- 1Department of Medical Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Department of Pediatric and Child Health Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 3Department of Surgical Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 4Department of Community Health Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 5Department of Emergency and Critical Care Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Termination of pregnancy is one of the biggest five causes of maternal mortality in countries with low and middle incomes. Although termination of pregnancy is hazardous, its prevalence and determinates are not well studied in developing countries. Therefore, this study aims to assess the prevalence and determinants of termination of pregnancy among reproductive-age women who had a short preceding birth interval in Sub-Saharan Africa.
Methods: Data from the most recent Demographic and Health Surveys, which covered 21 Sub-Saharan African countries from 2015 to 2022, were used for secondary data analysis. The study used a total of 283,785 women. Stata 14 was used to analyze the data. The determinants of termination of pregnancy were determined using a multilevel mixed-effects logistic regression model. Significant factors associated with termination of pregnancy were declared significant at p-values < 0.05. The result was interpreted using the confidence interval and adjusted odds ratio. The best-fit model was determined to be the one with the highest log likelihood ratio and the lowest deviance.
Results: In Sub-Saharan Africa, one in ten women with short birth intervals experienced pregnancy termination. Individual factors, including the sex of the preceding birth (AOR = 1.21, 95% CI: 1.05, 1.40), maternal age (AOR = 1.57, 95% CI: 1.27, 1.95), pregnancy complications (AOR = 1.28, 95% CI: 1.09, 1.49), No ANC visits (AOR = 2.29, 95% CI: 1.26, 4.14), previous cesarean section delivery (AOR = 1.74, 95% CI: 1.32, 2.30), <6 months of breastfeeding (AOR = 1.56, 95% CI: 1.35, 1.81), traditional contraception usage (AOR = 1.67, 95% CI: 1.13, 2.46), poor wealth status (AOR = 1.50, 95% CI: 1.22, 1.85), and community-level factors such as urban residence (AOR = 1.31, 95% CI: 1.06, 1.62) had higher odds of pregnancy termination.
Conclusions: This study concludes that termination of pregnancy rates among women with short preceding birth interval is high. The study identified that both individual and community-level variables were determinants of termination of pregnancy. Therefore, the ministries of health in Sub-Saharan African countries should give attention to those women who underutilize antenatal care services and to women from urban areas while designing policies and strategies targeting reducing termination of pregnancy rates.
Introduction
The World Health Organization (WHO) defines an abortion as the termination of a pregnancy, whether induced or spontaneous, before 20 weeks of gestation (1). Termination of pregnancy is one of the biggest five causes of maternal mortality in countries with low and middle incomes (2). Globally, an estimated 73 million induced abortions have been carried out annually. Six out of 10 (61%) of all unintended pregnancies, and 3 out of 10 (29%) of all pregnancies, end in induced abortion (1, 3).
Short birth intervals are particularly concerning for maternal health as they increase risks of maternal depletion, insufficient recovery time, and heightened susceptibility to adverse outcomes in subsequent pregnancies (4). Short intervals limit time for physiological recuperation, which can lead to complications such as anemia, malnutrition, and heightened risk of uterine rupture, preterm birth, and maternal mortality (5). Evidence suggests that these intervals strain maternal health resources, impacting both physical and mental health recovery. Additionally, closely spaced pregnancies can exacerbate socioeconomic stressors, particularly in resource-limited settings, compounding health risks (6).
Nearly two thirds of termination of pregnancy occurs in developing countries. In Asia, particularly in south and central Asia, unsafe abortions account for more than half of all abortions undertaken (7). The World Health Organization (WHO) defines unsafe abortions as procedures for terminating unintended pregnancies that are carried out either by individuals lacking the necessary skills or in environments that do not conform to minimal medical standards, or both (8, 9). The WHO's recent definition emphasizes that unsafe abortions are a significant but preventable cause of maternal deaths and morbidities, particularly in developing countries where 97% of unsafe abortions occur. Most terminations of pregnancy (about three out of four) are potentially hazardous in Latin America and Africa. The least safe conditions are used for over half of all abortions in Africa (9). An estimated 55.9 million abortions are performed each year, 49.3 million of which take place in developing countries (10).
The prevalence of pregnancy termination practices varies across country, with 3.1% in western Africa and 3.8% in northern Africa (11, 12). Thirty-seven deaths per 100,000 live births in Sub-Saharan Africa account 13% of all maternal deaths worldwide, and are specifically associated with abortions (13). Termination of pregnancy rates remain high in developing countries, especially in Sub-Saharan Africa (SSA), where abortion is legally limited, despite being lower in developed countries where abortion laws have been liberalized and safe abortion services are freely accessible (14, 15). In Sub-Saharan Africa, 77% of abortions are unsafe because they are handled by unskilled individuals and use non-recommended methods. As of 2019, the region experienced about 6.2 million unsafe abortions annually, which have a detrimental effect on people, families, and healthcare systems.
The studies carried out in different parts of the world revealed that termination of pregnancy was significantly associated with women's age (16, 17), residence (18, 19), poor wealth index (20), use of substance (21), educational level (22, 23). Even though the WHO provides global technical and policy guidance on the use of contraception to prevent unintended pregnancy and abortion, maternal deaths related to abortion remain high in developing countries, especially in Sub-Saharan Africa.
Sub-Saharan African countries are actively working to improve family planning services to prevent unintended pregnancies and reduce the need for pregnancy termination. For instance, Angola is investing $500K USD annually to improve access for young people (24). Benin aims to raise its modern contraceptive prevalence rate to 25% by 2022 (25), while Burundi targets a substantial increase to 60% by 2030 (26). Ethiopia has made remarkable progress, reaching a 41% contraceptive rate (27), and Kenya envisions zero unmet needs by 2030 (28).
Despite the above efforts, maternal mortality and morbidity are still highly related to reproductive health. As far as our search of the literature and knowledge is concerned, there has been no study conducted on termination of pregnancy among women who had a short birth interval in Sub-Saharan Africa, a large sample from DHS data. Therefore, this study used multilevel mixed effect analysis of the most recent Demographic and Health Survey to investigate the prevalence and predictors of pregnancy termination among women who had short birth intervals in Sub-Saharan Africa.
Materials and methods
Study setting
The Sub-Saharan region of Africa is the part of the continent that is located south of the Sahara and consists of four large and diverse regions, including Eastern Africa, Central Africa, Western Africa, and Southern Africa. The region is tremendously diversified, consisting of low, lower-middle, upper-middle, and wealthy countries. The region constitutes an area of 9.4 million square miles and an estimated number of 407 million by 2030 and then 607 million by 2050 of reproductive-age women (29, 30). This study was conducted based on the recent DHS survey data from twenty one Sub-Saharan African countries such as Angola, Benin, Burundi, Cameron, Ethiopia, Gabon, Gambia, Guinea, Kenya, Liberia, Mali, Malawi, Nigeria, Rwanda, Senegal, Sera lion, Tanzania, Uganda, South Africa, Zambia, and Zimbabwe. Based on the World Bank's income classifications for the fiscal year 2024, those countries are categorized as: low-income countries: Burundi, Ethiopia, Gambia, Guinea, Liberia, Mali, Malawi, Sierra Leone, Tanzania, Uganda, and Zimbabwe (31). Lower-middle-income countries: Angola, Benin, Cameroon, Kenya, Nigeria, Rwanda, Senegal, Zambia (31). Upper-middle-income countries: Gabon, South Africa (31).
Study design and period
A mixed-effect cross-sectional study with a community-based approach has been carried out. A multilevel mixed effect analysis was undertaken using data from 21 Sub-Saharan African countries for a recent DHS survey that took place between 2015 and 2022. Part of the global Demographic and Health Survey, the Demographic and Health Survey (DHS) is a 5-year national survey project that uses pretested, validated, and structured instruments. A 7-year sample of DHS data (beginning in 2015) was obtained for each region of Sub-Saharan African countries in order to obtain a representative sample of recent data. Large sample sizes are used in these population-based, nationally representative surveys of every country.
Population and eligibility criteria
Reproductive age women who are 15–49 years old and who had short birth interval in Sub-Saharan African countries were the source population. The study population was all the reproductive age women who were in the selected enumeration areas included in the analysis. Women who are not within the reproductive age range as defined by the study. Participants who did not have a short preceding birth interval, according to the study's specific definition of “short”, Survey responses that are incomplete or missing crucial data for the multilevel mixed-effects logistic regression analysis, data from women who did not consent to the use of their information for research purposes were excluded from this study.
