- 1Department of Midwifery, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 2Department of Anesthesia, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 3Department of Medical Laboratory, College of Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 4Department of Public Health, College of Health Science, Debre Tabor University, Debre Tabor, Ethiopia
- 5Department of Environmental Health, Debre Tabor Health Science Collage, Debre Tabor, Ethiopia
- 6Department of Midwifery, College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia
Background: Prenatal vitamin and mineral supplements are commonly advised as clinical practice standard of care. In spite of Ethiopian government focus on maternal nutrition programmes targeting pregnant and lactating women, Micronutrient deficiencies are still quite common and are regarded as a serious public health issue and also little is known regarding utilization and barriers to prenatal vitamin use during pregnancy. This study aimed to assess utilization and associated factors of prenatal vitamins among pregnant women attending antenatal care at public hospitals in the south Gondar zone, 2024
Methods: Multi center crossectional study design was conducted among 416 pregnant women from March 1 to May 30, 2024. Systematic sampling technique was used to select the study participants. Data was collected using Interviewer administered questionnaire. After data, SPSS version 26 software was used for analysis. Factors associated with utilization of prenatal vitamins were identified using bi-variable and multi variable logistic regression models. Statistical significance was declared at 95%CI and p-value < 0.05.
Result: In this study, we found that 87.5% (95% CI: 84.31, 90.34) of pregnant women did not use prenatal vitamins. Women not having formal education (AOR = 2.72, 95%CI: 1.44–5.15), being unplanned pregnancy (AOR = 2.58, 95%CI: 1.76–3.78), husband being decision maker in health care (AOR = 1.71, 95%CI:1.09–2.68), having poor knowledge (AOR = 3.27, 95%CI: 1.44–7.42) and unfavorable attitude (AOR = 3.63, 95%CI: 1.61–8.18) on prenatal vitamins were significantly associated with non-users of prenatal vitamins.
Conclusion: The proportion of non-users of prenatal vitamin were higher. Educational level of women, pregnancy plan, decision on health care, knowledge and attitude on prenatal vitamins had statistically significant with utilization of prenatal vitamins. Developing and implementing targeted educational programs to increase awareness about the importance and benefits of prenatal vitamins and encouraging women to take an active role in their healthcare decisions is recommended to improve the utilization of prenatal vitamins.
Introduction
Pregnancy-related changes in physiology and homeostatic regulation result in an increase in micronutrient requirements (1, 2). Pregnant and childbearing women may not be able to achieve their demands for micronutrients like iron and calcium by food alone, even though increased nutrient consumption should ideally come from food sources (3). Pre-conception folic acid supplementation is recommended by the 2017 Neural Tube Defect Practice Bulletin from the American College of Obstetricians and Gynecologists (ACOG), as it has been demonstrated to lower the incidence and recurrence of neural tube defects (4). However, folic supplementation alone is not enough to cover nutritional gaps. For females of reproductive age, prenatal vitamins are approved as a nutritional supplement during preconception, pregnancy, or breastfeeding (5). Prenatal vitamins are advantageous for both the mother and fetus. The increased micronutrient demands of pregnancy can be addressed, as can dietary inadequacies more generally, with the use of multiple micronutrient supplements (MMS), which comprise 15 crucial vitamins and minerals (6).
Despite the lack of a standard formulation for prenatal vitamins, the United Nations Children's Fund (UNICEF), the United Nations University, and the World Health Organization (WHO) established the International Multiple Micronutrient Antenatal Preparation (UNIMMAP) formulation, which is regarded as the standard for components (7).
The recommended intakes of prenatal vitamins include niacin (18 mg), folic acid (400 µg), copper (2 mg), selenium (65 µg), iodine (150 µg), 30 mg of iron, and 15 mg of zinc for pregnant women. Additional recommended intakes of vitamins B1 (1.4 mg), B2 (1.4 mg), B6 (1.9 mg), B12 (2.6 mg), C (70 mg), D (200 IU), and E (10 mg) are also provided (7–9). The primary source of summary evidence on the effects of MMS was the 2015 Cochrane review, which comprised 17 trials involving 137,791 women. The analysis demonstrated that MMS decreased the risk of low birth weight, being born small for gestational age, and stillbirth (9).
Pregnancy diets high in fish have been demonstrated to be especially advantageous for the Intelligence Quotient (IQ) (intellectual capacity) of the baby (10, 11). However, all pregnant women may not access fish products. One of the key elements is iodine, which has been demonstrated to be beneficial when combined with prenatal vitamins. Children born to iodine-deficient mothers had lower verbal and reading Intelligence Quotient (IQ) scores (12). Recent studies showed that children born from women who had taken prenatal vitamins containing vitamin B12 had improved speech, mathematical abilities and memories (13, 14). In addition, prenatal vitamins have tremendous effect on the reduction of autism spectrum disorder (ASD) in childhood (15, 16). Children whose mothers took prenatal vitamins during the first month of pregnancy had a 14.1% prevalence of autism spectrum disorder, compared to 32.7% in children whose mothers did not take prenatal vitamins during that period (17).
In spite of Ethiopian government focus on maternal nutrition programmes targeting pregnant and lactating women (18), micronutrient deficiencies are still quite common and are regarded as a serious public health issue (19). In 2016, the Ethiopian demographic and health (EDHS) survey found that 23% of pregnant women were anemic (20). Studies showed that 59.9% of pregnant women in Ethiopia were found to be zinc-deficient (21), 23% were vitamin B12-deficient (22) and 68.68% were iodine deficient (23).
Despite prenatal vitamin and mineral supplements are commonly advised as clinical practice standard of care, little is known regarding utilization and barriers to prenatal vitamin use during pregnancy in Ethiopia. Therefore, this study aimed to assess utilization and associated factors of prenatal vitamins among pregnant women attending antenatal care at public hospitals in the south Gondar zone.
