- 1Specialist Perinatal Mental Health Service, Rotunda Hospital, Dublin, Ireland
- 2Department of Psychiatry, Mater Misericordiae University Hospital, Dublin, Ireland
Childbirth-related post-traumatic stress symptoms (CB-PTSS) occur in 12% of women and 3%–6% of mothers meet criteria for childbirth-related post-traumatic stress disorder (CB-PTSD). Eye Movement Desensitisation and Reprocessing (EMDR) therapy has shown promising results in this population. This study sought to assess the effectiveness of EMDR on CB-PTSS and CB-PTSD; to investigate the effect of EMDR duration on symptom reduction; to measure the EMDR completion rate; and to explore sample characteristics that may be associated with completion or effectiveness. A retrospective analysis was conducted of women (n = 34) who commenced EMDR for CB-PTSS or CB-PTSD in an Irish urban maternity hospital. Symptom severity was measured using the Posttraumatic Stress Disorder Checklist (PCL-5) pre- and post-EMDR. Pre-intervention, 64.7% (n = 22) of the sample met criteria for a provisional diagnosis of PTSD. The majority of women (61.8%) demonstrated a ≥ 10 point reduction on PCL-5 following EMDR. There was no correlation between reduction in PCL-5 score and number of EMDR sessions (r = −0.12, p = 0.504). The EMDR completion rate was 70.6%. Analyses did not identify any variables that were associated with EMDR completion or effectiveness. To our knowledge, this is the largest studied sample of women who have received EMDR for CB-PTSD or CB-PTSS. EMDR may be an effective intervention for CB-PTSS and CB-PTSD, even in women with a history of prior trauma, co-morbid mental health problems, or long-term symptoms. EMDR is easily-delivered with a low drop-out rate. Limitations include lack of a control group and long-term follow-up, and statistical analyses were limited by sample size.
Introduction
Traumatic birth experiences are common, with between 9% and 50% of mothers describing their birth experience as traumatic (1–3). A traumatic birth has been defined as “a woman's experience of interactions and/or events directly related to childbirth that caused overwhelming distressing emotions and reactions, leading to short- and/or long-term negative impacts on a woman's health and wellbeing” (4).
Twelve per cent of women experience childbirth-related post-traumatic stress symptoms (CB-PTSS) and 3%–6% of mothers meet criteria for childbirth-related post-traumatic stress disorder (CB-PTSD) (5). A PTSD diagnosis in this context requires the presence of symptoms in four symptom groups (re-experiencing the traumatic event, avoidance of reminders of the event, negative alterations in mood and cognition and hyperarousal), as well as exposure to actual or threatened death or serious injury (6). Numerous studies demonstrate that there are negative sequelae of CB-PTSS for women, whether they meet PTSD diagnostic criteria or not, including fear of subsequent births (7), reduced breastfeeding (8), mother-partner relationship problems (9) and possible mother-infant attachment difficulties (10). In terms of comorbidity, a significant proportion of women with CB-PTSD also endorse depressive symptoms (11–13), and CB-PTSD and postpartum depression seem to share underlying vulnerability factors, including traumatic birth (11, 14).
The National Institute for Health and Care Excellence (NICE) guidelines for antenatal and postnatal mental health recommend offering women with childbirth-related PTSD (CB-PTSD) a high-intensity psychological intervention, specifically trauma-focused CBT (TF-CBT) or Eye Movement Desensitisation and Reprocessing (EMDR) therapy (15). EMDR is based on the Adaptive Information Processing model (16) which considers the cause of posttraumatic stress symptoms to be inadequately processed memories of a past traumatic experience. It is a standardised, eight-phase psychological therapy. During EMDR, clients focus on the traumatic memory, while simultaneously experiencing bilateral stimulation (e.g., eye movements) which encourages reprocessing and integration of the stored trauma-related information as an adaptive contextualised memory (17).
There have been positive and promising results demonstrated in studies using EMDR for CB- PTSD. A meta-analysis demonstrated that trauma-focused psychological therapies, including EMDR, are effective in reducing PTSD symptoms in the early postnatal period (18). A systematic review also suggests that EMDR intervention reduces CB-PTSD symptoms (19). However, the conclusions of these review articles are limited by the evidence available, which to date has relied on very small case series samples (20, 21) studies without quantitative outcome measures (21), and studies using brief versions of EMDR e.g., one session in a pilot randomised controlled trial (RCT) (22). In light of the limited available evidence, there is also no current consensus on the acceptability of EMDR in CB-PTSD. Drawing on the wider PTSD literature (rather than childbirth-related PTSD specifically), a Cochrane review of psychological therapies for PTSD found that there was no difference in drop-out rates comparing EMDR intervention groups to individual trauma-focused CBT/exposure therapy intervention groups, nor to waitlist/usual care groups (23).