Data source and sampling procedure
To gain insight into pregnancy termination and determinates among women who had a short preceding pregnancy interval, 21 Sub-Saharan countries' DHS surveys were combined. Numerous datasets are used in each country's survey, including data on important health indicators like disease, mortality, use of family planning services, fertility, and access to maternity and child health care. Using a stratified two-stage cluster design, the Demographic and Health Survey first creates the enumeration areas and then generates a sample of households from each enumeration area in the second stage. The dependent and independent variables for each country were extracted using the individual record dataset (IR file) for this study and the data were subsequently appended using STATA. The outcome variable (termination of pregnancy) was generated by recoding the variables “ever had a terminated pregnancy” (v228) from the individual record (IR) data set. The study included a weighted sample of 283,785 women of reproductive age with a short interval between births (Table 1).
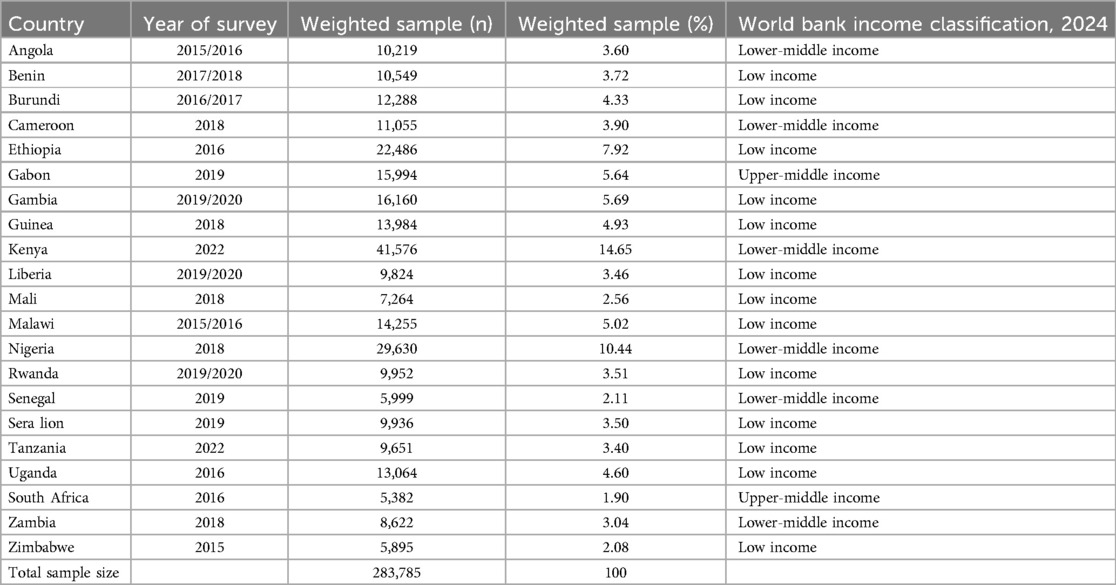
Table 1. Sample size for prevalence and determinants of termination of pregnancy among reproductive age women who had short preceding birth interval in Sub-Saharan Africa, DHS 2015–2022.
Study variables
Dependent variables
Pregnancy termination was the study's outcome variable, and it was generated from the individual record (IR) data set. The response option for the outcome variable “Have you ever had a terminated pregnancy” was binary: “Yes” meant the woman had had an abortion, and “No” meant she hadn't during the study period (32, 33).
Short birth interval
A short birth interval takes place when two consecutive live births occur less than 33 months apart. In following WHO guidelines, a non-short birth interval was defined as a previous birth interval greater than 33 months. By subtracting the first child's birthdate from the second child's birthdate, the birth interval was computed (34, 35).
Independent variables
Two sources of independent variables (individual and community-level variables) were included for this analysis because DHS data are hierarchical in nature. The individual-level independent variables were: sex of preceding birth (male, female) Sex of household head (male, female), Maternal age (15–24, 25–34, 35–49), Maternal educational status (no formal education, primary, secondary, higher), Husband educational status (no formal education, primary, secondary, higher), Religion (Orthodox, Catholic, Protestant, Muslim, Others), Maternal employment (no working, governmental employee, self-employee), marital status of the mother (unmarried, married, ever married), pregnancy complications (no, yes), number of ANC visits (no visit, 1–3, ≥4), total children ever born (≤3, 4–6, 7–9, >9), duration of breastfeeding (<6 months, ≥6 months), usage of contraception(yes, no), type of contraception used (not used, modern, traditional), household wealth index (poor, middle, rich), distance to health facility (big problem, not big problem), household media exposure (no, yes), smoking (no, yes), drinking alcohol (no, yes), previous mode of delivery (vaginal, caesarean section), type of current pregnancy (single, multiple). The community-level variables were place of residence (urban or rural), community-level women's illiteracy (low or high), community-level poverty (low or high), community-level media exposure (low or high), and community-level ANC utilization (low or high) (Figure 1).
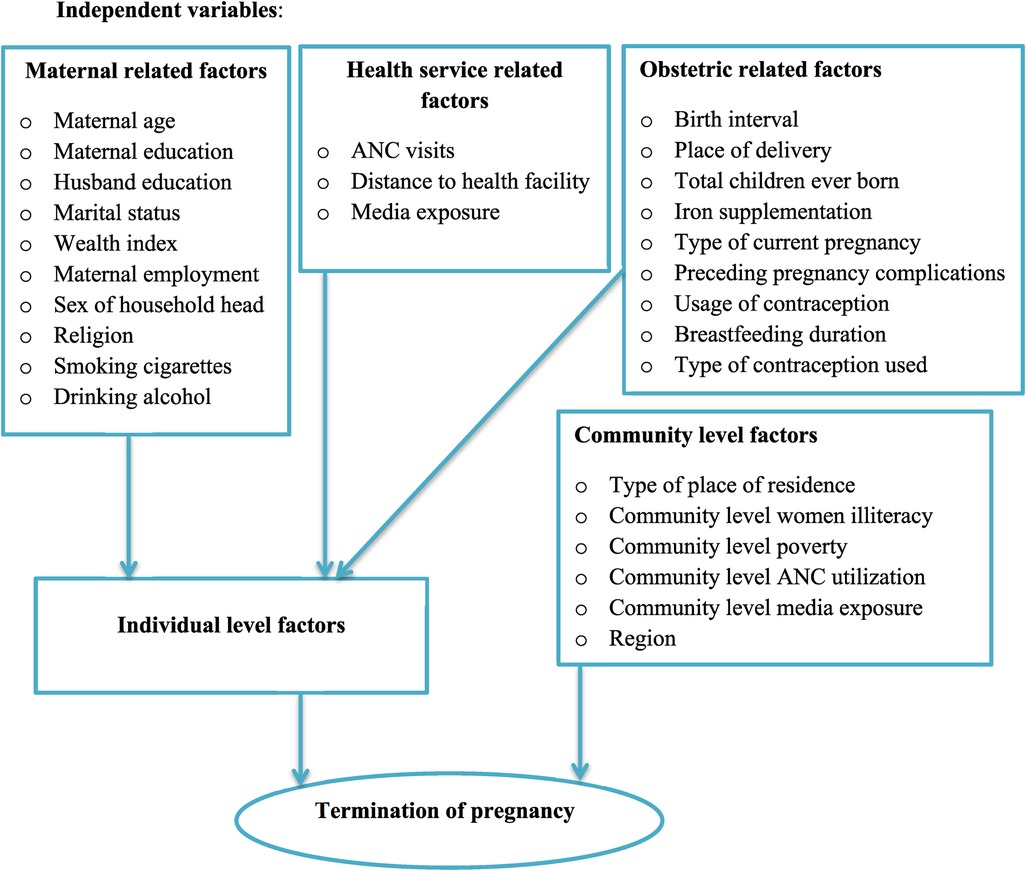
Figure 1. Conceptual framework for individual and community level factors associated with of termination of pregnancy among reproductive-age women who had short preceding birth interval in Sub-Saharan Africa.
