- Département Biomedical et Santé Publique, Institut de Recherche en Sciences de la Santé (IRSS), Centre National de la Recherche Scientifique et Technologique (CNRST), Ouagadougou, Burkina Faso
Introduction: This study aimed to identify the determinants that influence the use of DMPA-SC/Sayana Press among women who use modern contraceptive methods in Burkina Faso.
Methods: This study used secondary data obtained from the 2021 Burkina Faso Demographic and Health Survey (EDSBF). The dependent variable is the use of DMPA-SC among women aged 15–49 who employ modern contraceptive methods. The descriptive analysis used percentages to describe the study variables. The Pearson chi-square test was used to assess the associations between the explanatory variables and the study variable of interest. Bivariate logistic regression was used to examine the crude odds ratios of each explanatory variable with respect to the dependent variable. The multivariate model was used to determine the net effect of each independent variable on the dependent variable. The significance levels were defined at p < 0.05, with corresponding confidence intervals.
Results: The study revealed significant differences in the use of DMPA-SC according to age, marital status, region of residence, level of education, number of children, and involvement in contraceptive decision-making within the couple. Younger women (aged 15–29 aOR = 2.12, p < 0.001)) and women aged 30–39 (aOR = 1.51, p = 0.02) are also more likely to use DMPA-SC compared to those aged 40–49. Married women or those living with a partner [aOR = 1.93 (1.22, 3.05)] are more likely to use DMPA-SC. Women with 1–3 children are twice as likely to use DMPA-SC as those without children (aOR = 1.97, p = 0.02). Region and Wealth Index were significantly associated with DMPA-SC use. The Boucle du Mouhoun region showed a significantly higher likelihood of DMPA-SC use (aOR = 8.10) and women in the highest wealth group are significantly less likely to use DMPA-SC (aOR = 0.59, p = 0.001).
Conclusion: These results demonstrated the importance of adapting interventions to account for socio-demographic, regional, and cultural differences. This will enable the provision of services to the entire female population in a fair and equitable manner, while also addressing the limitations and enhancing the understanding of the underlying factors influencing the use of DMPA-SC.
1 Introduction
Adopting a modern contraceptive method reduces maternal morbidity and mortality rates (1, 2). Pregnancies that occur too early, too late, too frequently, and too closely spaced are primary causes of direct obstetric complications, which account for over 70% of maternal deaths in low-income countries (3). Consequently, family planning is crucial for reducing fertility rates and maternal mortality by avoiding high-risk pregnancies and decreasing the need for abortions, thereby helping to increase women's life expectancy (4). Central to achieving the 2030 Sustainable Development Goals (SDGs), family planning has major implications in areas such as gender, employment, poverty reduction, and health (5).
Despite these benefits, contraceptives remain underused in many developing regions (6, 7). Typically, women from favourable backgrounds and living conditions exhibit higher contraceptive use, whereas women from impoverished households, who are in greater need of contraceptives, often have limited access to them (4).
The global sexual and reproductive health and rights (SRHR) agenda now prioritizes the right of women to freely choose the number and timing of their children (8). A number of recent initiatives call for the gaps in access to modern contraception to be filled, particularly when women wish to avoid pregnancy but do not have the means or use traditional methods (9). One of the flagship initiatives in this area is Family Planning 2020, a global partnership launched in 2012. It aims to add 120 million new modern contraceptive users in the world's 69 least-developed countries by 2020 (9).
For family planning to be effective, it is essential to ensure continuity in the use of contraception. However, many factors, such as cost, convenience, satisfaction with the method, side effects, partner disagreement, and limited method options, lead many women to abandon contraception, resulting in higher unwanted pregnancies and a higher total fertility rate (10).
Injectable contraceptives, widely used for preventing pregnancy, particularly in sub-Saharan Africa (11–13), represent a major advance. Subcutaneous injectable contraception based on medroxyprogesterone acetate (DMPA-SC) (brand name Sayana® Press) represents a major advance, enabling self-administration and considerably widening access to contraception (14). It is an effective method, rivalling intrauterine devices, implants, and sterilisation. Moreover, the discreet nature of DMPA-SC is crucial, particularly for women living in rural communities who seek confidential family planning (15).
Self-care approaches, such as self-injection of contraceptives, have the potential to revolutionise healthcare systems and contribute to the achievement of universal public health. When integrated into primary healthcare, these self-care practices can significantly impact health and well-being (16). Self-injection of DMPA-SC or other injectable contraceptives could remove barriers and enhance contraception accessibility, facilitating its continued use, particularly for women who have difficulty gaining regular access to health facilities or where the availability of providers is limited (14, 17). Kim et al. found that self-administration of injectable contraceptives improves contraceptive compliance by eliminating the requirement of clinic visits for each injection (18).
Studies conducted in Burkina Faso, Niger, Senegal, and Uganda have demonstrated the favourable reception of DMPA-SC, paving the way for increased access to family planning for women who already use contraceptive methods, as well as new users and young women (16, 19–21). Economic analyses conducted in Senegal and Uganda suggest that self-injection can result in significant savings for women and health systems (16).