There is a paucity of research investigating interventions for women experiencing childbirth-related posttraumatic stress symptoms that are subthreshold for PTSD. Two recent pilot RCTs have demonstrated the feasibility of brief EMDR (1–3 sessions) (24) and effectiveness of one EMDR session in the early postpartum period for improving subthreshold symptoms (22). Interestingly, Furuta's meta-analysis found that there were more favourable results for trauma-focused therapies in subclinical PTSS compared with PTSD (18).
Given the limited research to date on EMDR in CB-PTSS (i.e., subclinical CB-PTSD), it may be useful to look to the literature more generally. EMDR early interventions for subthreshold symptoms following a variety of traumas have been shown to siginficantly reduce PTSD symptoms (25), generally in 1–3 sessions. The available data suggests low drop out rates; for example, Jarero and colleagues report a 100% completion rate in two studies using two-session EMDR interventions (26, 27). While EMDR is not currently recommended by NICE for disorders other than PTSD, it has also shown promising results in a wide range of conditions including obsessive-compulsive disorder (28), panic disorer (29), phobias including tokophobia (fear of childbirth) (30), and prolonged grief disorder symptoms (31). Furthermore, the study of pregnant women who received EMDR for fear of childbirth reported a dropout rate of 10%, which was similar to care as usual (30).
Pregnant women are often excluded or underrepresented in clinical research (32). However, a systematic review of treatment of pregnant women with PTSD (not specific to childbirth) demonstrated no harm from psychological interventions including EMDR (33). Furthermore, a randomised-controlled trial assessed the safety and efficacy of EMDR in pregnant women (30). While the study's focus was on fear of childbirth (rather than PTSD symptoms), the results supported EMDR as a safe treatment in pregnancy.
Women experiencing PTSD related to a non-live birth (i.e., miscarriage, intrauterine death or stillbirth) are often excluded from CB-PTSD studies. While the aetiology of developing symptoms in these cases may differ to live births (34), the same diagnostic criteria are applied to diagnose PTSD in this cohort, and guidelines suggests these women should also be offered EMDR or TF-CBT (35).
There is currently no widely agreed standardised treatment protocol for EMDR in CB-PTSD, nor do guidelines recommend an optimal number of treatment sessions. The EMDR Recent Birth Trauma Protocol (36) suggests a number of treatment steps, specific to CB-PTSD. Guidelines for PTSD in general are more directive. For example, in the case of non-combat-related trauma, NICE recommends that EMDR is typically provided over 8–12 sessions (more if clinically indicated, e.g., in the case of multiple traumas) (37).
Our understanding of the acceptability of EMDR for CB-PTSD is limited. In a study of pregnant women who received EMDR for fear of childbirth, the dropout rate from the EMDR intervention group was 10%, which was similar to care as usual (30).
Methods
Objectives
The objectives of the present study were four-fold.
Our primary outcomes were:
(1) To assess the effectiveness of EMDR treatment on CB-PTSS and CB-PTSD
(2) To ascertain whether there is an effect of EMDR treatment duration on symptom reduction
Our secondary outcomes were:
(3) To measure the completion rate of EMDR (i.e., participants who completed the number of EMDR sessions recommended by the EMDR therapist)
(4) To explore sample characteristics that may be associated with EMDR completion and or EMDR effectiveness
Study design and sample
A retrospective analysis was conducted of all women who commenced EMDR for CB-PTSS or CB-PTSD over a three year period (between January 2020 and January 2024). This study received ethical approval from the hospital's Research Advisory Group (RAG-2023-023).
Inclusion criteria were:
(1) Post-traumatic stress symptoms related to childbirth (i.e., onset post-birth and ≥1 month duration of symptoms)
(2) Aged ≥ 18 years at presentation to Birth Trauma Clinic
Exclusion criteria were:
(1) Did not commence EMDR sessions
(2) Completed only one EMDR session
(3) Missing/uncompleted pre- or post-EMDR quantitative symptom measures
Setting
The setting was the Birth Trauma Clinic at a large urban standalone university-affiliated maternity hospital in Ireland. The Birth Trauma Clinic is a publicly funded multidisciplinary service for women with CB-PTSS or CB-PTSD, run by the Specialist Perinatal Mental Health Service within the hospital. The Clinic is available to women attending for both public and private obstetric/maternity healthcare.
Measures
The posttraumatic stress disorder checklist (PCL-5)
The PCL-5 is the measure currently used in the Birth Trauma Clinic to screen for CB-PTSS and CB-PTSD, and to measure treatment response. The PCL-5 is a widely used 20-item self-report measure which corresponds with the DSM-5 symptom criteria for PTSD. The tool demonstrates strong psychometric properties (38) and has previously been used in CB-PTSD research (39).
