- 1Department of Pediatrics and Child Health Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Department of Emergency and Critical Care Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 3Department of Surgical Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 4Department of Medical Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 5School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 6Department of Clinical Midwifery, School of Midwifery, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: During the Coronavirus Disease 2019 (COVID-19) pandemic, intimate partner violence increased globally, but most notably in Africa. Conditions such as movement restrictions, staying home, and school closures increased the risk of domestic violence against women. Intimate partner violence is violence demonstrated by an intimate partner against women including physical, sexual, and psychological violence. Despite existing laws against intimate partner violence in Ethiopia, enforcement by law and the judicial system remains inadequate. Thus, this research aims to identify factors contributing to intimate partner violence among women during the COVID-19 pandemic, drawing insights from the current literature.
Method: We searched electronic databases, including PubMed, Google Scholar, CINAHL, Cochrane, and others. Two reviewers separately carried out the search, study selection, critical appraisal, and data extraction. A third party was involved in resolving disagreements among the reviewers. All 10 studies included in this study were published in English, with publication dates before 25 February 2024. Articles lacking an abstract and/or full-text, studies that did not identify the intended outcome, and qualitative studies were excluded from the analysis. A Microsoft Excel checklist was used to extract the data, which were then exported to STATA 11. I2, funnel plots, and Egger's test were employed to measure heterogeneity and detect publication bias, respectively. A random-effects model was used to estimate the pooled prevalence of intimate partner violence and associated factors among women during the COVID-19 pandemic.
Result: The meta-analysis includes a sample size of 6,280 women from 10 articles. The pooled prevalence of intimate partner violence and associated factors among women during the COVID-19 pandemic was found to be 31.60% (95% CI: 21.10–42.11) and significant factors were partner alcohol use with a pooled odds ratio of 1.93 (95% CI: 1.60–2.23), income loss during the COVID-19 pandemic with a pooled odds ratio of 9.86 (95% CI: 6.35–15.70), partner’s literacy level/education status with a pooled odds ratio of 2.03 (95% CI: 1.57–2.63), and decision-making in the household with a pooled odds ratio of 1.82 (95% CI: 1.33–2.50).
Conclusion: This systematic review and meta-analysis found preliminary evidence that intimate partner violence increased during the COVID-19 pandemic. A partner who has a history of alcohol use, women who had lost income during COVID-19, a partner who has no formal education, and household decisions made by the husband alone were statistically significant factors for intimate partner violence during the COVID-19 pandemic. This implies that the health sector must play a significant role in providing women who are victims of violence with comprehensive healthcare, advocating that violence against women should be viewed as unacceptable, and improving literacy to minimize the consequences of intimate partner violence among women.
Introduction
The Coronavirus Disease 2019 (COVID-19) outbreak was first detected in Wuhan City, Hubei Province, China (1) and was proclaimed a global pandemic by the World Health Organization (WHO) on 11 March 2020 (2) because of the virus's high severity and ease of transmission, which resulted in an estimated 7 million infections and almost half a million deaths (3). As a result of this, nations all over the globe implemented various preventative actions to assist in stopping the spread. These measures included limiting population movement, isolating people at home, and closing schools as well as other social services, some of which have been demonstrated to increase the likelihood of women being victims of domestic violence (4). Intimate partner violence (IPV) is defined as “violence demonstrated by an intimate partner against women including physical, sexual, and psychological violence or controlling behaviors that cause physical, sexual, or psychological harm” (5). Intentional use of physical force is considered “physical violence,” while forcing a woman to engage in a sexual act is referred to as “sexual violence” (6). “Emotional,” “psychological,” or “verbal” violence refers to acts of intimidation, control over activities, isolation, name-calling, and threats (7). During the COVID-19 pandemic, IPV increased globally, but most notably in Africa (8). In their lives, 35% of women globally have either been victims of physical or sexual abuse at the hands of an intimate partner or of non-partner sexual violence (9). Approximately 27% of women between the ages of 15 and 49 who have been in a relationship worldwide claim that their intimate partner has physically or sexually abused them (10). The prevalence was much greater in sub-Saharan Africa, where 46.5% of women had been the victim of intimate partner violence (8). Situations such as being confined to one's house, moving limitations, and closing schools raise the possibility of domestic violence against women (11, 12). IPV has been linked to long-term problems with mental, physical, and reproductive health (13–15). Women who experience IPV also have the risk of conflicts with others and developing social disorders (16, 17). During the COVID-19 pandemic restrictions, the majority of IPV victims were women whose spouses had financial and behavioral control, as well as women who had partners who consumed alcohol (18). In Ethiopia, in particular, similar measures were taken to reduce the COVID-19 pandemic's spread. These measures included closing educational institutions, workplaces, and recreational facilities; restricting travel; setting up isolation and quarantine facilities; and declaring a national emergency (19, 20). However, the federal government did not respond to any of the consequences of these preventative actions, such as IPV against women (21). IPV was more common during the COVID-19 period, even though Target 5.2 of the Sustainable Development Goals (SDG) 5 is intended to eradicate all kinds of violence against all women by 2030 (22). While some studies have reported determinants of intimate partner violence and associated factors among women during the COVID-19 pandemic in Ethiopia, none of them have systematically reviewed intimate partner violence and associated factors among women during the COVID-19 pandemic. These differ and are not uniform throughout the region. To end violence against women, public health stakeholders need to be aware of the impact of the COVID-19 pandemic on intimate partner violence as well as the most up-to-date information on the prevalence of IPV. The reported determinants include economically disadvantaged women, women of a young age, non-educated women, women whose partners control behavior, women who have partners who drink alcohol and/or use substances, and women who spend more time at home (23–32). Thus, the current work aims to identify relevant studies and summarize major determinants of intimate partner violence and associated factors among women during the COVID-19 pandemic in Ethiopia. Furthermore, the review's findings will broaden our understanding of the issue and provide crucial information to planners of programs, legislators, and other interested parties who want to see an end to violence against women in Ethiopia.
Methods
Searching strategy and data source
Following the criteria of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA), a systematic review of relevant papers was carried out (33). A thorough search of all English-language publications released before 25 February 2024 was conducted using PubMed, Google, Google Scholar, Cochrane Library, and CINAHL. In addition, we searched the reference lists of the included studies in addition to these databases to find possible literature. The search was performed using key terms such as intimate partner violence, violence against girls, perinatal intimate partner violence, reproductive age women, pregnant women, postpartum mothers, married women, prenatal clients, during COVID-19 pandemic, impact of the COVID-19 pandemic, associated factors, risk factors, prevalence, predictors, determinants, and Ethiopia separately and/or in combination using the Boolean operators “OR” or “AND.” Two of the authors searched independently. To make the process of selecting articles and managing citations easier, articles that were extracted from the databases were imported into Endnote version X9.
