- 1Department of Nursing, Adama General Hospital and Medical College, Adama, Ethiopia
- 2Department of Public Health, Adama General Hospital and Medical College, Adama, Ethiopia
- 3Department of Biomedical Sciences, Adama Hospital Medical College, Adama, Ethiopia
- 4Department of Medicine, Adama General Hospital and Medical College, Adama, Ethiopia
Background: Substance use, including tobacco, alcohol, khat, and illicit drugs, is a significant preventable contributor to the global burden of disease. Women are particularly vulnerable during their reproductive years, with substance use during pregnancy posing serious risks to maternal and fetal health. Therefore, this study aimed to assess of prevalence of substance use and determine associated risk factors among pregnant women in Adama, Central Ethiopia.
Methods: A health facility-based cross-sectional study was conducted among 472 pregnant women. Participants were selected using a systematic sampling technique. Data were collected through an interviewer-administered structured questionnaire. Binary logistic regression was employed to model the association between substance use and explanatory variables. Adjusted odds ratios (AORs) with 95% confidence intervals (CIs) were used to estimate the strength of association. Statistical significance was determined at a p-value < 0.05.
Result: The overall prevalence of substance use during pregnancy was 22.0% (95% CI: 18.2–26.0). Unplanned pregnancy (AOR = 3.49, 95% CI: 1.23–9.89), pre-pregnancy substance use (AOR = 24.16, 95% CI: 11.49–40.82), husband/partner substance use (AOR = 4.51, 95% CI: 1.44–14.20), and ever heard about the side effects of substance use (AOR = 14.60, 95% CI: 5.31–17.65) were factors significantly associated with maternal substance use during pregnancy.
Conclusion: Nearly one in four pregnant women reported using substances during pregnancy. Educational and counseling interventions during antenatal care should emphasize the risks of substance use on maternal health and fetal development, particularly targeting women with a history of substance use or unplanned pregnancies. Efforts should also involve partners and employ community-based strategies to raise awareness of these risks.
Introduction
Substance use is the consumption of harmful stimulant substances, including alcohol, tobacco products, caffeine, khat leaves, illicit drugs, inhalants, and other substances that can be ingested, inhaled, injected, or absorbed into the body, potentially leading to dependence and adverse effects on physiological, mental, physical, or emotional functions (1, 2). Substance use is a major preventable contributor to the global burden of disease (3). Tobacco, alcohol, and other illicit drugs are recognized by the World Health Organization (WHO) as leading contributors to ill health worldwide (4).
Women are more vulnerable to substance use during their reproductive years, which means that those who are pregnant or planning to become pregnant face a higher risk of substance abuse (5, 6). Substance use during pregnancy is a major public health issue due to its harmful effects on both the mother and the fetus (6–8). This includes an increased risk of inadequate parenting, miscarriage, ectopic pregnancy, premature rupture of membranes, placental abruption, intrauterine growth restriction, early labor, spontaneous abortion, infant mortality, stillbirth, congenital anomalies, neonatal abstinence syndrome, Fetal Alcohol Spectrum Disorder (FASD), low birth weight, and preterm delivery (6, 7, 9–12).
According to the WHO, women comprise about 40% of the global substance-using population (13). The prevalence of substance use during pregnancy varies widely across countries, regions, and ethnic groups (14). Tobacco is the most commonly used substance during pregnancy, followed by alcohol, cannabis, and other illicit drugs (6). In Sub-Saharan Africa, substance use during pregnancy ranges from 2.2% to 36.5% (15–17), while in East African countries, including Ethiopia, it ranges from 11.3% to 60% (18–23). Previous studies have identified various factors associated with substance use during pregnancy, including maternal age, maternal and partner/husband's education level, monthly income, occupation, partner/husband's substance use, lack of antenatal care, gestational age, pregnancy status, pre-pregnancy substance use, and place of residence (6, 17, 19, 20, 23–25).
Globally, various strategies have been introduced to address substance use during pregnancy, including the WHO guidelines for identifying and managing substance use in expectant mothers (26, 27). In Ethiopia, efforts to limit cigarette smoking and khat chewing have been made, but enforcement varies across regions. Cultural practices also pose significant challenges. For instance, alcohol consumption is deeply embedded in social and religious traditions, particularly in rural areas, where alcoholic beverages are commonly consumed during social gatherings and ceremonies. Additionally, khat chewing is not only a social norm in many communities but also serves ritualistic and economic purposes, making its reduction particularly complex. These deeply rooted cultural norms hinder public health efforts to reduce substance use during pregnancy (20, 23).
