- 1Department of Psychology, University of South Florida, St. Petersburg, FL, United States
- 2Department of Pediatrics, University of South Florida, Tampa, FL, United States
- 3Perinatal HIV Research Unit, School of Clinical Medicine, University of Witwatersrand, Johannesburg, South Africa
- 4Department of Mental Health Law and Policy, University of South Florida, Tampa, FL, United States
- 5Department of Global Health and Social Medicine, Harvard Medical School, Boston, MA, United States
- 6Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA, United States
- 7Department of Psychology, University of South Florida, Tampa, FL, United States
- 8Department of Social Work, University of South Florida, Tampa, FL, United States
HIV stigma among people living with HIV (PLWH) is well documented and linked to adverse physical and mental health outcomes among this population. Further, stigma may affect HIV disclosure decisions, which has important individual and public health implications. For women, HIV stigma and disclosure may be compounded by gender-based discrimination and violence. Despite the ill effects of HIV stigma, particularly for women, few evidence-based disclosure interventions to reduce stigma among PLWH exist. However, there is strong evidence for the efficacy of Honest, Open, Proud (HOP), a disclosure-based stigma-reduction intervention for people with mental illness. Given that mental illness and HIV are similar in that they are both stigmatized yet concealable conditions, we propose using the ADAPT-ITT model to adapt HOP into Positive, Open, Proud, a disclosure-based stigma-reduction intervention for PLWH, describing its unique potential for women living with HIV.
1 Introduction
In his seminal work, Irving Goffman (1) defined stigma as a social phenomenon that discredits and devalues individual characteristics. Since then, defining and conceptualizing stigma has presented numerous challenges given the broad range of circumstances to which stigma applies (2), leading researchers to approach stigma from different theoretical lenses based on their respective fields. Nonetheless, there is considerable overlap in the types of stigmas that have been studied. Here, we focus on public stigma and self-stigma.
Public stigma, also referred to as social stigma, personal stigma, public prejudice, labeling, marginalization, or cultural bias, encompasses the stereotypes (cognitions or beliefs) and corresponding prejudice (emotional reactions) of the general public toward individuals who are marginalized, and the resulting discrimination of stigmatized group members (3).
Self-stigma, also known as internalized stigma, internalized shame, self-devaluation, or internalized prejudice involves individuals who occupy marginalized identities accepting and integrating the negative attitudes, beliefs, and stereotypes of the broader society (4). Stigma can be intersectional in nature (5), meaning several forms of interlocking forms of stigma (e.g., gender-based stigma, race-based stigma, HIV stigma) manifest simultaneously to produce a heightened and nuanced experience. Intersecting stigmas often reinforce power dynamics, leading to varied impacts based on societal hierarchies and differential stigma experiences. For example, a Black woman living with HIV [LWH] may experience stigma differently than a white man LWH. Both public and self-stigma contribute to label avoidance and concealment, further limiting access to social support systems that may help alleviate stressors. Further, public stigma poses a serious public health concern given its relationship with various negative outcomes, including residential segregation, educational and health disparities, social isolation, and diminished quality of life (6), thus, perpetuating inequality and marginalization. Public stigma is directly linked to self-stigma when societal beliefs are internalized (7), leading to maladaptive psychological responses, such as rumination and depression, as well as behavioral outcomes, like substance use (6). Two of the most highly stigmatized conditions are HIV and mental illness (8). In this paper, we explore the similarities and differences between mental illness and HIV as stigmatized conditions; provide an overview of existing HIV stigma interventions and their limitations; describe an evidence-based disclosure intervention to reduce mental illness stigma, Honest, Open, Proud (HOP); describe how HOP might be adapted to provide a novel disclosure-based HIV stigma-reduction intervention, Positive, Open, Proud (POP); and explain why POP may be particularly useful for women living with HIV (WLWH) given the impact of gender-based power dynamics on disclosure decisions.
2 Similarities and differences between mental illness and HIV as stigmatized conditions
Stigma is broadly understood to be undesirable and harmful, regardless of the health condition, and is often described in monolithic terms, which may belie important differences between stigmatized conditions. While mental illness and HIV stigma share some similarities, there are crucial differences in HIV that necessitate unique, targeted interventions (8). Here, we consider the key similarities and differences between mental illness and HIV that affect the manifestation of stigma.
