
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Health Serv. , 01 August 2023
Sec. Implementation Science
Volume 3 - 2023 | https://doi.org/10.3389/frhs.2023.1227360
Background: Despite the overwhelming evidence of its effectiveness, there is poor implementation of take-home naloxone by pharmacists. Barriers have been explored and mapped to the capability, opportunity, motivation—behaviour (COM-B) model of behaviour change, yet no theoretically informed implementation strategies that target known barriers have been developed. Single-session implementation strategies have been proposed as a simple, scalable way to target multiple barriers.
Methods: Qualitative participatory methods, incorporating design-thinking principles, were used to develop the key messages of a single-session implementation strategy. The key messages were drafted against COM-B mapped implementation barriers identified in the literature. A participatory workshop involving a pre-mortem exercise and incorporating design-thinking principles were used to refine the messages and generate methods for dissemination. Messages were mapped to interview questions to naturally illicit stories and delivered via storytelling from a pharmacist, a general practitioner, and a person with lived experience of using naloxone.
Results: A 3 minute 40 second video and a two-page printable infographic were developed and hosted on a website, with links to additional downloadable resources as a single-session implementation strategy. Email was the preferred method for receiving simple professional development communications, with social media also widely accessed.
Discussion: Implementation science, behavioural change theory, and participatory design methods are a complementary combination to develop implementation strategies. Some pharmacists questioned the participatory design approach to developing an implementation strategy, as it was outside of their comfort zone. However, the participatory process involving end-users resulted in unique ideas that are unlikely to have been generated using more traditional consultative approaches. The delivery as a single-session implementation strategy allows for widespread dissemination and delivery at scale.
Each day in Australia, approximately 5 people die, 150 people are hospitalised, and 14 people are treated in emergency departments for opioid-related health concerns (1–3). Naloxone is a life-saving medication that reverses the effect of an opioid overdose with few side effects and no psychoactive or addictive qualities (4). Take-home naloxone (THN) is an evidence-based programme of providing naloxone and educating laypersons (e.g., people taking opioids and friends, family members, and anyone who may witness an overdose) on recognising and responding to an opioid overdose, including the administration of naloxone (4). THN saves lives and should be implemented at scale worldwide (5); however, THN programmes are poorly implemented despite the overwhelming evidence of their safety and effectiveness (6–8).
One avenue to improve the distribution of naloxone is provision of THN by community pharmacists. Due to their geographical distribution, long opening hours, role in other harm reduction services, and ability to talk with consumers without them needing to schedule an appointment, community pharmacists can reach the broad and diverse at-risk population who use illicit and/or prescription opioids. Pharmacists appear to generally support overdose education and naloxone distribution (9–12). However, a number of barriers to implementation of naloxone by pharmacists exist including the perception of the pharmacists of a lack of time, lack of awareness, workflow issues, and perceived poor comprehension by patients, stigma, training, cost, and remuneration (13–17). Implementation strategies that have been developed and tested include education programmes, academic detailing, screening tools, checklists, and pocket guides (11, 12). Strategies that address underlying stigma are needed as well as implementation strategies that may be scaled up.
In the past decade, several major barriers to implementing THN provision by community pharmacists have been removed. For example, in Australia in 2016, naloxone was down-scheduled from a prescription-only to a pharmacist-only medicine (18). This rescheduling removed a significant barrier to the implementation of THN as it enabled pharmacists to dispense naloxone without a prescription. Two other major implementation barriers were tackled in 2019 when free THN was piloted in three states of Australia (19), removing the cost barrier for patients and providing remuneration for pharmacists in the form of a dispensing fee. Unfortunately, outside of providing a dispensing fee, the roll-out of the pilot lacked additional implementation strategies for pharmacists or an awareness campaign for the public (19). Many barriers to THN access remained, including poor communication and education on THN, and harm reduction not being normalised across the sector (15). The study described here was conceived to demonstrate one approach that could be helpful in this regard following on from the work of Nielsen and Olsen (15).
Nielsen and Olsen (15) interviewed 37 Australian pharmacists to investigate the barriers to THN implementation and used the capability, opportunity, motivation—behaviour (COM-B) model to analyse their data. The COM-B model sits at the core of the behaviour change wheel (BCW), which is used to inform the development of interventions and implementation strategies by purposefully targeting identified barriers (20). The model posits that for a behaviour (B) to occur, the person needs the capability (C), opportunity (O), and motivation (M) to do so. Nielsen and Olsen (15) findings highlighted that in terms of capability, pharmacists had poor knowledge and low confidence in relation to dispensing naloxone and engaging with consumers on the topic of overdose. Regarding physical opportunity, there was poor availability of naloxone and time was a barrier, whilst social opportunity barriers related to negative attitudes towards harm reduction and a limited understanding of both naloxone's benefits and the population at risk of overdose. Pertaining to motivation, some pharmacists had negative attitudes towards people dependent on opioids and found the lack of remuneration as demotivating.