Although limited studies have examined maternal substance use in Ethiopia, particularly during pregnancy, evidence remains scarce, especially within the study area. A thorough review of the literature indicates that while some study exists at the national level, there is a lack of location-specific data on the prevalence and associated factors of substance use among pregnant women in Adama, central Ethiopia. Given regional variations in substance use patterns and risk factors, localized data are crucial for designing effective interventions. Therefore, this study aimed to assess the prevalence and associated factors of maternal substance use in this setting. The findings will provide insights to guide targeted interventions, build awareness, provide effective care, improve maternal and child health outcomes, and contribute to the broader understanding of substance use during pregnancy and its implications for maternal and child well-being.
Methods
Study design and setting
A health facility-based cross-sectional study was conducted from February 1 to April 30, 2024, in Adama town, located in central Ethiopia. Adama is situated 99 km southeast of Addis Ababa, in the East Shoa zone of the Oromia region. According to the 2007 Census conducted by the Central Statistical Agency (CSA) of Ethiopia, the town has a total population of 220,212, comprising 108,872 men and 111,340 women (28). The town's healthcare system comprises one government hospital and eight health centers. The hospital, situated within the town, delivers preventive and curative services to a population exceeding five million. Meanwhile, the health centers collectively serve an estimated catchment population of nearly half a million.
Study population and eligibility criteria
The source population consisted of all pregnant women attending antenatal care at public health facilities in Adama town. The study population included pregnant women attending antenatal care at selected public health facilities in Adama town during the study period. However, pregnant women who were seriously ill or unable to communicate were excluded from the study.
Sample size determination and sampling procedure
The required sample size for this study was calculated using the single population proportion formula with the following assumptions: a 95% confidence interval (CI) (critical value Zα/2 = 1.96), a calculated margin of error of 4% (d = 0.04), and a proportion of substance use (p = 0.265) of 26.5%, based on a study conducted in Eastern Ethiopia (23). After accounting for a 5% non-response rate, the final sample size was calculated to be 490.
The public health facilities in the town were stratified into hospitals and health centers. Out of the eight health centers, four were selected through simple random sampling, while the hospital was chosen purposively. The total sample size was distributed proportionally among the selected facilities based on their average ANC patient flow over the preceding three months. Study participants were then selected independently from each facility using a systematic sampling technique. The sampling interval for each facility was determined by dividing the average number of pregnant women attending ANC in the previous three months by the required sample size for that facility.
Variables of the study
Dependent variable
The dependent variable was maternal substance use during pregnancy, defined as a self-reported exposure to at least one of the three substances (alcohol, khat, or tobacco) at any point during the current pregnancy before the interview, regardless of the dose or frequency (20, 23, 26).
Alcohol use was defined as the consumption of any alcoholic beverage at any time during the pregnancy, regardless of the amount or frequency. This included both industrially produced alcohol (containing ethanol or ethyl alcohol) and locally produced beverages such as Teji, Areke, or Tela (9, 20, 23).
Khat use was defined as chewing khat at any time during the pregnancy, regardless of the amount or frequency (20, 23, 29).
Tobacco use was defined as the use of any tobacco product at any time during the pregnancy. This included cigarettes, other smoking forms such as shisha/hookah and bidi, as well as non-smoking forms like snuff or chewing tobacco, regardless of the amount or frequency (20, 23, 30).
Independent variables
The independent variables include socio-demographic and economic factors (age, religion, marital status, residence, educational status, occupational status, and monthly income), Obstetric and health-related characteristics [gravidity, parity, gestational age, pregnancy status, antenatal care (ANC) follow-up, history of adverse birth outcomes, and history of medical problems before or during pregnancy], and Behavioral-related characteristics (pre-pregnancy substance use, ever heard about the side effects of substance use, husband or partner substance use, and a history of intimate partner violence).
Data collection tools and procedure
Data were collected using a structured, interviewer-administered questionnaire adapted from a review of previous literature (6, 19, 20, 22, 23, 25). The questionnaire included sections on sociodemographic and economic characteristics, obstetric and health-related factors, and behavioral characteristics relevant to mothers’ experiences during their pregnancy. Initially prepared in English, the questionnaire was translated into the local languages, Amharic and Afan Oromo, with back-translation performed to ensure accuracy.
