- 1University of Rochester, Rochester, NY, United States
- 2Brown University School of Public Health, Providence, RI, United States
- 3The Fenway Institute, Boston, MA, United States
Background: Multiple national organizations recommend that cancer care providers and oncology practices be responsive to the needs of sexual and gender minority (SGM) patients. Oncology practices have attempted to incorporate this recommendation through SGM-focused cultural humility training interventions. It is unclear how best to adapt and implement such training across practices. This manuscript outlines one process for adapting a widely-used SGM training from The Fenway Institute to the context of oncology settings using the Framework for Reporting Adaptations and Modifications-Enhanced (FRAME) model.
Methods: We conducted training sessions in two oncology care settings: a breast oncology center and a radiation oncology department. Subsequently, we conducted in-depth interviews with the three trainers involved in adapting The Fenway Institute's training to these two practices. Two independent investigators coded the interviews using components of the FRAME model as an analytic guide.
Results: Training team members described the mechanisms by which FRAME adaption occurred both proactively and reactively; the importance of involving SGM-identified trainers of diverse backgrounds as well as champions from within oncology practices in which trainings were conducted; the importance of adapting both the context and content of training to be relevant to oncology audiences; and the ways in which fidelity to the core principles of improving health care for SGM patients was maintained throughout the process.
Discussion: SGM cultural humility training for oncology providers and staff must undergo iterative adaptation to address the political and social context of specific practice environments and advocate for broader institutional culture change to achieve responsiveness to SGM health needs.
Introduction
Sexual and gender minority individuals (SGM; e.g., lesbian, gay, bisexual, transgender, queer; LGBTQ+) experience high rates of psychological distress, low rates of insurance coverage, and difficulty accessing culturally competent and culturally humble healthcare services (1–6). These same disparities affect SGM people with cancer, reducing access to oncology care, quality of life following cancer care, and, potentially, rates of survival from cancer (7–9). Some studies have found that SGM cancer patients report higher psychological distress, depression, and anxiety than heterosexual and cisgender patients (i.e., those who are primarily attracted to people of genders different from their own and whose gender identities match societal expectations based on their sex assigned at birth; H/C) (10, 11). This is a major concern given the link between higher psychological distress and increased risk of mortality from cancer (12–14). These studies also highlight unique factors that affect distress for SGM cancer patients (15–17). One unique factor is minority stress, or chronic stress arising from experiences of prejudice and discrimination based on sexual orientation or gender identity (2, 5). Pre-existing disparities in distress, caused by minority stress, may be exacerbated by stigma and discrimination experienced during cancer diagnosis and treatment (e.g., discrimination from cancer care providers based on sexual orientation and/or gender identity) (18–21). In the face of minority stress, SGM cancer patients have asked for providers to “treat us with dignity” (22).
Given this request, interventions to improve SGM cultural competency and humility of oncology personnel as they treat SGM patients are urgently needed. Throughout this manuscript we will refer to “cultural humility” as the preferred approach to training interventions. Cultural humility training emphasizes awareness of trainees' personal biases, patient-centeredness, and openness to lifelong learning (23). The literature on racial/ethnic minority cultural humility training interventions highlights that such interventions are effective in improving provider knowledge and skills (24, 25) as well as patient satisfaction with care (26, 27). Importantly, satisfaction with care is a fundamental component of high-quality care, underscoring the importance of promoting cultural humility training (28, 29). While the literature on SGM humility training is still in its infancy (24, 30), based on limited evidence, SGM humility training has been shown to be effective in improving clinicians' knowledge and attitudes regarding SGM patients (31–35). Such training must also acknowledge that SGM identities also cut across all populations and that SGM people with multiple marginalized identities experience multiplicative marginalization and barriers to care (36). Examples of populations with intersecting marginalized identities include SGM people of color (37), SGM people who are economically disadvantaged (38, 39), or SGM people with disabilities (40). To date, no studies have tailored intersectional SGM cultural humility training specifically to the context of oncology (41).
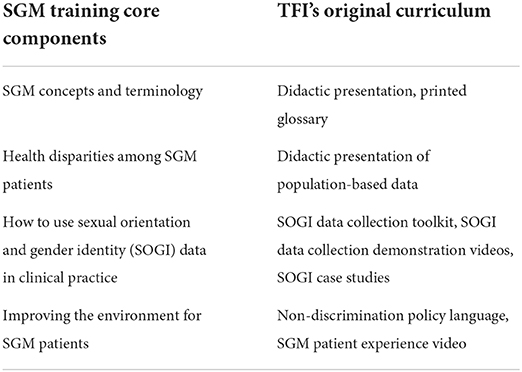
Despite limited data on the efficacy of training, cancer care facilities have begun to mandate SGM cultural humility training in response to the requests of patients and clinicians (42). The Fenway Institute's (TFI) National LGBTQIA+ Health Education Center has been at the forefront of delivering SGM-relevant training to healthcare facilities nationwide (43–45). Their SGM humility training intervention is based on a decade of program evaluation in non-cancer healthcare settings and was developed with a diverse community advisory board, based on survey data, chart review, and literature reviews (44, 46, 47). TFI's intervention focuses on four components, which are presented in Table 1. The TFI intervention has not included oncology-specific examples and has not been evaluated in the context of oncology.
