- 1School of Nursing and Midwifery, University of Rwanda, Kigali, Rwanda
- 2Department de Recherche, Enseignement et Formation, Maison Medicale Jeanne Garnier, Paris, France
- 3Ndera Neuro-Psychiatric Hospital, Kigali, Rwanda
Introduction: Family planning knowledge and access to quality family planning services occupy a central position in the lives of all women of reproductive age. However, women with mental illness and epilepsy who are at a high risk of sexual violence, unwanted pregnancies, poor obstetric outcomes, and drug interaction consequences, need it the most. Understanding their family planning knowledge and utilization remains crucial for meeting their needs. The present study aims to assess knowledge, use of family planning, and associated factors among women living with mental illness and epilepsy who attend the Ndera Neuropsychiatric Hospital and affiliated branches.
Methodology: A cross-sectional study was conducted between October 2022 and February 2023. The study involved a purposive sample of 289 women who attended the Ndera Neuropsychiatric Hospital and its two affiliated branches during the data collection period. Psychiatric nurses administered a structured questionnaire. Data were analyzed using descriptive statistics, and multiple logistic regression analysis was performed to assess the factors associated with the use of family planning methods.
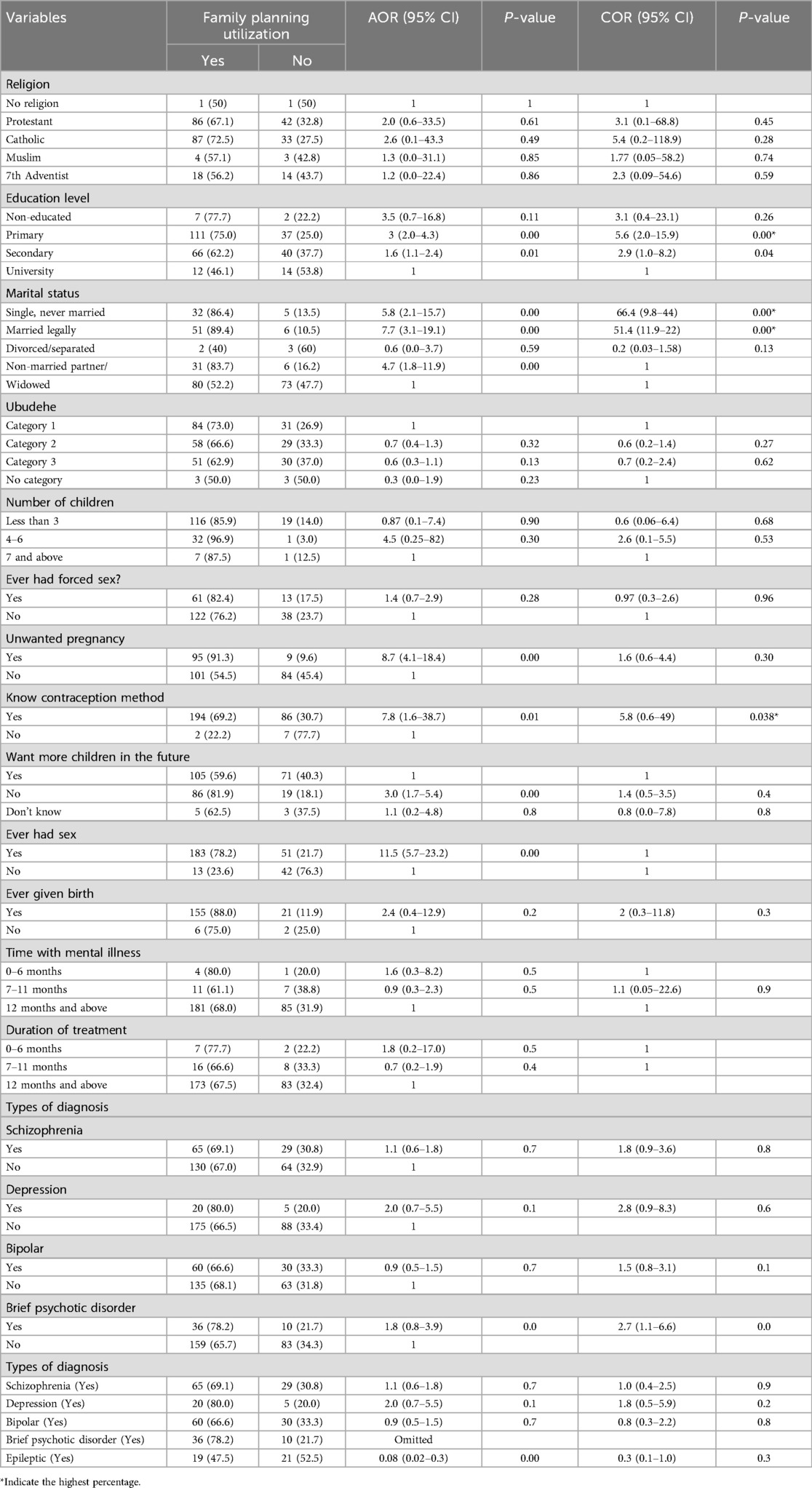
Results: Out of 289 who participated in the study, the majority (96.9%) were aware of family planning methods, most (67.8%) had used one method once in their life course, a half (51.9%) were using a family planning method at the time of data collection, and a slight number (26%) expressed intentions of using a family planning method in the future. The most known and used methods were respectively the injectable (17.5%) and oral contraceptive pill (17.5%). Regarding the natural family planning methods, breastfeeding and withdrawal were less used. Being single (AOR = 66.4, 95% CI: 9.8, 44) or married (AOR = 51.4, 95% CI: 11.9–22), having a primary level of education (AOR = 5.6, 95% CI: 2.0, 15.9), knowing a contraceptive method (AOR = 5.8, 95% CI: 0.6, 49) and suffering from brief psychotic disorders (AOR = 2.7, 95% CI: 1.1, 6.6) predicted a higher utilization of family planning.
Conclusion: Most of the women with mental illness in this study were aware of family planning methods and had used one of the family planning methods in life. The national average is below when it comes to family planning awareness. It is important to improve family planning education and counseling for women who attend psychiatric outpatient clinics.
1 Introduction
The World Health Organization strives to include people with mental illnesses in society (1). Motherhood and other reproductive health-related issues require specific attention among women with mental illness. Family planning is important for all women of reproductive age, but women with mental diseases, such as schizophrenia, bipolar disorder, and severe depression, may face additional problems and concerns (2). Family planning (FP) is particularly important for women with mental illness since they carry a high risk of sexual violence, unwanted pregnancies, and poor obstetric outcomes