- 1Department of Midwifery, College of Health Science, Woldia University, Woldia, Ethiopia
- 2Department of Nursing, College of Health Science, Woldia University, Woldia, Ethiopia
- 3Department of Medical Laboratory Sciences, College of Health Science, Woldia University, Woldia, Ethiopia
- 4College of Medicine and Health Sciences, Woldia University, Woldia, Ethiopia
- 5Department of Pediatrics and Child Health Nursing, School of Nursing, College of Health Science, Woldia University, Woldia, Ethiopia
Introduction: Effective use of the partograph is crucial in identifying abnormal labor (prolonged and obstructed labor) and taking appropriate actions. However, in Ethiopia, the prevalence of obstructed labor is much higher at 11.8% and contributes to 14.4% of the total maternal deaths due to underutilization of the partograph by obstetric caregivers. Although a previous systematic review and meta-analysis (SRMA) had been conducted, they were not representative on a national level as they included a limited number of studies and did not evaluate the current prevalence of partograph utilization beyond July 2019. Since then, there have been inconsistent studies assessing the proportion of partograph utilization and its associated factors. Therefore, this systematic review and meta-analysis aimed to estimate the pooled prevalence of partograph utilization and its associated factors in Ethiopia.
Method: Comprehensive literature searches were conducted in PubMed, Google Scholar, and HINARI from 1 September 2013 to 23 October 2023. A random-effects model was used to estimate pooled prevalence and adjusted odds ratio. Stata (version 11.0) was used to analyze the data. Cochrane I2 statistics were computed to assess heterogeneity among studies. A subgroup analysis was done based on the study region to minimize underlying heterogeneity. Funnel plot and Eggers test were conducted to assess publication bias.
Result: Overall, 661 articles were retrieved, and finally, 23 studies were included in this systematic review, including 7,649 participants. The pooled prevalence of partograph utilization was 54.92% (95% CI: 43.38–66.45). The subgroup analysis showed that partograph utilization was highest in the Dire Dawa region and lowest in the Amhara region. Factors such as partograph training [adjusted odds ratio (AOR) = 3.63, 95% CI: 2.57–5.25], good knowledge about partograph (AOR = 2.63, 95% CI: 1.62–4.26), a favorable attitude toward partograph (AOR = 1.95, 95% CI: 1.35–2.82), partograph availability (AOR = 0.89, 95% CI: 2.24–6.61), and being in the midwifery profession (AOR = 0.09, 95% CI: 1.78–5.25) were significantly associated with partograph utilization.
Conclusion: The pooled prevalence of partograph utilization in Ethiopia was low. Partograph training, good knowledge about partograph, favorable attitude toward partograph, partograph availability in the health facility, and being in the midwifery profession were significantly associated with partograph utilization.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier (CRD42023475818).
Introduction
The partograph is a standardized tool used to monitor the health status of both the mother and fetus during labor. It consists of three components: the fetal component, which monitors the fetal condition; the labor progress component, which tracks the progress of labor; and the maternal component, which assesses the mother's condition. The World Health Organization (WHO) recommends the use of the partograph to detect any abnormalities and aid in timely decision-making regarding the continuation of labor, augmentation, or the need for a cesarean delivery, starting from the active first stage of labor or when the cervix is dilated to 4 cm (1). By providing a visual overview of it, the partograph enables healthcare professionals to identify and diagnose abnormal labor progression, including prolonged and obstructed labor, which are major causes of maternal and neonatal deaths in developing countries, including Ethiopia (2). Globally, it is estimated that obstructed labor occurs in 5% of pregnancies and accounts for approximately 8% of maternal deaths (3, 4). However, in Ethiopia, the prevalence of obstructed labor is much higher at 11.8% and contributes to 14.4% of total maternal deaths (5, 6). Prolonged labor is also a leading cause of maternal and newborn deaths in developing countries. Therefore, the effective use of the partograph is crucial in identifying abnormal labor and taking appropriate actions (2). Research has shown that the utilization of the partograph can lead to significant improvements in labor outcomes. For example, its use has been associated with a reduction in the rate of prolonged labor, the proportion of labor requiring augmentation, emergency cesarean deliveries, and stillbirths (1, 7). The partograph includes a specific line that indicates the presence of difficulties such as slow labor progress, prolonged labor, fetal distress, obstructed labor, and ruptured uterus or when these issues should be addressed. Early detection of protracted or obstructed labor greatly aids in preventing complications such as postpartum hemorrhage, ruptured uterus, puerperal infections, and obstetric fistulas (6). However, there are barriers to the effective use of the partograph, particularly in low-resource settings. Challenges include limited resources, a shortage of healthcare personnel, low competency in using the tool, inadequate supervision, low acceptability of the tool, and a lack of functioning referral systems (8). Partograph utilization varies in different healthcare settings in Ethiopia, ranging from 6.9% in Jimma University Hospital (9) to 92.6% in eastern Ethiopia (10). Factors such as supervision, training on the partograph, knowledge about its use, the number of obstetric caregivers per shift, the working institution, and attitudes toward its utilization have been identified as factors influencing its utilization (11–15). Although a previous systematic review and meta-analysis (SRMA) have been conducted, they were not representative on a national level as they included a limited number of studies and did not evaluate the current prevalence of partograph utilization beyond July 2019 (16). Since then, there have been inconsistent studies assessing the proportion of partograph utilization and its associated factors. Therefore, this systematic review and meta-analysis aimed to estimate the pooled prevalence of partograph utilization and its associated factors in Ethiopia.
Methods
Study design and setting
A systematic review and meta-analysis (SRMA) were conducted to assess the partograph utilization in Ethiopians among obstetric caregivers who were in the process of labor follow-up. The study adhered to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines, which consist of checklists that provide guidance for conducting and reporting systematic reviews and meta-analyses (Supplementary Table S1). These guidelines aim to enhance transparency and accuracy in reviews conducted across various disciplines, including medicine (17). Ethiopia, classified as a low-income country, is located in the Horn of Africa and is projected to have a population of 123.4 million in 2022, 133.5 million in 2032, and 1,71.8 million in 2,050. From an administrative perspective, Ethiopia is divided into 11 regions and two city administrations. The regions are further subdivided into zones, and zones are further divided into districts. Finally, districts are divided into kebeles, which represent the smallest administrative divisions and typically have a population ranging from 2,000 to 3,500 residents.