Before the primary data collection, a pretest was conducted on 5% (n = 25) of the sample to assess clarity and reliability. Data collectors received two days of training on the data collection tools, procedures, and study objectives. Ten trained midwives collected the data. Mothers were interviewed in private places to ensure their privacy and to encourage participation. Regular meetings and continuous supervision were implemented to ensure quality and consistency throughout the data collection process.
Data processing and statistical analysis
Data were entered using Epi-Info Version 7.2 and then exported to SPSS Version 25 for processing and analysis. Before analysis, the data were cleaned, coded, and categorized. Descriptive statistics were used to describe the characteristics of the participants, and the proportion of substance use was calculated with a 95% confidence interval. The association between independent variables and substance use was modeled using binary logistic regression. Initially, bivariable binary logistic regression analysis was conducted to identify variables with a crude association with substance use. At this level, variables with a p-value < 0.25 were considered candidates for inclusion in the multivariable logistic regression analysis. Subsequently, multivariable logistic regression analysis was performed to identify factors independently associated with substance use. The regression model was fitted using a standard model-building approach. Adjusted odds ratios (AOR) with 95% confidence intervals (CI) were used to estimate the strength of the association. The statistical significance of associations was declared for variables with a p-value < 0.05.
Ethical consideration
Ethical approval was obtained from the Institutional Review Board of Adama General Hospital and Medical College. A permission letter was subsequently submitted to the Adama Town Health Office and public health facilities, where approval was granted to conduct the study. Participants were fully informed about the study's potential benefits and risks, and their voluntary participation or refusal was documented through written consent. Privacy and anonymity were rigorously maintained to protect participants’ rights and ensure confidentiality. All procedures adhered to the principles outlined. All procedures were conducted under the ethical principles outlined in the Helsinki Declaration.
Result
Socio-demographic and economic characteristics
A total of 472 study participants were included in this study, with a response rate of 96.3%. Nearly half 248 (52.5%) of the participants were aged 24 years or younger, and the majority 383 (81.1%) resided in urban areas. In terms of religion, 199 participants (42.2%) were Orthodox Christians. Most participants 433 (91.7%) were married, while 152 (32.2%) had completed elementary education, and 315 (66.7%) were housewives (Table 1).
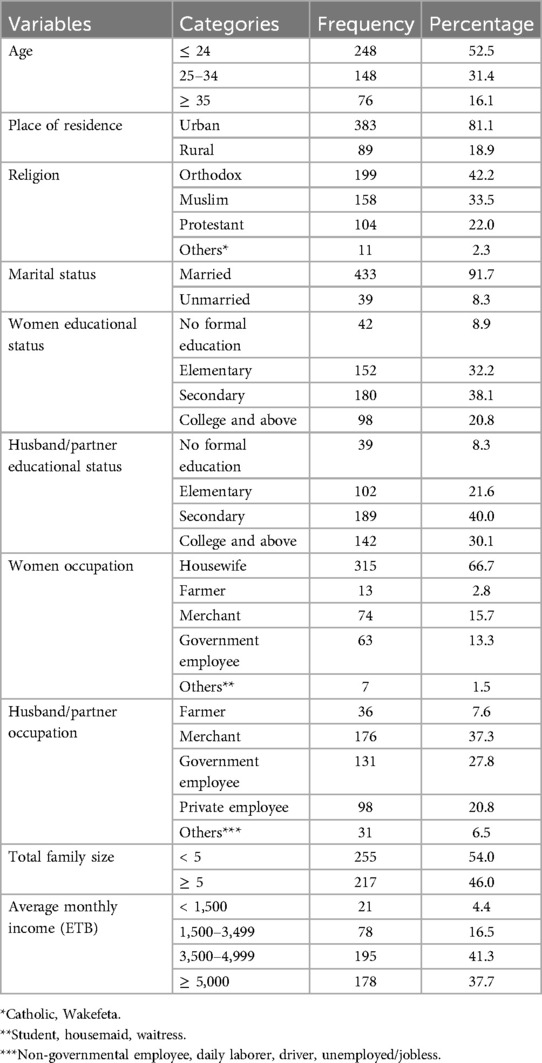
Table 1. Socio-demographic and economic characteristics of pregnant women in Adama, central Ethiopia (n = 472).