due to their mental illness (3). A retrospective study from the Epilepsy Birth Control Registry web-based survey of women with epilepsy (WWE) reported that 65% of pregnancies in women with epilepsy were unplanned, more common among younger, and 34.7% of unintended pregnancies occurred in women with epilepsy who were not taking contraceptives (4). Nevertheless, a study conducted in Japan found that WWE with planned pregnancies were less likely to have seizures during pregnancy and less likely to undergo medication changes (5). It is, therefore, very crucial for women with epilepsy to have access to reproductive health services including FP methods to lower the risks that may be associated with maternal epilepsy.
Despite the increased sexual and reproductive health risks associated with mental illness and epilepsy, access to, and utilization of FP by women with mental health and epilepsy remains low globally, particularly within resources-limited countries (3). Factors previously reported to affect the use of family planning included the influence of severe mental health illness symptoms, knowledge and attitudes regarding family planning, stigma, reproductive coercion, and sexual violence (6). Additionally, compared to other women without mental health conditions, those with mental illness and epilepsy demonstrated a lack of awareness, less reproductive and contraceptive knowledge, and less use of birth control methods with no mental illness history (3, 7, 8).
In Rwanda, the recent mental health survey involving the general population revealed that females are more affected by mental illness compared to males, with a proportion of 23.2% and 16.6% respectively (9). Researchers investigated mental-health-seeking behaviors in Rwandan men and women and its social and gender implications. It was found that both men and women with mental health issues were unable to fully benefit from mental health services available due to the considerable influence of stigma and persisting traditional roles in some mental healthcare settings (10). Similarly, lack of FP awareness and cultural misbelieves about FP are among the factors that hinder FP utilization in the general population (11). It is hypothetical whether women with mental health illnesses seek reproductive health services, specifically family planning, and little is known about factors that might hinder or support their FP-seeking behaviors.
Mental health services in Rwanda are provided through community, district, and referral hospital levels. One of the referral hospitals providing mental health and neurological services is the Ndera Neuropsychiatric Hospital, with two affiliated branches. Rwanda Health Sector report confirmed that 73,675 mental health cases were followed up by Caraes Ndera hospital and its branches, of which 69.831% were treated at CARAES Ndera, 20.661% at CARAES Butare, and 9.507% at Centre Icyizere Kicukiro (12). To the authors' knowledge, no family planning services are provided in these settings, and little is known about the knowledge and utilization of FP methods among women consulting these centers. This study aimed to assess the knowledge, utilization, and factors that might influence the use of FP by women with mental illness and epilepsy in Rwanda.
