- 1Department of Midwifery, Debre Markos University, Debre Markos, Ethiopia
- 2School of Women’s and Children’s Health, University of New South Wales Sydney, Sydney, NSW, Australia
Introduction: Maternal mortality is a global issue, with developing countries accounting for over 99% of maternal deaths, with 30% of Ethiopian mothers dying from pregnancy-related causes. This study aimed to assess the magnitude, associated factors, and reasons for home delivery among women who gave birth after antenatal care follow-up in the last 6 months in Jabitehnan District, Northwest Ethiopia.
Methods: A mixed community-based study was conducted on women who gave birth after antenatal care follow-up in the last 6 months. Data was collected through face-to-face interviews and structured questionnaires. Bivariate and multivariable logistic regressions were performed to identify factors associated with home delivery. Qualitative data were collected through focus group discussions and in-depth interviews and analyzed using a thematic content analysis method.
Result: In this study, the magnitude of home delivery after ANC follow-up among mothers who gave birth in the last 6 months was 37%, with a 95% CI of 32.5 and 41.5. Pregnancy plan [AOR: 4.56 (2.65, 7.86)], experience of abortion AOR: 3.01 [1.631, (5.55)], ANC follow-up at public hospitals [AOR: 1.89 (1.119, 3.18)], and pregnant mothers visited at home by healthcare providers during their ANC follow-up absent [AOR: 1.61 (1.02, 2.53)] were predictors of home delivery. Poor counseling during ANC, and lack of pregnancy plans, traditions, and beliefs were reasons for home delivery.
Conclusion: The study reveals a high magnitude of home delivery as compared to a study done in Bahir Dar (21.2%). Factors include pregnancy plans, health institution type, abortion experience, and absence from antenatal care. Poor counseling during ANC, and lack of pregnancy plans, traditions, and beliefs were reasons for home delivery. Health professionals should receive training in communication and counseling techniques, and they should encourage mothers to plan their pregnancies and visit facility delivery services during ANC follow-up.
Introduction
Maternal mortality and morbidity are still tragedies for developing countries. Nowadays, around 1,000 maternal deaths happen every day, and more than 99% of maternal mortality occurs in low-income countries (1, 2). The most common risk factors for this tragedy are infection, hemorrhage, obstructed labor, abortion, and hypertension in pregnancy (3). From this, 75% of maternal mortalities are due to direct obstetric causes, which are common in Africa (4, 5).
In developing countries, the majority of maternal mortalities occur in Sub-Saharan Africa (SSA), and the majority are child-bearing women who are in danger of death during labor due to pregnancy-related causes (6). In Ethiopia, slightly over one in 4 live births in the five years preceding the survey were delivered by a skilled provider (28%) or in a health facility (26%). The percentage of live births delivered by a skilled provider remained virtually unchanged for 5 years after 2000, but increased substantially after 2005; from 6% in the 2000 and 2005 EDHS to 10% in the 2011 EDHS, and reached 28% in the 2016 EDHS. A similar trend is observed for the percentage of live births that occurred in a health facility; it increased from 5% in the 2000 and 2005 EDHS surveys, to 10% in the 2011 EDHS, and to 26% in the 2016 EDHS (7).
The percentage of deliveries in a health facility is more than twice from 10% the 2011 EDHS; while home delivery decreased slightly from 90% to the current level of 64%. Even though ANC follow-up and institutional delivery have significant associations, of women attending antenatal care visits, 36% of them end up with home delivery (7).
According to Jabitehnan District Health Office 2018 annual report, has coverage of ANC 87% with low health facility delivery of 54%. Many factors affect the place of delivery like lack of information and adequate knowledge about danger signs during pregnancy and labor, quality of services, site service utilized, and previous experience (8).
Trends and the rates of maternal mortality and level of home delivery and its associated factors are essential for different interventions, resource mobilization, planning, and evaluation of progress towards sustainable development goal 3 (9).
The Federal Ministry of Health/FMOH in Ethiopia has applied multi-pronged approaches to reducing maternal and newborn morbidity and mortality. Improving access and strengthening facility-based maternal services is one such approach, and is also a health sector development plan/HSDP strategic objective (10).
