
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Health Serv., 29 November 2023
Sec. Mental Health Services
Volume 3 - 2023 | https://doi.org/10.3389/frhs.2023.1272285
 Cerina Lee1*
Cerina Lee1* Thanh-Huyen T. Vu2
Thanh-Huyen T. Vu2 John A. Fuller3,4
John A. Fuller3,4 Melanie Freedman5
Melanie Freedman5 Jacqueline Bannon1,5
Jacqueline Bannon1,5 John T. Wilkins2,6
John T. Wilkins2,6 Judith T. Moskowitz5
Judith T. Moskowitz5 Lisa R. Hirschhorn5,7
Lisa R. Hirschhorn5,7 Amisha Wallia1,2,8
Amisha Wallia1,2,8 Charlesnika T. Evans1,2,9
Charlesnika T. Evans1,2,9
Introduction: During the coronavirus disease 2019 pandemic, high levels of burnout were reported among healthcare workers. This study examines the association of work absenteeism and frequency of thoughts in leaving current job with burnout among a cohort of healthcare workers during the COVID-19 pandemic.
Methods: A cross-sectional survey of healthcare workers was conducted from April-May, 2022 on healthcare workers from 10 hospitals, 18 immediate care centers, and 325 outpatient practices in the Chicago area and surrounding Illinois suburbs. Logistic regression models were used to assess the association of burnout scores (Oldenburg Burnout Inventory—OLBI) and its sub-scores (exhaustion and disengagement scores) with work absenteeism and thoughts of leaving work.
Results: One-fifth and 60% of respondents (n = 1,825) reported unplanned absenteeism and thoughts of leaving their job, respectively. After adjusting for covariates, higher burnout scores, especially exhaustion scores, were associated with increased odds of unplanned absenteeism (OR = 1.04, 95% CI: 1.01–1.08). Burnout scores and both sub-scores were also positively associated with the frequency of thoughts of leaving work, e.g., each unit increase in the OLBI burnout score was associated with 1.39 (95% CI: 1.34–1.43) times higher odds of thinking about leaving work “a lot/constantly” vs. “never”.
Discussion: Overall, this study cohort showed a positive association between burnout scores and unplanned work absenteeism (and frequency of thoughts in leaving job) during the COVID-19 pandemic. More research is needed to support healthcare worker well-being during times of stress and direct solutions to addressing unplanned absenteeism in the light of a pandemic.
Throughout the COVID-19 pandemic, frontline healthcare workers (HCWs) have experienced increased stress due to additional working hours, potential exposure to COVID-19, and subsequent COVID-19 related illness, all of which may have led to increased levels of burnout (1, 2). Indeed, a 2022 U.S. Surgeon General Report has highlighted the increasing rates of HCW burnout and its harmful consequences on the workforce and patient care as a result of the pandemic (3). In fact, a systematic review (4) that examined HCW and burnout during the pandemic showed that “task-related coping” was the primary strategy of coping for HCWs, in which HCWs would focus their efforts and thoughts at solving a problem to provide optimal results during stressful situations.
Previous studies (5) on HCWs have characterized burnout as having elements of emotional exhaustion (during patient contact), depersonalization (feeling detached from others), and lack of personal accomplishment (in personal skills, job success, and competency). Burnout is associated with poor quality of care and increases in medical errors, which can have dire consequences for patient safety and overall healthcare delivery effectiveness (3). Research has also found that higher levels of burnout are associated with lower levels of patient satisfaction, resulting in increased patient and family complaints (6). In addition, burnout can reduce quality of life and lead to adverse health behaviors among providers (7). Furthermore, a recent study (8) on HCWs (who had been working since before the start of the COVID-19 pandemic) reported high levels of depression and anxiety, which were significantly associated with higher levels of HCW burnout. Indeed, another systematic review (9) revealed that the current state of mental health in HCWs is exacerbated by the role of stress, anxiety, and depression, which can lead to burnout.
Particularly, negative consequences from HCW burnout have been widely reported in healthcare settings during COVID-19, which can include high rates of absenteeism and thoughts of leaving one's current job position. A range of possible causes for absenteeism were identified, including high levels of burnout, poor leadership, job dissatisfaction, lack of childcare, health issues, and job stress (10–13). Specific to burnout, one study (13) reported that 45.8% of physicians reported having a symptom of burnout, and it was directly associated with job satisfaction. Another study (14) that sampled 5,000 actively licensed nurses showed that nurses who had intention to leave their current job were more likely to report burnout and psychological stress. Indeed, increased rates of any type of HCW absenteeism (planned and unplanned) have been reported to negatively affect quality of healthcare services (14, 15). Another recent review on work absenteeism also emphasized the need for support for frontline HCWs, to mitigate elevated levels of burnout as well as staff shortage, particularly during a time of crisis (16). Finally, a scoping review showed that sustainable employment and absenteeism were directly impacted by exacerbated mental health problems as a result of the COVID-19 pandemic (17).
HCWs serve as the foundation of the healthcare system but worker absenteeism and turnover can have significant detrimental impacts on the quality of care and costs to the healthcare system (18, 19). Thus, understanding how burnout and other factors may be independently associated with work absenteeism and intentions to leave work will be important for developing efficacious interventions to reduce deleterious impacts of absenteeism and turnover to the healthcare environment. Existing studies that address work absenteeism during the pandemic are sparse, although a number have reported absenteeism due to COVID-19 in HCWs in low-income countries. This means there is a gap in the literature to fully understand the association between HCW burnout with absenteeism and thoughts of leaving work, specifically during a pandemic (20–23).