2 Methods
2.1 Research design and setting
A cross-sectional descriptive study was done to explore the FP knowledge, use, and associated factors among women with mental illness and epilepsy in Rwanda. The study site was the Ndera Neuropsychiatric Hospital and its branches. The hospital is a referral neuropsychiatric hospital located in Kigali and provides multidisciplinary inpatient and outpatient mental health and neurological services. It has two affiliated branches, one located in Southern Province, Huye District, known as CARAES-Butare, and another one located in Kigali City, Kicukiro District, known as Icyizere. Both branches provide mental health services.
2.2 Study population
The study included all women of reproductive age, who are living with mental illness and epilepsy with a stable mental health status and recommended by the physicians in charge who have been following them for at least 6 months.
2.3 Sample size
G*Power software as a free power analysis program for a variety of statistical tests commonly used in the social, behavioral, and biomedical sciences (13) was used to determine the sample size. With an effect size of 0.05, α error probability = and 0.05, Power (1-β error probability) = 0.95, the approximated sample size calculated was 396 women attending the Ndera Neuropsychiatric Hospital and its branches. Although, the study collected data from 289 women who attended those facilities during the period of data collection.
2.4 Sampling procedure
All women of reproductive age (15–49) who have an individual history of mental illness or epilepsy, who had a stable mental health status, and who attended the three centers during the study period were eligible to participate in the study.
Through a purposive sample procedure, we selected women whose current stable mental health status was confirmed by their attending physician and were scheduled to be discharged from Ndera Hospital, CARAES Butare, and Icyizere centers, and those who were visiting the outpatient services of these settings as follow-up visits after discharge between October 2022 and February 2023.
Women whose mental status was judged not compatible with their participation in a study were excluded. This age category was based on the recommended WHO reproductive age limit, as well as the Rwanda DHS (14). These criteria were set to ensure that the mental status of potential participants is stabilized enough to allow them to articulate more coherently.
2.5 Data collection methods
A structured questionnaire developed by Prachi et al. for assessing knowledge, attitude, and practice of family planning among the women of reproductive age group was adopted and adopted in the context of the study (15). The questionnaire included the following sections: socio-demographic characteristics, clinical mental health characteristics of the participants, reproductive characteristics of the respondents, fertility intentions, family planning awareness and methods used, self-reported source of information about contraception, and factors associated with family planning utilization. The questionnaire was translated into the local language “Kinyarwanda” spoken by participants and back-translated to English. The questionnaire was administered by experienced psychiatric nurses working at Ndera Neuropsychiatric Hospital, Caraes Butare, and Icyizere Centre, it was therefore not required of participants to have the ability to read or write. The participants responded to the questionnaire after receiving the required services during their follow-up visit.
2.6 Data analysis
The collected data were analyzed using SPSS version 26 software. Descriptive statistics were employed to quantify and summarize data for socio-demographics and knowledge, and bivariate and multivariate analysis were used to assess the factors associated with the use of family planning methods.
2.7 Ethical considerations
Before conducting data collection, researchers applied and obtained ethical clearance from IRB/CMHS (Number: 299/CMHS IRB/2022), and then permission to conduct research was requested from Ndera Neuropsychiatric Hospital.
2.8 Informed consent, ascent, and incentives
Stabilized women living with mental illness and epilepsy were contacted and explained the study's aim. Before data collection women who were willing to participate in the study signed the consent form. Anonymity was guaranteed by using codes instead of names. Participants were explained that there would be no consequences for participating or refusing to participate in the study and that they could withdraw from the study at any time. The ascent form was also used to ensure that minor participants who met the criteria to participate in the study were still able to participate in the study. In such cases, a legal representative or guardian was approached for their consent on behalf of the participant. This process involved explaining the study's aim and obtaining their permission for the participants to take part. The participants' legal guardians provided written informed consent to participate in this study. They were also informed that the participant's anonymity would be protected and that they could withdraw their consent at any time. By obtaining ascent from both the participant and their representative or guardian, the researchers ensured that the rights and well-being of all participants were respected, even in situations where informed consent may not have been fully possible. There were also incentives for participating in this study. To ensure anonymity, the consent and ascent were kept separate from the questionnaire.