In this paper, we outline the development of a “single session for implementation strategy” to target identified implementation barriers to the provision of take-home naloxone by community pharmacists. To date, there appear to be few implementation strategies to increase the provision of THN targeting community pharmacists that are mapped to theory or identified barriers (12). Single sessions for implementation strategies are a new concept adapted from single-session patient-level interventions (21, 22). Single sessions for implementation involve a theory-led one-off encounter with a provider that can target multiple implementation determinants (22). They are “targeted, theory-informed activities aimed at promoting the uptake and sustainment of evidence-based clinical practices among clinicians” (21). In this study, we developed a short video, hosted on a website alongside an infographic and links to THN resources, as a single-session implementation strategy for THN. Furthermore, we integrate design-thinking methods into the implementation strategy development process through participatory workshops.
Whilst design-led approaches to driving healthcare innovation are widespread (23, 24), design methods are still in their infancy in implementation science, particularly with healthcare clinicians as active participants (25). In the expansive discipline of design, a number of process models and methods are human-centred (26–29). Whilst often conflated as “design thinking” (30), over 300 qualitative and quantitative methods (31) from ethnographic studies to rapid prototyping are drawn upon for problem-solving, aiming to improve project outcomes through the use of empathic, iterative, speculative, and generative methods. Such an approach to innovation does not always guarantee specific, measurable outcomes (29). By contrast, the goal of implementation is to increase the uptake of new evidence-based innovations into practice (32). Whilst implementation science and design disciplines may appear disparate, they share a common ground in their focus on finding solutions to problems or needs through human-centred, participatory methods. One such method—“co-design”—has the ability to build partners, alliances, and coalitions for action and can confirm or challenge previously held ideas and rapidly create artefacts for testing (33). We describe our process of using design-thinking with community pharmacists in combination with theoretically informed mapping of barriers to the implementation of THN provision.
In the present study, we build on the work of Nielsen and Olsen (15), with the aim to design a single-session implementation strategy targeting their identified barriers. Specifically, the study intend to engage a group of pharmacists in a design-thinking process to tackle the problem of how to encourage pharmacists to stock and dispense over the counter naloxone, and particularly, what messages would resonate with pharmacists and how to disseminate the information.
Qualitative participatory methods, incorporating design-thinking principles, were used to develop the key messages of a single-session implementation strategy. Ethics approval was obtained from Curtin University Human Research Ethics Committee (Reference number HRE2019-0816).
First, preliminary messages were drafted by the lead researcher and programme lead at the West Australian Department of Health Mental Health Commission against the identified barriers mapped to COM components of the behaviour change wheel (15) to streamline the subsequent meeting with export stakeholders. These messages (see Table 1) were reviewed and amended at an expert stakeholder advisory group meeting (n = 5) consisting of subject matter experts, policymakers, and the State director of one of the leading professional societies for pharmacists.
Next, a 2.5-h participatory and design-thinking-oriented workshop with community pharmacists (n = 8) was conducted to gather ideas and perspectives on the key messages. Purposive and snowball sampling was used to recruit participants. Informed consent was obtained from all participants prior to the workshop, which was held on February 2020 at the offices of the WA branch of the Pharmaceutical Society of Australia (PSA). Workshop instructions were provided to the participants, including sharing experiences, deferring judgement, and respecting the opinions of others. The workshop was facilitated by an expert in design-thinking (PE) and a pharmacist with expertise in implementation science (JM). Data were collected through notetaking and collection of written documents and photographs (JM).
After introductions and provision of background information on naloxone, the participants discussed how they receive professional news and information generally and their preferred format for education and training. This initial question acted as an icebreaker and to gauge important information on improving dissemination to pharmacists. In addition, and in line with the behaviour change wheel process for developing interventions, the pharmacists were asked to consider the key behaviours associated with the provision of THN and what were the most important for a change to occur.
A pre-mortem exercise (34) was conducted with the participants, whereby the pharmacists were posed with the problem, “Provision of naloxone is not occurring,” followed by the question, “How do we get pharmacists to stock naloxone, initiate conversations about and educate on naloxone with their patients on long-term strong opioids?” A pre-mortem exercise is a methodology that “uses prospective hindsight—a group imagines a failure and generates an explanation for it—to reduce the likelihood of the failure” (34). The pre-mortem exercise used the design-thinking iterative and cyclic phases of (i) ideation (divergence), followed by (ii) ideation (convergence), and (iii) prototyping.
