- 1Public Health and Environment, The Water Institute, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 2Department of Implementation Science, Wake Forest School of Medicine, Winston-Salem, NC, United States
- 3Wake Forest Baptist Comprehensive Cancer Center, Medical Center Boulevard, Winston-Salem, NC, United States
- 4School of Civil Engineering, University of Leeds, Leeds, United Kingdom
- 5Gangarosa Department of Environmental Health, Rollins School of Public Health, Emory University, Atlanta, GA, United States
Background: Safe water, sanitation, and hygiene (WaSH) is important for health, livelihoods, and economic development, but WaSH programs have often underdelivered on expected health benefits. Underperformance has been attributed partly to poor ability to retain effectiveness following adaptation to facilitate WaSH programs' implementation in diverse contexts. Adaptation of WaSH interventions is common but often not done systematically, leading to poor outcomes. Models and frameworks from the adaptation literature have potential to improve WaSH adaptation to facilitate implementation and retain effectiveness. However, these models and frameworks were designed in a healthcare context, and WaSH interventions are typically implemented outside traditional health system channels. The purpose of our work was to develop an adaptation model tailored specifically to the context of WaSH interventions.
Methods: We conducted a scoping review to identify key adaptation steps and identify tools to support systematic adaptation. To identify relevant literature, we conducted a citation search based on three recently published reviews on adaptation. We also conducted a systematic database search for examples of WaSH adaptation. We developed a preliminary model based on steps commonly identified across models in adaptation literature, and then tailored the model to the WaSH context using studies yielded by our systematic search. We compiled a list of tools to support systematic data collection and decision-making throughout adaptation from all included studies.
Results and Conclusions: Our model presents adaptation steps in five phases: intervention selection, assessment, preparation, implementation, and sustainment. Phases for assessment through sustainment are depicted as iterative, reflecting that once an intervention is selected, adaptation is a continual process. Our model reflects the specific context of WaSH by including steps to engage non-health and lay implementers and to build consensus among diverse stakeholders with potentially competing priorities. We build on prior adaptation literature by compiling tools to support systematic data collection and decision-making, and we describe how they can be used throughout adaptation steps. Our model is intended to improve program outcomes by systematizing adaptation processes and provides an example of how systematic adaptation can occur for interventions with health goals but that are implemented outside conventional health system channels.
Introduction
Despite decades of effort and investment, water, sanitation, and hygiene (WaSH) interventions in low- and middle-income countries have often failed to deliver expected health benefits, and even infrastructure access and behavioral outcomes have been poorly sustained. WaSH interventions have shown health benefits in small-scale pilots and tightly controlled trial settings. However, adapting these evidence-based interventions to facilitate implementation at-scale in ways that maintain originally demonstrated levels of effectiveness has proved challenging (1–3). These challenges have been attributed in part to poor ability to adapt to context and retain effectiveness as interventions are implemented at scale (4–10).
Rapid scale-up has outpaced learning on what adaptations are necessary and effective processes for making them. Across WaSH interventions, adaptation is common but often does not follow a systematic process (11, 12). Overall, there is little guidance on how adaptation should occur throughout WaSH intervention development, implementation, and sustainment. In some cases, documentation of adaptation may be actively suppressed, as implementers sometimes perceive that any modification to the original intervention is undesirable (11).
Adaptation literature as a subfield of implementation science provides concepts and tools that could be leveraged to improve adaptation in the WaSH sector. The past decade has seen substantial advancement of theoretical tools and methods to understand how, when, and why to adapt, and to support systematic and replicable study of adaptations and their effects on program outcomes (13–17). Theoretical tools and systematic methods from adaptation literature have been successfully applied for improving outcomes in health programming, but, to the best of our knowledge, have yet to be applied in WaSH.
Most published literature of WaSH intervention adaptation reports adaptation in the early stages of programming, typically in intervention design stage before any implementation has been done, or in the pilot stage before implementation at-scale [see, e.g., (18–21)]. These studies report adaptations designed and implemented with strong support from academics. This poorly reflects the realities of WaSH programs, where adaptation is an ongoing process done by practitioners throughout implementation and rarely applies academic frameworks and theories (12).
We argue that adaptation models and frameworks have been underused in WaSH to date but offer valuable insights for achieving effectively implementing and sustaining WaSH interventions. These tools, when applied in the health sector, have been shown to improve outcomes such as intervention acceptability, adoption, and sustainability (16, 22). However, existing adaptation models were predominantly developed in the context of healthcare delivery [see, e.g., (17, 23)]. While WaSH interventions have health goals, they also have non-health human rights and development goals. Implementation and regulation are often divided across different ministries and interest groups. At the local level, some implementers may be health workers (e.g., community health workers), but overall stakeholders are diverse and include a variety of non-health and for-profit implementers (e.g., rural development committees, engineers, and small business owners). Existing adaptation models assume interventions are implemented by trained healthcare professionals, whereas in WaSH implementation by volunteers, beneficiaries, and laypersons is common. These contextual differences warrant more in-depth examination and tailoring of existing adaptation tools to better match the context of WaSH and similar interventions implemented outside traditional health system channels.
We developed a model specifically tailored to WaSH interventions to guide stakeholders through systematic adaptation. The purpose of this model is to improve adaptation by describing a series of key steps and providing tools to support systematic decision-making throughout, thereby improving outcomes. We propose that applying this model will improve adaptation in WaSH by systematizing the adaptation process and reducing unsystematic decision-making (12, 24).
Methods
We followed the five steps for scoping reviews outlined by Arksey and O'Malley (25): (1) identifying the research question, (2) identifying relevant studies, (3) selecting studies, (4) charting the data, and (5) collating, summarizing, and reporting the results. We conducted a scoping review as opposed to a systematic review to explore the breadth of available adaptation literature and capture evolving concepts and terminology that would be difficult to capture through a systematic review approach (25, 26).
Identifying the Research Question
Our scoping review was guided by two research questions: (a) What are the steps required for systematic intervention adaptation in WaSH? and (b) What tools exist to guide these adaptation steps?
We focused our review on WaSH interventions targeting drinking water, sanitation, and handwashing with soap. We included adaptations to interventions that were user-facing (e.g., household toilets and sinks) and non-user facing (e.g., municipal water and sewage treatment plants). We considered the following to be out of scope: water resource management for recreational, agricultural, and other non-consumption uses; non-sewerage wastewater treatment; and hygiene programs without a handwashing component.
Identifying Relevant Studies
Scoping Search
We began with three recent reviews that have synthesized models of key adaptation steps from prior literature: Movsisyan et al. (15), Kirk et al. (16), and Escoffery et al. (17). We then searched for updates, refinements, or alternatives to these models using forward and backward citation searching in Google Scholar. Forward and backward citation searching entails beginning with an initial set of seed studies—in our case reviews by Movsisyan, Kirk, and Escoffery—then reviewing the references cited therein and references that have subsequently cited those seed studies. This approach has been found to have comparable success in identifying relevant papers as keyword searches, and is recommended for exploratory, scoping reviews where an initial narrowly defined keyword search may not capture all relevant concepts (27).
To identify tools to guide the adaptation process, we identified three additional recent reviews of adaptation theory and practice (13, 14, 28) and repeated our process of citation searching. We also reviewed three recent papers on implementation science in WaSH and environmental health (1, 29, 30).
Systematic Database Search
We conducted a systematic search to identify references describing adaptations in WaSH. We searched PubMed, Web of Science, and Scopus for English language studies published between 1st January 2000 and 21 June 2021 (the search date). For a full listing of search terms, see Supplementary File 1.
Study Selection
For studies identified through forward and backward citation searching in our scoping search, we reviewed the full text of identified studies and included those intended to be applicable to a wide variety of interventions. We excluded studies applicable only to a specific type of intervention or context not relevant to WaSH (e.g., models specific to HIV/AIDS programs). We prioritized publications from the past 5 years and stopped citation searching when we reached concept saturation (i.e., references did not yield new information or meaningfully refine our findings from previously identified references).
For studies identified through our systematic database search, we included studies that described adaptations to WaSH interventions delivered in households, institutional settings (e.g., healthcare facilities, schools), and water and sanitation utilities. We included retrospective studies of previous adaptations and prospective studies describing designing and planning adaptations for future implementation. We also included studies that presented tools to support adaptation. We excluded studies that identified a need for adaptation but undertook no further steps to design or implement any modifications. We assessed these inclusion and exclusion criteria in two rounds of screening: first of titles and abstracts, then the full-texts of studies that passed the initial screening.