Methods and materials
Study design, setting, and period
A multi-center, institution-based cross-sectional study was conducted among clients attending antenatal care at selected public hospitals in the south Gondar zone, Ethiopia, from March 1 to May 30, 2024. The south Gondar zone is one of the ten administrative zones in the Amhara region, Ethiopia. Debre Tabor town is the capital city of south Gondar zone. The town is located approximately 669 km northwest of Addis Ababa, the capital city of Ethiopia, and 97 km southwest of Bahir Dar, the capital city of the Amhara region. It has an elevation of 2,706 m above sea level. According to the 2022 population projection, Debre Tabor town has a total population of 125,312, with 64,322 males and 60,990 females. Addis Zemen Hospital, Debre Tabor Comprehensive Specialized Hospital, Mekaneyesus Hospital, and Tesfaye Getachew Memorial Hospital were randomly selected among the ten public hospitals in the south Gondar zone.
Source and study population: All pregnant women who were attended antenatal care at south Gondar zone public hospitals were the source population for this study. Whereas, selected pregnant women who were attended antenatal care at the selected public hospitals during data collection periods were the study population.
Inclusion and Exclusion criteria: The inclusion criteria were pregnant mothers who were attended antenatal care at selected public hospitals during the study period. Women who were seriously ill, unable to hear and/or speak during data collection period were excluded from the study.
Sample size and sampling procedure
The sample size was determined using a single population proportion formula using a 50% proportion because no previous research had been done in Ethiopia. P = 50%, 10% non-response rate, 5% margin of error, and 95% confidence interval. After adding 10% non-response rate, 423 study participants were finally taken into account. Simple random sampling was used to choose the study hospitals. To choose the study subjects, systematic random selection was used. First, we determine the approximate number of women who have used antenatal care within the last three months for the selected facilities. The number of antenatal attendees in each selected hospitals were 567 in Debre Tabor comprehensive specialized hospital, 393 in Addis Zemen hospital, 386 in Mekaneyesus hospital and 346 in Tesfaye Getachew memorial hospital with a total of 1,692. The Kth intervals were calculated by dividing total number of attendees for the total sample size (1,692/423 = 4). The first study participant was selected via lottery method from 1 up to 4 which was 3. Finally, every 3rd pregnant women were interviewed until total sample size was reached (Figure 1).
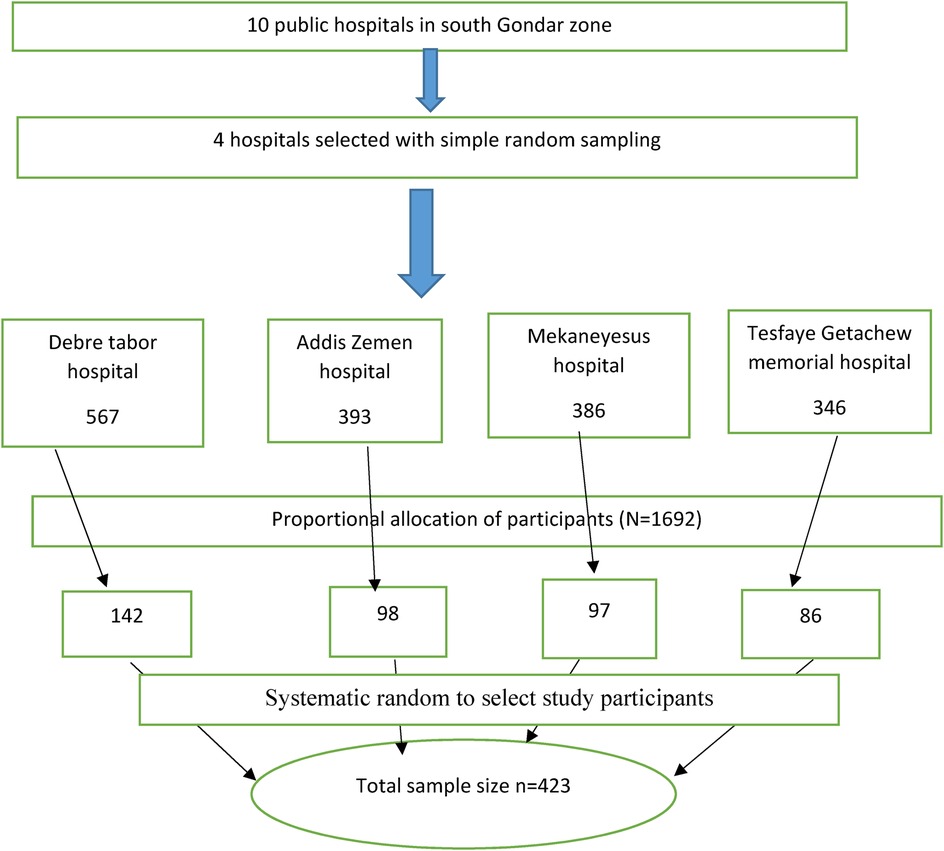
Figure 1. Schematic presentation of the sampling procedure at south Gondar zone public hospitals 2024.
Variables of the study
Dependent variable
Prenatal vitamin use: yes no
Independent variables
Socio demographic and economic characteristics
Age, religion, educational level of women, educational level husband/partner/, marital status, residency, family size, head of house hold, decision on health care, income generator (the one who earns income in the family).
Reproductive and health service related factors
Gravidity, parity, pregnancy planned or not, hours to reach health institution, means of transportation, gestational age when antenatal care started.
Knowledge and attitude
Good knowledge and poor knowledge.
Favorable attitude and unfavorable attitude.
Operational definitions
Prenatal vitamin utilization: it was measured by asking women whether they have used prenatal vitamins before conception or during pregnancy. Then it was considered as users of prenatal vitamin if the response was yes for one of two questions, otherwise non-users.