Study selection and eligibility criteria
Studies that were conducted in Ethiopia with the main goal of examining intimate partner violence and related factors were included in this review and meta-analysis. Studies published in English, conducted at both facility and community levels, and related to reproductive age, pregnant women, postpartum mothers, perinatal clients, and married women were included. The titles, abstracts, and full review of the research were used to evaluate the studies for inclusion criteria prior to their inclusion in the final review. Where the required data were not available (articles lacking abstract and/or full-text, the study that did not meet the inclusion criteria, studies that did not identify the intended outcome), the study was excluded from the review.
Outcome measure
The primary outcome of this review was the prevalence of intimate partner violence among women during the COVID-19 pandemic (the response to each item was either “Yes” or “No” for any form of physical, sexual, and emotional violence against women by an intimate partner) (5). An intimate partner is a person who has an intimate relationship with a woman either in the form of marriage or in the form of cohabitation (34). The factors linked to intimate partner violence among women during the COVID-19 pandemic were the second outcome of this review. A factor was included in this review and meta-analysis if it was found to be linked with intimate partner violence among women during the COVID-19 pandemic in two or more research articles; however, if it was found to be connected with intimate partner violence in just one study, it was not taken into consideration. The age of the woman, residence, income loss during COVID-19, partner alcohol use, partner substance use, marital status, women's education, partner education, decision-making in the household, age of the husband, partner smoking habit, women's occupation, and history of abortion were the exposure variables included.
Quality assessment and data extraction
Two reviewers independently assessed the quality of the studies by adopting a specific protocol. The criteria proposed by the Joanna Briggs Institute (JBI) were used to assess the quality of the included studies (35). The following eight parameters were assessed: inclusion criteria, study subject and setting description, valid and reliable exposure measurement, objective and standard criteria applied, confounder identification, confounder handling strategies, outcome measurement, and appropriate statistical analysis. When a study achieved a quality assessment indicator score between 75% and 100%, it was categorized as high quality; scores between 50% and 74% indicated moderate quality, and scores between 0% and 49% indicated low quality. Therefore, if a study achieved a quality assessment indicator score of 50% or more, it was categorized as low risk (Table 1). A third reviewer was involved in the discussion process to resolve any discrepancies between the two reviewers. The names of the author(s), the year of publication, the study period, the study design, the sample size, the prevalence of intimate partner violence, and related factors were all gathered using a predetermined data extraction format.
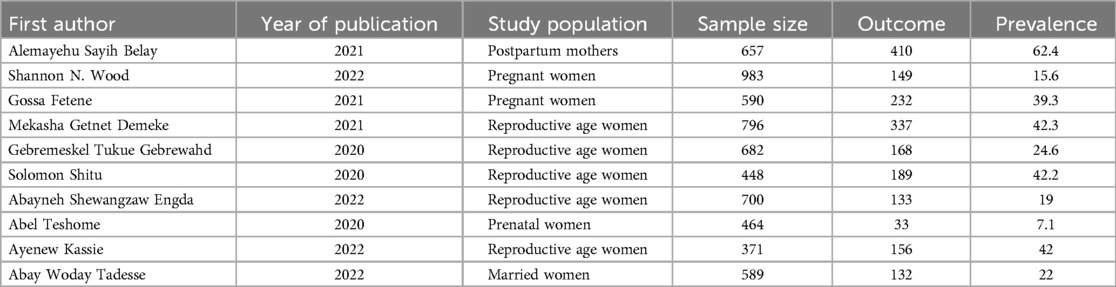
Table 1. Characteristics and quality status of the studies included to assess the pooled prevalence of intimate partner violence among women during the COVID-19 pandemic in Ethiopia.
Publication bias and heterogeneity
Funnel plots were scattered and their asymmetry was checked to determine whether publication bias existed. The Egger's test was estimated (36). The statistical significance of publication bias was determined via a p-value of <0.05. I2 test statistics were used to verify the heterogeneity of the studies following the authors' thorough review of each one. The overall variation across studies was described by I2 statistics. I2 test statistics of <50%, 50%–75%, and >75% were designated as low, moderate, and high heterogeneity, respectively (37).
Statistical methods and analysis
Statistical analysis was carried out using STATA version 11. Initially, data were entered into Microsoft Excel and then exported to STATA version 11 for further analysis. The effect size of the meta-analysis was the prevalence of intimate partner violence and the odds ratio (OR) of the associated factors. A weighted inverse variance random-effects model was used as a method of analysis (38). By examining the adjusted ORs and 95% confidence intervals (CIs) provided by each study, we were able to determine associated risk factors for intimate partner violence among women who satisfied the eligibility requirements for the meta-analysis. The study population was used to do subgroup analysis. The effect of selected associated factors was analyzed using separate categories of meta-analysis. The findings of the review and meta-analysis were presented using tables, forest plots, OR, and 95% CIs.
Results
Study searches and selection
In the initial search, we found a total of 4,643 records from different electronic search databases which included PubMed (11), Google Scholar (4,618), and the Cochrane Library (14). From these, 1,917 duplicate records were removed and 2,690 records were excluded after screening by title and abstracts. After determining the eligibility of the 36 remaining records based on their full texts, 26 records were eliminated based on the inclusion and exclusion criteria. Finally, 10 studies were considered for the final review and meta-analysis (23–30, 31, 32) (Figure 1).
Characteristics of the studies
Every study that was part of this review was cross-sectional in nature. The analysis had a total of 6,280 women participants. The included studies reported sample sizes ranging from 371 (27) to 983 (31). Of the women in the included study, 50% were of reproductive age, 20% were pregnant, and the remaining women were postpartum mothers, perinatal clients, or married women. One study was conducted at the national level, two more were carried out in central Ethiopia, one study was carried out in eastern Ethiopia, three more were carried out in northern Ethiopia, and the final three were carried out in southern Ethiopia. Intimate partner violence was found to be most common in southern Ethiopia (62.4%) and least common in central Ethiopia (Addis Ababa) (7.1%) (Table 1).
Prevalence of intimate partner violence among women during the COVID-19 pandemic
To determine the pooled prevalence of intimate partner violence among women during the COVID-19 pandemic, 10 studies were included in the analysis. The 10 studies that were utilized to estimate the pooled prevalence of intimate partner violence among women during the COVID-19 pandemic showed a very high level of heterogeneity (p < 0.000 and I2 = 99.1%). Using the random-effects model, the pooled prevalence of intimate partner violence among women during the COVID-19 pandemic was 31.60% (95% CI: 21.10–42.11) (Figure 2). Based on participant characteristics, a subgroup analysis was conducted to compare the prevalence of intimate partner violence among women during the COVID-19 pandemic. Thus, the pooled prevalence estimated for characteristics was high in postpartum mothers [62.40% (95% CI: 58.70–66.11)], and the least was in perinatal women [7.11% (95% CI: 4.77–9.45)] (Figure 3).