Search strategies and sources of information
We conducted a search in the PROSPERO database (https://www.crd.york.ac.uk/prospero/) to determine if any recently published or ongoing projects exist on the same topic, to avoid unnecessary duplication. Our search revealed that there were no ongoing or published articles related to this specific topic. Therefore, we registered this systematic review and meta-analysis in the PROSPERO database with the ID number CRD42023475818. To gather relevant articles, we conducted a comprehensive literature search using international databases such as PubMed, Google Scholar, Scopus, Web of Science, and HINARI. The search terms we used in this SRMA were as follows: “Prevalence” OR “epidemiology” OR “proportion” AND “associated factor” OR “factors” AND “utilization” OR “utilization of partograph” OR “partograph” AND “obstetric care givers” OR “obstetric care providers” AND “Ethiopia.”
Inclusion criteria
This systematic review and meta-analysis focused on articles that met the specific criteria. We included studies that reported the prevalence or proportion of partograph utilization and the associated factors. Both gray literature and published articles written in the English language were considered. Specifically, we looked for cross-sectional studies that reported the prevalence or proportion of partograph utilization and its associated factors. The time frame for inclusion ranged from 1 September 2013 to 23 October 2023.
Since the SRMA was published on the topic in 2019, there have been inconsistent primary studies conducted in different parts of Ethiopia. This indicates that the SRMA conducted in 2019 does not show the current national figure of parthograph utilization. Therefore, we conducted an SRMA to estimate the current and most recent utilization level of partograph on studies published from 1 September 2013 to 23 October 2023.
Exclusion criteria
In our selection process, we excluded articles that did not have full abstracts or complete texts available. We also excluded case reports, case studies, systematic reviews, meta-analyses, and articles that did not report on the outcome of interest. These exclusion criteria were applied to ensure that we included only relevant and complete studies in our systematic review and meta-analysis.
Outcome of measurement
The first outcome of this systematic review and meta-analysis study focused on partograph utilization. The second outcome of this study aimed to identify the associated factors of partograph utilization.
Data extraction
The datasets were exported to Mendeley Reference Manager, and from there, they were transferred to a Microsoft Excel spreadsheet for further analysis. The first step in the analysis process involved removing any duplicate data from the review. To ensure accurate data extraction, three authors (MA, EL, and BA) independently extracted all the relevant data using a standardized Joanna Briggs Institute (JBI) data extraction format. In cases where there were disagreements between the reviewers, a second team of reviewers (GY, BT, and AZ) was involved to resolve the discrepancies. The resolution process involved critical discussions and evaluations of the articles by an independent group of reviewers. The following information was extracted from the articles: author names, sample size, publication year, study area, region, study design, prevalence of partograph utilization, and adjusted odds ratios with a 95% confidence interval for factors associated with partograph utilization. By following this systematic data extraction process, the study aimed to ensure consistency and accuracy in capturing the relevant information from the selected articles.
Quality assessment
To assess the quality of the included studies, the Newcastle-Ottawa Quality Assessment Scale (NOS) was used for both cross-sectional and case–control study designs (18) (Supplementary Table S2). Three authors (MA, BT, and GY) were responsible for independently assessing the quality of each study. The assessment covered various aspects, including methodological quality, sample selection, sample size, comparability, outcome assessment, and statistical analysis of the study.
In cases where there were disagreements among the three authors during the quality assessment, three additional authors (EL, GG, and BA) were involved. The disagreements were discussed and resolved through thorough deliberation and consensus among the authors. This process ensured that the quality assessment was conducted in a rigorous and comprehensive manner, considering multiple perspectives and expertise among the author team.
Data processing and analysis
The extracted data in Microsoft Excel spreadsheet format was imported into STATA version 11 for analysis. A random-effects model was employed to estimate the pooled prevalence of partograph utilization among obstetric caregivers in Ethiopia. To assess the heterogeneity among the included studies, Cochrane I2 statistics were calculated. The I2 value provides an indication of the percentage of variation across studies that can be attributed to heterogeneity rather than chance.
Based on the I2 values, heterogeneity was categorized as follows: 0%–40% indicating mild heterogeneity, 40%–70% indicating moderate heterogeneity, and 70%–100% indicating considerable heterogeneity (19). A subgroup analysis was conducted based on the study region to explore potential variations in the prevalence of partograph utilization. To examine the potential risk of publication bias, funnel plots and Egger's test were performed (20). The p-value of the Egger's test (0.345) indicated the absence of publication bias, as it was greater than the significance level of 0.05.
The pooled prevalence and pooled adjusted odds ratios (OR) for factors associated with partograph utilization among obstetric caregivers were presented in a forest plot format. The forest plot included the point estimates of prevalence and OR, along with their corresponding 95% confidence intervals (CI). This format allowed for a visual representation of the pooled results and provided a comprehensive overview of the estimates and their precision.
Subgroup and sensitivity analyses
Subgroup analyses were performed based on the study region to examine potential variations in the prevalence of partograph utilization among obstetric caregivers in different regions of Ethiopia. This analysis aimed to explore whether the prevalence estimates differed significantly across different geographical areas.
In addition, sensitivity analysis was conducted to assess the stability and robustness of the pooled estimates to outliers and the potential impact of individual studies on the overall results. Sensitivity analysis helps evaluate the influence of individual studies on the overall findings by systematically excluding one study at a time and reanalyzing the data. This analysis allows for a better understanding of the potential impact of specific studies on the pooled estimates and the overall conclusions of the systematic review and meta-analysis.
Result
Characteristics of the included studies
A total of 661 articles were found using our search strategy in HINARI, Google Scholar, and PubMed databases and repositories since 2013. After removing duplicates (369), 292 articles remained. Subsequently, 198 articles were excluded based on reviewing the titles, and another 49 were excluded based on the abstracts. Full-text papers were then accessed and evaluated for inclusion criteria, leading to the exclusion of 22 more articles based on the aforementioned criteria. Therefore, 23 papers were eligible for inclusion in the final systematic review and meta-analysis (Figure 1). Of the included studies in this SRMA, seven were conducted in Oromia (2, 9, 14, 21–24), six in South Nation Nationality and People Region (SNNPR) (11, 25–29), three in Amhara (30–32), two in Addis Ababa (12, 33) and Tigray (34, 35), and one in Somali (36), Sidama (37), and Dire Dawa (10). All 23 included studies were cross-sectional, involving a total of 7,649 participants, ranging from 127 to 594 participants per study. The studies reported partograph utilization rates of 6.9% to 92.6%. In terms of the quality of included studies, the Newcastle-Ottawa Quality Assessment Scale score for all included studies ranged from 8 to 9, indicating good quality (Table 1).