To address this gap, we adapted TFI modules to address specific issues confronted by diverse SGM patients in oncology settings. In this article, we report on the process of iterative adaptation and implementation of TFI's SGM cultural humility training modules in two different oncology contexts: a breast oncology center and a radiation oncology department. We use the Framework for Reporting Adaptations and Modifications-Enhanced (FRAME) as a foundation for documenting and reporting our adaptation efforts (48). We present the results of our adaptation in order to establish a roadmap that other groups can follow when adapting TFI or other cultural humility training interventions to their specific healthcare contexts.
Methods
Initial adaptation of intervention
A team of four clinicians and scientists (AA, a Non-Hispanic White, queer, non-binary person who is a medical oncologist; CD, a Non-Hispanic White, gay cisgender man who is a radiation oncologist; CK, a Non-Hispanic White, gay cisgender man who is a clinical psychologist; and PV, a Non-Hispanic Black, gay cisgender man who was a public health graduate student) came together to implement a series of SGM-focused cultural humility trainings for oncology practices in the Wilmot Cancer Institute care network. The core training materials had been developed by TFI as described above. Oncology-specific content included in the training was based on feedback from a mixed-methods study conducted by the National LGBT Cancer Network (22, 49), findings from qualitative interviews with SGM cancer patients, their caregivers, and their providers (50), a focus group of transgender and gender diverse individuals affected by cancer (51), and the clinical experiences of the team members. The team also discussed pragmatic aspects of adaptation to address the needs of different oncology clinics. The training was implemented at two regional care locations in the Wilmot Cancer Institute (Wilmot) network in upstate New York.
Ethical review
These trainings and subsequent data collection were approved by the Institutional Review Board of the University of Rochester.
First training
Three training team members (CD, CK, PV) delivered a 1-h training session to breast oncology clinicians and staff. Sixteen personnel attended, including six nurses, four social workers, four administrative staff, and two medical oncologists. The delivery and presentation of training materials took place in a conference-style room with a single large table for attendees and trainers, as well as a wall-mounted screen for the slide presentation.
Second adaptation
Four training team members (AA, CD, CK, PV) reviewed the findings from the first training. Based on personal reflections of the trainers and comments from attendees, the training materials were further adapted before the second training session.
Second training
Two training team members (CD, CK), delivered a 1-h training session to a radiation oncology department. Forty-one personnel attended, including 14 nurses, 12 radiation oncologists, eight administrative staff, four administrators, and three dosimetrists. The delivery and presentation of training materials took place in a lecture-style classroom with tables for attendee seating, a projection screen, and a podium for the trainer(s) speaking.
Follow-up interviews
After the second training, two authors (MR, PD) conducted in-depth semi-structured interviews with three training team members (CD, CK, PV), all of whom are also authors on this paper. The interview guide was based on the FRAME model for adapting interventions and the purpose of the interviews was to capture the team's reflections on the adaptation process. Interviews were audio-recorded using Zoom and transcribed using otter.ai software, along with coder review. We analyzed transcripts in Dedoose, a qualitative data analysis program, using the components of FRAME as an explicit guide for analysis (48, 52). Two coders (MR, PD) independently reviewed the three interviews using Dedoose to extract quotes that exemplified the different components of the FRAME model. The coders discussed and refined these quotes collaboratively to create a preliminary codebook consisting of 36 codes, which both coders consistently applied to the 3 interviews. Two auditors (CK, RYN) reviewed the data to assess whether codes aligned with the quotes from interviewees; based on this feedback, final codes were aligned with the components of the FRAME model, and a table was generated based on the modular structure of the FRAME-Implementation Strategies tool (FRAME-IS) (53). The data presented here include the final set of FRAME components, relevant codes, and illustrative quotes, which have been minimally edited for readability.