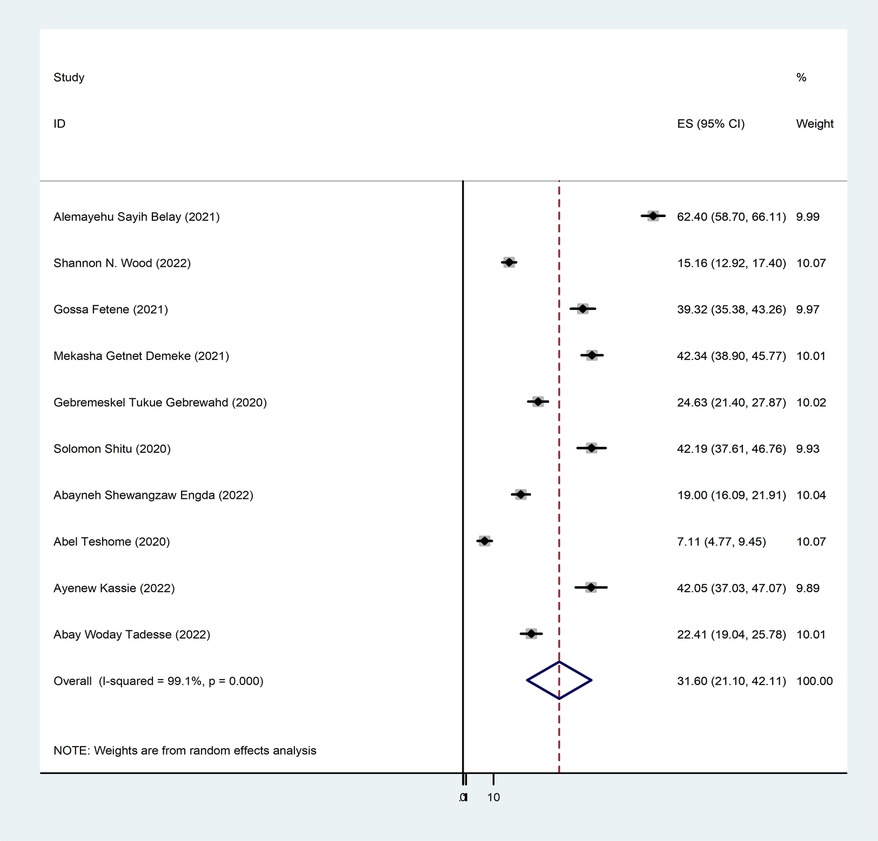
Figure 2. Forest plot pooled prevalence of intimate partner violence among women during the COVID-19 pandemic in Ethiopia, 2024.
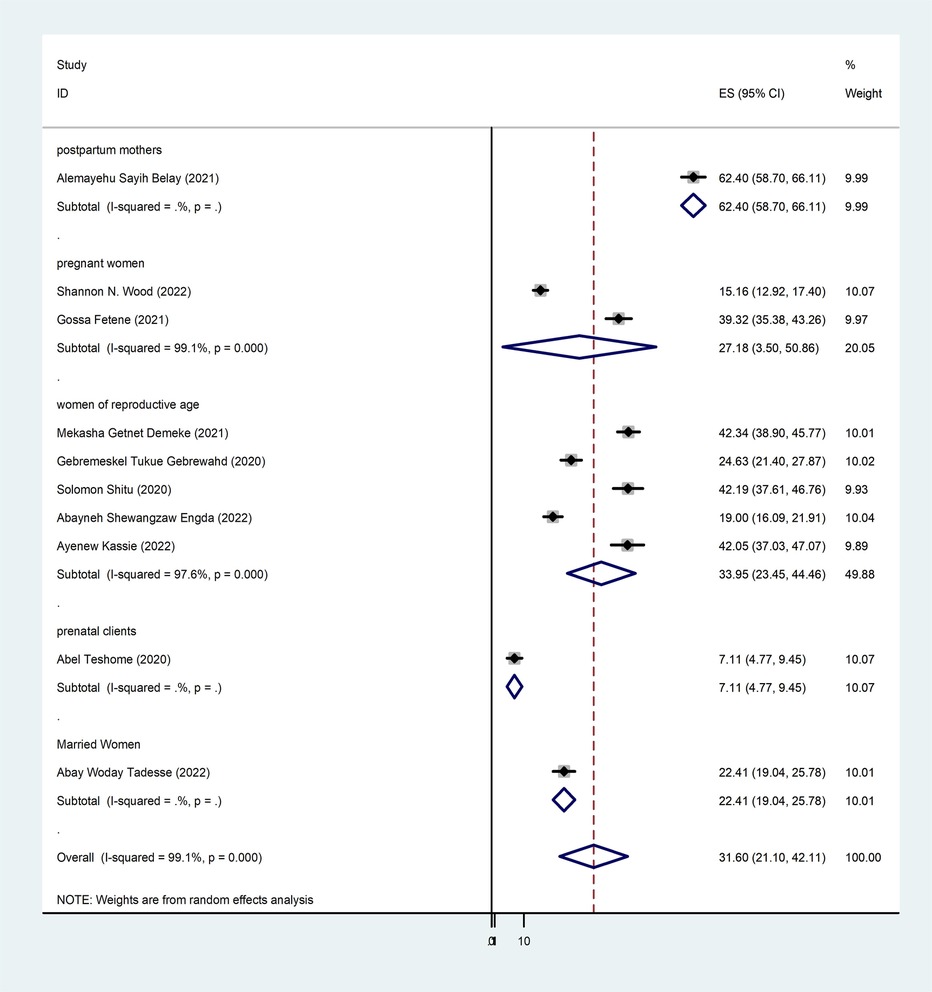
Figure 3. Forest plot subgroup prevalence of intimate partner violence among women during the COVID-19 pandemic in Ethiopia, 2024.
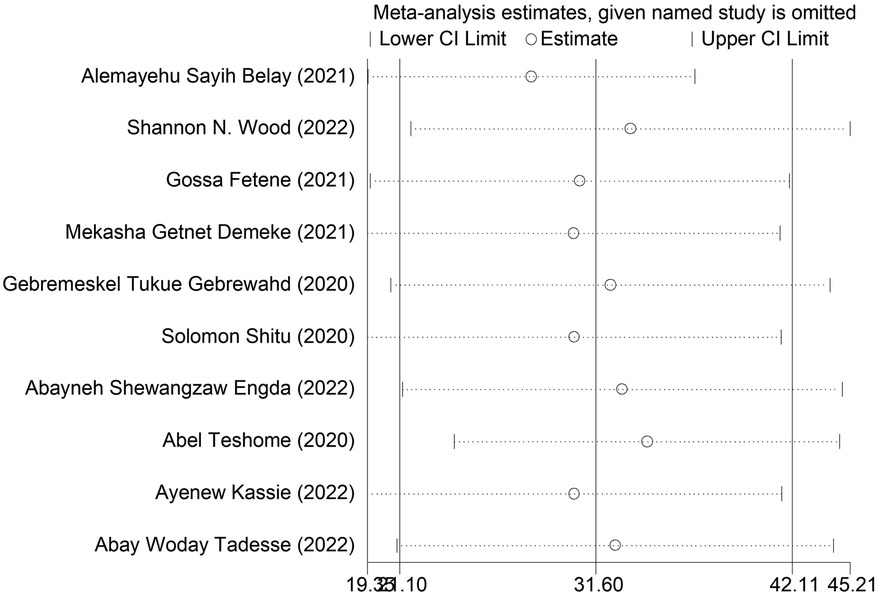
Publication bias and sensitivity analysis
Egger's regression test and a funnel plot were used to assess publication bias. Subjectively, a funnel plot with an uneven distribution suggests the existence of publishing bias (Figure 4). Furthermore, Egger's regression test's objective p-value of 0.006 suggested the existence of publication bias.