(i) Ideation (divergence): In groups of —two to three, consisting of participants sitting at the same table, individual contributions to the pre-mortem question were written on sticky notes and placed in the middle of the table. Examples of ideas were not proposed to the participants so not to lead their thinking. The participants were asked to generate lots of ideas quickly, even ones that seemed ridiculous, to address the research question. It was explained that ideas did not need to be developed in detail and could be conferred in any form, for example, a single word, a picture, or a dot point.
To help guide and expand their thinking, the groups were given scenarios (based on COM-B) of different reasons why supply may not be occuring. Group 1 were to consider the scenario that pharmacists were uncertain about providing naloxone as it would take too long, is too complicated, may offend patients, and would condone misuse. This was based on the Motivation component of COM-B and barriers of time and seeing naloxone as a moral hazard. Group 2 were to consider that pharmacists did not know how to provide naloxone, based on the capability component of the COM-B and barriers of lack of awareness and poor knowledge. Finally, Group 3 were to consider pharmacists as being uncertain about providing naloxone as they did not feel it was their role. This scenario was focussed on the opportunity component of the COM-B and barrier of harm reduction not being normalised.
(ii) Ideation (convergence): The participant groups were asked to cluster ideas into themes, select two ideas (through dot-voting or “dot-mocracy”), and to share the idea with the most votes with the other groups. Following this, ideation (divergence) round 2: Using a divergent idea-generating method—the “Merlin” method (35)—the participants developed new ideas from the shortlisted two on large pieces of paper, applying the principles of “enlarge,” “shrink,” “vanish,” and “reverse” on their selected idea.
(iii) Prototyping: One idea from each group was selected by consensus for paper prototyping.
The participants were presented with the message drafted by the expert advisory group. A group discussion was facilitated on the messages, their wording, and which they believed may shift the attitudes or intentions of the pharmacists to provide naloxone.
First, ideas were clustered into themes, and outputs conducive to be delivered in a video or infographic were added to the key messages. A video and infographic were selected as the modes of delivery due to the COVID-19 pandemic, making face-to-face and time-consuming professional development activities inappropriate for pharmacists. Next, the intervention functions and behaviour change techniques (BCTs) were considered to try and include as many as possible in the single-session implementation strategy. Three different narrators, a pharmacist, a general practitioner, and an end-user, were chosen to provide a credible source to the messages.
An interview guide was developed whereby interview questions were mapped to the key messages, to prompt a natural delivery rather than dictation of the key messages. Campaign branding and video production were coordinated by the Make it Happen initiative of the Digital Agency Media on Mars. The dissemination plan was developed based on the responses to Activity 1, as well as what was feasible with the intervention only targeting the WA pharmacists (rather than pharmacists nationally).
Eight pharmacists attended the participatory co-design workshop: four pharmacy owners, two employee pharmacists, one country locum pharmacist, and one professional services manager for a pharmacy group. One of the attendees was an owner and board member of the WA branch of the Pharmacy Guild of Australia (membership body for pharmacy owners). Of the eight attending pharmacists, none had previously given out naloxone over the counter, and dispensing had only occurred for Doctor's Bags, as opposed to prescriptions for patients. Half of the participants had naloxone in stock in their pharmacy at the time of the workshop, and five of the eight worked in a pharmacy that is registered to provide medication-assisted treatment for opioid dependence (MATOD) (see Table 2).
Initially, 10 messages were drafted against the barriers to naloxone provision by community pharmacists by the research lead and programme lead at the West Australian Department of Health Mental Health Commission and presented to the expert advisory panel. The panel adapted the messages, added three new messages and clustered them into five themes: (i) Commonwealth pilot—take advantage of it, (ii) Public health issue, (iii) Pharmacists’ role, (iv) Myth busters, and (v) Dispensing/process education (see Table 2). The final messages and information for the video, infographic, and website were mapped across all domains of the COM-B and identified barriers from Nielsen and Olsen (15) as presented in Table 3.