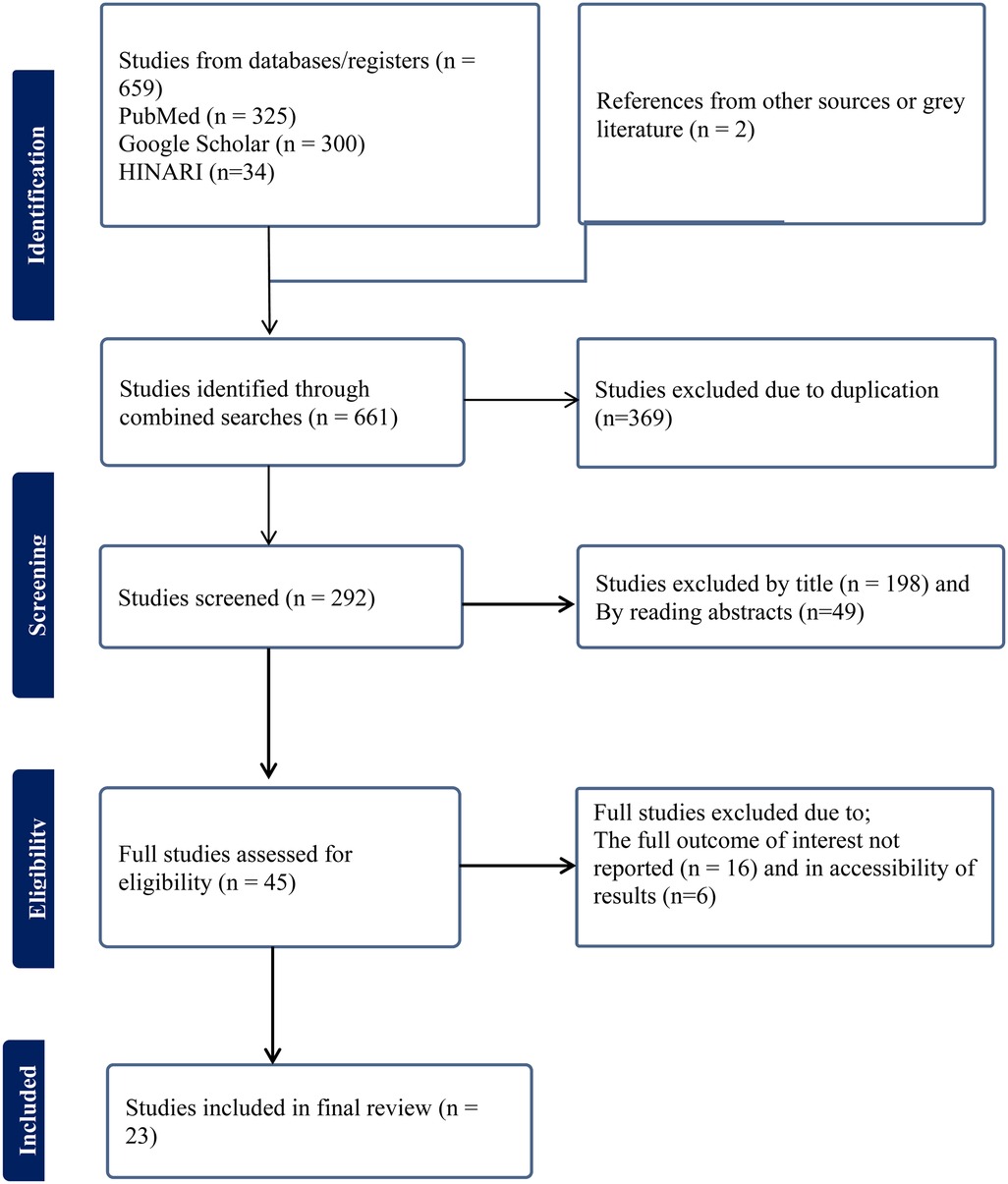
Figure 1. Flowchart of selection for systematic review and meta-analysis on partograph utilization among obstetric caregivers in Ethiopia, 2023.

Table 1. Characteristics of included studies in the systematic review and meta-analysis on utilization of partograph among obstetric caregivers in Ethiopia, 2023.
Pooled prevalence of partograph utilization among obstetric caregivers in Ethiopia
The pooled prevalence of partograph utilization among obstetric caregivers in Ethiopia was 54.92% (CI: 43.38–66.45), with the Cochrane heterogeneity index (I2 = 99.4%, p = 0.000) indicating substantial heterogeneity among different studies (I2 > 70%). Therefore, we used the random-effects model to address the issue of heterogeneity among the included studies. Additionally, we considered subgroup analysis as a potential way of addressing heterogeneity (Figure 2).
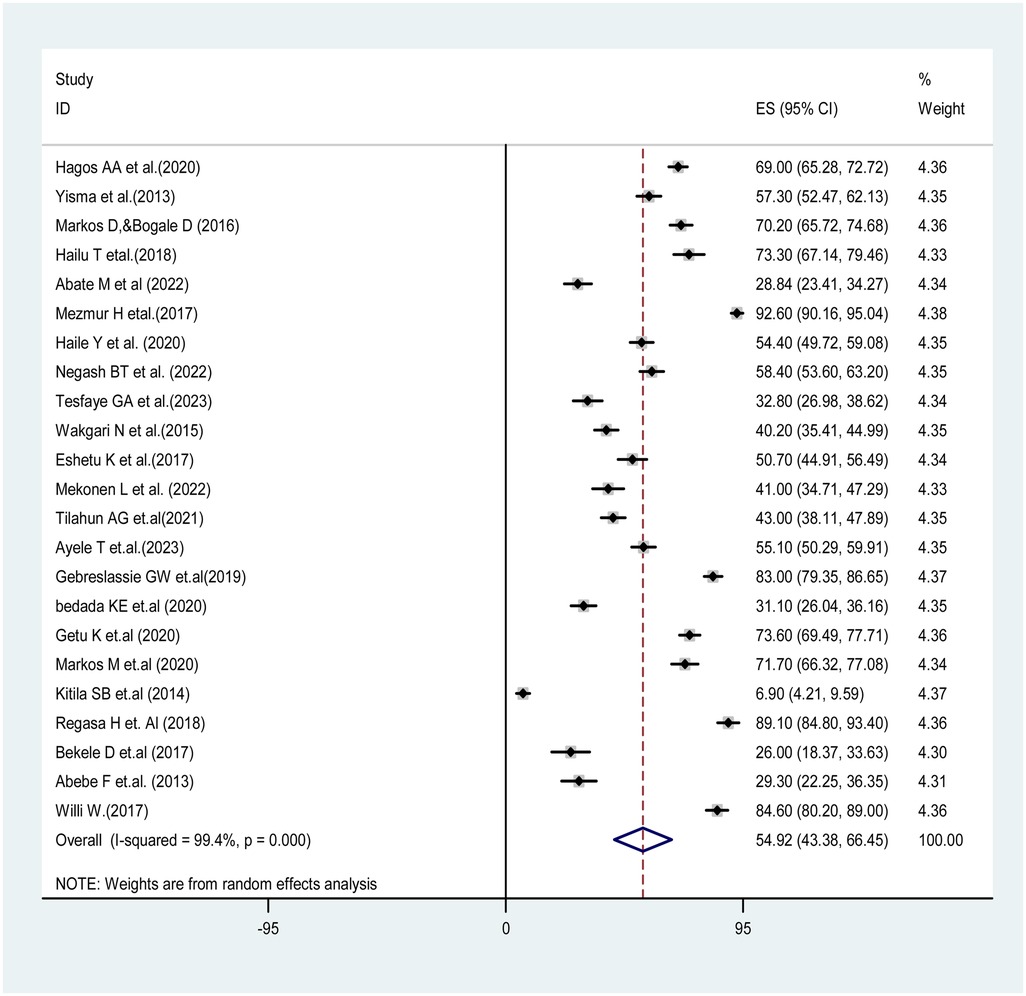
Figure 2. The pooled prevalence of partograph utilization among obstetric caregivers in Ethiopia, 2023.