With a total fertility rate of 4.4 children per woman (22), Burkina Faso remains one of the countries with the highest fertility rate in the world. Despite an improvement in contraceptive prevalence, rising from 10% in 2010 (23) to 30.1% in 2021 (22), the most recent DHS data reveals that 13% of women still have unmet needs, and total demand for family planning remains low, with only 43% expressing a need for it (34% for birth spacing and 9% for contraception). Numerous barriers hinder the use of contraception, including poor access to services, women's marginalised status, high illiteracy rates among women, the patriarchal structure of society, and opposition from men (24, 25).
Increasing the supply of contraceptive methods through the introduction of DMPA-SC in 2014 and rapidly scaling up within public health facilities was a strategy implemented by the Ministry of Health to reduce barriers to women's access to family planning (26).
Since the introduction of self-administered injectable contraception, which offers the potential to address unmet family planning needs in developing countries, including Burkina Faso, numerous studies have been conducted. However, the main limitation of these studies lies in the use of samples that are not representative of the population of women of childbearing age who use contraceptive methods (27–28). Some studies recruited samples of women from health centres (29–31), which is not necessarily representative of the diversity of women nationwide. Others have used a cohort of women recruited during family planning campaigns organised in specific areas (32). Our study benefits from utilizing data sourced from the Demographic and Health Survey (DHS), ensuring the attainment of a nationally representative sample.
This study aims to understand the determinants that influence the use of DMPA-SC/Sayana Press among women who use modern contraceptive methods in Burkina Faso.
2 Methods
2.1 Study area
Burkina Faso is a landlocked country in the Sahel region, with a total area of approximately 272,969 km2. It shares borders with Mali to the northwest, Niger to the northeast, Benin to the southeast, and Côte d'Ivoire, Ghana, and Togo to the south. Administratively, Burkina Faso is divided into thirteen (13) regions and forty-five (33) provinces, which are, in turn, subdivided into 351 departments and 8,228 villages.
According to the results of the 5th General Census of Population and Housing (RGPH) in 2019, Burkina Faso had a total population of 20,505,155. This population breaks down into 9,900,847 men and 10,604,308 women, equivalent to a sex ratio of 107.1 women for every 100 men (34).
Women of childbearing age, i.e., those aged between 15 and 49, will represent 44.0% of the female population and 22.7% of the total population in 2019. Despite a downward trend in recent years, Burkina Faso has high fertility levels, comparable to other countries in sub-Saharan Africa.
2.2 Data source
This study uses secondary data obtained from the 2021 Burkina Faso Demographic and Health Survey (EDSBF). The survey employed a two-stage stratified sampling technique. In the first stage, clusters/enumeration areas (EAs) were selected from the national sampling frame, derived from the 2019 census. Details of the EDSBF methodology are described in detail in the EDSBF final report (22). The EDSBF sampling process is designed to ensure representativeness at the national level, considering the place of residence (urban, rural) and the regions of Burkina Faso.
The Demographic and Health Survey collects data on various health and social issues, including fertility, mortality, family planning, women's health, children's health, and men's health (35–37). This study focussed on a sample of women aged 15–49 who use modern contraceptive methods.
2.3 Study variables
2.3.1 Dependent variable
The dependent variable was the use of DMPA-SC among women aged 15–49 who use modern contraceptive methods. Users of modern contraceptive methods are defined as women who use pills, intrauterine devices (IUDs), implants, injectable contraceptives, including DMPA/Sayana Press, male or female condoms, emergency contraception, female or male sterilisation, and other modern contraceptive methods. The dependent variable was coded as follows: 1 if the woman used DMPA-SC/Sayana Press, and 0 if she used any other modern contraceptive method.
2.3.2 Independent variables
The explanatory variables used were selected in the light of the literature review (38–43) and include the woman's age, marital status, level of education, occupation, religion, parity, region and area of residence, media exposure, and her husband's level of education. In addition, variables such as discussion within the couple about family planning were considered in the analysis. Wealth quintiles and the question of distance to the health centre were also included in the analyses.
2.4 Data analysis
This study used both descriptive statistics and logistic regression models to analyse the data. The descriptive analysis used percentages to describe the study variables. Pearson's chi-square test was used to assess the associations between the explanatory variables and the study variable of interest. Bivariate logistic regression was used to examine the crude odds ratios of each explanatory variable to the dependent variable. The multivariate model was used to determine the net effect of each independent variable on the dependent variable. Significance levels were defined at p < 0.05, with corresponding confidence intervals. The results were presented in tabular form. Analysis was performed using Stata version 18 software.
2.5 Ethical considerations
This study is based on the analysis of secondary data without the use of any information enabling participants to be identified. The EDS survey was approved by ICF International and by a national ethics committee, and it received all the necessary authorisations to collect household data. All participants gave written informed consent before taking part in the survey. Although no additional ethical approval was required for this study, we obtained written permission from the DHS programme to use the data.