2.1 Similarities
The first similarity between HIV and mental illness is their potential for concealment (9). Although there are exceptions (e.g., untreated HIV resulting in Kaposi sarcoma, a rare cancer that is a hallmark of advanced HIV disease, and certain severe mental illnesses involving disorganized speech or involuntary motor movements), most PLWH and/or a mental illness can hide their condition from others, thus avoiding the resulting stigma (9). Of note, although people with less visible chronic health conditions may report less stigma, the magnitude of its adverse effects on mental health may be greater than those with visible conditions (10). A second similarity is that both HIV and mental illness tend to be chronic and require regular intervention (whether medication, self-care strategies, or other therapeutic approaches) to maintain wellness. Left untreated, both can cause serious morbidity and mortality. A third commonality between HIV and mental illness is that both may invoke negative perceptions of character, for example, promiscuity or immorality for PLWH and weakness and chosen fragility for persons with mental illness.
2.2 Differences
As an infectious disease, the first significant difference between HIV and mental illness is that HIV, unlike mental illness, is both acquired and can be transmitted to others. While emerging evidence suggests genetic correlates for some serious mental disorders (e.g., schizophrenia), this differs from a virus that can be isolated and passed to others. Further, how HIV is transmitted, primarily through sexual contact (though not always, as in the case of acquiring HIV via a blood transfusion or during birth), is also frequently stigmatized especially same-sex sexual activity, forced/non-consensual sex, commercial sex work, or sex outside an established primary relationship. These differences in stigma are especially important when disclosing HIV to others because the process may simultaneously reveal the HIV status of someone other than the discloser and/or personal information (11). For example, disclosing living with HIV invariably conjures the question “How did you get it?” and may lead to the disclosure of other people (e.g., sex partner, mother) or reveal past trauma (e.g., rape, sexual assault) or other information that might generally be kept private. Finally, HIV disclosure also frequently involves the revelation of other stigmatized identities (e.g., sexual orientation, gender identity) or behaviors (e.g., same-sex sexual partnerships, substance use including intravenous drug use) (12) for which there may be magnified disclosure consequences.
3 HIV stigma and disclosure among women: unique considerations
WLWH often face significant compounded stigmas based on their multiple marginalized identities which are characterized by power dynamics and gender-based discrimination resulting in poorer mental health and quality of life (13, 14). Societal norms and cultural expectations about women's behavior, including sexual conduct and fidelity, may result in unfair blame and increased moral and social judgement, exacerbating the HIV stigma they face (14, 15). Women may have less access to healthcare resources due to gender biases in healthcare systems, restricted mobility, childcare obligations, and other gender-related barriers (16). HIV stigma can further limit women's ability to seek and receive appropriate medical care and impact their ability to fulfill caretaking roles, affecting both their well-being and that of those they care for, which is particularly problematic given that women often bear the primary responsibility for caregiving within families. Fear of HIV stigma can strain social networks, reducing the support women receive from friends, relatives, and community members.
The interplay between HIV stigma and HIV disclosure decisions can be complicated by gender-based power dynamics. Women may face increased risks of interpersonal violence or abandonment if they disclose their HIV status (17). The fear of physical, emotional, or economic abuse from partners or family members can deter women from disclosing their HIV status. Many women, especially in patriarchal societies, may be financially dependent on their partners or families. Disclosure of HIV status could jeopardize their financial security and that of their children, making them more vulnerable to poverty and homelessness. In a recent study of 118 pregnant WLWH in Ghana, fear of loss of financial support was the most common reason for nondisclosure of HIV status (18). Women of childbearing age face specific concerns related to pregnancy and childbirth. Disclosure of HIV status is crucial for accessing prevention of mother-to-child transmission services, but fear of blame and stigma can deter women from seeking these and other healthcare services (19, 20).
4 Evidence-based disclosure interventions to reduce self-stigma
In the mental health stigma reduction field, two predominant approaches are used to reduce self-stigma: (1) education-based and cognitive restructuring strategies teaching people ways to counter stereotypes by providing facts that counter myths (21), and (2) disclosure-based strategies, which recognize that due to the concealable nature of the stigmatized identity of mental illness, people with mental illness face the choice of whether to disclose or conceal (1). Disclosure-based self-stigma reduction strategies rest on research showing that people with concealable stigmatized identities (e.g., mental illness, HIV) who identify with peers and are publicly out with their stigmatized identity may experience better mental and physical health as well as better relationships (21–23).