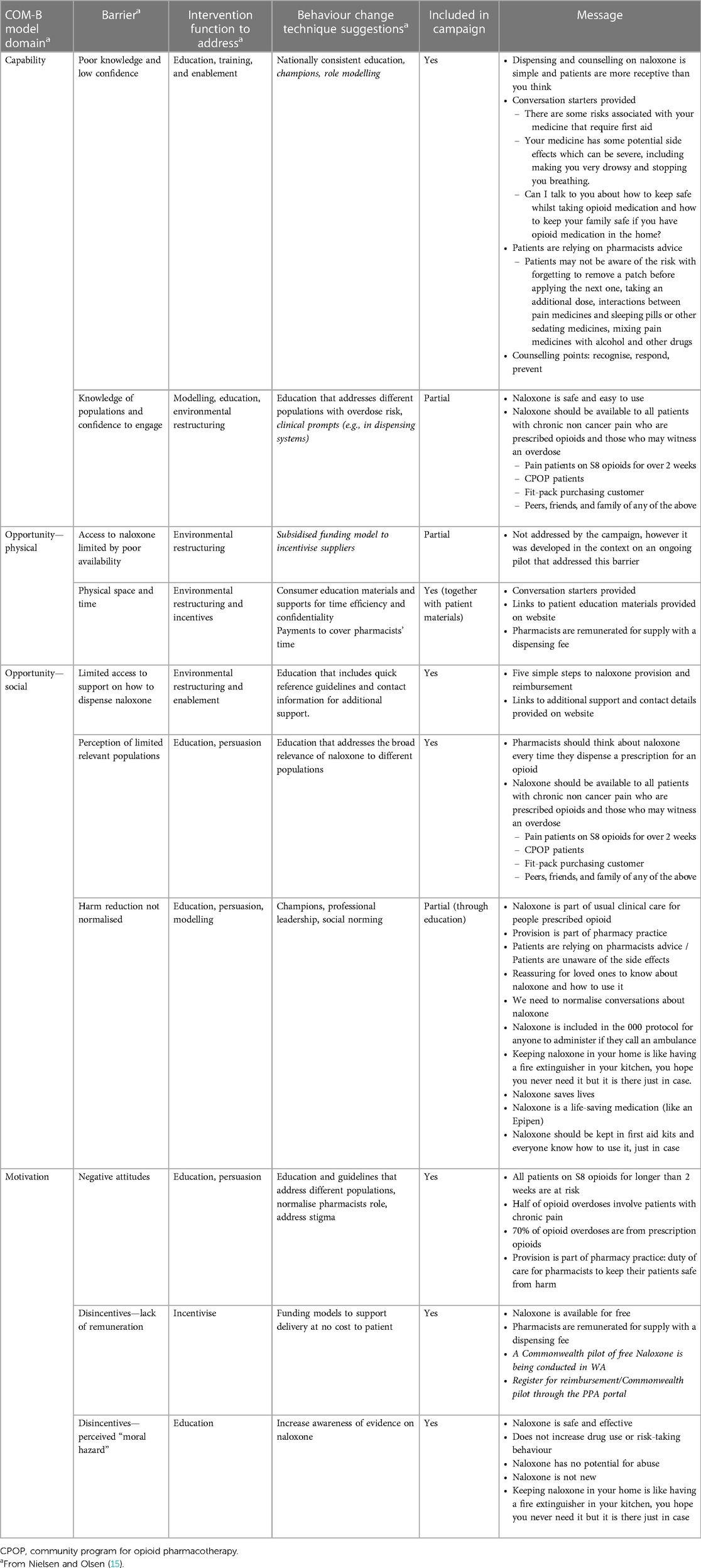
Table 3. Campaign messages mapped to the behaviour change wheel COM-B barriers identified in Nielsen and Olsen (15).
A 3 min and 40 s video was developed. The video included interviews with a pharmacist, a general practitioner, and a person with lived experience. The messages in the video addressed barriers to implementation, while being delivered naturally, as a response to conversational questions asked by the video director. To complement the video and to address other identified barriers, a two-page printable infographic (provided in the Supplementary Material) was developed. Both the video and infographic were hosted on a Squarespace website, www.pharmacy-opioid-harm-reduction.com. The website included a list of other resources including patient leaflets, training videos, and contact details for information on the naloxone pilot and for the research team.
Emails were the primary method that pharmacists received professional pharmacy-related information and messages. The participants reported checking their personal emails on average once per day and professional emails multiple times per day, including at lunchtime and in the evening. Emails from the Pharmacy Guild (membership body for pharmacy owners) were most read by pharmacy owners. Daily emails by the Australian Journal of Pharmacy (AJP) were popular with other daily “pharmacy news” emails skimmed or looked at occasionally (e.g., Pharmacy News and Pharmacy Daily). Emails from the Professional Society for Pharmacists (PSA) were read for training-related information and guidelines, and emails from indemnity insurance, wholesalers, and pharmacy banner/staff emails were also mentioned. In addition, pharmacists received information from flyers, fax, websites, social media, podcasts, service providers, pharmaceutical representatives, and word of mouth. Social media was used professionally by six of the eight participants, with Facebook being most popular, followed by Twitter, LinkedIn, and Instagram. Podcasts were listened to for professional information by three attendees.