Subgroup analysis of partograph utilization among obstetric care providers in Ethiopia
In this systematic review and meta-analysis, the finding of subgroup analysis by region showed that the pooled prevalence of partograph utilization among obstetric caregivers was lowest in the Amhara region [32.99%; 95% CI: (25.08–40.91), I2 = 82.8%, p = 0.003], while it was highest in the Dire Dawa region (92.6%; 95% CI: (90.16–95.04), I2 = .%, p = .). These findings suggest regional variations in the prevalence of partograph utilization in Ethiopia, with lower rates observed in the Amhara region and higher rates in the Dire Dawa region. These differences may reflect variations in healthcare practices, resource availability, or other regional factors influencing partograph utilization (Figure 3).
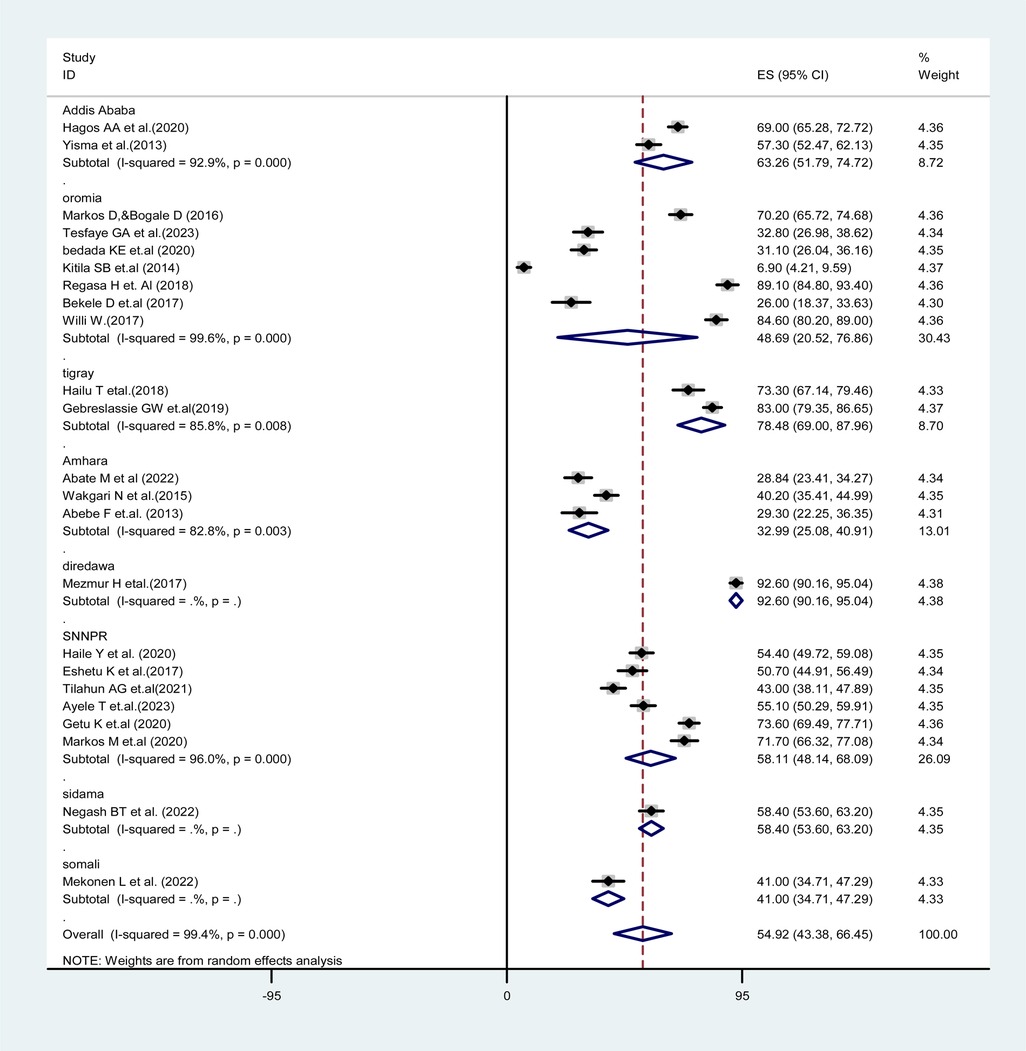
Figure 3. Forest plot showing the subgroup analysis of partograph utilization among obstetric caregivers in Ethiopia, 2023.
Publication bias
In this systematic review and meta-analysis, the presence of publication bias was assessed using a funnel plot and contour-enhancing funnel plot, which visually inspected the asymmetry of the distribution of partograph utilization studies. Additionally, Egger's regression test was conducted, resulting in a p-value of 0.345 (p > 0.05), indicating the absence of publication bias (Figures 4a,b).

Figure 4. (a) Funnel plot for assessing publication bias of the prevalence of partograph utilization among obstetric caregivers in Ethiopia, 2023. (b) Contour funnel plot for assessing the publication bias of the prevalence of partograph utilization among obstetric caregivers in Ethiopia, 2023.
Sensitivity analysis
The results of the random-effects model indicated that the overall pooled prevalence of partograph utilization among obstetric care providers in Ethiopia was influenced by a specific individual study (Figure 5).