Data processing and statistical analysis
Statistical software (STATA/SE) version 14 was used to clean, record, and analyze the data once it had been extracted from recent DHS data sets. Prior to conducting any statistical analysis, the data were weighted using the sampling weight, primary sampling unit, and stratum in order to restore the survey's representativeness and account for the sampling design when computing standard errors to produce accurate statistical estimations. We used the weighting variable (v005) as a relative weight normalized to make the analysis survey-specific, while for the pooled data, we denormalized reproductive age women's individual standard weight variable by dividing the women's individual standard weight by the sampling fraction of each country: (women adjusted weight = V005× (total women aged 15–59 years in the country at the time of the survey)/(number of women aged 15–59 years in the survey).
The assumptions of standard logistic regression model such as independence observations and equal variance are broken due to the hierarchical nature of the DHS data. Mothers, for example, are nested within clusters, and we believe that those who participated in one cluster may have similar characteristics to those in another, which goes against the equal variance and independence assumptions between clusters in the ordinal logistic regression model. This implies that accounting for between-cluster effects requires the use of a complex model. In light of this, multilevel mixed-effects logistic regression was applied to identify the variables associated with pregnancy termination. Multilevel mixed effect logistic regression uses four models: the null model (outcome variable only), model I (only individual level variables), model II (only community level variables), and model III (both individual and community level variables).
The null model, which lacks independent variables, was employed to investigate the variation in abortion rates within the cluster. Evaluations were conducted on the relationships between the outcome variable (Model I) and the factors at the individual and community levels (Model II). The association between the community- and individual-level variables and the outcome variable was fitted simultaneously in the final model (Model III). To manage potential confounding, a multivariable analysis has been performed. To mitigate multicollinearity issues the Variance Inflation Factor (VIF) for all independent variables has been conducted and we have systematically removed those with VIF values exceeding 10. Additionally, we set a criterion for including variables in the final model at a p-value threshold of < 0.25. Applying a binary logistic regression model, the variables associated with termination of pregnancy were identified. Factors associated with pregnancy termination were expressed as an adjusted odds ratio (AOR) with a 95% significance threshold. In multivariable logistic regression, all variables with p values <0.05 were deemed statistically significant.
Random effects
Random effects or measures of variation such as Likelihood Ratio test (LR), Intra-class Correlation Coefficient (ICC), and Median Odds Ratio (MOR) were computed to measure the variation of abortion across clusters. Taking clusters as a random variable, the ICC quantifies the degree of heterogeneity of termination of pregnancy between clusters (the proportion of the total observed variation in termination of pregnancy that is attributable to between cluster variations) (36) is computed as; . The Median Odds Ratio (MOR) is the median value of the odds ratio which quantifies the variation or heterogeneity in abortion between clusters in terms of odds ratio scale and is defined as the median value of the odds ratio between the cluster at high likelihood of abortion and cluster at lower risk when randomly picking out individuals from two clusters (37); MOR = e 0.95√VC.
Moreover, the PCV demonstrates the variation in the termination of pregnancy explained by determinants and computed as; ; where Vnull = variance of the null model and VC = cluster level variance (38). The fixed effects were used to estimate the association between the likelihood of abortion and individual and community level independent variables. It was assessed and the strength was presented using adjusted odds ratio (AOR) and 95% confidence intervals with a p-value of <0.05. Deviance = −2 (log likelihood ratio) was used to compare the models due to the nested nature of the model; the model with the lowest deviance and the highest log likelihood ratio has been selected as the best-fit model.
Ethical approval and consent to participate
Since this study is merely a secondary review of the DHS data, ethical approval is not needed. We enrolled with the DHS web archive, requested the dataset for our study, and were granted permission to view and download the data files. As per the DHS study, all participant data were anonymized at the time of survey data collection. Visit in order to understand more about DHS data and ethical standards https://www.dhsprogram.com.
Result
Socio-demographic and economic characteristics of women who had short birth interval in Sub-Saharan Africa, DHS 2015–2022
A total of 283,785 women who had short birth intervals were included in this study. A quarter of women 70,122 (24.71%) had no formal education. More than half 6,909 (56.20%) of the women had pregnancy complications, and about 165,709 (58.39%) were living in rural areas of Sub-Saharan African countries. About 14,041 (4.95%) of women did not have ANC visits. More than half 145,376 (51.23%) of women living in Sub-Saharan African countries have high community poverty (Table 2).
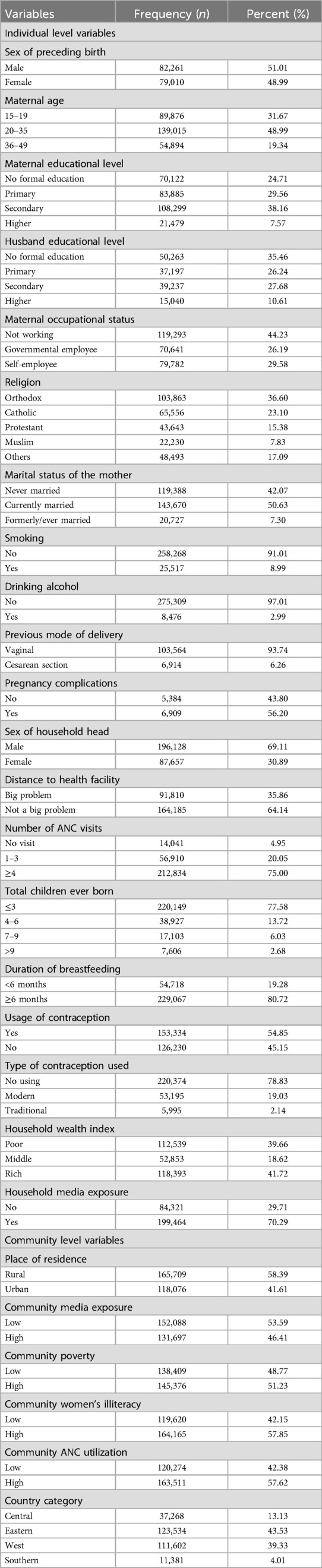
Table 2. Socio-demographic, economic, and obstetric characteristics of women who had short preceding birth interval in Sub-Saharan Africa, DHS 2015–2022.
Prevalence of termination of pregnancy among women who had short preceding birth interval in Sub-Saharan Africa countries
The prevalence of termination of pregnancy among women who had short birth interval in Sub-Saharan African countries was 9.80% [95% CI: (9.69, 9.91)]. The magnitude of urban and rural abortion in Sub-Saharan African countries was found to be 41.95% and 58.05%, respectively (Figure 2). East Sub-Saharan Africa (40.72%) and Southern Sub-Saharan Africa (3.560%) countries had the highest and lowest rates of termination of pregnancy, respectively (Figure 3).
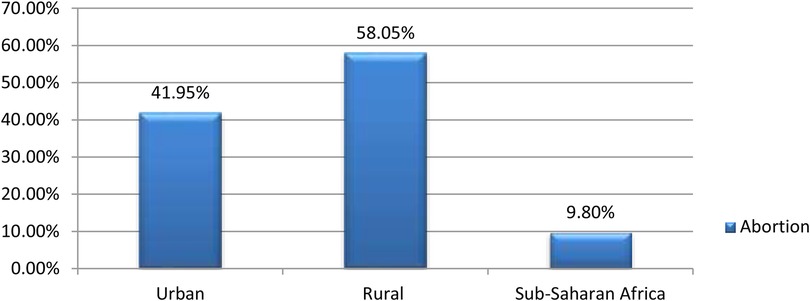
Figure 2. Prevalence of termination of pregnancy among reproductive age women who had short preceding birth interval in Sub-Saharan Africa.
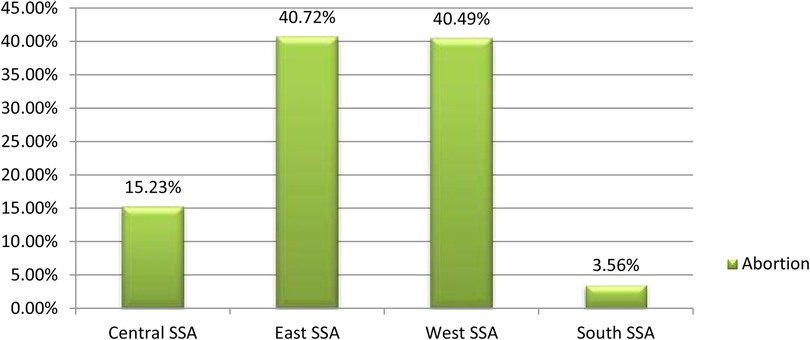
Figure 3. Regional prevalence of termination of pregnancy among women who had short preceding birth interval in Sub-Saharan Africa.