Pharmacists identified four behaviours as being roadblocks to the implementation of THN: stocking naloxone, initiating conversations with patients, educating patients, and signing up for the Commonwealth pilot. Identifying patients, dispensing naloxone, providing educational materials, patient follow-up, and educating other staff were not prioritised by the participants, although knowing where to go for educational materials was flagged as important.
Obtaining naloxone stock has been an issue and is crucial for the THN provision to become routine (15). The participants felt that the topic was sensitive and expressed a need for training on initiating conversations and appropriate language to not accuse patients. They liked the idea of calling THN a “first aid measure” as it would “make life a lot easier to start conversations.” Using the term “side effect” was also perceived as easier and more acceptable than “overdose.” Similarly, educating patients was raised as a barrier due to lack of knowledge. There was a desire for a cheat sheet or flyer targeting consumers for pharmacists to give out, or a poster in the pharmacy to normalise talking about naloxone. Signing up for the pilot was considered a major issue, due to a lack of awareness of the programme.
During the design-thinking workshop, the participants were able to think beyond the scope of the initial problem statement. Themes from generated ideas were related to stock, patient groups, patient education/awareness, pharmacist education, messaging/language, and system changes. The generated ideas are presented in Table 4.
Three ideas were taken forward for the second round of ideation and prototyping. Idea #1 considered including naloxone as part of Medication Review consultations. This provides additional time and reimbursement for having the conversation about naloxone every 12 months. Idea #2 was to normalise the conversation by attaching naloxone to the opioid medication packaging. Concepts within this idea ranged from Velcro-sticking the two items together, to a message inside the box to be taken to the pharmacist to receive naloxone, or a sticker to be placed on the prescriptions of the doctors to encourage collaboration (co-prescribing). Idea #3 was the provision of free stock to pharmacies or include free stock in first aid kits and providing free “first aid kits” for patients who live with pain (medication and naloxone in a bag).
The participants highlighted the key messages. Firstly, “naloxone is now available for free and pharmacists are remunerated for supply with a dispensing fee. Only takes five simple steps,” as they thought there was a general lack of awareness of the Commonwealth pilot and the process for supplying naloxone. Second, “all patients on S8 opioids for longer than two weeks are at risk,” corresponding to poor knowledge around relevant populations. Third, “provision of naloxone is simple, language is an addressable barrier,” together with “pharmacist have a key public health and harm reduction role” were raised due to the need to normalise naloxone for people taking opioids to relieve pain, and finally, the myth busters to normalise naloxone and reduce stigma “naloxone is part of first aid courses, kits and 000 protocols. It's a life-saving medication like glucagon and Epipens®” and “Naloxone does not increase drug use or risk-taking behaviour but saves lives.”
This project was built on the work of Nielsen and Olsen (15) to develop a theoretically informed, participatory designed, single-session implementation strategy that aimed to increase the implementation of THN by community pharmacists.
The implementation strategy consisted of a video that includes the intervention functions of education, modelling, persuasion, and promoting available incentivisation and linked BCTs. The video addressed known barriers, provided education for pharmacists on opioid-related overdose, naloxone, identifying at-risk patients, delivering advice, stigma and discrimination, and included content delivered by champions and role models from the pharmacy and the affected community (individuals who use opioids, peers, and those likely to witness an overdose). Some intervention functions and techniques were not appropriate or feasible due to the format of the implementation strategy being a communication campaign. These intervention functions included environmental restructuring, training, and enablement and BCTs such as clinical prompts, as well as those associated with the system level barrier of stock availability. This is consistent with the proposition that single-session implementation strategies may address multiple implementation barriers in a scalable and efficient manner (21); however, additional multilevel strategies are likely to be also required to target all determinants of change across all levels.
The design-thinking process resulted in creative and valuable ideas, but was uncomfortable for some pharmacists. These pharmacists spoke directly with researchers and were noted in the field notes about seeing the activities as futile and not initially seeing the merit in their “crazy” ideas. However, the idea from the activity of “expanding their idea” (using the Merlin method) led one group suggesting for naloxone to be provided for free in all first aid kits. With a little tweaking, this became a key message. As many healthcare professionals are not accustomed to open-ended creative inquiry, we suggest that additional time be provided to acknowledge and normalise all reactions to the process up-front, allowing these to be noted before moving on, in addition to providing examples of the potential impact of such processes (36). We also encourage researchers to engage in these methods to extract ideas that may not come from a simple or prescribed/pre-determined line of questioning: the reasoning logic of design-led approaches is largely abductive (37), focussing on the generative possibilities of “what if?” (36).