Separate bodies of literature document HIV stigma reduction interventions (24, 25) and HIV disclosure uptake interventions (26, 27) for PLWH. Existing HIV stigma reduction interventions have utilized primarily psychoeducation-based approaches (28), shown wide variability in producing change in targeted outcomes (24), and targeted a single socio-ecological level (e.g., individual level) focusing on one domain of stigma (29). Structural HIV stigma reduction interventions such as economic strengthening, social empowerment, and antiretroviral treatment provision coupled with individual components (e.g., health education) have been most effective in reducing self-stigma in PLWH (30). Few individual and relational interventions are documented, and existing studies have not found significant reductions in self-stigma (30). Further, few HIV stigma reduction interventions that possess strong methodological rigor have considered intersectional stigmas in HIV (25). Meanwhile, available HIV disclosure uptake interventions are narrow in scope, often focusing on a specific form of disclosure (e.g., sexual partner disclosure only). These interventions are characterized by variable content and operationalization of disclosure (26). There remains a need to not only advance the quality of methodological rigor in HIV stigma reduction and disclosure uptake interventions but also to combine these complementary approaches, which is not common practice (30).
The few combined HIV stigma and disclosure-targeted interventions available have demonstrated mixed efficacy, with one randomized control entertainment-education intervention finding positive changes in disclosure attitudes, self-efficacy, and intentions to disclose, but no changes in internalized stigma in Black women in the Southern United States (31). Similarly, a randomized control trial of a community-based culturally informed motivational interviewing style intervention for Black PLWH found no changes in internalized stigma and disclosure across a 13-month period (32). Considering the complexities surrounding HIV stigma reduction and disclosure uptake interventions, it is essential to explore innovative approaches that hold promise in addressing these challenges and fostering positive outcomes for PLWH.
5 Honest, open, proud: a model evidence-based disclosure intervention to reduce self-stigma
A model evidence-based disclosure intervention to reduce mental illness self-stigma, Honest, Open, Proud (HOP) was developed using community-based participatory research methods to directly target key mediators of mental illness self-stigma and its harmful impact (33). The core intervention consists of three lessons by two trained peer facilitators (individuals also living with the stigmatized condition) in groups of six to ten participants. Lesson delivery can occur in a one-day session, in two half-day sessions, or over the course of three consecutive weeks for two hours per week. As described below, each of the three lessons is focused on developing a disclosure-related skill, followed by a booster session.
5.1 Lesson 1: evaluate the pros and cons of disclosing
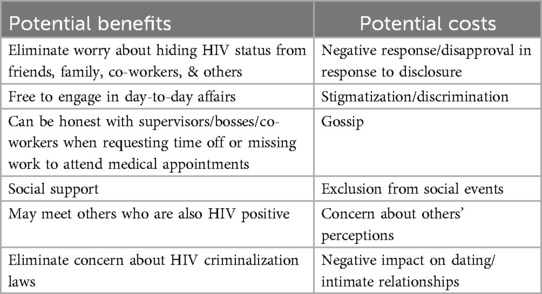
Motivators have important and dynamic effects on disclosure (34). HOP teaches participants to identify the costs and benefits of disclosure, which are likely to vary by setting or recipient (e.g., disclosing to family vs. friends, schoolmates, partners). Hence, program participants learn the skills to think through potential risks and complete cost-benefit analyses in terms of specific settings or people. Participants learn that disclosure is not a “one size fits all” endeavor but must be tailored to each individual.
5.2 Lesson 2: learn ways to identify safe people to disclose to
Given the importance of social support in disclosure, HOP participants learn strategies to test the likelihood that specific people in specific settings (e.g., a medical provider in a clinic, or a classmate at school) are likely to react positively to disclosure.
5.3 Lesson 3: craft a personal disclosure story
Rooted in research demonstrating that the quality of the story and personal narrative is associated with decreased self-stigma (35), participants learn the elements of an effective disclosure story that they can use to write their own story for future disclosure.
5.4 Booster
A fourth booster session is delivered a month post-intervention for participant reflection on any disclosure experiences since completing lessons 1 through 3, and to provide ongoing peer support.