Knowledge on prenatal vitamins: women who scored above the median score (≥3) were classified as having good knowledge otherwise they were considered as poor knowledge (<3).
Attitude towards prenatal vitamins: women who scored above the median score (≥2) were classified as having favorable attitude otherwise they were considered as unfavorable attitude (<2).
Data collection tools and procedures
Validated semi-structured questionnaires from prior studies were used (24–27). The tool was initially prepared in English. To ensure uniformity, this questionnaire was translated into Amharic and then back into English by a different translator. The data were collected by five diploma midwives at the exit of antenatal care service. Two bachelor degree midwives supervised the data collection process, which involved conducting in-person interviews with participants using a semi-structured questionnaire that the interviewer administered. Two days training was given for data collectors and supervisors. Pretest was done on 5% of sample size.
Quality assurance
To make sure the data was of high quality, a half-day tool discussion with the authors was conducted. To ensure data quality, the supervisors and data collectors underwent comprehensive training on how and what information to collect from the specific data sources. The questionnaires were checked for accuracy and missing information before the data was collected. The principal investigator and supervisors swiftly offered input and checked the completeness of the data each day as it was being collected. The primary investigator cleaned the data before beginning the analysis. A pre-test was conducted 1 week prior to the start of the actual data collection at Megbaru Kebede memorial hospital. Subsequently, the questionnaire was assessed for its length, lucidity, and comprehensiveness, and any requisite modifications were implemented based on the findings.
Data processing and analysis
Data entry and coding were done using EpiData version 3.1 software. The entered data were exported into the Statistical Package for Social Science (SPSS) version 26 software for further analysis. The analysis process includes several steps. First, basic descriptive statistics such a frequency distribution and percentages were used to describe the respondents' demographic, socioeconomic, and obstetric aspects. Second, a bivariate logistic regression was performed, pairing each independent variable with the outcome variable. If the bivariate test of a variable yielded a p-value of less than 0.2, it was considered a possible candidate for the multivariable model. Following the determination of the variables, multivariable analysis was performed. To determine whether the data was appropriate for multiple logistic regression analysis, the Hosmer and Lemeshow goodness-of-fit test was used (p = 0.27). Multicolliniarity was checked and there was no Multicolliniarity between independent variables. A multivariable logistic regression model was ultimately developed in order to determine distinct factors of prenatal vitamin utilization. The crude and adjusted odds ratios, as well as the corresponding 95% confidence intervals, were computed to assess the strength of the association. For all two-sided tests, a statistical significance level of P < 0.05 was employed.
Results
Socio demographic and economic characteristics
In this study, 416 pregnant women participated with response rate of 98.34%. The mean age of the women were 25.8(SD ± 4.62). Among 416 pregnant women, 382 (91.83) of them were orthodox Christians. More than half (53.13%) of principal income generator of the household were husbands (Table 1).
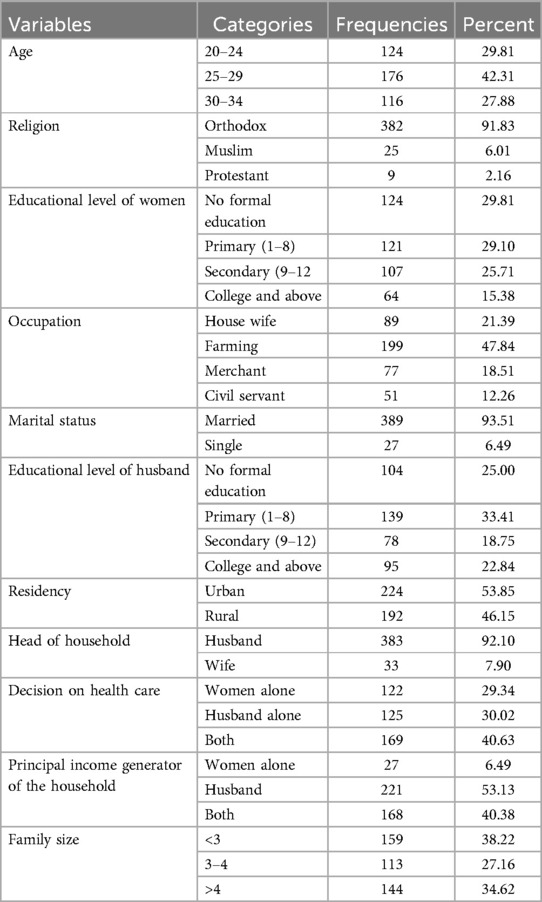
Table 1. Socio demographic and economic characteristics of pregnant women attending antenatal care at south Gondar zone public hospitals, 2024 (N = 416).
Reproductive and health service related factors
More than half (55.04%) of pregnant women were multigravida. Two hundred fifty five (61.25%) of participants reaches to health institution with in 1 h of travel. From the total of study participant, 59.13% of them started antenatal care at second trimester (Table 2).
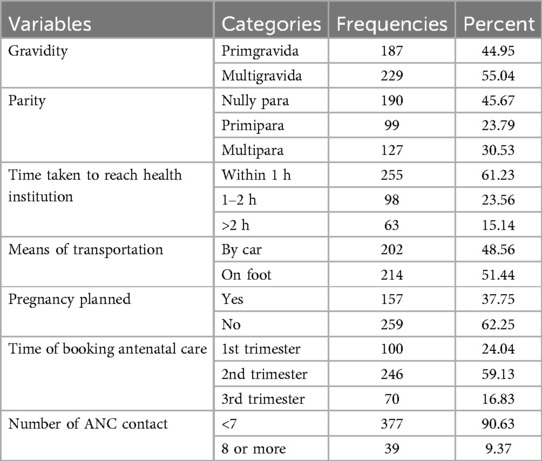
Table 2. Reproductive and health service related factors of pregnant women attending antenatal care at south Gondar zone public hospitals, 2024 (N = 416).
