
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Glob. Womens Health, 01 April 2025
Sec. Contraception and Family Planning
Volume 6 - 2025 | https://doi.org/10.3389/fgwh.2025.1510299
This article is part of the Research TopicCurrent Advances in Contraceptive Use, Technology, and PromotionView all 11 articles
 Yohanes Abera Belachwe1*†
Yohanes Abera Belachwe1*† Midekso Sento2
Midekso Sento2 Melese Negash Gobena3
Melese Negash Gobena3 Mihiret Shawel Getahun4
Mihiret Shawel Getahun4 Yohannes Mekuria Negussie5*†
Yohannes Mekuria Negussie5*†
Background: The World Health Organization advocates dual contraceptive methods for women with Human Immunodeficiency Virus (HIV) to prevent unintended pregnancies and sexually transmitted infections (STIs), enhancing education, economic opportunities, and maternal-child health outcomes. However, persistent global challenges stem from inadequate use of dual contraceptives and unsafe sexual practices, resulting in high rates of unintended pregnancies and significant health risks. Hence, this study aimed to assess dual contraceptive use among women living with HIV on anti-retroviral therapy (ART) in Boset District, Ethiopia.
Method: A facility-based cross-sectional study was conducted among 342 women living with HIV from September 12 to October 18, 2023. Participants were selected by systematic random sampling, and data were collected using an interviewer-administered structured questionnaire. The collected data were entered using Epi Info version 7.2.6 and analyzed using SPSS version 26.0. Bivariable and multivariable binary logistic regression analyses were performed to assess the association between the outcome and explanatory variables. In the multivariable analysis, an adjusted odds ratio (AOR) with a 95% confidence interval (CI) was used to show the strength of the association, and the level of significance was set at a p-value of <0.05.
Results: The magnitude of dual contraceptive use was 33.7% (95% CI: 28–40). Urban residence (AOR = 2.5; 95% CI: 1.97–8.08), good knowledge about dual contraceptives (AOR = 3.8; 95% CI: 2.36–8.67), STIs history in the past 12 months (AOR = 2.6, 95% CI: 1.25–4.72) and having two or more number of sexual partners, (AOR = 1.9; 95% CI: 1.18–6.68), were factors significantly associated with dual contraceptive use.
Conclusion: One-third of women living with HIV on ART utilized dual contraceptives. Place of residence, knowledge about dual contraceptives, history of STIs in the past 12 months, and number of sexual partners were factors associated with dual contraceptive use. It is essential to implement focused educational programs to increase knowledge about dual contraceptives, alongside expanding access to contraceptive services in rural and underserved areas.
Dual contraceptive utilization involves using a barrier contraceptive to lower the risk of transmitting sexually transmitted infections (STIs) alongside another effective birth control method to prevent unplanned pregnancies (1, 2). The World Health Organization (WHO) advocates for women living with HIV (WLHIV) to employ dual contraceptive methods to prevent unintended pregnancies and STIs (3). Rising rates of STIs are more common in women with HIV than in those without HIV (4). Studies show that unintended pregnancy often happens when individuals engage in sexual intercourse without using contraception, use contraception improperly, or face contraceptive failure despite using it correctly (5).
For women and girls with HIV, using dual contraceptives correctly and consistently leads to better education and economic opportunities, helping to achieve gender equality, empower women, and reduce poverty. It also improves infant and child health by preventing illness and death from unintended pregnancies and STIs, including HIV. This allows for safer, planned pregnancies, benefiting both maternal and child health (6, 7).
Poor utilization of dual contraceptives not only increases the incidence of unplanned pregnancies but also contributes to the spread of HIV/AIDS and other STIs (2, 8). Globally, inadequate use of dual contraceptives and unsafe sexual practices result in over 2 million HIV-infected women becoming pregnant annually, leading to over half a million deaths from pregnancy-related complications (3, 9). Women living with the Human Immunodeficiency Virus often experience unintended pregnancies because women either use ineffective birth control, inadequate education, sexual violence, contraceptive failure, or lack access to family planning services (10). Evidence also suggests that a majority of unintended pregnancies result in unsafe abortion (2).
Studies conducted in different settings indicated that the prevalence of dual contraceptive utilization among WLHIV was 10.7% in Swiss (11), 29.6% in Thailand (3), 27% in Atlanta Georgia (12), 27% in Brazil (13), 32% in Nigeria (14), 33.3% in Cameroon (15), 38.5% in Kenya (16) and 40% in Rwanda (17).
In Ethiopia, the pooled prevalence of dual contraception use among WLHIV was 34.08% (18). The highest proportion of dual contraceptive methods was reported in Bishoftu town which accounts for 56.9% (19). Other studies have found that the prevalence of dual contraceptive utilization among WLHIV was 13.2% in the University of Gondar Hospital (20), 15.7% in Mekelle town (21) 19.4% in Borana district (22), 19.8% in Gebretsadik Shawo Hospital (23), 21.4% in West Shewa Zone (24), 30% in Gimbie town (25).
Previous studies have indicated that factors such as age, marital status, place of residence, educational status, occupational status, having children, fertility desire, counseling on family planning, family support, discussion with a partner, number of sexual partners, disclosure of HIV status, Clusters of differentiation (CD4) cell count were significantly associated with dual contraceptive method utilization (2, 23, 26–28).