The rating scale is 0–4 for each symptom. A total symptom severity score (range - 0–80) can be obtained by summing the scores for each of the 20 items. The PCL-5 assesses the four symptom clusters of PTSD. A symptom is considered as present when the corresponding item is scored ≥2.
The PCL-5 can determine a provisional PTSD diagnosis by using cut-off score of 31–33 (38). The more stringent cut-off of 33 was chosen for the purposes of this study. A 10 point (or more) reduction on the PCL-5 is deemed to be a clinically meaningful improvement (40).
Screening and intervention
All patients attending the Birth Trauma Clinic were routinely screened for CB-PTSS/CB-PTSD at their first apointment, using the PCL-5. Alongside a clinical interview, the PCL-5 identified patients with CB-PTSS and CB-PTSD. Patients were offered EMDR (rather than other trauma-focussed interventions, including TF-CBT) in the first instance, in line with the expertise and training of clinicians within the service. EMDR, with a focus on childbirth-related trauma, was delivered by one of two EMDR therapists, who both engage in regular external supervision. The recommended duration of EMDR (number of sessions) was decided during therapy by the therapist, according to treatment response. Session duration was 60–90 min. Sessions were delivered in person or online.
Data collection
EMDR clinic patient lists were obtained for the period of study and subject data was extracted from the hospital's electronic health records (Cerner Powerchart software) into an Excel file. Data was anonymised at the point of extraction. Data collection was performed by author AD. Data was coded as “unknown” if the relevant variable detail was missing or unknown after reviewing the patient's health record.
Maternal demographic variables of interest included: age, ethnicity, relationship status, employment status, public/private patient. Maternal obstetric variables (of index birth) included parity, pregnancy planning, fertility treatment, method of labour onset, analgesia use during labour/birth, mode of birth. Maternal psychiatric variables included: psychiatric comorbidity (i.e., documented comorbid psychiatric diagnosis in index perinatal period), previous trauma history, psychotropic use during EMDR, pregnancy status during EMDR, date commenced EMDR (days since index birth), EMDR completion status, duration of EMDR (sessions), duration of EMDR (days), diagnosis of PTSD pre-EMDR, PCL-5 score pre-EMDR, diagnosis of PTSD post-EMDR, PCL-5 score post-EMDR. Neonatal variables were: gestational age at delivery, NICU admission requirement.
Statistical analyses
Statistical analyses were performed using JASP (version 0.14.1) for MacOS. Parametric or non-parametric tests were chosen depending on whether the appropriate statistical assumptions were met.
Descriptive statistics were used to assess demographic and clinical characteristics of the sample, provisional PTSD diagnosis and EMDR completion rates and pre- and post- EMDR mean symptom scores. A paired samples t-test was used to compare pre- and post-EMDR PCL-5 scores to determine the effectiveness of EMDR on CB-PTSS in this sample. Pearson's correlation was used to ascertain whether there was an effect of EMDR treatment duration (i.e., number of sessions) on CB-PTSS symptom reduction. Kendall's correlation was used to assess whether there was an effect of birth-to-EMDR interval on CB-PTSS symptom reduction. Univariate regression analyses were used to explore potential variables associated with EMDR completion, using EMDR completion as the dependent variable. Given that this was an exploratory analysis, a multivariate regression model was not used. Possible associations between variables and EMDR effectiveness (i.e., CB-PTSS symptom reduction) were explored using independent samples T-tests, Mann Whitney U and ANOVA analyses (depending on the appropriate statistical test).