Knowledge and attitude on prenatal vitamin
Among the total respondents, 242 (58.17%) of had no ever heard about prenatal vitamins. Nearly one quarter (25.25%) and 23.56% of study participants had good knowledge and favorable attitude respectively (Table 3).
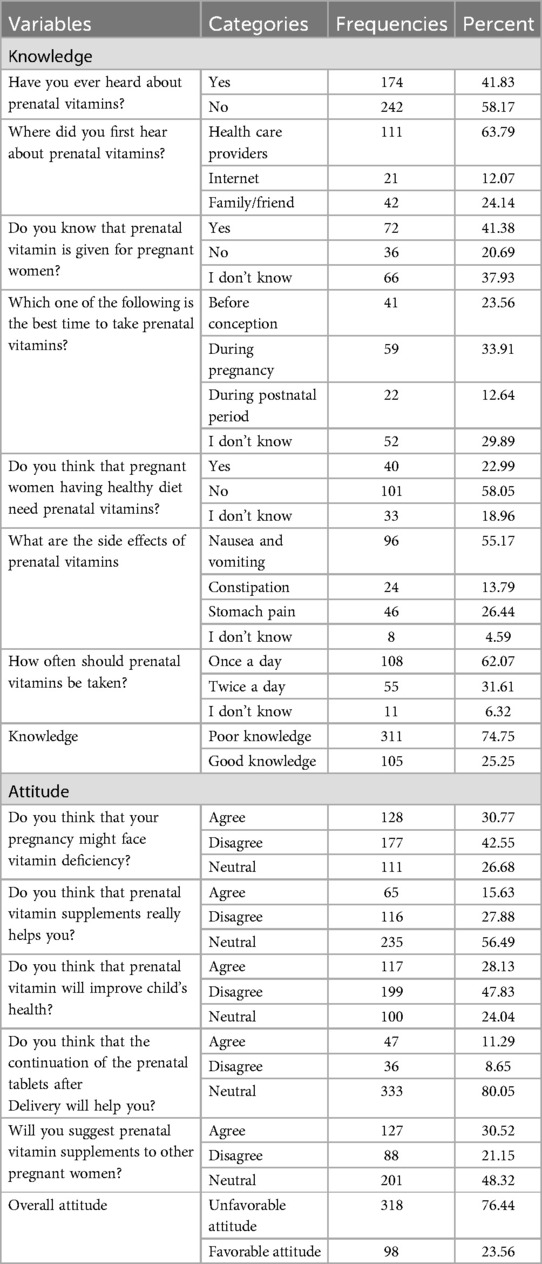
Table 3. Knowledge and attitude on prenatal vitamin of pregnant women attending antenatal care at south Gondar zone public hospitals, 2024 (N = 416).
Utilization of prenatal vitamins
In this study, we found that 87.5% (95% CI: 84.31, 90.34) of pregnant women didn't use prenatal vitamins (Figure 2).
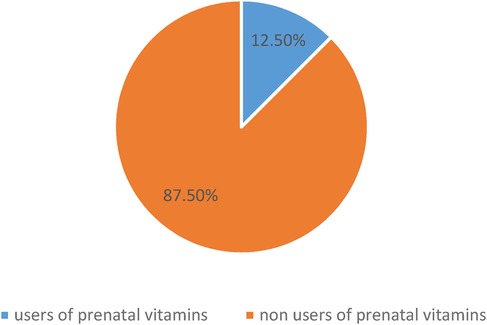
Figure 2. Utilization of prenatal vitamins among pregnant women attending antenatal care at south Gondar zone public hospitals, 2024 (N = 416).
Reasons for not using prenatal vitamins
From the total study participants, 178(48.9%) of them listed absence of information on prenatal vitamins as the reason for not using it (Figure 3).
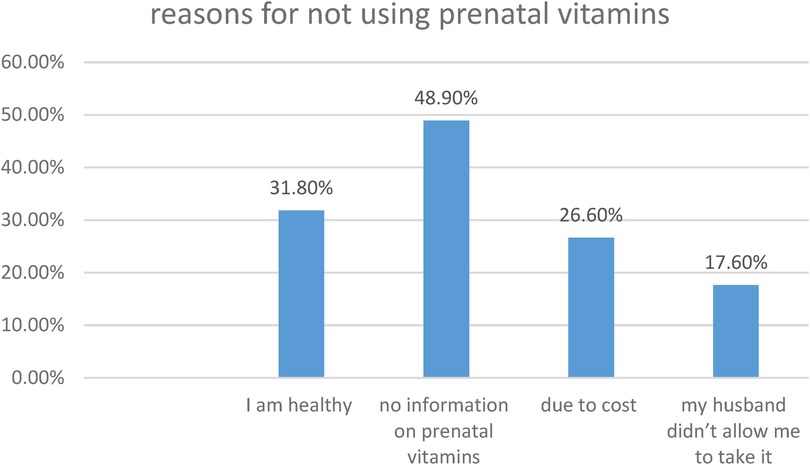
Figure 3. Reasons for non-utilization of prenatal vitamins among pregnant women attending antenatal care at south Gondar zone public hospitals, 2024 (N = 416).
Factors associated with utilization of prenatal vitamins
Age of women, educational status, residency, gravidity, pregnancy planned, decision on health care, knowledge and attitude on prenatal vitamins were candidate variables for multivariable logistic regression analysis.
Women not having formal education were 2.72 times higher to be non-users of prenatal vitamin compared with women whose educational level were college and above (AOR = 2.72, 95%CI: 1.44–5.15). Non-users of prenatal vitamins were 2.58 times higher among unplanned pregnancy compared with planned pregnancy (AOR = 2.58, 95%CI: 1.76–3.78). The odds of being non-users of prenatal vitamins were 1.71 times higher among women whose husband were decision maker in health care compared with women who decide alone (AOR = 1.71, 95%CI:1.09–2.68). Women who had poor knowledge (AOR = 3.27, 95%CI: 1.44–7.42) and unfavorable attitude (AOR = 3.63, 95%CI: 1.61–8.18) on prenatal vitamins were less likely to take it compared with their counter parts (Table 4).