Despite these activities, maternal mortality and morbidity are still high, and they influence the social, political, and economic aspects of the country (2). Even though the problem is high, maternal mortality and morbidity could be lowered by creating different methods, like increasing the quality and number of skilled birth attendants, and by making the health institution more convenient by fulfilling the necessary materials needed for quality delivery services (11). Therefore, to minimize maternal mortality and morbidity, the place of delivery and a safe environment have a significant role in avoiding maternal and neonatal mortality, which is imposed by an unhygienic environment and other technical problems (12).
Therefore, the purpose of this study was to assess the magnitude, associated factors, and reasons for home delivery among women who gave birth after antenatal care follow-up in the last 6 months in Jabitehnan District, Northwest Ethiopia.
Methods
Study area and period
The study was conducted in Amhara regional state, West Gojjam Zone, and Jabitehnan district from September 1 to 30, 2019. This area is surrounding Fenote-Selam Town, located 387 KM and 178 KM from Addis Ababa and Bahir Dar, respectively. It has an estimated area of 1,169.5 km2. The district has 38 kebeles and an estimated total population of 225,558 in 2019. Of this, 113,907 (50.5%) are females. 26,859 (23.58%) are reproductive-age women. The district has 11 health centers, 38 health posts, and six private clinics that provide different maternity and child health services.
Study design
Community-based qualitative and quantitative study methods were employed.
Study participants
The source population was all women who gave birth within the last 6 months of ANC follow-up in the Jabitehnan district. The study population was all women who gave birth within the last 6 months after ANC follow-up in the selected kebeles of the district.
Eligibility criteria
All women who had ANC follow-ups and gave birth in the Jabitehnan district were included in the study. However, all women who were not residents of the Jabitehnan district and all women who were critically ill were excluded from this study.
Sample size determination
The sample size was determined by the single population proportion formula (13). The expected proportion of home delivery (75.3%) from the previous study in the Gozamen district (9) and a 5% confidence limit (margin of error) were used.
Considering a 1.5 design effect and a 10% non-response rate (286 × 1.5 × 0.1), the final sample size was 472.
In the qualitative study, a total of six to eight individuals were conducted with mothers who had home deliveries after their ANC follow-up. A total of 24 women who gave birth at home with three sessions participated in the focused group discussions (FGD) and six women participated in in-depth interviews (IDIs).
Sampling technique
The multistage sampling technique was carried out. First, 25% of the 38 kebeles that are found in the study area were randomly selected with the lottery method, and then study participants were allocated proportionally to each randomly selected kebele of the district to determine the total sample size of the study. Participants were selected using systematic sampling techniques from randomly selected kebele at every second interval (Figure 1).
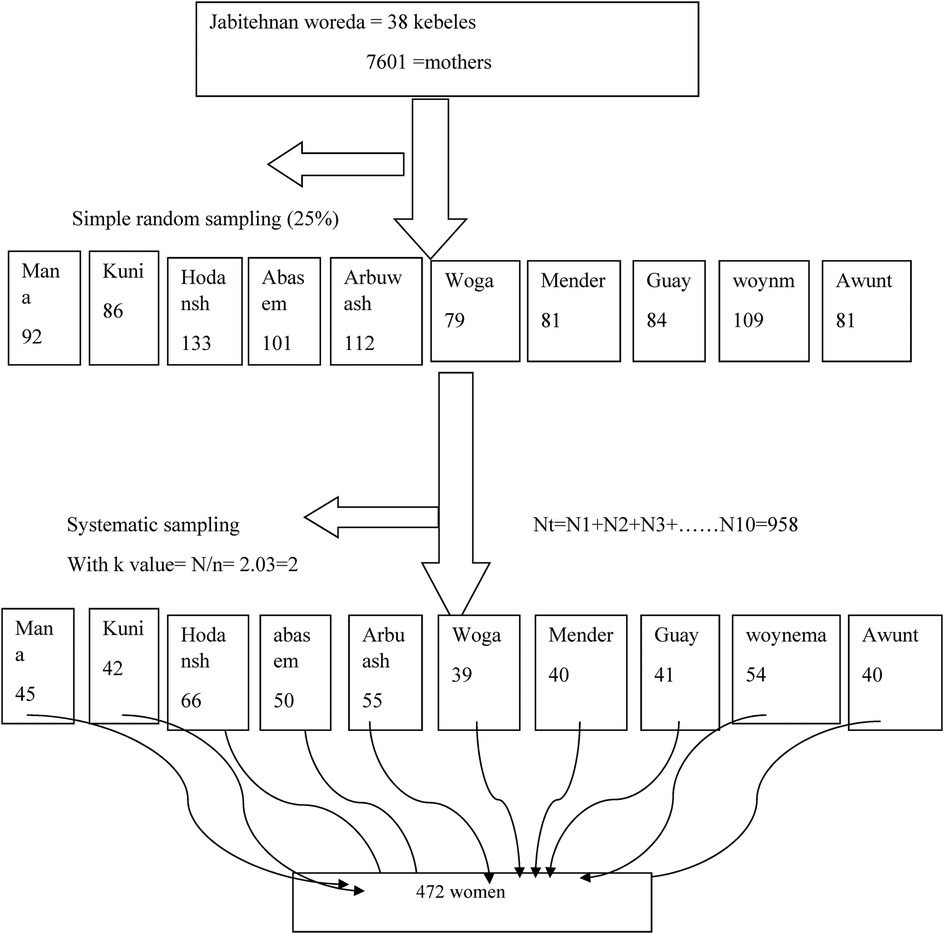
Figure 1. Schematic presentation of the sampling procedure for prevalence and associated factors of home delivery among women who gave birth after antenatal care in the last 6 months of Jabitehnan District, 2019.