Charting the Data; Collating, Summarizing, and Reporting Results
First, we identified the adaptation steps described in the three adaption models that formed the basis of our literature search (15–17). We synthesized steps that were common across all models into a preliminary model of key steps. We also added steps that were not included in all models but reflected a new development in adaptation theory. We then compiled a list of actions required to complete each step.
Second, we conducted two rounds of revision to this preliminary model. We revised model steps based on updates or refinements from adaptation literature identified through forward and backward citation searching. We then revised our model based on the specific characteristics of WaSH programs. For studies of WaSH adaptations identified in our systematic database search, we documented the following: steps taken, stakeholders engaged, and barriers and facilitators. We used this information to tailor our model to WaSH interventions.
Third, we compiled a list of tools available to support data collection and decision-making for each step. We compiled these tools from both non-WaSH adaptation literature and WaSH-specific adaptation examples. We sorted these tools into groups based on their primary purpose (e.g., assessing needs, evaluating outcomes).
Our results summarize the scope of literature reviewed, review key adaptation principles based on included literature, and present our refined model of adaptation steps and the tools available to support each step. We then discuss how this paper synthesizes prior models and contributes to existing adaptation literature and the specific considerations for adaptation in a WaSH context.
Results
Scope of Literature Reviewed
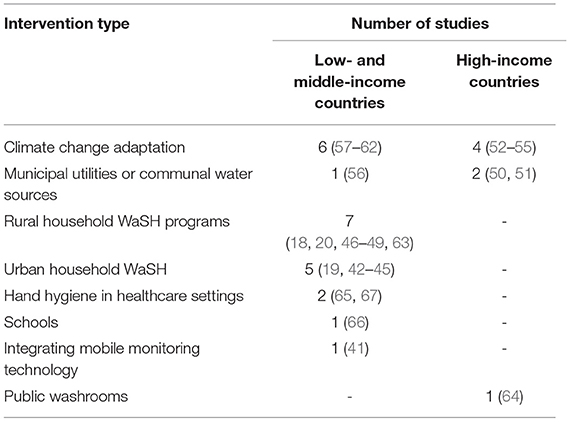
Our model is grounded in previous adaptation models proposed by Movsisyan (15), Kirk (16), and Escoffery (17). We identified an additional 19 references in adaptation literature to refine and update our model (1, 10, 13, 14, 23, 24, 28–40). Our systematic search for WaSH adaptation studies yielded 1,649 unique references across all databases. After screening, we identified 30 relevant studies (18–20, 41–67) (Table 1). An overview of the setting, target population, and intervention of each of these 30 studies is included in Supplementary File 2.
Key Principles in Adaptation
A key principle within adaptation literature is the distinction between core functions of an intervention (i.e., its purpose and mechanisms by which outcomes and health impacts are achieved) vs. its forms (i.e., the specific steps or activities used to carry out each core function) (40). The purpose of adaptation is to alter the forms of an intervention to improve performance, while preserving the underlying core functions. Distinguishing between core functions vs. forms allows for flexibility to deviate from the original specific activities of an intervention, while retaining the underlying mechanisms that drives its effectiveness.
Where adaptations do not appropriately identify and preserve core functions, they risk sacrificing effectiveness (16, 36, 38, 40). For example, if core functions are not well understood, adaptations may unknowingly undermine them, resulting in no improvement or even worse performance (11). Stakeholders can iterate adaptations through trial and error, but this can be highly inefficient when numerous adaptations must be tried and discarded before a suitable adaptation is identified. Understanding core functions can improve efficiency by guiding selection of adaptations that are more likely to be successful from the start (68).
In some cases, particularly in WaSH interventions where core functions were not well-defined during intervention development, it may be appropriate to intentionally modify core functions. However, this should be done with good understanding of core functions of the original intervention, such that modifications are intentionally designed to improve them based on robust understanding of needs and context, rather than undermining them accidentally.
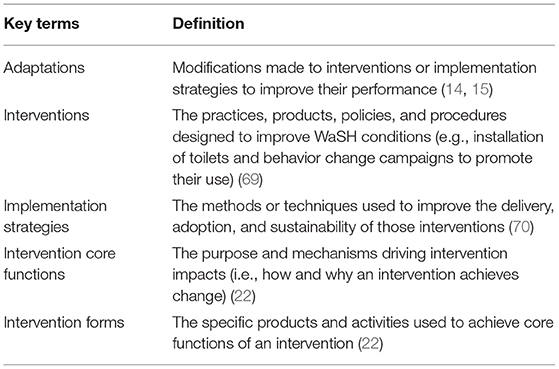
Terminology to describe key constructs and concepts within adaptation literature sometimes lacks consensus. To the extent possible, we have attempted to use the terms that best represent current consensus. For clarity and transparency, definitions of key terms as operationalized in this paper are presented in Table 2.
A Model for Adapting WaSH Programs
Model Overview and Application
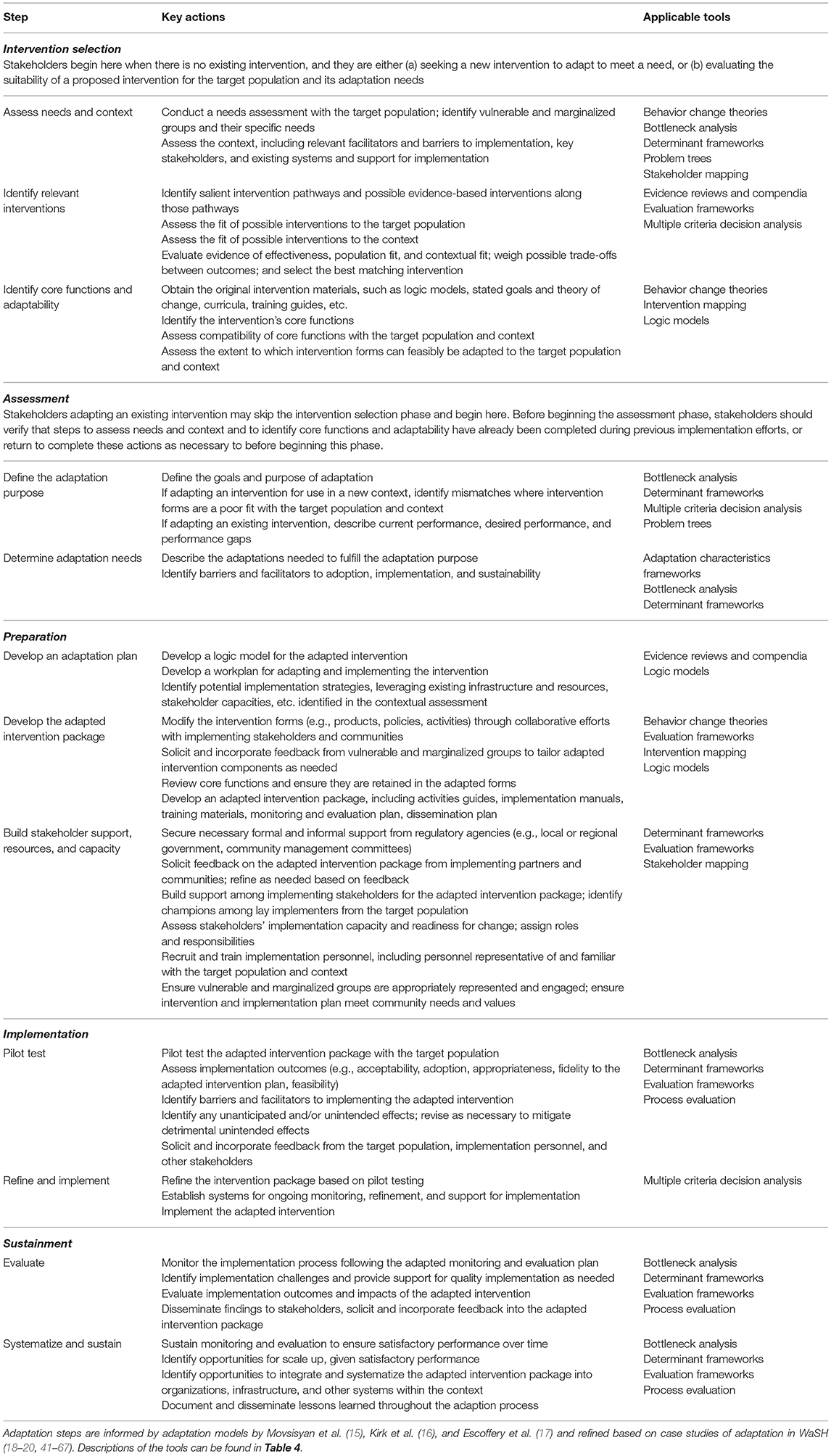
Our model presents adaptation steps in five phases: intervention selection, assessment, preparation, implementation, and sustainment. Phases 2–4 (i.e., assessment through sustainment) are depicted as cyclical, reflecting the fact that once an intervention is selected, adaptation is an ongoing process that can be iterated to address unanticipated challenges and continually improve performance (16, 38). Each phase contains between two and four individual steps (Figure 1). Table 3 describes the specific actions required to complete each step. Table 4 presents tools that can support data collection and decision-making throughout the model steps.