Measures of variation and model fitness
Findings from the null model showed that there were significant differences in termination of pregnancy between communities, with a variance of 0.0661827. In the null model, about 1.97% of the total variation on termination of pregnancy was occurred at the cluster level and is attributable to the community-level factors. In addition, the null model also had the highest median odds ratio (MOR) value (2.17) indicating when randomly select an individual from one cluster with a higher risk of termination of pregnancy and the other cluster at lower risk, individuals at the cluster with a higher risk of termination of pregnancy had 2.17 times higher odds of having termination of pregnancy as compared with their counterparts. The intraclass correlation value for Model I indicated that 1.81% of the variation in termination of pregnancy accounts for the disparities between communities. Next, we built Model II using community-level variables and the null model. Cluster variations were the basis for 1.79% of the differences in abortion, according to the ICC value from Model II. In the final model (model III), which attributed approximately 9.56% of the variation in the likelihood of termination of pregnancy to both individual and community-level factors. The model fitness was conducted by using log likelihood ratio and deviance in the final model (model III), which was the best-fitted model since it had the lowest deviance (6,054.7712) and the highest log likelihood ratio (−3,027.3856) (Table 3).
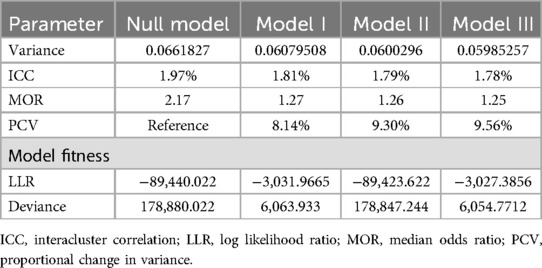
Table 3. Model comparison and random effect analysis for termination of pregnancy among women who had short preceding birth intervals in Sub-Saharan Africa, DHS 2015–2022.
Association of individual and community-level determinants and abortion among reproductive age women in Sub-Saharan Africa
Sex of preceding birth, maternal age, presence of pregnancy complications, no ANC visits, previous mode of delivery, duration of breastfeeding, type of contraception used, poor household wealth status, and urban residence were significantly associated with termination of pregnancy among reproductive age women who had short birth intervals at a p-value of <0.05 in multivariable multilevel mixed-effect logistic regression analysis, where both the individual and community level factors were fitted simultaneously.
The odds of pregnancy termination were 1.21 times higher among women whose preceding birth was male compared to women whose preceding birth was female (AOR = 1.21, 95% CI: 1.05, 1.40). The odds of pregnancy termination were 1.57 times higher among women whose ages were 36–49 years compared to women whose ages were 15–19 years (AOR = 1.57, 95% CI: 1.27, 1.95). The odds of pregnancy termination were 1.28 times higher among women who had pregnancy complications as compared to women who did not have pregnancy complications (AOR = 1.28, 95% CI: 1.09, 1.49). Termination of pregnancy was 2.29 times higher among women who had no ANC visits as compared to women who had four or more ANC visits during pregnancy (AOR = 2.29, 95% CI: 1.26, 4.14).
The odds of pregnancy termination were 1.56 times higher among women who breastfeed as compared to women who did not feed (AOR = 1.56, 95% CI: 1.35, 1.81). The odds of pregnancy termination were 1.67 times higher among women who used traditional contraceptive methods as compared to women who modern contraceptive methods (AOR = 1.67, 95% CI: 1.13, 2.46). The odds of pregnancy termination were 1.74 times higher among women whose previous mode of delivery was cesarean section as compared to women who had vaginal delivery. (AOR = 1.74, 95% CI: 1.32, 2.30). Termination of pregnancy among reproductive age women who lives in poor wealth status was 1.50 times higher as compared to rich women (AOR = 1.50, 95% CI: 1.22, 1.85). The odds of pregnancy termination were 1.31 times higher among women whose place of residence was urban as compared to women from rural areas (AOR = 1.31, 95% CI: 1.06, 1.62) (Table 4).
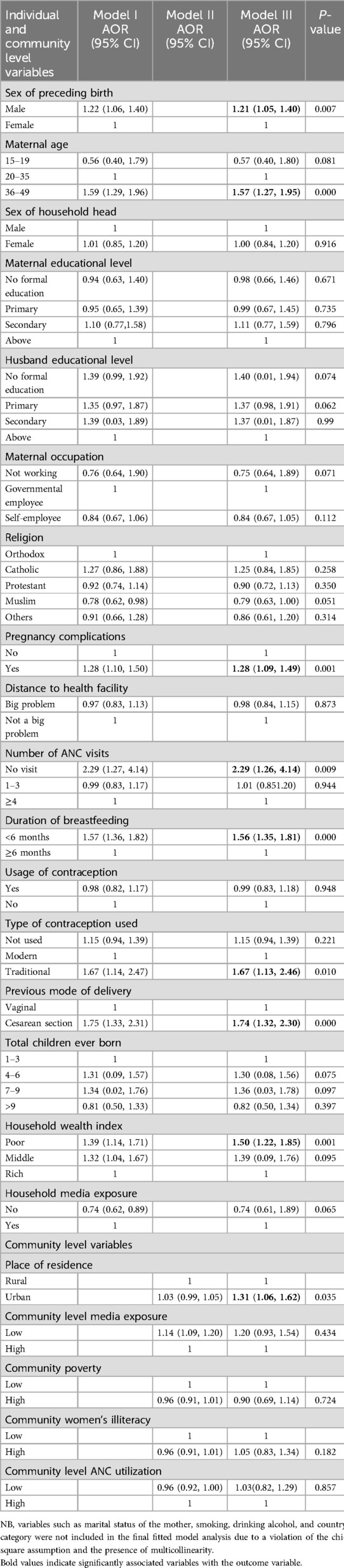
Table 4. Multivariable multilevel logistic regression analysis of individual-level and community level determinants of pregnancy termination among women who had preceding short birth intervals in Sub-Saharan Africa, DHS 2015–2022.
Discussion
This study aimed to assess the prevalence and determinants of pregnancy termination among reproductive-age women who had short birth intervals in Sub-Saharan Africa using 2015–2022 Demography and Health Survey data from each country. In this study, the prevalence of pregnancy termination among women who had short birth interval in Sub-Saharan African countries was 9.80% (95% CI: 9.69, 9.91). This finding was consistent with a previous study conducted in Ethiopia, 9.8% (33), Sierra Leone, 9% (39), and Ghana, 9% (40). The prevalence of pregnancy termination in this study was higher than the findings conducted in Nigeria, 4.9% (41), East Africa, 5.96% (32), Brazil, 4.5% (42), and Iran, 3.8% (43). These discrepancies could be explained by variations in health policies, healthcare quality, and socioeconomic and cultural differences between countries. The higher percentage of pregnancy termination in our analysis indicates that this issue needs to be given more attention in Sub-Saharan Africa.
On the other hand, the prevalence of pregnancy termination in this study was lower than the findings conducted in Ethiopia, 14.5% (44), Cameroon, 21% (45), Egypt, 21% (46), Nepal, 21.1% (20), and Mozambique, 25% (40). A plausible reason might be attributed to variations in the study period and study population, as well as the progressive enhancement of maternal health care service accessibility and utilization.
In multivariable, multilevel mixed-effect logistic regression analysis, sex of preceding birth, maternal age, presence of pregnancy complications, no ANC visits, previous caesarean section delivery, duration of breastfeeding, type of contraception used, poor household wealth status, and urban residence were found to be significantly associated with pregnancy termination among reproductive-age women who had short birth intervals.
Compared to women whose preceding birth was female, the odds of terminating a pregnancy were 1.21 times greater for women whose previous birth was male. This finding is consistent with the studies conducted in Sub-Saharan Africa (47, 48). The explanation could be cultural Gender preferences, particularly the desire for a male child, can significantly influence pregnancy termination decisions, especially in societies where sons are valued for economic, social, or cultural reasons. Families may feel compelled to continue pregnancies until a male child is born, resulting in higher rates of pregnancy termination, particularly when previous children are female or if there is a perceived need for gender balance. This practice can lead to gender imbalances within populations, affecting social structures and perpetuating discriminatory attitudes toward women. Moreover, the societal pressure to conform to these gender norms can restrict women's reproductive autonomy, reinforcing patriarchal values that undervalue female children and contribute to a cycle of gender-based discrimination that persists across generations. This dynamic not only has implications for individual families but also poses significant challenges to gender equality, with long-term effects on women's health, empowerment, and societal roles (48). The other explanation could be family balancing: Some families may seek a balance in the genders of their children. If a family already has one or more male children, they may choose to terminate a subsequent pregnancy if prenatal testing indicates another male child, in the hope of having a female child in the future (49).
