- 1Elza Berquó Center for Population Studies, State University of Campinas (UNICAMP), Campinas, Brazil
- 2Department of Sociology, University of São Paulo (USP), São Paulo, Brazil
- 3Latin American Center for Perinatology, Women and Reproductive Health, Pan American Health Organization (PAHO), Montevideo, Uruguay
- 4Department of Sectoral Development, Brazilian Regulatory Agency for Private Plans (ANS), Rio de Janeiro, Brazil
- 5Labor Movens - Working conditions in Tourism, University of Brasília, Brasília, Brazil
Introduction: The impact of COVID-19 on mental health has become a relevant object of research. Studies have demonstrated that women have experienced greater mental health challenges, highlighting the importance of public health systems to address women's specific needs.
Methods: This literature review explores the effects of the coronavirus pandemic on psychological distress among women, aiming to provide a comprehensive understanding of the subject and to explore how these research findings can guide public mental health care responses in crisis settings. A total of 131 studies were analyzed and four dimensions were discussed: study characteristics, factors impacting women's mental health in the pandemic setting, particularities of pregnancy and the postpartum period, and proposed interventions. Most studies exclusively addressed populations of adult women, predominantly during pregnancy and the postpartum period.
Results: Anxiety, depression, and stress were the most common outcomes. Lower education and income, preexisting mental health problems, and living alone or with children were risk factors for higher levels of anxiety and depression.
Discussion: A comprehensive care approach supported by public health policies and focused on intersectional factors, including race, socioeconomic status, and access to resources, is necessary to improve women's mental health care response in future crises.
Introduction
During the COVID-19 pandemic, the necessary measures of movement restriction, social isolation, and prioritization of treatment for patients with COVID-19 by health care services have profoundly changed individual and family routines and have aggravated the problem of inequality between population groups. Women are especially affected by these changes. Not only have they maintained their usual tasks, but have also accumulated activities involving education of their children and caring for older and/or sick family members. In many cases, they have lost or abandoned their jobs to meet the needs of their families.
Triple duty, children, work, shortage of material resources, lockdown and fear of illness, and, in some cases, violence have considerably increased the emotional burden women have had to deal with in their different ways of coping with the crisis. Additionally, they had no access to recreational and social activities or to health care services for matters of sexuality and reproductive health, pregnancy, delivery, and the postpartum period. These circumstances also seem to have deteriorated the preexisting state of their subjectivities, their position in the world, their perspectives on life, and their personal resources to face the new demands.
A systematic review titled “Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic” (1) and published by The Lancet in October 2021 indicates that approximately 53 million cases of depression and 76 million cases of anxiety were due to the COVID-19 pandemic. The study also highlighted that women and young people were the most affected population groups, but that additional studies are required to determine the severity and duration of the impact. However, even before the pandemic, the leading causes of disease burden were anxiety and depressive disorders, as the study emphasized. A key methodological issue raised by the authors is the quality of the instruments available for such measurements, which makes the question of how to promote mental well-being and target mental health determinants even more complex. Similarly, “Strengthening mental health responses to COVID-19 in the Americas: A health policy analysis and recommendations,” (2) a study published in November 2021, reports that women and young people were substantially affected during the pandemic and that mental health should be consistently addressed by public health systems given the severity of the emotional burden people have experienced.
This is the gap that this study aims to fill: making the issue of women's mental health in the critical period of the pandemic more visible. Contrary to initial assumptions, the effects of the COVID-19 pandemic on different population groups were not homogeneous in view of social determinants hierarchically determined by gender, race/ethnicity, age, sexual orientation, and economic status structures. An estimated 72% of health workers who have lost their lives to the COVID-19 pandemic are women (3). Studies have shown that female health workers usually present with more symptoms of anxiety and depression, insomnia, and burnout given their working conditions, especially frontline female workers who must permanently wear personal protective equipment (4).
The Region of the Americas has surpassed 100 million cases of COVID-19 and accounts for most of the reported deaths. The catastrophic situation is associated with social, economic, and health issues (3, 5–7). Pregnant women are more vulnerable and tend to develop more severe symptoms. Approximately 20 million women in the Americas have stopped using contraceptives either because they cannot pay for them or because their sexual practices have changed during isolation, as physical encounters have become rarer, with possible psychological impacts (8).
The Pan American Health Organization (PAHO) stated in 2021 that continued disruption of women's health services due to COVID-19 could erase more than 20 years of progress in reducing maternal mortality and increasing access to contraceptive use. A Latin American Center for Perinatology/Women's Health and Reproductive Health study showed that maternal mortality increased during the pandemic, which slowed down the Region's achievements in the past decade (3).
According to the COVID-19 Sex-Disaggregated Data Tracker, the gender/sex system has determined important variations in the facts and consequences associated with the pandemic (9). It is worth mentioning a Brazilian article on maternal mortality from COVID-19 published in The Lancet Regional Health—Americas (10). The study revealed that failures in medical care for pregnant women with COVID-19 are exacerbated by racial and gender discrimination, especially with regard to sexual and reproductive health. The authors found, for example, that interventions for preserving women's lives, such as intubation and preterm labor induction, were postponed by physicians for awaiting fetal development.
Importantly, the course of the first period of the pandemic has showed that the configurations of social, political, cultural, and economic practices that determine how people fall ill and die also pave the way for a greater chance of survival for women and men during the COVID-19 pandemic. There have been many impacts in terms of access to health care services and vaccinations, revealing relevant gender variations in pandemic management results.
In this context, the present study aimed to map the discussion about the influence of COVID-19 on women's mental health based on the literature published in the first period of the pandemic and to identify how scientific research was produced with a description of the main results.
Women, mental disorders, and subjectivities: a conceptual tour
In recent years, the United Nations has made important efforts in an attempt to understand the issue. A PAHO study titled “The Burden of Mental Disorders in the Region of the Americas, 2018” presented an overview of perceived disabilities from substance use and specific neurological disorders and self-harm, combined or not with premature mortality, the imbalance between mental health spending and the related disease burden, and the limited allocation of mental health resources by countries of the Region (11). The study revealed that depressive disorders account for 7.8% of total years lived with disability (YLDs), while self-harm and pain disorders account for 4.7% of YLDs. The paper is also part of a process that, albeit slow, has managed to add the concern with the burden of mental distress to the global agenda, with the introduction of specific mental health indicators in the Sustainable Development Goals (SDGs) and the 2030 Agenda (12). SDG 3, which refers to health issues, specifically established an indicator for reducing suicide mortality rates by 2030. Additionally, there is a specific goal for strengthening the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol.
Although the burden of anxiety, depression, and self-harm among women has grown significantly in recent decades, few studies have focused on analyzing the evidence systematically and consistently. Of all WHO mental health publications (13–29), only two (17, 21) refer specifically to the female population. The Lancet Psychiatry Series on Women's Mental Health aims to explore social and biological factors in an attempt to understand the so-called mental disorders in women (30). As the Series describes, although some elements of the prevalence and pattern of psychological problems in women are known, the underlying reasons are still under-researched. Thus, a certain group of psychoses, depressive disorders, including perinatal and postpartum depression, anxiety disorders, and issues associated with gender violence are addressed, but in a very controversial way if a gender lens is used to interpret the findings.
Women are at the center of all new and complex situations involving panic, depression, anxiety, bereavement, and sadness. Concomitantly, they seek to preserve their life projects, their affective-sexual bonds, their personal perspectives on productive and reproductive life, and especially their attitude towards facing isolation and losses in the family, community, and relationship contexts. This emotional turbulence accumulates in their daily lives, often with no space to be expressed. Countless were the demands of life adaptation for finding new possibilities of survival.
To meet the challenge of addressing human suffering in this context, we must review the notion of subject that each disciplinary field adopts. This is a process of conceptual review that makes it possible to overcome a fragmented view of each of the subjects in question and approach them — in this case, women — in their singularities, multidetermined by social factors and inserted into their configuration of language, their own network of meanings and signifiers. Such perspective could remove women from the place of carriers of disorders and make them subjects fully capable of operating with their own emotional life in processes of listening.
Many authors have proposed a shift from the idea of a subject defined by disorders to that of a subject defined by desires and rights. According to Birman, distress and trauma translate into helplessness and dismay in the subjects (women) who need spaces to manage their own psyche and favor the crucial transformation of pain into words (language) (31). The role of public policies is to bring to the forefront, as Birman indicates, “the possibility for the subject, as a citizen, to be able to count on the Other, to trust the ruler as an unmistakable real and psychic instance of protection in the face of a misfortune for defending life and thus preventing the possible advent of death” (free translation). Thus, distress as experienced by the citizens would be appeased by means of concrete actions. If the pandemic has exacerbated a group of psychological and psychiatric conditions such as panic syndromes, obsessions, phobias, and eating disorders, among others, what specific meanings have been triggered in the singular stories of each woman in their coping, distancing, and caring processes in the pandemic? What is the place of anxiety and depression, two famous conditions since the second half of the past century, in this context (32, 33)?
Intertwining these issues with those referring to sociocultural structures that codetermine cultural foundations, ie, the field of inequalities, is a key feature of our perspective. Working with social determinants is a strategy that has been developed by the WHO since 2005, when the Commission on Social Determinants of Health was created. In this context, several sociocultural determinants cooperate to create health inequalities and, in our view, should be considered markers of the language of subjects who seek acceptance in any clinical setting. However, it is not only a matter of accepting that subjects are constructed in specific hierarchical cultures with distinct established power relations, but that the different determinants themselves construct the body of identifications that each one carries inside and ultimately operate in the formation of subjectivities, of the singularity of each subject. This comprehensive perspective of psychological distress leads to some questions, including, how public health emergencies, as the COVID-19 pandemic, impacts women's mental health?
Methods
A literature review based on the scoping review method, a strategy employed to map the extent and nature of publications in a given research area, was conducted (34, 35). The PubMed and Scopus databases were searched using the terms “COVID-19,” “SARS-CoV-2,” “Woman,” “Women,” and variations of the term “mental health” combined with specific terms related to subjectivity, violence, and sexual and reproductive health. Articles published between January 1, 2020 and June 30, 2021 in English, Portuguese, and Spanish with any type of study design were included; the bibliographic search was carried out in August 2021 (Supplementary Material S1 and S2).
Publications were considered eligible for inclusion if they reported at least one mental health outcome and mentioned specific data on women. For the purposes of this study, mental health outcome is understood as the group of most common symptoms in the psychiatric literature and in the fields of clinical psychology, psychiatry, and psychoanalysis, extending to a set of terms and concepts commonly used in these fields, such as anguish, melancholy, bereavement, and psychological distress, among others.
General population studies not reporting specific results on women, studies focusing on specific conditions (cancer, hypertension, diabetes, rheumatism, and others), and studies addressing specific professional categories, except health workers in public health fields, teachers, and workers linked to a single institution, were excluded. The resulting publications were submitted to full-text screening, and final selection was determined by agreement of at least two team members. Disagreements were resolved by a researcher with a background in women's mental health. The inclusion and exclusion criteria are detailed in Supplementary Material S3.
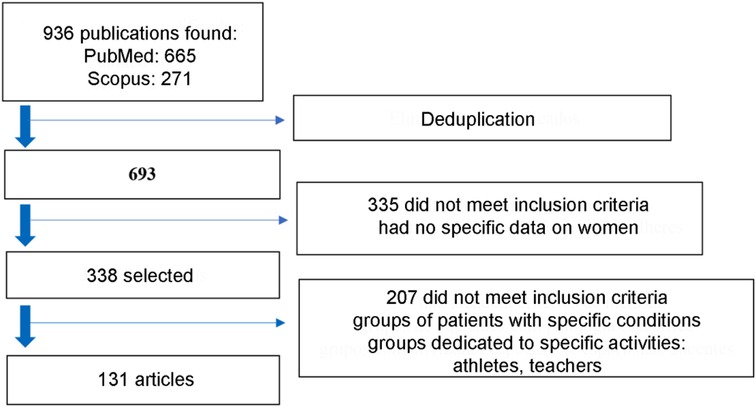
Initially, 936 publications were found; after deduplication and screening, 131 publications were included in the review (Figure 1).