3 Results
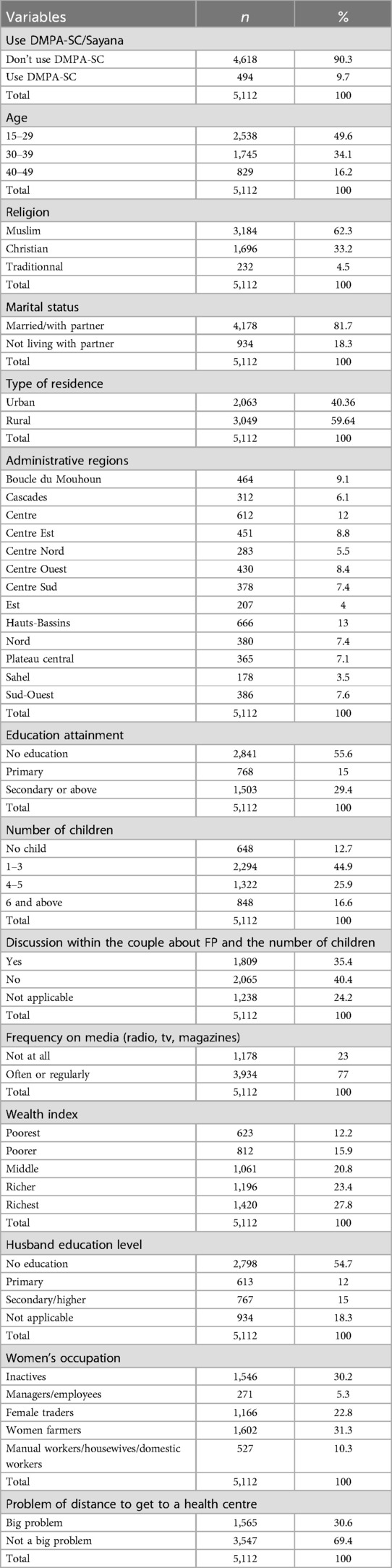
In total, this study used a sample of 5112 women who use modern contraceptive methods. Table 1 presents the characteristics of the women according to the variables used in the study. DMPA-SC was used by 10.1% of women. The majority of the women included were aged between 15 and 29 (49.7%), followed by those aged between 30 and 39 (34.3%) and those aged between 40 and 49 (16.0%) and most women were Muslim (62.8%). The breakdown by marital status shows that a large proportion of women were married or living with a partner (82.2%), while 17.8% were not living with a partner.
More than half of the women have no formal education (56.5%). Most women have between 1 and 3 children (45.0%), while 13.1% have no children yet. A significant proportion of women (40.2%) do not discuss family planning with their partner. The women have a variety of occupations, with a high proportion of farmers (30.6%) and shopkeepers (21.6%). For some women, the distance to a health centre is a significant problem (31.5%), which may have an impact on their ability to obtain contraceptive services.
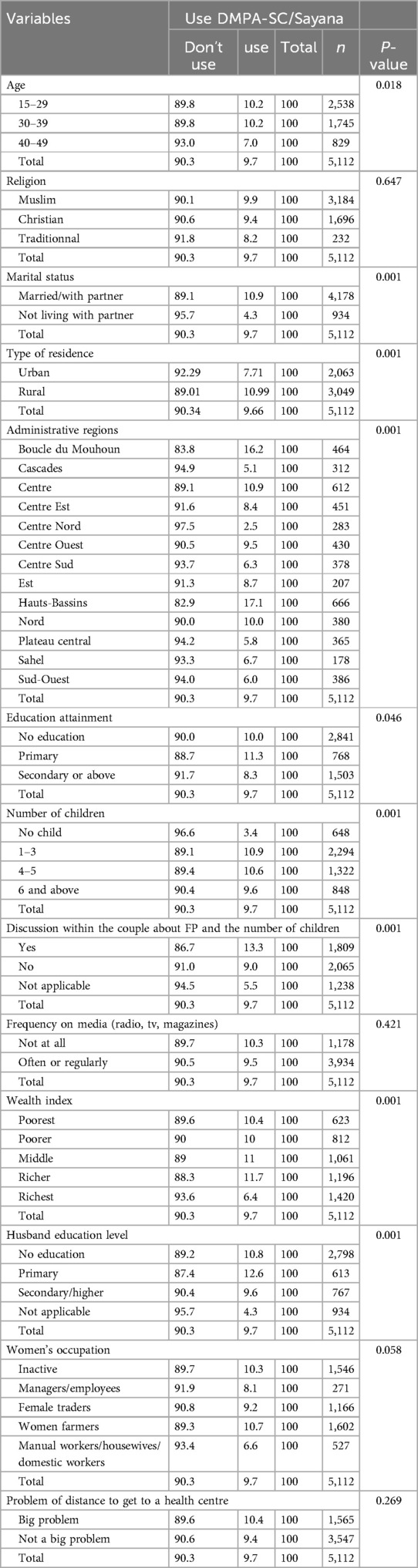
Table 2 examines the associations between different explanatory variables and using DMPA-SC (Subcutaneous Depot of Medroxyprogesterone Acetate) in Burkina Faso. The results indicate significant associations with several demographic, socio-economic, and behavioural factors.
Table 2 examines the associations between different explanatory variables and the use of DMPA-SC (Subcutaneous Medroxyprogesterone Acetate Depot) in Burkina Faso. The results show significant associations with several demographic, socio-economic and behavioural factors.