Obstetrics and health-related characteristics
In this study, 341 participants (72.2%) were multigravida, and 281 (59.5%) were multiparous. The majority, 281 (80.7%), had attended antenatal care (ANC) follow-ups. Additionally, 203 participants (43%) were in their second trimester of pregnancy, and 392 pregnancies (83.1%) were planned (Table 2).
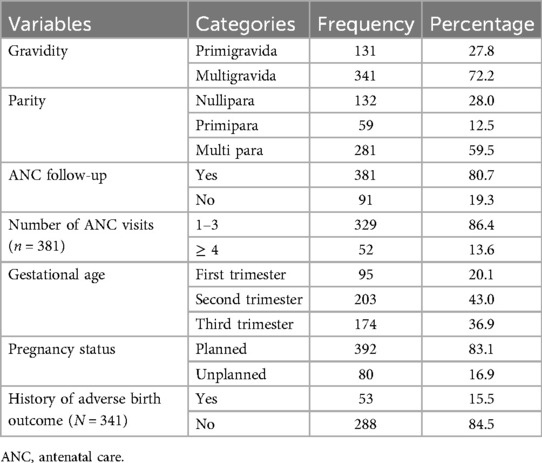
Table 2. Obstetrics and health-related characteristics of pregnant women in Adama, central Ethiopia (n = 472).
Maternal substance use and behavioral-related characteristics
In this study, the overall prevalence of substance use during pregnancy was 22.0% (95% CI: 18.2–26.0). Among the substances used during the current pregnancy, alcohol was the most common (97.1%), followed by khat (51.0%) and tobacco (33.7%). Moreover, 177 participants (47.5%) reported a history of substance use before the current pregnancy, while 296 (62.7%) stated that their husband or partner used substances (Table 3).
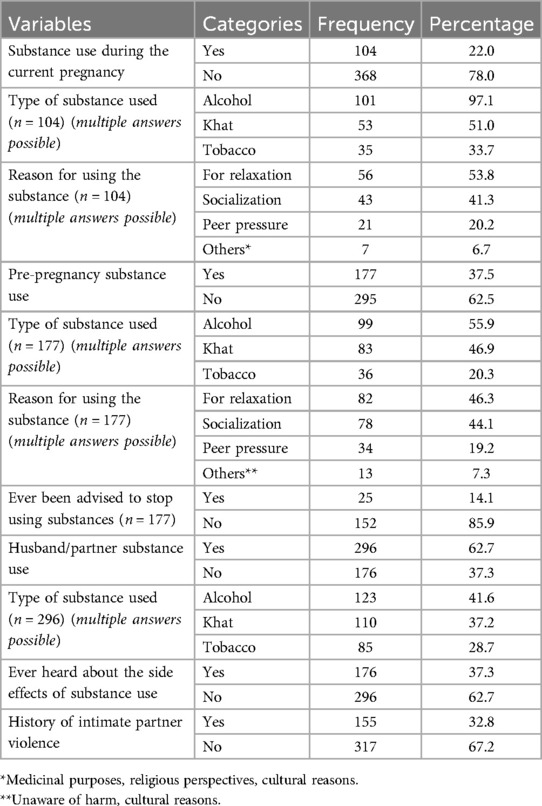
Table 3. Maternal substance use and other behavioral-related characteristics of pregnant women in Adama, central Ethiopia (n = 472).
Factors associated with substance use
In the multivariable binary logistic regression analysis, pregnancy status, pre-pregnancy substance use, husband/partner substance use, and awareness of the side effects of substance use were identified as statistically significant factors associated with substance use during pregnancy.
In this study, women with unplanned pregnancies had 3.5 times greater odds of substance use during pregnancy compared to those with planned pregnancies (AOR = 3.49, 95% CI: 1.23–9.89). The odds of substance use during pregnancy was higher among women with a history of pre-pregnancy substance use compared to their counterparts (AOR = 24.16, 95% CI: 11.49–40.82). This study also revealed that pregnant women with substance-user husbands/partners had 4.5 times higher odds of substance use during pregnancy compared to women with non-user husbands (AOR = 4.51, 95% CI: 1.44–14.20). Furthermore, women who had never heard about the side effects about the side effects of substance use had higher odds of substance use during pregnancy compared to those who were aware of the side effects (AOR = 14.60, 95% CI: 5.31–17.65) (Table 4).