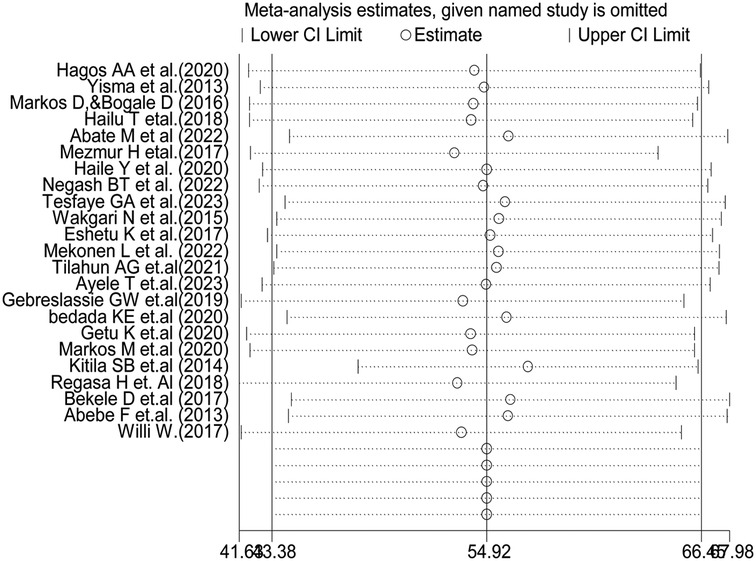
Figure 5. Sensitivity analysis of partograph utilization among obstetric caregivers in Ethiopia, 2023.
Determinants of partograph utilization among obstetric caregivers in Ethiopia
In our systematic review and meta-analysis, several factors were found to be significantly associated with partograph utilization among obstetric care providers in Ethiopia. These factors include receiving partograph training, having good knowledge about the partograph, maintaining a favorable attitude toward partograph utilization, partograph availability, and being in the midwifery profession.
Obstetric care providers who were trained in using the partograph were 3.63 times more likely to utilize the partograph during labor follow-up, starting from the active first stage of labor, compared to their counterparts [adjusted odds ratio (AOR) = 3.63, 95% CI: 2.57–5.25]. Obstetric care providers with good knowledge were 2.63 times more likely to use partograph than those with less knowledge (AOR = 2.63, 95% CI: 1.62–4.26). Similarly, obstetric care providers with a favorable attitude were almost twice as likely to use the partograph compared to those with an unfavorable attitude toward partograph utilization (AOR = 1.95, 95% CI: 1.35–2.82).
The study revealed that participants who had access to the partograph in their health facility were almost 3.89 times more likely to utilize the partograph compared to those without access (AOR = 3.89, 95% CI: 2.24–6.61). Additionally, being in the midwifery profession was associated with almost three times higher odds of using partograph compared to other professions (AOR = 3.09, 95% CI: 1.78–5.25) (Table 2).
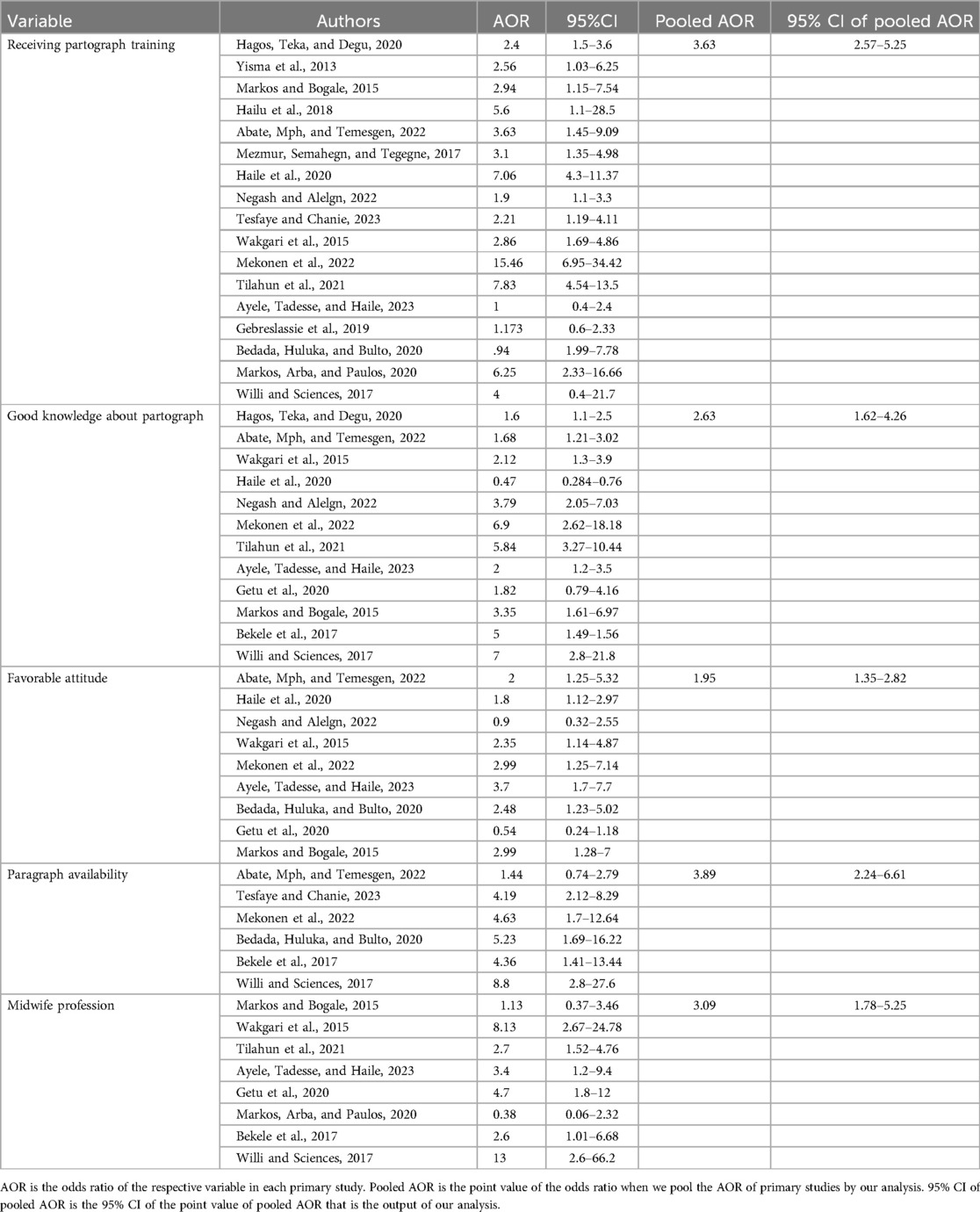
Table 2. Factors associated with partograph utilization among obstetric caregivers in Ethiopia, 2023.