A purposive sampling technique was employed to select qualitative study participants. The selection was based on gravid status, age, and educational status. These participants were selected in six kebeles.
Study variables
Dependent variable: home delivery.
Independent variables
Socio-demographic factors: age of mother, marital status, religion, education, occupation, ethnicity, income.
Obstetric history: previous obstetric history, gravidity, parity, the experience of prolonged labor place of the previous delivery, pregnancy plan, place where ANC attends, number of ANC visits, the experience of stillbirth.
Health service-related: time to reach a health facility, media exposure, counseling and communication with health providers, husbands, traditional birth attendants (TBAs), and family influence about the place of delivery preference.
Health service experience: the place of current ANC service, place of recent delivery, time to get ANC, the experience of abortion, privacy protection, and knowledge about the free charge of the service.
Knowledge of obstetric danger signs: excessive vaginal bleeding, blurred vision, convulsion, and high-grade fever.
Discussion habit and maternal decision power on a place of delivery: choice of place of delivery.
Cultural and traditional factors: birth assistant.
Operational definitions
Home delivery: delivery that is not taken place at health facilities (hospitals, health centers, and any private health facilities) (9).
ANC follow-up: pregnant women who have attended antenatal clinics during their recent pregnancy and have attended ANC at least once.
Adequate knowledge of obstetric danger signs: a delivered mother who could be able to mention obstetric danger signs that occur during pregnancy, childbirth, and the postpartum period above the calculated mean could be considered to have adequate knowledge, and those who could state below the mean were considered to have inadequate knowledge (14).
TBAs: a birth attendant who initially acquired the ability by delivering babies herself (9).
Access to health services: mothers have access to health services if the distance to a health institution takes less than 1 h.
Good waiting time to get ANC: for pregnant women who have attended antenatal care waiting time is less than one hour during the visit (15).
Data collection and data quality control
To assure quality, the data were collected through face-to-face interviews by eight trained midwives after 2-day data collection training was given to them together with two senior public health officer supervisors. The questionnaire for the quantitative study was structured and adapted from related literatures (9, 14, 15). The questionnaire was also prepared in English and translated to the local (Amharic) language and then translated back to English. A pretest was conducted on 5% of the respondents in the adjacent district, Bure to ensure the consistency of the questionnaire, and then the questionnaire was modified accordingly., but the results of the pretest were not included in the final analysis. For the qualitative study, focus group discussions and interviews were used to collect data. The data collection checklist contained open-ended questions and was adapted from previous similar studies (9, 16). The FGD and IDIs were intended to explore experiences, feelings, attitudes, thoughts, and ideas of discussants on determinants of home delivery.
Data processing and analysis
Epi Info version 7 software was used for data entry, and SPSS version 24 was used for analysis. Bivariate logistic regression was employed to identify an association between independent and dependent (home delivery; Yes = 1, No = 0) variables. Variables with a P-value ≤ 0.25 in the bivariate logistic regression analysis were fitted into the multivariable logistic regression model. The 95% confidence interval of the odds ratio was computed, and a variable with a P-value < 0.05 in the multivariable logistic regression analysis was considered statistically significant.