The difference in DMPA-SC use between age groups was statistically significant (p = 0.018). The proportion of DMPA-SC users was higher among women aged 15–29 (10.2%) and 30–39 (10.2%) than among women aged 40–49 (7.0%). Marital status was associated with DMPA-SC use (p = 0.001). Women who were married or living with a partner (10.9%) had a significantly higher rate of use than those not living with a partner (4.3%).
There were also significant variations in the use of DMPA-SC according to administrative region (p = 0.001) and place of residence. The results show geographical disparities, with higher rates of use in some regions than in others. Women's level of education was another factor associated with the use of DMPA-SC (p = 0.046). The results show that women with secondary or higher education have a lower rate of use than those with no education or primary education (p = 0.046). The number of children already born was significantly associated with the use of DMPA-SC (p = 0.000). Women without children or with a higher number of children had a lower rate of DMPA-SC use. Women who discuss family planning within the couple are more likely to use DMPA-SC (p = 0.001). Wealth was significantly associated with DMPA-SC use (p = 0.001). The spouse's level of education was significantly associated with the use of DMPA-SC (p = 0.001).
Religion, place of residence, frequency of listening to the media, occupation of the woman, and the problem of distance to the health centre were not significantly associated with the use of DMPA.
Table 3 presents the results of the multivariate logistic regression analysis. The results of the logistic regression present the adjusted odds ratios (aOR) and 95% confidence intervals (95% CI) for different explanatory variables concerning the use of DMPA-SC. The age of the woman was significantly associated with the use of DMPA-SC. Women aged between 15 and 29 were twice as likely to use DMPA-SC as those between 40 and 49 (aOR = 2.12, p = 0.000). Women aged 30 to 39 were also more likely to use DMPA-SC than the reference group (aOR = 1.51, p = 0.02).
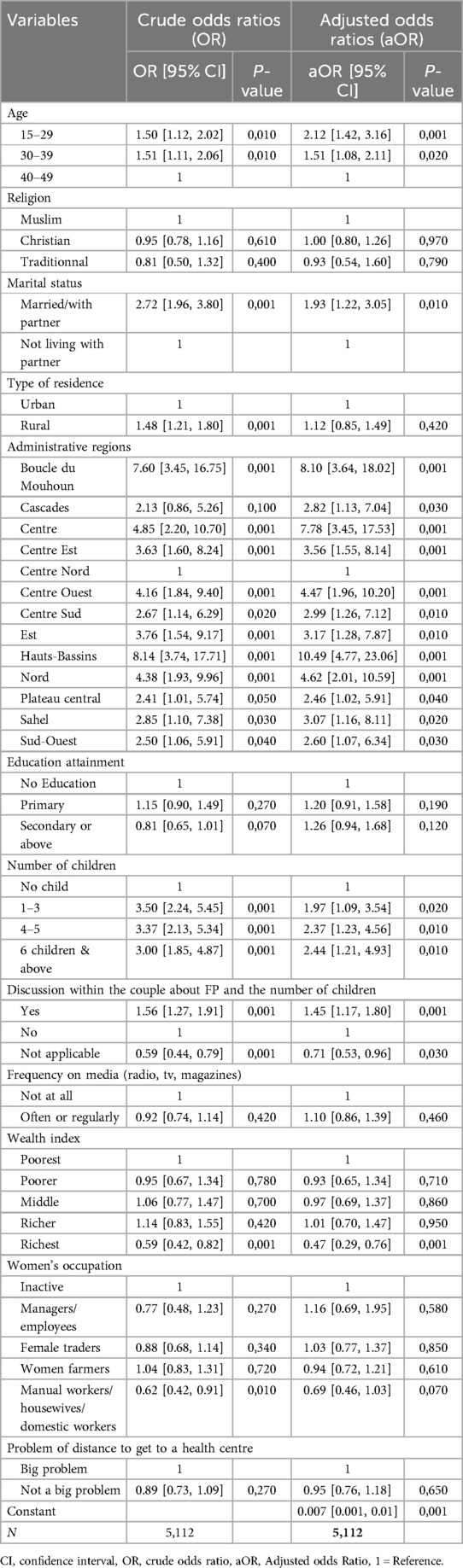
Table 3. Results of multivariate analysis of DMPA-SC use and explanatory variables among women using modern contraceptive methods in Burkina Faso.
Several regions showed a strong association with the use of DMPA-SC. For example, the Boucle du Mouhoun region had a high aOR of 8.10, which means that women in this region are significantly more likely to use DMPA-SC. Married women or those living with a partner [aOR = 1.93 (1.22, 3.05)] are more likely to use DMPA-SC. Women's level of education showed no significant association with the use of DMPA-SC.
Concerning the number of children the woman has, women with 1–3 children are approximately twice as likely to use DMPA-SC compared with those without children (aOR = 1.97, p = 0.02). Similarly, women with 4 to 5 children or 6 or more children were also significantly more likely to use DMPA-SC.
Women who discussed family planning within the couple were 1.45 times more likely to use DMPA-SC (aOR = 1.45, p = 0.001). Women for whom this discussion was not applicable were less likely to use it. The results show that women in the highest wealth group are significantly less likely to use DMPA-SC (aOR = 0.59, p = 0.001).
Women's occupations and problem of distance to get to a health centre showed no significant association with the use of DMPA-SC among women.