In this study, we assessed the cross-sectional association of burnout with work absenteeism and frequency of thoughts of leaving current position in a cohort of HCWs in Illinois during the COVID-19 pandemic.
A cross-sectional survey was conducted April–May 2022 in a cohort of HCWs currently being followed in a prospective cohort study [Northwestern Medicine (NM) SARS-CoV-2 cohort]. This is a large tertiary academic health care system located in the Chicago area and surrounding suburbs in Illinois. Details of the study and cohort have been previously published (24, 25). Briefly, the cohort includes HCWs from 10 hospitals, 18 immediate care centers, and 325 outpatient practices. Recruitment of the original cohort occurred in May 2020 with 6,510 HCWs enrolled in the study. In June 2021, 3,569 participants re-consented to enroll for continued follow-up (26). In April–May 2022, a survey via REDCap was sent to all 3,569 participants and 2,266 participants completed the survey with an overall response rate of 64.5%. Of 2,266 participants who completed the survey, 441 were excluded due to missing values of variables of interest (n = 439), retired (n = 1), and withdrawal from the study (n = 1) (Figure 1).
Burnout was the main independent variable in this study and measured using the Oldenburg Burnout Inventory (OLBI) (5) a validated 16–item inventory that measures two of these core dimensions of burnout—exhaustion and disengagement (from work). It has strong validity and reliability among English-speaking workers in the United States (5). Sample items include “I always find new and interesting aspects in my work”; “During my work, I often feel emotionally drained”; and “After my work, I usually feel worn out and weary.” Responses to each OLBI item range from 1 (totally disagree) to 4 (totally agree) (5). Thus, the overall Burnout scores range from 16 to 64, and the exhaustion and disengagement (from work) subscale scores range from 8 to 32.
Absenteeism was the main outcome defined by four questions: “Within the past 6 months, have you been absent from your job?”, “How often have you been absent in the last 6 months?”, “What were the reasons you were absent from work in the last 6 months?”, and “If the main reason was due to own illness, was it due to COVID-19?”. Aligned with previous studies on absenteeism, reasons for absenteeism were classified into planned or unplanned (23, 27). Planned absenteeism was defined as voluntary planned leave, such as annual leave, vacation, study leave, or maternity/paternity leave; whereas unplanned absenteeism was due to involuntary circumstances, such as emergency leave, short-term self-certified sickness absence, medically certified sickness, taking care of a family member, and other family responsibilities (Supplementary Table S1). We used this typology to categorize participants into 2 groups: (1) “Yes” for reporting unplanned absenteeism; and (2) “No” for no unplanned absenteeism. Participants who were in the unplanned only group may have also indicated planned absenteeism in addition to their unplanned absenteeism.
Similar to absenteeism, the construct of “intention to leave work” has been defined by the CDC (14) and studies of absenteeism (15, 28) as an individual's intention to leave the organization where one is currently employed, within a specific period of time. For this study, this construct was defined as “frequency of thoughts of leaving current job”. Participants were asked: “Within the past 6 months how often have you considered leaving your job?”, in which respondents were grouped by “never/a little” or “a lot/constantly”.
Participants also self-reported demographics (e.g., age, sex, race/ethnicity), household size, whether they lived with children under the age of 12, and type of occupation at NM. Occupation type was divided into four categories: registered nurse, physician, administrative roles, or other HCWs. Questions on past patient contact (such as taking care of COVID-19 positive patients in person) were also asked.
Respondents to the current survey (n = 2,266) were compared to nonrespondents (n = 1,303) to determine whether there were any significant differences in participants socio-demographic characteristics. Chi-square tests were conducted for comparisons of proportions for categorical characteristics and t-tests for comparison of mean values of continuous characteristics.
For the main analysis, we used binomial logistic regression models to estimate the odds of reporting unplanned absenteeism by burnout score and its sub-categories. Analyses were adjusted for age, sex, race/ethnicity, occupation, patient contact, and “having young children in the household.” A similar adjustment approach was used in multinomial logistic regression models when examining the association between OLBI scores with the frequency of thoughts in leaving current job (with the “never” as the referent). Furthermore, an additional model was conducted to include further adjustment for “unplanned absenteeism.” Two sensitivity analyses were also conducted. Due to COVID-19 illness being associated with mental health (29), we evaluated whether our results changed if HCWs who were absent due to COVID-19 illness were excluded from the analysis.
Furthermore, we encountered missing data in covariates, i.e., sex, occupation, patient contact, and living with young children (n = 205) in the study (Figure 1). To ensure the validity and completeness of our analyses, we performed additional sensitivity analysis, using chained equations to obtain 20 multiple imputed datasets to account for all missing values of covariates.
Statistical significance was defined at the p < 0.05 level. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
The final included sample size for analysis was 1,825 participants. Compared to non-respondents, survey respondents were significantly older (mean age 44.6 vs. 41.5, p < 0.001), and more likely to identify as White (81.5% vs. 75.1%, p < 0.001). Respondents also were significantly less likely to work as a physician (18.3% vs. 21.1%, p < 0.001) or registered nurse (28.6% vs. 33.9%, p < 0.001) compared to non-respondents. There was no significant difference in gender of respondents vs. non-respondents (82.2% female vs. 80.2% female) (Table 1).