Results
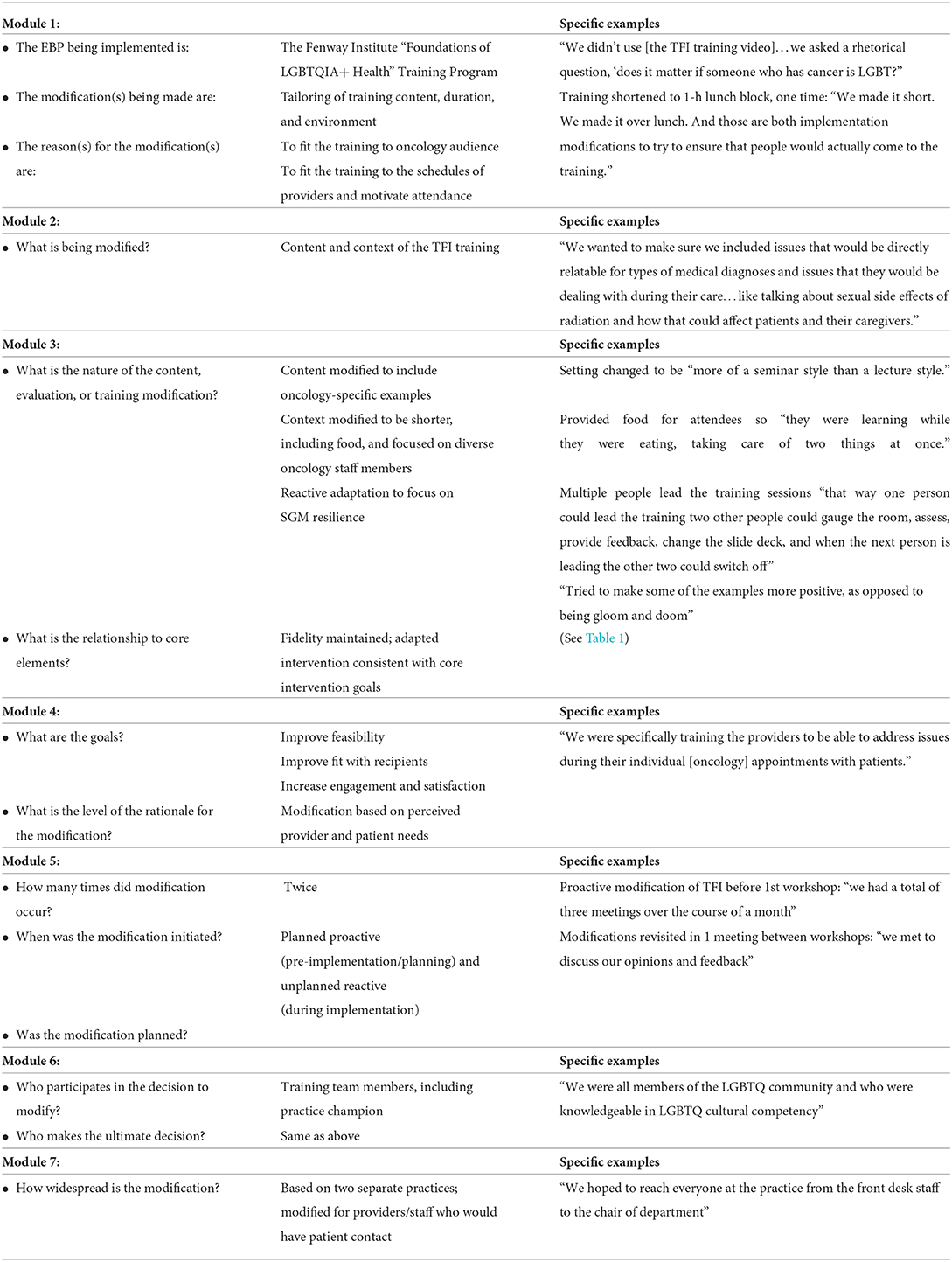
We structure the results based on the domains of the FRAME model and tabulate the results based on FRAME-IS modules. The table is comprised of 7 different modules used to document modifications to implementation strategies: a brief description of the EBP, implementation strategy, modification, and the reason for modification (Module 1); what is modified (Module 2); the nature of modification and the relationship between modifications and core-implementation strategies (Module 3); the goals and rationale for modification (Module 4) when the modification occurred, and whether it was planned (Module 5); who participated in the decision to modify (Module 6); and how widespread the modification is (Module 7). We present the modules in Table 2 using the order outlined in the original FRAME-IS manuscript, but for readability, we present the results below in the order in which topics were discussed by the interviewees. Interviewees offered further insights that were not captured by the existing FRAME model; these comments are presented as a separate section in the text and FRAME-IS table.
When did adaptation occur?
Team members stated that adaptation of TFI's SGM cultural humility training occurred both proactively and reactively. To proactively adapt the training, the team met in person at the beginning of 2020 for a total of 3 meetings over the course of a month. The modifications focused primarily on program materials, which were adapted before their implementation to make their content relevant to oncology clinicians and staff. Visuals such as pictures and cartoons from the TFI materials were adapted to include cancer patients and caregivers of diverse racial and ethnic backgrounds in order to highlight intersectionality and make SGM people of color visible. Following the first training, several reactive modifications were made in response to feedback from the training team and attendees at the first training.
Who was involved in adaptation?