The odds of pregnancy termination were 1.76 times higher among women whose ages were 36–49 years compared to women whose ages were 15–19 years. It is in line with study findings in Ethiopia (50), Ghana (51, 52), Mozambique (40), Sierra Leone (39), and China (53). This may be due to the fact that older women have an increased risk of cardiovascular disease, diabetes mellitus, and chromosomal abnormalities, making them more likely to experience pregnancy complications that could worsen pregnancy terminations (54). On the contrary, studies from Arba Minch and Wolayita Sodo town, Ethiopia (55), East Africa (56), and Chile (57) revealed a strong association between pregnancy termination and younger women age. The explanation might be that adolescent girls and young women are ignorant of safe sex practices, such as how to avoid unwanted pregnancy and complications related to pregnancy termination. Another explanation is that younger women don't know as much about family planning as older women do.
The odds of pregnancy termination were 1.28 times higher among women who had pregnancy complications as compared to women who did not have pregnancy complications. This finding is consistent with previous findings in Iran (58), the United Kingdom (59), Pennsylvania (60), and Canada (61). The possible explanation be due to most pregnancy complications are associated with decreased placental nutrient, which results placental insufficiency and these complications are associated with pregnancy termination, preterm birth and perinatal death (62).
Pregnancy termination was 2.40 times higher among women who had no ANC visits as compared to women who had four or more ANC visits during pregnancy. It is in line with the previous studies conducted in Ethiopia (63, 64), Uganda (65, 66), and Nigeria (67, 68). The possible explanation could be that the lack of ANC visits can hinder the timely detection and management of pregnancy-related issues. During these visits, healthcare providers can identify complications early and offer appropriate interventions, which are crucial in reducing the risk of pregnancy termination. The importance of optimal ANC visits cannot be overstated, as they significantly enhance the likelihood of receiving high-quality care throughout pregnancy, thereby preventing spontaneous pregnancy terminations. Furthermore, rural women often struggle with geographic distances, transportation issues, and socio-cultural factors that hinder their access. In urban areas, challenges such as overcrowded facilities, long waiting times, and economic constraints can also deter timely care (69, 70). Therefore, public health strategies must focus on enhancing ANC services, especially for women in disadvantaged communities.
The odds of pregnancy termination were 1.56 times higher among women who breastfeed for less than 6 months as compared to women who breastfeed for 6 and more months. This finding is in line with the studies conducted in low and middle income countries (49), Canada (71), and The USA (72). The association between short breastfeeding periods and pregnancy termination can be complex and multifaceted. Some of the potential justifications and factors that might explain this association could be breastfeeding as a natural contraceptive: Breastfeeding, especially exclusive breastfeeding, can act as a natural contraceptive method known as lactational amenorrhea, which can delay the return of fertility and menstruation. However, this method is not completely reliable, and its effectiveness can decrease with time, particularly after 6 months or when supplemental feeding is introduced (49). Another justification could be socioeconomic and health factors: Women who breastfeed for shorter periods may do so due to socioeconomic reasons, such as the need to return to work, or health issues that prevent prolonged breastfeeding. These same factors could also contribute to the decision or need for pregnancy termination (73).
Compared to women who utilized modern contraceptive methods, women who used traditional contraceptive methods had 1.67 times higher odds of terminating their pregnancy. This is corroborated by previous studies carried out in (74–76). The association between the use of traditional contraceptive methods and a higher likelihood of pregnancy termination, as compared to the use of modern contraceptive methods, can be attributed to several factors. This justification could be contraceptive effectiveness: Traditional contraceptive methods are generally less effective than modern methods. This lower effectiveness can lead to a higher incidence of unintended pregnancies, which may result in a greater number of pregnancy terminations (47). The other explanation might be personal preferences: Some women may choose traditional methods due to personal or religious beliefs, or due to concerns about the side effects of modern contraceptives. However, this choice may increase the risk of unintended pregnancies and the potential for pregnancy termination (77).
Furthermore, traditional methods often have lower effectiveness, leading to a higher incidence of unintended pregnancies and, consequently, increased pregnancy termination rates. Additionally, personal and religious beliefs significantly influence contraceptive choices; women may prefer traditional methods due to perceptions of safety or cultural acceptability, despite these methods being associated with higher risks of unintended pregnancies (41, 78).
The acceptability of contraception among women is a pivotal factor in the context of pregnancy termination. When contraception is widely accepted and utilized, the rate of unintended pregnancies tends to decrease, subsequently leading to a reduction in the number of pregnancy terminations. Conversely, when women are reluctant to use contraception due to personal beliefs, societal pressures, or lack of access the incidence of unintended pregnancies can increase, potentially resulting in a higher rate of pregnancy terminations (47). This association is further complicated by the influence of partners or spouses, whose acceptance or refusal of contraception can significantly impact a woman's reproductive choices. Therefore, understanding the nuances of contraception acceptability is crucial for public health initiatives aimed at reducing the prevalence of pregnancy termination by addressing the root causes of unintended pregnancies (79–81).
The odds of pregnancy termination were 1.71 times higher among women whose previous mode of delivery was caesarean section as compared to women who had vaginal delivery. It is consistent with studies in France (82) and Scotland (83), however to date, this finding is conflicting the study conducted in Germany (84). Although the exact causes of the link between pregnancy termination and Caesarean delivery are unknown, placental abnormalities may be implicated. But frequently, there is no clear underlying reason for these unfavorable incidences (85). According to this study's analysis of wealth status, women from the poorest homes were 1.50 times more likely than those from the richest households to undergo pregnancy termination. This is consistent with the studies conducted in Nepal (20), India (86), and China (87). The possible explanation could be that women from low-income households have inadequate access to healthcare, poor health care practices, and poor health-seeking behaviour. As a result, the women have a higher probability of pregnancy termination.
The odds of pregnancy termination were 1.31 times higher among women whose place of residence was urban as compared to women from rural areas. This is supported by the previous studies conducted in Ethiopia (19, 55, 88, 89), Cambodia (90), Ghana (91), and India (92). The possible explanation might be that, compared to women in rural areas, women in urban areas have more access to abortion services. In the same manner, premarital sex is more common in urban settings and can result in induced abortions and unwanted pregnancies. The finding of this study is inconsistent with the studies conducted in China (87), and Vietnam (93) where pregnancy termination is strongly associated with women from rural areas. This could be because rural areas lack access to media, which could lead to restricted information regarding abortion complications. It could also be because women are less likely to use maternal health care services, such as family planning, ANC visits, understanding of pregnancy signs, and birth planning.
The study's strength was the utilization of recently conducted large-sample national demography and health surveys from 21 Sub-Saharan African countries. Another strength of this study was the use of mixed multilevel logistic regression to determine two-level factors (individual and community-level factors), which could not be done using ordinary logistic regression. However, the study is limited by its reliance on secondary data, which may lack key variables, including maternal psychological factors that could influence the outcome variables. Additionally, potential biases, such as reporting bias in the DHS data, may further affect our findings.
Conclusions and recommendation
This study concludes that pregnancy termination rates among women with short birth intervals are high. The study identified that both individual and community-level variables were determinants of pregnancy termination. To effectively reduce pregnancy termination rates in Sub-Saharan Africa, ministries of health should implement targeted interventions that focus on enhancing antenatal care service utilization among women, particularly those from urban areas. This could involve developing comprehensive outreach programs that promote awareness of available services, providing incentives for women to attend antenatal visits, and establishing collaborations with local community organizations to ensure that tailored support reaches those most in need. We also suggested that future research could incorporate qualitative studies to further explore gender preferences and their influence on pregnancy termination.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
AZ: Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Writing – original draft, Writing – review & editing. TT: Investigation, Methodology, Project administration, Resources, Writing – review & editing. EM: Conceptualization, Data curation, Validation, Visualization, Writing – original draft. MT: Software, Supervision, Validation, Visualization, Writing – review & editing. BT: Conceptualization, Data curation, Resources, Writing – original draft. BW: Data curation, Investigation, Validation, Visualization, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We are grateful to the DHS programmes for letting us use the relevant DHS data in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bearak J, Popinchalk A, Ganatra B, Moller AB, Tunçalp Ö, Beavin C, et al. Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019. Lancet Glob Health. (2020) 8(9):e1152–61. doi: 10.1016/S2214-109X(20)30315-6
2. World Health Organization. Maternal Mortality Measurement: Guidance to Improve National Reporting. Geneva: World Health Organization (2022).