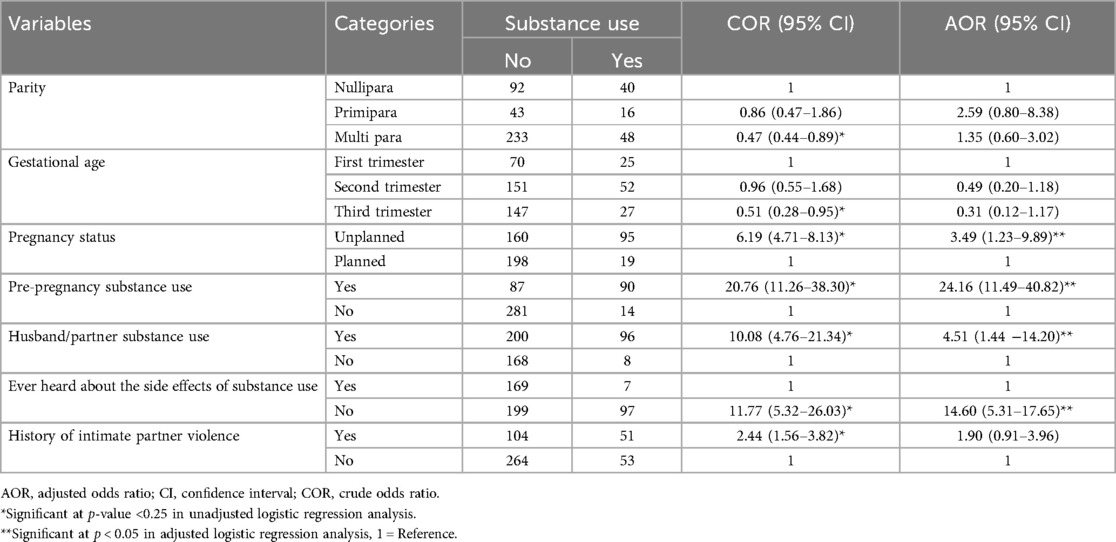
Table 4. Factors associated with maternal substance use during pregnancy pregnant women in Adama, central Ethiopia (n = 472).
Discussion
Substance abuse and dependency during pregnancy remain a pressing issue in many developing countries, including Ethiopia. This study assessed the prevalence and factors associated with maternal substance use during pregnancy in Adama, Central Ethiopia.
The prevalence of substance use among pregnant women in this study was 22.0% (95% CI: 18.2–26.0), which is comparable to a study conducted in the United States (25.8%) (31). However, the prevalence found in this study is lower than that reported in studies from Northeast Ethiopia (48.1%) (20), Eastern Ethiopia (26.5%) (23), South Central Ethiopia (60.1%) (22), Amhara, Ethiopia (38.3%) (25), and Jimma, Ethiopia (37.9%) (19). In contrast, the prevalence of substance use in this study is higher than that reported in a study from Southeast Iran (15%) (32) and the United States (33). The observed differences might be attributed to variations in cultural attitudes toward substance use, social norms, and the distribution and availability of substances. Additionally, differences in how substance use is defined and measured, as well as variations in study methodologies, sample sizes, and population characteristics, could contribute to the discrepancies in reported prevalence.
This study found that pregnant women with unplanned pregnancies had greater odds of substance use compared to those with planned pregnancies. This finding is consistent with studies conducted in Iran (32) and Northeast Ethiopia (20). A possible explanation for this is that women with unplanned pregnancies may be less likely to seek prenatal care or counseling from healthcare providers or family members. As a result, they may be more vulnerable to engaging in harmful behaviors, including the use of substances. Moreover, unplanned pregnancies often lead to emotional distress, and women may turn to substances like alcohol or drugs as a coping mechanism.
In this study, the odds of substance use during pregnancy was higher among women with a history of pre-pregnancy substance use compared to their counterparts. This finding is similar to previous studies (23, 34). This can be explained by the continuity of behaviors and the challenges associated with breaking established habits. Women who use substances before pregnancy may face difficulties in stopping due to addiction or dependency, and their established patterns of use may persist into the prenatal period.
Consistent with previous studies conducted in Iran (32) and Ethiopia (19, 20, 23), this study found that pregnant women with substance-using husbands/partners had higher odds of substance use during pregnancy compared to women with non-substance-using husbands/partners. This may be attributed to the influence of their partners’ behaviors. Substance use is often a shared activity in relationships, and women may be more likely to engage in substance use themselves if their partners also use substances. Additionally, the normalization of substance use within the household can reduce perceived risks and increase the likelihood of similar behaviors during pregnancy.