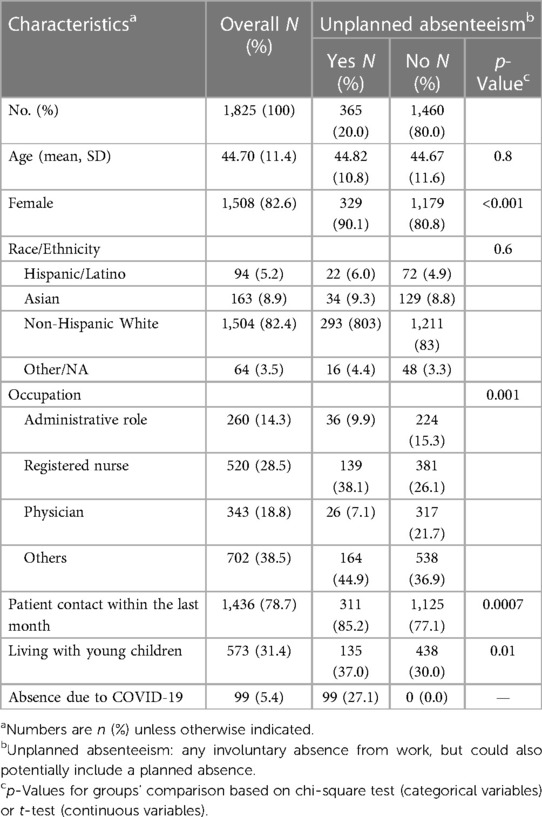
Table 1. Characteristics of the study sample by work absenteeism categories within the past 6 months between May and April 2022.
Approximately 20% of the cohort reported unplanned absenteeism (which could also include respondents with planned absences) (Supplementary Table S1). Within unplanned absenteeism, 78.6% were due to illness/injury/medical problems, and 23.8% due to family/personal obligations (Supplementary Table S2). Compared to those with no reports of unplanned absenteeism, unplanned absenteeism participants reported a significant higher proportion of being female, working as a nurse, working without patient contact, or living with younger children (p < 0.05) (Table 1). Exhaustion sub-scores were significantly higher in those with reporting unplanned absenteeism compared to those with no unplanned absenteeism in the unadjusted model (19.1 vs. 18.5, p = 0.007) (Table 2). Neither unadjusted overall burnout score (36.1 vs. 35.7, p = 0.056) or the disengagement subscale score (17.4 vs. 17.2, p = 0.42) differed between absenteeism groups (Table 2).
After adjusting for age, race/ethnicity, gender, occupation, patient contact, and having young children in the household, we observed an increase in the odds of reporting unplanned absenteeism for each score increment in overall burnout scores, but the association was only marginally statistically significant: (OR = 1.02, 95% CI: 1.00–1.03, p = 0.05). However, being older (OR = 1.02, 95% CI: 1.01–1.03), non-Hispanic Asian (vs. non-Hispanic White) (OR = 1.58, 95% CI: 1.03–2.43), a nurse (OR = 1.65, 95% CI: 1.07–2.54) or “other” job category (vs. administrative job) (OR = 1.58, 90% CI: 1.05–2.40), or having young children in the household (OR = 1.76, 95% CI: 1.34–2.30) were each associated with higher odds of reporting unplanned absenteeism. Male gender (OR = 0.62, 95% CI: 0.42–0.92), being a doctor (vs. administrative job) (OR = 0.35, 95% CI: 0.20–0.62), or work without patient contact (OR = 0.53, 95% CI: 0.38–0.75) had a lower odds of reporting unplanned absenteeism compared to those with no absence (Table 3). The association of exhaustion sub-scores by absenteeism remained after adjustment, (OR = 1.04, 95% CI: 1.01–1.08) (results not tabulated).
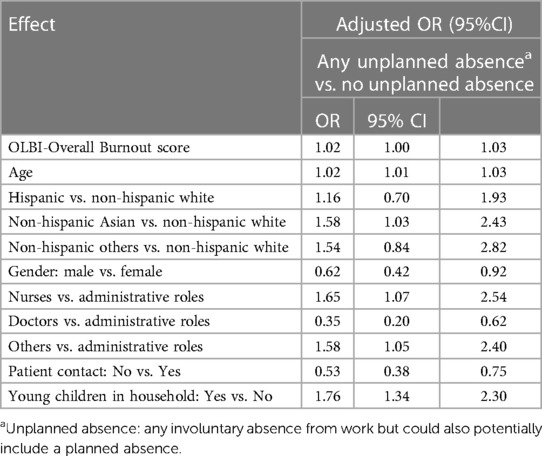
Table 3. Binomial logistic regression analysis of the association of unplanned absenteeism with burnout (OLBI scores) and covariates.