5.5 HOP research
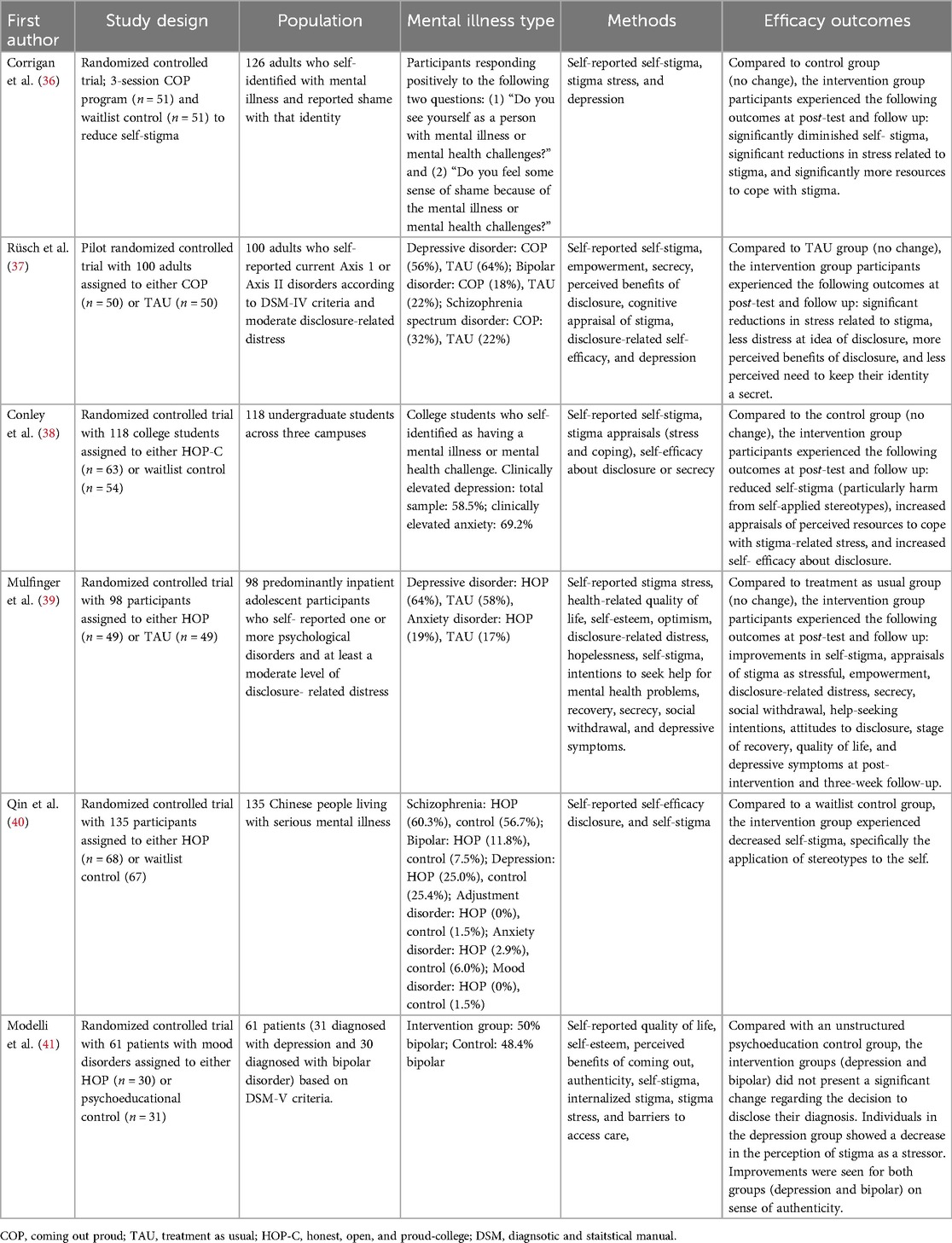
An accumulating evidence base, including multiple randomized controlled trials, suggests HOP is effective in reducing self-stigma and related outcomes among people living with mental illness. Table 1 summarizes the details of existing randomized controlled trials of HOP for mental illness. A recent meta-analysis of the literature on HOP revealed statistically significant positive effects on stigma stress as well as modest differences in self-stigma and depression (37). HOP has been adapted for other stigmatized conditions (e.g., suicide survivorship and Tourette's Syndrome) and special populations (e.g., Veterans) (https://hopprogramorg). For example, a pilot study of HOP for suicide survivors found significant effects among HOP participants relative to a control group for two measures of self-stigma, depression, and self-esteem (42).
6 Adapting HOP for HIV: Positive, Open, Proud
Given the similarities between mental illness and HIV, as described above, and existing research in support of the effectiveness of HOP for facilitating disclosure decisions and reducing stigma stress among people with mental illness (37), an adaptation of HOP for HIV offers a promising and innovative disclosure-based self-stigma reduction intervention. Like mental illness, HIV is a concealable, stigmatized identity. Therefore, PLWH face the choice of whether, how, and when to discuss their disease status with others, considering the potential benefits and costs of HIV disclosure. See Table 2. Theoretically, the decision-making and action of mental health disclosure is like HIV disclosure as it involves antecedent goals, outcome expectancies, intention, and action planning. Therefore, we are adapting the HOP curriculum for PLWH - Positive, Open, Proud (POP) - using the ADAPT-ITT model (43), which employs a systematic process for adapting evidence-based interventions using 8 steps: (1) assessment to obtain a comprehensive understanding of the target population (in this case, PLWH); (2) decision, which involves selecting an intervention (in this case, HOP) and deciding whether to adopt or adapt (in this case, adapt); (3) adaptation by using a pretested methodology to understand better how to adapt HOP for PLWH; (4) production, which requires creating an adaptation plan and determining goals; (5) topical experts, which involves obtaining substantive content and technical assistance; (6) integration, which involves integrating all forms of information; (7) training all personnel; and (8) testing via a pilot study to assess adaptation efficacy.