The team adapting the training was composed of faculty members and one graduate student from the University of Rochester Medical Center. As described above, all were members of SGM communities. Their training backgrounds included medical oncology, radiation oncology, clinical psychology, and public health. One member of the team (CK) was “the primary person leading the changes in the modifications. He had previously done similar training across the country in [LGBTQ+] cultural competency and wanted to tailor the program to the staff that we would be training…at the University of Rochester Medical Center” (CD). However, the team viewed the experience of adaptation as “pretty collaborative,” because “we were all intended to participate in providing the training,” and “having multiple people thinking about the tailoring ended up making it much stronger” (PV). Team members described the ways their diverse disciplinary viewpoints, alongside their shared lived experience as SGM people, informed their adaptation of the training: “All four of us were very knowledgeable in the area of LGBT cultural humility, and all four of us are also members of the LGBTQ community, so we knew what things we would want to see in a training as both healthcare providers and members of the community” (PV). In preparing for the second training, a team member (CD), who was a resident in the Department of Radiation Oncology, took a lead role in suggesting new examples relevant to radiation therapy, “bringing a focus on actual provider interest in behavior–like what does an oncologist need to know about sexual side effects for LGBT people after radiation” (CK). Team members reflected that including a champion from within the clinic being trained enhanced the success of this second training: “I just have a very supportive department but I'm also engaged with them…I'm telling people, and then it was really just like, word of mouth” (CD).
What was adapted and what was the nature of the adaptation?
Both the format and the content of the training were adapted to work within oncology settings. In terms of format, the team distilled the 2-h TFI training into a 1-h session. This decision was based on feedback collected before the training from staff and providers at the clinics that they needed the training to be shorter: “People were like, ‘We [staff and providers] cannot take a ton of time away from the clinic, please do it in a short burst, over lunch. We can make that work with the clinic schedule”' (CK). The training team also provided food to participants, an aspect added to encourage the attendance of providers and staff with very busy schedules: “We [the training team] offer Panera sandwiches, so I think that galvanized some people to come who wouldn't have come otherwise” (CK).
In terms of content, the training team iteratively adapted training materials (e.g., PowerPoint slides, handouts) to include content specific to the needs of different oncology audiences. After the first training at the breast oncology center, the training team mutually felt that the examples they had been using were too “negative” and “gloomy.” Therefore, the trainers decided to change the SGM-specific cancer examples to highlight resilience among SGM patients: “We need to revise the content enough so that it … doesn't frighten people away from thinking about [gender and sexuality] issues” (PV). Before the second training, they also changed the content to be specific to radiation oncology. As the participants at this second training were radiation oncologists, dosimetrists, staff, nurses, and a department leader, the trainers added content about the sexual side effects of radiation and ways in which these side effects could uniquely impact SGM patients and their caregivers.
What were the reasons for the adaptation?
Trainers explained that the primary reason behind the modifications of the TFI model was to increase applicability for the audience: “The Director of Education at Fenway…and I had a long conversation about how Fenway does their training. And he himself said, ‘You know, really these trainings are most effective when they are adapted to the specific healthcare audience where you're trying to deliver them”' (CK). Other reasons for adapting the training included improving feasibility (e.g., length of training), improving perceived applicability to recipients (e.g., oncology examples), addressing sociocultural differences between practices (e.g., all cisgender women at the breast oncology center training), and acknowledging the diversity of SGM cancer patients' experiences, with attention paid to intersectionality. In order to highlight the diversity of patient experiences, the training selected examples derived from interviews with actual SGM cancer patients (50): “We really tried to make it relevant to the trainees that you should care about your LGBTQ patients because look at these things that can happen when you don't, including some obvious discrimination that had occurred” (CD).
How was intervention fidelity ensured?
The core components of the TFI training program (Table 1) were maintained for this training. In both the original and our adapted version of the training, content addressed SGM terminology, SGM cancer disparities, sexual orientation and gender identity (SOGI) data collection, and institutional non-discrimination policies on the basis of SOGI. Data from the trainings were shared back with leaders at TFI to confirm fidelity with their approach: “He [the TFI Director of Education] had not up to that point done any modification to be oncology specific… it became pretty clear that should be done and we thought, ‘who better to do it than our modification team?”' (CK).
What were the results of the adaptation?
The training team felt that the adaptation increased participant engagement and improved knowledge gain. Team members reported receiving “verbal feedback” that attendees were “really appreciative of the information that we provided,” that they “actually seemed to gain some confidence in the knowledge portion,” and “they felt much more comfortable with being able to better serve the LGBTQ patient population” (CD). Pre- and post-training surveys (not published) showed significantly higher scores of trainee knowledge and self-efficacy, and reported satisfaction was high (average satisfaction score of 95% out of 100%).