3 Results
3.1 Socio-demographic and economic characteristics of participants
A total of 289 women of reproductive age participated in the study, making a participation rate of 73%. Tables 1 and 2 provide an overview of the participants' socio-demographic and clinical mental health characteristics. Most participants (63.7%; n = 184) were older than 30 years of age. Of all the participants, 12.8% (n = 37) were single, while 19.7% (n = 57) were legally married and lived with their husbands. Regarding the education level, (3.1%; n = 9) of women had no education, while slightly more than half (51.2%; n = 148) had a primary level of education. Protestant religious believers (44.3%; n = 128) and Catholic religious believers (41.5%; n = 120) were predominant among participants in this study. Regarding the socio-economic conditions, the majority of participants (77.5%; n = 224) reported that they were unemployed, whereas 39.8% (n = 115) were classified in Category 1 and 30.1% (n = 87) were in Category 2.
3.2 Mental health characteristics of the participants
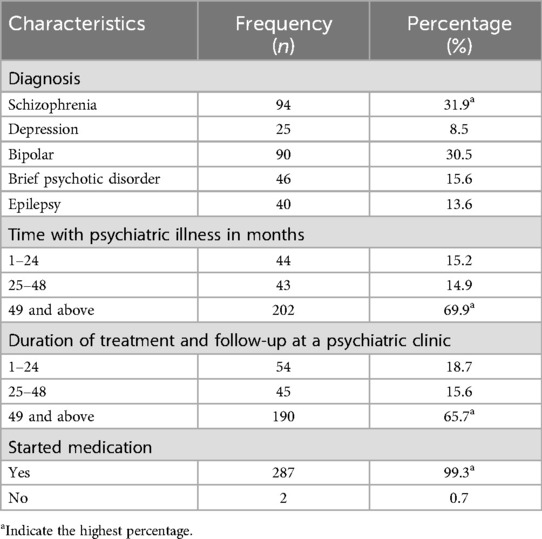
The majority of respondents (69.9%; n = 202) spent above 49 months living with a psychiatric illness and (30.5%; n = 90) of the respondents suffered from bipolar while (31.9%) were suffering from schizophrenia and (99.3%; n = 287) had already started taking medication (65.7; n = 190) had spent more than 49-month taking medication and making follow up at the psychiatric clinic.
3.3 Reproductive characteristics of the respondents
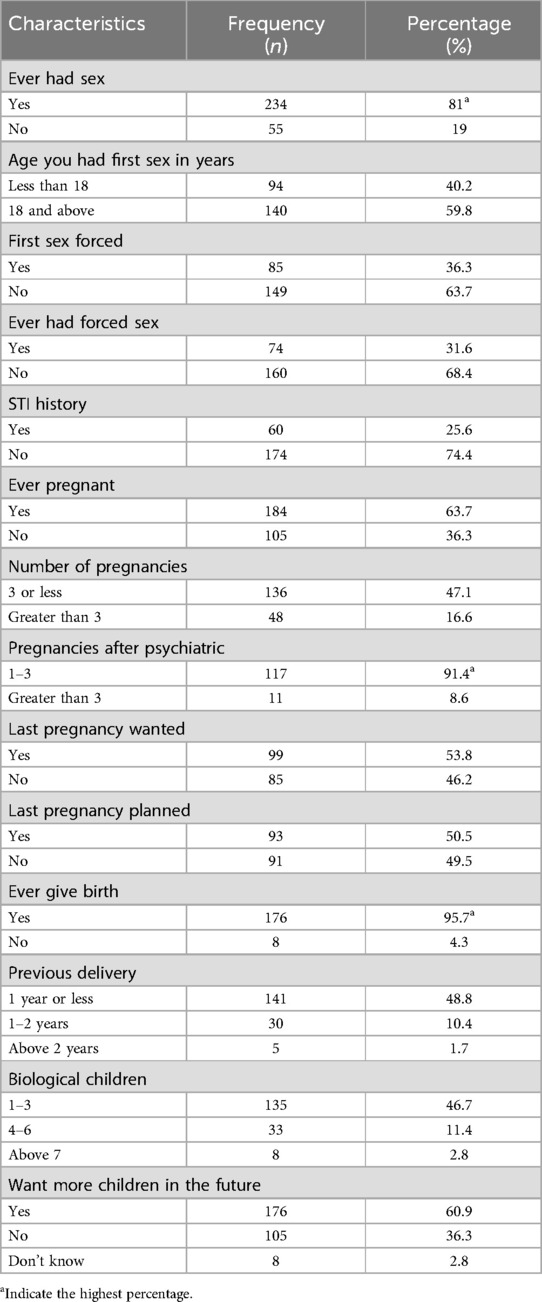
Most of the participants (81%; n = 234) had sex in life and (59.8%; n = 140) had their first sexual intercourse at the age of 18 years and above, of which 63.75% had a consenting first sexual intercourse, participants, while 31.6% had forced sex in their life. A relatively small number (25.6%) had a sexually transmitted illness history. Regarding pregnancy, (63.7%; n = 184) did not have a history of pregnancy while (95.7%; n = 176) had never given birth. Of those with pregnancy history, (47.1; n = 136) had 3 or fewer pregnancies and (46.7%; n = 135) had between 1 and 3 biological children. For participants who had fallen pregnant, more than half (53.8%) of the pregnancies were wanted, and 50.5% were planned. The women who had given previous delivery in 1 year or less at (48.8; n = 141). Of the participants who gave birth, a significant number (91.4%) gave birth after being diagnosed with a psychiatric disorder (91.4; n = 117). Among the participants only (60.9%, n = 176) wanted more children in the future (Table 3).