Despite several studies on dual contraceptive use among WLHIV in Ethiopia, there remains a limited body of evidence specific to the study setting. Given the regional and contextual differences in healthcare access, contraceptive utilization, and socio-cultural factors, this may limit the direct generalizability of previous findings. Therefore, this study aimed to provide valuable insights by examining the magnitude and factors associated with dual contraceptive use among WLHIV on antiretroviral therapy in Boset District, Ethiopia. The findings will contribute to locally tailored interventions to prevent unintended pregnancies and the transmission of STIs/HIV. Furthermore, the results will bolster planning and decision-making capacities, facilitating collaborative efforts with relevant stakeholders to identify and implement effective solutions to address these issues in the study setting.
A facility-based cross-sectional study was conducted in the Boset district, central Ethiopia, from September 12 to October 18, 2023. The Boset district is bounded by the Amhara Regional State to the north, Adama Woreda to the west, the Arsi Zone to the south, and Fentale Woreda to the east. The district is comprised of 5 urban and 37 rural kebeles, situated approximately 125 km from Addis Ababa, the capital of Ethiopia. It has a total population of 220,362, of which 112,385 are females (29). The district's healthcare infrastructure includes one hospital, seven health centers, and 30 private clinics. However, only three public health facilities (two health centers and one hospital) provide HIV care and treatment services. A total of 1,610 women were registered as receiving antiretroviral therapy (ART), of whom 764 were women of reproductive age: 206 at Olenchite Hospital, 454 at Olenchite Health Center, and 104 at Bole Health Center.
All WLHIV who were on ART follow-up in Boset district public health facilities were the source population, while all randomly selected WLHIV who were receiving ART during the study period constituted the study population. The study included women of reproductive age attending ART care services who had attended at least one visit before the study commenced. However, women who were critically ill, unable to communicate, or experiencing mental health issues were excluded. Additionally, women with medical conditions contraindicating the use of contraceptives or other conditions identified based on WHO medical eligibility criteria were excluded to ensure the appropriateness and safety of contraceptive use among participants.
A single population proportion formula was used to calculate the sample size with an assumption of 28.8% of the population proportion of dual method of contraceptive use (p) from a previous study done in Gonder City (30), 95% confidence level, 5% margin of error and a 10% non-response rate.
Where; n: Sample size; Z: Confidence coefficient; d: Margin of error (0.05); P: estimation of dual method of contraceptive use rate.
After adding 10% contingency for non-response the final sample size of the study becomes 347.
The study included all three public health facilities providing HIV care and treatment services in the Boset district. The calculated sample size was proportionally allocated to each of these facilities based on the average number of women on ART in the previous three months. Study participants were selected from each chosen health facility using systematic random sampling. The sampling interval at each facility was determined by dividing the average number of women on ART over the previous three months by the required sample size. Thus, the calculated k-value becomes two. The index participant was then chosen at random from 1 to 2 in each hospital. Accordingly, every second participant was chosen using a systematic random sampling technique until the required sample size was reached (Figure 1).
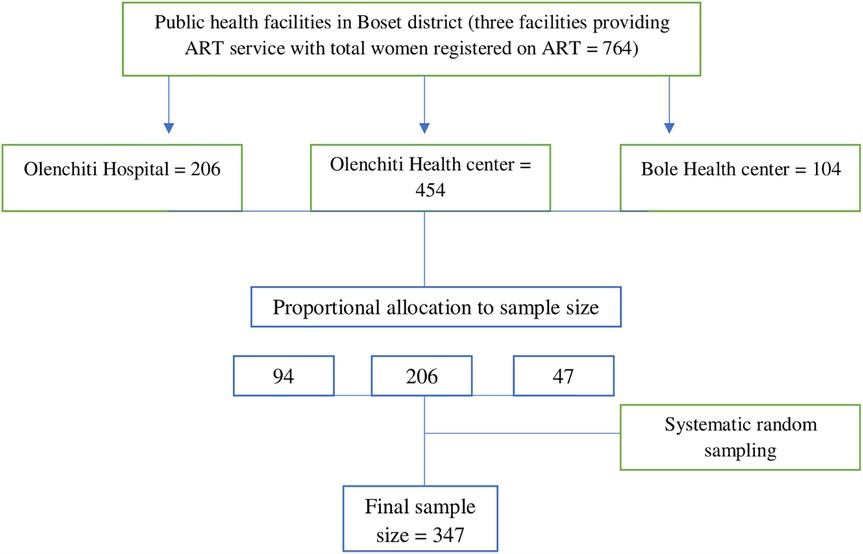
Figure 1. Schematic presentation of sampling procedure to assess dual contraceptive use among women living with HIV on anti-retroviral therapy in Boset District, Ethiopia, 2023.
Before data collection, eligibility criteria were established to determine the eligibility of WLHIV attending the ART clinic for participation. Once eligible participants were identified, they were assigned sequential numbers based on their arrival order. Participants were then selected at regular intervals (K). To prevent multiple enrollments of the same person, a mark was placed on their medical record.
Dependent variable
Dual contraceptive use (yes/no).
Independent variables:
Socio-demographic factors: age, place of residence, religion marital status, ethnicity, Women's educational status, spouse educational status, women occupation. Spouse occupation, and average monthly income.