Results
Sociodemographic and clinical characteristics
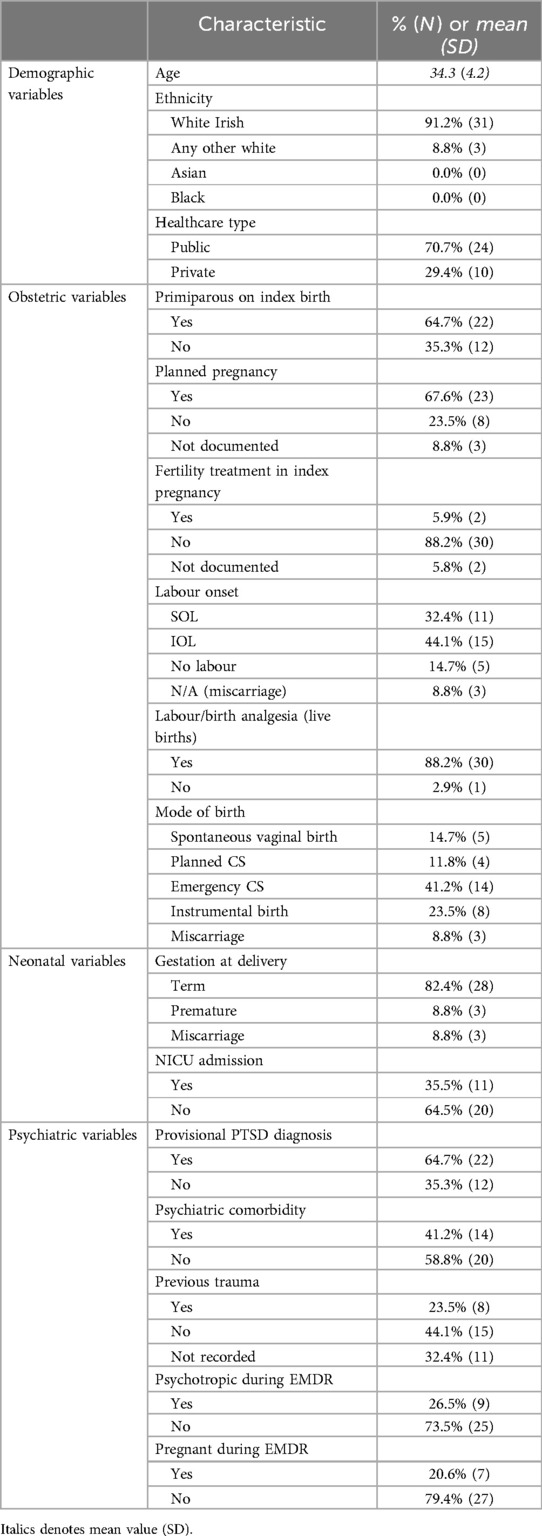
Thirty-four women were included in the study. All of the women (100%; n = 34) were in a relationship and 88.2% (n = 30) were in employment. The demographic and baseline obstetric, psychiatric and neonatal characteristics of the sample are reported in Table 1.
Prior to EMDR, 64.7% (n = 22) of the sample met criteria for a provisional diagnosis of PTSD. The remainder of the sample (35.3%, n = 12) had subthreshold symptoms (i.e., CB-PTSS). A comorbid psychiatric diagnosis was present in 41.2% (n = 14) of the sample, which included anxiety disorders (n = 6), depressive disorders (n = 2), both anxiety and depressive disorders (n = 4), dissociative disorder (n = 1) and neurodevelopmental disorders (i.e., ADHD, n = 1).
EMDR intervention
The mean number of EMDR sessions completed was 4.9 (SD 1.9, range 2–9). Participants commenced EMDR on average (mean) 333.6 days (SD 231.4) following the index childbirth (range 90–1,178 days).
Primary outcomes
The mean PCL-5 score commencing EMDR was 37.8 (SD 16.2, range 6–65) and the mean PCL-5 score on completion of EMDR was 23.7 (SD 20.5, range 0–67) (see Figure 1).
On average, there was a PCL-5 score reduction of 14.1 (SE 2.5) following EMDR and this reduction was significant [t (33) = 5.7, p < .001]. Cohen's d (1.0) suggests that this is a large effect. Comparing PCL-5 scores pre- and post-EMDR, the majority of the sample (61.8%, n = 21) demonstrated a ≥10 point reduction on PCL-5 (i.e., a clinically meaningful improvement). Of the 22 participants who met criteria for a provisional diagnosis of PTSD pre-EMDR, 50% of these (i.e., n = 11) no longer met criteria for PTSD following EMDR intervention.
Correlation analyses showed there was no correlation between reduction in PCL-5 score and number of EMDR sessions delivered (r = −0.12, p = 0.504) and no correlation between number of EMDR sessions delivered and symptom severity pre-intervention (i.e., pre-EMDR PCL-5 score) (r = 0.21, p = 0.264). There was no correlation between mean reduction in PCL-5 score and birth-to-EMDR interval (tau B = 0.05, p = 0.653).
Secondary outcomes
EMDR completion
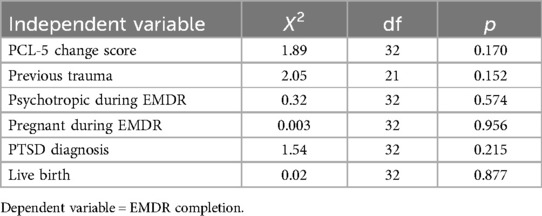
The EMDR completion rate was 70.6% (n = 24). Participants who completed the recommended number of EMDR sessions had a mean reduction in PCL-5 score of 16.2 (SE 3.2). Participants who did not complete the recommended number of sessions had a mean reduction in PCL-5 score of 9.1 (SE 3.2). This difference was not significant t (32) = 1.33, p = 0.195. The exploratory univariate regression analyses did not identify any variables significantly associated with EMDR completion rate (see Table 2).