Discussion
A continuous pictorial overview of labor through the partograph alerts midwives and obstetricians to identify and intervene in cases of abnormalities in maternal or fetal conditions, aiming to prevent prolonged labor, obstructed labor, and its complications (33, 38). In this systematic review and meta-analysis, the pooled prevalence of partograph utilization among obstetric caregivers was 54.92% (CI: 43.38–66.45). This finding aligns with a study done at a Regional Hospital in the eThekwini District, which a reported prevalence of 62% (38). However, our review finding was lower than the WHO recommendation, which recommends that all laboring women should be followed using partograph for the well-being of both the mother and the fetus (39). Similarly, this prevalence was lower than in studies conducted in Uganda (69.9%) (40), the Gambia (78%) (41), South Africa (79.4%) (42), and Gazi (89.9%) (43). This disparity can be attributed to differences in sample size, location, availability of the partograph, staffing level and experience, and variations in the implementation of WHO recommendations regarding partograph utilization.
On the other hand, our finding was higher than those of a study conducted in the 2016 National Emergency Obstetric and Newborn Care Survey of Ethiopia (21.5%) (44), Nigeria, (32.3%) (45), and Tanzania (38.7%) (46) another study in Nigeria (22.2%) (47), Malawi (3.9%), Cameron (35%) (48), and northwest and southwest Cameron 32.4% (49). The disparity between these studies and our finding could be attributed to differences in sample size and study period. Our findings represent a pooled prevalence that includes all the latest studies from various regions of the country, while those studies were single-centered with fewer samples, leading to variations in the prevalence of partograph utilization. The variation between the 2016 National Emergency Obstetric and Newborn Care Survey of Ethiopia and our finding is due to difference in study period. Our review includes all studies conducted from 2013 to 2023, capturing changes in obstetric care providers' awareness, attitude, practice, and training regarding partograph utilization. In contrast, the 2016 national survey only includes data from the 12 months preceding the survey (44). This makes difference in prevalence of partograph utilization among obstetric caregivers.
This systematic review and meta-analysis also identified factors that showed a significant association with partograph utilization among obstetric caregivers. Specifically, obstetric care providers who underwent partograph training were 3.63 times more likely to use partograph during labor follow-up starting from the active first stage of labor than their counterparts. This is supported by previous studies done in Gazi (43), Malawi (50), and Uganda (40). This is because training on partograph utilization and its importance enhances knowledge, improves attitude, and enhances skills, thereby increasing partograph utilization.
The current review showed that obstetric care providers with good knowledge were 2.63 times more likely to use the partograph than those with less knowledge. This finding is consistent with previous studies done in Nigeria (51, 52), Enugu Metropolis (53), and Cameron (49). This correlation may be attributed to the fact that effectively using the partograph requires knowledge about when to initiate it, its components, the procedures for its use, and its significance in reducing instances of prolonged and obstructed labor. Therefore, individuals with a strong understanding of these aspects are more likely to utilize the partograph effectively as a tool for monitoring labor, thereby reducing the risk of maternal and neonatal deaths related to prolonged and obstructed labor (53).
In this SRMA, obstetric care providers who had favorable attitudes toward partograph utilization were almost two times more likely to use partograph compared to those who had unfavorable attitudes toward partograph utilization. This finding is consistent with the findings of a previous study conducted in Gazi (43). The possible reason might be that those who had a positive attitude toward the use of partograph were likely committed to using it to monitor feto-maternal conditions starting from the active first stage of labor.
Regarding partograph availability, the study revealed that those participants who had partograph in their health facility were almost four times more likely to utilize partograph compared to those who had no partograph. This finding is supported by a study conducted in Nigeria (51, 52) and Sokoto metropolis in Nigeria (47). This might be due to the availability of partograph which is vital in motivating and encouraging obstetric caregivers to utilize it as a labor monitoring tool from the active first stage of labor.
Being in the midwifery profession was associated with almost three times higher odds of using the partograph compared to other professions. This finding is supported by a previous study conducted in South Africa (54). This could be due to midwives being primarily assigned to labor and intrapartum wards compared to other professionals, which increases their likelihood of receiving training in partograph utilization and motivates them to use the partograph as a labor monitoring tool for making informed decisions.
Limitations and strengths of the study
One of the strengths of this review is that it incorporates both published and unpublished studies, which helps reduce the risk of publication bias. Additionally, a significant number of studies from various regions were included, enhancing the representativeness of the findings. The limitation of this systematic review and meta-analysis is the lack of similar reviews conducted in other countries which makes it challenging to directly compare our findings with those of other studies, necessitating comparisons primarily with individual primary studies.
Conclusion
The prevalence of partograph utilization among obstetric caregivers in Ethiopia was low. Several factors, including on-site partograph training, knowledge about partograph, attitude toward partograph utilization, paragraph availability in the health facility, and being in the midwifery profession were significantly associated with partograph utilization. Based on these findings, on-site training about partograph utilization and its importance related to feto-maternal outcomes should be given to obstetric care providers to increase the knowledge, attitude, and practice of partograph utilization simultaneously. This decreases prolonged and obstructed labor-related maternal and neonatal morbidity and mortality in Ethiopia.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
MA: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. EL: Software, Supervision, Writing – original draft, Writing – review & editing, Validation. GY: Writing – original draft, Writing – review & editing, Software, Supervision. GK: Writing – original draft, Writing – review & editing. BA: Software, Supervision, Writing – original draft, Writing – review & editing. AZ: Software, Supervision, Validation, Writing – original draft, Writing – review & editing. BT: Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank all authors of the primary studies which are included in this systematic review and meta-analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2025.1339685/full#supplementary-material
References
1. WHO. World Health Organization partograph in management of labour. World Health Organization maternal health and safe motherhood programme. Lancet. (1994) 343(8910):1399–404.7910888
2. Markos D, Bogale D. Knowledge and utilization of partograph among health care professionals in public health institutions of Bale zone, Southeast Ethiopia. Public Health. (2016) 137:162–8. doi: 10.1016/j.puhe.2016.02.026
3. Black RE, Laxminarayan R, Temmerman M, Walker N. Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities, Third Edition (Volume 2). Washington, DC: The International Bank for Reconstruction and Development/The World Bank (2016).
4. Kayiga H, Ajeani J, Kiondo P, Kaye DK. Improving the quality of obstetric care for women with obstructed labour in the national referral hospital in Uganda: lessons learnt from criteria based audit. BMC Pregnancy Childbirth. (2016) 16:1–11. doi: 10.1186/s12884-016-0949-1
5. Addisu D, Mekie M, Melkie A, Yeshambel A. Burden of obstructed labor in Ethiopia: a systematic review and meta-analysis. Midwifery. (2021) 95(January):102930. doi: 10.1016/j.midw.2021.102930
6. Gizachew YG, Daniel B, Desta M, Kassa M. Obstructed labor and its effect on adverse maternal and fetal outcomes in Ethiopia: a systematic review and meta-analysis. PLoS One. (2022) 17:e0275400. doi: 10.1371/journal.pone.0275400
7. Lavender T, Cuthbert A, Smyth RMD. Effect of partograph use on outcomes for women in spontaneous labour at term and their babies. Cochrane Database Syst Rev. (2018) 2018(8):CD005461. doi: 10.1002/14651858.CD005461.pub5
8. Fistula Care and Maternal Health Task Force. Revitalizing The Partograph: Does The Evidence Support|A Global Call To Action?—Report of an Export Meeting; 2011 Nov 15–16; New York, NY. New York, NY: EngenderHealth/Fistula Care (2012).