The selected studies were organized with the aid of Mendeley, and the data were extracted by three researchers and later revised for greater precision. The following data were extracted: basic information (authorship, country and date, year of publication); study design (methods, inclusion criteria, exclusion criteria, sample, baseline sample characteristics, and analyzed outcomes); main results; risk and protective factors associated with mental health problems; recommendations; limitations; and funding. The characteristics of the publications are described in Supplementary Material S3, together with mental health outcomes and main results of interest for this review.
The content extracted from the publications was explored through quantification, categorization, and comparison strategies. Four dimensions are highlighted in the results, namely study characteristics, factors impacting women's mental health in the pandemic setting, particularities of pregnancy and the postpartum period, and proposed interventions.
Results
Study characteristics
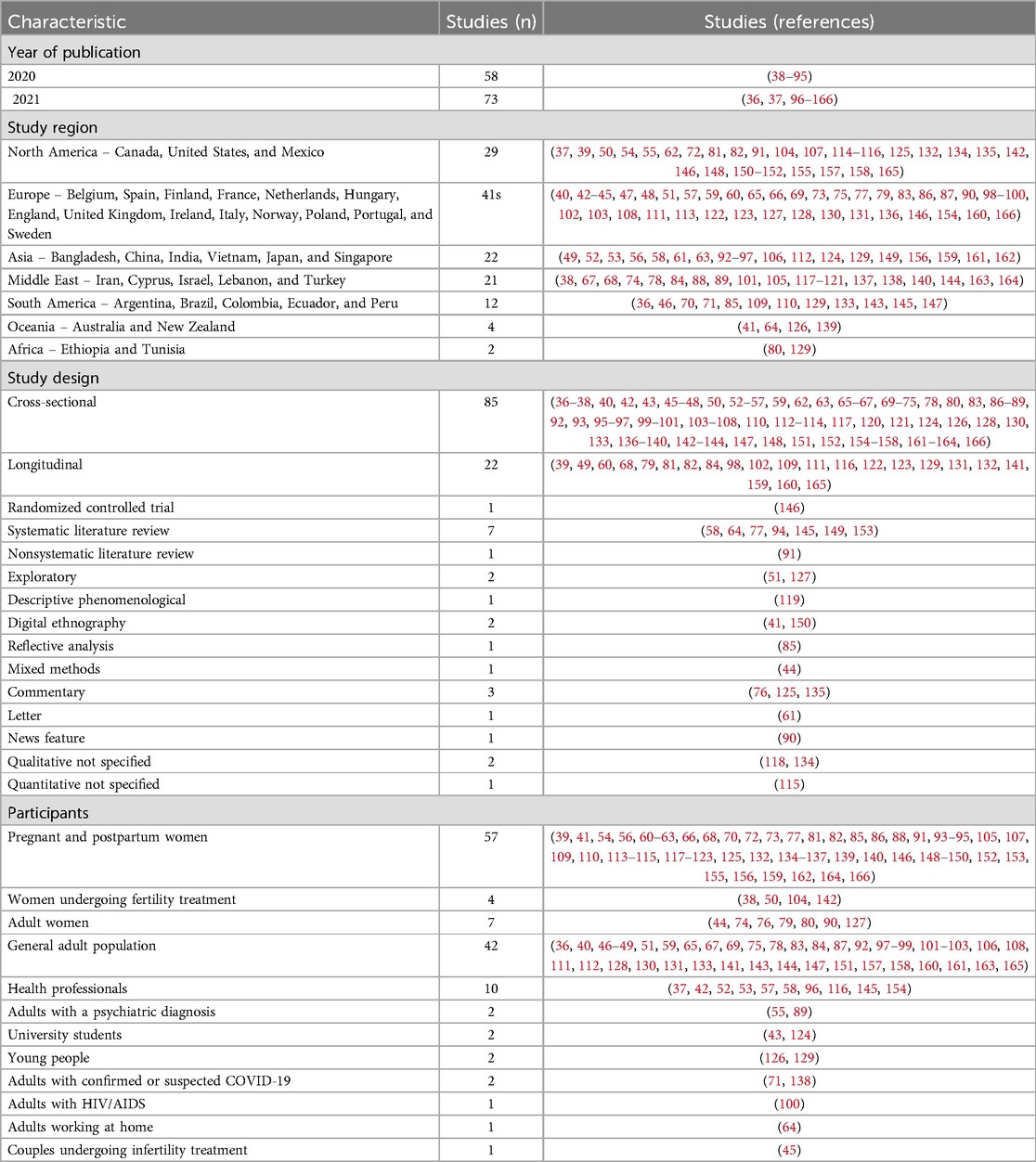
Of 131 publications selected, 58 refer to the first year of the pandemic (2020) and 73 to the first half of 2021, ending on June 30, 2021. Europe (n = 41), North America (n = 29), Asia (n = 22), and the Middle East (n = 21) account for most of the publications. South America accounts for 12 studies, with Brazil being the leading country in number of publications. Africa and Oceania were the bottom regions, ranging from one to four publications. Two multicountry studies, one including 49 countries (36) and the other including four countries (Ethiopia, India, Peru, and Vietnam) (37), were selected. Overall, the United States and China were the leading countries, with 17 and 16 studies, respectively. Study characteristics are summarized in Table 1.
A wide variety of sample sizes was observed; in studies on pregnant women, the sample ranged from 15 (118) to 15,428 individuals (156), while in studies including health professionals, the number ranged from 204 (116) to 12,596 individuals (96). The sample population was heterogeneous in more than 80% of studies.
When geographic distribution was analyzed by year of publication, China, Spain, and Italy were the countries that produced most research (36%) on COVID-19 and women's mental health during the first ten months of the pandemic, taking March 2020 as the beginning of the pandemic. These countries were greatly affected in the first period of the pandemic. It is worth noting that most empirical studies were conducted in the first half of 2020 (n = 106), which requires caution in using the results for later stages of the pandemic. Only a few Chinese studies (58, 149, 159) were initiated as early as 2019, considering that the virus was first detected in the Chinese province of Wuhan. Even among those published in 2021, most studies were conducted in the first months of 2020.
The group of analyzed publications consists mostly of empirical studies (n = 119), with a predominance of cross-sectional (n = 85) and longitudinal (n = 23) designs. Of the remaining studies, seven systematically reviewed previously published articles on mental health issues and the COVID-19 pandemic (58, 64, 77, 94, 145, 149, 153). The other publications covered the modalities of nonsystematic literature review, letter, commentary, and report. With regard to methods, the vast majority used online or telephone surveys/questionnaires to produce data, and only ten studies used some qualitative methodological strategy. Only one American randomized controlled trial was included, and the study involved 101 pregnant women, 50 in the intervention group (Calm meditation application) and 51 in the control group (146).
Qualitative investigations were dedicated to understanding how women experienced the pandemic, particularly focusing on social and family relationships (127), emotional and psychological consequences (51, 142), and specific experiences related to pregnancy and the postpartum period (41, 118, 119, 134, 139, 150). Difficulties in accessing abortion services during the pandemic were the object of mixed methods studies (44). In these studies, women's perceptions and experiences were captured through semi structured or in-depth interviews conducted by telephone or mobile instant messaging application (WhatsApp) and open online questionnaires, in addition to digital ethnography.
Most publications (52%) exclusively addressed adult women, predominantly pregnant and postpartum women (n = 57 or 43%). Studies on specific groups of women included those undergoing infertility treatment (38, 50, 104, 142) and married women with children (74).
Studies on the general adult population (31%) included health professionals, university students, people with mental health problems, people with COVID-19, people working from home, people with HIV/AIDS, and couples undergoing infertility treatment. Although the adolescent population was included in the search strategy used to find relevant articles, no publication analyzed in the screening stage reported specific results for female adolescents. Thus, no publications specifically addressing this audience were included in the review.
Of the topics that seemed to be of greatest interest, anxiety (n = 62), depression (n = 59), and stress (n = 32) were the most common outcomes, with many studies assessing more than one mental health outcome. Most studies used online surveys containing items from validated scales, which classify the severity of mental disorders according to different predefined levels, such as “mild,” “moderate,” and “severe.”
Factors impacting women's mental health
Most studies reported that women and young people are the groups most affected by mental distress during the pandemic. As an exception, a Chinese study observed higher levels of risk of mental disorder in men than in women (92).
Several factors seem to be key to women's mental health status in the pandemic context (Supplementary Material S4), and they can be grouped into five dimensions: sociodemographic (age, education, region of residence), economic (work, income), health aspects (history of mental health and chronic diseases, physical activities, psychological treatment, pregnancy and the postpartum period); social aspects (marital status, family composition, social relationships during the pandemic); and pandemic-specific factors (concern with being infected, job loss, poor housing conditions to face isolation — the latter was much debated, especially at the beginning of the pandemic).
Lower education and income, preexisting mental health problems, and living alone or with children were all risk factors for higher levels of anxiety and depression at the beginning of social restrictions. In some countries, such as England, many of these inequalities were reduced as lockdown continued, but differences were still evident 20 weeks after social isolation began (102). Pandemic-specific factors (social isolation, financial insecurity, job loss, and lack of access to basic goods and services) were associated with virtually all mental health outcomes assessed in the studies.
One study reported that women with lower household incomes had consistently worse mental health than those with higher household incomes (102), which seems to be related to a higher number of adverse experiences, such as job losses, income cuts, and inability to pay bills. Such changes were primarily driven by the financial impact of the pandemic and the challenges of balancing child schoolwork and working from home and lack of childcare (132).
However, there is evidence that people with a higher socioeconomic status may experience a greater increase in depressive symptoms and a decrease in life satisfaction during the COVID-19 pandemic compared with those with a lower socioeconomic status (167).
Another study showed that women are more anxious about the financial situation of close relatives than about themselves and that health-related anxiety was greater than economic-related anxiety (59). The study also found that men and women did not differ significantly in terms of economic-related anxiety. This result particularly contrasts with the findings of other studies, such as a United Kingdom study including a larger sample that observed considerably higher levels of distress in women experiencing economic insecurity (83). A single study showed differences in this regard. Liu et al. revealed that in China, because of cultural determinants, young married men had more psychological symptoms during the pandemic than young women (106). Such distress is associated with financial concerns, and this apparently is an important gender difference in that country.
Regarding the maintenance of social and family relationships, a study on Italian women reported that, during social isolation imposed by the pandemic, women perceived the home as a safe place despite an increase in family conflicts. This shows that family relationships are resilient and, even at difficult times, allow members to overcome loneliness, keep company, and take care of each other (127).
A study assessing the influence of gender differences on housework and psychological distress in the United Kingdom revealed that women spent much more time on unpaid care work than men during lockdown. Also, it was more likely to be the mother than the father who reduced working hours or changed employment schedules because of increased time spent on childcare (160). Women who spent long hours on housework and childcare were more likely to report increased levels of psychological distress. Working parents who adapted their work patterns showed increased psychological distress compared to those who did not. This association was much stronger if he or she was the only family member who adapted work patterns or if she was a single mother. Fathers who reduced working hours showed increased psychological distress if mothers did not. There are gender inequalities in the divisions of unpaid labor. Balancing working from home with remote schooling and childcare, as well as extra housework, is likely to pose health problems for people with families, especially for mothers.
Pregnancy and the postpartum period
Considering an extract of 57 articles whose population was pregnant women, including the perinatal and postpartum periods, approximately 30 different outcomes were assessed by either validated questionnaires or questionnaires developed by the authors. The most common outcomes in this extract (n = 62) included anxiety (n = 26), depression (n = 25), stress (n = 11), and postpartum stress and post-traumatic stress disorder (PTSD) (n = 11). Of note, studies may assess more than one outcome (Table 2). Less frequently assessed outcomes consisted of quality of life, well-being, sleep disorders, domestic violence, sexual function, psychological distress, pregnancy distress, satisfaction with childbirth, fear of childbirth, physical activity, and postpartum mood, among others.