EMDR effectiveness
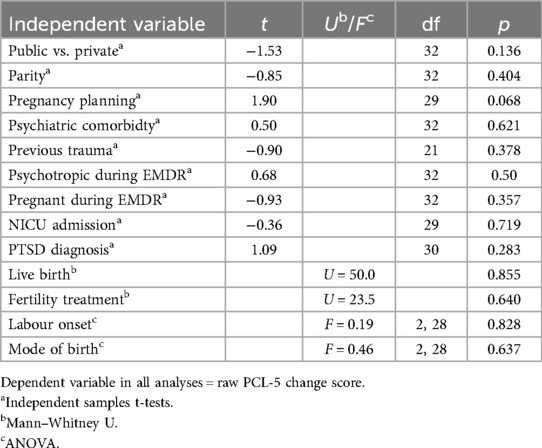
The independent samples t-tests, Mann–Whitney U, and ANOVA analyses did not identify any variables associated with EMDR effectiveness (see Table 3).
Discussion
Our study suggests that EMDR may be an effective intervention for CB-PTSS and CB-PTSD. Within our sample, there was a significant reduction in symptoms following EMDR intervention. The majority of the sample demonstrated a clinically meaningful improvement in symptoms. In those that met criteria for CB-PTSD prior to intervention, half of these women no longer met diagnostic criteria following EMDR.
Given its real-word design, this study did not limit the number of sessions of EMDR and the number of treatment sessions was tailored to treatment need. Our study found that effective EMDR was delivered within a relatively small number of sessions, with women attending an average of five treatment sessions. The effectiveness of brief EMDR (i.e., 1–3 sessions) has previously been demonstrated, but these studies delivered EMDR early in the postpartum period, within days (22) or 10–16 weeks (24) of birth. The mean duration of symptoms in this study sample, prior to EMDR intervention was 11 months. Therefore, we know that in this sample, symptoms remained significant even after a considerable amount of time had passed without intervention. This supports the hypothesis that the EMDR was the key factor in alleviating symptoms, despite the absence of a control group. Our study suggests that EMDR can be delivered effectively, in a small number of sessions, even when symptoms are chronic.
This study did not find an association between the number of EMDR sessions delivered and severity of symptoms, nor an association between number of EMDR sessions and symptom reduction. Furthermore, due to the small size of the study, we were unable to identify other maternal, obstetric, neonatal or psychiatric variables that may impact on EMDR effectiveness. This includes variables of particular interest including pregnancy status during EMDR and women with symptoms following a non-live birth.
The high completion rate of EMDR in this study also suggests that EMDR is an acceptable intervention for women with CB-PTSD and CB-PTSS, who are a cohort that is motivated to engage and complete treatment. It is worth noting that our dropout rate was higher than that reported in a study of EMDR for women with fear of childbirth, though the fear of childbirth study's intervention was shorter in duration (3 sessions). An exploration of reasons for non-completion is beyond the scope of this paper.
Women with psychiatric comorbidity or a history of previous trauma were not excluded from this study. Almost half of the sample had a comorbid psychiatric diagnosis recorded in the index perinatal period (including affective and anxiety disorders) and almost a quarter of the sample reported a previous trauma. This suggests that EMDR may be an effective treatment for women with CB-PTSS in the context of psychiatric complexity and previous trauma. This is in line with studies demonstrating EMDR effectiveness in women with non-childbirth-related PTSD who have experienced multiple traumas (24) or psychiatric co-morbidity (41).
A small number of women included in our study (n = 3) received EMDR following a miscarriage. Live birth did not determine EMDR effectiveness or completion in this study, but given the small number of women who were included following a miscarriage, we are unable to comment on how bereavement may impact EMDR effectiveness or completion.
An exploration of the multiple factors that contributed to the long duration of symptoms prior to intervention in this real-world design are beyond the scope of this study, but likely include delays in screening/detection of symptoms, the presence of a waiting list prior to intervention commencing, understaffing and underfunding of services. Currently, Specialist Perinatal Mental Health Services in Ireland operate in line with a Model of Care (42) that offers intervention up to one year post-birth. This may preclude women from accessing appropriate specialist treatments such as EMDR. Future Models of Care should ensure there is increased access to appropriate specialist treatments.
Strengths
To our knowledge, this is the largest studied sample of women who have received EMDR for CB-PTSD or CB-PTSS. The real-world design and setting allowed the number of sessions of EMDR to be tailored based on patient need, rather than a study protocol, and enabled inclusion of women with subclinical symptoms. The mean duration of symptoms in this sample prior to EMDR intervention suggests that EMDR remains effective in chronic CB-PTSD and CB-PTSS.