Qualitative: In addition to recording in an audio file, field notes were taken for each interview. The audio file, consent form, field note, and in-depth enrollment form were coded properly and consistently. Every day, every recorded audio file was checked for its appropriateness in terms of proper coding, signed consent, clear audibility, level of depth questioning, and consistency of the codes given for the audio file, consent, and field note. Finally, the data were analyzed under selected themes and summarized manually.
Ethical considerations
Ethical clearance for the study was obtained from the Research Institutional Research Ethics Review Committee of Debre Markos University (IRERC). Written and verbal informed consent was obtained from participants to confirm their willingness. Participants were interviewed in a separate room, and the anonymity and confidentiality of the data providers were strictly maintained.
Results
Quantitative study
Socio-demographic characteristics of the respondents
About 459 respondents participated in this study, with a response rate of 97.2%. The mean age of the respondents was 28 years. All respondents were Orthodox (459/100%), similar to all of the respondents' ethnicities. About 447 (97.3%) were married (Table 1).
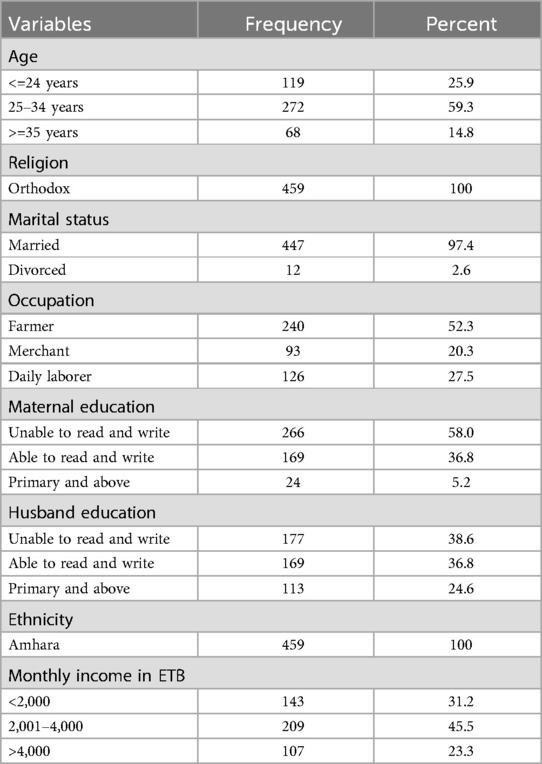
Table 1. Socio-demographic characteristics of women who had home delivery after ANC follow-up in Jabitehnan District Northwest Ethiopia, 2019.
Obstetric and gynecologic-related characteristics of respondents
About 56% of the respondents were below gravida four, and 40.1% had two to four children. About 13.5% of the respondents attended ANC only once, and 61.4% of the respondents had completed ANC follow-ups. Only 192 (41.8%) of the women were decision-makers (Table 2).
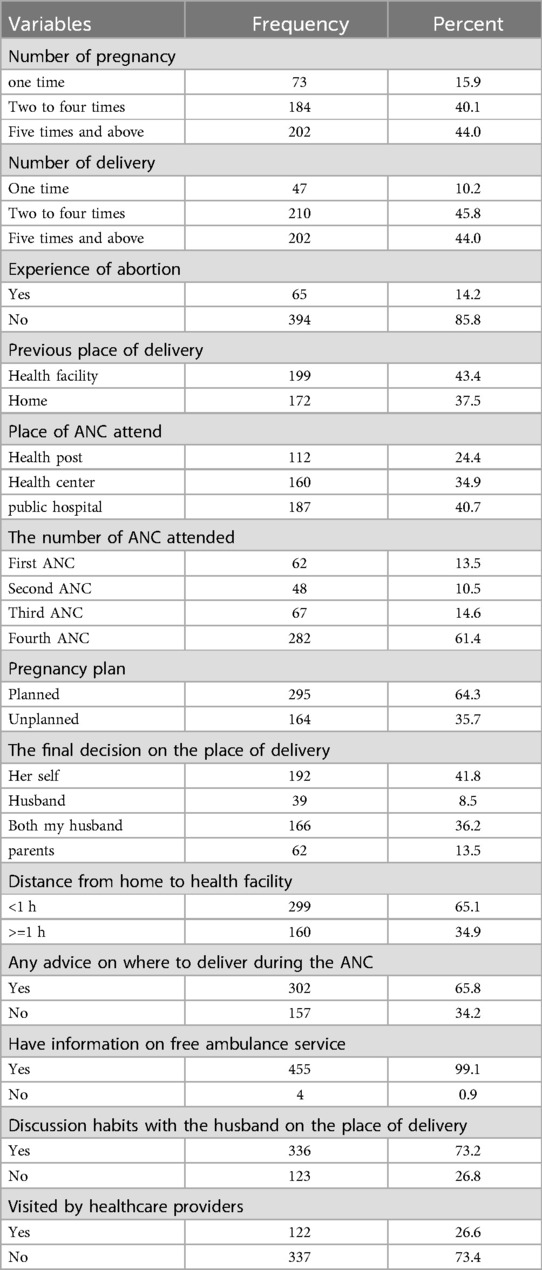
Table 2. Obstetric and other health-related characteristics of women who had home delivery after ANC in Jabitehnan District, Norwest Ethiopia, 2019.