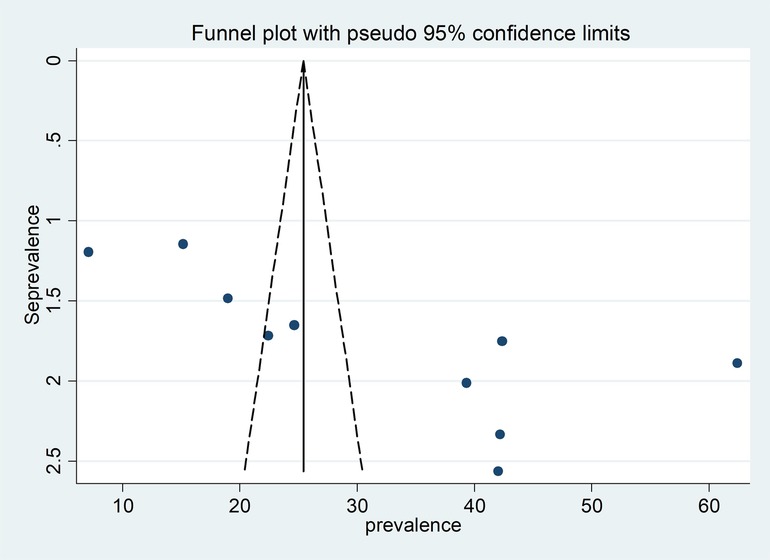
Figure 4. Funnel plot for publication bias, Log prop or LNP (log of proportion) represented in the x-axis and standard error of log proportion in the y-axis.
We conducted a sensitivity analysis to ascertain the weight of each study in relation to the total effect size of the prevalence of intimate partner violence and associated characteristics among women during the COVID-19 pandemic. The DerSimonian–Laird random-effects model sensitivity analysis revealed that no single study had an impact on the overall prevalence of intimate partner violence and associated factors among women during the COVID-19 pandemic in Ethiopia (Figure 5).
Associated factors of intimate partner violence
Among the included 10 studies, 6 studies reported the association between partner alcohol use and intimate partner violence. The pooled odds ratio from these studies was 1.93 (95% CI: 1.60–2.23), revealing that a woman with a partner who had a history of alcohol use was two times more likely to be a victim of intimate partner violence than their counterparts (Figure 6).
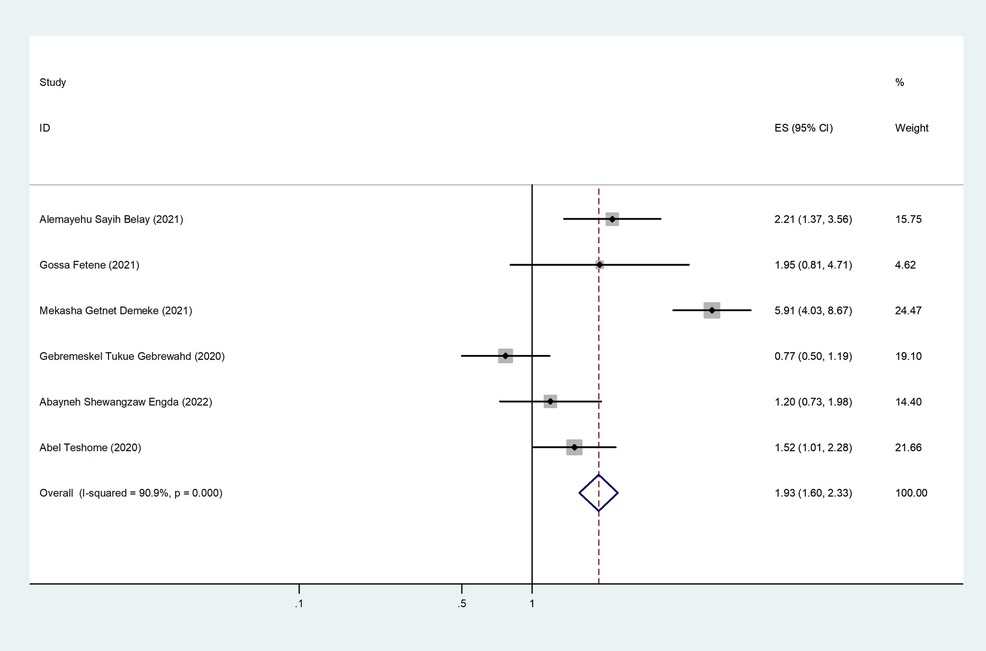
Figure 6. The pooled effect of partner alcohol use and the prevalence of intimate partner violence among women during the COVID-19 pandemic in Ethiopia.
Two of the 10 included studies revealed an association between intimate partner violence and income lost during the COVID-19 pandemic. The pooled odds ratio was 9.86 (95% CI: 6.35–15.70), indicating that those who lost income during the COVID-19 pandemic were 10 times more likely to be victimized by intimate partner violence than those who did not lose income during the COVID-19 pandemic (Figure 7).