Limitations
This study is limited by its retrospective design and lack of long-term follow-up. The lack of a control arm impacts the generalisability of the study findings. It is also limited by its reliance on self-report measures. The size of the study meant we were unable to identify statistically significant variables that may impact on EMDR acceptability and effectiveness. While the study hospital site is located in an area of social deprivation, our sample was not ethnically diverse, with participants only of white ethnicity. Furthermore, our study was not able to examine the complex relationship between trauma symptoms and attachment, which may impact the interpretation of some of our findings.
Future research
To confirm the effectiveness of EMDR in this cohort, controlled studies with larger sample sizes and longer follow-up periods will be helpful. Future research investigating whether there are variables which contribute to effectiveness and acceptability for this population (e.g., intervention components; clinical characteristics) is necessary. While use of the PCL-5 is consistent with much of the literature in the area, future studies may consider the use of the City Birth Trauma Scale (43) more appropriate, which was specifically developed for use in this group, adheres to DSM-5 diagnostic criteria and has good psychometric properties (43). We suggest that prospective studies should also endeavour to include more diverse populations including ethnic minorities (44), who are often excluded from, or have difficulty accessing, perinatal mental health services (45).
Conclusion
EMDR may be an effective intervention for CB-PTSS and CB-PTSD and is easily-delivered with a low drop-out rate. This study demonstrates the effectiveness of EMDR in individuals who have had symptoms for almost a year and in individuals with a history of prior trauma or comorbid mental health problems.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Research Advisory Group, Research and Ethics Committee, Rotunda Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
AD: Conceptualization, Data curation, Formal Analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing, Investigation. UN: Conceptualization, Methodology, Writing – review & editing, Investigation. JD: Conceptualization, Methodology, Writing – review & editing, Investigation. RD: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nagle U, Naughton S, Ayers S, Cooley S, Duffy RM, Dikmen-Yildiz P. A survey of perceived traumatic birth experiences in an Irish maternity sample - prevalence, risk factors and follow up. Midwifery. (2022) 113:103419. doi: 10.1016/j.midw.2022.103419
2. O'Donovan A, Alcorn KL, Patrick JC, Creedy DK, Dawe S, Devilly GJ. Predicting posttraumatic stress disorder after childbirth. Midwifery. (2014) 30(8):935–41. doi: 10.1016/j.midw.2014.03.011
3. Stramrood CA, Paarlberg KM, Huis In ‘t Veld EM, Berger LW, Vingerhoets AJ, Schultz WC, et al. Posttraumatic stress following childbirth in homelike- and hospital settings. J Psychosom Obstet Gynaecol. (2011) 32(2):88–97. doi: 10.3109/0167482X.2011.569801
4. Leinweber J, Fontein-Kuipers Y, Thomson G, Karlsdottir SI, Nilsson C, Ekström-Bergström A, et al. Developing a woman-centered, inclusive definition of traumatic childbirth experiences: a discussion paper. Birth. (2022) 49(4):687–96. doi: 10.1111/birt.12634
5. Heyne CS, Kazmierczak M, Souday R, Horesh D, Lambregtse-van den Berg M, Weigl T, et al. Prevalence and risk factors of birth-related posttraumatic stress among parents: a comparative systematic review and meta-analysis. Clin Psychol Rev. (2022) 94:102157. doi: 10.1016/j.cpr.2022.102157
6. American Psychiatric Association. DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Washington, D.C.: American Psychiatric Association (2013). xliv, p. 947.