Moreover, the current study indicated that women who had never heard about the side effects of substance use had higher odds of substance use during pregnancy compared to those who were aware of the side effects. The possible justification could be that women who lack awareness of the side effects of substance use during pregnancy are more likely to engage in such behaviors due to a limited understanding of the potential risks to maternal and fetal health. Knowledge serves as a critical deterrent, as awareness of the harmful effects can motivate pregnant women to avoid substances. Without this information, they may not perceive substance use as harmful, increasing their likelihood of use during pregnancy (35, 36).
This study has some limitations. It relied on self-reported information from mothers, which introduces the possibility of recall and reporting bias. Moreover, social desirability bias may have influenced participants to respond in ways they deemed socially acceptable. The inclusion of pregnant women at various gestational ages may affect the consistency of substance use patterns throughout pregnancy. Lastly, as a cross-sectional study, it shares the inherent limitations associated with this study design.
Conclusion
This study revealed that approximately one-fifth of pregnant women reported using substances (alcohol, khat, or cigarettes) during pregnancy. Factors significantly associated with substance use during pregnancy included unplanned pregnancy, pre-pregnancy substance use, substance use by the husband/partner, and lack of awareness of its side effects. Educational and counseling interventions during antenatal care should emphasize the risks of substance use on maternal health and fetal development, particularly targeting women with a history of substance use or unplanned pregnancies. It is also important to involve husbands and partners in these efforts, as their behavior can influence the use of substances. Furthermore, community-based strategies are needed to increase overall awareness of the risks associated with substance use during pregnancy.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethical approval was obtained from the Institutional Review Board of Adama General Hospital and Medical College. A permission letter was subsequently submitted to the Adama Town Health Office and public health facilities, where approval was granted to conduct the study. Participants were fully informed about the study’s potential benefits and risks, and their voluntary participation or refusal was documented through written consent. Privacy and anonymity were rigorously maintained to protect participants’ rights and ensure confidentiality. All procedures adhered to the principles outlined. All procedures were conducted under the ethical principles outlined in the Helsinki Declaration. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KM: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. MS: Conceptualization, Writing – original draft, Writing – review & editing. YA: Writing – original draft, Writing – review & editing. NM: Writing – original draft, Writing – review & editing. YM: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgements
The authors would like to thank Adama General Hospital and Medical College for its ethical approval. Moreover, our Heartfelt appreciation also goes to the data collectors, supervisors, and all participants for their invaluable contributions to advancing knowledge in this field.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscrip.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odds ratio; ANC, antenatal care; CI, confidence intervals; COR, crude odds ratio; OR, odds ratio; SPSS, statistical package for social sciences.
References
1. CDC. Substance use - Health, United States. (2024). Available online at: https://www.cdc.gov/nchs/hus/sources-definitions/substance-use.htm (cited December 5, 2024).
2. Keane R. Understanding Substances and Substance Use: A Handbook for Teachers. Kildare: The South Western Area Health Board (2006).
3. Degenhardt L, Whiteford HA, Ferrari AJ, Baxter AJ, Charlson FJ, Hall WD, et al. Global burden of disease attributable to illicit drug use and dependence: findings from the global burden of disease study 2010. Lancet. (2013) 382(9904):1564–74. doi: 10.1016/S0140-6736(13)61530-5
4. Rehm J, Manthey J, Shield KD, Ferreira-Borges C. Trends in substance use and in the attributable burden of disease and mortality in the WHO European region, 2010–16. Eur J Public Health. (2019) 29(4):723–8. doi: 10.1093/eurpub/ckz064
5. Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. (2007) 64(5):566. doi: 10.1001/archpsyc.64.5.566
6. Forray A. Substance use during pregnancy. F1000Res. (2016) 5:887. doi: 10.12688/f1000research.7645.1
7. Abuse NI on D. Substance Use While Pregnant and Breastfeeding | National Institute on Drug Abuse (NIDA). Available online at: https://nida.nih.gov/publications/research-reports/substance-use-in-women/substance-use-while-pregnant-breastfeeding (cited 2024 December 5, 2024).