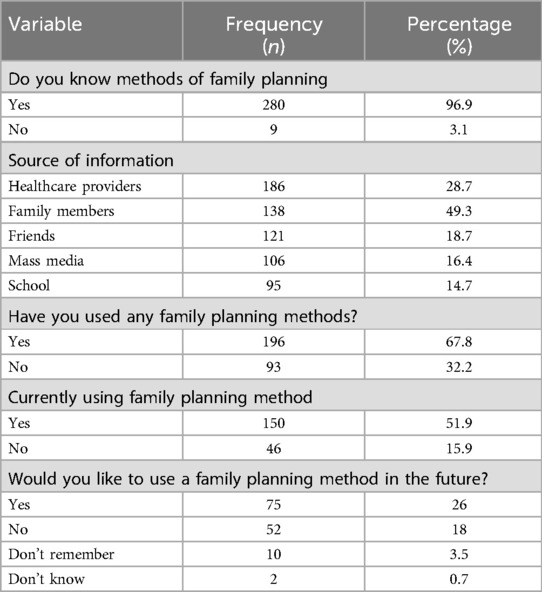
3.4 Family planning awareness, use, and self-reported source of information
The majority (96.9%, n = 280) of study participants were aware of FP methods, (67.8%, n = 196) had used one of the family planning methods in life and only (51.9%, n = 150) used the family planning methods at the time of data collection (see Table 4). Those who would like to use a family planning method in the future were at (26%, n = 75).
The women had information about the methods of family planning from health care providers (28.7%, n = 186) from family members, (49.3%, n = 138), from friends, (18.7%, n = 121), from mass media, (16.4%, n = 106), from school (14.7%, n = 95).
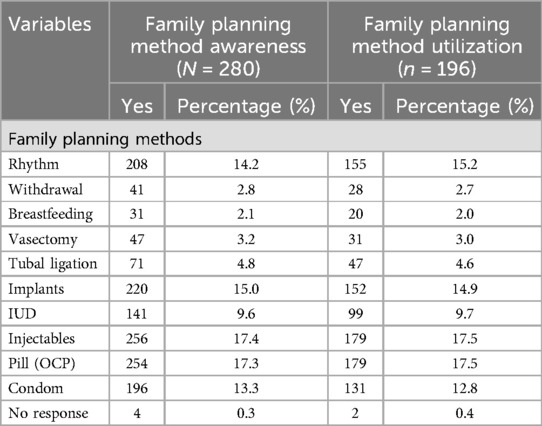
3.5 Family planning awareness and use based on the type of methods
The most commonly known methods were the injectable (17.3%; n = 256), oral contraceptive pill (17.3%; n = 254), contraceptive implant (15.0%; n = 220), rhythm (14.2%; n = 208) condoms (13.3%; n = 196), and intrauterine device (9.6%; n = 141), tube litigation(4.8%; n = 71), vasectomy(3.2%; n = 47); breastfeeding (2.1%; n = 31) and (2.8%; n = 41) reported the withdrawal as natural method (Table 5).
Regarding family planning utilization, the most frequently used methods of contraception were pills (17.5%; n = 179) and injectables (17.5%; n = 179). On the other hand, (14.9%; n = 152), (12.8%; n = 131), and (9.7%; n = 99) of women were using implants, condoms, and intrauterine devices respectively. The participants who used the tube litigation were (4.6%; n = 47), vasectomy (3.0%; n = 31). Regarding the natural methods breastfeeding was used by (2.0%; n = 20) and (2.7%; n = 155) reported having used withdrawal as a natural method.