Sexual and reproductive health characteristics: number of children, women's desire to have more children, partner's desire to have more children, ever used any contraceptive method since being HIV-positive, pregnancy since HIV positive, and knowledge about dual contraceptives.
Clinical and HIV-related characteristics: STI history in the past 12 months, number of sexual partners, knowing the HIV status of the partner, disclosed HIV status to partner, perceived disclosure of HIV status to a sexual partner is important, Duration on ART, current CD4 cell count, and Current viral load.
Dual contraceptive utilization: The concurrent use of two methods of contraception during sexual encounters in the 12 months preceding the study: a barrier method (male/female condom) and other highly effective modern contraceptive methods (such as the IUCD, contraceptive implants, injections, and pills) (19, 27, 30, 31).
Knowledge of dual contraceptives: In this study, the aggregate of eight dichotomized questions assessed knowledge about contraceptive methods. A score of 0 indicated an incorrect answer, while a score of 1 indicated a correct answer. Women who scored at or above the mean were classified as having good knowledge, while those scoring below the mean were classified as having poor knowledge (27).
Data were collected using a pretested, structured, interviewer-administered questionnaire and medical record review. The questionnaires were adapted from various relevant literature with necessary modifications tailored to the specific context of the study (2, 16, 19, 24, 27, 30, 32). A data abstraction format was used to gather the required information from patients' records. A team of six trained midwives conducted the data collection, while two public health officers served as supervisors during the process.
Data were collected using a pretested, self-structured, interviewer-administered questionnaire and medical record review. The questionnaire was adapted from various relevant literature with necessary modifications tailored to the specific context of the study (2, 16, 19, 24, 27, 30, 32). A data abstraction format was used to gather the required information from patients’ records. A team of six trained midwives conducted the data collection, while two public health officers served as supervisors during the process. The questionnaire has been included as Supplementary Material for reference.
The questionnaire was first written in English, then translated into Afan Oromo, and finally back into English to check for consistency. To ensure the questionnaire and data collection methods matched the study's objectives, a pre-test was conducted with 5% of the total patient sample. Data collectors and supervisors were trained for two days on research ethics, data collection tools, and procedures to ensure high-quality data. During the data collection phase, ongoing supervision of data collectors occurred, and regular meetings were held involving data collectors, supervisors, and investigators. Participants were interviewed in private places to ensure their privacy and confidentiality as well as to encourage participation. Before data entry, collected data underwent review and checks to ensure completeness.
Following the coding and inputting of data into Epi Info version 7.2.6, the data were exported to the Statistical Package for Social Sciences (SPSS) version 26 for cleaning and analysis. Descriptive statistics including frequency, percentage, mean, and standard deviation were used to present key characteristics of the study population. The association between independent variables and dual contraceptive use was modeled using binary logistic regression analysis. In the bivariable logistic regression model, a significance level of 0.25 was set as a threshold to select variables for multivariable logistic regression analysis, aiming to control for confounding effects. The existence of multicollinearity among explanatory variables was assessed using the variance inflation factor (VIF). In this study, the mean VIF was 1.3, indicating that there was no multicollinearity. The model was fitted using the standard model-building approach. Hosmer and Lemeshow's goodness-of-fit test was used to assess the model's fitness. The diagnostic result indicated the model fit the data well (p = 0.86). In the multivariable logistic regression analysis, the adjusted odds ratio (AOR) with a 95% confidence interval (CI) was utilized to determine predictors of dual contraceptive use. At this level, variables with a p-value less than 0.05 were deemed statistically significant.
Among the 347 sampled respondents, 342 completed the interview, yielding a response rate of 98.6%. The mean age of the participants was 33.52 (±5.16) years. One hundred five (30.7%) of the participants were in the age group of 30-34, and the majority, 212 (62% were urban residents. About 33.6% of women were able to read and write, and 156 (45.6%) were housewives (Table 1).
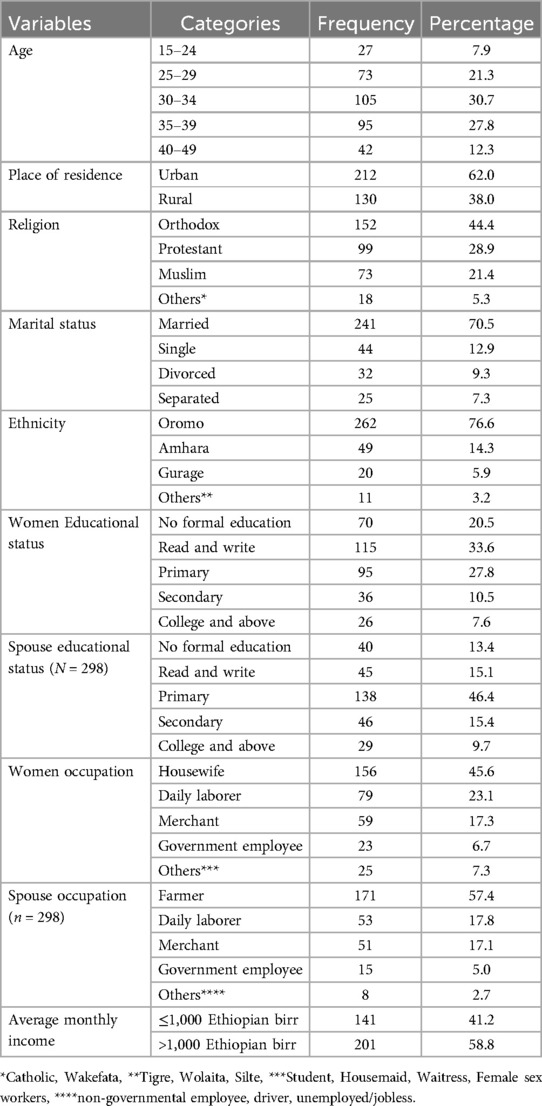
Table 1. Socio-demographic characteristics of women living with HIV receiving anti-retroviral therapy at public health facilities in boset district, Ethiopia, 2023 (n = 342).