The participatory nature of the workshop also allowed the participants to share some general ideas and demographic information including background on naloxone supply. For example, the participants shared that an educational flyer is provided for “Fit-packs” (needle and syringe packs in hard disposal containers sold in pharmacies for people who inject drugs), but not for other opioids, whilst others raised their concerns about doctors not engaging in the space and prescribing naloxone. Furthermore, supply issues were raised along with suggestions to increase Health Department-issued communication to increase awareness, targeting owners and employee pharmacists, and discuss naloxone with all patients who use opioids, including prescribed and elicit forms. These ideas have the potential to be included in subsequent implementation strategies.
This study was conducted at the onset of the COVID-19 pandemic and a feasible, acceptable, and appropriate mode of delivery for an implementation strategy was required given this context and the additional pressures and workload being placed on community pharmacists. As a result, the researchers and expert advisory group pre-determined, prior to the participatory workshops and placed as a boundary on the intervention, to develop a single-session implementation strategy through a video format. In addition, being a single-session implementation strategy, it was decided that the intervention was to target pharmacist and pharmacy level barriers, as these contained the most barriers in the literature, rather than be a complex multilevel implementation strategy. These boundaries placed a limitation on addressing all barriers identified in the preceding work, in particular those at a system level (e.g., stock availability) as well as consumer/end-user level influences. Another limitation of this study was the lack of involvement of consumers/end-users in the development workshop. This was due to a difficulty in recruiting end-users but was mitigated to some degree in production by the final messages being real responses from an affected end-user.
Finally, a second workshop was planned for pharmacists, but with the onset of the COVID-19 pandemic and the workload increase for pharmacists, it was not feasible to conduct this workshop. Whilst the first workshop (as described in this paper) ideated broadly about the strategies to address naloxone not being provided (regardless of the mode of delivery), the second workshop was to focus the activities on the messages that may address the problem in a video intervention. The implication of this was that the research team needed to determine the ideas that were reasonable to be delivered in the intervention.
As of 1 July 2022, due to the success of the pilot in three Australian States, the Australian Government announced that $19.6 million would be invested over the subsequent 4 years to implement free take-home naloxone in the country (38). This produces both an opportunity and challenge. Whilst the single-session nature of the intervention video is feasible for a national scale-up, there is a need for future studies to evaluate its implementation and impact.
Implementation science, behavioural change theory, and participatory design methods are a complementary combination to develop implementation strategies. Together, they can address theoretically and empirically derived implementation barriers and create unique ideas that are unlikely to have been generated using more traditional consultative approaches. Furthermore, it appears that multiple implementation barriers can be addressed in a single-session implementation strategy.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Curtin University Human Research Ethics Committee (Reference number HRE2019-0816). The patients/participants provided their written informed consent to participate in this study.
JM: conceptualization, funding acquisition, data curation, methodology, investigation, and writing—original draft. PE: data curation, methodology, and writing—reviewing and editing. LS: methodology and writing—reviewing and editing. HU: data curation, methodology, and writing—reviewing and editing. SN: supervision and writing—reviewing and editing. SL: supervision and writing—reviewing and editing. All authors contributed to the article and approved the submitted version.
The work by JM was supported by the Medical Research Future Fund (Grant number 1168155).
We would like to acknowledge the work of Grace Oh, Judi Stone, and Christianne White in the advisory group, and Juliette Dujardin and Kammi Rapsey for directing and producing the video.
The author JM declared that she was an editorial board member of Frontiers at the time of submission. This had no impact on the peer review process and the final decision.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2023.1227360/full#supplementary-material
AJP, Australian Journal of Pharmacy; BCTs, behaviour change techniques; BCW, behaviour change wheel; COM-B, capability, opportunity, motivation—behaviour; MATOD, medication-assisted treatment for opioid dependence; THN, take-home naloxone; PSA, Pharmaceutical Society of Australia.
1. Australian Institute of Health Welfare. Opioid harm in Australia and comparisons between Australia and Canada. Canberra: Australian Institute of Health and Welfare (2019).