Reflections on the next iteration
In addition to describing various aspects of the adaptation, interviewees also commented on other ways they would like to augment the training in future. Interestingly, many of these suggestions are directed at improving uptake and implementation, which are not explicitly addressed by FRAME. All three interviewees suggested follow-up training to reinforce skills, saying for example: “In the future, we can make the training more of a series…in the sense that we do one training on one day and then schedule a follow up [training] maybe two months later, or three months later” (PV). Trainers believed these future trainings could be more specific in scope than the initial training, e.g., could focus only on sexual orientation and gender identity data collection or on SGM relationships. They also suggested “doing more…small group… activities” rather than relying primarily on didactic lectures (CK). Interviewees also commented on the need for better training evaluation processes to inform future adaptations: “One thing that we could do…in the future is to have the…posttest as soon as possible [after the training], possibly on REDCap or some other electronic platform” (PV). Finally, interviewees commented that the early inclusion of champions from each practice receiving the intervention would assist with increasing buy-in from administrators and staff and could improve attendance. Additionally, this would increase the applicability of the trainings.
“One of the things that was so successful with the radiation oncology training was having [CD], a fellow in Radiation Oncology, be one of the trainers and promote the training within his facility. …From an implementation perspective, having buy-in from someone inside, preferably somebody with…clout or leadership, makes a huge difference. And, I'd like to think about capitalizing on that, and going up a level to the leadership of the clinic and having the champion connect me to that leader, so that we can, ideally, get the training to be made, if not mandatory, at least strongly encouraged for everybody to attend” (CK).
Discussion
In this manuscript, we describe an iterative process of adapting and implementing a SGM humility training in two different oncology settings. Our hope is to provide a roadmap that other trainers and implementation scientists can follow when adapting such training programs for their own settings. We used the FRAME model to structure interviews with team members involved in adaptation and implementation, as well as to organize qualitative findings. Commentary from the training team also expanded beyond the FRAME model to cover the importance of iterative adaptation, reflection, and future directions.
As healthcare systems expand regionally, incorporating multiple practices across a large geographic area, efforts to implement interventions may need to account for iterative adaptation on a practice-by-practice basis. Emerging models like FRAME help organize and document the process of such iterative adaptations. Process models also facilitate communication about and generalization of adaptation to other contexts. Given the different contexts of these practices, models like FRAME should be re-applied and the trainings revised to incorporate new lessons learned after each implementation. This is particularly true for interventions addressing diversity, equity, and inclusion, which may need to consider practices' different geographical, political, and social factors. For example, in the current study, we adapted our SGM humility intervention first for a multidisciplinary breast oncology practice, including attendees from the fields of nursing, social work, and oncology, with many cisgender women on staff serving primarily cisgender women; discussing issues like breast cancer in transgender men was relevant here. Second, we adapted for a radiation oncology practice, including radiation techs and front desk staff, with a large proportion of cisgender men on staff serving a more diverse patient base; talking about a range of sexual side effects of treatment was relevant here.
In this exercise, we found it difficult to separate adaptation and implementation, given the dynamic relationships between these processes. Reflecting on the use of FRAME as a qualitative analysis tool, we believe that this conceptual model could be enhanced by incorporating longitudinality and integrating adaptation with implementation. For example, as an intervention is implemented, it should be evaluated for potential adaptation to other care contexts. Future efforts to adapt and implement cultural humility training, specifically, should attend to the interplay between adaptation (e.g., accounting for the practice-level political and social factors mentioned earlier) and implementation (e.g., reach, effectiveness/outcomes).
One important goal for adapting the TFI SGM cultural humility training program for oncology settings was to maximize and facilitate implementation. Interviewees identified several factors that would aid in the implementation of future SGM oncology training programs for clinicians and staff, and these were incorporated into adaptation. For example, providing evaluation results in the form of post-training feedback to participants, as well as engaging department leaders and internal champions, are well-recognized implementation strategies that were suggested as adaptation activities (54). In our adaptation, including an internal champion from one practice allowed the training team to adapt the content of the intervention further to the needs of the practice, facilitating uptake and adoption as measured by verbal feedback about the relevance of the material. This point further highlights the interconnectedness of adaptation and implementation. Both are critical, intertwined, and mutually reinforcing.
Limitations
The present manuscript presents one example of this adaptation and implementation process. Results are based upon interviews with three team members who conducted two training sessions within a single regional cancer network. Interviews do not allow for collection of observational data and we did not assess the impact of trainings on trainees' behavior. Thus, the lessons learned from the adaptation and implementation of these training sessions may vary in their relevance to other cancer care settings. Finally, the end goal of cultural humility training is to improve patients' experiences with care, and so future research should incorporate the perspectives of patients about their relationship with trained, culturally humble providers.
Conclusion
The current study provides a real-world example of the adaptation and implementation of an SGM cultural humility training intervention in oncology. Adaptation of this sort of intervention is affected by issues such as the political climate of practices, biases of attendees, and the ongoing societal stigma that surrounds the assessment of sexual orientation and gender identity. Our adaptation methodologies balanced the needs of a cancer care audience with the goal of remaining faithful to the widely-used TFI cultural humility training intervention's core principles. Such training interventions, however, are only one aspect of the systemic and structural reform needed to ameliorate cancer-related disparities affecting SGM populations. These training interventions must coincide with culture change in cancer care practices for all members of the oncology team, including practice leadership, clinicians, front-line staff, and support staff. Practices must create an environment that not only accepts diversity based on sexual orientation and gender identity, but celebrates it. Cultural humility training programs must look beyond practice-level change to ascertain the impact of training on SGM patients' cancer outcomes. Future adaptations of SGM cultural humility training interventions for oncology must aim to incorporate these endpoints if we hope to achieve true health equity for SGM cancer patients.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by University of Rochester Research Subjects Review Board. The participants provided their written informed consent to participate in this study.