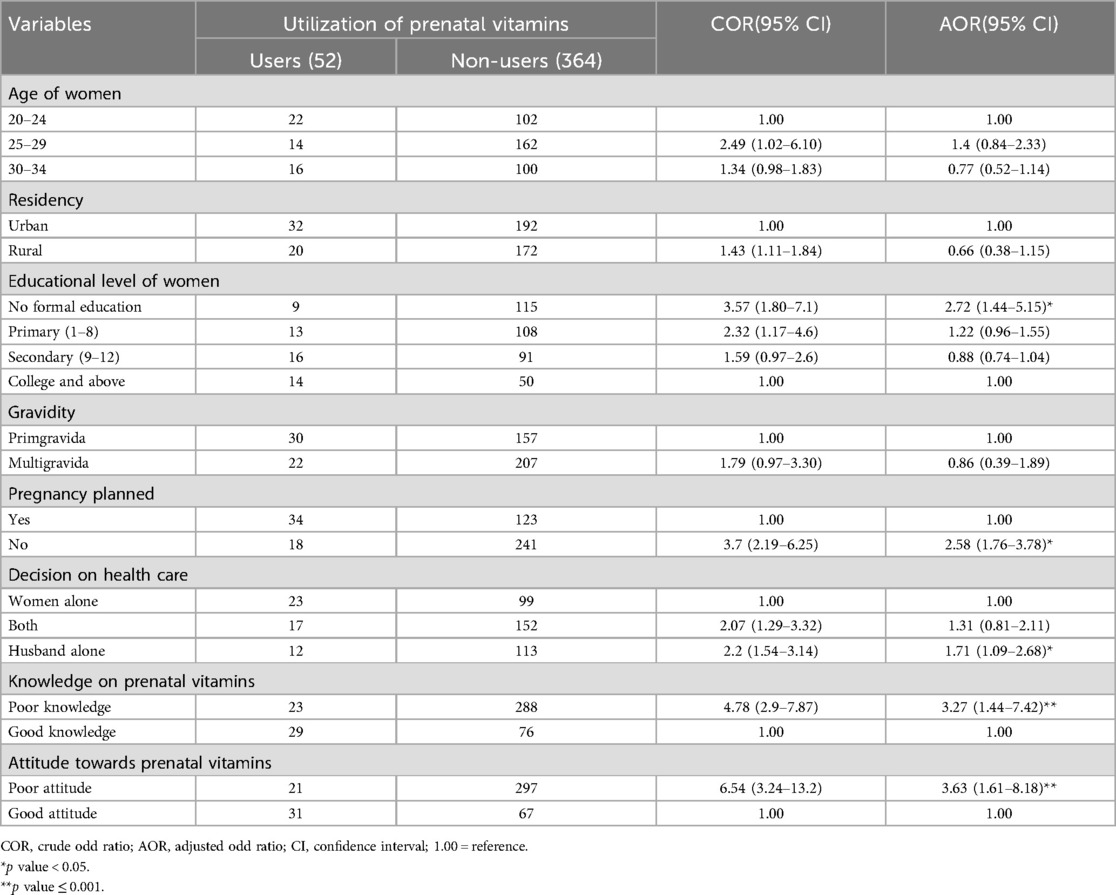
Table 4. Bi-variable and multivariable logistic regression analysis of factors associated with utilization of prenatal vitamins among pregnant women attending antenatal care at south Gondar zone public hospitals, 2024 (N = 416).
Discussion
During pregnancy, prenatal vitamins are essential for maintaining the best possible health for both the mother and the foetus. These dietary supplements are intended to supply essential minerals and vitamins that promote healthy fetal development and to address nutritional deficits. Even with the established advantages of prenatal vitamins, there are still differences in their use across various groups. To improve mother and child health outcomes, it is imperative to design effective public health initiatives that take into account the factors influencing prenatal vitamin use.
In this study, we found that 87.5% of pregnant women were not used prenatal vitamins. It was very higher compared with studies done in Bangladesh 50.23% (25), United States 22% (28) and Florida 47.1% (29). Various factors might contribute to this huge difference. The first reason could be economic factor (30). Since prenatal vitamins are not covered with health insurance or maternal exempted service in Ethiopia, women might not afford for such supplementation rather they prioritize for food and shelter. In addition, civil war between Amhara and Ethiopian military defense force hinders the accessibility of health care (31). Secondly, presence of cultural beliefs which masks modern medical advice might reduce the utilization of prenatal vitamins in developing countries like Ethiopia (32). In some cultures, there may be a preference for natural remedies over synthetic vitamins, affecting utilization.
Educational level of women was one of significant factor affecting prenatal vitamin utilization. Women not having formal education were 2.72 times higher to be non-users of prenatal vitamin compared with women whose educational level were college and above. Similar study done in United States also showed the association between educational level and prenatal vitamin utilization (28). The possible justification could be women not having formal education may not understand the importance of prenatal vitamins because they did not access health information through various channels, such as books and internet (33). Uneducated women might not have better job opportunities and economic stability, which can make it difficult for women to afford prenatal vitamins (34). Another potential reason might be that women not having formal education may have low influence in household decision-making regarding health, including the purchase and use of nutritional supplements (35).
Our study showed that non-users of prenatal vitamins were higher among unplanned pregnancy compared with planned pregnancy. Women who had no plan to be pregnant may not have preconception care (36). If women did not have preconception care, they might not get nutritional information including prenatal vitamins from health care providers which leads to low utilization. Women who are actively trying to conceive usually have a positive outlook towards pregnancy, which can motivate them to take care of their health and adhere to recommended vitamin regimens (37). On the other hand, women who had no plan to conceive may not adhere to nutritional recommendations which makes them for low utilization of prenatal vitamins.