9. Kitila SB, Gmariam A, Molla A, Nemera G. Utilization of partograph during labour and birth outcomes at Jimma University. J Pregnancy Child Health. (2014) 1(101):2. doi: 10.4172/jpch.1000101
10. Mezmur H, Semahegn A, Tegegne BS. Health professional’s knowledge and use of the partograph in public health institutions in eastern Ethiopia: a cross-sectional study. BMC Pregnancy Childbirth. (2017) 17:1–7. doi: 10.1186/s12884-017-1477-3
11. Eshetu K, Hussen E, Dulla D. Magnitude of partograph use and associated factors among obstetric care givers in public health institution in Sidama Zone, Southern Ethiopia, 2017. Divers Equal Heal Care. (2017) 14(6):316–23.
12. Hagos AA, Teka EC, Degu G. Utilization of partograph and its associated factors among midwives working in public health institutions, Addis Ababa City Administration, Ethiopia, 2017. BMC Pregnancy Childbirth. (2020) 20:1–9. doi: 10.1186/s12884-020-2734-4
13. Haile Y, Tafese F, Weldemarium TD, Rad MH. Partograph utilization and associated factors among obstetric care providers at public health facilities in Hadiya Zone, Southern Ethiopia. J Pregnancy. (2020) 2020:1–8. doi: 10.1155/2020/3943498
14. Bedada KE, Huluka TK, Bulto GA. Low utilization of partograph and its associated factors among obstetric care providers in governmental health facilities at West Shoa Zone, Central Ethiopia. Int J Reprod Med. (2020) 2020:1–9. doi: 10.1155/2020/3738673
15. Wakgari N, Tessema GA, Amano A. Knowledge of partograph and its associated factors among obstetric care providers in North Shoa Zone, Central Ethiopia: a cross sectional study. BMC Res Notes. (2015) 8:1–5. doi: 10.1186/s13104-015-1363-x
16. Ayenew AA, Zewdu BF. Partograph utilization as a decision-making tool and associated factors among obstetric care providers in Ethiopia: a systematic review and meta-analysis. Syst Rev. (2020) 9(1):1–11. doi: 10.1186/s13643-020-01505-4
17. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. (2009) 151(4):264–9; W64. doi: 10.7326/0003-4819-151-4-200908180-00135
18. Wells G, Shea B, Robertson J, Peterson J, Welch V, Losos M. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis bias. Ottawa Hosp Res Inst. (2012):1–21. Available online at: http://www.evidencebasedpublichealth.de/download/Newcastle_Ottowa_Scale_Pope_Bruce.pdf
19. Thorlund K, Imberger G, Johnston BC, Walsh M, Awad T, Thabane L, et al. Evolution of heterogeneity (I2) estimates and their 95% confidence intervals in large meta-analyses. PLoS One. (2012) 7(7):e39471. doi: 10.1371/journal.pone.0039471
20. Egger M, Smith GD. Meta-analysis: potentials and promise. Br Med J. (1997) 315(7119):1371–4. doi: 10.1136/bmj.315.7119.1371
21. Regasa H, Tilahun T, Adem H. Utilization of partograph and associated factors among obstetric care givers in hospitals of Western Oromia, Ethiopia, 2017. Panacea J Med Sci. (2018) 8(1):21–4. doi: 10.18231/2348-7682.2018.0005
22. Willi W, Sciences H. Partograph chart use among obstetric caregivers in public health institutions of west Shewa zone, Oromia regional state, Ethiopia, 2015. Ethiop J Reprod Health. (2017) 9(1):36–44. doi: 10.69614/ejrh.v9i1.12
23. Tesfaye GA, Chanie FT, Gemechu EN. Level of partograph utilization and its predictors among obstetrics care givers in Ilu Aba Bor Zone, Southwest Ethiopia. medRxiv [preprint]. (2023). doi: 10.1101/2023.01.20.23284834
24. Bekele D, Beyene K, Hinkosa L, Shemsu MN. Partograph utilization and associated factors among graduating health professional students in Asella Referal and Teaching Hospital, Ethiopia, 2016. Ethiop Sch. (2017):12–8.
25. Haile Y, Tafese F, Weldemarium TD, Rad MH. Research Article Partograph Utilization and Associated Factors among Obstetric Care Providers at Public Health Facilities in Hadiya Zone, Southern Ethiopia. J Comput Biol. (2020) 6(2).
26. Tilahun AG, Gebeyehu DG, Adinew YY, Mengstu FW. Utilization of partograph and its associated factors among obstetric caregivers in public health institutions of southwest Ethiopia. BMC Pregnancy Childbirth. (2021) 21(1):404. doi: 10.1186/s12884-021-03822-5
27. Ayele T, Tadesse S, Haile D. The extent of partograph use and associated factors among obstetric care providers in Government Hospitals in Southern Ethiopia: a cross-sectional study. E-Health Telecommun Syst Netw. (2023) 12(1):1–13. doi: 10.4236/etsn.2023.121001
28. Melese KG, Weji BG, Berheto TM, Bekru ET. Utilization of partograph during labour: a case of Wolaita zone, Southern Ethiopia. Heliyon (2020) 6(August):4–8.