Knowledge of the respondents
Around 26.6% of study participants had adequate knowledge about the overall key danger signs of obstetric complications that can occur during pregnancy, labor, delivery, and the postpartum period (Table 3).
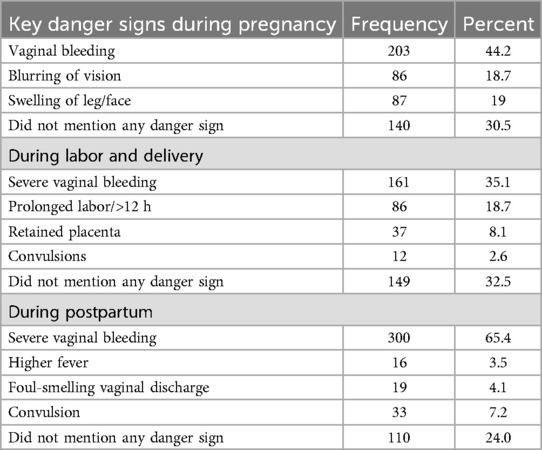
Table 3. Knowledge of key obstetric danger signs of home delivery after ANC and associated factors in Jabitehnan District Northwest Ethiopia, 2019.
Home delivery
In this study, the magnitude of home delivery after ANC follow-up among mothers who gave birth in the last 6 months was 37%, with a 95% CI of 32.5 and 41.5.
Factors associated with home delivery
After controlling the effect of other variables with logistic regression analysis, pregnancy plan [AOR: 4.562 (2.646, 7.864)], experience of abortion [AOR: 3.008 (1.631, 5.545)], place of ANC attendance [AOR: 1.886 (1.119, 3.179)], and visited by health care providers during ANC follow-up absence [AOR: 1.609 (1.023, 2.531)] were predictors of home delivery. Poor counseling during ANC, lack of planning, traditions, and beliefs were reasons for home delivery (Table 4).
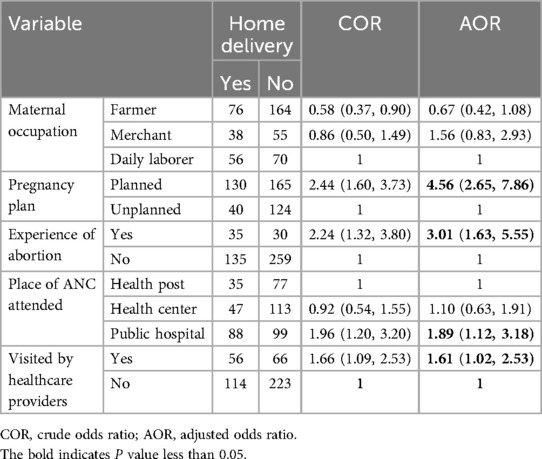
Table 4. Multivariable logistic regression analysis of home delivery and associated factors in Jabitehnan District, Northwest Ethiopia, 2019.
Qualitative study
Socio-demographic characteristics
About 30 study respondents participated in this study. From these respondents, 19 participants were between the ages of 20 and 29 years old; 17 participants were unable to read or write; and 27 participants were in paraII and above.
Simple and sudden onset of labor
Pregnant women who had an ANC follow-up had full information on their expected date of delivery.