2. Roxburgh A, Hall WD, Dobbins T, Gisev N, Burns L, Pearson S, et al. Trends in heroin and pharmaceutical opioid overdose deaths in Australia. Drug Alcohol Depend. (2017) 179:291–8. doi: 10.1016/j.drugalcdep.2017.07.018
3. Chrzanowska A, Man N, Sutherland R, Degenhardt L, Peacock A. Trends in overdose and other drug-induced deaths in Australia, 1997–2020. Sydney: National Drug & Alcohol Research Centre (2022).
4. Miller NM, Waterhouse-Bradley B, Campbell C, Shorter GW. How do naloxone-based interventions work to reduce overdose deaths: a realist review. Harm Reduct J. (2022) 19(1):18. doi: 10.1186/s12954-022-00599-4
5. World Health Organization. Community management of opioid overdose. Geneva: World Health Organization (2014).
6. Fomiatti R, Farrugia A, Fraser S, Dwyer R, Neale J, Strang J. Addiction stigma and the production of impediments to take-home naloxone uptake. Health. (2022) 26(2):139–61. doi: 10.1177/1363459320925863
7. Moustaqim-Barrette A, Dhillon D, Ng J, Sundvick K, Ali F, Elton-Marshall T, et al. Take-home naloxone programs for suspected opioid overdose in community settings: a scoping umbrella review. BMC Public Health. (2021) 21(1):597. doi: 10.1186/s12889-021-10497-2
8. Tse WC, Sanfilippo P, Lam T, Dietze P, Nielsen S. Community pharmacy naloxone supply, before and after rescheduling as an over-the-counter drug: sales and prescriptions data, 2014–2018. Med J Aust. (2020) 212(7):314–20. doi: 10.5694/mja2.50524
9. Thakur T, Frey M, Chewning B. Pharmacist roles, training, and perceived barriers in naloxone dispensing: a systematic review. J Am Pharm Assoc (2003). (2020) 60(1):178–94. doi: 10.1016/j.japh.2019.06.016
10. Nielsen S, Menon N, Larney S, Farrell M, Degenhardt L. Community pharmacist knowledge, attitudes and confidence regarding naloxone for overdose reversal. Addiction. (2016) 111(12):2177–86. doi: 10.1111/add.13517
11. Evoy KE, Groff L, Hill LG, Godinez W, Gandhi R, Reveles KR. Impact of student pharmacist-led naloxone academic detailing at community pharmacies in Texas. J Am Pharm Assoc (2003). (2020) 60(1):81–6. doi: 10.1016/j.japh.2019.09.007
12. Cid A, Daskalakis G, Grindrod K, Beazely MA. What is known about community pharmacy-based take-home naloxone programs and program interventions? A scoping review. Pharmacy. (2021) 9(1):30. doi: 10.3390/pharmacy9010030
13. Muzyk A, Smothers ZPW, Collins K, MacEachern M, Wu LT. Pharmacists’ attitudes toward dispensing naloxone and medications for opioid use disorder: a scoping review of the literature. Subst Abus. (2019) 40(4):476–83. doi: 10.1080/08897077.2019.1616349
14. Carpenter DM, Dhamanaskar AK, Gallegos KL, Shepherd G, Mosley SL, Roberts CA. Factors associated with how often community pharmacists offer and dispense naloxone. Res Soc Adm Pharm. (2019) 15(12):1415–8. doi: 10.1016/j.sapharm.2018.07.008
15. Nielsen S, Olsen A. Using the behaviour change wheel to understand and address barriers to pharmacy naloxone supply in Australia. Int J Drug Policy. (2021) 90:103061. doi: 10.1016/j.drugpo.2020.103061
16. Rawal S, Osae SP, Cobran EK, Albert A, Young HN. Pharmacists’ naloxone services beyond community pharmacy settings: a systematic review. Res Social Adm Pharm. (2023) 19(2):243–65. doi: 10.1016/j.sapharm.2022.09.002
17. Lai Joyce Chun K, Olsen A, Taing MW, Clavarino A, Hollingworth S, Dwyer R, et al. How prepared are pharmacists to provide over-the-counter naloxone? The role of previous education and new training opportunities. Res Social Adm Pharm. (2019) 15(8):1014–20. doi: 10.1016/j.sapharm.2019.03.003
18. Lenton S, Dietze P, Jauncey M. Perspective: Australia reschedules naloxone for overdose. Med J Aust. (2016) 4(7):146–7. doi: 10.5694/mja15.01181
19. Salom CL, Maravilla JC, Thomas N, Juckel J, Daly C, Peacock A, et al. Evaluation of the pharmaceutical benefits scheme subsidised take home naloxone pilot-final report. Brisbane: Institute for Social Science Research, The University of Queensland Australia (2022).