With frequency of thoughts of leaving one's job, 39.2% reported “never” thinking about leaving one's job, 39.6% reported “a little”, and 21.2% reported “a lot/constantly” thinking of leaving one's job. The frequency of thoughts of leaving one's job varied significantly by age and occupation: those who reported thinking “a lot/constantly” of leaving work were younger than other groups (mean age 42.8 compared to 46.15 and 44.29, p < 0.001). For occupation, more than a third (35%) of those who reported thinking “a lot/constantly” about leaving were registered nurses. Additionally, there was no significant difference in the proportion of individuals reporting any unplanned absenteeism based on their levels of thoughts about leaving work (Table 4). The unadjusted burnout score was significantly higher among those who reported frequent thoughts of leaving one's job compared to those with less frequent thoughts of leaving (“a lot/constantly”: 42.7 vs. “a little”: 36.7 vs. “never”: 31.3, p < 0.001). This association was the same for both exhaustion (p < 0.001) and disengagement subscale scores (p < 0.001) (results not tabulated). After adjustment, OLBI-overall burnout scores remained significantly and positively associated with the frequency of thoughts of leaving work (either “a lot/constantly” or “a little” vs. “never”). For example, the odds of reporting thinking about leaving work “a lot/constantly” vs. “never” was 1.39 (95% CI: 1.34–1.43) for each additional burnout score (Table 5). Results were consistent when sub-categories of burnout scores were analyzed. Both exhaustion and disengagement scores also showed a significant positive association with the frequency of thoughts of leaving work as “a lot/constantly” vs. “never”: OR (95% CI) were 1.56 (1.49–1.64) and 1.82 (1.72–1.93), respectively (data not tabled). In addition, being a nurse (vs. administrative job) and having no patient contact were associated with higher odds of reporting thinking about leaving work “a lot/constantly” (Table 5).
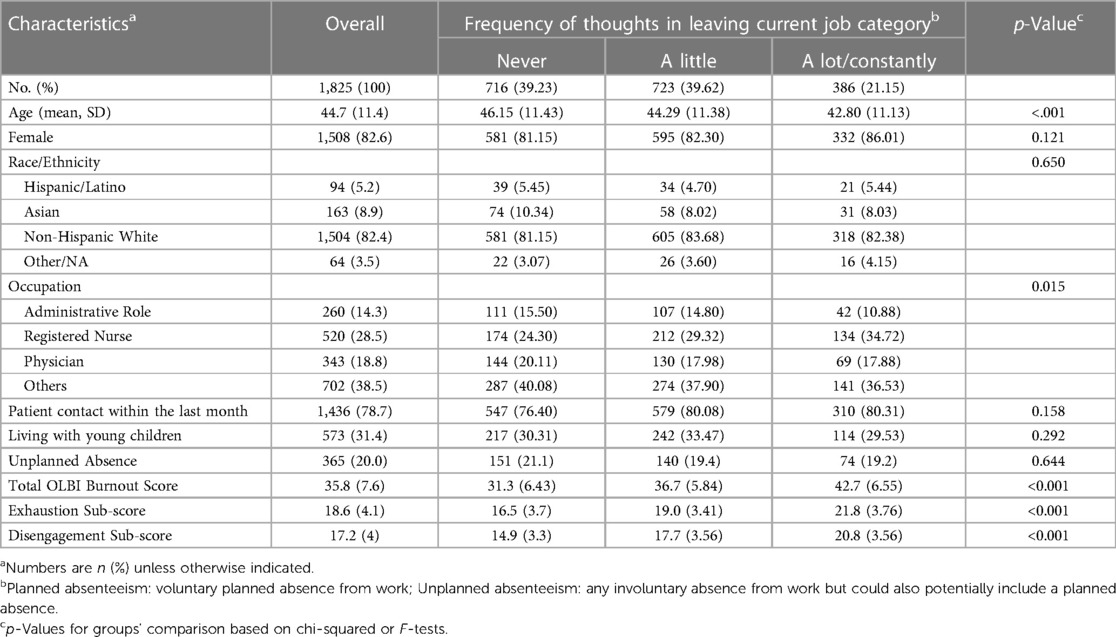
Table 4. Characteristics of the study sample by frequency of thoughts of leaving work within the past 6 months between May and April 2022.
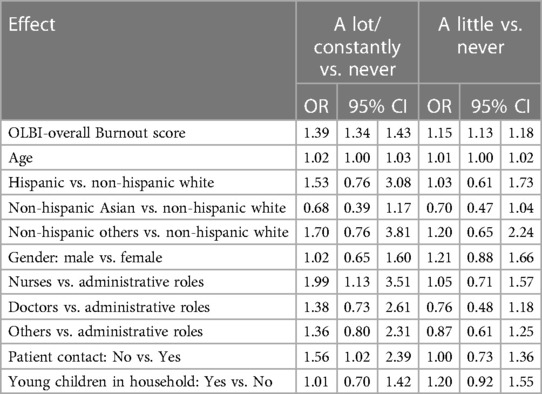
Table 5. Multinomial logistic regression analysis of the association between burnout (OLBI scores) and frequency of thoughts of leaving current job.
While there was an association between unplanned absenteeism and intention to leave work, the additional analyses to include further adjustment for “unplanned absenteeism” showed that this association was independent of the relationship between burnout score and intention to leave. For example, the odds of reporting frequent thoughts about leaving work “a lot/constantly” vs. “never” increased by 1.39 (95% CI: 1.35–1.44) for each score increment in burnout. These results were similar to the main analysis results, in which the association was also 1.39 (95% CI: 1.34–1.43). Thus, the results from our analysis adding unplanned absenteeism into the model demonstrated that the relationship between burnout scores and intention to leave work was not attenuated by unplanned absenteeism and remained statistically significant (results not tabulated).