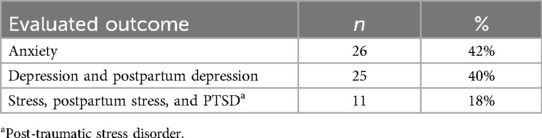
Table 2. Most common outcomes in the extract of articles addressing pregnancy and the postpartum period (n = 62).
In total, 43 research instruments were used to measure the outcomes listed in the extract of 57 articles, with the Edinburgh Postnatal Depression Scale (EPDS) (n = 12) being the most frequently used in the studies (n = 35). Other instruments are described in Table 3.
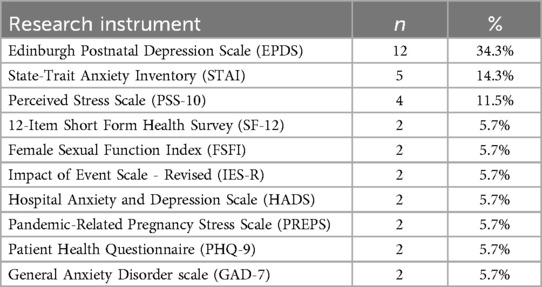
Table 3. Most common research instruments in the extract of articles addressing pregnancy and the postpartum period (n = 35).
With regard to prevalence, the level of psychological distress observed in pregnant and postpartum women exceeded that normally expected during pregnancy and that experienced by other groups during the current pandemic (39, 54, 56, 60). In contrast, one study found no difference in the levels of anxiety and depression in pregnant women before and after the onset of COVID-19 (166), and another found more symptoms of depression in nonpregnant women (164).
In pregnant women, specific concerns about COVID-19 affecting fetal health and prenatal care are associated with psychological distress, as well as concerns about changes imposed by the pandemic in childbirth conditions, especially with regard to the presence of a companion in the hospital. As noted, pregnant women are provided with inadequate and insufficient information about the effects of COVID-19 on pregnancy (63), which accentuates feelings of insecurity. In addition to fear and uncertainty about the clinical effects of COVID-19, these women often feel isolated, prevented from being with family or friends at a time when they long for more support (135). Interestingly, few authors (88, 135) addressed increased pressure on more vulnerable women, such as black and cultural minority women, who are already fighting social and health inequalities.
A lower risk of postpartum depression was observed among women who gave birth during strict isolation compared to those who gave birth before the pandemic (68). Probably because the study was conducted during isolation, mothers obtained greater support from family members who did not go to work or worked from home, and this gave them more opportunities to support pregnant women. Conversely, a Canadian longitudinal study demonstrated an increase in maternal depressive and anxiety symptoms in the first months of the COVID-19 pandemic (May to July 2020) compared to prepandemic periods (previous 10 years) (132). The findings suggest that this increase was universal, regardless of women's previous mental health history. These changes were primarily driven by the financial impact of the pandemic and challenges balancing child schoolwork and working from home and lack of childcare.
Proposed interventions
The use of technologies (mobile applications, remote consultations via telephone or video, etc.) to offer support to the most vulnerable groups, especially pregnant women, postpartum women, and people with a history of mental health problems, is regarded as a fundamental strategy for identifying risk situations and for providing care services. Specifically, studies suggested that alternative interaction strategies be used to offer counseling (119, 157, 158, 162), telepsychiatry (78), online psychotherapy (75, 128, 147), support groups, and online education activities focusing on developing skills that favor problem-solving and stress management (75, 128, 136, 143, 158, 162). Interventions need to be adjusted over time to suit the different stages of the pandemic (75).
Most studies on pregnant and postpartum women showed that screening and treatment actions for depression and anxiety should be prioritized in this group. Another relevant point is the importance of creating spaces where pregnant women can receive quality information about the risks of COVID-19 during pregnancy and the postpartum period, address the fear of childbirth, and exchange concerns with other women (41, 70, 85, 156). It is highlighted that pregnant women who remain in isolation should be able to maintain regular communication with their loved ones through social media and receive adequate social support. More intensive therapies (such as cognitive behavioral therapy and adaptive skills training) may be necessary for those experiencing severe anxiety or depressive symptoms. Specific educational strategies addressing COVID-19 and its effects on pregnancy are needed for young pregnant women with less education and public health insurance to help maintain their psychological well-being (70).
Studies also emphasize that public health departments should provide a central information repository that is accessible, reliable, and welcoming to the population (46, 157). These strategies may involve expanding telephone helplines, sending mobile messages with qualified and non-stigmatizing information about COVID-19, providing information on protective measures, providing updates and real-time reports on the pandemic, and disseminating information on how to access urgent medical services and alternative means of interpersonal communication (48, 71, 127, 129, 150, 161, 163). However, it is necessary to guide the population on how to deal with anxiety caused by information overload (65, 75).
Employers also play an important role in the creation of support networks within organizations with the purpose of favoring an inclusive and supportive organizational culture (157). Specifically, companies should provide psychological and childcare support to female workers during the pandemic. Thus, employers are recommended to sponsor childcare programs, including collaborative home-based childcare services, to address school closures (37, 160). Strategies also need to ensure that people who choose or are forced to work from home do not experience negative career consequences, such as not being offered job promotions or training opportunities (64). At the same time, government institutions should ensure financial security, expand job opportunities, and provide public childcare services to support maternal mental health and child well-being (81, 83, 132, 157).
Governments are encouraged to include essential services to address violence against women in COVID-19 response plans, identifying strategies to make them accessible despite social distancing (76). Also, basic material and financial benefits should be provided by governments to guarantee people's quality of life and enable the adoption of preventive measures. Expanding income transfer programs and waiving conditionalities to increase access for vulnerable groups are highlighted strategies (71, 83, 92, 129). Creating community mental health programs for future outbreaks of infectious diseases is another relevant strategy (144).
In the research field, COVID-19 scientific councils, available in many countries, should be strengthened with scientists from different backgrounds, such as psychology, psychiatry, sociology, pedagogy, and education, for a broader and more adequate assessment of the impact of taken measures (163).
Discussion
The multiple consequences of the COVID-19 pandemic on women's daily lives have generated expectations about the production of knowledge on how this context has impacted mental health in the female population. There has been a profusion of studies, including those that are analyzed here, showing that women have experienced significant psychological distress during the course of the pandemic, which applies to those who already had a history of mental disorders and those who developed psychological symptoms from the pandemic.
Most studies demonstrated that women and young people were the groups most affected by mental distress in the pandemic, confirming the results of other investigations that reported substantially worsening levels of psychological distress in these population groups in the pandemic setting (1, 98).
The characterization of risk factors that psychologically affect women is consistent with those of previous studies conducted before the onset of COVID-19 and outside the context of global health crises, which examined the impact of sources of psychosocial and socioeconomic stress on mental health (168). The so-called risk factors can be considered aspects of inequalities through which women's distress could be discursively circumscribed, and they include low education, low income, lack of support, no partnerships, difficulties in reconciling work and childcare, and lack of access to public services, among others.
The social isolation disproportionately affected women, forcing them into prolonged coexistence with family members who may not have had friendly or cordial relationships. The constant psychological strain, exacerbated by the fear of illness and death, led to numerous conflicts within families and communities. Women, regardless of their role as heads of household, were burdened with caregiving responsibilities, often going to great lengths to protect their families from contamination. The risk of illness or death, often more acutely understood by women themselves, fueled tensions within families. The pressure to maintain protective and caring functions for adults, especially the elderly, children, and adolescents, during these extraordinarily demanding times, further increased women's psychological burden. Women who were able to maintain their jobs faced the added strain of providing financially for their families. Moreover, the isolation from friends, family, and community support networks exacerbated the challenges faced by women.
The approach to domestic violence and its impacts in the pandemic context, or to self-inflicted violence — for example, a study on Japanese university students showing the burden on young women — was very limited in the group of studies, despite the relevance of these topics in women's lives. Reports indicate that social isolation and confinement measures during the pandemic led to increased incidents of domestic violence, contributing to psychological distress among women (169–171). The psychological impact of violence, coupled with limited access to healthcare services and support systems, has exacerbated womeńs mental health struggles.
It is noteworthy that the findings regarding the impact of economic factors on mental health are contradictory. A significant body of literature supports the notion that lower socioeconomic status is associated with poorer mental health outcomes, a conclusion supported by some studies examined. However, evidence was found suggesting that higher socioeconomic status may be linked to greater increase in depressive symptoms during the pandemic, when compared to lower socioeconomic status. This contradiction can be better understood by considering variations in the underlying causes of mental health issues during the pandemic. Women with lower socioeconomic status were generally associated with poorer mental health outcomes due to the financial impact of the pandemic and the challenges of balancing child schoolwork, working from home and lack of childcare. On the other hand, upper socioeconomic class was linked to mental health challenges possibly due to higher pressure to maintain status and greater disruptions in lifestyle. It's important to point out that contradictions in the findings could also be attributed to methodological differences between studies (sample populations, measurement tools and the mental health outcomes assessed), as well as to contextual factors, such as cultural differences.
Particularly regarding economic-related anxiety, the results show contrasting patterns between gender in different cultural settings. For example, a United Kingdom study observed higher levels of distress among women (83), while in China young married men had more psychological symptoms during the pandemic than young women (106).
Another relevant gender disparity lies in the domain of work. Women allocated significantly more time to unpaid care work than men during lockdowns, leading to greater psychological distress. The challenges of balancing remote work with homeschooling and childcare, coupled with increased domestic responsibilities, likely contributed to these heightened health risks, particularly for mothers.
It is noteworthy that substantial evidence indicates that women, beyond the scope of health emergencies, experience greater fear and are more likely to develop anxiety disorders than men, with socialization processes playing a moderating role in these gender differences (172). Women, often bearing the brunt of economic downturns, may experience compounded stressors that exacerbate feelings of helplessness and anxiety. This highlights the importance of considering economic factors alongside gender when addressing mental health.
Further exploring the cultural dimension, traditional gender roles have placed a disproportionate burden on women, particularly in caregiving and household responsibilities, as already mentioned. However, some studies show differences between ethnic groups suggesting that cultural context has influenced mental health outcomes. For example, in China, higher levels of risk of mental disorder were found in men than in women (92) and young married men had more psychological symptoms during the pandemic than young women (106). Taubman-Bem-Arti et al. assessed stress and anxiety associated with COVID-19 among pregnant Arab and Jewish women living in Israel and found higher rates for Arab women (88).
In addition to gender roles, it is worth mentioning the role of community and collective experiences in shaping mental health outcomes. Arab society, for example, tends to be more collective, with lower levels of education, income, and employment. Other crucial aspect is that cultural beliefs and practices play a pivotal role in shaping individuals’ understanding of mental health and illness. This is particularly relevant in contexts where western notions of psychopathology may differ from local conceptions.
Moreover, its important to mention that cultural contexts influence the stigma associated with mental illness, which can deter individuals from seeking help. For instance, women may generally be more likely to request assistance, but the ones who face stigma and prejudice, such as migrants and black women, may face systemic barriers that limit their access to mental health services. This gap between population groups warrants more substantial analyses questioning how cultural issues influence psychological status, when they are responsible for marks of inequities that are experienced in a particular way by each woman. This construction takes place in language and challenges the possibilities of being of each woman (173). In this process, women's relations with their maternal role can be deidealized, since, on the one hand, women are always in a place of failure, of not being able to, of not having control, and on the other hand, their mental health is a supposed place of sanity, health, and safety (174, 175).
However, although the present sample referred to women as a vulnerable group, it appears that most studies take a limited approach to the problem by adopting psychiatric disorders and their standardized symptoms as special parameters of analysis and preferentially focusing on the presence of depression and anxiety. Therefore, they forget to explore the meaning of the singular situations experienced by each woman.
Importantly, several variations of the expression “mental health” were used in the search strategy, and different types of study were included to cover a greater diversity of perspectives. Nonetheless, the prevalence of symptoms understood as those of mental disorders constituted the main object of analysis in the publications.