20. Michie S, Atkins L, West R. The behaviour change wheel. A guide to designing interventions. London: Silverback Publishing (2014). p. 1003–10.
21. Schleider JL, Beidas RS. Harnessing the single-session intervention approach to promote scalable implementation of evidence-based practices in healthcare. Front Health Serv. (2022) 2:997406. doi: 10.3389/frhs.2022.997406
22. Schleider JL, Dobias ML, Sung JY, Mullarkey MC. Future directions in single-session youth mental health interventions. J Clin Child Adolesc Psychol. (2020) 49(2):264–78. doi: 10.1080/15374416.2019.1683852
23. Kueh C, Durrant G, Peng F, Ely P, Bionat JF. Transforming complexity: A human-centred design approach to engage young people in the Philippines with dialogues about HIV service delivery. In: Pfannstiel MA, editor. Human-centered service design for healthcare transformation: development, innovation and change. Cham: Springer (2023). p. 243–64. doi: 10.1007/978-3-031-20168-4_14
24. Kueh C, Peng F, Ely P, Durrant G. A speculation for the future of service design in healthcare: looking through the lens of a speculative service design framework. In: Pfannstiel MA, Brehmer N, Rasche C, editors. Service design practices for healthcare innovation. Cham: Springer (2022). p. 115–31. doi: 10.1007/978-3-030-87273-1_6
25. Chen E, Neta G, Roberts MC. Complementary approaches to problem solving in healthcare and public health: implementation science and human-centered design. Transl Behav Med. (2020) 11(5):1115–21. doi: 10.1093/tbm/ibaa079
26. Agogino AM, Beckman SL, Castaños C, Kramer J, Roschuni C, Maria Y, editors. Design practitioners' perspectives on methods for ideation and prototyping. . Paper presented at the Mudd Design Workshop IX, Claremont, CA, Claremont: Mudd Design Workshop (2015).
30. Ely P. Conclusion-beyond normal design thinking: reflections on the evolution of a paradigm and ideas for the new incommensurable. Research handbook on design thinking. Cheltenham: Edward Elgar Publishing (2023). p. 294–314.
31. Roschuni C, Kramer J, Zhang Q, Zakskorn L, Agogino A. Design talking: an ontology of design methods to support a common language of design. In: Proceedings of the 20th International Conference on Engineering Design (ICED15), Milan, Italy. (2015).
32. van der Westhuizen D, Conrad N, Douglas TS, Mutsvangwa T. Engaging communities on health innovation: experiences in implementing design thinking. Int Q Community Health Educ. (2020) 41(1):101–14. doi: 10.1177/0272684X19900880
33. Sanders EBN, Stappers PJ. Co-creation and the new landscapes of design. CoDesign. (2008) 4(1):5–18. doi: 10.1080/15710880701875068
34. Beidas RS, Dorsey S, Lewis CC, Lyon AR, Powell BJ, Purtle J, et al. Promises and pitfalls in implementation science from the perspective of US-based researchers: learning from a pre-mortem. Implement Sci. (2022) 17(1):55. doi: 10.1186/s13012-022-01226-3
35. 18F. Build a greater understanding of your problem and the people it impacts. Available at: https://methods.18f.gov/discover/dot-voting/. (Accessed July 6, 2023).
36. Liedtka J. Innovative ways companies are using design thinking. Strategy Leadersh. (2014) 42(2):40–5. doi: 10.1108/SL-01-2014-0004
37. Dorst K. The core of ‘design thinking’ and its application. Des Stud. (2011) 32(6):521–32. doi: 10.1016/j.destud.2011.07.006
38. Take home naloxone program. Australian Government, Department of Health and Aged Care (2023). Available at: https://www.health.gov.au/our-work/take-home-naloxone-program. (Accessed July 6, 2023).
Keywords: opioid overdose, naloxone, pharmacy, implementation science, theoretical models, COM-B, design-thinking
Citation: Moullin JC, Ely P, Uren H, Staniland L, Nielsen S and Lenton S (2023) Developing a single-session strategy for the implementation of take-home naloxone by community pharmacists using COM-B and design-thinking. Front. Health Serv. 3:1227360. doi: 10.3389/frhs.2023.1227360
Received: 23 May 2023; Accepted: 14 July 2023;
Published: 1 August 2023.
Edited by:
Ann Catrine Eldh, Linköping University, SwedenReviewed by:
Meagen Rosenthal, University of Mississippi, United States© 2023 Moullin, Ely, Uren, Staniland, Nielsen and Lenton. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joanna C. Moullin SmNtb3VsbGluQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.