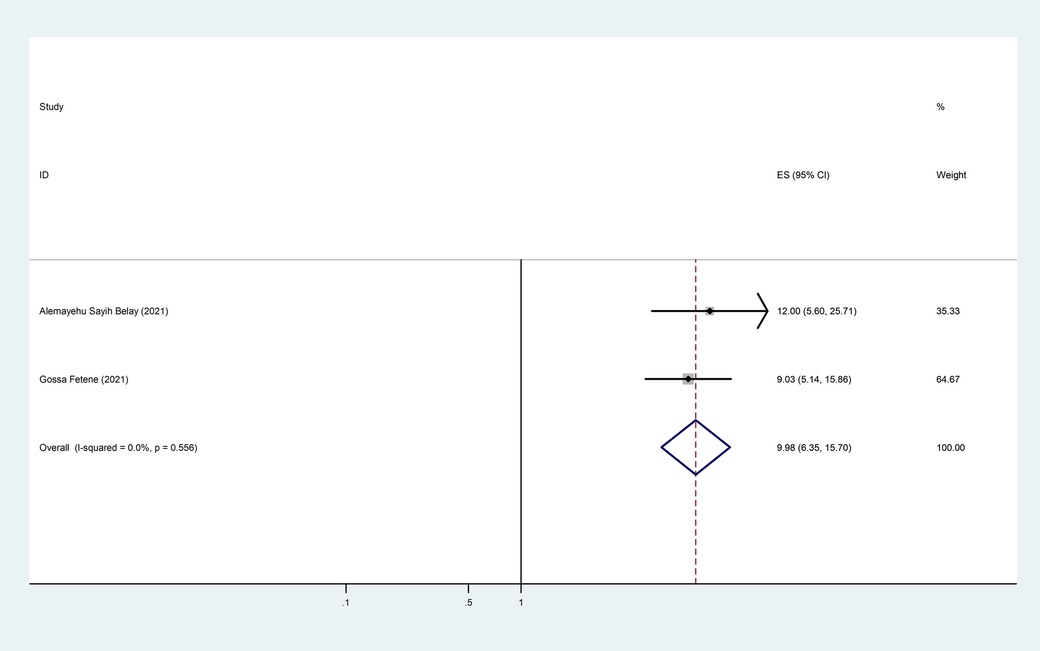
Figure 7. The pooled effect of income loss during the COVID-19 pandemic and the prevalence of intimate partner violence among women during the COVID-19 pandemic in Ethiopia.
Of the 10 studies that were considered, 7 of them showed an association between intimate partner violence and partner education. The pooled odds ratio was 2.03 (95% CI: 1.57–2.63), showing that partners who had no formal education are two times more likely to commit violence than partners who had formal education (Figure 8).
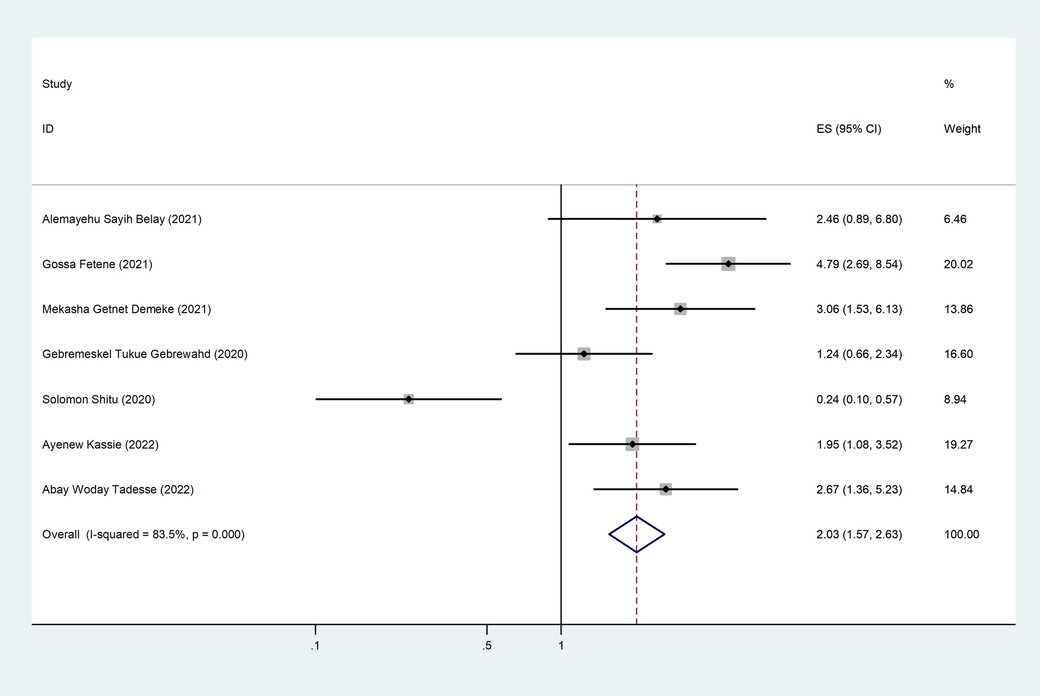
Figure 8. The pooled effect of partner education and the prevalence of intimate partner violence among women during the COVID-19 pandemic in Ethiopia.
Four of the seven included studies revealed an association between intimate partner violence and decision-making in the household. The pooled odds ratio was 1.82 (95% CI: 1.33–2.50), indicating that those women who had decisions made by their partner only in the household were 1.82 times more likely to experience intimate partner violence than their counterparts (Figure 9).
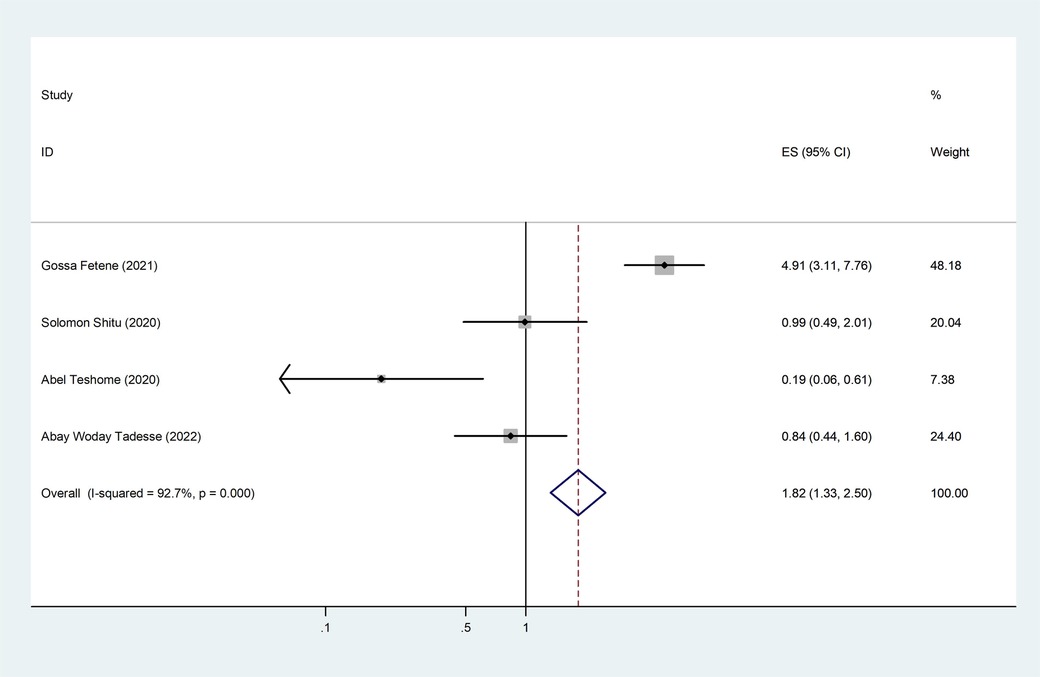
Figure 9. The pooled effect of decision-making in the household and the prevalence of intimate partner violence among women during the COVID-19 pandemic in Ethiopia.
Discussion
This review was conducted to estimate the pooled prevalence and associated factors of intimate partner violence against reproductive age women during the COVID-19 pandemic in Ethiopia.