Author contributions
Data collection and analysis were performed by MR and PD, with supervision by RY-N. The first draft of the manuscript was written by CK. All authors contributed to the study conception and design, commented on previous versions of the manuscript, and read and approved the final manuscript.
Funding
This research was supported by National Cancer Institute grants K07 CA190529, UG1 CA189961, and UG3 CA262602.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Meyer IH. Minority stress and mental health in gay men. J Health Soc Behav. (1995) 36:38–56. doi: 10.2307/2137286
2. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. (2003) 129:674–97. doi: 10.1037/0033-2909.129.5.674
3. Kertzner RM, Meyer IH, Frost DM, Stirratt MJ. Social and psychological well-being in lesbians, gay men, and bisexuals: the effects of race, gender, age, and sexual identity. Am J Orthopsychiatry. (2009) 79:500–10. doi: 10.1037/a0016848
4. Meyer IH, Dietrich J, Schwartz S. Lifetime prevalence of mental disorders and suicide attempts in diverse lesbian, gay, and bisexual populations. Am J Public Health. (2008) 98:1004–6. doi: 10.2105/AJPH.2006.096826
5. Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull. (2009) 135:707–30. doi: 10.1037/a0016441
6. Gonzales G, Henning-Smith C. The affordable care act and health insurance coverage for lesbian, gay, and bisexual adults: analysis of the behavioral risk factor surveillance system. LGBT Health. (2017) 4:62–7. doi: 10.1089/lgbt.2016.0023
7. Brown C, Mayer DK. Are we doing enough to address the cancer care needs of the LGBT community? Clin J Oncol Nurs. (2015) 19:242–3. doi: 10.1188/15.CJON.242-243
8. Boehmer U, Elk R. LGBT populations and cancer: is it an ignored epidemic? LGBT Health. (2015) 3:1–2. doi: 10.1089/lgbt.2015.0137
9. Alpert AB, Scout NFN, Schabath MB, Adams S, Obedin-Maliver J, Safer JD. Gender- and sexual orientation- based inequities: promoting inclusion, visibility, and data accuracy in oncology. Am Soc Clin Oncol Educ Book. (2022) 42:1–17. doi: 10.1200/EDBK_350175
10. Kamen CS, Peoples AR, Tejani MA, Flannery M, Janelsins MC, Peppone LJ, et al. Disparities in psychological distress among lesbian, gay, bisexual and transgender (LGBT) cancer survivors. Ann Behav Med. (2014) 47:S245. doi: 10.1002/pon.3746
11. Ussher JM, Perz J, Kellett A, Chambers S, Latini D, Davis ID, et al. Health-related quality of life, psychological distress, and sexual changes following prostate cancer: a comparison of gay and bisexual men with heterosexual men. J Sex Med. (2016) 13:425–34. doi: 10.1016/j.jsxm.2015.12.026
12. Barrera I, Spiegel D. Review of psychotherapeutic interventions on depression in cancer patients and their impact on disease progression. Int Rev Psychiatry. (2014) 26:31–43. doi: 10.3109/09540261.2013.864259
13. Hamer M, Chida Y, Molloy GJ. Psychological distress and cancer mortality. J Psychosomat Res. (2009) 66:255–8. doi: 10.1016/j.jpsychores.2008.11.002
14. Chida Y, Hamer M, Wardle J, Steptoe A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Clin Pract Oncol. (2008) 5:466–75. doi: 10.1038/ncponc1134
15. Kamen C, Jabson JM, Mustian KM, Boehmer U. Minority stress, psychosocial resources, and psychological distress among sexual minority breast cancer survivors. Health Psychol. (2017) 36:529–37. doi: 10.1037/hea0000465
16. Boehmer U, Glickman M, Milton J, Winter M. Health-related quality of life in breast cancer survivors of different sexual orientations. Qual Life Res. (2012) 21:225–36. doi: 10.1007/s11136-011-9947-y
17. Matthews AK, Hotton A, Li CC, Miller K, Johnson A, Jones KW, et al. An internet-based study examining the factors associated with the physical and mental health quality of life of LGBT cancer survivors. LGBT Health. (2016) 3:65–73. doi: 10.1089/lgbt.2014.0075
18. Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: evaluation of the Center for Epidemiological Studies Depression Scale (CES-D). J Psychosomat Res. (1999) 46:437–43. doi: 10.1016/S0022-3999(99)00004-5
19. Patterson JG, Jabson Tree JM, Kamen C. Cultural competency and microaggressions in the provision of care to LGBT patients in rural and appalachian Tennessee. Pat Educ Counsel. (2019) 102:2081–90. doi: 10.1016/j.pec.2019.06.003
20. Lick DJ, Durso LE, Johnson KL. Minority stress and physical health among sexual minorities. Perspect Psychol Sci. (2013) 8:521–48. doi: 10.1177/1745691613497965
21. Katz A. Gay and lesbian patients with cancer. Oncol Nurs Forum. (2009) 36:203–7. doi: 10.1188/09.ONF.203-207
22. Kamen CS, Alpert A, Margolies L, Griggs JJ, Darbes L, Smith-Stoner M, et al. “Treat us with dignity”: a qualitative study of the experiences and recommendations of lesbian, gay, bisexual, transgender, and queer (LGBTQ) patients with cancer. Support Care Cancer. (2019) 27:2525–32. doi: 10.1007/s00520-018-4535-0
23. Murray-Garcia J, Tervalon M. The concept of cultural humility. Health Affairs. (2014) 33:1303. doi: 10.1377/hlthaff.2014.0564
24. Butler M, McCreedy E, Schwer N, Burgess D, Call K, Przedworski J, et al. Improving Cultural Competence to Reduce Health Disparities. AHRQ Comparative Effectiveness Reviews. Rockville, MD: Agency for Healthcare Research and Quality (2016).