3. Coast E, Norris AH, Moore B, Mdee V. The microeconomics of abortion: a scoping review and analysis of the economic consequences for abortion care-seekers. PLoS One. (2021) 16(6):e0252005. doi: 10.1371/journal.pone.0252005
4. Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Effects of birth spacing on maternal health: a systematic review. Am J Obstet Gynecol. (2007) 196(4):297–308. doi: 10.1016/j.ajog.2006.05.055
5. Shifti DM, Tiruneh SA, Alemu AA, Hagos AK, Muchie KF. Short birth interval prevalence, determinants and effects on maternal and child health outcomes in Asia-pacific region: a systematic review and meta-analysis protocol. BMJ Open. (2023) 13(12):e076908. doi: 10.1136/bmjopen-2023-076908
6. Paul P, Chouhan P. Socio-demographic factors influencing utilization of maternal health care services in India. Clin Epidemiol Glob Health. (2020) 8(3):666–70. doi: 10.1016/j.cegh.2019.12.023
7. Mandal S, McGinnis T. Poor access to safe abortions is killing South Asian women. Lancet. (2021) 398(10302):1895–6.
8. Sedgh G, Bearak J, Singh S, Bankole A, Popinchalk A, Ganatra B, et al. Insights from an expert group meeting on the definition and measurement of unsafe abortion. Int J Gynaecol Obstet. (2016) 134(1):104–6. doi: 10.1016/j.ijgo.2015.11.017
9. Ganatra B, Gerdts C, Rossier C, Johnson BR, Tunçalp Ö, Assifi A, et al. Global, regional, and subregional classification of abortions by safety, 2010–14: estimates from a Bayesian hierarchical model. Lancet. (2017) 390(10110):2372–81. doi: 10.1016/S0140-6736(17)31794-4
10. Singh S, Remez L, Sedgh G, Kwok L, Onda T. Abortion Worldwide 2017: Uneven Progress and Unequal Access. New York, NY: Guttmacher Institute (2018).
11. Sedgh G, Bearak J, Singh S, Bankole A, Popinchalk A, Ganatra B, et al. Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends. Lancet. (2016) 388(10041):258–67. doi: 10.1016/S0140-6736(16)30380-4
12. Grimes DA, Benson J, Singh S, Romero M, Ganatra B, Okonofua FE, et al. Unsafe abortion: the preventable pandemic. Lancet. (2006) 368(9550):1908–19. doi: 10.1016/S0140-6736(06)69481-6
13. Rehnström Loi U, Gemzell-Danielsson K, Faxelid E, Klingberg-Allvin M. Health care providers’ perceptions of and attitudes towards induced abortions in Sub-Saharan Africa and Southeast Asia: a systematic literature review of qualitative and quantitative data. BMC Public Health. (2015) 15(1):1–13. doi: 10.1186/s12889-015-1502-2
14. Sedgh G, Singh S, Shah IH, Åhman E, Henshaw SK, Bankole A. Induced abortion: incidence and trends worldwide from 1995 to 2008. Lancet. (2012) 379(9816):625–32. doi: 10.1016/S0140-6736(11)61786-8
15. Singh K, Ratnam S. The influence of abortion legislation on maternal mortality. Int J Gynaecol Obstet. (1998) 63:S123–9. doi: 10.1016/S0020-7292(98)00194-5
16. Dai R, Li L, Zhu H, Geng D, Deng S, Liu R. Effect of maternal age on spontaneous abortion during the first trimester in northeast China. J Matern Fetal Neonatal Med. (2018) 31(14):1824–9. doi: 10.1080/14767058.2017.1330330
17. Heikinheimo O, Gissler M, Suhonen S. Age, parity, history of abortion and contraceptive choices affect the risk of repeat abortion. Contraception. (2008) 78(2):149–54. doi: 10.1016/j.contraception.2008.03.013
18. Becker D, Diaz-Olavarrieta C, Juarez C, Garcia SG, Smith PS, Harper CC. Sociodemographic factors associated with obstacles to abortion care: findings from a survey of abortion patients in Mexico city. Women’s Health Issues. (2011) 21(3):S16–20. doi: 10.1016/j.whi.2011.02.009
19. Senbeto E, Alene GD, Abesno N, Yeneneh H. Prevalence and associated risk factors of induced abortion in Northwest Ethiopia. Ethiop J Health Dev. (2005) 19(1):37–44. doi: 10.4314/ejhd.v19i1.9969
20. Yogi A, Prakash KC, Neupane S. Prevalence and factors associated with abortion and unsafe abortion in Nepal: a nationwide cross-sectional study. BMC Pregnancy Childbirth. (2018) 18:1–10. doi: 10.1186/s12884-018-2011-y
21. Nielsen A, Gerd Hannibal C, Eriksen Lindekilde B, Tolstrup J, Frederiksen K, Munk C, et al. Maternal smoking predicts the risk of spontaneous abortion. Acta Obstet Gynecol Scand. (2006) 85(9):1057–65. doi: 10.1080/00016340600589560
22. Yokoe R, Rowe R, Choudhury SS, Rani A, Zahir F, Nair M. Unsafe abortion and abortion-related death among 1.8 million women in India. BMJ Glob Health. (2019) 4(3):e001491. doi: 10.1136/bmjgh-2019-001491
23. Atakro CA, Addo SB, Aboagye JS, Menlah A, Garti I, Amoa-Gyarteng KG, et al. Contributing factors to unsafe abortion practices among women of reproductive age at selected district hospitals in the Ashanti region of Ghana. BMC Women’s Health. (2019) 19(1):1–17. doi: 10.1186/s12905-019-0759-5
24. FP2030. Angola family planning 2030. Available online at: https://www.fp2030.org/angola/
25. Benin Ministry of Health. National Health Strategy 2017-2022. Cotonou: Ministry of Health (2017). p. 45.
26. Munezero D, Manirakiza R. Impact of family planning on household size in Burundi. Int J Math Anal. (2022) 16(1):35–47. doi: 10.12988/ijma.2022.912411
27. DeMaria LM, Smith KV, Berhane Y. Sexual and reproductive health in Ethiopia: gains and reflections over the past two decades. Reprod Health. (2022) 19(Suppl 1):175. doi: 10.1186/s12978-022-01464-0
28. Otieno JA, Mawora T. Kenya family planning by 2030. DHS Working Papers. Available online at: https://www.fp2030.org/kenya/
30. Tupy M. Africa is Getting Richer, Thanks to Capitalism. Atlanta, GA: Foundation for Economic Education (2016).
31. Hamadeh N, Van Rompaey C, Metreau E. World Bank Group Country Classifications by Income Level for FY24 (July 1, 2023–June 30, 2024). New Hampshire, United States: The World Bank Group (2023).
32. Aalmneh TS, Alem AZ, Tarekegn GE, Kassew T, Liyew B, Terefe B. Individual and community-level factors of abortion in east Africa: a multilevel analysis. Arch Public Health. (2022) 80(1):184. doi: 10.1186/s13690-022-00938-8
33. Tesema GA, Mekonnen TH, Teshale AB. Spatial distribution and determinants of abortion among reproductive age women in Ethiopia, evidence from Ethiopian demographic and health survey 2016 data: spatial and mixed-effect analysis. PLoS One. (2020) 15(6):e0235382. doi: 10.1371/journal.pone.0235382
34. World Health Organization. WHO Expert Committee on Biological Standardization: Fifty-Sixth Report. Vol. 941. Geneva: World Health Organization (2007).