Four of the authors of this article have HIV expertise and work closely with affected communities and community advisory groups comprised of PLWH, thus facilitating Step 1 (Assessment). By collaborating with another author who has conducted extensive research on mental illness stigma-reduction through self-disclosure, we decided to adapt HOP for HIV (Step 2). In preparation for Steps 3–8, a person with lived experience with HIV assisted with an initial desk adaptation of the HOP curriculum to POP. Like HOP, POP consists of three lessons to help PLWH (1) evaluate the pros and cons of disclosure, (2) select ways to disclose and to whom, and (3) develop ways to tell their story. A fourth booster session one-month post-intervention is designed to provide ongoing peer support and allow participant reflection on any disclosure experiences following Lessons 1–3.
We plan to partner with an HIV community advisory board (CAB) comprised of a diverse group of PLWH to ensure, consistent with ADAPT-ITT guidelines, the target population/key stakeholders are involved in all phases of the adaptation process. Specifically, we will use a pretested methodology to understand better how to further adapt HOP to POP (Step 3), create an adaptation plan and determine goals (Step 4), engage topical experts to provide substantive content and technical assistance (Step 5), and to integrate all forms of information (Step 6). We will then train two peer facilitators with lived experience with HIV (Step 7). Finally, we will pilot POP with PLWH to determine its efficacy as a disclosure-based self-stigma reduction intervention (Step 8).
7 Potential benefits of POP for women living with HIV
Given the impact of gender dynamics on perceptions of HIV and decision-making around sexual health (44, 45) a need exists for HIV disclosure interventions for WLWH (18), especially interventions that prioritize choice (46). Therefore, we believe POP may be particularly useful for women as an HIV disclosure-based stigma-reduction intervention.
Gender-based power imbalances may affect women's ability to disclose their HIV status safely and confidently (17). POP may help provide women with the tools and support needed to navigate these power dynamics and make informed decisions about disclosure. Disclosure of HIV status can lead to better health outcomes by facilitating access to healthcare, support services, and social networks. For women, this is particularly important as they may have additional health needs related to reproductive health, pregnancy, and childcare. Reducing stigma can encourage women to seek and adhere to treatment, ultimately improving their health and quality of life. By providing knowledge, skills, and support to make autonomous decisions about their health and lives, POP may empower women, which may help them negotiate safer sexual practices, improve their self-esteem, and reduce their dependency on partners who may be unsupportive or abusive.
The association between HIV and gender-based violence is well documented (47). POP recognizes that HIV disclosure can sometimes trigger violence if not handled sensitively and, therefore, does not encourage disclosure but, rather, helps PLWH explore disclosure decisions. For women, this includes the exploration of safe and supportive options for disclosure.
8 Conclusion and future directions
Despite some unique differences, there are many similarities between HIV stigma and mental illness stigma. Given the strong evidence for the efficacy of HOP as a disclosure-based stigma-reduction intervention for people living with mental illness and other conditions, adapting this intervention to reduce stigma among PLWH shows promise, especially given the lack of evidence-based disclosure interventions to reduce HIV self-stigma. Therefore, we are using the ADAPT-ITT Model (43) to develop and pilot Positive, Open, Proud as a disclosure-based stigma-reduction intervention for PLWH. We believe POP may be particularly useful for addressing the unique challenges faced by WLWH, specifically related to the impact of gender-based discrimination, violence, and power dynamics on HIV stigma and disclosure.
Author contributions
TC: Conceptualization, Project administration, Writing – original draft, Writing – review & editing. KK: Conceptualization, Writing – original draft, Writing – review & editing. KG: Conceptualization, Writing – original draft, Writing – review & editing. MF: Conceptualization, Writing – original draft, Writing – review & editing. DS: Writing – review & editing, Writing – original draft. JG: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The contents of this paper are based partly on a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90IFRE0056; PI: Kosyluk). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this paper do not necessarily represent the policy of NIDILRR, ACL, or HHS, and you should not assume endorsement by the Federal Government.