25. Jongen C, McCalman J, Bainbridge R. Health workforce cultural competency interventions: a systematic scoping review. BMC Health Serv Res. (2018) 18:232. doi: 10.1186/s12913-018-3001-5
26. Govere L, Govere EM. How effective is cultural competence training of healthcare providers on improving patient satisfaction of minority groups? A systematic review of literature. Worldviews Evid Based Nurs. (2016) 13:402–10. doi: 10.1111/wvn.12176
27. Davey MP, Waite R, Nunez A, Nino A, Kissil K. A snapshot of patients' perceptions of oncology providers' cultural competence. J Cancer Educ. (2014) 29:657–64. doi: 10.1007/s13187-014-0619-9
28. Committee Committee on Improving the Quality of Cancer Care: Addressing the Challenges of an Aging Population; Board on Health Care Services; Institute of Medicine, Levit L, Balogh E, Nass S, Ganz PA, editors. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC: National Academies Press (2013).
29. Ganz PA, Hassett MJ, Miller DC. Challenges and opportunities in delivering high-quality cancer care: a 2016 update. Am Soc Clin Oncol Educ Book. (2016) 35:e294–300. doi: 10.1200/EDBK_159303
30. Bonvicini KA. LGBT healthcare disparities: what progress have we made? Pat Educ Counsel. (2017) 100:2357–61. doi: 10.1016/j.pec.2017.06.003
31. McGarry KA, Clarke JG, Cyr MG, Landau C. Evaluating a lesbian and gay health care curriculum. Teach Learn Med. (2002) 14:244–8. doi: 10.1207/S15328015TLM1404_8
32. Kelley L, Chou CL, Dibble SL, Robertson PA. A critical intervention in lesbian, gay, bisexual, and transgender health: knowledge and attitude outcomes among second-year medical students. Teach Learn Med. (2008) 20:248–53. doi: 10.1080/10401330802199567
33. Shrader A, Casero K, Casper B, Kelley M, Lewis L, Calohan J. Military lesbian, gay, bisexual, and transgender (LGBT) awareness training for health care providers within the military health system [formula: see text]. J Am Psychiatr Nurs Assoc. (2017) 23:385–92. doi: 10.1177/1078390317711768
34. Taylor AK, Condry H, Cahill D. Implementation of teaching on LGBT health care. Clin Teach. (2018) 15:141–4. doi: 10.1111/tct.12647
35. Wilsey CN, Cramer RJ, Macchia JM, Golom FD. Describing the nature and correlates of health service providers' competency working with sexual and gender minority patients: a systematic review. Health Promot Pract. (2021) 22:475–90. doi: 10.1177/1524839920943212
36. Damaskos P, Amaya B, Gordon R, Walters CB. Intersectionality and the LGBT cancer patient. Semin Oncol Nurs. (2018) 34:30–6. doi: 10.1016/j.soncn.2017.11.004
37. Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. (2014) 110:10–7. doi: 10.1016/j.socscimed.2014.03.022
38. Badgett MVL, Durso LE, Scheenbaum A,. New Patterns of Poverty in the Lesbian, Gay, Bisexual Community. (2013). Available online at: https://williamsinstitute.law.ucla.edu/wp-content/uploads/LGB-Poverty-Update-Jun-2013.pdf.
39. Movement Advancement Project (MAP),. Paying an Unfair Price: The Financial Penalty for LGBT People of Color in America. (2015). Available online at: http://www.lgbtmap.org/file/payingan-unfair-price-lgbt-people-of-color.pdf.