In the first sensitivity analysis (with an exclusion of those who reported their absence was due to a COVID illness), we observed that the effect sizes of burnout sub-scores on unplanned absenteeism were similar to those in the models without the exclusion of COVID-19-related absences in the main analysis. However, the association between the overall burnout scores and unplanned absenteeism became statistically significant (p < 0.05) (result not tabulated). In the second sensitivity analysis accounting for missing values of covariates, similar associations/patterns were observed when comparing results from the main analysis with a complete case for both outcomes.
This cohort study surveyed 1,825 HCWs during the COVID-19 pandemic where one-fifth reported unplanned absenteeism and 60% reported thoughts about leaving their jobs. Overall, we observed a marginally significant association in the main analysis, but a significant association was found in both sensitivity analyses. Overall burnout scores were not associated with having unplanned absenteeism. However, burnout subscale of exhaustion scores were found to be significantly associated with reporting unplanned absenteeism, independent from COVID-19 illness status. Further, age, ethnicity, occupation, no patient contact, and having young children in the household—also correlated with higher likelihood of unplanned absenteeism. Furthermore, burnout scores and both sub-categories (exhaustion and disengagement) were significantly associated with higher frequency of thoughts of leaving one's current job.
These findings concur with similar studies that report that HCWs are reporting high levels of burnout at this specific point in time during the pandemic and that burnout could be one factor in explaining high rates of work absenteeism (30–33). The few studies available, however, focus on sick absenteeism (absence due to health reasons), which is consistent with this study's findings. The most recent cross-sectional study by Aiken et al. (34) reported that high stress work conditions were highly associated with burnout and job dissatisfaction, even in workplaces that were deemed “good to work”. Sexton et al. (35) reported significant increases in emotional exhaustion from 31% to 40% in a cohort of HCWs between 2019 and 2021, with only nurses having a steady increase over the 2 years. A cross-sectional survey by Dyrbye et al. (21) reported that 35% of the nurses reported scores that indicated burnout and nurses were more likely to be absent for more than 1 day within the past month, compared to those who were not burned out. It is important to note that the majority of studies available on HCW burnout is focused on nurses. Even prior to the epidemic, a study on nurses in Poland showed that excessive working hours were associated with burnout and higher odds of a sickness absence (36). Outside of sick leave, there were no other studies specific to family obligations, maternity/paternity leave, or conditions where individuals could not find proper work (reasons that were captured in this study).
Specific to work absenteeism, this study found that being a nurse was associated with higher odds of reporting unplanned absenteeism and more frequent thoughts of leaving the work position. Although this may have been because most nurses in this cohort were female, these findings are consistent with the recent U.S. Surgeon General Report, which revealed that nurses, particularly nurses living with young children, had a higher likelihood of reporting unplanned absenteeism. During the pandemic, other similar studies reported that female workers (who were nurses as well as other HCW positions) also reported higher scores of burnout and were more likely than men to face work disruptions as a result of childcare responsibilities (3, 11). Furthermore, the most frequently reported reason for unplanned absenteeism in this cohort was own illness, injury, or others/medical problems (n = 287, 15.7%), in which 99 participants reported that it was due to COVID-19. Alongside this, another large proportion of overall participants reported that their absenteeism was a result of family obligations (n = 87).
Similarly, a study by Gohar et al. reported that increases of sickness absences in HCWs could be attributed to sickness caused by COVID-19, the flu, injury and/or other health conditions (37). Likewise, another study showed that on average, HCWs took 12.5 absent days after having a COVID-19 infection (38). A study in Turkey (39) showed that there was a total lost time from work of 14,635 days in their HCWs across the span of 1 year (2020–2021). A study in Brazil (40) showed that absenteeism due to a medical reason increased from 633 individuals to 837 from 2019 to 2020, in which nursing assistants were reported to have the highest frequency of medical leave. Other existing literature on HCW absenteeism also reported that sick absenteeism in HCWs was due to a result of COVID-19 vaccine-associated side effects (22, 41). In addition, others reported differing severity in percentages of HCW sickness absenteeism, pending the wave and phase of the COVID-19 pandemic (42). Specific to nurses, Barr (43) reported that 21% of their nurse cohort were considering leaving their job—with burnout and work environment being the top two causes of their intention to leave work.
This study findings also showed that OLBI-overall burnout scores were positively associated with frequency of thoughts to leave work with 21% of this sample reporting thoughts of leaving their job a lot/constantly over the previous 6 months Other studies (pre-COVID-19) have also reported the link between burnout and intention to leave work due to stress (13, 14, 28). LeClaire et al. (44) found that HCWs experiencing burnout had a 50% greater odds of intention to leave work in the next 2 years (defined as likelihood of leaving their practice) than HCWs not experiencing burnout. Literature on the pandemic and rates of absenteeism are primarily international (outside of the US).
A recent burnout framework for HCWs, specific to the pandemic, has listed both absenteeism and intention to leave work as potential sequelae of burnout (31). While frameworks and recommendations exist to reduce burnout in a healthcare setting (3, 20), researchers have yet to provide an extension of a framework for HCWs that targets work absenteeism during extraordinarily stressful times such as a pandemic (16).