3.6 Factors associated with family planning utilization
Table 6 shows the association between different factors with family planning utilization. On multivariable analysis, women who had primary school were more likely to use FP than those who had a high level of education (AOR = 5.6, 95% CI: 2.0, 15.9). Women who were married (AOR = 51.4, 95% CI: 11.9–22) and those who were single (AOR = 66.4, 95% CI: 9.8, 44) were more likely to use FP (AOR = 0.31, 95% CI: 0.19, 0.51) compared to those who were divorced or separated. The women who knew the contraceptive method (AOR = 5.8, 95% CI: 0.6, 49) were more likely to use FP than those who were not aware of the contraceptive. On multivariable analysis, women who suffer from Brief psychotic disorders had six times the odds of using family planning than those who didn't suffer from it (AOR = 2.7, 95% CI: 1.1, 6.6).
4 Discussion
This cross-sectional study attempted to assess knowledge, utilization of FP, and associated factors among women with a mental illness and epilepsy history in Rwanda. It included 289 women who were scheduled to be discharged from a psychiatric hospital and those who visited the outpatient services of the same hospital and its affiliated branches from October 2022 to February 2023. The majority of respondents have been living with a psychiatric condition for more than 49 months, and 31.9% were diagnosed with schizophrenia, while 13.6% had epilepsy. Of the respondents, a significant number had their pregnancies following their psychiatric diagnosis, and more than half (60.9%) had plans for future pregnancies. These findings underscore the FP needs of women with mental illness and epilepsy and reiterate the need to understand the FP use patterns in this vulnerable group.
Contrary to previous studies exploring FP among women with a psychiatric history within Sub-Saharan Africa, which found that this population was less aware of FP than the general population (2, 3), a huge majority of respondents (96.9%) from our study had an increased awareness of FP methods, 67.8% had used at least one FP method in the past, and more than half were using FP. The recent Rwanda Demographic Health survey found lower but closer estimates of the use of FP among married women (64%), while another Rwandan study revealed that 90% of the general population women were aware of family planning (16). Such an unexpected finding lends evidence to the positive uptake of FP among women with mental illness and epilepsy to the same level as women without a mental illness history in Rwanda.
Different factors are likely contributing to this reasonable knowledge of FP. First, Rwanda's efforts to strengthen the health system and to prevent unintended pregnancies, including increasing access to FP services and information (17), might have led to a massive reach of the majority of women of reproductive age, including those with mental health problems. Second, and as evidenced by the findings from our study, healthcare providers are the main source of information on FP for most respondents. Third, the integration of mental health services into primary care might have allowed women with mental health problems who attend these integrated services during their follow-up treatment to benefit from other health-related information, such as FP. It is therefore important that these strategies be maintained to continue accessing various categories of women.
Similar utilization patterns were found in terms of types of FP methods mostly used by women with a psychiatric history compared to the general population (18). In this study, the most frequently used methods of contraception were pills (17.5%) and injectables (17.5%). On the other hand, 14.9%, 12.8%, and 9.7% of women were using implants, condoms, and intrauterine devices respectively. A relatively small proportion of participants who used the tube litigation were (4.6%; n = 47), vasectomy (3.0%; n = 31). This confirmed the research conducted in Rwanda among women of reproductive age in the general population where pills and injections were the methods most commonly used (16), as well as research conducted in other African countries such as Ethiopia (19), and Uganda (18).
A possible explanation for the low awareness of long-acting reversible methods, intrauterine devices, tube litigation, and vasectomy found in the current study might be that due to the limited availability of these FP methods in resources-limited countries, health information for FP in these settings probably focuses mainly on the most available and affordable methods such as pills and injectable. However, even the natural traditional family planning methods that are less costly are also less known by women in our study, as only a relatively small number of respondents (2.1% and 2.8%) respectively mentioned breastfeeding and withdrawal among known FP methods, a finding that is similar to what was found among reproductive age women in Ethiopia (20). Health systems in low-resource countries should diversify the health information regarding FP to provide reproductive-age women with a wide range of FP methods, including natural FP methods. Particularly women with mental illness and epilepsy have an increased likelihood of inconsistent use, inadequate collaboration, and poor hygiene, which may make it impossible to use an intrauterine device (2); and are likely to discontinue their regular use of FP due to diminished judgment and have a high risk of drug interactions between antipsychotic and oral contraceptives (21). Conversely, injectables can be utilized when compliance cannot be ensured, the risk of discontinuation is high, and there are no contraindications (22). Hence, increased awareness of other FP options might be a benefit to women with mental illness and epilepsy.