4 Discussion
This study aimed to understand the determinants influencing the use of DMPA-SC/Sayana Press among women who use modern contraceptive methods in Burkina Faso. The results show several significant associations between different explanatory variables and DMPA-SC use. These results provide crucial information to guide public health policies and awareness programmes aimed at improving access to this contraceptive method and promoting family planning in the country.
The studies showed that DMPA-SC users were more numerous among women aged 15–29 and those aged 30–39 than among women aged 40 and over. This result appears to be consistent with findings elsewhere. In a study in Uganda, Corneliess et al. found that, compared with adult women, adolescents were more likely to use a modern contraceptive method for the first time when they opted for self-injection (44). Also, in Uganda and the DRC, results showed that young women (15–19 years) were more likely to use DMPA-SC compared to those aged 45–49 years, which could result from DMPA-SC programmes targeting younger women in these contexts (33). Also, many current DMPA-SC users are first-time contraceptive users, suggesting that DMPA-SC is reaching new populations and potentially increasing the overall prevalence of modern contraceptives in some settings (33, 45). In addition, the fact that self-infection allows great discretion and fewer visits to health centres makes DMPA-SC an attractive method for young women and married and unmarried teenagers, particularly those in need of secret contraception (46). In addition, community distribution of DMPA-SC appears to be an effective service delivery model for hard-to-reach populations, those most at risk of unmet need for FP, and key populations such as young people and unmarried users (47) and aids in decreasing the discontinuation and abandonment of contraception usage (19, 48, 49).
Our results also showed that marital status is significantly associated with the use of DMPA-SC. Married women were more likely to use the Sayana press than women who were not in a union. This result is also consistent with previous research. In a study conducted in Burkina Faso, the Democratic Republic of Congo, and Uganda, the results showed that never-married women were more likely to use male condoms than DMPA-SC, which is consistent with research conducted elsewhere showing that never-married women were less likely to use DMPA-SC than all other modern methods combined. This may be because condoms are not generally used in marriage in sub-Saharan Africa (33).
The region of residence and the number of children per woman also play a role in the use of the DMPA-SC. Use of the DMPA-SC varies considerably from one region to another, with women living in the Hauts-Bassins, Boucle du Mouhoun, Centre, Centre West, and North being more likely to use the DMPA-SC than those living in other regions of the country. This variation between regions could be linked to the strategy for moving to the DMPA-SC in the health districts at the national level. Indeed, prior to the scale-up, the DMPA-SC was only available in four pilot health districts in Burkina Faso before being gradually extended to all health districts nationwide (26). Furthermore, Anglewicz et al., in their study, found that stocks of DMPA-SC varied according to context, with more regular stocks in private establishments in the DRC and public establishments in Burkina Faso and Nigeria (45). Also, persistent stock-outs and limited method options can disrupt contraceptive use and increase discontinuation (45).
This study emphasised the significance of parity (number of children per woman) in the use of DMPA-SC. Women with children were more likely to choose DMPA-SC than those without children. This result is consistent with the findings of Anglewicz et al. in both Uganda and the DRC, who found that women with two or more children (compared with no children or a single birth) were more likely to choose implants over DMPA-SC in both Uganda and the DRC (33).
The main strength of this study lies in its use of nationally representative data. However, several limitations were also identified. The cross-sectional nature of the study design prevents us from establishing a causal link between variables. In addition, the use of secondary data limited the integration of other determinants, such as quality of care, including advice on side effects, accessibility of services, and cultural factors, which were not considered in the models.
The results of the study serve as a starting point for further debate. In light of the results of this study, there are many crucial policy implications for improving access to and use of modern contraceptive methods in Burkina Faso. Policies should aim to increase education and awareness of contraceptive methods, with a focus on demographic groups least likely to use DMPA-SC, such as women aged 40–49. Specific information campaigns need to be developed for these groups. Also, the geographical disparities observed in the use of DMPA-SC require interventions to ensure equitable access to family planning services in all regions of the country. This could involve expanding services in regions where their use is less widespread.
5 Conclusion
Research into the use of DMPA-SC among women who use modern contraceptive methods in Burkina Faso has produced significant and informative results. The study, based on a representative sample of 5,112 women, revealed striking associations between several socio-demographic and behavioural variables and the use of this contraceptive method. The results of the study highlight significant differences in the use of DMPA-SC according to age, marital status, region of residence, level of education, number of children, and contraceptive discussion within the couple. Younger women are more likely to use DMPA-SC, as are those who are married or living with a partner. Geographical disparities and differences in the number of children a woman has are also significant factors in contraceptive use.
These results underline the need to adapt interventions to take account of socio-demographic, regional, and cultural differences to ensure an adapted and equitable service offer for the entire female population while addressing limitations and deepening understanding of the underlying determinants of DMPA-SC use. It is crucial to expand the distribution and enhance the accessibility of DMPA-SC to guarantee equal access to this family planning method in all regions. Additionally, we suggest intensifying awareness campaigns regarding this method, which would facilitate outreach to and enable marginalised women (rural, poor economic and social conditions) and young women to conveniently obtain DMPA-SC.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: http://dhsprogram.com/data/available-datasets.cfm.