The present study is one of very few studies that provides insight in HCWs' experiences of burnout and its association with absenteeism and frequency of thoughts of leaving work in a large cohort of HCWs. However, this study has several limitations. The study is cross-sectional, which limits the ability to determine the causal mechanism linking work absenteeism, frequency of thoughts of leaving work, and burnout. Secondly, there was a lack of information on all previous COVID-19 infections/illnesses in our data, so we were unable to investigate whether the association of interest could be influenced by COVID-19 infection/illness status (or recovery times). However, the association remained similar when we excluded those who reported their absence was due to a COVID-1I illness from the analysis. Furthermore, other studies (45) have also reported that post-COVID-19 patients may also have differing rates of absenteeism and intention to leave work, as a result of slow recovery times. Although our survey did inquire about the reason for absenteeism, we were unable to investigate recovery times and whether intention to work was associated with differing recovery times.
The study findings have important implications for experiences within the HCW workforce during the pandemic. Healthcare systems around the world have faced tremendous stress due to the COVID-19 pandemic. Hence, the findings can provide information on the state of burnout and psychological well-being among HCWs—that could be potentially generalizable to other healthcare organizations during the pandemic. Secondly, as burnout can have negative consequences on healthcare delivery effectiveness and significant cost implications due to medical errors, this study provides insight on how burnout can directly impact HCW absenteeism and future turnover. Maintaining psychological and physical well-being are essential to ensuring a healthy HCW workforce. Thus, the findings of this study indicate how HCWs respond to significant stressors, such as the COVID-19 pandemic, and contribute to lessons learned on how to support HCWs in reducing burnout and ensuring resiliency in the healthcare delivery system.
In this cohort of HCWs, a significant portion of the HCW cohort reported unplanned absenteeism or were considering leaving their jobs. Notably, the sensitivity analyses showed a statistically significant association between burnout scores and unplanned absenteeism, which was underestimated in the main analyses. We also found that higher levels of burnout were associated with higher frequency of thoughts to leave current position in healthcare. Exhaustion scores were also significantly associated with unplanned absenteeism. Continued examinations of trends in unplanned work absenteeism and frequency of thoughts of leaving work can be useful in fully understanding the impact of post-COVID conditions on burnout. Hence, this study calls for the development of organizational and individual-level programs that can help HCWs cope with the stress of working, particularly during unprecedented times such as COVID-19.
The dissemination of data results to study participants and or patient organizations in this research project is not available nor possible due to restrictions that are applied to the public availability of these data and our data access agreements for the current study. Requests to access the datasets should be directed toaGN3c3R1ZHlAbm9ydGh3ZXN0ZXJuLmVkdQ==.
The studies involving humans were approved by Research ethics approval was obtained from the Northwestern University Institutional Review Board Office (ID#: STU00212515). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
CL: Investigation, Methodology, Writing – original draft, Writing – review & editing. TV: Data curation, Formal Analysis, Investigation, Methodology, Software, Validation, Writing – review & editing, Resources, Visualization. JF: Writing – review & editing. MF: Writing – review & editing. JB: Writing – review & editing. JW: Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review & editing. JM: Conceptualization, Funding acquisition, Investigation, Methodology, Validation, Writing – review & editing. LH: Conceptualization, Funding acquisition, Writing – review & editing. AW: Conceptualization, Funding acquisition, Writing – review & editing. CE: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This work was supported by the Northwestern University Clinical and Translational Sciences Institute (UL1TR001422), the Northwestern Memorial Foundation, and from the Peter G. Peterson Foundation Grant.
We are grateful to the NM employees who volunteered to participate in this project.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2023.1272285/full#supplementary-material
1. Zareei M, Tabanejad Z, Oskouie F, Ebadi A, Mesri M. Job burnout among nurses during COVID-19 pandemic: a systematic review. J Educ Health Promot. (2022) 11:107. doi: 10.4103/jehp.jehp_797_21
2. Wei H, Aucoin J, Kuntapay GR, Justice A, Jones A, Zhang C, et al. The prevalence of nurse burnout and its association with telomere length pre and during the COVID-19 pandemic. PLoS ONE. (2022) 17(3):e0263603. doi: 10.1371/journal.pone.0263603