8. Latuskie KA, Andrews NCZ, Motz M, Leibson T, Austin Z, Ito S, et al. Reasons for substance use continuation and discontinuation during pregnancy: a qualitative study. Women Birth. (2019) 32(1):e57–64. doi: 10.1016/j.wombi.2018.04.001
9. Behnke M, Smith VC, Committee on Substance Abuse, Committee on Fetus and Newborn, Behnke M, Smith VC, et al. Prenatal substance abuse: short- and long-term effects on the exposed Fetus. Pediatrics. (2013) 131(3):e1009–24. doi: 10.1542/peds.2012-3931
10. Bayih WA, Belay DM, Ayalew MY, Tassew MA, Chanie ES, Feleke DG, et al. The effect of substance use during pregnancy on neonatal outcomes in Ethiopia: a systematic review and meta-analysis. Heliyon. (2021) 7(4):e06740. doi: 10.1016/j.heliyon.2021.e06740
11. Ordean A, Graves L, Chisamore B, Greaves L, Dunlop A. Prevalence and consequences of perinatal substance use—growing worldwide concerns. Subst Abus. (2017) 11:1178221817704692.
12. Hacker M, Firk C, Konrad K, Paschke K, Neulen J, Herpertz-Dahlmann B, et al. Pregnancy complications, substance abuse, and prenatal care predict birthweight in adolescent mothers. Arch Public Health. (2021) 79(1):137. doi: 10.1186/s13690-021-00642-z
13. Rodriguez JJ, Smith VC. Epidemiology of perinatal substance use: exploring trends in maternal substance use. Semin Fetal Neonatal Med. (2019) 24(2):86–9. doi: 10.1016/j.siny.2019.01.006
14. Suntai Z. Substance use among women who are pregnant: examining treatment completion by race and ethnicity. J Subst Abuse Treat. (2021) 131:108437. doi: 10.1016/j.jsat.2021.108437
15. Popova S, Lange S, Probst C, Shield K, Kraicer-Melamed H, Ferreira-Borges C, et al. Actual and predicted prevalence of alcohol consumption during pregnancy in the WHO African region. Tropical Med Int Health. (2016) 21(10):1209–39. doi: 10.1111/tmi.12755
16. Addila AE, Bisetegn TA, Gete YK, Mengistu MY, Beyene GM. Alcohol consumption and its associated factors among pregnant women in Sub-Saharan Africa: a systematic review and meta-analysis’ as given in the submission system. Subst Abuse Treat Prev Policy. (2020) 15(1):29. doi: 10.1186/s13011-020-00269-3
17. Petersen Williams P, Jordaan E, Mathews C, Lombard C, Parry CDH. Alcohol and other drug use during pregnancy among women attending midwife obstetric units in the cape metropole, South Africa. Adv Prev Med. (2014) 2014:1–10. doi: 10.1155/2014/871427
18. Dargie A, Eshetie Y, Asmare Y, Shibabaw W, Dagne K. Prevalence of alcohol use during pregnancy and its association with partner alcohol use in east Africa: systematic review and meta-analysis. bioRxiv. (2019). Available online at: http://biorxiv.org/lookup/doi/10.1101/687467 (cited December 5, 2024).
19. Tesso FY, Woldesemayat L, Kebede DB. Magnitude of substance use and associated factors among pregnant women attending Jimma town public health facilities, Jimma zone, Oromia regional state southwest Ethiopia. Clinics Mother Child Health. (2017) 14(275):2.
20. Aychiluhm SB, Haji A, Abdulkadir O, Mare KU, Duko B, Dachew BA, et al. Determinants of maternal substance use during pregnancy among the pastoral community, northeast Ethiopia: Bayesian analysis approach. Cogent Public Health. (2023) 10(1):2205712. doi: 10.1080/27707571.2023.2205712
21. Addis N, Azage M, Nigatu D, Kirksey K. Alcohol use and its associated factors during pregnancy in Ethiopia: a population-based survey. (2020). Available online at: https://www.researchsquare.com/article/rs-52915/v1 (Accessed December 04, 2024).
22. Alamneh AA, Endris BS, Gebreyesus SH. Caffeine, alcohol, khat, and tobacco use during pregnancy in butajira, south central Ethiopia. PLoS One. (2020) 15(5):e0232712. doi: 10.1371/journal.pone.0232712
23. Fetene MT, Teji K, Assefa N, Bayih WA, Tsehaye G, Hailemeskel HS. Magnitude and associated factors of substance use among pregnant women attending antenatal care in public hospitals of eastern Ethiopia. BMC Psychiatry. (2021) 21(1):96. doi: 10.1186/s12888-021-03078-5
24. Onwuka CI. Prevalence and predictors of alcohol consumption during pregnancy in south-eastern Nigeria. JCDR. (2016). Available online at: http://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2016&volume=10&issue=9&page=QC10&issn=0973-709x&id=8449 (cited December 6, 2024).27790525
25. Seid J, Mohammed E, Muktar Y. Factors associated with perinatal substance use among Ethiopian women: an institutional-based cross-sectional study. Adv Drug Alcohol Res. (2023) 3:11913. doi: 10.3389/adar.2023.11913
26. World Health Organization. Guidelines for the Identification and Management of Substance use and Substance use Disorders in Pregnancy. Geneva: World Health Organization (WHO) (2014).