Acknowledgments
We would like to acknowledge Hunter Drake for assisting with the initial adaptation of HOP for HIV; Karah Greene and Ananda Myers for helping to compile and organize relevant literature; and Eric Sumpter, Brianna Duncan, and Elham Azamian Jazi for assistance with manuscript formatting including tables.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Goffman E. Stigma: Notes on the Management of Spoiled Identity. New York, NY: Simon and Schuster (2009).
2. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. (2001) 27(1):363–85. doi: 10.1146/annurev.soc.27.1.363
3. Corrigan PW, Kosyluk KA. Mental illness stigma: types, constructs, and vehicles for change. In: Corrigan PW, editor. The Stigma of Disease and Disability: Understanding Causes and Overcoming Injustices. American Psychological Association (2014). p. 35–56. doi: 10.1037/14297-003
4. Corrigan PW, Rao D. On the self-stigma of mental illness: stages, disclosure, and strategies for change. Can J Psychiatry. (2012) 57(8):464–9. doi: 10.1177/070674371205700804
5. Kerr J, Lelutiu-Weinberger C, Nelson LE, Turan JM, Frye V, Matthews DW, et al. Addressing intersectional stigma in programs focused on ending the HIV epidemic. Am J Public Health. (2022) 112(S4):S362–6. doi: 10.2105/AJPH.2021.306657
6. Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. (2013) 103(5):813–21. doi: 10.2105/AJPH.2012.301069
7. Vogel DL, Bitman RL, Hammer JH, Wade NG. Is stigma internalized? The longitudinal impact of public stigma on self-stigma. J Couns Psychol. (2013) 60(2):311. doi: 10.1037/a0031889
8. Mann CE, Olson MA, Malik HB, Tovey TL. Stories against stigma: comparing efficacy of a perspective-taking intervention to reduce prejudice toward persons with mental illness versus persons with HIV. Stig Health. (2024) 9(3):278. doi: 10.1037/sah0000447
9. Camacho G, Reinka MA, Quinn DM. Disclosure and concealment of stigmatized identities. Curr Opin Psychol. (2020) 31:28–32. doi: 10.1016/j.copsyc.2019.07.031
10. Serpas DG, Ignacio DA, Gabbidon K, Cherry BJ. Ableist microaggressions and psychological distress among adults with disabilities: the role of disability visibility. Rehabil Psychol. (2024). doi: 10.1037/rep0000582
11. Mandalazi P, Bandawe C, Umar E. HIV disclosure: parental dilemma in informing HIV infected children about their HIV status in Malawi. Malawi Med J. (2014) 26(4):101–4.26167257
12. Maiorana A, Zamudio-Haas S, Santiago-Rodríguez EI, Sauceda JA, Rodríguez-Díaz CE, Brooks RA, et al. HIV Disclosure practices to family among Mexican and Puerto Rican sexual minority men with HIV in the continental USA: intersections of sexual orientation and HIV stigma. J Homosex. (2023) 70(9):1911–35. doi: 10.1080/00918369.2022.2043731
13. Logie CH, Wang Y, Lacombe-Duncan A, Wagner AC, Kaida A, Conway T, et al. HIV-related stigma, racial discrimination, and gender discrimination: pathways to physical and mental health-related quality of life among a national cohort of women living with HIV. Prev Med. (2018) 107:36–44. doi: 10.1016/j.ypmed.2017.12.018
14. Valencia-Garcia D, Starks H, Strick L, Simoni JM. After the fall from grace: negotiation of new identities among HIV-positive women in Peru. Cult Health Sex. (2008) 10(7):739–52. doi: 10.1080/13691050802213563
16. Remien RH, Chowdhury J, Mokhbat JE, Soliman C, El Adawy M, El-Sadr W. Gender and care: access to HIV testing, care, and treatment. J Acquir Immune Defic Syndr. (2009) 51:S106–10. doi: 10.1097/QAI.0b013e3181aafd66
17. Sullivan T. The intersection of intimate partner violence and HIV: detection, disclosure, discussion, and implications for treatment adherence. Top Antivir Med. (2019) 27(2):84.31136996
18. Agyarko-Poku T, Bannor R, Sorvor E, Ankobea-Kokroe F. HIV status disclosure and sexual activity among pregnant women in Ghana. AIDS Care. (2023) 35(3):385–91. doi: 10.1080/09540121.2022.2121375
19. Johnson M, Samarina A, Xi H, Valdez Ramalho Madruga J, Hocqueloux L, Loutfy M, et al. Barriers to access to care reported by women living with HIV across 27 countries. AIDS Care. (2015) 27(10):1220–30. doi: 10.1080/09540121.2015.1046416
20. Twimukye A, Alhassan Y, Ringwald B, Malaba T, Myer L, Waitt C, et al. Support, not blame: safe partner disclosure among women diagnosed with HIV late in pregnancy in South Africa and Uganda. AIDS Res Ther. (2024) 21(1):14. doi: 10.1186/s12981-024-00600-z
21. Mittal D, Sullivan G, Chekuri L, Allee E, Corrigan PW. Empirical studies of self-stigma reduction strategies: a critical review of the literature. Psychiatr Serv. (2012) 63(10):974–81. doi: 10.1176/appi.ps.201100459
22. Smart L, Wegner DM. The hidden costs of hidden stigma. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The Social Psychology of Stigma. New York: Guilford Press (2000). p. 220–42.