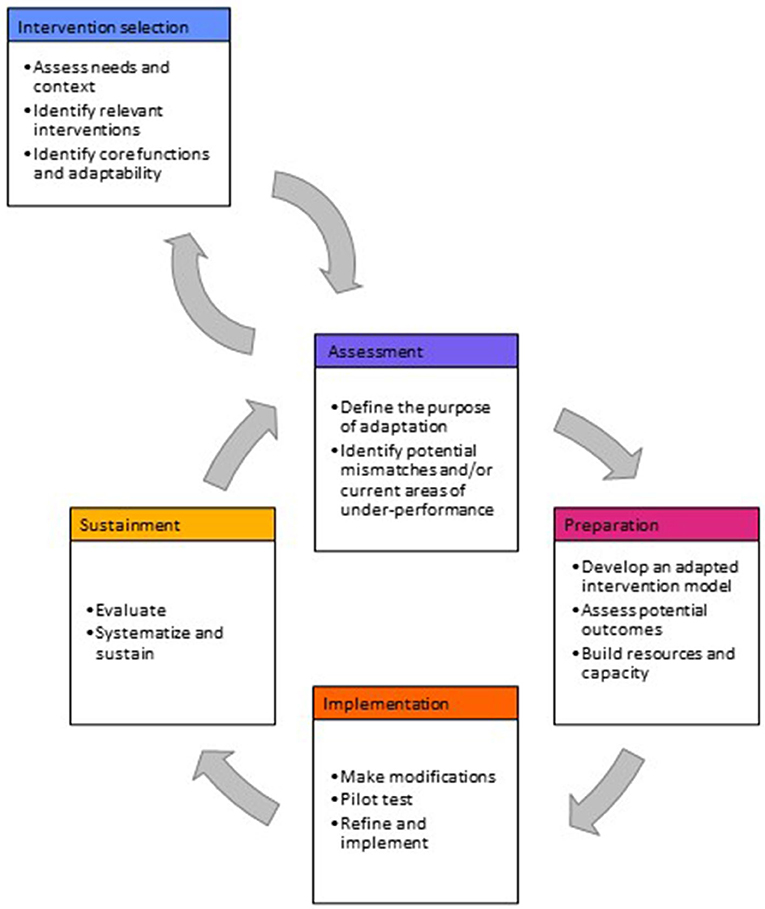
Figure 1. Steps for adaptation in WaSH programs. Model is informed by adaptation models by Movsisyan et al. (15), Kirk et al. (16), and Escoffery et al. (17) and refined based on case studies of adaptation in WaSH (18–20, 41–67).
This model is designed to support two possible adaptation scenarios. In the first scenario, there is no pre-existing intervention. Stakeholders are selecting an intervention from another context to adapt for delivery in a new context. This may occur for several reasons. One, stakeholders have identified a health or development need that is not currently being met through an existing intervention. Stakeholders decide to meet this need through adapting an intervention from another context, rather than conducting de novo intervention development. Two, advocates for a particular intervention argue for its implementation in a new context, and adaptations are needed to improve contextual fit. In this case, stakeholders responsible for funding and implementing must determine if a need exists that warrants adapting and implementing this new intervention and whether other interventions would be more suitable. The first phase of the model (intervention selection) guides stakeholders through conducting a needs assessment, determining what interventions exist to meet this need, and selecting an intervention that is appropriate and adaptable in the target context. Subsequent phases of the model guide practitioners through adapting the selected intervention and implementing it in the new context.
In the second scenario, stakeholders have identified a need to adapt an existing intervention to improve its performance or address unanticipated problems encountered during implementation. In this case, stakeholders can skip the first phases of intervention selection and begin at the assessment phase. During assessment, stakeholders describe the purpose and specific needs for adaptation of the existing intervention, then proceed through subsequent phases of the model to prepare and implement the adaptation. In some cases, stakeholders in this scenario may still need to conduct selected actions under the intervention selection phase if they lack important information on an interventions' core functions or other contextual factors necessary for subsequent steps. In other cases, the assessment phase may reveal that an intervention is fundamentally incompatible with context, indicating a need to return to the intervention selection phase.
In both scenarios, this model is designed to guide stakeholders through a systematic adaptation process. Adaptations made through systematic processes have more beneficial effects on program outcomes, compared to adaptations that are unsystematic (12, 24). Steps in this model are intended to help stakeholders adhere to key principles of adaptation (i.e., identifying and preserving core functions), design effective adaptations, and understand adaptations' effects on program outcomes.
Adaptation Steps
In the intervention selection phase, stakeholders first assess the target population's needs and the context in which adaptation will occur. Stakeholders then identify possible interventions to address these needs and assess their core functions and adaptability (15, 17). This phase is intended for stakeholders who have identified a health need that is not currently met by an existing intervention and are adapting an intervention from another context. Stakeholders adapting an existing intervention may skip this phase.
In the assessment phase, stakeholders determine the purpose of the adaptation and identify adaptation needs. Where the purpose of adaptation is modifying an intervention for delivery in a new context, adaptation needs will center around mismatches between the selected intervention and target context (13–17). Where the purpose of adaptation is improving performance of an existing intervention, adaptation needs will center around identifying gaps between current and desired performance (16, 38). In some cases, the assessment phase may reveal a need to return to the intervention selection phase, either to complete key steps such as assessing core functions if they are not already known, or to fully select a new intervention if assessment reveals fundamental incompatibilities between the existing intervention and the current context that are unlikely to be rectified through adaptation.
In the preparation phase, stakeholders develop an adaptation plan and assemble an adapted intervention package, including adapted activities, an implementation plan, evaluation plan, and training materials (13–17). This adapted intervention package will use different intervention forms from the original intervention but should retain the same core functions (16, 40). In the final step of preparation, stakeholders build support for the adapted intervention package (e.g., recruiting local champions) (39), and recruit and train implementers (13–15, 17, 39).
In the implementation phase, stakeholders pilot test and refine the adapted intervention (14, 15, 17). During pilot testing, stakeholders assess implementation outcomes [e.g., acceptability, feasibility (80)], barriers and facilitators to adaptation, and any potential unintended consequences (e.g., instances where adaptation undermined core functions and reduced effectiveness). If pilot testing indicates substantial deficiencies, stakeholders may choose not to proceed to implementation at scale and instead return to earlier steps to iterate adaptation development (38). Otherwise, the adapted intervention package is refined, then implemented at scale.
In the sustainment phase, stakeholders evaluate the adaptation, following the evaluation plan identified in the preparation phase (15, 17). Then, assuming satisfactory performance, stakeholders work to systematize and sustain the adapted intervention through identifying opportunities for scale up and integrating the adapted intervention package into organizational structures and implementation systems (15).
Depending on the scale of the adaptation, stakeholder may need to dedicate proportionally more or less effort to specific steps and actions. For example, adaptations to tailor a behavior change messaging intervention to improve relevance to local behavioral drivers may not require securing formal permission from regulatory agencies but will require capacity building among implementers. This model is designed to be comprehensive for adaptations making major modifications. For smaller-scale adaptations, stakeholders may omit specific actions but should have appropriate justification for doing so.