The pandemic context created limitations to the methodological processes of participant recruitment and data collection. This resulted in a scenario in which the production of knowledge resorted almost exclusively to the use of self-administered questionnaires or, more infrequently, questionnaires administered via telephone by researchers. It is worth mentioning that research on mental health often relies heavily on self-reported data, which can introduce significant methodological challenge. Participants may overreport positive attributes or underreport negative ones to present a favorable self-image. Furthermore, individuals from different socioeconomic backgrounds may have varying levels of literacy, numeracy, or cultural factors that influence their ability to understand and respond to survey questions.
Although the articles included detailed descriptions of the measurement methods, the use of scales as a key parameter for assessing participant mental health status was rarely questioned by the authors. In general, if addressed, this concern was restricted to indicating that self-administration of scales, associated with lack of validation of the results by a mental health professional, were limiting factors for assessing participant mental health.
The most privileged approaches (quantitative and based on syndromic diagnoses) allowed establishing correlations between phenomena, but they also hampered an investigation of the true network of causal relationships between them. The studies also showed an important bias in sample selection, as they were conducted basically online and included participants who might have been biased. The study samples were significantly heterogeneous in terms of population, and the outcomes and research instruments used were highly diverse, which favored part of the population with access to communication media and ability to complete self-administered scales and questionnaires.
Cross-sectional studies, performed mostly at the peak of the pandemic in different countries, provided one overview of women's mental health at this stage. However, the evaluated outcomes may be very sensitive to the health and social isolation measures applied and the evolution of the response to these measures in each country or region. It is worth noting that specific cultural issues faced by female respondents may have different impacts on their mental health.
Conversely, since methodological choices surpass the simple definition of the most adequate means to approach a given object and express the authors’ position in the face of different conceptions and understandings of reality (176), the high number of quantitative designs focused on the use of scales seems to reflect a typical approach from the field of psychopathology. It sees the phenomenon of psychological distress not as a condition experienced by human subjects in their singularities, but as manifestations of the pathological condition that cause disorders to be corrected.
Regardless of country or culture of origin, as well as marital status and age, studies revealed that women (pregnant or not) showed more exuberant psychological symptoms in the COVID-19 pandemic context, including distress, when compared to men. There are, therefore, gender differences in psychological manifestations in response to the pandemic.
However, when discussing the results, the studies established little or no interaction with theoretical references that would help expand the understanding of how psychological distress has been experienced by women throughout the pandemic. The same observation applies to the proposed strategies and interventions.
There is a prevailing interest in pregnant and postpartum women, who are the object of 43% of the studies, including three literature reviews assessing the prevalence of psychiatric symptoms in the perinatal period (77, 94, 149). However, an analysis of the study discussions shows that choosing pregnant and postpartum women as the main subjects of interest denotes a concern with the consequences of the pandemic on the development of babies and their future psychic life, with less attention to the consequences on the lives of these women. This view of sexual and reproductive health negatively affects the health care services provided to pregnant women (10).
Importantly, women's health in the 19th and 20th centuries was intended to seek, with the development of healthy bodies destined for reproduction, fetal health. Löwy describes how, since the late 19th century, medicine has sought to foster the birth of healthy children by increasing surveillance of the bodies of pregnant women (177). One of the expressions of this surveillance was named prenatal care, which grew significantly in the mid-20th century. This parameter strongly inspired feminist criticisms in the 1970s and will expand on the submission of female bodies to normative practices that are often coercive (178).
In contemporary times, prenatal care incorporates, on the one hand, the universally accepted diagnostic tests that monitor mother-fetus health and, on the other hand, more controversial tests that make fetal anomalies visible. In any case, the bodies of pregnant women would essentially be used to monitor the fetus. Similarly, this study identified a concern with the construction of maternal mental health that seems to be mostly intended to ensure the birth of psychically healthy babies, which, in theory, would guarantee a future full of mentally healthy adults over time. In our perspective, women's mental health should be regarded as a primary focus per se, and studies should seek to show the penalties and emotional costs of their insertion in the social bond considering their specific perspectives in conversation with other social determinants of health, such as poverty, race/ethnicity, age, and sexual orientation.
Regarding policy implications, the studies present proposals across several areas of, but most of them focused on health care, with special attention to regular communication, screening for more severe cases, and specific psychotherapies. However, what is missing in the suggestions is the development of approaches that take the particularities of women's distress into account. Sociocultural elements should be considered, such as the prominence of women in caregiving roles, and the physical, psychological, financial, and caregiving impacts on the female population. Beyond immediate healthcare, social protection measures should be guaranteed immediately, supporting the specific needs that a health emergency requiring social isolation can generate. Additionally, specific training focused on women's mental health care should be developed at national and local levels, involving professionals from different areas, with a special focus on primary health care. A critical area for future research is the role of digital mental health resources during the pandemic. Telehealth has presented opportunities and challenges for mental health service delivery, especially for underserved populations. Research should evaluate the effectiveness of these digital interventions and identify barriers to access, ensuring that all minority groups can benefit from such services.
It´s important to remember that WHO has highlighted the relevance of social determinants of health, including gender, in specific processes of consultation and agreement with counterparts, the governments of the countries, and in articulation with partners such as academia, nongovernmental organizations, and companies, among others, as previously mentioned. However, in the specific case of COVID-19, communities and health systems seem to have generally preferred to consider women as carriers of excessive signs of psychological distress than to understand such signs as important effects in response to a very serious pandemic setting in which, as stated by Birman, women's feeling of helplessness was determined by real external, family, and institutional threats (31).
The results of this study show that the place where each woman is culturally, socially, and economically situated matters in the development of a higher or lower degree of psychological distress. Even in case of previous psychiatric symptoms, women seem to reveal through their psychological and social manifestations the difficulties of living and surviving in a pandemic world that threatens their own existence and that of their loved ones. Lower income and education, limited access to goods and services, and living alone or with children were all aspects that seem to push women towards greater psychological distress, as previously reported.
What cannot be deduced from the studies analyzed is how each woman psychically organizes her singular subjectivity, who listens to her suffering, where, and how she works out her emotional issues. These are probably important questions for future research. Therefore, perhaps depression and anxiety, in processes of the magnitude of the pandemic, as described by Dunker, could be understood not as a single, extremely severe illness, but as conditions that are variable and that function as an expression of collective systemic symptoms and indicators of social distress (32).
A relevant point when addressing the field of demands of the subject and subjectivities is that overcoming difficulties related to infrastructure or the search for equality will not definitively solve the problem of women's distress, who should be able to voice their uncertainties and be heard in their loneliness due to the pandemic isolation. The association of their mental state with other social determinants of health should also be explored.
In terms of limitations, we would like to note that our analysis excluded studies involving adolescents, as discussed previously. Nonetheless, it is known that children and adolescents has been significantly impacted by the pandemic, with female adolescents exhibiting a higher risk of depression and anxiety compared to their male counterparts (179, 180). The pandemic's limitations on social interaction have had a greater negative impact on adolescents and youth, who often depend on community support for validation and belonging. Adolescents may have experienced disappointments and frustrations, both in the school and family environments. In these cases, isolation and technology formed a closed system with very little exchange in situations of affective and sexual interactions. A topic for future research could be to investigate what new mechanisms could be in place for female adolescents in the post-pandemic time.
Likewise, it is important to note the limitation of the studies with respect to minority women. Even though this group was not well represented in the studies examined in our review, literature shows that situations of stigma, prejudice, limited access to services, increased isolation, and work restrictions have disproportionately affected refugee, migrant and other racialized women, particularly those living in poverty or facing economic hardship due to COVID-19 (181–183).
Conclusions
The post-pandemic period is an opportunity to build more integrated mental health strategies capable of addressing future public health crises. By synthesizing key findings, this study shed light on the nuanced ways in which the pandemic has affected women's mental health, contributing to the development of informed strategies and interventions to support women's mental well-being in times of adversity.
As captured by the reviewed studies, the amount of distress expressed by women, basically as anxiety and depression, seems to be more significant than that of men. However, instead of being understood as greater empathy with the experienced settings requiring immediate responses, this is considered a more vulnerable feature. Women are therefore seen as a group to be strengthened, and not as a product of relations between themselves and their symptoms, desires, and languages, or as an expression of a symbolic way of functioning in the social bond. In an attempt to protect themselves and the people around them, often in a context of inequality and greater distress in their territories of origin, they have developed actions of attention, concern, and care.
As a first conclusion, the strong and immediate reaction of women, as a group, shows that, in addition to individual responses, they had a particular position implying a deep subjective responsibility, as gender, social psychology, and psychoanalysis literatures suggest (184–187). Subjective responsibility, ie, responsibility of the subject (in this case, women), implies attesting to a deep commitment to one's desire or intention (in this case, maintenance and care of biological and social life). Women, as the study shows, adopt a position of great concern with the matters concerning their lives and those of their children and families. They are concerned about how to reconcile working and caring for themselves and their surroundings, and about how to develop actions associated with physical, psychological, and social maintenance around their own lives and those of their children, families, and community, while strongly resenting the isolation requirements. Thus, instead of reading women as “more fragile,” a more appropriate approach would be to understand this group as singularly resilient.
A second aspect to consider is that the studies on pregnant women generally aimed to find ways of diagnosing their condition and “psychologically stabilizing” them, since the disorders are believed to cause harm in the short, medium, and long terms to women, but especially to the neurobehavioral development of their fetuses. Stress as a factor that reduces women's immune capacity is also highlighted, but always referring to a biological aspect, namely the long-lasting action of stress, which is a quite limiting approach. Modulating this argumentative mode could be relevant because perinatal mental health also reveals, as previously mentioned, discourses associated with the sociocultural systems into which they are inserted.
Although studies added some complexity by including different population groups, the academic contribution to the construction of explanatory hypotheses that seek to understand and directly alleviate the distress experienced by women has been limited. Thus, from our perspective, one of the main aspects in the process of expanding the understanding of how women operate in the field of mental health would be to remove them from a place of vulnerability to introduce them in spaces that value their psychological singularities, embedded in their own cultures, where they can comprehend gender, race, age, and economic inequalities and respond to them through language in specific ways.
A third observation is that the anxieties identified in the reviewed studies do not allow us to determine any special biological condition that could justify an experience of greater distress for women. On the contrary, psychological distress generally refers to recurrent psychological manifestations that reinforce the feeling of emotional helplessness regardless of the territories and processes in which they develop. This is related to how women's singularities are structured. Thus, women should be able to access health care or other services that are prepared to listen to what each one of them has to say.
Public policies for women's mental health must be reviewed in the short, medium, and long terms and analyzed through interdisciplinary and intersectoral frameworks. Recognizing the problem, listening to it, and assessing its magnitude require, in addition to a concern with disease burden and health system costs, a comprehensive prevention and care approach that goes beyond health services and reaches other areas, such as labor. Adopting policies that focus on distress experienced by women may favor a psychological reorganization of each subject, providing them with greater autonomy and singularity when facing critical situations. In the same direction, health decision-makers need to allocate increased resources to all fields to enable specific listening and care processes for women in different territories, avoiding pathologization and considering social markers translated into the language of each one. Women need to be heard and search for their own meanings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
MA: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Supervision, Validation, Visualization, Writing – original draft. AC: Formal Analysis, Investigation, Methodology, Writing – original draft. TF: Data curation, Investigation, Project administration, Resources, Validation, Visualization, Writing – review & editing. CR: Investigation, Methodology, Validation, Writing – review & editing. BB: Data curation, Investigation, Writing – original draft. SS: Conceptualization, Funding acquisition, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
To the Latin American Center for Perinatology, Women, and Reproductive Health (CLAP/WR), and the Pan American Health Organization/World Health Organization for its support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
Some of the authors are a staff member of the Pan American Health Organization. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the views, decisions or policies of the Pan American Health Organization.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1414355/full#supplementary-material
References
1. Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398(10312):1700–12. Available online at: http://www.thelancet.com/article/S0140673621021437/fulltext (cited May 7, 2022). doi: 10.1016/S0140-6736(21)02143-7
2. Tausch A, E Souza RO, Viciana CM, Cayetano C, Barbosa J, Hennis AJ. Strengthening mental health responses to COVID-19 in the Americas: a health policy analysis and recommendations. Lancet Reg Heal Am. (2022) 5:100118. doi: 10.1016/j.lana.2021.100118
3. Organización Panamericana de la Salud (OPS). COVID-19 ocasiona impactos “devastadores” en las mujeres, afirma la Directora de la OPS. Available online at: https://www.paho.org/es/noticias/26-5-2021-covid-19-ocasiona-impactos-devastadores-mujeres-afirma-directora-ops (Accessed May 6, 2022).