23. Pachankis JE. The psychological implications of concealing a stigma: a cognitive-affective-behavioral model. Psychol Bull. (2007) 133(2):328. doi: 10.1037/0033-2909.133.2.328
24. Andersson GZ, Reinius M, Eriksson LE, Svedhem V, Esfahani FM, Deuba K, et al. Stigma reduction interventions in people living with HIV to improve health-related quality of life. Lancet HIV. (2020) 7(2):e129–40. doi: 10.1016/S2352-3018(19)30343-1
25. Stangl AL, Atkins K, Leddy AM, Sievwright KM, Sevelius JM, Lippman SA, et al. What do we know about interventions to reduce intersectional stigma and discrimination in the context of HIV? A systematic review. Stig Health. (2023) 8(3):393. doi: 10.1037/sah0000414
26. Conserve DF, Groves AK, Maman S. Effectiveness of interventions promoting HIV serostatus disclosure to sexual partners: a systematic review. AIDS Behav. (2015) 19:1763–72. doi: 10.1007/s10461-015-1006-1
27. Kennedy CE, Fonner VA, Armstrong KA, O’Reilly KR, Sweat MD. Increasing HIV serostatus disclosure in low and middle-income countries: a systematic review of intervention evaluations. AIDS. (2015) 29:S7–23. doi: 10.1097/QAD.0000000000000671
28. Ma PH, Chan ZC, Loke AY. Self-stigma reduction interventions for people living with HIV/AIDS and their families: a systematic review. AIDS Behav. (2019) 23:707–41. doi: 10.1007/s10461-018-2304-1
29. Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. (2013) 16:18734. doi: 10.7448/IAS.16.3.18734
30. Pantelic M, Steinert JI, Park J, Mellors S, Murau F. “Management of a spoiled identity”: systematic review of interventions to address self-stigma among people living with and affected by HIV. BMJ Global Health. (2019) 4(2):e001285. doi: 10.1136/bmjgh-2018-001285
31. Bryant JV, Carcioppolo N, Lun D, Potter J. Entertainment-education to reduce internalized stigma, increase intimate partner status disclosure intentions, and increase antiretroviral medical adherence intentions: a randomized controlled trial targeting black women living with HIV in the southern US. Soc Sci Med. (2023) 327:115945. doi: 10.1016/j.socscimed.2023.115945
32. Bogart LM, Mutchler MG, Goggin K, Ghosh-Dastidar M, Klein DJ, Saya U, et al. Randomized controlled trial of rise, a community-based culturally congruent counseling intervention to support antiretroviral therapy adherence among black/African American adults living with HIV. AIDS Behav. (2023) 27(5):1573–86. doi: 10.1007/s10461-022-03921-0
33. Corrigan PW, Kosyluk KA, Rüsch N. Reducing self-stigma by coming out proud. Am J Public Health. (2013) 103(5):794–800. doi: 10.2105/AJPH.2012.301037
34. Chaudoir SR, Quinn DM. Revealing concealable stigmatized identities: the impact of disclosure motivations and positive first-disclosure experiences on fear of disclosure and well-being. J Soc Issues. (2010) 66(3):570–84. doi: 10.1111/j.1540-4560.2010.01663.x
35. Roe D, Hasson-Ohayon I, Mashiach-Eizenberg M, Derhy O, Lysaker PH, Yanos PT. Narrative enhancement and cognitive therapy (NECT) effectiveness: a quasi-experimental study. J Clin Psychol. (2014) 70(4):303–12. doi: 10.1002/jclp.22050
36. Corrigan PW, Larson JE, Michaels PJ, Buchholz BA, Del Rossi R, Fontecchio MJ, et al. Diminishing the self-stigma of mental illness by coming out proud. Psychiatry Res. (2015) 229(1–2):148–54. doi: 10.1016/j.psychres.2015.07.053
37. Rüsch N, Abbruzzese E, Hagedorn E, Hartenhauer D, Kaufmann I, Curschellas J, et al. Efficacy of coming out proud to reduce stigma’s impact among people with mental illness: pilot randomised controlled trial. Br J Psychiatry. (2014) 204(5):391–7. doi: 10.1192/bjp.bp.113.135772