40. Lacombe-Duncan A. An intersectional perspective on access to HIV-related healthcare for transgender women. Transgend Health. (2016) 1:137–41. doi: 10.1089/trgh.2016.0018
41. Seay J, Hicks A, Markham MJ, Schlumbrecht M, Bowman M, Woodard J, et al. Developing a web-based LGBT cultural competency training for oncologists: the COLORS training. Pat Educ Counsel. (2019) 102:984–9. doi: 10.1016/j.pec.2019.01.006
42. Hudson KD. Identity-conscious services for diverse patients: a descriptive analysis of lesbian, gay, bisexual, and transgender-focused federally qualified community health centers. J Gay Lesbian Soc Serv. (2018) 30:282–98. doi: 10.1080/10538720.2018.1478353
43. Cahill S, Singal R, Grasso C, King D, Mayer K, Baker K, et al. Do ask, do tell: high levels of acceptability by patients of routine collection of sexual orientation and gender identity data in four diverse American community health centers. PLoS ONE. (2014) 9:e107104. doi: 10.1371/journal.pone.0107104
44. Grasso C, McDowell MJ, Goldhammer H, Keuroghlian AS. Planning and implementing sexual orientation and gender identity data collection in electronic health records. J Am Med Inform Assoc. (2019) 26:66–70. doi: 10.1093/jamia/ocy137
45. Ard KL, Keuroghlian AS. Training in sexual and gender minority health - expanding education to reach all clinicians. N Engl J Med. (2018) 379:2388–91. doi: 10.1056/NEJMp1810522
46. Cahill S, Makadon H. Sexual orientation and gender identity data collection in clinical settings and in electronic health records: a key to ending LGBT health disparities. LGBT Health. (2014) 1:34–41. doi: 10.1089/lgbt.2013.0001
47. Cahill SR, Baker K, Deutsch MB, Keatley J, Makadon HJ. Inclusion of sexual orientation and gender identity in stage 3 meaningful use guidelines: a huge step forward for LGBT health. LGBT Health. (2016) 3:100–2. doi: 10.1089/lgbt.2015.0136
48. Stirman SW, Baumann AA, Miller CJ. The FRAME: an expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement Sci. (2019) 14:58. doi: 10.1186/s13012-019-0898-y
49. Kamen C, Smith-Stoner M, Heckler CE, Flannery M, Margolies L. Social support, self-rated health, and lesbian, gay, bisexual, and transgender identity disclosure to cancer care providers. Oncol Nurs Forum. (2015) 42:44–51. doi: 10.1188/15.ONF.44-51
50. Kamen C, Alpert A, Murray N, Janelsins M, Mohile S, Mustian K, et al. “My Partner is My Family”: Psychosocial Oncology Needs of Sexual and Gender Minority Cancer Patients and Their Caregivers. Society of Behavioral Medicine, Washington, DC (2019).
51. Alpert AB, Gampa V, Lytle MC, Manzano C, Ruddick R, Poteat T, et al. I'm not putting on that floral gown: enforcement and resistance of gender expectations for transgender people with cancer. Pat Educ Counsel. (2021) 104:2552–8. doi: 10.1016/j.pec.2021.03.007
52. SocioCultural Research Consultants LLC. Dedoose Version 9.0.17, Web Application for Managing, Analyzing, and Presenting Qualitative and Mixed Method Research Data. Los Angeles, CA: SocioCultural Research Consultants LLC (2021).
53. Miller CJ, Barnett ML, Baumann AA, Gutner CA, Wiltsey-Stirman S. The FRAME-IS: a framework for documenting modifications to implementation strategies in healthcare. Implement Sci. (2021) 16:36. doi: 10.1186/s13012-021-01105-3
Keywords: cancer, sexual orientation, gender identity, health disparities, sexual and gender minorities, cultural humility
Citation: Kamen CS, Reichelt M, Dadgostar P, Alpert AB, Doucette C, Vaughan P, Keuroghlian AS and Yousefi-Nooraie R (2022) Sexual and gender minority cultural humility training for oncology settings: An example of iterative adaptation and implementation. Front. Health Serv. 2:958274. doi: 10.3389/frhs.2022.958274
Received: 31 May 2022; Accepted: 19 October 2022;
Published: 10 November 2022.
Edited by:
Borsika Adrienn Rabin, University of California, San Diego, United StatesReviewed by:
Bethany Rhoten, Vanderbilt University, United StatesWenxing Liu, Zhongnan University of Economics and Law, China
Copyright © 2022 Kamen, Reichelt, Dadgostar, Alpert, Doucette, Vaughan, Keuroghlian and Yousefi-Nooraie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Charles S. Kamen, Y2hhcmxlc19rYW1lbkB1cm1jLnJvY2hlc3Rlci5lZHU=
 Charles S. Kamen
Charles S. Kamen Melhaney Reichelt1
Melhaney Reichelt1