Tools to Support Adaptation
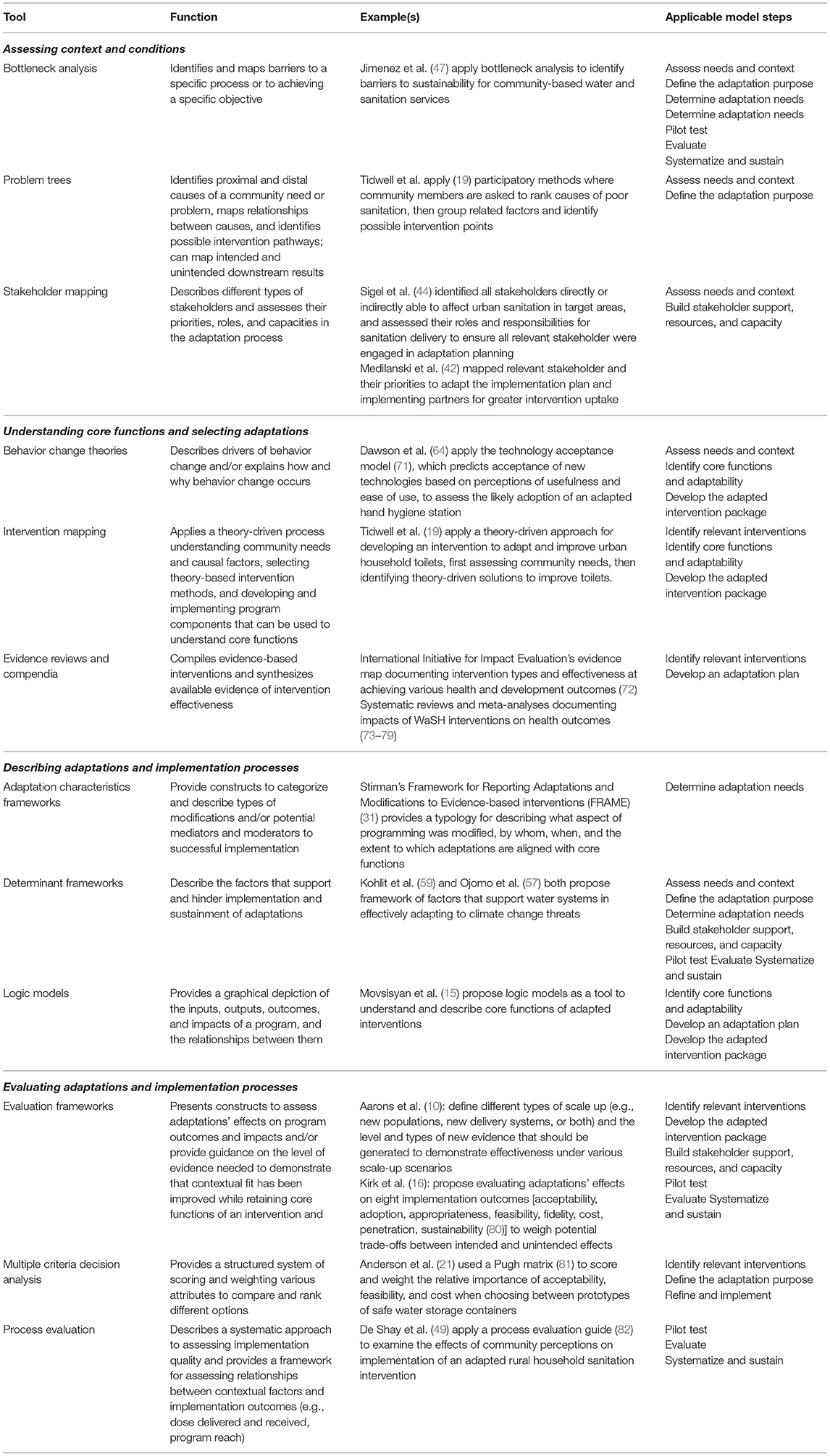
In this section, we present tools that can support stakeholders in executing steps of the adaptation model. Table 4 provides a description of each tool, an example of its application, and indicates the adaptation model steps in which it can be applied. Table 3 describing the model steps also contains a column indicating applicable tools for each step.
We organized these tools into four groups based on their function: assessing context and conditions, understanding core functions and selecting adaptations, describing adaptations and implementation processes, and evaluating adaptations and implementation. We categorized each tool into only a single group based on its primary function, but some tools can serve multiple functions. For example, we included bottleneck analysis in the group of tools for assessing context and conditions, as bottleneck analysis can be used to determine barriers to achieving a particular health target. However, bottleneck analysis could also be used for describing implementation processes. We encourage stakeholders to apply these tools throughout the adaptation process wherever they are useful.
Tools for assessing context and conditions can be applied in the intervention selection and assessment phase for steps to understand the target population's needs and context. They may also be applied in the preparation, implementation, or evaluation phases to assess contextual barriers and facilitators to successful implementation. Tools for understanding core functions and selecting adaptations apply primarily in the intervention selection phase. These tools may also be useful in subsequent steps if stakeholders are adapting an existing intervention where documentation of the original intervention is poor or core functions are not well defined, and stakeholders require additional information to develop an adapted intervention plan.
Tools for describing adaptations and implementation processes can be used in the preparation stage to plan the adapted intervention package, in the implementation stage to understand and improve implementation, and in the sustainment phase to disseminate findings. These tools allow for more systematic and comprehensive description of the adaption and can also be used in combination with monitoring and evaluation data to explore barriers and drivers to success. Tools for evaluating adaptations and implementation are most applicable in the implementation and sustainment phases, to support steps for pilot testing and evaluation.
Discussion
We developed an adaptation model tailored specifically to the context of WaSH programs. Adaptation is an important part of program cycle, facilitating implementation of evidence-based interventions while retaining their effectiveness. Our model is intended to improve outcomes by systematizing the adaptation process, as is consistent with literature showing that unsystematic adaptations have poorer outcomes (24). While a wealth of adaptation models and frameworks exist, they originate from a healthcare context, which differs substantially from the WaSH context. Limited tools are available to support adaptation outside the healthcare context. Our model addresses this evidence gap by specifically considering the needs of WaSH interventions implemented outside conventional health system channels.
Our model also contributes to the adaptation literature by synthesizing prior models and frameworks. Adaptation literature has seen proliferation of models and frameworks over the past two decades especially, but few attempts to synthesize them. New concepts (e.g., core functions) have been recognized but not yet integrated into existing models (13, 14). Proliferation of models and frameworks without comprehensive synthesis efforts can create challenges where concepts develop overlapping, conflicting, or ambiguous meanings (83). Our model combats this challenge by synthesizing a broad array of adaptation models and frameworks and aligning them with current concepts in adaptation literature.
Below, we discuss how our model updates and refines prior adaptation literature and the specific contextual needs of WaSH adaptation.
Updates and Refinements to Prior Adaptation Models
Our model is grounded in previous adaptation models proposed by Movsisyan (15), Kirk (16), and Escoffery (17). Movsisyan et al. (15) propose 11 steps divided into four phases—exploration, preparation, implementation, and sustainment—and draw from prior literature proposing the same phases for de novo intervention delivery (84). Escoffery et al. (17) propose 11 similar steps, which are similarly ordered but not explicitly divided into phases.
These steps are well represented in examples of WaSH literature yielded by our systematic search. While studies did not explicitly reference these models or use their terminology, we found adaptation stakeholders commonly taking steps throughout all phases. For example, studies reported steps in the exploration phase to identify performance gaps and the need for adaptation (43, 67, 85), in the preparation phase to prepare the adapted intervention materials (19, 20, 48), in the implementation phase to pilot test and refine the adapted intervention (18, 44), and in the sustainment phase to evaluate the adapted intervention (56, 66). Most studies focused on the early stages of assessment and preparation to identify adaptation needs and propose solutions. We found fewer examples where proposed adaptations had been actually implanted and refined in pilot projects (44, 46, 56, 66, 67), and fewer still that had been evaluated in larger-scale trials and integrated into programming at-scale (49, 63).
Kirk et al.'s model (16) is aimed primarily at assessing whether adaptations are systematic and aligned with core functions of the original intervention. It provides constructs to describe adaptations, outlines steps to assess potential outcomes, and guides decision-making surrounding whether adaptations should proceed to implementation at scale based on their potential outcomes. It also makes an important contribution to the literature by incorporating steps to consider core functions as part of the adaptation process.
Our systematic literature search yielded no examples that referenced core functions, nor analogous concepts under a different name. We found two examples of WaSH adaptation taking a systematic approach to assessing potential outcomes, but this was done through empirical data collection on key pre-selected outcomes using continuous quality improvement framework (21, 86). Overall, the scope of potential outcomes considered by all WaSH studies was limited, typically only direct health impacts expected of the intervention (e.g., diarrheal disease prevalence) or intermediate outcomes such as functionality and use of WaSH infrastructure. We found few examples of studies anticipating or exploring other potential effects on other health or non-health impacts, despite evidence that WaSH intervention adaptation can have broad, unanticipated effects on mental, social, and economic wellbeing (12).
Our model retains analogous steps to those proposed by Movsisyan and Escoffery. We integrated Kirk's model by including specific actions for identifying core functions and potential outcomes throughout steps in the preparation and implementation phases. Throughout the model, we have also updated steps and actions to reflect the concept of core functions vs. forms. Models from Movsisyan and Escoffery contain actions for identifying and preserving important “core components” (an early variant of the concept of core functions). We have updated these to reflect current thinking on core functions and forms, as described by Kirk (16) and others (13, 22, 40).