36. Rodriguez G, Elo I. Intra-class correlation in random-effects models for binary data. Stata J. (2003) 3(1):32–46. doi: 10.1177/1536867X0300300102
37. Merlo J, Ohlsson H, Lynch KF, Chaix B, Subramanian S. Individual and collective bodies: using measures of variance and association in contextual epidemiology. J Epidemiol Community Health. (2009) 63(12):1043–8. doi: 10.1136/jech.2009.088310
38. Al-Sadi AM, Al-Oweisi FA, Edwards SG, Al-Nadabi H, Al-Fahdi AM. Inhibitory effect of Zingiber officinale towards streptococcus mutans virulence and caries development: in vitro and in vivo studies. BMC Microbiol. (2015) 15:1–11. doi: 10.1186/s12866-014-0320-5
39. Sesay FR, Anaba EA, Manu A, Maya E, Torpey K, Adanu RM. Determinants of induced abortion among women of reproductive age: evidence from the 2013 and 2019 Sierra Leone demographic and health survey. BMC Women’s Health. (2023) 23(1):1–10. doi: 10.1186/s12905-023-02175-9
40. Dickson KS, Adde KS, Ahinkorah BO. Socio—economic determinants of abortion among women in Mozambique and Ghana: evidence from demographic and health survey. Arch Public Health. (2018) 76(1):1–10. doi: 10.1186/s13690-018-0286-0
41. Onukwugha FI, Magadi MA, Sarki AM, Smith L. Trends in and predictors of pregnancy termination among 15–24 year-old women in Nigeria: a multi-level analysis of demographic and health surveys 2003–2018. BMC Pregnancy Childbirth. (2020) 20:1–13. doi: 10.1186/s12884-020-03164-8
42. Souza MG, Fusco CL, Andreoni SA, Silva RdS. Prevalence and sociodemographic characteristics of women with induced abortion in a population sample of São Paulo, Brazil. Rev Bras Epidemiol. (2014) 17:297–312. doi: 10.1590/1809-4503201400020002ENG
43. Hosseini H, Erfani A, Nojomi M. Factors associated with incidence of induced abortion in Hamedan, Iran. Arch Iran Med. (2017) 20(5):282–7.28510463
44. Zeleke AM. Prevalence and determinants of induced abortion among reproductive-aged women in Aykel town north west, Ethiopia: a community-based cross-sectional study. World J Adv Re Rev. (2021) 12(2):032–41. doi: 10.30574/wjarr.2021.12.2.0501
45. Bongfen MC, Abanem EEB. Abortion practices among women in Buea: a socio-legal investigation. Pan Afr Med J. (2019) 32(1):1–6. doi: 10.11604/pamj.2019.32.146.17732
46. Yassin K. Incidence and socioeconomic determinants of abortion in rural Upper Egypt. Public Health. (2000) 114(4):269–72. doi: 10.1016/S0033-3506(00)00343-7
47. Adde KS, Dickson KS, Ameyaw EK, Amo-Adjei J. Contraception needs and pregnancy termination in sub-Saharan Africa: a multilevel analysis of demographic and health survey data. Reprod Health. (2021) 18(1):177. doi: 10.1186/s12978-021-01227-3
48. Ahinkorah BO. Socio-demographic determinants of pregnancy termination among adolescent girls and young women in selected high fertility countries in sub-Saharan Africa. BMC Pregnancy Childbirth. (2021) 21:1–8. doi: 10.1186/s12884-020-03485-8
49. Ba DM, Zhang Y, Pasha-Razzak O, Khunsriraksakul C, Maiga M, Chinchilli VM, et al. Factors associated with pregnancy termination in women of childbearing age in 36 low-and middle-income countries. PLOS Glob Public Health. (2023) 3(2):e0001509. doi: 10.1371/journal.pgph.0001509
50. Gelaye AA, Taye KN, Mekonen T. Magnitude and risk factors of abortion among regular female students in Wolaita Sodo University, Ethiopia. BMC Women’s Health. (2014) 14:1–9. doi: 10.1186/1472-6874-14-50
51. Sundaram A, Juarez F, Bankole A, Singh S. Factors associated with abortion-seeking and obtaining a safe abortion in Ghana. Stud Fam Plann. (2012) 43(4):273–86. doi: 10.1111/j.1728-4465.2012.00326.x
52. Mote CV, Otupiri E, Hindin MJ. Factors associated with induced abortion among women in Hohoe, Ghana. Afr J Reprod Health. (2010) 14(4):53–60.
53. Gao GP, Zhang RJ, Zhang XJ, Jia XM, Li XD, Li X, et al. Prevalence and associated factors of induced abortion among rural married women: a cross-sectional survey in Anhui, China. J Obstet Gynaecol Res. (2015) 41(3):383–91. doi: 10.1111/jog.12547
54. Ryan E, Savu A, Yeung R, Moore L, Bowker S, Kaul P. Elevated fasting vs post-load glucose levels and pregnancy outcomes in gestational diabetes: a population-based study. Diabetic Med. (2020) 37(1):114–22. doi: 10.1111/dme.14173
55. Abebe M, Mersha A, Degefa N, Gebremeskel F, Kefelew E, Molla W. Determinants of induced abortion among women received maternal health care services in public hospitals of Arba Minch and Wolayita Sodo town, southern Ethiopia: unmatched case-control study. BMC Womens Health. (2022) 22(1):1–12. doi: 10.1186/s12905-022-01695-0
56. Hailegebreal S, Enyew EB, Simegn AE, Seboka BT, Gilano G, Kassa R, et al. Pooled prevalence and associated factors of pregnancy termination among youth aged 15–24 year women in east Africa: multilevel level analysis. PLoS One. (2022) 17(12):e0275349. doi: 10.1371/journal.pone.0275349
57. Huneeus A, Capella D, Cabieses B, Cavada G. Induced abortion according to socioeconomic status in Chile. J Pediatr Adolesc Gynecol. (2020) 33(4):415–20.e1. doi: 10.1016/j.jpag.2020.03.003
58. Poorolajal J, Cheraghi P, Cheraghi Z, Ghahramani M, Irani AD. Predictors of miscarriage: a matched case-control study. Epidemiol Health. (2014) 36:e2014003. doi: 10.4178/epih/e2014031
59. Panaitescu AM, Syngelaki A, Prodan N, Akolekar R, Nicolaides KH. Chronic hypertension and adverse pregnancy outcome: a cohort study. Ultrasound Obstet Gynecol. (2017) 50(2):228–35. doi: 10.1002/uog.17493
60. Gracia CR, Sammel MD, Chittams J, Hummel AC, Shaunik A, Barnhart KT. Risk factors for spontaneous abortion in early symptomatic first-trimester pregnancies. Obstet Gynecol. (2005) 106(5 Part 1):993–9. doi: 10.1097/01.AOG.0000183604.09922.e0
61. Aris A. A 12-year cohort study on adverse pregnancy outcomes in eastern townships of Canada: impact of endometriosis. Gynecol Endocrinol. (2014) 30(1):34–7. doi: 10.3109/09513590.2013.848425
62. Melese MF, Badi MB, Aynalem GL. Perinatal outcomes of severe preeclampsia/eclampsia and associated factors among mothers admitted in Amhara region referral hospitals, North West Ethiopia, 2018. BMC Res Notes. (2019) 12:1–6. doi: 10.1186/s13104-019-4161-z
63. Yeshialem E, Abera M, Tesfay A. Determinants of adverse pregnancy outcomes among mothers who gave birth from Jan 1–Dec 31/2015 in Jimma University specialized hospital, case control study, 2016. Ethiop J Reprod Health. (2019) 11(1):10. doi: 10.69614/ejrh.v11i1.235
64. Beyene GM, Azale T, Gelaye KA, Ayele TA. The effect of antenatal depression on birth weight among newborns in South Gondar zone, Northwest Ethiopia: a population-based prospective cohort study. Arch Public Health. (2021) 79(1):1–12. doi: 10.1186/s13690-020-00513-z
65. Asiki G, Baisley K, Newton R, Marions L, Seeley J, Kamali A, et al. Adverse pregnancy outcomes in rural Uganda (1996–2013): trends and associated factors from serial cross sectional surveys. BMC Pregnancy Childbirth. (2015) 15(1):1–12. doi: 10.1186/s12884-015-0708-8
66. Kananura RM, Wamala R, Ekirapa-Kiracho E, Tetui M, Kiwanuka SN, Waiswa P, et al. A structural equation analysis on the relationship between maternal health services utilization and newborn health outcomes: a cross-sectional study in Eastern Uganda. BMC Pregnancy Childbirth. (2017) 17(1):1–12. doi: 10.1186/s12884-017-1289-5