During the COVID-19 pandemic, women's pooled prevalence of any form of IPV was 31.60% (95% CI: 21.10–42.11). This prevalence was comparable to a systematic review performed globally (31%) (39) and in Europe (21%) (40). However, the pooled prevalence was higher than that in studies performed before the pandemic: Southern Asia (19%) (41), Western Asia (13%) (42), France (7%) (43), North Africa (15%) (44), and sub-Saharan Africa (20%) (45). This may be due to the stay-at-home or lockdown policy because of the COVID-19 pandemic; long periods of time spent together at home exacerbate the situation and raise the risk of violence. In addition, the lockdown has an impact on many facets of society, including socioeconomic circumstances that can drive interpersonal conflict and violent acts. Our findings were lower than those of a study conducted in Bangladesh (45.29%) (46), Peru (48.0%) (47), and Iran (65.4%) (48). This may be due to the sociodemographic characteristics of the countries, study design, and sample size difference.
Intimate partner violence is a serious public health issue and a violation of women's human rights (10). Violence may raise the chance of human immunodeficiency virus (HIV) infection in specific situations and have a detrimental impact on women's sexual, emotional, physical, and reproductive health (10).
This study found partner alcohol use was a significant determinant of intimate partner violence. In this regard, we found that a partner who had a history of alcohol use had a higher likelihood of committing violence than their counterparts. This is consistent with studies conducted in different countries (49, 50). This may be explained by the fact that drinking alcohol might impair a person's ability to think clearly and cognitively. As a result, women who have alcohol-using spouses are more likely to experience violence than women who do not. This demonstrates the significance for the government and organizations that promote women's health to pay attention to alcohol-related activities in the nation.
Women who lost income during the COVID-19 pandemic were nearly 10 times more likely to be targeted by intimate partner violence than those who did not lose income during the COVID-19 pandemic. This finding is consistent with systematic reviews done on intimate partner violence in different regions of the globe (51, 52). This could be due to staying at home being one of the COVID-19 pandemic preventive and control strategies that led to a woman's income loss, which increases her risk of IPV. Furthermore, this could be because women who rely on their male partners for financial support are more vulnerable to IPV. Working on the rehabilitation of women who lost their income due to the COVID-19 pandemic is an excellent strategy since it may reduce the number of women who experience violence from their partners and improve the health of women.
Educational status was much associated with intimate partner violence. Partners who had no formal education were two times more likely to commit violence than partners who had formal education. This result is consistent with different studies (53–55). This might be because education influences people's perspectives in various ways and because educated individuals communicate more effectively than their less-educated counterparts. As a result, they believe that problems can be resolved via dialogue rather than by violating the rights of others. In addition, due to their lack of understanding of their wives’ and partners’ legal rights, illiterate husbands may not be aware of the implications of their violent behavior, be unable to establish flexible and caring behavior, and view violence against women as the norm.
Moreover, this systematic review and meta-analysis observed that partners who made household decisions alone were 1.82 times more likely to commit intimate partner violence than their counterparts. This could be due to the fact that a woman who lacks decision-making authority in the household is indicative of a relationship that is unhealthy and violent, and women are not comfortable discussing household issues with their partners. Improving women's decision-making in the home is crucial since it may reduce the likelihood that their partners may use violence against them.
This study highlights the urgent need for enhanced enforcement of IPV laws and support systems. The findings also serve as a foundation for advocating women's justice in Ethiopia and other similar contexts. In addition, future research should explore longitudinal changes in IPV rates and expand on the identified risk factors to better understand and address IPV dynamics.
Limitation
There are certain limitations to the current work. The study's reliance on cross-sectional studies conducted during the pandemic period may not capture the longitudinal effects of the COVID-19 pandemic on IPV trends, and that only 10 articles were reviewed for this study may limit the generalizability of the results. Furthermore recall bias, response bias, and differential misclassification within the reviewed studies are potential biases. Furthermore, the study's inability to compare IPV rates before and during the pandemic makes it difficult to draw firm conclusions on an increase in IPV. However, the study also has strengths such as assessments for heterogeneity, publication bias, and sensitivity analyses, ensuring robust and consistent findings. As a result, this will enhance the transparency and credibility of the study. Correspondingly, it has novelty since this is the first systematic review and meta-analysis focusing on IPV in Ethiopia during the COVID-19 pandemic.
Conclusion
This systematic review and meta-analysis found preliminary evidence that IPV increased during the COVID-19 pandemic. This finding also identified several key determinants of intimate partner violence during the COVID-19 pandemic. Based on the findings of this review, a partner who has a history of alcohol use, women who lost income during COVID-19, a partner who has no formal education, and household decisions made by the husband alone were statistically significant factors for intimate partner violence during the COVID-19 pandemic. Hence, this implies that the health sector must play a significant role in providing women who are victims of violence with comprehensive healthcare, advocating that violence against women should be viewed as unacceptable, and improving literacy to minimize the consequences of intimate partner violence among women. Moreover, to comprehend and examine IPV dynamics more deeply, future research should also look into longitudinal changes in IPV rates and elaborate on the risk variables that have been found.
Author contributions
TA: Conceptualization, Data curation, Formal Analysis, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. TT: Conceptualization, Data curation, Validation, Writing – review & editing. BW: Data curation, Software, Validation, Writing – review & editing. EM: Conceptualization, Methodology, Validation, Writing – review & editing. MA: Methodology, Software, Validation, Writing – review & editing. AZ: Conceptualization, Methodology, Validation, Writing – review & editing. MW: Data curation, Software, Validation, Writing – review & editing. AK: Investigation, Methodology, Validation, Writing – review & editing, Conceptualization, Data curation, Formal Analysis, Funding acquisition, Project administration, Resources, Software, Supervision, Visualization. BT: Methodology, Software, Validation, Writing – review & editing. AG: Conceptualization, Methodology, Software, Validation, Writing – review & editing. MT: Methodology, Software, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to acknowledge the authors who conducted and published the original studies.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
COVID-19, Coronavirus Disease 2019; HIV, human immunodeficiency virus; IPV, intimate partner violence; JBI, Joanna Briggs Institute; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analysis; SDG, Sustainable Development Goals; WHO, World Health Organization.
References
1. Cheng ZJ, Shan J. 2019 novel coronavirus: where we are and what we know. Infection. (2020) 48:155–63. doi: 10.1007/s15010-020-01401-y
2. J WHO. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. Geneva: WHO library (2020).
3. WHO TJG, Switzerland. WHO Director-General’s opening remarks at the media briefing on COVID-19—11 March 2020. Geneva: World Health Organization (2020).
4. Alshammari TM, Alenzi KA, Alnofal FA, Fradees G, Altebainawi AF. Are countries’ precautionary actions against COVID-19 effective? An assessment study of 175 countries worldwide. Saudi Pharm J. (2021) 29(5):391–409. doi: 10.1016/j.jsps.2021.03.011
5. World Health Organization. Responding to Intimate Partner Violence and Sexual Violence Against Women: WHO Clinical and Policy Guidelines. Geneva: WHO library (2013).