In this study, 159 respondents (46.5%) reported having 1–2 children, while approximately two-thirds of the participants (217, 63.5%) expressed a desire to have more children. Among the respondents, 216 individuals (63.2%) had used some form of contraception since testing positive for HIV. Additionally, 173 participants (51.0%) demonstrated good knowledge of dual contraceptive methods (Table 2).
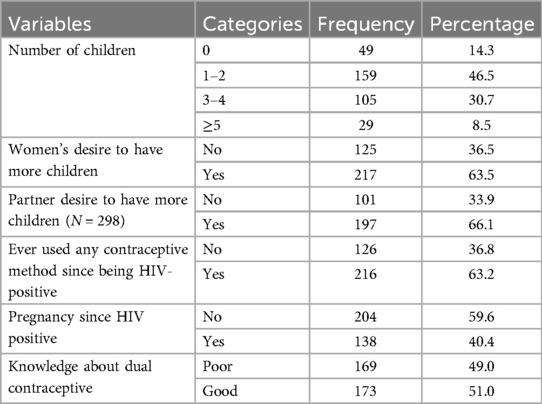
Table 2. Sexual and reproductive health-related characteristics of women living with HIV receiving anti-retroviral therapy at public health facilities in boset district, Ethiopia, 2023 (n = 342).
Out of all participants, only 53 (15.5%) reported having a history of other STIs in the past year, and the majority, 299 (87.4%), had single sexual partners. About 221 (74.2%) disclosed their HIV status to their partner (Table 3).
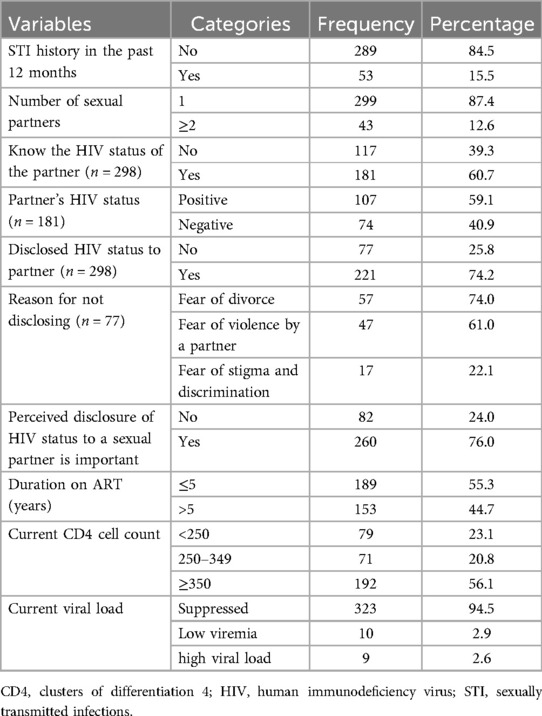
Table 3. Clinical and HIV related characteristics among women living with HIV receiving anti-retroviral therapy at public health facilities in boset district, Ethiopia, 2023(n = 342).
The utilization of dual contraceptives among women living with HIV who are receiving antiretroviral therapy at public health facilities in the Boset district was found to be 33.7% (95% CI: 28–40). Among those who used dual contraceptives, the majority used condoms plus implants (54.9%), followed by condoms plus injectables (20.7%).
Place of residence, women's desire to have more children, knowledge about dual contraceptives, STI history in the past 12 months, number of sexual partners, perceived disclosure of HIV to a sexual partner, and current CD4 cell count were the variables that fulfilled the criteria P < 0.25 and transferred to multivariable analysis. After adjusting for confounding variables in the multivariable analysis, place of residence, knowledge about dual contraceptives, STI history in the past 12 months, and the number of sexual partners were found to be statistically significant factors associated with dual contraceptive utilization.
Accordingly, the odds of dual contraceptive use were 2.5 times greater among urban residents compared with rural residents (AOR = 2.5, 95% CI: 1.97–8.08). Compared to women with poor knowledge of dual contraceptives those with good knowledge of dual contraceptives had nearly 4-fold higher odds of dual contraceptive utilization (AOR = 3.8, 95% CI: 2.36–8.67). Women who had a history of STIs in the past 12 months had 2.6 times higher (AOR = 2.6, 95% CI: 1.25–4.72) odds of dual contraceptive use than their counterparts. Moreover, the odds of dual contraceptive utilization were about twice as high among women with two or more sexual partners compared to those with a single sexual partner (AOR = 1.9, 95% CI: 1.18–6.68) (Table 4).