The odds of being non-users of prenatal vitamins were 1.71 times higher among women whose husband were decision maker in health care compared with women who decide alone. This difference might be related with resource allocation. Financial resources may be allocated differently in marriages where men control healthcare decisions. If spouses put other medical costs prior to prenatal vitamins, their wives may not use prenatal vitamins (38). The wife's behaviour may be influenced by her husband's views on maternal health and pregnancy. Lower utilization may result from his lack of support or knowledge regarding the advantages of prenatal vitamins (39).
Knowledge of pregnant women on prenatal vitamins was one of the factor affecting prenatal vitamin utilization. Women who had poor knowledge on prenatal vitamins were less likely to take it compared with their counter parts. It was supported with other study in Florida (29). The reason might be due to absence of information on prenatal vitamins (40). In addition there may be misunderstanding of the role of prenatal vitamins for their baby and themselves that leads to low utilization.
Women with unfavorable attitude towards prenatal vitamins were more likely to be non-users of the supplement compared to those with a positive attitude. This difference may be due to the belief that a balanced diet alone can meet all their nutritional needs, leading them to see no need for additional supplementation.
Policy and practical implications of the study
The results of this study highlight the need for laws governing public health to encourage pregnant women to take prenatal multivitamins, especially in groups where nutrient deficiencies are more likely to occur. Policy makers ought to think about launching educational initiatives that increase the knowledge of prenatal multivitamins. Incorporating prenatal multivitamin supplements in to current maternal health initiatives can also help guarantee that all women have access to vital nutrients, which will lower the prevalence of unfavorable pregnancy outcomes linked to deficiencies. Healthcare professionals should give special attention to talking about the usage of prenatal multivitamins. This entails clearing up any misunderstandings regarding the advantages of vitamins and minerals and offering precise instructions on the kinds required for optimum pregnancy wellness. Additionally, by collaborating with pharmacies and community health organizations, healthcare systems can make it easier for people to obtain reasonably priced prenatal multivitamins. We can improve maternal care and promote healthier pregnancies by implementing these measures, which will eventually benefit women and their offspring.
Strength and limitation of the study
Being multi-center is one of the strength of the study since it increases the representativeness of the population. At the start of the interview, participants were assured that their responses would be kept entirely anonymous, which helped to minimize the desirability bias. However, absence of adequate literatures on the area makes it difficult to compare and discuss.
Conclusion
This study concluded that the proportion of non-users of prenatal vitamin were higher. Educational level of women, pregnancy plan, decision on health care, knowledge and attitude on prenatal vitamins had statistically significant with utilization of prenatal vitamins. Developing and implementing targeted educational programs to increase awareness about the importance and benefits of prenatal vitamins is needed to increase the utilization. These programs can be integrated into existing maternal health services and tailored to different educational levels to ensure accessibility and understanding. In addition, encouraging women to take an active role in their healthcare decisions by providing them with comprehensive information on prenatal vitamins and supporting them in making informed choices is also the pillar area to improve the utilization of prenatal vitamins.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the study was carried out after receipt of an ethical clearance letter from Debre Tabor University's institutional ethical review committee with reference number DTU/126/2024. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BM: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. DA: Formal Analysis, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. WY: Conceptualization, Investigation, Software, Writing – original draft, Writing – review & editing. FS: Data curation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. AM: Conceptualization, Funding acquisition, Investigation, Resources, Software, Writing – original draft, Writing – review & editing. TB: Conceptualization, Formal Analysis, Investigation, Project administration, Software, Validation, Writing – original draft, Writing – review & editing. TS: Data curation, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing. HW: Writing – review & editing, Software, Supervision, Validation, Visualization, Writing – original draft. ST: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Writing – original draft, Writing – review & editing. NG: Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. AM: Formal Analysis, Funding acquisition, Software, Supervision, Writing – original draft, Writing – review & editing. MA: Conceptualization, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. TM: Funding acquisition, Investigation, Project administration, Writing – original draft, Writing – review & editing. YY: Data curation, Funding acquisition, Investigation, Validation, Writing – original draft, Writing – review & editing. RA: Funding acquisition, Methodology, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing. AD: Formal Analysis, Investigation, Resources, Visualization, Writing – original draft, Writing – review & editing. FG: Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing. GB: Conceptualization, Funding acquisition, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing. HA: Funding acquisition, Resources, Software, Visualization, Writing – original draft, Writing – review & editing. AA: Formal Analysis, Project administration, Validation, Writing – original draft, Writing – review & editing. YG: Data curation, Formal Analysis, Funding acquisition, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. BB: Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal Analysis, Investigation, Methodology.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We are thankful to Debre Tabor University for giving us ethical clearance. We are also grateful to the data collectors; women participated in the data collection, hospital managers, health professionals, and all individuals who were willing to support us in any kind.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1474928/full#supplementary-material
Abbreviations
ANC, antenatal care; AOR, adjusted odds ratio; ACOG, American College of Obstetricians and Gynecologists; COR, crude odds ratio; CI, confidence interval; MMS, multiple micronutrient supplements; UNICEF, United nations children's fund; WHO, World Health Organization.
References
1. Pregnancy CoNSD, Lactation. Nutrition During Pregnancy: Part I: Weight Gain, Part II: Nutrient Supplements. National Academies Press (1990).