One woman explained: “I presumed I had 10 days more, but I was mistaken. Consequently, labor started unexpectedly, so I gave birth at home with the help of my grandmother. I was not aware of my expected date of delivery. But I planned to give birth in the health facility with the help of health providers” (Participant # 9, age 26, and Para ii).
Infrastructure and accessible transport
Accessibility to health facilities is a crucial issue in choosing health facility delivery. A 32-year-old woman asserted, “Getting birth is an expected event and difficult to plan. It was midnight and raining when my labor started. My husband and relatives searched for a vehicle to take me to the health facility. But they could not get it yet. Walking on foot was not possible. Therefore, my last option was to call neighbors’ old women to help me and give birth at home” (Participant # 12, Para i).
Similarly, a 28-year-old woman who gave birth at home clearly stated that “it is good to give birth at the health center. But the distance from my home to this health center is far, and the ambulance service is not easily accessible. Therefore, unless labor becomes difficult, it is better to give birth at home” (Participant # 13, Para ii).
Counseling during antenatal care follow-up
ANC follow-up is a golden time for health providers to enhance health facility delivery. But a 24-year-old mother said, “I got birth at home. No one offered me a piece of advice on the importance of giving birth in a health center rather than giving vaccinations, and some tablets attended ANC three times regularly. Going through, I did not remember health care providers counseling me on the place of delivery” (Participant # 28, para v).
A 34-year-old woman explained regarding time: “Why do I spend my time visiting the health facility? Healthcare providers did not tell me something different. The follow-up was the same. I believe it is not as important for a healthy mother unless she gets sick” (Participant # 21, para ii).
Normal pregnancy during antenatal care follow-up might be considered an indication of normal delivery. One woman asserted that “heath providers can predict any future birth complications. Therefore, if the provider told me my pregnancy was good, what is the importance of birth in a health facility? I understood the facility delivery required when the provider told me that my pregnancy is not normal” (Participant # 7, para iv).
Previous experience regarding health care provision motivated me to give birth at home. One 42-year-old woman stated, “I have delivered my previous child at the health center. It was at night, and the health worker with untidy hair rising made me on the delivery coach; he left me alone for about 15 min and slapped and insulted me during delivery. Therefore, if the practice is like this, why should I go to the health center?”
Traditions and beliefs
The existence of psychological and social gaps between the community and healthcare providers may be a barrier to seeking facility delivery. Seven women said, “Giving birth is not a disease; it is a natural life. Therefore, facility delivery is only for those unable to deliver normally and those who had the experience of stillbirth and spontaneous abortion previously” (Participant # 16, 12, 19, 3, 6, 11, 5).
Many participants believed traditional birth attendants were comfortable caregivers. Some women said that “I gave birth by traditional birth attendant without complications or difficulty of labor” (participant #s 1, 4, 18, 23, 26, 29, 27, 30, 21). Some explained the issue of privacy based on their experience and said, “Health providers are many in number at the delivery room; they took away privacy and performed several physical vaginal examinations, which were uncomfortable; therefore, how can I go to a health facility knowing what my elder daughter has experienced?” (Participant # 8, 17, 22, 24, 6, 2).
Discussion
The magnitude of home delivery in this study was 37% [95% CI: 32.5%, 41.5%] which was in line with a study conducted in Adigrat (35%) (17), Arbaminch (39.9%) (18), and Nepal district (33%) (19).
In this study, home delivery is lower than in the 2016 Ethiopian demographic health survey (74%) (7) and the study was done among women who booked ANC in the Gozamin district (75.3%), Fogera district (68.4%), and Dodota (81.8%), in Ethiopia (7, 9, 11, 20). This difference might be due to time, which could be the government and other concerned bodies investing in different interventions to reverse the problem and study method, the data collection tools, and huge geographical coverage, particularly the Ethiopian demographic health survey. This study was also lower than the study conducted in Nyandarua, South District, Kenya (52%) (21). This could be due to different tribes with different cultural beliefs.
On the other hand, the magnitude of home delivery is higher than the findings of a study conducted in Bahir Dar town (21.2%), and Debre Markos town (19.5% and 25.3%) (15, 22, 23). This difference could be due to the residents having better infrastructure, accessibility, and education since the current study area is the rural community of Jabitehnan district. Similarly, the study was conducted in Tanzania (21.4%) (24). This might be due to the difference in health care services and the differences in culture. The previous study was conducted in the urban community of Dodoma region which might create media exposure, adequate health information, and better accessibility.