4. Organização Pan-Americana da Saúde (OPS). Saúde nas Américas. Resumo do panorama regional e perfil do Brasil. Available online at: https://iris.paho.org/bitstream/handle/10665.2/34323/9789275719671_por.pdf?sequence=8 (cited May 7, 2022).
5. Ferreira-Filho ES, de Melo NR, Sorpreso ICE, Bahamondes L, Simões RDS, Soares-Júnior JM, et al. Contraception and reproductive planning during the COVID-19 pandemic. Expert Rev Clin Pharmacol. (2020) 13(6):615–22. doi: 10.1080/17512433.2020.1782738
6. Vasconcellos Freitas-Jesus J, Rodrigues L, Surita FG. The experience of women infected by the COVID-19 during pregnancy in Brazil: a qualitative study protocol. Reproductive Health. (2020) 17:108. doi: 10.1186/s12978-020-00958-z
7. Biehl J, Prates LEA, Amon JJ. Supreme court v. Necropolitics: the chaotic judicialization of COVID-19 in Brazil. Health Hum Rights. (2021) 23(1):151. Available online at:/pmc/articles/PMC8233022/(cited May 7, 2022).34194209
8. Rosales Flores RA, Pereira Abagaro C, Valongueiro Alves S, Boy MG, Muñoz Muñoz C, Marmolejo J. El trabajo que nunca se termina: mujeres, trabajo doméstico y teletrabajo en la pandemia de COVID-19: La situacion de Argentina, Brasil, Chile e México. In: Pereira Abagaro C, Boy M, Rosales Flores RA, Marmolejo J, Muñoz Muñoz C, editors. La pandemia social de COVID-19 en América Latina. Buenos Aires, Argentina: Teseo (2021). p. 29–66. Available online at: http://hdl.handle.net/11336/134835
9. Global Health 50/50. COVID-19 Sex-Disaggregated Data Tracker. Available online at: https://globalhealth5050.org/the-sex-gender-and-covid-19-project/the-data-tracker/(Accessed May 6, 2022).
10. Diniz D, Brito L, Rondon G. Maternal mortality and the lack of women-centered care in Brazil during COVID-19: preliminary findings of a qualitative study. Lancet Reg Heal Am. (2022) 10:100239. doi: 10.1016/j
11. Organización Panamericana de la Salud (OPS). La carga de los trastornos mentales en la Región de las Américas. (2018). Available online at: https://iris.paho.org/bitstream/handle/10665.2/49578/9789275320280_spa.pdf?sequence=9 (Accessed May 6, 2022).
12. Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The lancet commission on global mental health and sustainable development. Lancet. (2018) 392(10157):1553–98. doi: 10.1016/S0140-6736(18)31612-X
13. World Health Organization (WHO). Making the investment case for mental health: a WHO/UNDP methodological guidance note. Available online at: https://apps.who.int/iris/handle/10665/325116 (Accessed May 6, 2022).
14. World Health Organization (WHO). Mental health in the pandemic. Bulletin of the World Health Organization. doi: 10.2471/BLT.21.020921 (Accessed May 6, 2022).
15. World Health Organization (WHO). Mental Health ATLAS 2020. Available online at: https://www.who.int/publications/i/item/9789240036703 (Accessed May 6, 2022).
16. World Health Organization (WHO). Mental health crisis services: promoting person-centred and rights-based approaches. Available online at: https://www.who.int/publications/i/item/9789240025721 (Accessed May 6, 2022).
17. World Health Organization (WHO). Mental health aspects of women’s reproductive health: a global review of the literature. Available online at: https://apps.who.int/iris/handle/10665/43846 (Accessed May 6, 2022).
18. World Health Organization (WHO). Supporting the mental health and well-being of the health and care workforce. Available online at: https://www.euro.who.int/en/health-topics/noncommunicable-diseases/mental-health/publications/2021/supporting-the-mental-health-and-well-being-of-the-health-and-care-workforce-2021 (Accessed May 6, 2022).
19. World Health Organization (WHO). Investing in mental health for sustainable development. Available online at: https://apps.who.int/iris/handle/10665/324949?locale-attribute=pt& (Accessed May 6, 2022).
20. World Health Organization (WHO). Mental health investment case: a guidance note. Available online at: https://apps.who.int/iris/rest/bitstreams/1336737/retrieve (Accessed May 6, 2022).
21. World Health Organization (WHO). Women’s mental health: an evidence based review. Available online at: https://apps.who.int/iris/handle/10665/66539 (Accessed May 6, 2022).
22. World Health Organization (WHO). Mental health in primary care: illusion or inclusion? Available online at: https://apps.who.int/iris/handle/10665/326298 (Accessed May 6, 2022).
23. World Health Organization (WHO). Comprehensive mental health action plan 2013-2030. Available online at: https://www.who.int/publications/i/item/9789240031029 (Accessed May 6, 2022).
24. World Health Organization. WHO menu of cost-effective interventions for mental health. Available online at: https://www.who.int/publications/i/item/9789240031081 (Accessed May 6, 2022).
25. World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak. Available online at: https://apps.who.int/iris/bitstream/handle/10665/331490/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf?sequence=1&isAllowed=y (Accessed May 6, 2022).
26. World Health Organization. Community mental health centres: Promoting person-centred and rights-based approaches. Available online at: https://www.who.int/publications/i/item/9789240025769 (Accessed May 6, 2022).
27. World Health Organization. The mental health of health workers in the pandemic. Bull World Health Organ. (2021) 99(6):410–1. doi: 10.2471/BLT.21.020621
28. Vanderkruik R, Gonsalves L, Kapustianyk G, Allen T, Say L. Mental health of adolescents associated with sexual and reproductive outcomes: a systematic review. Bull World Health Organ. (2021) 99(5):359–373K. doi: 10.2471/BLT.20.254144
29. World Health Organization. Resolution EB 148. R2. Available online at: https://apps.who.int/gb/e/e_eb148.html (Accessed May 6, 2022).
30. Lancet Psychiatry Series on Women’s Mental Health. The Lancet Psychiatry. Available online at: https://www.thelancet.com/series/women-mental-health (Accessed May 7, 2022).
31. Birman J. O trauma na pandemia do coronavírus: suas dimensões políticas, sociais, econômicas, ecológicas, culturais, éticas e científicas. Rio de Janeiro: Civilização Brasileira (2021).
33. Pereira MEC. Projeto de uma (psico)patologia do sujeito (I): Redefinição do conceito de psicopatologia à luz da questão do sujeito. (2020) 22:828–58.
34. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8(1):19–32. doi: 10.1080/1364557032000119616
35. The Joanna Briggs Institute. Joanna Briggs Institute Reviewers’ Manual. Available online at: https://nursing.lsuhsc.edu/JBI/docs/ReviewersManuals/Scoping-.pdf (Accessed May 7, 2022).
36. Mandelkorn U, Genzer S, Choshen-Hillel S, Reiter J, E Cruz MM, Hochner H, et al. Escalation of sleep disturbances amid the COVID-19 pandemic: a cross-sectional international study. J Clin Sleep Med. (2021) 17(1):45–53. doi: 10.5664/jcsm.8800
37. Mavroudis CL, Landau S, Brooks E, Bergmark R, Berlin NL, Blumenthal B, et al. The relationship between surgeon gender and stress during the COVID-19 pandemic. Ann Surg. (2021) 273(4):625–9. doi: 10.1097/SLA.0000000000004762
38. Ben-Kimhy R, Youngster M, Medina-Artom TR, Avraham S, Gat I, Haham LM, et al. Fertility patients under COVID-19: attitudes, perceptions and psychological reactions. Hum Reprod. (2020) 35:deaa248–undefined. doi: 10.1093/humrep/deaa248
39. Berthelot N, Lemieux R, Garon-Bissonnette J, Drouin-Maziade C, Martel É, Maziade M. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet Gynecol Scand. (2020) 99(7):848–55. doi: 10.1111/aogs.13925
40. Bonsaksen T, Heir T, Schou-Bredal I, Ekeberg Ø, Skogstad L, Grimholt TK. Post traumatic stress disorder and associated factors during the early stage of the COVID-19 pandemic in Norway. Int J Environ Res Public Health. (2020) 17(24):1–10. doi: 10.3390/ijerph17249210
41. Chivers BR, Garad RM, Boyle JA, Skouteris H, Teede HJ, Harrison CL. Perinatal distress during COVID-19: thematic analysis of an online parenting forum. J Med Internet Res. (2020) 22(9). doi: 10.2196/22002
42. Conti C, Fontanesi L, Lanzara R, Rosa I, Porcelli P. Fragile heroes. The psychological impact of the COVID-19 pandemic on health-care workers in Italy. PLoS One. (2020) 15(11 November). doi: 10.1371/journal.pone.0242538
43. Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw Open. (2020) 3(10):e2025591. doi: 10.1001/jamanetworkopen.2020.25591
44. De Zordo S, Mishtal J, Zanini G, Gerdts C. Consequences of gestational age limits for people needing abortion care during the COVID-19 pandemic. Reprod Health Matters. (2020) 28(1). doi: 10.1080/26410397.2020.1818377
45. Esposito V, Rania E, Lico D, Pedri S, Fiorenza A, Strati MF, et al. Influence of COVID-19 pandemic on the psychological status of infertile couples. Eur J Obstet Gynecol Reprod Biol. (2020) 253:148–53. doi: 10.1016/j.ejogrb.2020.08.025
46. Fernández RS, Crivelli L, Guimet NM, Allegri RF, Pedreira ME. Psychological distress associated with COVID-19 quarantine: latent profile analysis, outcome prediction and mediation analysis. J Affect Disord. (2020) 277:75–84. doi: 10.1016/j.jad.2020.07.133
47. García-Fernández L, Romero-Ferreiro V, López-Roldán PD, Padilla S, Rodriguez-Jimenez R. Mental health in elderly Spanish people in times of COVID-19 outbreak. Am J Geriatr Psychiatry. (2020) 28(10):1040–5. doi: 10.1016/j.jagp.2020.06.027
48. Gómez-Salgado J, Andrés-Villas M, Domínguez-Salas S, Díaz-Milanés D, Ruiz-Frutos C. Related health factors of psychological distress during the COVID-19. Int J Environ Res Public Health. (2020) 17(11):3947. doi: 10.3390/ijerph17113947
49. Gopal A, Sharma AJ, Subramanyam MA. Dynamics of psychological responses to COVID-19 in India: a longitudinal study. PLoS One. (2020) 15(10 OCTOBER). doi: 10.1371/journal.pone.0240650
50. Gordon JL, Balsom AA. The psychological impact of fertility treatment suspensions during the COVID-19 pandemic. PLoS One. (2020) 15(9):e0239253–undefined. doi: 10.1371/journal.pone.0239253
51. Hidalgo MD, Balluerka N, Gorostiaga A, Espada JP, Santed MÁ, Padilla JL, et al. The psychological consequences of COVID-19 and lockdown in the Spanish population: an exploratory sequential design. Int J Environ Res Public Health. (2020) 17(22):1–17. doi: 10.3390/ijerph17228578
52. Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. (2020) 87:11–7. doi: 10.1016/j.bbi.2020.03.028
53. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3(3). doi: 10.1001/jamanetworkopen.2020.3976
54. Lebel C, Mackinnon A, Bagshawe M, Tomfohr-Madsen L, Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. (2020) 277:5–13. doi: 10.1016/j.jad.2020.07.126