3. Surgeon General US. Addressing Health Worker Burnout. Public Health Service (2022). Available at: https://www.hhs.gov/sites/default/files/health-worker-wellbeing-advisory.pdf
4. Rossi MF, Gualano MR, Magnavita N, Moscato U, Santoro PE, Borrelli I. Coping with burnout and the impact of the COVID-19 pandemic on workers’ mental health: a systematic review. Front Psychiatry. (2023) 14:1139260. doi: 10.3389/fpsyt.2023.1139260
5. Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. (Jun 2016) 15(2):103–11. doi: 10.1002/wps.20311
6. Profit J, Sharek PJ, Amspoker AB, Kowalkowski MA, Nisbet CC, Thomas EJ, et al. Burnout in the NICU setting and its relation to safety culture. BMJ Qual Saf. (Oct 2014) 23(10):806–13. doi: 10.1136/bmjqs-2014-002831
7. Salvagioni DAJ, Melanda FN, Mesas AE, Gonzalez AD, Gabani FL, Andrade SM. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS ONE. (2017) 12(10):e0185781. doi: 10.1371/journal.pone.0185781
8. Bannon J, Evans CT, Freedman M, Lee C, Vu TH, Wallia A, et al. Psychological wellbeing and the association with burnout in a cohort of healthcare workers during the COVID-19 pandemic. Front Health Serv. (2022) 2:994474. doi: 10.3389/frhs.2022.994474
9. Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. (2020) 18(1):100. doi: 10.1186/s12960-020-00544-1
10. Bordignon M, Monteiro MI. Predictors of nursing workers’ intention to leave the work unit, health institution and profession. Rev Lat Am Enfermagem. (2019) 27:e3219. doi: 10.1590/1518-8345.3280.3219
11. Dall'Ora C, Ball J, Reinius M, Griffiths P. Burnout in nursing: a theoretical review. Hum Resour Health. (2020) 18(1):41. doi: 10.1186/s12960-020-00469-9
12. Yue Z, Qin Y, Li Y, Wang J, Nicholas S, Maitland E, et al. Empathy and burnout in medical staff: mediating role of job satisfaction and job commitment. BMC Public Health. (2022) 22(1):1033. doi: 10.1186/s12889-022-13405-4
13. Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. (2012) 172(18):1377–85. doi: 10.1001/archinternmed.2012.3199
14. Han K, Trinkoff AM, Gurses AP. Work-related factors, job satisfaction and intent to leave the current job among United States nurses. J Clin Nurs. (2015) 24(21–22):3224–32. doi: 10.1111/jocn.12987
15. Kivimaki M, Vanhala A, Pentti J, Länsisalmi H, Virtanen M, Elovainio M, et al. Team climate, intention to leave and turnover among hospital employees: prospective cohort study. BMC Health Serv Res. (2007) 7:170. doi: 10.1186/1472-6963-7-170
16. Tujjar O, Simonelli M. Absenteeism of frontline healthcare workers during COVID-19: the need for a framework of support. SN Compr Clin Med. (2020) 2(12):2715–7. doi: 10.1007/s42399-020-00609-1
17. van den Broek A, van Hoorn L, Tooten Y, de Vroege L. The moderating effect of the COVID-19 pandemic on the mental wellbeing of health care workers on sustainable employability: a scoping review. Front Psychiatry. (2022) 13:1067228. doi: 10.3389/fpsyt.2022.1067228
18. Hewitt DB, Ellis RJ, Chung JW, Cheung EO, Moskowitz JT, Huang R, et al. Association of surgical resident wellness with medical errors and patient outcomes. Ann Surg. (2021) 274(2):396–402. doi: 10.1097/SLA.0000000000003909
19. Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med. (2018) 178(10):1317–31. doi: 10.1001/jamainternmed.2018.3713
20. De Hert S. Burnout in healthcare workers: prevalence, impact and preventative strategies. Local Reg Anesth. (2020) 13:171–83. doi: 10.2147/LRA.S240564
21. Dyrbye LN, Shanafelt TD, Johnson PO, Johnson LA, Satele D, West CP. A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs. (2019) 18:57. doi: 10.1186/s12912-019-0382-7
22. Maltezou HC, Panagopoulos P, Sourri F, Giannouchos TV, Raftopoulos V, Gamaletsou MN, et al. COVID-19 vaccination significantly reduces morbidity and absenteeism among healthcare personnel: a prospective multicenter study. Vaccine. (2021) 39(48):7021–7. doi: 10.1016/j.vaccine.2021.10.054
23. Belita A, Mbindyo P, English M. Absenteeism amongst health workers–developing a typology to support empiric work in low-income countries and characterizing reported associations. Hum Resour Health. (2013) 11:34. doi: 10.1186/1478-4491-11-34
24. Wilkins JT, Hirschhorn LR, Gray EL, Wallia A, Carnethon M, Zembower TR, et al. Serologic status and SARS-CoV-2 infection over 6 months of follow up in healthcare workers in Chicago: a cohort study. Infect Control Hosp Epidemiol. (2022) 43(9):1207–15. doi: 10.1017/ice.2021.367
25. Wilkins JT, Gray EL, Wallia A, Hirschhorn LR, Zembower TR, Ho J, et al. Seroprevalence and correlates of SARS-CoV-2 antibodies in health care workers in Chicago. Open Forum Infect Dis. (2021) 8(1):ofaa582. doi: 10.1093/ofid/ofaa582
26. Evans CT, DeYoung BJ, Gray EL, Wallia A, Ho J, Carnethon M, et al. Coronavirus disease 2019 (COVID-19) vaccine intentions and uptake in a tertiary-care healthcare system: a longitudinal study. Infect Control Hosp Epidemiol. (2022) 43(12):1806–12. doi: 10.1017/ice.2021.523