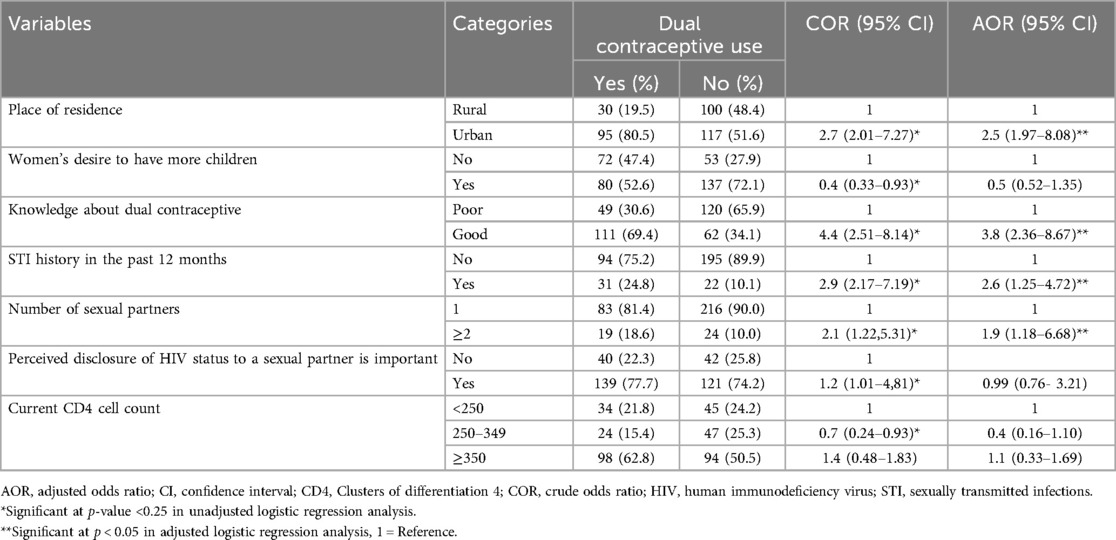
Table 4. Factors associated with dual contraceptive utilization among women living with HIV receiving anti-retroviral therapy at public health facilities in boset district, Ethiopia, 2023.
This study revealed that the magnitude of dual contraceptive use was 33.7% (95% CI: 28–40), knowledge about dual contraceptives, STI history in the past 12 months, and number of sexual partners, were factors significantly associated with dual contraceptive use.
The current study revealed that the magnitude of dual contraceptive use was 33.7% (95% CI: 28–40). This finding is comparable to results from studies conducted in Thailand (29.6%), India (30%) (33), South Africa (33%) (34), Bungoma City, Kenya (38.5%) (16), Wolaita Zone, Southern Ethiopia (28.6%) (27), Hossana Hospital, Ethiopia (28.3%) (35), Gondar City, Northwest Ethiopia (28.8%) (30), Gimbie Town, Ethiopia (30%) (25), and Fitche Hospital, Ethiopia (32%) (26). However, it was higher than studies conducted in Switzerland (10.7%) (11), Zambia (17.7%), South Africa (6.8%), Mekelle, Ethiopia (15.7%) (21), Addis Ababa, Ethiopia (14.7%), West Showa Zone, Ethiopia (21.4%) (24), Gebretsadik Shawo Hospital, SNNPR, South West Ethiopia (19.8%) (23), Finote-Selam Hospital, Northwest Ethiopia (21.8%) (36), and Gondar Hospital, Ethiopia (13.2%) (20). The higher dual contraceptive use in this study compared to previous findings may be due to enhanced integration of family planning with HIV services, improved healthcare access, and increased awareness of dual protection. Differences in study periods, sample characteristics, and regional variations in contraceptive uptake could also explain the discrepancy.
Moreover, the use of dual contraceptives in this study was lower than in studies done in Brazil (72%) (37), Mumbai India (69%) (38), Bahirdar town, Ethiopia (64.2%) (28), and Bishoftu town, Ethiopia (56.9%) (19). This discrepancy may be attributed to variations in the sociodemographic and cultural characteristics of the study participants. Furthermore, inconsistencies between studies might arise from differences in sample size, study period, and the settings in which the studies were conducted.
Urban women had higher odds of using dual contraceptives compared to their rural counterparts. This finding is supported by studies conducted in Finote-Selam Hospital, Northwest Ethiopia (36), Hossana, Southern Ethiopia (32), Gondar City, Northwest Ethiopia (30), and West Showa Zone, Ethiopia (24). This could be attributed to disparities in access to information and contraceptive services. Urban residents have greater exposure to information and technologies related to contraceptives, which may facilitate their effective use. Furthermore, urban women are thought to have easier access to contraceptive methods (39).
Women with good knowledge of dual contraceptive methods had higher odds of using dual contraception compared to those with poor knowledge. This is in line with a study undertaken in Bungoma City, Kenya (16). Increased awareness and understanding of these methods likely empower women to make informed choices about their contraceptive practices, thereby enhancing their likelihood of use (40).
This study also revealed that the odds of dual contraceptive use were greater among women with a history of STI. This finding aligns with a study conducted in Wolaita zone, Southern Ethiopia (27). This may be attributed to increased risk awareness among women with a history of STIs, which motivates them to adopt dual contraceptive methods for comprehensive protection against both STIs and unintended pregnancies (41, 42).