27. Thomas S, Treffers R, Berglas NF, Drabble L, Roberts SCM. Drug use during pregnancy policies in the United States from 1970 to 2016. Contemp Drug Probl. (2018) 45(4):441–59. doi: 10.1177/0091450918790790
28. Population Census Commission. The 2007 Population and Housing Census of Ethiopia. Addis Ababa: Central Statistical Agency (CSA) of Ethiopia (2010).
29. Nakajima M, Jebena MG, Taha M, Tesfaye M, Gudina E, Lemieux A, et al. Correlates of khat use during pregnancy: a cross-sectional study. Addict Behav. (2017) 73:178–84. doi: 10.1016/j.addbeh.2017.05.008
30. Shanmugam PK. The influence of social factors in drug addiction–A mini review of work by Miller & Carroll (2006). J Alcohol Drug Depend. (2017) 05(04). doi: 10.4172/2329-6488.1000272
31. Havens JR, Simmons LA, Shannon LM, Hansen WF. Factors associated with substance use during pregnancy: results from a national sample. Drug Alcohol Depend. (2009) 99(1–3):89–95. doi: 10.1016/j.drugalcdep.2008.07.010
32. Tabatabaei SM, Behmanesh-Pour F, Salimi-Khorashad A, Zaboli M, Sargazi-Moakhar Z, Shaare-Mollashahi S. Substance abuse and its associated factors among pregnant women: a cross-sectional study in the southeast of Iran. Addict Health. (2018) 10(3):162–72. doi: 10.22122/ahj.v10i3.209
33. Nidey N, Kair LR, Wilder C, Froehlich TE, Weber S, Folger A, et al. Substance use and utilization of prenatal and postpartum care. J Addict Med. (2022) 16(1):84–92. doi: 10.1097/ADM.0000000000000843
34. Floyd RL, Jack BW, Cefalo R, Atrash H, Mahoney J, Herron A, et al. The clinical content of preconception care: alcohol, tobacco, and illicit drug exposures. Am J Obstet Gynecol. (2008) 199(6):S333–9. doi: 10.1016/j.ajog.2008.09.018
35. Escañuela Sánchez T, Matvienko-Sikar K, Linehan L, O’Donoghue K, Byrne M, Meaney S. Facilitators and barriers to substance-free pregnancies in high-income countries: a meta-synthesis of qualitative research. Women Birth. (2022) 35(2):e99–110. doi: 10.1016/j.wombi.2021.04.010
Keywords: Ethiopia, maternal substance use, pregnancy, public health, Adama
Citation: Mohammed K, Shawel Getahun M, Abera Belachwe Y, Mohammed Fati N and Mekuria Negussie Y (2025) Maternal substance use during pregnancy and associated factors in Adama, central Ethiopia. Front. Glob. Women's Health 6:1540814. doi: 10.3389/fgwh.2025.1540814
Received: 6 December 2024; Accepted: 14 February 2025;
Published: 27 February 2025.
Edited by:
Anna Maria Lavezzi, University of Milan, ItalyReviewed by:
Projestine Selestine Muganyizi, University of Dar es Salaam, TanzaniaYimer Muktar, Woldia University, Ethiopia
Copyright: © 2025 Mohammed, Shawel Getahun, Abera Belachwe, Mohammed Fati and Mekuria Negussie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yohannes Mekuria Negussie, eW9oYW5uZXNfbWVrdXJpYUB5YWhvby5jb20=
†ORCID:
Yohannes Mekuria Negussie
orcid.org/0000-0002-1332-670X
 Kimiya Mohammed1
Kimiya Mohammed1 Mihiret Shawel Getahun
Mihiret Shawel Getahun Yohanes Abera Belachwe
Yohanes Abera Belachwe Yohannes Mekuria Negussie
Yohannes Mekuria Negussie