In the current study women who had unplanned pregnancies were 4.56 times more likely to have a home birth as compared with women who had planned pregnancies. This study was supported by studies done in Debre Markos town (15, 25). This might be due to the plan to have a child who particularly needs psychological and mental readiness. Again, planned pregnancy indicates the presence of a support person, either the husband or partner, which means having a chance to share ideas. Consequently, if pregnancy is planned and supported, the chance of seeking facility delivery increases. This is also supported by those women who were unaware of the expected date of delivery and explained (Participant # 9, aged 26, para ii).
In the current study, the type of health institution for antenatal care follow-up was also found to be another predictor of home delivery. Attending ANC at a health post was 1.89 times more likely to give birth at home than those women who were attending ANC at a public health hospital. This is because in the hospital, most of the time there are midlevel and senior educated and experienced health professionals that enable them to receive proper counseling during ANC at the place of delivery, while in health care, a lack of such professionals and investigations led to an increase in home delivery (15).
Women who had no abortion experience were 3.01 times more likely to have home deliveries as compared to those who had no abortion history. The possible reason might be that learning from exposure might lead them to seek facility delivery, so those who had not experienced a problem previously may have high home delivery. This is supported by one's belief, which is learned from exposure to a problem (Participant # 16, 12, 19, 3, 6, 11, 5).
Another associated factor for this study was that visits by health care providers during ANC follow-up absence were 1.61 times more likely to give birth at home as compared with their counterparts. The possible explanation could be that healthcare providers might not arrive at a consensus regarding the importance of the service and the complications of home delivery. This idea was supported by one study participant (participant # 21, Para ii).
Recall bias was the limitation of the study since the respondents were requested to respond about the events that happened 6 months prior to this study; high numbers of those unable to read and write may affect the study outcome.
This study's strengths included its community-based design, which improved the findings' generalizability by addressing mothers who were unable to visit healthcare facilities, and its mixed-methods data, which can address research questions that cannot be satisfactorily answered by using only qualitative or quantitative data collection techniques.
Conclusion and recommendations
The study reveals a high magnitude of home delivery despite national expectations. Factors include pregnancy plans, health institution type, abortion experience, and absence from antenatal care. Poor counseling during ANC, lack of planning, traditions, and beliefs were reasons for home delivery. The government should increase awareness of the importance of planned pregnancy. Other stakeholders should create training in client-provider communication and counseling skills for health professionals. Healthcare professionals should take the opportunity to motivate mothers to attend facility delivery services during ANC follow-up.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Research Institutional Research Ethics Review Committee of Debre Markos University (IRERC). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. TZ: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Software, Supervision, Writing – original draft. AA: Conceptualization, Data curation, Methodology, Writing – original draft. BM: Conceptualization, Formal Analysis, Methodology, Project administration, Writing – review & editing. LZ: Writing – review & editing, Conceptualization, Data curation. GK: Conceptualization, Formal Analysis, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. EDHS E. Demographic and health survey 2016: key indicators report. DHS Program ICF. (2016) 363:364.
3. Federal Democratic Republic of Ethiopia moH, editor. Basic emergency obstetric and newborn care. (2014).
4. USAID S, MOH U, UNFPA U, EHNRI C. Ethiopia Demographic and Health Survey 2011. Calverton, Maryland, USA: Central Statistical Agency Addis Ababa, Ethiopia ICF International (2012).
6. Requejo JH, Bryce J, Barros AJ, Berman P, Bhutta Z, Chopra M, et al. Countdown to 2015 and beyond: fulfilling the health agenda for women and children. Lancet. (2015) 385(9966):466–76. doi: 10.1016/S0140-6736(14)60925-9
7. Central Statistical Aency Addis Ababa TDPIR. Maryland, USA: Ethiopia Demoraphic and Health Survey. (2016).
9. Mekonnen Y, Ayichiluhm M, Dejenu G. Prevalence and determinants of home birth after antenatal care attendance in Gozamin District, Northwest Ethiopia. Health Sci J. (2015) 9(6):1.