Author contributions
AB: Conceptualization, Formal Analysis, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kamissoko A. Etude des facteurs limitant l’utilisation de la contraception moderne dans l’aire de santé de Badinko, district sanitaire de Kita. (2017). Available online at: https://bibliosante.ml/handle/123456789/6127 (Accessed December 13, 2023).
2. Maïga A, Hounton S, Amouzou A, Akinyemi A, Shiferaw S, Baya B, et al. Trends and patterns of modern contraceptive use and relationships with high-risk births and child mortality in Burkina Faso. Glob Health Action. (2015) 8:29736. doi: 10.3402/gha.v8.29736
3. Ntambue AM, Tshiala RN, Malonga FK, Ilunga TM, Kamonayi JM, Kazadi ST, et al. Utilisation des méthodes contraceptives modernes en république démocratique du Congo: prévalence et barrières dans la zone de santé de Dibindi à mbuji-Mayi. Pan Afr Med J. (2017) 26:1–8. doi: 10.11604/pamj.2017.26.199.10897
4. Ndayizigiye M, Fawzi MCS, Lively CT, Ware NC. Understanding low uptake of contraceptives in resource-limited settings: a mixed-methods study in rural Burundi. BMC Health Serv Res. (2017) 17:209. doi: 10.1186/s12913-017-2144-0
5. Duminy J, Cleland J, Harpham T, Montgomery MR, Parnell S, Speizer IS. Urban family planning in low-and middle-income countries: a critical scoping review. Frontiers in Global Women’s Health. (2021) 2:749636. doi: 10.3389/fgwh.2021.749636
6. Moreira LR, Ewerling F, Barros AJD, Silveira MF. Reasons for nonuse of contraceptive methods by women with demand for contraception not satisfied: an assessment of low and middle-income countries using demographic and health surveys. Reprod Health. (2019) 16:148. doi: 10.1186/s12978-019-0805-7
7. Bellizzi S, Pichierri G, Menchini L, Barry J, Sotgiu G, Bassat Q. The impact of underuse of modern methods of contraception among adolescents with unintended pregnancies in 12 low-and middle-income countries. J Glob Health. (2019) 9(2):020429. doi: 10.7189/jogh.09.020429
8. Utami DA, Samosir OB. Women’s empowerment and unmet needs for family planning in Indonesia. IOP Conference Series: Earth and Environmental Science. IOP Publishing (2021). p. 012057. Available online at: https://iopscience.iop.org/article/10.1088/1755-1315/716/1/012057/meta (Accessed December 13, 2023).
9. Sedgh G, Ashford LS, Hussain R. Unmet need for contraception in developing countries: examining women’s reasons for not using a method. (2016) Available online at: https://www.guttmacher.org/report/unmet-need-for-contraception-in-developing-countries?utm_source=Master+List&utm_campaign=037b9b172b-NR_Intl_Unmet_Need_6_28_16&utm_medium=email&utm_term=0_9ac83dc920-037b9b172b-244275881 (Accessed December 13, 2023).
10. Liu J, Shen J, Diamond-Smith N. Predictors of DMPA-SC continuation among urban Nigerian women: the influence of counseling quality and side effects. Contraception. (2018) 98:430–7. doi: 10.1016/j.contraception.2018.04.015
11. Cover J, Ba M, Drake JK, NDiaye MD. Continuation of self-injected versus provider-administered contraception in Senegal: a nonrandomized, prospective cohort study. Contraception. (2019) 99:137–41. doi: 10.1016/j.contraception.2018.11.001
12. Ayuk BE, Yankam BM, Saah FI, Bain LE. Provision of injectable contraceptives by community health workers in sub-Saharan Africa: a systematic review of safety, acceptability and effectiveness. Hum Resour Health. (2022) 20:66. doi: 10.1186/s12960-022-00763-8
13. Burke HM, Chen M, Buluzi M, Fuchs R, Wevill S, Venkatasubramanian L, et al. Effect of self-administration versus provider-administered injection of subcutaneous depot medroxyprogesterone acetate on continuation rates in Malawi: a randomised controlled trial. Lancet Glob Health. (2018) 6:e568–78. doi: 10.1016/S2214-109X(18)30061-5
14. Kennedy CE, Yeh PT, Gaffield ML, Brady M, Narasimhan M. Self-administration of injectable contraception: a systematic review and meta-analysis. BMJ Global Health. (2019) 4:e001350. doi: 10.1136/bmjgh-2018-001350
15. Prata N, Weidert K, Fraser A, Gessessew A. Meeting rural demand: a case for combining community-based distribution and social marketing of injectable contraceptives in tigray, Ethiopia. PLoS One. (2013) 8:e68794. doi: 10.1371/journal.pone.0068794
16. Brady M, Drake JK, Namagembe A, Cover J. Self-care provision of contraception: evidence and insights from contraceptive injectable self-administration. Best Pract Res Clin Obstet Gynaecol. (2020) 66:95–106. doi: 10.1016/j.bpobgyn.2020.01.003
17. Cover J, Blanton E, Ndiaye D, Walugembe F, LaMontagne DS. Operational assessments of sayana® press provision in Senegal and Uganda. Contraception. (2014) 89:374–8. doi: 10.1016/j.contraception.2014.01.005