67. Awoleke JO, Olofinbiyi BA. Poor prenatal service utilization and pregnancy outcome in a tertiary health facility in Southwest Nigeria. Pan Afr Med J. (2020) 35. doi: 10.11604/pamj.2020.35.28.20426
68. Onwuhafua PI, Williams ICO, Kolawole AO, Adze JA. The effect of frequency of antenatal visits on pregnancy outcome in Kaduna, Northern Nigeria. Trop J Obstet Gynaecol. (2016) 33(3):317. doi: 10.4103/0189-5117.199813
69. Lattof SR, Tunçalp Ö, Moran AC, Bucagu M, Chou D, Diaz T, et al. Developing measures for WHO recommendations on antenatal care for a positive pregnancy experience: a conceptual framework and scoping review. BMJ Open. (2020) 9(4):e024130. doi: 10.1136/bmjopen-2018-024130
70. Dahab R, Sakellariou D. Barriers to accessing maternal care in low income countries in Africa: a systematic review. Int J Environ Res Public Health. (2020) 17(12):4292. doi: 10.3390/ijerph17124292
71. Hobbs AJ, Mannion CA, McDonald SW, Brockway M, Tough SC. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth. (2016) 16:1–9. doi: 10.1186/s12884-016-0876-1
72. Haas DM, Yang Z, Parker CB, Chung J, Parry S, Grobman WA, et al. Factors associated with duration of breastfeeding in women giving birth for the first time. BMC Pregnancy Childbirth. (2022) 22(1):722. doi: 10.1186/s12884-022-05038-7
73. Byamukama O, Migisha R, Kalyebara PK, Tibaijuka L, Lugobe HM, Ngonzi J, et al. Short interbirth interval and associated factors among women with antecedent cesarean deliveries at a tertiary hospital, Southwestern Uganda. BMC Pregnancy Childbirth. (2022) 22(1):268. doi: 10.1186/s12884-022-04611-4
74. Ajayi AI, Adeniyi OV, Akpan W. Use of traditional and modern contraceptives among childbearing women: findings from a mixed methods study in two Southwestern Nigerian states. BMC Public Health. (2018) 18:1–9. doi: 10.1186/s12889-018-5522-6
75. Tiruneh GA, Erega BB, T/mariam AB, Abebe EC, Ayele TM, Baye ND, et al. Level of knowledge, attitude, and practice on modern contraceptive method and its associated factors among housemaids living in Debre Tabor town, northwest Ethiopia: a community-based cross-sectional study. BMC Women’s Health. (2023) 23(1):632. doi: 10.1186/s12905-023-02783-5
76. Cavallaro FL, Benova L, Owolabi OO, Ali M. A systematic review of the effectiveness of counselling strategies for modern contraceptive methods: what works and what doesn’t? BMJ Sexual Reprod Health. (2020) 46(4):254–69. doi: 10.1136/bmjsrh-2019-200377
77. Ahinkorah BO, Budu E, Aboagye RG, Agbaglo E, Arthur-Holmes F, Adu C, et al. Factors associated with modern contraceptive use among women with no fertility intention in sub-Saharan Africa: evidence from cross-sectional surveys of 29 countries. Contracept Reprod Med. (2021) 6:1–13. doi: 10.1186/s40834-021-00165-6
78. D’Souza P, Bailey JV, Stephenson J, Oliver S. Factors influencing contraception choice and use globally: a synthesis of systematic reviews. Eur J Contracept Reprod Health Care. (2022) 27(5):364–72. doi: 10.1080/13625187.2022.2096215
79. Sarnak DO, Wood SN, Zimmerman LA, Karp C, Makumbi F, Kibira SP, et al. The role of partner influence in contraceptive adoption, discontinuation, and switching in a nationally representative cohort of Ugandan women. PLoS One. (2021) 16(1):e0238662. doi: 10.1371/journal.pone.0238662
80. Ezeanolue EE, Iwelunmor J, Asaolu I, Obiefune MC, Ezeanolue CO, Osuji A, et al. Impact of male partner’s awareness and support for contraceptives on female intent to use contraceptives in southeast Nigeria. BMC Public Health. (2015) 15:1–6. doi: 10.1186/s12889-015-2216-1
81. Kriel Y, Milford C, Cordero J, Suleman F, Beksinska M, Steyn P, et al. Male partner influence on family planning and contraceptive use: perspectives from community members and healthcare providers in KwaZulu-Natal, South Africa. Reprod Health. (2019) 16:1–15. doi: 10.1186/s12978-019-0749-y
82. Mazouni C, Provensal M, Porcu G, Guidicelli B, Heckenroth H, Gamerre M, et al. Termination of pregnancy in patients with previous cesarean section. Contraception. (2006) 73(3):244–8. doi: 10.1016/j.contraception.2005.09.007
83. Mollison J, Porter M, Campbell D, Bhattacharya S. Primary mode of delivery and subsequent pregnancy. BJOG. (2005) 112(8):1061–5. doi: 10.1111/j.1471-0528.2005.00651.x
84. Jacob L, Taskan S, Macharey G, Sechet I, Ziller V, Kostev K. Impact of caesarean section on mode of delivery, pregnancy-induced and pregnancy-associated disorders, and complications in the subsequent pregnancy in Germany. GMS Ger Med Sci. (2016) 14:Doc06. doi: 10.3205/000233
85. Flenady V, Koopmans L, Middleton P, Frøen JF, Smith GC, Gibbons K, et al. Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. Lancet. (2011) 377(9774):1331–40. doi: 10.1016/S0140-6736(10)62233-7
86. Gogoi M. Association of maternal age and low socio-economic status of women on birth outcome. Int Res J Soc Sci. (2014) 3(10):21–7.
87. Zheng D, Li C, Wu T, Tang K. Factors associated with spontaneous abortion: a cross-sectional study of Chinese populations. Reprod Health. (2017) 14(1):1–9. doi: 10.1186/s12978-017-0297-2
88. Nigussie T, Feyisa M, Yosef T, Berhanu M, Asefa A. Prevalence of induced abortion and its associated factors among female students of health science in south west Ethiopia. Open Nurs J. (2020) 14(1):1–9. doi: 10.2174/1874434602014010248
89. Mekie M, Addisu D, Dagnew E, Necho W. The level and deriving factors of repeat-induced abortion in Ethiopia: a systematic review and meta-analysis. Heliyon. (2021) 7(1):e05891. doi: 10.1016/j.heliyon.2021.e05984
90. Smith C, Scott RH, Free C, Edwards T. Characteristics and contraceptive outcomes of women seeking medical or surgical abortion in reproductive health clinics in Cambodia. Contracept Reprod Med. (2019) 4(1):1–9. doi: 10.1186/s40834-019-0086-0
91. Baruwa OJ, Amoateng AY, Biney E. Induced abortion in Ghana: prevalence and associated factors. J Biosoc Sci. (2022) 54(2):257–68. doi: 10.1017/S0021932020000772
92. Vinita D, Swati J, Prabha GH, Anjoo A, Sujata AP. Evaluation of newer methods of early pregnancy termination. J Obstet Gynecol India. (2005) 55(5):454–6.
Keywords: determinants, prevalence, pregnancy termination, short birth intervals, Sub-Saharan Africa
Citation: Zegeye AF, Tamir TT, Mekonen EG, Techane MA, Terefe B and Workneh BS (2024) Prevalence and determinants of termination of pregnancy among reproductive-age women who had a short preceding birth interval in Sub-Saharan Africa: a multilevel analysis. Front. Glob. Womens Health 5:1471187. doi: 10.3389/fgwh.2024.1471187
Received: 26 July 2024; Accepted: 7 November 2024;
Published: 27 November 2024.
Edited by:
Sarosh Iqbal, University of Management and Technology, PakistanReviewed by:
Wesler Lambert, Zanmi Lasante/Partners In Health, HaitiSubhadra Priyadarshini, Kalinga Institute of Medical Sciences (KIMS), India
Copyright: © 2024 Zegeye, Tamir, Mekonen, Techane, Terefe and Workneh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alebachew Ferede Zegeye, YWxleGZlcmVkZTI0QGdtYWlsLmNvbQ==
 Alebachew Ferede Zegeye
Alebachew Ferede Zegeye Tadesse Tarik Tamir
Tadesse Tarik Tamir Enyew Getaneh Mekonen
Enyew Getaneh Mekonen Masresha Asmare Techane
Masresha Asmare Techane Bewuketu Terefe
Bewuketu Terefe Belayneh Shetie Workneh
Belayneh Shetie Workneh