7. Garthus-Niegel S, Horsch A, von Soest T, Haga SM, Drozd F, Ayers S, et al. Posttraumatic stress symptoms following childbirth: associations with prenatal attachment in subsequent pregnancies. Arch Womens Ment Health. (2020) 23(4):547–55. doi: 10.1007/s00737-019-01011-0
8. Garthus-Niegel S, Horsch A, Ayers S, Junge-Hoffmeister J, Weidner K, Eberhard-Gran M. The influence of postpartum PTSD on breastfeeding: a longitudinal population-based study. Birth. (2018) 45(2):193–201. doi: 10.1111/birt.12328
9. Garthus-Niegel S, Horsch A, Handtke E, von Soest T, Ayers S, Weidner K, et al. The impact of postpartum posttraumatic stress and depression symptoms on couples’ relationship satisfaction: a population-based prospective study. Front Psychol. (2018) 9:1728. doi: 10.3389/fpsyg.2018.01728
10. Van Sieleghem S, Danckaerts M, Rieken R, Okkerse JME, de Jonge E, Bramer WM, et al. Childbirth related PTSD and its association with infant outcome: a systematic review. Early Hum Dev. (2022) 174:105667. doi: 10.1016/j.earlhumdev.2022.105667
11. Söderquist J, Wijma B, Thorbert G, Wijma K. Risk factors in pregnancy for post-traumatic stress and depression after childbirth. BJOG. (2009) 116(5):672–80. doi: 10.1111/j.1471-0528.2008.02083.x
12. White T, Matthey S, Boyd K, Barnett B. Postnatal depression and post-traumatic stress after childbirth: prevalence, course and co-occurrence. J Reprod Infant Psychol. (2009) 24(2):107–20. doi: 10.1080/02646830600643874
13. Dekel S, Ein-Dor T, Dishy GA, Mayopoulos PA. Beyond postpartum depression: posttraumatic stress-depressive response following childbirth. Arch Womens Ment Health. (2020) 23(4):557–64. doi: 10.1007/s00737-019-01006-x
14. Waller R, Kornfield SL, White LK, Chaiyachati BH, Barzilay R, Njoroge W, et al. Clinician-reported childbirth outcomes, patient-reported childbirth trauma, and risk for postpartum depression. Arch Womens Ment Health. (2022) 25(5):985–93. doi: 10.1007/s00737-022-01263-3
15. National Collaborating Centre for Mental Health (Great Britain), British Psychological Society, Royal College of Psychiatrists, National Institute for Health and Care Excellence (Great Britain). Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance. Leicester, London: The British Psychological Society; The Royal College of Psychiatrists (2014). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK305023/
16. Shapiro F. EMDR, adaptive information processing, and case conceptualization. J EMDR Pract Res. (2007) 1:68–87. doi: 10.1891/1933-3196.1.2.68
17. Landin-Romero R, Moreno-Alcazar A, Pagani M, Amann BL. How does eye movement desensitization and reprocessing therapy work? A systematic review on suggested mechanisms of action. Front Psychol. (2018) 9:1395. doi: 10.3389/fpsyg.2018.01395
18. Furuta M, Horsch A, Ng ESW, Bick D, Spain D, Sin J. Effectiveness of trauma-focused psychological therapies for treating post-traumatic stress disorder symptoms in women following childbirth: a systematic review and meta-analysis. Front Psychiatry. (2018) 9:591. doi: 10.3389/fpsyt.2018.00591
19. de Bruijn L, Stramrood CA, Lambregtse-van den Berg MP, Rius Ottenheim N. Treatment of posttraumatic stress disorder following childbirth. J Psychosom Obstet Gynaecol. (2020) 41(1):5–14. doi: 10.1080/0167482X.2019.1593961
20. Sandström M, Wiberg B, Wikman M, Willman AK, Högberg U. A pilot study of eye movement desensitisation and reprocessing treatment (EMDR) for post-traumatic stress after childbirth. Midwifery. (2008) 24(1):62–73. doi: 10.1016/j.midw.2006.07.008
21. Stramrood CA, van der Velde J, Doornbos B, Marieke Paarlberg K, Weijmar Schultz WC, van Pampus MG. The patient observer: eye-movement desensitization and reprocessing for the treatment of posttraumatic stress following childbirth. Birth. (2012) 39(1):70–6. doi: 10.1111/j.1523-536X.2011.00517.x
22. Chiorino V, Cattaneo MC, Macchi EA, Salerno R, Roveraro S, Bertolucci GG, et al. The EMDR recent birth trauma protocol: a pilot randomised clinical trial after traumatic childbirth. Psychol Health. (2020) 35(7):795–810. doi: 10.1080/08870446.2019.1699088
23. Bisson JI, Roberts NP, Andrew M, Cooper R, Lewis C. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. (2013) 2013(12):CD003388. doi: 10.1002/14651858.CD003388.pub4
24. Kopmeiners EHM, Hollander MH, van Voorst N, Stramrood CAI. Effect of early postpartum EMDR on reducing psychological complaints in women with a traumatic childbirth experience. J Psychosom Obstet Gynaecol. (2023) 44(1):2229010. doi: 10.1080/0167482X.2023.2229010
25. Shapiro E, Maxfield L. The efficacy of EMDR early interventions. J EMDR Pract Res. (2019) 13(4):291–301. doi: 10.1891/1933-3196.13.4.291