55. Liu CH, Stevens C, Conrad RC, Hahm HC. Evidence for elevated psychiatric distress, poor sleep, and quality of life concerns during the COVID-19 pandemic among U.S. Young adults with suspected and reported psychiatric diagnoses. Psychiatry Res. (2020) 292:113345. doi: 10.1016/j.psychres.2020.113345
56. Liu X, Chen M, Wang Y, Sun L, Zhang J, Shi Y, et al. Prenatal anxiety and obstetric decisions among pregnant women in Wuhan and Chongqing during the COVID-19 outbreak: a cross-sectional study. BJOG An Int J Obstet Gynaecol. (2020) 127(10):1229–40. doi: 10.1111/1471-0528.16381
57. Luceño-Moreno L, Talavera-Velasco B, García-Albuerne Y, Martín-García J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in spanish health personnel during the COVID-19 pandemic. Int J Environ Res Public Health. (2020) 17(15):1–29. doi: 10.3390/ijerph17155514
58. Luo M, Guo L, Yu M, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—a systematic review and meta-analysis. Psychiatry Res. (2020) 291. doi: 10.1016/j.psychres.2020.113190
59. Maaravi Y, Heller B. Not all worries were created equal: the case of COVID-19 anxiety. Public Health. (2020) 185:243–5. doi: 10.1016/j.puhe.2020.06.032
60. Mappa I, Distefano FA, Rizzo G. Effects of coronavirus 19 pandemic on maternal anxiety during pregnancy: a prospectic observational study. J Perinat Med. (2020) 48(6):545–50. doi: 10.1515/jpm-2020-0182
61. Matsubara S, Matsubara D, Matsubara T. Letter to ‘clinical update on COVID-19 in pregnancy: a review article’: obstetric or gynecologic papers on COVID-19 should have an informative title. Journal of Obstetrics and Gynaecology Research. (2020) 46. doi: 10.1111/jog.14470
62. Moyer CA, Compton SD, Kaselitz E, Muzik M. Pregnancy-related anxiety during COVID-19: a nationwide survey of 2740 pregnant women. Arch Womens Ment Health. (2020) 23(6):757–65. doi: 10.1007/s00737-020-01073-5
63. Ng QJ, Koh KM, Tagore S, Mathur M. Perception and feelings of antenatal women during COVID-19 pandemic: a cross-sectional survey. Ann Acad Med Singapore. (2020) 49(8):543–52. doi: 10.1186/s12884-020-03378-w
64. Oakman J, Kinsman N, Stuckey R, Graham M, Weale V. A rapid review of mental and physical health effects of working at home: how do we optimise health? BMC Public Health. (2020) 20(1). doi: 10.1186/s12889-020-09875-z
65. Orte C, Sánchez-Prieto L, Barrientos-Báez A, Domínguez DC. Evaluation of distress and risk perception associated with COVID-19 in vulnerable groups. Int J Environ Res Public Health. (2020) 17(24). doi: 10.3390/ijerph17249207
66. Ostacoli L, Cosma S, Bevilacqua F, Berchialla P, Bovetti M, Carosso AR, et al. Psychosocial factors associated with postpartum psychological distress during the COVID-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. (2020) 20(1). doi: 10.1186/s12884-020-03399-5
67. Özdin S, Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish Socisety: the importance of gender. Int J Soc Psychiatry. (2020) 66(5):504–11. doi: 10.1177/0020764020927051
68. Pariente G, Wissotzky Broder O, Sheiner E, Lanxner Battat T, Mazor E, Yaniv Salem S, et al. Risk for probable post-partum depression among women during the COVID-19 pandemic. Arch Womens Ment Health. (2020) 23(6):767–73. doi: 10.1007/s00737-020-01075-3
69. Parrado-González A, León-Jariego JC. COVID-19: factors associated with emotional distress and psychological morbidity in spanish population | COVID-19: factores asociados al malestar emocional y morbilidad psíquica en población española. Rev Esp Salud Publica. (2020) 94. doi: 10.1016/j.comppsych.2020.152192
70. Parra-Saavedra M, Villa-Villa I, Pérez-Olivo J, Guzman-Polania L, Galvis-Centurion P, Cumplido-Romero Á, et al. Attitudes and collateral psychological effects of COVID-19 in pregnant women in Colombia. Int J Gynecol Obstet. (2020) 151(2):203–8. doi: 10.1002/ijgo.13348
71. Paz C, Mascialino G, Adana-Díaz L, Rodríguez-Lorenzana A, Simbaña-Rivera K, Gómez-Barreno L, et al. Behavioral and sociodemographic predictors of anxiety and depression in patients under epidemiological surveillance for COVID-19 in Ecuador. PLoS One. (2020) 15(9 September). doi: 10.1371/journal.pone.0240008
72. Preis H, Mahaffey B, Heiselman C, Lobel M. Vulnerability and resilience to pandemic-related stress among U.S. Women pregnant at the start of the COVID-19 pandemic. Soc Sci Med. (2020) 266:266. doi: 10.1016/j.socscimed.2020.113348
73. Ravaldi C, Ricca V, Wilson A, Homer C, Vannacci A, Riecher-Rössler A. Previous psychopathology predicted severe COVID-19 concern, anxiety, and PTSD symptoms in pregnant women during “lockdown” in Italy. Arch Womens Ment Health. (2020) 23:783–6. doi: 10.1007/s00737-020-01086-0
74. Reizer A, Koslowsky M, Geffen L. Living in fear: the relationship between fear of COVID-19, distress, health, and marital satisfaction among Israeli women. Health Care Women Int. (2020) 41(11–12):1273–93. doi: 10.1080/07399332.2020.1829626
75. Rodríguez-Rey R, Garrido-Hernansaiz H, Collado S. Psychological impact of COVID-19 in Spain: early data report. Psychol Trauma Theory, Res Pract Policy. (2020) 12:550–2. doi: 10.1037/tra0000943
76. Roesch E, Amin A, Gupta J, García-Moreno C. Violence against women during COVID-19 pandemic restrictions. The BMJ. (2020) 369. doi: 10.1136/bmj.m1712
77. Ryan GA, Purandare NC, McAuliffe FM, Hod M, Purandare CN. Clinical update on COVID-19 in pregnancy: a review article. J Obstet Gynaecol Res. (2020) 46:1235–45. doi: 10.1111/jog.14321
78. Salameh P, Hajj A, Badro DA, Abou selwan C, Aoun R, Sacre H. Mental health outcomes of the COVID-19 pandemic and a collapsing economy: perspectives from a developing country. Psychiatry Res. (2020) 294. doi: 10.1016/j.psychres.2020.113520
79. Schiavi MC, Spina V, Zullo MA, Colagiovanni V, Luffarelli P, Rago R, et al. Love in the time of COVID-19: sexual function and quality of life analysis during the social distancing measures in a group of Italian reproductive-age women. J Sex Med. (2020) 17(8):1407–13. doi: 10.1016/j.jsxm.2020.06.006
80. Sediri S, Zgueb Y, Ouanes S, Ouali U, Bourgou S, Jomli R, et al. Women’s mental health: acute impact of COVID-19 pandemic on domestic violence. Arch Womens Ment Health. (2020) 23(6):749–56. doi: 10.1007/s00737-020-01082-4
81. Silverman ME, Burgos L, Rodriguez ZI, Afzal O, Kalishman A, Callipari F, et al. Postpartum mood among universally screened high and low socioeconomic status patients during COVID-19 social restrictions in New York City. Sci Rep. (2020) 10(1). doi: 10.1038/s41598-020-79564-9
82. Silverman ME, Medeiros C, Burgos L. Early pregnancy mood before and during COVID-19 community restrictions among women of low socioeconomic status in New York City: a preliminary study. Arch Womens Ment Health. (2020) 23(6):779–82. doi: 10.1007/s00737-020-01061-9
83. Simha A, Prasad R, Ahmed S, Rao NP. Effect of gender and clinical-financial vulnerability on mental distress due to COVID-19. Arch Womens Ment Health. (2020) 23(6):775–7. doi: 10.1007/s00737-020-01097-x
84. Solomou I, Constantinidou F. Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: age and sex matter. Int J Environ Res Public Health. (2020) 17(14). doi: 10.3390/ijerph17144924
85. Souto S, Albuquerque RS, Prata AP. Fear of childbirth in time of the new coronavirus pandemic. Rev Bras Enferm. (2020) 73:e20200551. doi: 10.1590/0034-7167-2020-0551
86. Stepowicz A, Wencka B, Bieńkiewicz J, Horzelski W, Grzesiak M. Stress and anxiety levels in pregnant and post-partum women during the COVID-19 pandemic. Int J Environ Res Public Health. (2020) 17(24). doi: 10.3390/ijerph17249450
87. Szabo A, Ábel K, Boros S. Attitudes toward COVID-19 and stress levels in Hungary: effects of age, perceived health status, and gender. Psychol Trauma Theory Res Pract Policy. (2020) 12(6):572–5. doi: 10.1037/tra0000665
88. Taubman–Ben-Ari O, Chasson M, Abu Sharkia S, Weiss E. Distress and anxiety associated with COVID-19 among Jewish and Arab pregnant women in Israel. J Reprod Infant Psychol. (2020) 38(3):340–8. doi: 10.1080/02646838.2020.1786037
89. Vahedian-Azimi A, Moayed MS, Rahimibashar F, Shojaei S, Ashtari S, Pourhoseingholi MA. Comparison of the severity of psychological distress among four groups of an Iranian population regarding COVID-19 pandemic. BMC Psychiatry. (2020) 20(1). doi: 10.1186/s12888-020-02804-9
90. Wenham C, Smith J, Davies SE, Feng H, Grépin KA, Harman S, et al. Women are most affected by pandemics — lessons from past outbreaks. Nature. (2020) 583:194–8. doi: 10.1038/d41586-020-02006-z
91. Werner EA, Aloisio CE, Butler AD, D’antonio KM, Kenny JM, Mitchell A, et al. Addressing mental health in patients and providers during the COVID-19 pandemic. Semin Perinatol. (2020) 44(7):151279–undefined. doi: 10.1016/j.semperi.2020.151279
92. Wu M, Han H, Lin T, Chen M, Wu J, Du X, et al. Prevalence and risk factors of mental distress in China during the outbreak of COVID-19: a national cross-sectional survey. Brain Behav. (2020) 10(11). doi: 10.1002/brb3.1818
93. Wu Y, Zhang C, Liu H, Duan C, Li C, Fan J, et al. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am J Obstet Gynecol. (2020) 223(2). doi: 10.1016/j.ajog.2020.05.009
94. Yee J, Kim W, Han JM, Yoon HY, Lee N, Lee KE, et al. Clinical manifestations and perinatal outcomes of pregnant women with COVID-19: a systematic review and meta-analysis. Sci Rep. (2020) 10(1). doi: 10.1038/s41598-020-75096-4
95. Zheng QX, Jiang XM, Lin Y, Liu GH, Lin YP, Kang YL, et al. The influence of psychological response and security sense on pregnancy stress during the outbreak of coronavirus disease 2019: a mediating model. J Clin Nurs. (2020) 29:4248–57. doi: 10.1111/jocn.15460
96. Chen R, Sun C, Chen J-J, Jen H-J, Kang XL, Kao C-C, et al. A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int J Ment Health Nurs. (2021) 30(1):102–16. doi: 10.1111/inm.12796
97. Chen Y, Liu Y. Which risk factors matter more for psychological distress during the COVID-19 pandemic? An application approach of gradient boosting decision trees. Int J Environ Res Public Health. (2021) 18(11). doi: 10.3390/ijerph18115879
98. Davillas A, Jones AM. The first wave of the COVID-19 pandemic and its impact on socioeconomic inequality in psychological distress in the UK. Heal Econ (United Kingdom). (2021) 30(7):1668–83. doi: 10.1002/hec.4275
99. Del Rio-Casanova L, Sanchez-Martin M, Garcia-Dantas A, Gonzalez-Vazquez A, Justo A. Psychological responses according to gender during the early stage of COVID-19 in Spain. Int J Environ Res Public Health. (2021) 18. doi: 10.3390/ijerph18073731
