Med Hyg. (2019) 101(4 Suppl):107–12. doi: 10.4269/ajtmh.19-0036
91. GPEI. Polio Eradication Strategy 2022–2026 Delivering on a promise: Stakeholder consultation report [Internet]. (2021). p. ix–x. Available online at: https://reliefweb.int/report/world/polio-eradication-strategy-2022-2026-delivering-promise-enarruzh#:∼:text=We%20look%20forward%20to%20working,particularly%20in%20Pakistan%20and%20Afghanistan
92. Peters MA, Cloete K, Odwe G, Tadele G, Hirschhorn LR, Magge H, et al. Embedding implementation research to cross the quality of care chasm during the COVID-19 pandemic and beyond. Br Med J. (2023) 383:e076331. doi: 10.1136/bmj-2023-076331
Keywords: implementation research, implementation strategies, implementation outcomes, polio, global polio eradication initiative
Citation: Neel AH, Olateju A, Peters MA, Schleiff M and Alonge O (2024) Lessons from polio eradication: a synthesis of implementation strategies for global health services delivery from a scoping review. Front. Health Serv. 4:1287554. doi: 10.3389/frhs.2024.1287554
Received: 1 September 2023; Accepted: 3 July 2024;
Published: 7 August 2024.
Edited by:
Shefaly Shorey, National University of Singapore, SingaporeReviewed by:
Nick Sevdalis, National University of Singapore, SingaporeTaufique Joarder, SingHealth Duke-NUS Global Health Institute, Singapore
© 2024 Neel, Olateju, Peters, Schleiff and Alonge. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Olakunle Alonge, b2Fsb25nZUB1YWIuZWR1
 Abigail H. Neel1
Abigail H. Neel1 Olakunle Alonge
Olakunle Alonge