6. Petersen R, Saltzman LE, Goodwin M, Spitz A. Key Scientific Issues for Research on Violence Occurring Around the Time of Pregnancy. Georgia: National Center for Chronic Disease Prevention (1998).
7. Women P, Yawn B, Yawn R, Uden D. American Medical Association diagnostic and treatment guidelines on domestic violence. Arch Fam Med. (1992) 1:39. doi: 10.1001/archfami.1.1.39
8. McCloskey LA, Boonzaier F, Steinbrenner SY, Hunter T. Determinants of intimate partner violence in sub-Saharan Africa: a review of prevention and intervention programs. Partner Abuse. (2016) 7(3):277–315. doi: 10.1891/1946-6560.7.3.277
9. WHO. Violence Against Women: Key Facts. Vol. 29. Geneva: World Health Organization (2017). p. 2017. https://www.who.int/health-topics/violence-against-women
11. Davis M, Gilbar O, Padilla-Medina DM. Intimate partner violence victimization and perpetration among US adults during the earliest stage of the COVID-19 pandemic. Violence Victim. (2021) 36(5):583–603. doi: 10.1891/VV-D-21-00005
12. Jarnecke AM, Flanagan JC. Staying safe during COVID-19: how a pandemic can escalate risk for intimate partner violence and what can be done to provide individuals with resources and support. Psychol Trauma. (2020) 12(S1):S202. doi: 10.1037/tra0000688
13. Van Parys A-S, Verhamme A, Temmerman M, Verstraelen H. Intimate partner violence and pregnancy: a systematic review of interventions. PLoS One. (2014) 9(1):e85084. doi: 10.1371/journal.pone.0085084
14. Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. (2020) 4(6):421. doi: 10.1016/S2352-4642(20)30109-7
15. Bott S, Guedes A, Ruiz-Celis AP, Mendoza JA. Intimate partner violence in the Americas: a systematic review and reanalysis of national prevalence estimates. Rev Panam Salud Publica. (2019) 43:40–50. doi: 10.26633/RPSP.2019.26
16. Vives-Cases C, Ruiz-Cantero MT, Escribà-Agüir V, Miralles JJ. The effect of intimate partner violence and other forms of violence against women on health. J Public Health (Oxf). (2011) 33(1):15–21. doi: 10.1093/pubmed/fdq101
17. Beydoun HA, Beydoun MA, Kaufman JS, Lo B, Zonderman AB. Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: a systematic review and meta-analysis. Soc Sci Med. (2012) 75(6):959–75. doi: 10.1016/j.socscimed.2012.04.025
18. Moreira DN, Da Costa MP. The impact of the COVID-19 pandemic in the precipitation of intimate partner violence. Int J Law Psychiatry. (2020) 71:101606. doi: 10.1016/j.ijlp.2020.101606
19. FMOH. Infection Prevention and Control Interim Protocol for COVID-19 in Health Care Settings in Ethiopia. Addis Ababa, Ethiopia: FMOH (2020).
20. Duncan TK, Weaver JL, Zakrison TL, Joseph B, Campbell BT, Christmas AB, et al. Domestic violence and safe storage of firearms in the COVID-19 era. Ann Surg. (2020) 272(2):e55. doi: 10.1097/SLA.0000000000004088
21. FMOH EJEFMoH. National Comprehensive Covid-19 Management Handbook. Addis Abeba: United Nations General Assembly (2020).
22. Assembly GJTowt. Sustainable Development Goals. SDGs. New York: United Nations General Assembly (2015). p. 2030.
23. Tadesse AW, Tarekegn SM, Wagaw GB, Muluneh MD, Kassa AM. Prevalence and associated factors of intimate partner violence among married women during COVID-19 pandemic restrictions: a community-based study. J Interpers Violence. (2022) 37(11–12):NP8632–50. doi: 10.1177/0886260520976222
24. Shewangzaw Engda A, Dargie Wubetu A, Kasahun Amogne F, Moltot Kitaw T. Intimate partner violence and COVID-19 among reproductive age women: a community-based cross-sectional survey, Ethiopia. Womens Health (Lond). (2022) 18:17455065211068980. doi: 10.1177/17455065211068980
25. Teshome A, Gudu W, Bekele D, Asfaw M, Enyew R, Compton SD, et al. Intimate partner violence among prenatal care attendees amidst the COVID-19 crisis: the incidence in Ethiopia. Int J Gynaecol Obstet. (2021) 153(1):45–50. doi: 10.1002/ijgo.13566
26. Belay AS, Kassie Gidafie A, Abera Gudeta T. Perinatal intimate partner violence during COVID-19 and its associated factors among postpartum mothers attending newborn immunization in southern Ethiopia, 2021: a cross-sectional study. SAGE Open Med. (2022) 10:20503121221116671. doi: 10.1177/20503121221116671
27. Kassie A, Handebo S, Adugna A, Shitu K. Violence against girls during COVID-19 pandemic and associated factors in Gondar city, north west Ethiopia. Epidemiol Infect. (2022) 150:e31. doi: 10.1017/S0950268822000140
28. Gebrewahd GT, Gebremeskel GG, Tadesse DB. Intimate partner violence against reproductive age women during COVID-19 pandemic in northern Ethiopia 2020: a community-based cross-sectional study. Reprod Health. (2020) 17(1):1–8. doi: 10.1186/s12978-020-01002-w
29. Fetene G, Alie MS, Girma D, Negesse Y. Prevalence and its predictors of intimate partner violence against pregnant women amid COVID-19 pandemic in southwest Ethiopia, 2021: a cross-sectional study. SAGE Open Med. (2022) 10:20503121221079317. doi: 10.1177/20503121221079317
30. Demeke MG, Shibeshi ET. Intimate partner violence against women of reproductive age and associated factors during COVID-19 pandemic in northern Ethiopia, 2021: a community-based cross-sectional study. Front Glob Womens Health. (2023) 3:977153. doi: 10.3389/fgwh.2022.977153
31. Wood SN, Yirgu R, Wondimagegnehu A, Qian J, Milkovich RM, Decker MR, et al. Impact of the COVID-19 pandemic on intimate partner violence during pregnancy: evidence from a multimethods study of recently pregnant women in Ethiopia. BMJ Open. (2022) 12(4):e055790. doi: 10.1136/bmjopen-2021-055790
32. Shitu S, Yeshaneh A, Abebe H. Intimate partner violence and associated factors among reproductive age women during COVID-19 pandemic in southern Ethiopia, 2020. Reprod Health. (2021) 18:1–10. doi: 10.1186/s12978-021-01297-3
33. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 151(4):264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
34. García-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts C. WHO Multi-country Study on Women’s Health and Domestic Violence Against Women. Geneva: WHO library (2005).
35. Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Systematic Reviews of Etiology and Risk. Joanna Briggs Institute Reviewer’s Manual. 5th ed. Adelaide, Australia: The Joanna Briggs Institute (2017). p. 217–69.
36. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. (1997) 315(7109):629–34. doi: 10.1136/bmj.315.7109.629
37. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. (2003) 327(7414):557–60. doi: 10.1136/bmj.327.7414.557
38. Marín-Martínez F, Sánchez-Meca J. Weighting by inverse variance or by sample size in random-effects meta-analysis. Educ Psychol Meas. (2010) 70(1):56–73. doi: 10.1177/0013164409344534
39. Kifle ME, Aychiluhm SB, Anbesu EW. Global prevalence of intimate partner violence during the COVID-19 pandemic among women: systematic review and meta-analysis. BMC Womens Health. (2024) 24(1):1–14. doi: 10.1186/s12905-023-02845-8
40. Costa D, Scharpf F, Weiss A, Ayanian AH, Bozorgmehr K. Intimate partner violence during COVID-19: systematic review and meta-analysis according to methodological choices. BMC Public Health. (2024) 24(1):313. doi: 10.1186/s12889-024-17802-9
41. Devries KM, Mak JY, Garcia-Moreno C, Petzold M, Child JC, Falder G, et al. The global prevalence of intimate partner violence against women. Science. (2013) 340(6140):1527–8. doi: 10.1126/science.1240937
42. García-Moreno C, Pallitto C, Devries K, Stöckl H, Watts C, Abrahams N. Global and Regional Estimates of Violence Against Women: Prevalence and Health Effects of Intimate Partner Violence and non-Partner Sexual Violence. Geneva: WHO library (2013).
43. Peraud W, Quintard B, Constant A. Factors associated with violence against women following the COVID-19 lockdown in France: results from a prospective online survey. PLoS One. (2021) 16(9):e0257193. doi: 10.1371/journal.pone.0257193
44. Maheu-Giroux M, Sardinha L, Stöckl H, Meyer SR, Godin A, Alexander M, et al. A framework to model global, regional, and national estimates of intimate partner violence. BMC Med Res Methodol. (2022) 22(1):1–17. doi: 10.1186/s12874-022-01634-5
45. Sardinha L, Maheu-Giroux M, Stöckl H, Meyer SR, García-Moreno C. Global, regional, and national prevalence estimates of physical or sexual, or both, intimate partner violence against women in 2018. Lancet. (2022) 399(10327):803–13. doi: 10.1016/S0140-6736(21)02664-7
46. Rayhan I, Akter K. Prevalence and associated factors of intimate partner violence (IPV) against women in Bangladesh amid COVID-19 pandemic. Heliyon. (2021) 7(3):5–10. doi: 10.1016/j.heliyon.2021.e06619
47. Agüero JM. COVID-19 and the rise of intimate partner violence. World Dev. (2021) 137:105217. doi: 10.1016/j.worlddev.2020.105217
48. Fereidooni R, Mootz J, Sabaei R, Khoshnood K, Heydari ST, Moradian MJ, et al. The COVID-19 pandemic, socioeconomic effects, and intimate partner violence against women: a population-based cohort study in 2020, Iran. Am J Public Health. (2023) 113(2):228–37. doi: 10.2105/AJPH.2022.306839
49. Hamadani JD, Hasan MI, Baldi AJ, Hossain SJ, Shiraji S, Bhuiyan MSA, et al. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Health. (2020) 8(11):e1380–9. doi: 10.1016/S2214-109X(20)30366-1
50. Roland N, Ahogbehossou Y, Hatem G, Yacini L, Feldmann L, Saurel-Cubizolles MJ, et al. Violence against women and perceived health: an observational survey of patients treated in the multidisciplinary structure ‘the women’s house’ and two family planning centres in the metropolitan Paris area. Health Soc Care Community. (2022) 30(6):e4041–50. doi: 10.1111/hsc.13797
51. Devries KM, Child JC, Bacchus LJ, Mak J, Falder G, Graham K, et al. Intimate partner violence victimization and alcohol consumption in women: a systematic review and meta-analysis. Addiction. (2014) 109(3):379–91. doi: 10.1111/add.12393
52. Mojahed A, Alaidarous N, Kopp M, Pogarell A, Thiel F, Garthus-Niegel S. Prevalence of intimate partner violence among intimate partners during the perinatal period: a narrative literature review. Front Psychiatry. (2021) 12:601236. doi: 10.3389/fpsyt.2021.601236
53. Ajala AO. Sexual violence against women in marital dyads, prevalence, correlates, and consequences: among the Ijesa of south-western Nigeria. Arch Bus Res. (2017) 5(12):12–24. https://www.academia.edu/download/92112624/3902-Article_Text-10250-1-10-20171214.pdf
54. Leite FMC, Amorim MHC, Wehrmeister FC, Gigante DP. Violence against women, Espírito Santo, Brazil. Rev Saúde Pública. (2017) 51:51–60. doi: 10.1590/S1518-8787.2017051006815
Keywords: intimate partner, violence, factors, women, COVID-19 pandemic, Ethiopia
Citation: Alemu TG, Tamir TT, Workneh BS, Mekonen EG, Ali MS, Zegeye AF, Wassie M, Kassie AT, Tekeba B, Gonete AT and Techane MA (2024) Intimate partner violence and associated factors among women during the COVID-19 pandemic in Ethiopia: a systematic review and meta-analysis. Front. Glob. Womens Health 5:1425176. doi: 10.3389/fgwh.2024.1425176
Received: 29 April 2024; Accepted: 31 July 2024;
Published: 23 August 2024.
Edited by:
Daudet Tshiswaka, University of West Florida, United StatesReviewed by:
Colette Davis, University of West Florida, United StatesDanielle Belemsaga/Yugbare, Research Institute for Health Sciences (IRSS), Burkina Faso
Tetti Solehati, Padjadjaran University, Indonesia
Copyright: © 2024 Alemu, Tamir, Workneh, Mekonen, Ali, Zegeye, Wassie, Kassie, Tekeba, Gonete and Techane. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tewodros Getaneh Alemu, dGV3b2Ryb3NnZXRhbmVoN0BnbWFpbC5jb20=
 Tewodros Getaneh Alemu
Tewodros Getaneh Alemu Tadesse Tarik Tamir
Tadesse Tarik Tamir Belayneh Shetie Workneh
Belayneh Shetie Workneh Enyew Getaneh Mekonen
Enyew Getaneh Mekonen Mohammed Seid Ali
Mohammed Seid Ali Alebachew Ferede Zegeye
Alebachew Ferede Zegeye Mulugeta Wassie
Mulugeta Wassie Alemneh Tadesse Kassie6
Alemneh Tadesse Kassie6 Berhan Tekeba
Berhan Tekeba Almaz Tefera Gonete
Almaz Tefera Gonete Masresha Asmare Techane
Masresha Asmare Techane