100. Delle Donne V, Ciccarelli N, Massaroni V, Lombardi F, Lamonica S, Borghetti A, et al. Psychological distress during the initial stage of the COVID-19 pandemic in an Italian population living with HIV: an online survey. Infez Med. (2021) 29(1):54–64. doi: 10.21203/rs.3.rs-98904/v2
101. Duran S, Erkin Ö. Psychologic distress and sleep quality among adults in Turkey during the COVID-19 pandemic. Prog Neuro-Psychopharmacology Biol Psychiatry. (2021) 107. doi: 10.1016/j.pnpbp.2021.110254
102. Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. (2021) 8(2):141–9. doi: 10.1016/S2215-0366(20)30482-X
103. Garcia-Fernandez L, Romero-Ferreiro V, Padilla S, David Lopez-Roldan P, Monzo-Garcia M, Rodriguez-Jimenez R. Gender differences in emotional response to the COVID-19 outbreak in Spain. Brain Behav. (2021) 11:e01934. doi: 10.1002/brb3.1934
104. Haham LM, Youngster M, Shani AK, Yee S, Ben-Kimhy R, Medina-Artom TR, et al. Suspension of fertility treatment during the COVID-19 pandemic: views, emotional reactions and psychological distress among women undergoing fertility treatment. Reprod Biomed Online. (2021) 42(4):849–58. doi: 10.1016/j.rbmo.2021.01.007
105. Hocaoglu M, Ayaz R, Gunay T, Akin E, Turgut A, Karateke A. Anxiety and post-traumatic stress disorder symptoms in pregnant women during the COVID-19 pandemic’s delay phase. Psychiatr Danub. (2021) 32(3–4):521–6. doi: 10.24869/psyd.2020.521
106. Liu C, Liu D, Huang N, Fu M, Ahmed JF, Zhang Y, et al. The combined impact of gender and age on post-traumatic stress symptoms, depression, and insomnia during COVID-19 outbreak in China. Front Public Heal. (2021) 8:620023. doi: 10.3389/fpubh.2020.620023
107. Liu CH, Erdei C, Mittal L. Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 pandemic. Psychiatry Res. (2021) 295. doi: 10.1016/j.psychres.2020.113552
108. Lorant V, Smith P, Van den Broeck K, Nicaise P. Psychological distress associated with the COVID-19 pandemic and suppression measures during the first wave in Belgium. BMC Psychiatry. (2021) 21(1). doi: 10.1186/s12888-021-03109-1
109. Lorentz MS, Chagas LB, Perez AV, da Silva Cassol PA, Vettorazzi J, Lubianca JN. Correlation between depressive symptoms and sexual dysfunction in postpartum women during the COVID-19 pandemic. Eur J Obstet Gynecol Reprod Biol. (2021) 258:162–7. doi: 10.1016/j.ejogrb.2020.12.039
110. Machado MMT, Rocha HAL, Castro MC, Sampaio EGM, Oliveira FA, da Silva JPF, et al. COVID-19 and mental health of pregnant women in ceará, Brazil. Rev Saude Publica. (2021) 55. doi: 10.11606/s1518-8787.2021055003225
111. Megalakaki O, Kokou-Kpolou CK, Vaudé J, Park S, Iorfa SK, Cénat JM, et al. Does peritraumatic distress predict PTSD, depression and anxiety symptoms during and after COVID-19 lockdown in France? A prospective longitudinal study. J Psychiatr Res. (2021) 137:81–8. doi: 10.1016/j.jpsychires.2021.02.035
112. Mamun MA, Sakib N, Gozal D, Bhuiyan AKMI, Hossain S, Bodrud-Doza M, et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: a population-based nationwide study. J Affect Disord. (2021) 279:462–72. doi: 10.1016/j.jad.2020.10.036
113. Mariño-Narvaez C, Puertas-Gonzalez JA, Romero-Gonzalez B, Peralta-Ramirez MI. Giving birth during the COVID-19 pandemic: the impact on birth satisfaction and postpartum depression. Int J Gynecol Obstet. (2021) 153(1):83–8. doi: 10.1002/ijgo.13565
114. Mayopoulos GA, Ein-Dor T, Dishy GA, Nandru R, Chan SJ, Hanley LE, et al. COVID-19 is associated with traumatic childbirth and subsequent mother-infant bonding problems. J Affect Disord. (2021) 282:122–5. doi: 10.1016/j.jad.2020.12.101
115. McFarland MJ, McFarland CAS, Hill TD, D’Oria R. Postpartum depressive symptoms during the beginning of the COVID-19 pandemic: an examination of population birth data from Central New Jersey. Matern Child Health J. (2021) 25(3):353–9. doi: 10.1007/s10995-020-03116-w
116. Miguel-Puga JA, Cooper-Bribiesca D, Avelar-Garnica FJ, Sanchez-Hurtado LA, Colin-Martínez T, Espinosa-Poblano E, et al. Burnout, depersonalization, and anxiety contribute to post-traumatic stress in frontline health workers at COVID-19 patient care, a follow-up study. Brain Behav. (2021) 11(3). doi: 10.1002/brb3.2007
117. Mirzaei N, Jahanian Sadatmahalleh S, Bahri Khomami M, Moini A, Kazemnejad A. Sexual function, mental health, and quality of life under strain of COVID-19 pandemic in Iranian pregnant and lactating women: a comparative cross-sectional study. Health Qual Life Outcomes. (2021) 19(1). doi: 10.1186/s12955-021-01720-0
118. Mizrak Sahin B, Kabakci EN. The experiences of pregnant women during the COVID-19 pandemic in Turkey: a qualitative study. Women Birth. (2021) 34:162–9. doi: 10.1016/j.wombi.2020.09.022
119. Mortazavi F, Ghardashi F. The lived experiences of pregnant women during COVID-19 pandemic: a descriptive phenomenological study. BMC Pregnancy Childbirth. (2021) 21(1). doi: 10.1186/s12884-021-03691-y
120. Mortazavi F, Mehrabadi M, KiaeeTabar R. Pregnant women’s well-being and worry during the COVID-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. (2021) 21(1). doi: 10.1186/s12884-021-03548-4
121. Naghizadeh S, Mirghafourvand M, Mohammadirad R. Domestic violence and its relationship with quality of life in pregnant women during the outbreak of COVID-19 disease. BMC Pregnancy Childbirth. (2021) 21(1). doi: 10.1186/s12884-021-03579-x
122. Naurin E, Markstedt E, Stolle D, Enström D, Wallin A, Andreasson I, et al. Pregnant under the pressure of a pandemic: a large-scale longitudinal survey before and during the COVID-19 outbreak. Eur J Public Health. (2021) 31(1):7–13. doi: 10.1093/eurpub/ckaa223
123. Niela-Vilen H, Auxier J, Ekholm E, Sarhaddi F, Mehrabadi MA, Mahmoudzadeh A, et al. Pregnant women’s daily patterns of well-being before and during the COVID-19 pandemic in Finland: longitudinal monitoring through smartwatch technology. PLoS One. (2021) 16(2 February). doi: 10.1371/journal.pone.0246494
124. Nomura K, Minamizono S, Maeda E, Kim R, Iwata T, Hirayama J, et al. Cross-sectional survey of depressive symptoms and suicide-related ideation at a Japanese national university during the COVID-19 stay-home order. Environ Health Prev Med. (2021) 26(1). doi: 10.1186/s12199-021-00953-1
125. Osborne LM, Kimmel MC, Surkan PJ. The crisis of perinatal mental health in the age of COVID-19. Matern Child Health J. (2021) 25:349–52. doi: 10.1007/s10995-020-03114-y
126. Oswald TK, Rumbold AR, Kedzior SGE, Kohler M, Moore VM. Mental health of young Australians during the COVID-19 pandemic: exploring the roles of employment precarity, screen time, and contact with nature. Int J Environ Res Public Health. (2021) 18(11). doi: 10.3390/ijerph18115630
127. Parisi R, Lagomarsino F, Rania N, Coppola I. Women face to fear and safety devices during the COVID-19 pandemic in Italy: impact of physical distancing on individual responsibility, intimate, and social relationship. Front Public Heal. (2021) 9. doi: 10.3389/fpubh.2021.622155
128. Paulino M, Dumas-Diniz R, Brissos S, Brites R, Alho L, Simões MR, et al. COVID-19 in Portugal: exploring the immediate psychological impact on the general population. Psychol Heal Med. (2021) 26(1):44–55. doi: 10.1080/13548506.2020.1808236
129. Porter C, Favara M, Hittmeyer A, Scott D, Sánchez Jiménez A, Ellanki R, et al. Impact of the COVID-19 pandemic on anxiety and depression symptoms of young people in the global south: evidence from a four-country cohort study. BMJ Open. (2021) 11(4). doi: 10.1136/bmjopen-2021-049653
130. Prati G. Mental health and its psychosocial predictors during national quarantine in Italy against the coronavirus disease 2019 (COVID-19). Anxiety, Stress Coping. (2021) 34(2):145–56. doi: 10.1080/10615806.2020.1861253
131. Proto E, Quintana-Domeque C. COVID-19 and mental health deterioration by ethnicity and gender in the UK. PLoS One. (2021) 16(1 January). doi: 10.1371/journal.pone.0244419
132. Racine N, Hetherington E, McArthur BA, McDonald S, Edwards S, Tough S, et al. Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: a longitudinal analysis. Lancet Psychiatry. (2021) 8(5):405–15. doi: 10.1016/S2215-0366(21)00074-2
133. Ribeiro FS, Santos FH, Anunciação L, Barrozo L, Landeira-Fernandez J, Leist AK. Exploring the frequency of anxiety and depression symptoms in a Brazilian sample during the COVID-19 outbreak. Int J Environ Res Public Health. (2021) 18(9). doi: 10.3390/ijerph18094847
134. Rice K, Williams S. Women’s postpartum experiences in Canada during the COVID-19 pandemic: a qualitative study. C Open. (2021) 9(2):556–62. doi: 10.9778/cmajo.20210008
135. Robinson GE, Benders-Hadi N, Conteh N, Brown KM, Grigoriadis S, Nadelson CC, et al. Psychological impact of COVID-19 on pregnancy. J Nerv Ment Dis. (2021) 209:396–7. doi: 10.1097/NMD.0000000000001339
136. Romero-Gonzalez B, Puertas-Gonzalez JA, Mariño-Narvaez C, Peralta-Ramirez MI. Confinement variables by COVID-19 predictors of anxious and depressive symptoms in pregnant women. Med Clin (Barc). (2021) 156(4):172–6. doi: 10.1016/j.medcli.2020.10.002
137. Saadati N, Afshari P, Boostani H, Beheshtinasab M, Abedi P, Maraghi E. Health anxiety and related factors among pregnant women during the COVID-19 pandemic: a cross-sectional study from Iran. BMC Psychiatry. (2021) 21(1). doi: 10.1186/s12888-021-03092-7
138. Şahan E, Ünal SM, Kırpınar İ. Can we predict who will be more anxious and depressed in the COVID-19 ward? J Psychosom Res. (2021) 140. doi: 10.1016/j.jpsychores.2020.110302
139. Sakalidis VS, Rea A, Perrella SL, McEachran J, Collis G, Miraudo J, et al. Wellbeing of breastfeeding women in Australia and New Zealand during the COVID-19 pandemic: a cross-sectional study. Nutrients. (2021) 13(6). doi: 10.3390/nu13061831
140. Özkan Şat S, Yaman Sözbir Ş. Use of mobile applications by pregnant women and levels of pregnancy distress during the COVID-19 (Coronavirus) pandemic. Matern Child Health J. (2021) 25(7):1057–68. doi: 10.1007/s10995-021-03162-y
141. Savolainen I, Oksa R, Savela N, Celuch M, Oksanen A. COVID-19 anxiety-A longitudinal survey study of psychological and situational risks among Finnish workers. Int J Environ Res Public Heal Artic. (2021) 18(2):794. doi: 10.3390/ijerph18020794
142. Seifer DB, Petok WD, Agrawal A, Glenn TL, Bayer AH, Witt BR, et al. Psychological experience and coping strategies of patients in the Northeast US delaying care for infertility during the COVID-19 pandemic. Reprod Biol Endocrinol. (2021) 19:28. doi: 10.1186/s12958-021-00721-4