Findings from multivariate regression analysis revealed that FP awareness was a predictor of FP use since women with mental illness and epilepsy in the current study who were aware of the contraceptive technique (AOR = 5.8, 95% CI: 0.6, 49) were more likely to use FP than those who were not. Therefore, efforts to increase awareness will eventually increase the amount of use since the gap between knowledge and use of FP is a measure of FP's unmet needs (23). Despite an increased awareness of FP, only 67.8% of the women who took part in our survey reported using any FP methods. This gap between knowledge and use from our study indicates that additional efforts will need to be undertaken to raise awareness of FP among women with mental disorders, to narrow that utilization gap, and to equip them with the necessary information to make FP choices that meet their specific needs.
The stigma, ignorance of the interactions between psychiatric medications and contraceptives, and other illness-related difficulties may have contributed to the differences between awareness and use among our study participants and the general population. The other factor might be because women with severe mental illness engage less with general health services and frequently with mental health professionals, who might not include FP information in their interactions with patients. Exploring these various potential barriers to FP use will require further research.
The multivariate regression analysis also revealed that women with mental illness who only completed primary school were more likely to use FP than those who completed high school (AOR = 5.6, 95% CI: 2.0, 15.9). This is another striking finding from our study since it does not seem to be the case in other studies conducted within Sub-Saharan Africa. Several other studies have shown that lower educational attainment is associated with less FP awareness and use (24), lending more credence to the idea that a lack of education prevents people from changing their contraceptive behavior (25). There are several possible explanations for this different finding. This may indicate that factors that affect FP utilization in such a vulnerable population as women with mental illness could be different from the general population. It can also be explained by the fact that in many cases involving women with mental health; FP decisions might be made by significant others, such as guardians, who might have a higher education level than the women using FP. Also, the study revealed that Women with no education or only primary education are more inclined to participate in high-risk fertility behaviors compared to those with higher levels of education. Each additional year of schooling decreases the likelihood of engaging in these high-risk behaviors by 6%, which may expose them to use FP methods (26).
However, we did not evaluate these factors or the severity of the mental disorder in this investigation and future studies may help enlighten this.
5 Limitations
This study does have some limitations. It could be challenging to determine a cause-and-effect link between the variables because the study is cross-sectional. Given the time and funding limitations, this study was unable to expand the sample to include other categories of women attending other settings. The results may not be generalizable to women with mental illness who do not attend psychiatric facilities because the study was carried out in hospitals where patients were believed to have better access to information.
6 Conclusion
Despite its limitations, this research is the first to have examined FP awareness and use among Rwandan women with mental illness and epilepsy. Findings revealed that women with mental illness are empowered with the necessary knowledge of FP to the same level as women without a mental illness history, but a significant gap between awareness and use remains. A personalized and systematic approach to empowering women with mental illness on FP methods is vital to meet the FP needs of this vulnerable group. Mental health services should integrate FP information into their routine practices to mitigate the remaining gap. Other FP types such as condoms should be advised to women with mental illness who are of reproductive age regardless of the method utilized due to the protection provided against sexually transmitted diseases. To gain a deeper understanding of the enablers and barriers to accessing family planning among women with mental illness and epilepsy, qualitative studies are needed. Additionally, a study on the interactions between FP contraceptives and psychiatric drugs is required.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by College of Medicine and Health Sciences (University of Rwanda) IRB. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