Moreover, women who had multiple sexual partners had increased odds of using dual contraceptives compared to their counterparts. This finding is consistent with a study done in Hossana, Southern Ethiopia (32). This can be justified by the heightened awareness and perceived risk of STIs and unintended pregnancies among women with multiple partners. The need for additional protection against both STIs and pregnancy likely motivates these women to adopt dual contraceptive methods to ensure comprehensive protection (43). Conversely, findings from Finote-Selam Hospital, Northwest Ethiopia, showed that women with multiple sexual partners had lower odds of dual contraceptive utilization (36).
The findings of this study have important public health implications. The moderate level of dual contraceptive use indicates the need for intensified efforts to promote dual protection among WLHIV. Health education programs should emphasize the benefits of dual contraceptive use, particularly in rural areas, where access remains limited. Integrating reproductive health services with ART programs can enhance access to contraceptive counseling and increase uptake. Moreover, healthcare providers should leverage STI treatment visits as opportunities for reinforcing dual protection messages.
Being a cross-sectional study prevented the establishment of causal relationships between variables. Additionally, because it was conducted in health facilities, the findings may not apply to HIV-positive women outside the study area or those who do not access healthcare. The study also lacked qualitative data and did not include perspectives from sexual partners, limiting its depth. Furthermore, recall bias may have affected the accuracy of participants' reports on past contraceptive use or STI history. Social desirability bias could also be a concern, as some participants might have provided responses, they deemed socially acceptable rather than truthful.
In this study, one-third of WLHIV on ART utilized dual contraceptives. Factors such as place of residence, knowledge about dual contraceptives, history of STIs in the past 12 months, and number of sexual partners were identified as statistically significant factors associated with dual contraceptive use. The findings suggest the need for targeted educational programs to enhance awareness and knowledge about dual contraceptives, especially in rural areas, and expanding access to contraceptive services in rural and underserved areas are crucial steps forward.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethical approval was obtained from the Institutional Ethical Review Board of Adama General Hospital Medical College. The study's proposal was formally presented to both the Oromia Regional Health Office and the Boset district Health Office to secure official approval for carrying out the study. The data was collected after getting official permission from the Boset district health office administration. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
YAB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MS: Writing – original draft, Writing – review & editing. MNG: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. MSG: Writing – original draft, Writing – review & editing. YMN: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research and/or publication of this article.
The authors extend their sincere appreciation to Adam General Hospital and Medical College, along with the Boset district health office, for their invaluable assistance throughout the study. Special thanks are also extended to the dedicated team of data collectors, supervisors, and all the study participants for their crucial contributions.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2025.1510299/full#supplementary-material
AIDS, acquired immunodeficiency syndrome; AOR, adjusted odds ratio; ART, antiretroviral therapy; CD4, cluster of differentiation; CI, confidence interval; COR, crude odds Ratio; HIV, human immunodeficiency virus; STIs, sexually transmitted diseases; WLHIV, women living with human immunodeficiency virus.
1. Wilson TE, Koenig LJ, Walter E, Fernandez I, Ethier K. Dual contraceptive method use for pregnancy and disease prevention among HIV-infected and HIV-uninfected women: the importance of an event-level focus for promoting safer sexual behaviors. Sex Transm Dis. (2003) 30(11):809–12.14603086
2. Mesfin Y, Argaw M, Geze S, Tefera B. Dual contraceptive use and factor associated with people living with HIV/AIDS: a systematic review and meta-analysis. Infect Dis Obstet Gynecol. (2021) 2021:5440722.34434041
3. Munsakul W, Lolekha R, Kowadisaiburana B, Roongpisuthipong A, Jirajariyavej S, Asavapiriyanont S, et al. Dual contraceptive method use and pregnancy intention among people living with HIV receiving HIV care at six hospitals in Thailand. Reprod Health. (2015) 13(1):8. doi: 10.1186/s12978-016-0123-2
4. Muyindike W, Fatch R, Steinfield R, Matthews LT, Musinguzi N, Emenyonu NI, et al. Contraceptive use and associated factors among women enrolling into HIV care in Southwestern Uganda. Infect Dis Obstet Gynecol. (2012) 2012:1–9. doi: 10.1155/2012/340782
5. Oulman E, Kim THM, Yunis K, Tamim H. Prevalence and predictors of unintended pregnancy among women: an analysis of the Canadian maternity experiences survey. BMC Pregnancy Childbirth. (2015) 15(1):260. doi: 10.1186/s12884-015-0663-4
6. Pillai VK, Teboh C. A decade of contraceptive use in Cameroon: influences of structural changes. Open Access J Contracept. (2010) 2:5–11.
7. Joshi B, Girase B, Shetty S, Verma V, Acharya S, Deoraj P, et al. Improving public health service delivery response to address contraceptive needs of socio-economically disadvantaged HIV positive people in Maharashtra, India. Contracept Reproduct Med. (2021) 6:1–11.
8. McCoy SI, Buzdugan R, Ralph LJ, Mushavi A, Mahomva A, Hakobyan A, et al. Unmet need for family planning, contraceptive failure, and unintended pregnancy among HIV-infected and HIV-uninfected women in Zimbabwe. PLoS One. (2014) 9(8):e105320.25144229
9. Renzaho JN, Rutayisire E. Dual contraceptive use and associated factors among women aged 15–49 years on antiretroviral therapy in Kayonza district, Rwanda: a cross-sectional study. Pan Afr Med J. (2022) 42:1–14.