Our model makes several important refinements to previous models. First, we proposed the addition of a distinct phase for intervention selection as the first phase in the adaptation process. In our model, we group the initial steps in both the Movsisyan and Escoffery models into a phase for intervention selection, and propose that some stakeholders may skip this first phase if they are adapting a preexisting intervention. When stakeholders begin with intervention selection, they are engaging in proactive adaptation (i.e., adaptations made in response to anticipated needs before they arise). When stakeholders skip the intervention selection phase and begin at assessment, they are engaging in reactive adaptation (i.e., adaptations made in response to unanticipated needs that arise during implementation (16, 31).
Reactive adaptation is the norm in WaSH and other sectors (24). Previous models include intervention selection steps as an essential part of the process, and provide little guidance for what to do in the case of reactive adaptation where an intervention is already in place. Our model better accounts for the realities of reactive intervention by separating these steps into a separate, optional phase. Second, we depict the adaptation process as a cycle. Movsisyan and Escoffery both recognize that some adaptation steps may require iteration but present their models as linear and offer little guidance for when iteration should occur. Kirk (16) and others (38) explicitly depict iterative adaptation design and refinement, but it is unclear where in the overall adaptation process this should occur. Our model puts this in context by depicting the assessment, implementation, and sustainment phases as a cycle that is initiated after intervention selection, which can be iterated for multiple rounds of adaptation and ongoing improvement throughout the adapted intervention delivery.
Third, we integrated actions to identify, engage, and build support among stakeholders throughout the model. This reflects the specific context of WaSH adaptation, where stakeholders are diverse and represent government, non-governmental organizations, and the private sector across multiple disciplines, as well as lay implementers and volunteers from within beneficiary communities. These stakeholders can have competing goals and objectives that require additional efforts to solicit and incorporate their feedback and build consensus, which is not reflected in non-WaSH specific adaptation models (1, 47, 61, 62, 87).
Fourth, we integrate a list of tools that can support data collection and decision-making throughout the adaptation process (Table 4). Prior models broadly describe the steps and actions required for adaptation but provide few tools to guide stakeholders explicitly through completing these actions.
Specific Considerations for Adapting Interventions in the WaSH Context
Below, we discuss four specific contextual considerations for adapting WaSH interventions, which we derived from literature describing examples of WaSH adaptations presented in Table 1. They reflect commonly reported challenges, opportunities, and lessons learned in these studies. While not all these considerations are necessarily unique to WaSH, they introduce complexities into the adaptation process that warrant particular attention.
Multi-Component, Complex Interventions
WasH interventions are complex, often including both a hardware and a software component that are interdependent. Hardware interventions are the infrastructure or other physical goods that provide people access to WaSH, such as water taps and toilets used by individuals and large systems for water and sewerage treatment. Software interventions are the efforts to change WaSH practices by altering knowledge, attitudes, norms, and other behavioral drivers. Interventions can be either supply- or demand-side to increase availability of WaSH products for consumers or to increase consumer demand for those products, respectively. WaSH interventions may also target policy from the national to local levels.
Despite the interconnectedness of WaSH components, responsibilities for implementation, financing, monitoring, regulation are often fragmented across multiple stakeholders at various levels within government, non-governmental organizations, and the private sector. This fragmentation can create challenges with funding shortfalls, lack of leadership to coordinate and champion the original intervention and associated adaptation activities, and non-comprehensive monitoring efforts (47, 61, 87). Furthermore, poorly aligned objectives and insufficient coordination and communication between stakeholders can lead to competing and conflicting adaptations (1, 62). Additional efforts may be needed to generate buy-in from stakeholders in the preparation phase, compared to interventions in other sectors with fewer or less diverse stakeholders (53). Evaluation frameworks and multiple criteria decision analysis may be useful to describe intervention and adaptation goals more comprehensively and to facilitate compromises between differing stakeholder priorities.
Identifying Core Functions and the “Performance Envelope”
Many WaSH programs have been critiqued for lacking well-defined core functions (1, 87, 88). Disentangling core functions of multiple simultaneous interventions at different levels (e.g., policy-level subsidies and household-level behavior change messaging for sanitation) can be particularly challenging but is important for effective adaptation (13). For interventions where core functions are not already well defined, stakeholders may need to allocate time and resources to identify them. Methods for identifying core functions are beyond the scope of this paper but have been described elsewhere (22).
Recent studies have suggested that WaSH interventions have a “performance envelope” (i.e., a limited range of settings in which the contextual conditions align with the core functions of the intervention) (89, 90). For example, one study of a participatory urban sanitation intervention in which community engagement was critical to the theory of change concluded that the intervention should only be selected for adaptation in areas where communities show “willingness to participate in planning, training, and operation and maintenance” (44). Similarly, the specific pathogens and transmission pathways contributing to the burden of disease will vary by context, such that interventions to control the predominant transmission pathway in one setting may not produce comparable effects in another setting (1). Tools such as behavior change theories and intervention mapping can help identify incompatibilities between core functions and the intended context.
Decentralized Programming and Lay Implementers
Adaptation models developed for medical and public health settings typically assume that implementers and beneficiary populations are distinct groups, and that implementers are trained professionals. However, in WaSH these assumptions may not hold. Some WaSH programs are decentralized, with governance, planning, and implementation being conducted at the village or sub-regional level (47). Programs may emphasize recruitment of community volunteers and other lay individuals to organize and champion grassroots implementation efforts. Furthermore, WaSH programs typically have a distinct health goal but are often implemented and managed by non-health ministries, organizations, and other entities. Stakeholder mapping can be used to explore the diversity of relevant stakeholders and map their priorities and capabilities (42, 44).
Decentralization and lay implementers require specific consideration for adaption in WaSH compared to interventions in other sectors. Lay implementers have deep knowledge of the local context that makes them highly effective at designing contextually appropriate adaptations (91), and various studies have emphasized the importance of engaging community members and local-level implementers in decision-making processes (44, 45, 60). However, studies have also found that institutional support structures may be lacking in highly decentralized programs, and low access to information, funding, and support structures can hinder adaptation (62).
In response, adaptation in WaSH will likely require additional effort, time, and resources to fully engage and leverage the knowledge and skills of local level implementers and community members. WaSH programs may benefit from parallel efforts to build the skills of local-level implementers to autonomously engage in formal data collection and research and program evaluation efforts (12). In some cases, modifying or simplifying tools to make them more user-friendly may be necessary to improve engagement of community members and lay implementers and to improve overall program outcomes (56).
Inclusive Interventions
WaSH programs often target entire communities and aim to reach universal coverage. Universal coverage targets are informed by evidence that community-wide coverage is necessary to achieve “herd protection,” where exposure to fecal pathogens is reduced not only within the home but also in the broader community environment (92). However, targeting an entire community's population can raise challenges to ensure that adapted interventions are accessible and appropriate for all. In some cases, multiple adaptations may be necessary to develop different tailored versions of the intervention that separately address different demographics within a community, as individuals' specific WaSH needs and preferences will vary based on factors such as age, gender, and ability (48). Efforts to engage community members throughout the adaptation process, especially vulnerable and marginalized populations, is important for ensuring that adapted interventions are inclusive for all.
Strengths, Limitations, and Next Steps
The purpose of study was to identify the steps required for successful adaptation of WaSH interventions and to identify tools to guide these steps. Our scoping review methods were designed to explore the breadth of available literature and synthesize key principles and illustrative examples, rather than to systematically identify all cases. We identified broad categories of tools to support data collection and decision-making in adaptation, and the specific examples included under each category are not intended to be exhaustive. It is also likely that sectors outside of WaSH use different tools that may also aid WaSH adaptation, which this search methodology was not designed to capture. Future systematic reviews to identify tools more narrowly but deeply within each category could aid future adaptation research and practice.
We prioritized our review for adaptation literature from the past 5 years, and we restricted our search to WaSH studies published from 2000 onwards. These search periods reflect the newness of adaptation as an area of systematic study. Adaptation as a subfield of implementation science has undergone substantial evolution in recent years [for an in-depth discussion, see, e.g., (34, 36)]. Concepts from earlier literature been revised in favor of the more current concepts we present here, and we therefore did not prioritize this early literature in our search. Similarly, adaption has been the norm in WaSH for decades, but literature systematically describing the process using concepts from adaptation literature (or early analogous ideas) prior to 2000 is unlikely.