2. Picciano MF. Pregnancy and lactation: physiological adjustments, nutritional requirements and the role of dietary supplements. J Nutr. (2003) 133(6):1997S–2002. doi: 10.1093/jn/133.6.1997S
3. Turner RE, Langkamp-Henken B, Littell RC, Lukowski MJ, Suarez MF. Comparing nutrient intake from food to the estimated average requirements shows middle-to upper-income pregnant women lack iron and possibly magnesium. J Am Diet Assoc. (2003) 103(4):461–6.12669009
4. Dillon CM, Ennen CS, Bailey KJ, Thagard AS. ACOG Practice Bulletin No. 187. Neural tube defects. Obstet Gynecol. (2017) 130(6):e279–90. doi: 10.1097/AOG.0000000000002412
5. Prenatal multivitamins and minerals. Revision date November 13, 2020. Available online at: https://www.clinicalkey.com/pharmacology/ (accessed January 7).
6. Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. (2013) 382(9890):452–77. doi: 10.1016/S0140-6736(13)60996-4
7. Tuncalp Ö, Rogers LM, Lawrie TA, Barreix M, Peña-Rosas JP, Bucagu M, et al. WHO recommendations on antenatal nutrition: an update on multiple micronutrient supplements. BMJ Specialist J. (2020) 5:e003375.
8. Organization WH. The Global Prevalence of Anaemia in 2011. World Health Organization (2015). 2015.
9. Oh C, Keats EC, Bhutta ZA. Vitamin and mineral supplementation during pregnancy on maternal, birth, child health and development outcomes in low-and middle-income countries: a systematic review and meta-analysis. Nutrients. (2020) 12(2):491. doi: 10.3390/nu12020491
10. Hibbeln JR, Davis JM, Steer C, Emmett P, Rogers I, Williams C, et al. Maternal seafood consumption in pregnancy and neurodevelopmental outcomes in childhood (ALSPAC study): an observational cohort study. Lancet. (2007) 369(9561):578–85. doi: 10.1016/S0140-6736(07)60277-3
11. Bramante CT, Spiller P, Landa M. Fish consumption during pregnancy: an opportunity, not a risk. JAMA Pediatr. (2018) 172(9):801–2. doi: 10.1001/jamapediatrics.2018.1619
12. Bath SC, Steer CD, Golding J, Emmett P, Rayman MP. Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: results from the avon longitudinal study of parents and children (ALSPAC). Lancet. (2013) 382(9889):331–7. doi: 10.1016/S0140-6736(13)60436-5
13. Golding J, Gregory S, Clark R, Iles-Caven Y, Ellis G, Taylor CM, et al. Maternal prenatal vitamin B12 intake is associated with speech development and mathematical abilities in childhood. Nutr Res. (2021) 86:68–78. doi: 10.1016/j.nutres.2020.12.005
14. Cruz-Rodríguez J, Canals-Sans J, Hernández-Martínez C, Voltas-Moreso N, Arija V. Prenatal vitamin B12 status and cognitive functioning in children at 4 years of age: the ECLIPSES study. Matern Child Nutr. (2024) 20(1):e13580. doi: 10.1111/mcn.13580
15. Levine SZ, Kodesh A, Viktorin A, Smith L, Uher R, Reichenberg A, et al. Association of maternal use of folic acid and multivitamin supplements in the periods before and during pregnancy with the risk of autism spectrum disorder in offspring. JAMA Psychiatry. (2018) 75(2):176–84. doi: 10.1001/jamapsychiatry.2017.4050
16. Brieger KK, Bakulski KM, Pearce CL, Baylin A, Dou JF, Feinberg JI, et al. The association of prenatal vitamins and folic acid supplement intake with odds of autism spectrum disorder in a high-risk sibling cohort, the early autism risk longitudinal investigation (EARLI). J Autism Dev Disord. (2022) 52(6):2801–11. doi: 10.1007/s10803-021-05110-9
17. Mayor S. Prenatal vitamins in early pregnancy may lower risk of autism in high risk families. BMJ. (2019) 364.
18. National Nutrition Program—Ministry of Health. Available online at: http://www.nipn-nutrition-platforms.org/Ethiopia (cited April 2019).
19. Harika R, Faber M, Samuel F, Kimiywe J, Mulugeta A, Eilander A. Micronutrient status and dietary intake of iron, vitamin A, iodine, folate and zinc in women of reproductive age and pregnant women in Ethiopia, Kenya, Nigeria and South Africa: a systematic review of data from 2005 to 2015. Nutrients. (2017) 9(10):1096. doi: 10.3390/nu9101096
20. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF (2016).
21. Berhe K, Gebrearegay F, Gebremariam H. Prevalence and associated factors of zinc deficiency among pregnant women and children in Ethiopia: a systematic review and meta-analysis. BMC Public Health. (2019) 19:1–11. doi: 10.1186/s12889-019-7979-3
22. Gibson RS, Abebe Y, Stabler S, Allen RH, Westcott JE, Stoecker BJ, et al. Zinc, gravida, infection, and iron, but not vitamin B-12 or folate status, predict hemoglobin during pregnancy in southern Ethiopia. J Nutr. (2008) 138(3):581–6. doi: 10.1093/jn/138.3.581
23. Kabthymer RH, Shaka MF, Ayele GM, Malako BG. Systematic review and meta-analysis of iodine deficiency and its associated factors among pregnant women in Ethiopia. BMC Pregnancy Childbirth. (2021) 21:1–11. doi: 10.1186/s12884-021-03584-0
24. Saini S, Hasan N. A survey of multivitamin supplement knowledge, attitude, and use in the urban community of bikaner, rajasthan. CHRISMED J Health Res. (2015) 2(4):329–32. doi: 10.4103/2348-3334.165743
25. Kraemer K, Beesabathuni K, Askari S, Khondker R, Khan TU, Rahman M, et al. Knowledge, attitudes and practices of pregnant women and healthcare providers in Bangladesh regarding multivitamin supplements during pregnancy. Healthcare. (2023) 11.36900718
26. Tsegai MB, Berhe AH, Tesfaezgi SB, Weldemariam DG, Petros KT, Weldetinsae HB, et al. Knowledge, attitude, and practice regarding supplemental iron and folic acid amongst women delivering in Edaga-Hamus community hospital: a cross-sectional study in Asmara, Eritrea. Int J Women’s Health. (2023):1593–609. doi: 10.2147/IJWH.S419813
27. Goswami M, Dadwani R, Koringa H, Vekariya D, Solanki N. A cross-sectional study on knowledge, attitude and practice regarding the use of iron–folic acid supplementation amongst antenatal women of Surendranagar district. NMO J. (2023) 17(2):72–6. doi: 10.4103/JNMO.JNMO_5_23
28. Sullivan KM, Ford ES, Azrak MF, Mokdad AH. Multivitamin use in pregnant and nonpregnant women: results from the behavioral risk factor surveillance system. Public Health Rep. (2009) 124(3):384–90. doi: 10.1177/003335490912400307
29. Darbhanga P, McManus K. Investigating the Adherence of Maternal Prenatal Vitamin Supplementation in Sarasota, Florida (2024).