26. Jarero I, Uribe S, Artigas M, Givaudan M. EMDR Protocol for recent critical incidents: a randomized controlled trial in a technological disaster context. J EMDR Pract Res. (2015) 9(4):166–73. doi: 10.1891/1933-3196.9.4.166
27. Jarero I, Amaya C, Givaudan M, Miranda A. EMDR individual protocol for paraprofessional use: a randomized controlled trial with first responders. J EMDR Pract Res. (2013) 7(2):55–64. doi: 10.1891/1933-3196.7.2.55
28. Talbot D. Examination of initial evidence for EMDR as a treatment for obsessive-compulsive disorder. J EMDR Pract Res. (2021) 15(3):167–73. doi: 10.1891/EMDR-D-21-00004
29. Faretta E, Del Farra M. Efficacy of EMDR therapy for anxiety disorders. J EMDR Pract Res. (2019) 13(4):325–32. doi: 10.1891/1933-3196.13.4.325
30. Baas MAM, van Pampus MG, Stramrood CAI, Dijksman LM, Vanhommerig JW, de Jongh A. Treatment of pregnant women with fear of childbirth using EMDR therapy: results of a multi-center randomized controlled trial. Front Psychiatry. (2021) 12:798249. doi: 10.3389/fpsyt.2021.798249
31. Spicer L. Eye movement desensitisation and reprocessing (EMDR) therapy for prolonged grief: theory, research, and practice. Front Psychiatry. (2024) 15:1357390. doi: 10.3389/fpsyt.2024.1357390
32. Shields KE, Lyerly AD. Exclusion of pregnant women from industry-sponsored clinical trials. Obstet Gynecol. (2013) 122(5):1077–81. doi: 10.1097/AOG.0b013e3182a9ca67
33. Baas MAM, van Pampus MG, Braam L, Stramrood CAI, de Jongh A. The effects of PTSD treatment during pregnancy: systematic review and case study. Eur J Psychotraumatol. (2020) 11(1):1762310. doi: 10.1080/20008198.2020.1762310
34. Daugirdaitė V, van den Akker O, Purewal S. Posttraumatic stress and posttraumatic stress disorder after termination of pregnancy and reproductive loss: a systematic review. J Pregnancy. (2015) 2015:646345. doi: 10.1155/2015/646345
35. Excellence NIfHaC. Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance. London: NICE (2020).
36. Cattaneo MC, Chiorino V, Roveraro S, Salemo R, Fernandez I. The EMDR recent birth trauma protocol. In: Luber M, editor. Eye Movement Densensitzation and Reprocessing (EMDR) Therapy Scripted Protocols and Summary Sheets Treating Trauma in Somatic and Medical Related Conditions. New York, NY: Springer (2019). p. 377–425.
37. National Institute for Health and Care Excellence (Great Britain), National Guideline Centre (Great Britain). Post-traumatic Stress Disorder. London: National Institute for Health and Care Excellence (2018). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK542453/
38. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. (2015) 28(6):489–98. doi: 10.1002/jts.22059
39. Deforges C, Sandoz V, Noël Y, Avignon V, Desseauve D, Bourdin J, et al. Single-session visuospatial task procedure to prevent childbirth-related posttraumatic stress disorder: a multicentre double-blind randomised controlled trial. Mol Psychiatry. (2023) 28(9):3842–50. doi: 10.1038/s41380-023-02275-w
40. Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) (2013).
41. Valiente-Gómez A, Moreno-Alcázar A, Treen D, Cedrón C, Colom F, Pérez V, et al. EMDR beyond PTSD: a systematic literature review. Front Psychol. (2017) 8:1668. doi: 10.3389/fpsyg.2017.01668
42. Wrigley M, O'Riordan F, Cassidy E. Specialist Perinatal Mental Health Services: Model of Care for Ireland. Ireland: Health Service Executive (2017).
43. Ayers S, Wright DB, Thornton A. Development of a measure of postpartum PTSD: the city birth trauma scale. Front Psychiatry. (2018) 9:409. doi: 10.3389/fpsyt.2018.00409
44. Horsch A, Garthus-Niegel S, Ayers S, Chandra P, Hartmann K, Vaisbuch E, et al. Childbirth-related posttraumatic stress disorder: definition, risk factors, pathophysiology, diagnosis, prevention, and treatment. Am J Obstet Gynecol. (2024) 230(3S):S1116–S27. doi: 10.1016/j.ajog.2023.09.089
Keywords: EMDR (eye movement desensitization and reprocessing), Birth Trauma, PTSD - posttraumatic stress disorder, effectiveness, childbirth
Citation: Doherty A, Nagle U, Doyle J and Duffy RM (2025) Eye movement desensitisation and reprocessing for childbirth-related post-traumatic stress symptoms: effectiveness, duration and completion. Front. Glob. Womens Health 6:1487799. doi: 10.3389/fgwh.2025.1487799
Received: 28 August 2024; Accepted: 22 January 2025;
Published: 4 February 2025.
Edited by:
Stephen Kennedy, University of Oxford, United KingdomReviewed by:
Francesca Palestra, World Health Organization, SwitzerlandSean Naughton, St John of God Community Services, Ireland
Copyright: © 2025 Doherty, Nagle, Doyle and Duffy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: A. Doherty, YWlsYmhlbWRvaGVydHlAZ21haWwuY29t
 A. Doherty
A. Doherty U. Nagle
U. Nagle J. Doyle1
J. Doyle1