29. Markos M, Arba A, Paulos K. Partograph utilization and associated factors among obstetric care providers working in public health facilities of Wolaita Zone, 2017. J Pregnancy. (2020) 2020:1–8. doi: 10.1155/2020/3631808
30. Abate M, Mph SW, Temesgen K. Parthograph utilization and its determinant factors among health care workers in public health facilities, Dessie town, North East Ethiopia. J Midwifery Reprod Health. (2023) 11(3):3839. doi: 10.22038/JMRH.2023.66133.1928
31. Wakgari N, Amano A, Berta M, Tessema GA. Partograph utilization and associated factors among obstetric care providers in North Shoa Zone, Central Ethiopia: a cross sectional study. Afr Health Sci. (2015) 15(2):552–9. doi: 10.4314/ahs.v15i2.30
32. Abebe F, Birhanu D, Awoke W, Ejigu T. Assessment of knowledge and utilization of the partograph among health professionals in Amhara region, Ethiopia. Sci J Clin Med. (2013) 2(2):26–42. doi: 10.11648/j.sjcm.20130202.11
33. Yisma E, Dessalegn B, Astatkie A, Fesseha N. Knowledge and utilization of partograph among obstetric care givers in public health institutions of Addis Ababa, Ethiopia. BMC Pregnancy Childbirth. (2013) 13(1):1–9. doi: 10.1186/1471-2393-13-17
34. Gebreslassie GW, Weldegeorges DA, Assefa NE, Gebrehiwot BG, Gebremeskel SG, Tafere BB, et al. Utilization of the partograph and its associated factors among obstetric care providers in the Eastern zone of Tigray, Northern Ethiopia, 2017: a cross-sectional study. Pan Afr Med J. (2019) 34(1):4–7. doi: 10.11604/pamj.2019.34.181.18246
35. Hailu T, Nigus K, Gidey G, Hailu B, Moges Y. Assessment of partograph utilization and associated factors among obstetric care givers at public health institutions in central zone, Tigray, Ethiopia. BMC Res Notes. (2018) 11:1–6. doi: 10.1186/s13104-018-3814-7
36. Ayehubizu LM, Tibebeu AT, Fetene MT, Yohannes SH, Yadita ZS. Partograph utilization and associated factors among obstetric care givers in governmental health institutions of Jigjiga and Degehabur towns, Somali region, Ethiopia: a cross- sectional study. PLoS One. (2022) 17:e0264373. doi: 10.1371/journal.pone.0264373
37. Negash BT, Alelgn Y. Proper partograph utilization among skilled birth attendants in Hawassa city public health facilities, Sidama region, Ethiopia, in 2021. BMC Womens Health. (2022) 22(1):539. doi: 10.1186/s12905-022-02117-x
38. Msomi LA. Exploring knowledge, attitudes and utilisation of the partograph by midwives and obstetricians in a regional hospital in the Ethekwini district (thesis). University of Kwazulu Natal, Durban, South Africa (2016).
39. World Health Organization. The Partograph: The Application of The WHO Partograph in the Management of Labour, Report of a WHO Multicentre Study, 1990-1991. Geneva: World Health Organization (1994).
40. Ogwang S, Karyabakabo Z, Rutebemberwa E. Assessment of partogram use during labour in Rujumbura Health Sub District, Rukungiri District, Uganda. Afr Health Sci (2009) 9(1):27–34.
41. Badjie BB, Kao CH, Gua ML, Lin KC. Partograph use among midwives in the Gambia. Afr J Midwifery Womens Health. (2013) 7(2):65–9. doi: 10.12968/ajmw.2013.7.2.65
42. Maphasha OM, Govender I, Motloba DP, Barua C. Use of the partogram by doctors and midwives at Odi District Hospital, Gauteng, South Africa. S Afr Fam Pract. (2017) 59(2):82–6. doi: 10.1080/20786190.2017.1280899
43. Ahmed YN. Knowledge, attitude, and utilization of the partograph among nurses and midwives at labour departments in governmental maternal hospitals in Gaza Strip (MSc thesis). Palestine: Al-Quds University (2020).
44. Gebrehiwot SW, Abrha MW, Weldearegay HG. Health care professionals’ adherence to partograph use in Ethiopia: analysis of 2016 national emergency obstetric and newborn care survey. BMC Pregnancy Childbirth. (2020) 20(1):1–9. doi: 10.1186/s12884-020-03344-6
45. Fawole AO, Hunyinbo KI, Adekanle DA. Knowledge and utilization of the partograph among obstetric care givers in South West Nigeria. Afr J Reprod Health. (2008) 12(1).
46. Peter DE, Millanzi WC, Joho AA. Practice and factors influencing partograph utilization on the delivery of nursing care: an analytical cross – sectional study among nurses in Singida, Tanzania. PREPRINT (Version 1) available at Research Square (2020). doi: 10.21203/rs.3.rs-70920/v1
47. Ango UM, Panti AA, Adamu A. Knowledge and utilization of partograph among primary healthcare workers in Sokoto metropolis, Nigeria. Int Arch Med Health Res Original Article. (2019) 1(3):8–9.
48. Amin ET, Nyiawung FN, Amin ET, Fondungallah JA, Egbe TO. The partogram: knowledge, attitude and use by healthcare providers at two hospitals in the South West Region of Cameroon. Arch Community Med Public Health. (2018) 4:073–7. doi: 10.17352/2455-5479.000041
49. Dingana TN, Angwafo FF. Knowledge and utilization of the partograph: a cross-sectional survey among obstetric care providers in urban referral public health institutions in northwest and southwest. (2017) 71:1–14. doi: 10.1371/journal.pone.0172860
50. Mandiwa C, Zamawe C. Documentation of the partograph in assessing the progress of labour by health care providers in Malawi’s South-West zone. Reprod Health. (2017) 14:1–7. doi: 10.1186/s12978-017-0401-7
51. Adesola O, Omolola I, Adekemi O, Audu O. Partograph utilization at three levels of health care delivery services inIle-ife, Nigeria. Int J Caring Sci. (2014) 7(2):678.
52. Ojong IN. Knowledge and utilization of partograph in labor monitoring among nurses and midwives in a tertiary health facility in South-South Nigeria. Afr J Biomed Res (2021) 24(1):59–64.
53. Ada N, Okafor E. Evaluation of factors affecting the utilization of partograph by nurses/midwives in primary/secondary health facilities in Enugu Metropolis. Gynecol Obstet. (2017) 7:2–5. doi: 10.4172/2161-0932.1000446
Keywords: partograph, partograph utilization, systematic review, systematic review and meta-analysis, Ethiopia
Citation: Ayele M, Lake ES, Yilak G, Kumie G, Abate BB, Zemariam AB and Tilahun BD (2025) Utilization of partograph and associated factors among obstetric caregivers in Ethiopia: a systematic review and meta-analysis. Front. Glob. Womens Health 6:1339685. doi: 10.3389/fgwh.2025.1339685
Received: 21 February 2024; Accepted: 2 January 2025;
Published: 27 January 2025.
Edited by:
Stephen Kennedy, University of Oxford, United KingdomReviewed by:
Dejen Tsegaye, Debre Markos University, EthiopiaTemesgen Lera Abiso, Wolaita Sodo University, Ethiopia
Copyright: © 2025 Ayele, Lake, Yilak, Kumie, Abate, Zemariam and Tilahun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mulat Ayele, YXltdWxhdDI5QGdtYWlsLmNvbQ==
†Present Address: Biruk Beletew Abate,School of Population Health, Curtin University, WA, Australia
 Mulat Ayele
Mulat Ayele Eyob Shitie Lake
Eyob Shitie Lake Gizachew Yilak
Gizachew Yilak Getinet Kumie3
Getinet Kumie3 Biruk Beletew Abate
Biruk Beletew Abate Alemu Birara Zemariam
Alemu Birara Zemariam