We found few instances where models, frameworks, and other tools from adaptation literature were applied in studies of WaSH adaptation, even within recent literature. The studies of WaSH adaptation that we reviewed often developed their own tools as part of the study, rather than drawing on existing tools in adaptation literature. Yet in many cases, these tools were purpose-built and had low generalizability beyond the original study context. Tools in adaptation literature were more generalizable across a broad range of contexts. While they have not yet been widely applied in WaSH, they offer the potential to improve the efficiency and effectiveness of adaptation by reducing the burden to develop new tools for every context and improving the ability to compare and apply learnings across settings.
Under-utilization of tools from adaptation literature in WaSH likely reflects in part the newness of adaptation as a discipline, and we expect that application of adaptation tools in WaSH will increase over time. We expect that our model may need revision as adaptation literature disseminates more broadly into WaSH research and practice, and more evidence becomes available.
Conclusions
Adaptation of WaSH interventions is common but does not always follow a systematic process. Unsystematic adaptation can lead to sub-optimal or even detrimental outcomes, such as decreased effectiveness if adaptations undermine core functions (11) or even harm if modifications are made without considering the range of possible detrimental effects on physical, mental, and social wellbeing (12). Adaptation literature offers a variety of tools to guide stakeholders through the process of designing, implementing, and evaluating adaptations to facilitate implementation while retaining effectiveness. However, these tools have rarely been applied in WaSH, and they were designed predominantly for interventions in a healthcare context, which differs substantially from the WaSH context in terms of the diversity of health and non-health actors involved in implementation and regulation.
We developed a model and framework of tools to assist adaptation tailored specifically to the WaSH context. Our model is underpinned primarily by evidence of household-level WaSH interventions, though we expect it could be successfully applied in institutional contexts as well (e.g., healthcare, schools) settings as well. We anticipate that application of this model will improve the effectiveness of adapted WaSH interventions by systematizing the adaptation process. Our model advances implementation science literature by proposing steps for adapting interventions that are implemented outside the healthcare sector by diverse lay and non-health stakeholders, and by specifically identifying tools that can support data collection and decision-making for more systematic adaptation processes and improved program outcomes.
Author Contributions
DA, JB, and MF: conceptualization. DA: formal analysis and writing—original draft. DA, SB, JB, and MF: writing—review and editing. All authors read and approved the final manuscript.
Funding
DA was supported by grants from the University of North Carolina Royster Society of Fellows and from the National Institute of Environmental Health Sciences (T32ES007018). The funders had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript, or decision to submit for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the following individuals for their feedback on drafts on this manuscript: Clarissa Brocklehurst, Aaron Salzberg.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2022.896234/full#supplementary-material
References
1. Haque SS, Freeman MC. The applications of implementation science in water, sanitation, and hygiene (WASH) research and practice. Environ Health Perspect. (2021) 129:65002. doi: 10.1289/EHP7762
2. Andres LA, Borja-Vega C, Fenwick C, De Jesus Filho J, Gomez Suarez RE. Overview and Meta-Analysis of Global Water, Sanitation, and Hygiene (WASH) Impact Evaluations. Policy Research Working Paper. Washington, DC: The World Bank (2018). doi: 10.1596/1813-9450-8444
3. Hueso A. Is ‘access to adequate and equitable sanitation' for all by 2030 achievable? Perspectives from sector experts on what needs to change to realise the sustainable development goal. J Water Sanit Hyg Dev. (2016) 6:650–7. doi: 10.2166/washdev.2016.078
4. Parvez SM, Rahman MJ, Azad R, Rahman M, Unicomb L, Ashraf S, et al. Achieving equitable uptake of handwashing and sanitation by addressing both supply and demand-based constraints: findings from a randomized controlled trial in rural Bangladesh. Int J Equity Health. (2021) 20:16. doi: 10.1186/s12939-020-01353-7
5. Sanitation Hygiene Infant Nutrition Efficacy (SHINE) Trial Team, Humphrey JH, Jones AD, Manges A, Mangwadu G, Maluccio JA, et al. The sanitation hygiene infant nutrition efficacy (SHINE) trial: rationale, design, and methods. Clin Infect Dis. (2015) 61(suppl_7):S752–S8. doi: 10.1093/cid/civ844
6. Boisson S, Sosai P, Ray S, Routray P, Torondel B, Schmidt W-P, et al. Promoting latrine construction and use in rural villages practicing open defecation: process evaluation in connection with a randomised controlled trial in Orissa, India. BMC Res Notes. (2014) 7:486. doi: 10.1186/1756-0500-7-486
7. Routray P, Torondel B, Jenkins MW, Clasen T, Schmidt W-P. Processes and challenges of community mobilisation for latrine promotion under Nirmal Bharat Abhiyan in rural Odisha, India. BMC Public Health. (2017) 17:453. doi: 10.1186/s12889-017-4382-9
8. Cameron L, Olivia S, Shah M. Scaling up sanitation: evidence from an RCT in Indonesia. J Dev Econ. (2019) 138:1–16. doi: 10.1016/j.jdeveco.2018.12.001
9. Chambers R. Going to scale with community-led total sanitation: reflections on experience, issues and ways forward. IDS Practice Papers. (2009) 2009:01–50. doi: 10.1111/j.2040-0225.2009.00001_2.x
10. Aarons GA, Sklar M, Mustanski B, Benbow N, Brown CH. “Scaling-out” evidence-based interventions to new populations or new health care delivery systems. Implementation Science. (2017) 12:111. doi: 10.1186/s13012-017-0640-6
11. Venkataramanan V. Testing CLTS Approaches For Scalability: Lessons From CLTS Implementation in Severn Countries. Washington, DC: Plan International USA Inc. (2016).
12. Anderson DM, Gupta AK, Birken SA, Sakas Z, Freeman MC. Adaptation in rural water, sanitation, and hygiene programs: a qualitative study in Nepal. Int J Hyg Environ Health. (2022) 240:113919. doi: 10.1016/j.ijheh.2022.113919
13. Evans RE, Moore G, Movsisyan A, Rehfuess E. How can we adapt complex population health interventions for new contexts? Progressing debates and research priorities. J Epidemiol Community Health. (2021) 75:40–5. doi: 10.1136/jech-2020-214468
14. Movsisyan A, Arnold L, Copeland L, Evans R, Littlecott H, Moore G, et al. Adapting evidence-informed population health interventions for new contexts: a scoping review of current practice. Health Res Policy Sys. (2021) 19:13. doi: 10.1186/s12961-020-00668-9
15. Movsisyan A, Arnold L, Evans R, Hallingberg B, Moore G, O'Cathain A, et al. Adapting evidence-informed complex population health interventions for new contexts: a systematic review of guidance. Implementation Sci. (2019) 14:105. doi: 10.1186/s13012-019-0956-5