10. Osuafor GN, Maputle SM. Dual protection and contraceptive method use among women in heterosexual relationships in Mahikeng, South Africa. Afr J Reprod Health. (2017) 21(1):64–72. doi: 10.29063/ajrh2017/v21i1.5
11. Aebi-Popp K, Mercanti V, Voide C, Nemeth J, Cusini A, Jakopp B, et al. Neglect of attention to reproductive health in women with HIV infection: contraceptive use and unintended pregnancies in the Swiss HIV cohort study. HIV Med. (2018) 19(5):339–46. doi: 10.1111/hiv.12582
12. Haddad LB, Brown JL, King C, Gause NK, Cordes S, Chakraborty R, et al. Contraceptive, condom and dual method use at last coitus among perinatally and horizontally HIV-infected young women in Atlanta, Georgia. Mitchell C, editor. PLoS One. (2018) 13(9):e0202946.30208062
13. Tsuyuki K, Gipson JD, Urada LA, Barbosa RM, Morisky DE. Dual protection to address the global syndemic of HIV and unintended pregnancy in Brazil. J Fam Plann Reprod Health Care. (2016) 42(4):271–9.26880759
14. Lawani LO, Onyebuchi AK, Iyoke CA. Dual method use for protection of pregnancy and disease prevention among HIV-infected women in South East Nigeria. BMC Women’s Health. (2014) 14(1):39.
15. Tsafack M, Essiben F, Momo RJ, Moyo GPK, Mpoah YM, Mbu RE. Dual contraception use and associated factors among HIV positive women follow-up at treatment center unit of Yaounde Central Hospital, Cameroon. OALib. (2020) 07(05):1–12.
16. Mulongo AM, Lihana RW, Githuku J, Gura Z, Karanja S. Factors associated with uptake of dual contraception among HIV-infected women in Bungoma county, Kenya: a cross-sectional study. Pan Afr Med J. (2017) 28(Suppl 1):2.30167030
17. Renzaho JN, Rutayisire E. Dual contraceptive use and associated factors among women aged 15–49 years on antiretroviral therapy in Kayonza district, Rwanda: a Cross-sectional study. Pan Afr Med J. (2022) 42:45. Available from: https://www.panafrican-med-journal.com/content/article/42/45/full35949473
18. Ayenew A. Women living with HIV and dual contraceptive use in Ethiopia: systematic review and meta-analysis. Contracept Reprod Med. (2022) 7(1):11.35778746
19. Bedecha DY, Gurmu MA, Gejo NG. Dual contraception method utilization and associated factors among women on anti-retroviral therapy in public facilities of Bishoftu Town, Oromia, Ethiopia. Edwards RJ, editor. PLoS One. (2023) 18(1):e0280447. doi: 10.1371/journal.pone.0280447
20. Reta MM, Tessema GA, Shiferaw G. Prevalence of dual contraceptive use and associated factors among HIV positive women at university of Gondar Hospital, Northwest Ethiopia. BMC Res Notes. (2019) 12(1):36.30658683
21. Gebrehiwot SW, Azeze GA, Robles CC, Adinew YM. Utilization of dual contraception method among reproductive age women on antiretroviral therapy in selected public hospitals of Northern Ethiopia. Reprod Health. (2017) 14(1):125.28982364
22. Amare G, Cherie N, Mekonen AM. Dual contraceptive use and associated factors among reproductive age group on antiretroviral therapy in Borena district, Northeast Ethiopia: a cross-sectional study. HIV AIDS (Auckl). (2021) 13:107–14.33531844
23. Erashi MWM, Tesso F, Beyene T. Dual-contraceptive method utilization and associated factors among HIV positive women attending art clinic in Gebretsadik Shawo Hospital, SNNPR, South West Ethiopia. Women’s Health Care. (2015) 4(6):107–14.
24. Tilahun Y, Bala ET, Bulto GA, Roga EY. Dual contraceptive utilization and associated factors among reproductive-age women on anti-retroviral therapy at hospitals in Central Ethiopia. Risk Manag Healthc Policy. (2021) 14:619–27.33623452
25. Polisi A, Gebrehanna E, Tesfaye G, Asefa F. Modern contraceptive utilization among female ART attendees in health facilities of Gimbie town, West Ethiopia. Reprod Health. (2014) 11(1):30.24731751
26. Demissie DB, Girma T, Abdissa G. Dual contraceptive utilization and associated factors among people living with HIV attending ART clinic in Fitche Hospital, Ethiopia. J Health Med Nurs. (2015) 2015:20.
27. Haile D, Lagebo B. Magnitude of dual contraceptive method utilization and the associated factors among women on antiretroviral treatment in Wolaita zone, southern Ethiopia. Heliyon. (2022) 8(6):e09595. doi: 10.1016/j.heliyon.2022.e09595
28. Kebede HG, Nahusenay H, Birhane Y, Tesfaye DJ. Assessment of contraceptive use and associated factors among HIV positive women in Bahir-Dar town, Northwest Ethiopia. OALib. (2015) 02(10):1–19.