31. Alene GD, Ayenew GM, Bantie GM, Zeru T, Yismaw G. Impact of war on maternal health services in the war affected areas of the Amhara region, Ethiopia: disruption of antenatal care, institutional delivery and postnatal services. Ethiop J Transl Sci. (2023) 1(1).
32. de Diego-Cordero R, Rivilla-Garcia E, Diaz-Jimenez D, Lucchetti G, Badanta B. The role of cultural beliefs on eating patterns and food practices among pregnant women: a systematic review. Nutr Rev. (2021) 79(9):945–63. doi: 10.1093/nutrit/nuaa119
33. Lee HY, Jin SW, Henning-Smith C, Lee J, Lee J. Role of health literacy in health-related information-seeking behavior online: cross-sectional study. J Med Internet Res. (2021) 23(1):e14088. doi: 10.2196/14088
34. Gauly B, Lechner CM. Self-perfection or self-selection? Unraveling the relationship between job-related training and adults’ literacy skills. PLoS One. (2019) 14(5):e0215971. doi: 10.1371/journal.pone.0215971
35. Blasch J, Boogen N, Daminato C, Filippini M. Empower the consumer! Energy-related financial literacy and its implications for economic decision making. Econ Energy Environ Policy. (2021) 10(2):149–80. doi: 10.5547/2160-5890.10.2.jbla
36. Callegari LS, Ma EW, Schwarz EB. Preconception care and reproductive planning in primary care. Med Clin. (2015) 99(3):663–82.
37. El-Atar E, FMNED S, Hafez SKM. Comparison between planned versusun planned pregnancy out comes. Nov J. (2021) 8(1):40–9.
38. Rizkianti A, Afifah T, Saptarini I, Rakhmadi MF. Women’s decision-making autonomy in the household and the use of maternal health services: an Indonesian case study. Midwifery. (2020) 90:102816. doi: 10.1016/j.midw.2020.102816
39. Nguyen PH, Frongillo EA, Sanghvi T, Wable G, Mahmud Z, Tran LM, et al. Engagement of husbands in a maternal nutrition program substantially contributed to greater intake of micronutrient supplements and dietary diversity during pregnancy: results of a cluster-randomized program evaluation in Bangladesh. J Nutr. (2018) 148(8):1352–63. doi: 10.1093/jn/nxy090
Keywords: prenatal, multivitamins, pregnancy, preconception, supplementation
Citation: Mekuriaw BY, Addisu D, Yazie Ferede W, Sisay FA, Mitiku Ak, Belachew TW, Seid Yimer T, Wubet HB, Tadesse SG, Gobezie NZ, Mebratie AF, Alachew MK, Mengistu TD, Yiregu YZ, Arage RB, Dessie AM, Gebeyehu FG, Bishaw Mekonen G, Alemayehu HD, Ayalew AB, Goshu YA and Berihun Erega B (2025) Prenatal vitamin utilization and its determinants among pregnant women in south Gondar zone: multicenter cross-sectional study. Front. Glob. Womens Health 5:1474928. doi: 10.3389/fgwh.2024.1474928
Received: 18 October 2024; Accepted: 11 December 2024;
Published: 6 January 2025.
Edited by:
Olutosin Ademola Otekunrin, University of Ibadan, NigeriaReviewed by:
Ewunetie Mekashaw Bayked, Wollo University, EthiopiaHabtamu Bekele, Haramaya University, Ethiopia
Copyright: © 2025 Mekuriaw, Addisu, Yazie Ferede, Sisay, Mitiku, Belachew, Seid Yimer, Wubet, Tadesse, Gobezie, Mebratie, Alachew, Mengistu, Yiregu, Arage, Dessie, Gebeyehu, Bishaw Mekonen, Alemayehu, Ayalew, Goshu and Berihun Erega. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Begizew Yimenu Mekuriaw, YmVnaXpld3lpbWVudUBnbWFpbC5jb20=
 Begizew Yimenu Mekuriaw
Begizew Yimenu Mekuriaw Dagne Addisu
Dagne Addisu Wassie Yazie Ferede
Wassie Yazie Ferede Fillorenes Ayalew Sisay1
Fillorenes Ayalew Sisay1 Assefa kebie Mitiku
Assefa kebie Mitiku Tegegne Wale Belachew
Tegegne Wale Belachew Tigist Seid Yimer
Tigist Seid Yimer Alemie Fentie Mebratie
Alemie Fentie Mebratie Temesgen Dessie Mengistu
Temesgen Dessie Mengistu Yonas Zenebe Yiregu
Yonas Zenebe Yiregu Anteneh Mengist Dessie
Anteneh Mengist Dessie Geremew Bishaw Mekonen
Geremew Bishaw Mekonen Yitayal Ayalew Goshu
Yitayal Ayalew Goshu Besfat Berihun Erega
Besfat Berihun Erega