16. Kirk MA, Moore JE, Wiltsey Stirman S, Birken SA. Towards a comprehensive model for understanding adaptations' impact: the model for adaptation design and impact (MADI). Implementation Sci. (2020) 15:56. doi: 10.1186/s13012-020-01021-y
17. Escoffery C, Lebow-Skelley E, Udelson H, Böing EA, Wood R, Fernandez ME, et al. A scoping study of frameworks for adapting public health evidence-based interventions. Transl Behav Med. (2019) 9:1–10. doi: 10.1093/tbm/ibx067
18. Manjang B, Hemming K, Bradley C, Ensink J, Martin JT, Sowe J, et al. Promoting hygienic weaning food handling practices through a community-based programme: intervention implementation and baseline characteristics for a cluster randomised controlled trial in rural Gambia. BMJ Open. (2018) 8:e017573. doi: 10.1136/bmjopen-2017-017573
19. Tidwell JB, Chipungu J, Chilengi R, Curtis V, Aunger R. Using a theory-driven creative process to design a peri-urban on-site sanitation quality improvement intervention. BMC Public Health. (2019) 19:565. doi: 10.1186/s12889-019-6898-7
20. Nordhauser J, Rosenfeld J. Adapting a water, sanitation, and hygiene picture-based curriculum in the Dominican Republic. Glob Health Promot. (2020) 27:6–14. doi: 10.1177/1757975919848111
21. Anderson DM, Fisher MB, Kwena O, Kambou H, Broseus R, Williams AR, et al. Adapting a safe water storage container to improve household stored water quality in rural Burkina Faso: a cluster randomized trial. J Water Sanit Hyg Dev. (2021) 11:719–31. doi: 10.2166/washdev.2021.065
22. Kirk MA, Haines ER, Rokoske FS, Powell BJ, Weinberger M, Hanson LC, et al. A case study of a theory-based method for identifying and reporting core functions and forms of evidence-based interventions. Transl Behav Med. (2021) 11:21–33. doi: 10.1093/tbm/ibz178
23. Aarons GA, Green AE, Palinkas LA, Self-Brown S, Whitaker DJ, Lutzker JR, et al. Dynamic adaptation process to implement an evidence-based child maltreatment intervention. Implementation Sci. (2012) 7:32. doi: 10.1186/1748-5908-7-32
24. Moore JE, Bumbarger BK, Cooper BR. Examining adaptations of evidence-based programs in natural contexts. J Prim Prev. (2013) 34:147–61. doi: 10.1007/s10935-013-0303-6
25. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
26. Sucharew H, Macaluso M. Progress notes: methods for research evidence synthesis: the scoping review approach. J Hosp Med. (2019) 14:416–8. doi: 10.12788/jhm.3248
27. Hinde S, Spackman E. Bidirectional citation searching to completion: an exploration of literature searching methods. Pharmacoeconomics. (2015) 33:5–11. doi: 10.1007/s40273-014-0205-3
28. Escoffery C, Lebow-Skelley E, Haardoerfer R, Boing E, Udelson H, Wood R, et al. A systematic review of adaptations of evidence-based public health interventions globally. Implementation Sci. (2018) 13:125. doi: 10.1186/s13012-018-0815-9
29. Hering JG. Implementation science for the environment. Environ Sci Technol. (2018) 52:5555–60. doi: 10.1021/acs.est.8b00874
30. Setty K, Cronk R, Setty K, Cronk R, George S, Anderson D, et al. Adapting translational research methods to water, sanitation, and hygiene. Int J Environ Res Public Health. (2019) 16:4049. doi: 10.3390/ijerph16204049
31. Wiltsey Stirman S, Baumann AA, Miller CJ. The FRAME: an expanded framework for reporting adaptations and modifications to evidence-based interventions. Implementation Sci. (2019) 14:58. doi: 10.1186/s13012-019-0898-y
32. Stirman SW, Miller CJ, Toder K, Calloway A. Development of a framework and coding system for modifications and adaptations of evidence-based interventions. Implementation Sci. (2013) 8:65. doi: 10.1186/1748-5908-8-65
33. Miller CJ, Barnett ML, Baumann AA, Gutner CA, Wiltsey-Stirman S. The FRAME-IS: a framework for documenting modifications to implementation strategies in healthcare. Implementation Sci. (2021) 16:36. doi: 10.1186/s13012-021-01105-3
34. Castro FG, Barrera M, Martinez CR. The cultural adaptation of prevention interventions: resolving tensions between fidelity and fit. Prev Sci. (2004) 5:41–5. doi: 10.1023/B:PREV.0000013980.12412.cd
35. Mark MM. Adding adaptation/modification size and scope to frameworks for classifying changes to an intervention. Prev Sci. (2021) 22:923–7. doi: 10.1007/s11121-021-01248-1
36. Chambers DA, Norton WE. The adaptome: advancing the science of intervention adaptation. Am J Prev Med. (2016) 51:S124–S31. doi: 10.1016/j.amepre.2016.05.011
37. von Thiele Schwarz U, Aarons GA, Hasson H. The value equation: three complementary propositions for reconciling fidelity and adaptation in evidence-based practice implementation. BMC Health Serv Res. (2019) 19:868. doi: 10.1186/s12913-019-4668-y
38. Miller CJ, Wiltsey-Stirman S, Baumann AA. Iterative decision-making for evaluation of adaptations (IDEA): a decision tree for balancing adaptation, fidelity, and intervention impact. J Community Psychol. (2020) 48:1163–77. doi: 10.1002/jcop.22279
39. Chen EK, Reid MC, Parker SJ, Pillemer K. Tailoring evidence-based interventions for new populations: a method for program adaptation through community engagement. Eval Health Prof. (2012) 36:73–92. doi: 10.1177/0163278712442536
40. Perez Jolles M, Lengnick-Hall R, Mittman BS. Core functions and forms of complex health interventions: a patient-centered medical home illustration. J Gen Intern Med. (2019) 34:1032–8. doi: 10.1007/s11606-018-4818-7
41. Murthy SL, Shemie D, Bichai F. The role of adaptation in mobile technology innovation for the water, sanitation and hygiene sector. Water Pract Technol. (2018) 13:143–56. doi: 10.2166/wpt.2018.002
42. Medilanski E, Chuan L, Mosler HJ, Schertenleib R, Larsen TA. Identifying the institutional decision process to introduce decentralized sanitation in the city of Kunming (China). Environ Manage. (2007) 39:648–62. doi: 10.1007/s00267-005-0321-0
43. Lako SM, Ngnikam E, Ndongo B, Tina M editors. Urine diverting dry toilets as appropriate adaptation to flood prone cities of developing countries. 38th WEDC International Conference. Loughborough UK: Loughborough University (2015).
44. Sigel K, Staudel J, Londong J. Experiences with stakeholder involvement in strategic sanitation planning: a case study of the city of Darkhan, Mongolia. Water Sci Technol. (2014) 14:504–12. doi: 10.2166/ws.2014.001
45. Putri HE, Maraputra AN, Efna MJ, Permana Y, Martiningtyas MP, Listiyanti PA, et al, editors. Improvement of student awareness on cleanliness and environmental health through stop motion video technology. J Phys Conf Ser. (2020) 1521:042042. doi: 10.1088/1742-6596/1521/4/042042
46. Ogunjobi B, Lawal U, Abdullahi R, Otusanya S editors. Sustaining the gains of community-led total sanitation (CLTS) through latrine demonstration centre: a case study of rural communities' challenge of constructing latrines on loose soil formation in Jigawa state, Nigeria. 36th WEDC International Conference: Delivering Water, Sanitation and Hygiene Services in an Uncertain Environment. Loughborough (2013).
47. Jimenez A, Jawara D, LeDeunff H, Naylor KA, Scharp C. Sustainability in Practice: Experiences from Rural Water and Sanitation Services in West Africa. Sustainability-Basel. (2017) 9:14. doi: 10.3390/su9030403
48. Kamban N, Ray Norman W editors. Inclusive WASH development: Technology adaptations for persons with disabilities. 36th WEDC International Conference: Delivering Water, Sanitation and Hygiene Services in an Uncertain Environment. Loughborough (2013).