18. Kim C, Fønhus M, Ganatra B. Self-administration of injectable contraceptives: a systematic review. BJOG. (2017) 124:200–8. doi: 10.1111/1471-0528.14248
19. Cover J, Namagembe A, Tumusiime J, Nsangi D, Lim J, Nakiganda-Busiku D. Continuation of injectable contraception when self-injected vs. Administered by a facility-based health worker: a nonrandomized, prospective cohort study in Uganda. Contraception. (2018) 98:383–8. doi: 10.1016/j.contraception.2018.03.032
20. Spieler J. Sayana® Press: can it be a “game changer” for reducing unmet need for family planning? Contraception. (2014) 89:335–8. doi: 10.1016/j.contraception.2014.02.010
21. Cover J, Namagembe A, Tumusiime J, Lim J, Drake JK, Mbonye AK. A prospective cohort study of the feasibility and acceptability of depot medroxyprogesterone acetate administered subcutaneously through self-injection. Contraception. (2017) 95:306–11. doi: 10.1016/j.contraception.2016.10.007
22. INSD, ICF. Enquête Démographique et de Santé du Burkina Faso 2021. Rockville, Maryland, USA: Ouagadougou, Burkina Faso et (2022). Available online at: https://dhsprogram.com/pubs/pdf/PR139/PR139.pdf
23. INSD, ICF. Enquête Démographique et de Santé et à Indicateurs Multiples du Burkina Faso 2010. Calverton, Maryland, USA: INSD et ICF International (2012). Available online at: https://dhsprogram.com/pubs/pdf/fr256/fr256.pdf
24. Bado AR, Badolo H, Zoma LR. Use of modern contraceptive methods in Burkina Faso: what are the obstacles to male involvement in improving indicators in the Centre-East and Centre-North Regions? OAJC. (2020) 11:147–56. doi: 10.2147/OAJC.S274570
25. Barro A, Bado AR. Religious Leaders’ knowledge of family planning and modern contraceptive use and their involvement in family planning programmes in Burkina Faso: a qualitative study in dori in the sahel region. OAJC. (2021) 12:123–32. doi: 10.2147/OAJC.S315395
26. Ministère de la Santé-Burkina Faso. Plan National de Planification Familiale 2021-2025 du Burkina Faso. (2022). Available online at: http://www.healthpolicyplus.com/ns/pubs/18628-19085_BFPNPF.pdf
27. Sherpa LY, Tinkari BS, Gentle P, Sah RK, Shrestha A, Sahani SK, et al. A prospective cohort study to assess the acceptability of Sayana Press among 18–49-year-old women in Nepal. Contraception. (2021) 104:623–7. doi: 10.1016/j.contraception.2021.07.009
28. Osinowo K, Ojomo O, Ibitoye S, Oluwayemi P, Rufus F. Self-injected Depot–Medroxyprogesterone Acetate Subcutaneous (DMPA-SC) Uptake in Nigeria: A Paradigm Shift. Available online at: https://arfh-ng.org/wp-content/uploads/2021/08/Self_injected_Depot_Medroxyprogesterone.pdf (Accessed February 12, 2024).
29. Liu J, Shen J, Schatzkin E, Adedeji O, Kongnyuy E, Onuoha C, et al. Accessing DMPA-SC through the public and private sectors in Nigeria: users’ characteristics and their experiences. Gates Open Res. (2019) 2:73. doi: 10.12688/gatesopenres.12890.2
30. Osinowo K, Fintirimam S-D, Ojomo O, Ladipo O, Ojo P, Majiyagbe T, et al. Knowledge, perception, and practice of DMPA-SC/self-injectable contraceptive among women: findings from mixed-method study in South-West and North-Central, Nigeria. Communities. (2022) 7:8. Available online at: https://www.texilajournal.com/thumbs/article/Public_Health_Vol9_Issue3_Article_7.pdf (Accessed February 12, 2024).
31. Diamond-Smith N, Treleaven E, Omoluabi E, Liu J. Comparing simulated client experiences with phone survey self-reports for measuring quality of information given in family planning counseling: The case of depot medroxyprogesterone acetate – subcutaneous (DMPA-SC) in Nigeria [version 2; peer review: 1 approved, 1 approved with reservations]. Gates Open Res. (2019) 3:1092. doi: 10.12688/gatesopenres.12935.2
32. Osinowo K, Ekholuenetale M, Ojomo O, Hassan A, Ladipo OA. Patterns of triggers, ideation and motivational factors of contraceptive utilization among women and gate-keepers in Nigeria: a scoping study on the resilient and accelerated scale up of DMPA-SC in Nigeria (RASUDIN). Contracept Reprod Med. (2020) 5:38. doi: 10.1186/s40834-020-00141-6
33. Anglewicz P, Larson E, Akilimali P, Guiella G, Kayembe P, Kibira SP, et al. Characteristics associated with use of subcutaneous depot medroxyprogesterone acetate (DMPA-SC) in Burkina Faso, democratic Republic of Congo, and Uganda. Contraception: X. (2021) 3:100055. doi: 10.1016/j.conx.2021.100055
34. INSD. Cinquième Recensement Général de la Population et de l’Habitation du Burkina Faso. (2022). Available online at: https://www.insd.bf/fr/file-download/download/public/2071 (Accessed December 13, 2023).