143. Serafim AP, Durães RSS, Rocca CCA, Gonçalves PD, Saffi F, Cappellozza A, et al. Exploratory study on the psychological impact of COVID-19 on the general Brazilian population. PLoS One. (2021) 16(2 February). doi: 10.1371/journal.pone.0245868
144. Shechory Bitton M, Laufer A. Mental health and coping in the shadow of the COVID-19 pandemic: the Israeli case. Front Public Heal. (2021) 1:568016. doi: 10.3389/fpubh.2020.568016
145. Silva DFO, Cobucci RN, Soares-Rachetti VP, Lima S, Andrade FB. [Prevalence of anxiety among health professionals in times of COVID-19: a systematic review with meta-analysis]. Cien Saude Colet. (2021) 26:693–710. doi: 10.1590/1413-81232021262.38732020
146. Smith RB, Mahnert ND, Foote J, Saunders KT, Mourad J, Huberty J. Mindfulness effects in obstetric and gynecology patients during the coronavirus disease 2019 (COVID-19) pandemic: a randomized controlled trial. Obstet Gynecol. (2021) 137(6). doi: 10.1097/AOG.0000000000004316
147. Souza ASR, Souza GFA, Souza GA, Cordeiro ALN, Praciano GAF, de Souza Alves AC, et al. Factors associated with stress, anxiety, and depression during social distancing in Brazil. Rev Saude Publica. (2021) 55. doi: 10.11606/s1518-8787.2021055003152
148. Suárez-Rico BV, Estrada-Gutierrez G, Sánchez-Martínez M, Perichart-Perera O, Rodríguez-Hernández C, González-Leyva C, et al. Prevalence of depression, anxiety, and perceived stress in postpartum Mexican women during the COVID-19 lockdown. Int J Environ Res Public Health. (2021) 18(9). doi: 10.3390/ijerph18094627
149. Sun F, Zhu J, Tao H, Ma Y, Jin W. A systematic review involving 11,187 participants evaluating the impact of COVID-19 on anxiety and depression in pregnant women. J Psychosom Obstet Gynecol. (2021) 42(2):91–9. doi: 10.1080/0167482X.2020.1857360
150. Talbot J, Charron V, Konkle AT. Feeling the void: lack of support for isolation and sleep difficulties in pregnant women during the COVID-19 pandemic revealed by twitter data analysis. Int J Environ Res Public Health. (2021) 18(2). doi: 10.3390/ijerph18020393
151. Terán-Pérez G, Portillo-Vásquez A, Arana-Lechuga Y, Sánchez-Escandón O, Mercadillo-Caballero R, González-Robles RO, et al. Sleep and mental health disturbances due to social isolation during the COVID-19 pandemic in Mexico. Int J Environ Res Public Health. (2021) 18(6). doi: 10.3390/ijerph18062804
152. Thayer ZM, Gildner TE. COVID-19-related financial stress associated with higher likelihood of depression among pregnant women living in the United States. Am J Hum Biol. (2021) 33(3). doi: 10.1002/ajhb.23508
153. Tomfohr-Madsen LM, Racine N, Giesbrecht GF, Lebel C, Madigan S. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res. (2021) 300. doi: 10.1016/j.psychres.2021.113912
154. Torrente M, Sousa PAC, Sánchez-Ramos A, Pimentao J, Royuela A, Franco F, et al. To burn-out or not to burn-out: a cross-sectional study in healthcare professionals in Spain during COVID-19 pandemic. BMJ Open. (2021) 11(2). doi: 10.1136/bmjopen-2020-044945
155. Vigod SN, Brown HK, Huang A, Fung K, Barker LC, Hussain-Shamsy N, et al. Postpartum mental illness during the COVID-19 pandemic: a population-based, repeated crosssectional study. CMAJ. (2021) 193(23):835–43. doi: 10.1503/cmaj.210151
156. Wang Q, Mo PKH, Song B, Di JL, Zhou FR, Zhao J, et al. Mental health and preventive behaviour of pregnant women in China during the early phase of the COVID-19 period. Infect Dis Poverty. (2021) 10(1). doi: 10.1186/s40249-021-00825-4
157. Wickens CM, Hamilton HA, Elton-Marshall T, Nigatu YT, Jankowicz D, Wells S. Household- and employment-related risk factors for depressive symptoms during the COVID-19 pandemic. Can J Public Heal. (2021) 112:391–9. doi: 10.17269/s41997-020-00472-6
158. Wickens CM, McDonald AJ, Elton-Marshall T, Wells S, Nigatu YT, Jankowicz D, et al. Loneliness in the COVID-19 pandemic: associations with age, gender and their interaction. J Psychiatr Res. (2021) 136:103–8. doi: 10.1016/j.jpsychires.2021.01.047
159. Xie M, Wang X, Zhang J, Wang Y. Alteration in the psychologic status and family environment of pregnant women before and during the COVID-19 pandemic. Int J Gynecol Obstet. (2021) 153(1):71–5. doi: 10.1002/ijgo.13575
160. Xue B, McMunn A. Gender differences in unpaid care work and psychological distress in the UK COVID-19 lockdown. PLoS One. (2021) 16(3 March). doi: 10.1371/journal.pone.0247959
161. Yan S, Xu R, Stratton TD, Kavcic V, Luo D, Hou F, et al. Sex differences and psychological stress: responses to the COVID-19 pandemic in China. BMC Public Health. (2021) 21(1). doi: 10.1186/s12889-020-10085-w
162. Yang X, Song B, Wu A, Mo PKH, Di J, Wang Q, et al. Social, cognitive, and eHealth mechanisms of COVID-19-related lockdown and mandatory quarantine that potentially affect the mental health of pregnant women in China: cross-sectional survey study. J Med Internet Res. (2021) 23. doi: 10.2196/24495
163. Yıldırım M, Geçer E, Akgül Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Psychol Heal Med. (2021) 26(1):35–43. doi: 10.1080/13548506.2020.1776891
164. Yirmiya K, Yakirevich-Amir N, Preis H, Lotan A, Atzil S, Reuveni I. Women’s depressive symptoms during the COVID-19 pandemic: the role of pregnancy. Int J Environ Res Public Health. (2021) 18(8). doi: 10.3390/ijerph18084298
165. Zheng J, Morstead T, Sin N, Klaiber P, Umberson D, Kamble S, et al. Psychological distress in North America during COVID-19: the role of pandemic-related stressors. Soc Sci Med. (2021) 270. doi: 10.1016/j.socscimed.2021.113687
166. Zilver SJM, Broekman BFP, Hendrix YMGA, de Leeuw RA, Mentzel S V, van Pampus MG, et al. Stress, anxiety and depression in 1466 pregnant women during and before the COVID-19 pandemic: a Dutch cohort study. J Psychosom Obstet Gynecol. (2021) 42(2):108–14. doi: 10.1080/0167482X.2021.1907338
167. Wanberg CR, Csillag B, Douglass RP, Zhou L, Pollard MS. Socioeconomic Status and well-being during COVID-19: a resource-based examination. J Appl Psychol. (2020) 105:1382–96. doi: 10.1037/apl0000831 (cited May 8, 2022).
168. Pearlin LI, Bierman A. Current issues and future directions in research into the stress process. Handbooks Sociol Soc Res. (2013):325–40. Available online at:/record/2012-23183-016 (cited May 8, 2022). doi: 10.1007/978-94-007-4276-5_16
169. Drieskens S, Braekman E, Ridder K, Gisle L, Charafeddine R, Hermans L, et al. Domestic violence during the COVID-19 confinement: do victims feel more socially isolated? Arch Public Health. (2022) 80(1):39. doi: 10.1186/s13690-021-00765-3
170. Mittal S, Singh T. Gender-Based violence during COVID-19 pandemic: a Mini-review. Front Glob Womens Health. (2020) 1:4. doi: 10.3389/fgwh.2020.00004
171. Opanasenko A, Lugova H, Mon AA, Ivanko O. Mental health impact of gender-based violence amid COVID-19 pandemic: a review. Bangladesh J Med Sci. (2021) 20(5):17–25. doi: 10.3329/bjms.v20i5.55396
172. McLean CP, Anderson ER. Brave men and timid women? A review of the gender differences in fear and anxiety. Clin Psychol Rev. (2009) 29(6):496–505. doi: 10.1016/j.cpr.2009.05.003
173. Vidas Pretas LF. Processos de Subjetivação e Sofrimento Psíquico: sobre viveres, feminismo, interseccionalidades e mulheres negras. In: de Oliveira MP, Passos RG, editors. Luta antimanicomial e feminismos: discussões de gênero, raça e classe para a reforma psiquiátrica brasileira. Rio de Janeiro: Autografia (2017). p. 70–88.
174. Katz I. O recurso à criança para dizer o indizível. Lacuna uma Rev psicanálise. (2021). (11). Available online at: https://revistalacuna.com/2021/08/26/n-11-05/(cited May 7, 2022).
177. Löwy I. Tangled Diagnoses: Prenatal Testing, Women, and Risk. Chicago/London: University of Chicago Press (2018). p. 319.
178. Petchesky RP. Global Prescriptions: Gendering Health and Human Rights. New York: Zed Books (2003). p. 306.
179. Meherali S, Punjani N, Louie-Poon S, Abdul Rahim K, Das JK, Salam RA, et al. Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int J Environ Res Public Health. (2021) 18(7):3432. doi: 10.3390/ijerph18073432
180. Hawke LD, Monga S, Korczak D, Hayes E, Relihan J, Darnay K, et al. Impacts of the COVID-19 pandemic on youth mental health among youth with physical health challenges. Early Interv Psychiatry. (2021) 15(5):1146–53. doi: 10.1111/eip.13052
181. Spiritus-Beerden E, Verelst A, Devlieger I, Langer Primdahl N, Botelho Guedes F, Chiarenza A, et al. Mental health of refugees and migrants during the COVID-19 pandemic: the role of experienced discrimination and daily stressors. Int J Environ Res Public Health. (2021) 18(12):6354. doi: 10.3390/ijerph18126354
182. Fisher CB, Tao X, Liu T, Giorgi S, Curtis B. COVID-related victimization, racial bias and employment and housing disruption increase mental health risk among U.S. Asian, black and latinx adults. Front Public Health. (2021) 9:772236. doi: 10.3389/fpubh.2021.772236
183. Alarcão V, Virgolino A, Stefanovska-Petkovska M, Neves J. Exploring the effects of the COVID-19 pandemic on mental health and well-being of migrant populations in Europe: an equity-focused scoping review. Behav Sci (Basel). (2022) 12(10):393. doi: 10.3390/bs12100393
185. De Oliveira RD. Elogio da Diferença: O Feminino Emergente. Rio de Janeiro: Rocco Digital (2012).
186. Eidelsztein A, Kushnir CQ. A “responsabilidade subjetiva” em psicanálise. Fractal Rev Psicol. (2021) 33(1):41–6. doi: 10.22409/1984-0292/v33i1/36050
Keywords: mental health, COVID-19, women, review, pandemics
Citation: Arilha M, Carvalho AP, Forster TA, Rodrigues CVM, Briguglio B and Serruya SJ (2024) Women's mental health and COVID-19: increased vulnerability and inequalities. Front. Glob. Womens Health 5:1414355. doi: 10.3389/fgwh.2024.1414355
Received: 8 April 2024; Accepted: 5 September 2024;
Published: 2 October 2024.
Edited by:
Jitender Aneja, All India Institute of Medical Sciences (AIIMS Bathinda), IndiaReviewed by:
Yolanda Contreras-García, University of Concepcion, ChileShahla Eltyeb, Naif Arab University for Security Sciences (NAUSS), Saudi Arabia
Copyright: © 2024 Arilha, Carvalho, Forster, Rodrigues, Briguglio and Serruya. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Margareth Arilha, YXJpbGhhQGhvdG1haWwuY29t
 Margareth Arilha
Margareth Arilha Adriana P. Carvalho
Adriana P. Carvalho Thais A. Forster
Thais A. Forster Carla V. M. Rodrigues4
Carla V. M. Rodrigues4