49. De Shay R, Comeau DL, Sclar GD. Community perceptions of a multilevel sanitation behavior change intervention in rural Odisha, India. Int J Environ Res Public Health. (2020) 17:4472. doi: 10.3390/ijerph17124472
50. Tscheikner-Gratl F, Mikovits C, Rauch W, Kleidorfer M. Adaptation of sewer networks using integrated rehabilitation management. Water Sci Technol. (2014) 70:1847–56. doi: 10.2166/wst.2014.353
51. Curk BC, Zeleznik BB, Bogardi I. Adaptation of water supply to changing climate and land-Use activities, case of ljubljana water supply, Slovenia. Water (Switzerland). (2020) 12:288. doi: 10.3390/w12010288
52. Van Engelenburg J, Van Slobbe E, Hellegers P. Towards sustainable drinking water abstraction: an integrated sustainability assessment framework to support local adaptation planning. J Integr Environ Sci. (2019) 16:89–122. doi: 10.1080/1943815X.2019.1636284
53. Hasse JU, Weingaertner DE. From vision to action: roadmapping as a strategic method and tool to implement climate change adaptation-the example of the roadmap 'water sensitive urban design 2020. Water Sci Technol. (2016) 73:2251–9. doi: 10.2166/wst.2016.065
54. Garnier M. Critical review of adaptation measures to reduce the vulnerability of European drinking water resources to the pressures of climate change. Environ Mol Mutagen. (2019) 64:138–53. doi: 10.1007/s00267-019-01184-5
55. Clark RM, Li Z, Buchberger SG. Adapting water treatment design and operations to the impacts of global climate change. Front Earth Sci. (2011) 5:363–70. doi: 10.1007/s11707-011-0197-7
56. Barrington D, Fuller K, McMillan A. Water safety planning: adapting the existing approach to community-managed systems in rural Nepal. J Water Sanit Hyg Dev. (2013) 3:392–401. doi: 10.2166/washdev.2013.120
57. Ojomo E, Bartram J. Adapting drinking-water systems to coastal climate change: evidence from Viet Nam and the Philippines. Reg Environ Change. (2016) 16:2409–18. doi: 10.1007/s10113-016-0965-8
58. Mukheibir P, Boronyak-Vasco L, Alofa P. Dynamic Adaptive Management Pathways for Drinking Water Security in Kiribati. Climate Change Management (2017). p. 287–301. doi: 10.1007/978-3-319-50094-2_17
59. Kohlitz J, Chong J, Willetts J. Analysing the capacity to respond to climate change: a framework for community-managed water services. Clim Dev. (2019) 11:775–85. doi: 10.1080/17565529.2018.1562867
60. Chan T, MacDonald MC, Kearton A, Elliott M, Shields KF, Powell B, et al. Climate adaptation for rural water and sanitation systems in the Solomon Islands: A community scale systems model for decision support. Sci Total Environ. (2020) 714:919–31. doi: 10.1016/j.scitotenv.2020.136681
61. Bollinger LA, Bogmans CWJ, Chappin EJL, Dijkema GPJ, Huibregtse JN, Maas N, et al. Climate adaptation of interconnected infrastructures: a framework for supporting governance. Reg Environ Change. (2014) 14:919–31. doi: 10.1007/s10113-013-0428-4
62. Alhassan S, Hadwen WL. Challenges and opportunities for mainstreaming climate change adaptation into WaSH development planning in Ghana. Int J Environ Res Public Health. (2017) 14:749. doi: 10.3390/ijerph14070749
63. Mehta KM, Irani L, Chaudhuri I, Mahapatra T, Schooley J, Srikantiah S, et al. Health layering of self-help groups: impacts on reproductive, maternal, newborn and child health and nutrition in Bihar, India. J Glob Health. (2020) 10:021007. doi: 10.7189/jogh.10.0201007
64. Dawson CH, Mackrill JB, Cain R. Assessing user acceptance towards automated and conventional sink use for hand decontamination using the technology acceptance model. Ergonomics. (2017) 60:1621–33. doi: 10.1080/00140139.2017.1316018
65. Salmon S, Pittet D, Sax H, McLaws ML. The 'My five moments for hand hygiene' concept for the overcrowded setting in resource-limited healthcare systems. J Hosp Infect. (2015) 91:95–9. doi: 10.1016/j.jhin.2015.04.011
66. Lang MC. Implementation of an evidence-based hand hygiene program in elementary schools in Ghana, as part of a city-to-city partnership between ottawa public health and KEEA health directorate. Fam Community Health. (2012) 35:203–11. doi: 10.1097/FCH.0b013e318250bc56
67. Muller SA, Diallo AOK, Wood R, Bayo M, Eckmanns T, Tounkara O, et al. Implementation of the WHO hand hygiene strategy in Faranah regional hospital, Guinea. Antimicrob Resist Infect Control. (2020) 9:65. doi: 10.1186/s13756-020-00723-8
68. Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Quality & Safety. (2015) 24:228–38. doi: 10.1136/bmjqs-2014-003627
69. Brown CH, Curran G, Palinkas LA, Aarons GA, Wells KB, Jones L, et al. An overview of research and evaluation designs for dissemination and implementation. Annu Rev Public Health. (2017) 38:1–22. doi: 10.1146/annurev-publhealth-031816-044215
70. Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implementation Sci. (2015) 10:21. doi: 10.1186/s13012-015-0209-1
71. Lee Y, Kozar KA, Larsen KR. The technology acceptance model: Past, present, and future. Commun Assoc Inf Syst. (2003) 12:50. doi: 10.17705/1CAIS.01250
73. Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM Jr. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis. (2005) 5:42–52. doi: 10.1016/S1473-3099(04)01253-8
74. Esrey SA, Potash JB, Roberts L, Shiff C. Effects of improved water supply and sanitation on ascariasis, diarrhoea, dracunculiasis, hookworm infection, schistosomiasis, and trachoma. Bull World Health Organ. (1991) 69:609–21.
75. Clasen TF, Alexander KT, Sinclair D, Boisson S, Peletz R, Chang HH, et al. Interventions to improve water quality for preventing diarrhoea. Cochrane Database Syst Rev. (2015) 10:CD004794. doi: 10.1002/14651858.CD004794.pub3
76. Ejemot-Nwadiaro RI, Ehiri JE, Arikpo D, Meremikwu MM, Critchley JA. Hand washing promotion for preventing diarrhoea. Cochrane Database Syst Rev. (2015) 9:Cd004265. doi: 10.1002/14651858.CD004265.pub3
77. Wolf J, Pruss-Ustun A, Cumming O, Bartram J, Bonjour S, Cairncross S, et al. Assessing the impact of drinking water and sanitation on diarrhoeal disease in low- and middle-income settings: systematic review and meta-regression. Trop Med Int Health. (2014) 19:928–42. doi: 10.1111/tmi.12331
78. Freeman MC, Garn JV, Sclar GD, Boisson S, Medlicott K, Alexander KT, et al. The impact of sanitation on infectious disease and nutritional status: a systematic review and meta-analysis. Int J Hyg Environ Health. (2017) 220:928–49. doi: 10.1016/j.ijheh.2017.05.007
79. Sclar GD, Penakalapati G, Caruso BA, Rehfuess EA, Garn JV, Alexander KT, et al. Exploring the relationship between sanitation and mental and social well-being: A systematic review and qualitative synthesis. Soc Sci Med. (2018). doi: 10.1016/j.socscimed.2018.09.016
80. Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Adm Policy Ment Health. (2011) 38:65–76. doi: 10.1007/s10488-010-0319-7
82. Saunders RP, Evans MH, Joshi P. Developing a process-evaluation plan for assessing health promotion program implementation: a how-to guide. Health Promot Pract. (2005) 6:134–47. doi: 10.1177/1524839904273387
83. Martinez RG, Lewis CC, Weiner BJ. Instrumentation issues in implementation science. Implementation Sci. (2014) 9:118. doi: 10.1186/s13012-014-0118-8
84. Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health. (2011) 38:4–23. doi: 10.1007/s10488-010-0327-7
85. Putri NS, Herlily editors. Investigating community adaptability and resilience in Urban Kampung, study case: Water and sanitation infrastructure of Kampung Muka, North Jakarta. IOP Conference Series: Earth and Environmental Science (2020) 452:012095. doi: 10.1088/1755-1315/452/1/012095
86. Fisher MB, Danquah L, Seidu Z, Fechter AN, Saga B, Bartram JK, et al. WaSH CQI: applying continuous quality improvement methods to water service delivery in four districts of rural northern Ghana. PLoS ONE. (2020) 15:e0233679-e. doi: 10.1371/journal.pone.0233679
87. Venkataramanan V, Crocker J, Karon A, Bartram J. Community-led total sanitation: a mixed-methods systematic review of evidence and its quality. Environ Health Perspect. (2018) 126:026001. doi: 10.1289/EHP1965
88. Sigler R, Mahmoudi L, Graham JP. Analysis of behavioral change techniques in community-led total sanitation programs. Health Promot Int. (2015) 30:16–28. doi: 10.1093/heapro/dau073
90. Rehfuess EA, Bartram J. Beyond direct impact: evidence synthesis towards a better understanding of effectiveness of environmental health interventions. Int J Hyg Environ Health. (2014) 217:155–9. doi: 10.1016/j.ijheh.2013.07.011
91. Anderson DM, Gupta AK, Birken SA, Sakas Z, Freeman MC. Successes, challenges, and support for men versus women implementers in water, sanitation, and hygiene programs: a qualitative study in rural Nepal. Int J Hyg Environ Health. (2021) 236:113792. doi: 10.1016/j.ijheh.2021.113792
Keywords: adaptation model, evidence-based intervention (EBI), implementation science, water, sanitation, hygiene, WaSH
Citation: Anderson DM, Birken SA, Bartram JK and Freeman MC (2022) Adaptation of Water, Sanitation, and Hygiene Interventions: A Model and Scoping Review of Key Concepts and Tools. Front. Health Serv. 2:896234. doi: 10.3389/frhs.2022.896234
Received: 14 March 2022; Accepted: 19 April 2022;
Published: 09 May 2022.
Edited by:
Ann Catrine Eldh, Linköping University, SwedenReviewed by:
Sandul Yasobant, Indian Institute of Public Health Gandhinagar (IIPHG), IndiaMadhumita Dobe, All India Institute of Hygiene and Public Health, India
Copyright © 2022 Anderson, Birken, Bartram and Freeman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Darcy M. Anderson, ZGFyY3kuYW5kZXJzb25AYWx1bW5pLnVuYy5lZHU=
 Darcy M. Anderson
Darcy M. Anderson Sarah A. Birken
Sarah A. Birken Jamie K. Bartram1,4
Jamie K. Bartram1,4