35. Boerma JT, Sommerfelt AE. Demographic and health surveys (DHS: contributions and limitations. World Health Statistics Quarterly. (1993) 46(4):222–6. Available online at: https://apps.who.int/iris/bitstream/handle/10665/51969/WHSQ_1993_46_4_p222-226_eng.pdf (Accessed December 13, 2023).
36. Courtney K A, Fleuret J, Ahmed J. Data Quality in Demographic and Health Surveys That Used Long and Short Questionnaires. [DHS Methodological Reports]. Rockville, Maryland, USA: ICF (2020). Available online at: https://dhsprogram.com/pubs/pdf/AB17/MR30.pdf (Accessed January 2, 2024).
37. Pullum T, Staveteig S. An Assessment of the Quality and Consistency of Age and Date Reporting in DHS Surveys, 2000-2015. [DHS Methodological Reports]. Rockville, Maryland, USA: ICF (2017). Available online at: https://www.dhsprogram.com/pubs/pdf/MR19/MR19.pdf (Accessed January 2, 2024).
38. Meselu W, Habtamu A, Woyraw W, Tsegaye TB. Trends and predictors of modern contraceptive use among married women: analysis of 2000–2016 Ethiopian demographic and health surveys. Public Health Pract. (2022) 3:100243. doi: 10.1016/j.puhip.2022.100243
39. Noormal AS, Winkler V, Eshraqi AM, Deckert A, Sadaat I, Dambach P. Factors influencing the uptake of short-term contraceptives among women in Afghanistan. Sci Rep. (2022) 12:6632. doi: 10.1038/s41598-022-10535-y
40. Palamuleni ME. Determinants of high marital fertility in Malawi: evidence from 2010 to 2015–16 Malawi demographic and health surveys. Open Public Health J. (2023) 16. doi: 10.2174/18749445-v16-e230419-2022-150
41. Worku AG, Tessema GA, Zeleke AA. DHS WORKING PAPERS. (2014). p. 1–31. Available online at: https://dhsprogram.com/publications/pdf/WP103/WP103.pdf (Accessed December 17, 2023).
42. Digitale J, Psaki S, Soler-Hampejsek E, Mensch BS. Correlates of contraceptive use and health facility choice among young women in Malawi. Ann Am Acad Pol Soc Sci. (2017) 669:93–124. doi: 10.1177/0002716216678591
43. Chintsanya J. Trends and correlates of contraceptive use among married women in Malawi: evidence from 2000 to 2010 Malawi demographic and health surveys. Calverton, Maryland: ICF International (2013). Available online at: https://dhsprogram.com/pubs/pdf/WP87/WP87.pdf (Accessed December 13, 2023).
44. Corneliess C, Cover J, Secor A, Namagembe A, Walugembe F. Adolescent and youth experiences with contraceptive self-injection in Uganda: results from the Uganda self-injection best practices project. J Adolesc Health. (2023) 72:80–7. doi: 10.1016/j.jadohealth.2022.08.010
45. Magalona S, Wood SN, Makumbi F, OlaOlorun FM, Omoluabi E, Pierre AZ, et al. DMPA-SC stock: cross-site trends by facility type. Contraception: X. (2022) 4:100075. doi: 10.1016/j.conx.2022.100075
46. Ali G, Porter Erlank C, Birhanu F, Stanley M, Chirwa J, Kachale F, et al. Perspectives on DMPA-SC for self-injection among adolescents with unmet need for contraception in Malawi. Front Glob Womens Health. (2023) 4:1059408. doi: 10.3389/fgwh.2023.1059408
47. Osinowo K, Sambo-Donga F, Ojomo O, Ibitoye SE, Oluwayemi P, Okunfulure M, et al. Resilient and accelerated scale-up of subcutaneously administered depot–medroxyprogesterone acetate in Nigeria (RASuDiN): a mid-line study in COVID-19 era. OAJC. (2021) 12:187–99. doi: 10.2147/OAJC.S326106
48. Ali MM, Cleland JG, Shah IH. Causes and consequences of contraceptive discontinuation: evidence from 60 demographic and health surveys. Geneva, Switzerland: World Health Organization (2012). Available online at: https://apps.who.int/iris/bitstream/handle/10665/75429/?sequence=1 (Accessed December 13, 2023).
Keywords: determinants, DMPA-SC, contraception, DHS, Burkina Faso
Citation: Bado AR (2024) Determinants of DMPA-SC self-care/self-injectable contraceptive uptake among modern contraceptive users in Burkina Faso: findings from the 2021 demographic and health survey. Front. Glob. Womens Health 5:1385446. doi: 10.3389/fgwh.2024.1385446
Received: 12 February 2024; Accepted: 13 August 2024;
Published: 5 September 2024.
Edited by:
Allen Kabagenyi, Makerere University, UgandaReviewed by:
Olufemi Adetutu, Obafemi Awolowo University, NigeriaMuswamba Mwamba, Stephen F. Austin State University, United States
Copyright: © 2024 Bado. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aristide Romaric Bado, YXJiYWRvQGdtYWlsLmNvbQ==
 Aristide Romaric Bado
Aristide Romaric Bado