38. Conley CS, Hundert CG, Charles JLK, Huguenel BM, Al-khouja M, Qin S, et al. Honest, open, proud–college: effectiveness of a peer-led small-group intervention for reducing the stigma of mental illness. Stig Health. (2020) 5(2):168–78. doi: 10.1037/sah0000185
39. Mulfinger N, Müller S, Böge I, Sakar V, Corrigan PW, Evans-Lacko S, et al. Honest, open, proud for adolescents with mental illness: pilot randomized controlled trial. J Child Psychol Psychiatry. (2018) 59(6):684–91. doi: 10.1111/jcpp.12853
40. Qin S, Sheehan L, Yau E, Chen Y, Wang Y, Deng H, et al. Adapting and evaluating a strategic disclosure program to address mental health stigma among Chinese. Int J Ment Health Addict. (2024) 22(3):1029–46. doi: 10.1007/s11469-022-00911-0
41. Modelli A, Candal Setti VP, van de Bilt MT, Gattaz WF, Loch AA, Rossler W. Addressing mood disorder diagnosis’ stigma with an honest, open, proud (HOP)-based intervention: a randomized controlled trial. Front Psychiatry. (2020) 11:582180. doi: 10.3389/fpsyt.2020.582180
42. Sheehan L, Oexle N, Bushman M, Glover L, Lewy S, Armas SA, et al. To share or not to share? Evaluation of a strategic disclosure program for suicide attempt survivors. Death Stud. (2023) 47(4):392–9. doi: 10.1080/07481187.2022.2076266
43. Wingood GM, DiClemente RJ. The ADAPT-ITT model: a novel method of adapting evidence-based HIV interventions. J Acquir Immune Defic Syndr. (2008) 47:S40–6. doi: 10.1097/QAI.0b013e3181605df1
44. DiCarlo AL, Mantell JE, Remien RH, Zerbe A, Morris D, Pitt B, et al. “Men usually say that HIV testing is for women”: gender dynamics and perceptions of HIV testing in Lesotho. Cult Health Sex. (2014) 16(8):867–82. doi: 10.1080/13691058.2014.913812
45. MacQueen KM, Dlamini S, Perry B, Okumu E, Sortijas S, Singh C, et al. Social context of adherence in an open-label 1% tenofovir gel trial: gender dynamics and disclosure in KwaZulu-Natal, South Africa. AIDS Behav. (2016) 20(11):2682–91. doi: 10.1007/s10461-016-1339-4
46. Mackworth-Young CRS, Bond V, Wringe A. Secrets and silence: agency of young women managing HIV disclosure. Med Anthropol. (2020) 39(8):720–34. doi: 10.1080/01459740.2020.1764551
Keywords: HIV, disclosure, women, social stigma, psychosocial intervention, mental disorders
Citation: Chenneville T, Kosyluk K, Gabbidon K, Franke M, Serpas D and Galea JT (2024) Positive, Open, Proud: an adapted disclosure-based intervention to reduce HIV stigma. Front. Glob. Womens Health 5:1469465. doi: 10.3389/fgwh.2024.1469465
Received: 23 July 2024; Accepted: 5 November 2024;
Published: 27 November 2024.
Edited by:
Simon Manga, Cameroon Baptist Convention Health Services, CameroonReviewed by:
Nishanth Krishna Kodyalamoole, Father Muller Medical College, IndiaCopyright: © 2024 Chenneville, Kosyluk, Gabbidon, Franke, Serpas and Galea. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tiffany Chenneville, Y2hlbm5ldmlAdXNmLmVkdQ==
†ORCID:
Tiffany Chenneville
orcid.org/0000-0001-5598-9387
Kristin Kosyluk
orcid.org/0000-0002-9478-3506
Kemesha Gabbidon
orcid.org/0000-0001-9900-4308
Molly Franke
orcid.org/0000-0002-4890-5728
Dylan Serpas
orcid.org/0000-0001-5531-3280
Jerome T. Galea
orcid.org/0000-0001-8732-6959
 Tiffany Chenneville
Tiffany Chenneville Kristin Kosyluk
Kristin Kosyluk Kemesha Gabbidon
Kemesha Gabbidon Molly Franke
Molly Franke Dylan Serpas
Dylan Serpas Jerome T. Galea
Jerome T. Galea