11. Fikre AA, Demissie M. Prevalence of institutional delivery and associated factors in Dodota Woreda (District), Oromia Regional State, Ethiopia. Reprod Health. (2012) 9(1):33. doi: 10.1186/1742-4755-9-33
13. Suresh K, Chandrashekara S. Sample size estimation and power analysis for clinical research studies. J Hum Reprod Sci. (2012) 5(1):7. doi: 10.4103/0974-1208.97779
14. Amenu G, Mulaw Z, Seyoum T, Bayu H. Knowledge About Danger Signs of Obstetric Complications and Associated Factors among Postnatal Mothers of Mechekel District Health Centers, East Gojjam Zone, Northwest Ethiopia, 2014. Scientifica (2016).
15. Kasaye HK, Endale ZM, Gudayu TW, Desta MS. Home delivery among antenatal care booked women in their last pregnancy and associated factors: community-based cross sectional study in Debremarkos town, North West Ethiopia, January 2016. BMC Pregnancy Childbirth. (2017) 17(1):225. doi: 10.1186/s12884-017-1409-2
16. Adinew YM, Assefa NA. WhyDo Some Ethiopian Women Give Birth at Home after Receiving Antenatal Care? Phenomenological Study. (2018) 2018, Article ID 3249786, 8 pages.
17. Hiluf M, Fantahun M. Birth preparedness and complication readiness among women in Adigrat town, north Ethiopia. Ethiop J Health Dev. (2008) 22(1):14–20. doi: 10.4314/ejhd.v22i1.10057
18. Workineh Y, Hailu D, Gultie T, Degefu N, Mihrete M, Shimeles M, et al. Knowledge of obstetric danger signs and its associated factors in Arba Minch Town, Ethiopia. Am J Health Res. (2014) 2(5):255–9. doi: 10.11648/j.ajhr.20140205.16
19. Misra R, Chaurasia N. Utilization of safe motherhood services in Jhorahat PHC area of Morang district, Nepal. Am J Public Health Res. (2015) 3:123–9.
20. Desalegn E, Mekonnen A, Abeje G. Place of delivery after antenatal care: the case of Fogera district, Amhara region, North West, Ethiopia; 2013. J Gynecol Obstetr. (2014) 2(1):1–6. doi: 10.11648/j.jgo.20140201.11
21. Wanjira C, Mwangi M, Mathenge E, Mbugua G. Delivery practices and associated factors among mothers seeking child welfare services in selected health facilities in Nyandarua South District, Kenya. BMC Public Health. (2011) 11(1):360. doi: 10.1186/1471-2458-11-360
22. Bayu H, Adefris M, Amano A, Abuhay M. Pregnant women’s preference and factors associated with institutional delivery service utilization in Debra Markos town, North West Ethiopia: a community based follow up study. BMC Pregnancy Childbirth. 15(1):15. doi: 10.1186/s12884-015-0437-z
23. Abeje G, Azage M, Setegn T. Factors associated with institutional delivery service utilization among mothers in Bahir Dar City administration, Amhara region: a community based cross sectional study. Reprod Health. (2014) 11(1):22. doi: 10.1186/1742-4755-11-22
24. Ngowi AF, Kamazima SR, Kibusi S, Gesase A, Bali T. Women’s determinant factors for preferred place of delivery in Dodoma region Tanzania: a cross sectional study. Reprod Health. (2017) 14(1):112. doi: 10.1186/s12978-017-0373-7
Keywords: home delivery, magnitude, Jabitehnan, District, Ethiopia
Citation: Aynalem BY, Zerihun T, Alemu AA, Meselu BT, Zeleke LB and Kassa GM (2024) Home delivery and associated factors among women who gave birth after antenatal care follow-up in the last 6 months in Jabitehnan District, Northwest Ethiopia: mixed community-based study. Front. Glob. Womens Health 5:1458453. doi: 10.3389/fgwh.2024.1458453
Received: 2 July 2024; Accepted: 22 November 2024;
Published: 6 December 2024.
Edited by:
Mesfin Tadese, Debre Berhan University, EthiopiaReviewed by:
Ageeth Rosman, Rotterdam University of Applied Sciences, NetherlandsMastewal Belayneh Aklil, University of Gondar, Ethiopia
Copyright: © 2024 Aynalem, Zerihun, Alemu, Meselu, Zeleke and Kassa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bewket Yeserah Aynalem, YnkxMjNiZXdrZXRAZ21haWwuY29t
 Bewket Yeserah Aynalem
Bewket Yeserah Aynalem Tamene Zerihun1
Tamene Zerihun1 Liknaw Bewket Zeleke
Liknaw Bewket Zeleke