27. Mat Saruan NA, Mohd Yusoff H, Mohd Fauzi MF, Wan Puteh SE, Muhamad Robat R. Unplanned absenteeism: the role of workplace and non-workplace stressors. Int J Environ Res Public Health. (2020) 17(17):1–16. doi: 10.3390/ijerph17176132
28. Ayalew E, Workineh Y, Semachew A, Woldgiorgies T, Kerie S, Gedamu H, et al. Nurses’ intention to leave their job in Sub-Saharan Africa: a systematic review and meta-analysis. Heliyon. (2021) 7(6):e07382. doi: 10.1016/j.heliyon.2021.e07382
29. Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. (2021) 8(5):416–27. doi: 10.1016/S2215-0366(21)00084-5
30. Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. (2021) 126:252–64. doi: 10.1016/j.neubiorev.2021.03.024
31. Maunder RG, Heeney ND, Hunter JJ, Strudwick G, Jeffs LP, Ginty L, et al. Trends in burnout and psychological distress in hospital staff over 12 months of the COVID-19 pandemic: a prospective longitudinal survey. J Occup Med Toxicol. (2022) 17(1):11. doi: 10.1186/s12995-022-00352-4
32. Shechter A, Norful AA. A peripandemic examination of health care worker burnout and implications for clinical practice, education, and research. JAMA Netw Open. (2022) 5(9):e2232757. doi: 10.1001/jamanetworkopen.2022.32757
33. Parent-Lamarche A, Laforce S. A moderated mediation analysis of new work-related stressors, psychological distress, and absenteeism in health care during a pandemic: is recognition the cure for preventing falling in battle? J Occup Environ Med. (2022) 64(10):839–47. doi: 10.1097/JOM.0000000000002619
34. Aiken LH, Lasater KB, Sloane DM, Pogue CA, Fitzpatrick Rosenbaum KE, Muir KJ, et al. Physician and nurse well-being and preferred interventions to address burnout in hospital practice: factors associated with turnover, outcomes, and patient safety. JAMA Health Forum. (2023) 4(7):e231809. doi: 10.1001/jamahealthforum.2023.1809
35. Sexton JB, Adair KC, Proulx J, Profit J, Cui X, Bae J, et al. Emotional exhaustion among US health care workers before and during the COVID-19 pandemic, 2019–2021. JAMA Netw Open. (2022) 5(9):e2232748. doi: 10.1001/jamanetworkopen.2022.32748
36. Kowalczuk K, Krajewska-Kulak E, Sobolewski M. Working excessively and burnout among nurses in the context of sick leaves. Front Psychol. (2020) 11:285. doi: 10.3389/fpsyg.2020.00285
37. Gohar B, Lariviere M, Nowrouzi-Kia B. Sickness absence in healthcare workers during the COVID-19 pandemic. Occup Med (Lond). (2020) 70(5):338–42. doi: 10.1093/occmed/kqaa093
38. Sakr CJ, Fakih L, Melhem NM, Fakhreddine M, Musharrafieh U, Banna H, et al. COVID-19 infections and predictors of sickness related absences among healthcare workers: the experience of a tertiary care center with the COVID-19 pandemic. J Occup Environ Med. (2023) 65(7):590–4. doi: 10.1097/JOM.0000000000002857
39. Pirdal BZ, Toplu FS, Esen BK, Aydin SN, Erginoz E, Can G. An assessment on loss of workforce due to COVID-19 among healthcare personnel: a university hospital experience. Work. (2022) 73(1):59–67. doi: 10.3233/WOR-211308
40. Garbin AJI, Nascimento C, Zacharias FCM, Garbin CAS, Moimaz SAS, Saliba NA. Sickness absenteeism of primary health care professionals before and during the COVID-19 pandemic. Rev Bras Enferm. (2022) 75(Suppl 1):e20220028. doi: 10.1590/0034-7167-2022-0028
41. Chrissian AA, Oyoyo UE, Patel P, Lawrence Beeson W, Loo LK, Tavakoli S, et al. Impact of COVID-19 vaccine-associated side effects on health care worker absenteeism and future booster vaccination. Vaccine. (2022) 40(23):3174–81. doi: 10.1016/j.vaccine.2022.04.046
42. Al-Nuaimi AA, Abdeen S, Abed Alah M, AlHajri S, Semaan S, Al-Kuwari MG. Sickness absenteeism among primary health care workers in Qatar before and during the COVID-19 pandemic. J Occup Med Toxicol. (2023) 18(1):3. doi: 10.1186/s12995-023-00369-3
43. Barr P. Moral distress and considering leaving in NICU nurses: direct effects and indirect effects mediated by burnout and the hospital ethical climate. Neonatology. (2020) 117(5):646–9. doi: 10.1159/000509311
44. LeClaire M, Poplau S, Linzer M, Brown R, Sinsky C. Compromised integrity, burnout, and intent to leave the job in critical care nurses and physicians. Crit Care Explor. (2022) 4(2):e0629. doi: 10.1097/CCE.0000000000000629
Keywords: healthcare workers, absenteeism, COVID-19, burnout, psychological health
Citation: Lee C, Vu TH-T, Fuller JA, Freedman M, Bannon J, Wilkins JT, Moskowitz JT, Hirschhorn LR, Wallia A and Evans CT (2023) The association of burnout with work absenteeism and the frequency of thoughts in leaving their job in a cohort of healthcare workers during the COVID-19 pandemic. Front. Health Serv. 3:1272285. doi: 10.3389/frhs.2023.1272285
Received: 3 August 2023; Accepted: 13 November 2023;
Published: 29 November 2023.
Edited by:
Fraser Gaspar, Mitre, United StatesReviewed by:
Mats Brommels, Karolinska Institutet (KI), Sweden© 2023 Lee, Vu, Fuller, Freedman, Bannon, Wilkins, Moskowitz, Hirschhorn, Wallia and Evans. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cerina Lee amFlLmxlZTRAbm9ydGh3ZXN0ZXJuLmVkdQ==
Abbreviations COVID-19, coronavirus disease; HCW, healthcare worker; OLBI, oldenburg burnout inventory; US, United States.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.