29. Gebre W, Kidane EM, Negussie YM, Getahun MS, Bekele NT, Gurara AM. Assessment of menstrual hygiene management knowledge, practice, and associated factors among girls in Boset district, Ethiopia: a school-based cross-sectional study. Contracept Reprod Med. (2023 1) 8(1):34.37259164
30. Abay F, Yeshita HY, Mekonnen FA, Sisay M. Dual contraception method utilization and associated factors among sexually active women on antiretroviral therapy in Gondar city, Northwest, Ethiopia: a cross sectional study. BMC Women’s Health. (2020) 20(1):26. doi: 10.1186/s12905-020-0890-3
31. Jifar M, Handiso T, Mare T, Ibrahim S. Dual contraceptive utilization and associated factors among human immunodeficiency virus (HIV) positive women attending anti retro viral therapy (ART) clinic in Hossana Hospital, Southern Ethiopia. SM J Gynecol Obstet. (2017) 3(2):1023.
32. Ashore A, Erkalo D, Prakash R. Dual contraceptives and associated predictors in HIV positive women: a case–control study. Reprod Health. (2022) 19(1):168. doi: 10.1186/s12978-022-01475-x
33. Chakrapani V, Kershaw T, Shunmugam M, Newman PA, Cornman DH, Dubrow R. Prevalence of and barriers to dual-contraceptive methods use among married men and women living with HIV in India. Infect Dis Obstet Gynecol. (2011) 2011:376432. doi: 10.1155/2011/376432
34. Kaida A, Laher F, Strathdee SA, Money D, Janssen PA, Hogg RS, et al. Contraceptive use and method preference among women in soweto, South Africa: the influence of expanding access to HIV care and treatment services. Myer L, editor. PLoS One. (2010) 5(11):e13868. doi: 10.1371/journal.pone.0013868
35. Tilahun BH. Proportion of dual protection use at a time to prevent unwanted pregnancy and HIV/AIDS/sexually transmitted infections and its predictors among human immunodeficiency virus (HIV) positive women attending anti retro viral therapy (ART) Clinic Hosanna hospital, Southern Ethiopia; institution based cross sectional study. JOJPH. (2019) 4(5):555649. doi: 10.19080/JOJPH.2019.04.555649
36. Jemberie A, Aynalem BY, Zeleke LB, Alemu AA, Tiruye TY. Dual contraceptive method utilization and associated factors among HIV positive women attending ART clinic in Finote-Selam hospital: cross-sectional study. Arch Sex Behav. (2023) 52(6):2639–46.37027108
37. Tsuyuki K, Barbosa RM, Pinho ADA. Dual protection and dual methods in women living with HIV: the Brazilian context. J Sex Transm Dis. (2013 20) 2013:1–8. doi: 10.1155/2013/540789
38. Joshi B, Velhal G, Chauhan S, Kulkarni R, Begum S, Nandanwar Y, et al. Contraceptive use and unintended pregnancies among HIV-infected women in Mumbai. Indian J Community Med. (2015) 40(3):168. doi: 10.4103/0970-0218.158855
39. Sserwanja Q, Turimumahoro P, Nuwabaine L, Kamara K, Musaba MW. Association between exposure to family planning messages on different mass media channels and the utilization of modern contraceptives among young women in Sierra Leone: insights from the 2019 Sierra Leone demographic health survey. BMC Women’s Health. (2022 16) 22(1):376. doi: 10.1186/s12905-022-01974-w
40. Pazol K, Zapata LB, Dehlendorf C, Malcolm NM, Rosmarin RB, Frederiksen BN. Impact of contraceptive education on knowledge and decision making: an updated systematic review. Am J Prev Med. (2018) 55(5):703–15. doi: 10.1016/j.amepre.2018.07.012
41. Bello OO, Oluwasola TA, Bello FA. Awareness and practice of dual contraception among female tertiary institution students in Ibadan, Nigeria. Open Access J Contracept. (2016) 7:109–15. doi: 10.2147/OAJC.S103261
42. Dorji T, Wangmo K, Tshering D, Tashi U, Wangdi K. Knowledge and attitude on sexually transmitted infections and contraceptive use among university students in Bhutan. PLoS One. (2022) 17(8):e0272507. doi: 10.1371/journal.pone.0272507
Keywords: antiretroviral therapy, dual contraceptives use, women living with HIV, Ethiopia, Boset district
Citation: Belachwe YA, Sento M, Gobena MN, Getahun MS and Negussie YM (2025) Dual contraceptive use among women living with HIV on anti-retroviral therapy in Boset district, Ethiopia. Front. Glob. Women's Health 6:1510299. doi: 10.3389/fgwh.2025.1510299
Received: 12 October 2024; Accepted: 20 March 2025;
Published: 1 April 2025.
Edited by:
Stephen Kennedy, University of Oxford, United KingdomReviewed by:
Bilal Ahmed Usmani, Aga Khan University, PakistanCopyright: © 2025 Belachwe, Sento, Gobena, Getahun and Negussie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yohanes Abera Belachwe, eW9oYW5lc2FiZXJhOTlAZ21haWwuY29t; Yohannes Mekuria Negussie, eW9oYW5uZXNfbWVrdXJpYUB5YWhvby5jb20=
†ORCID:
Yohanes Abera Belachwe
orcid.org/0009-0008-0479-1221
Yohannes Mekuria Negussie
orcid.org/0000-0002-1332-670X
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.