PM: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Formal Analysis, Funding acquisition, Investigation, Project administration, Supervision, Validation. MU: Conceptualization, Formal Analysis, Writing – original draft, Writing – review & editing. BU: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing, Validation. DM: Project administration, Writing – original draft, Writing – review & editing. DG: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. VB: Data curation, Formal Analysis, Writing – original draft, Writing – review & editing. PU: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. FS: Investigation, Supervision, Validation, Writing – original draft, Writing – review & editing. OB: Methodology, Writing – original draft, Writing – review & editing. CK: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Data curation.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded with support from the Center for International Reproductive Health Training at the University of Michigan (CIRHT-UM).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1373051/full#supplementary-material
References
1. dos Santos JC, Barros S, Huxley PJ. Social inclusion of the people with mental health issues: compare international results. Int J Soc Psychiatry. (2018) 64(4):344–50. doi: 10.1177/0020764018763941
2. Zerihun T, Sorsdahl K, Hanlon C. Family planning for women with severe mental illness in rural Ethiopia: a qualitative study. Reprod Health. (2021) 18(1):1–11. doi: 10.1186/s12978-021-01245-1
3. Zerihun T, Bekele D, Birhanu E, Worku Y, Deyesa N, Tesfaye M. Family planning awareness, utilization and associated factors among women of reproductive age attending psychiatric outpatient care, a cross-sectional study, Addis Ababa, Ethiopia. PLoS One. (2020) 15(9):1–12. doi: 10.1371/journal.pone.0238766
4. Herzog AG, Mandle HB, Cahill KE, Fowler KM, Fowler KM, Hauser WA. Predictors of unintended pregnancy in women with epilepsy. Neurology. (2017) 8:728–33. doi: 10.1212/WNL.0000000000003637
5. Abe K, Hamada H, Yamada T, Obata-Yasuoka M, Minakami H, Yoshikawa H. Impact of planning of pregnancy in women with epilepsy on seizure control during pregnancy and on maternal and neonatal outcomes. Seizure. (2014) 23(2):112–6. doi: 10.1016/j.seizure.2013.10.003
6. Nikolajski C. Contraceptive and Family Planning Experiences, Priorities, and Preferences of Women with Serious Mental Illness. Thesis University of Pittsburgh, Oakland, CA. (2018). Available online at: http://d-scholarship.pitt.edu/34006/1/Nikolajski_Cara_Dissertation_April2018.pdf
7. Ayinmode MFT. Current knowledge and pattern of use of family planning methods among a severely ill female Nigerian psychiatric outpatients: implication for existing service. Ann Afr Med. (2013) 12(1):16–23. doi: 10.4103/1596-3519.108245
8. Sethuraman B, Rachana A, Kurian S. Knowledge, attitude, and practice regarding contraception among women with schizophrenia: an observational study from south India. Indian J Psychol Med. (2019) 41(4):323–3230. doi: 10.4103/IJPSYM.IJPSYM_134_19
9. Kayiteshonga Y, Sezibera V, Smith-Swintosky S, Iyamuremye JD, Kamukunzi M, Nyandwi A, et al. Rwanda Mental Health Survey (RMHS). Kigali: Rwanda Biomedical Center (2018). Available online at: https://rbc.gov.rw/rnhrr/article?code=22
10. Rugema L, Ntaganira J, Persson M, Krantz G. A qualitative study of healthcare professionals’ perceptions of men and women’s mental healthcare seeking in Rwanda. J Community Psychol. (2020) 48(2018):891–903. doi: 10.1002/jcop.22308
11. Ministry of Health. National study in Rwanda family planning barriers. Rwanda Public Health Bull. (2019) 1(1):31–2.
13. Erdfelder E, Faul F, Buchner A, Lang AG. Statistical power analyses using G*power 3.1: tests for correlation and regression analyses. Behav Res Methods. (2009) 41(4):1149–60. doi: 10.3758/BRM.41.4.1149
14. Mental Health Among Women Of Reproductive Age. A Report of the Center for Chronic Diseases Prevention, Division of Reproductive Health. Atlanta, GA: National Center for Chronic Disease Prevention and Health Promotion Division of Reproductive Health (2016). p. 2014–7. Available online at: https://www.cdc.gov/ccindex/pdf/mentalhealthamongwomenofreproductiveage_vb.pdf
15. Prachi R, Das GS, Ankur B, Shipra J, Binita K. A study of knowledge, attitude and practice of family planning among the women of reproductive age group in sikkim. J Obstet Gynecol India. (2008) 58(1):63–7. https://www.researchgate.net/publication/228480182
16. Frederic TM, Phoibe K, Ntaganira J. Assessment of knowledge, attitudes, and practice on contraceptive use among women attending family planning services in some health centers of Muhima district hospital, Rwanda. Open Sci J. (2017) 2(3):1–17. doi: 10.23954/osj.v2i3.978
17. Schwandt H, Boulware A, Corey J, Herrera A, Hudler E, Imbabazi C, et al. Family planning providers and contraceptive users in Rwanda employ strategies to prevent discontinuation. BMC Womens Health. (2021) 21(1):1–13. doi: 10.1186/s12905-021-01503-1
18. Alege SG, Matovu JKB, Ssensalire S, Nabiwemba E. Knowledge, sources and use of family planning methods among women aged 15–49 years in Uganda: a cross-sectional study. Pan Afr Med J. (2016) 24:1–12. doi: 10.11604/pamj.2016.24.39.5836
19. Mekonnen G, Enquselassie F, Tesfaye G, Semahegn A. Prevalence and factors affecting use of long acting and permanent contraceptive methods in Jinka town, Southern Ethiopia: a cross sectional study. Pan Afr Med J. (2014) 18:1–8. doi: 10.11604/pamj.2014.18.98.3421
20. CSA. Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia and Rockvile, Maryland, USA: Central Statistical Agency (CSA) [Ethiopia] and ICF (2016). p. 134. Available online at: www.DHSprogram.com
21. Schoretsanitis G, Deligiannidis KM, Paulzen M, Spina E, de Leon J. Drug-drug interactions between psychotropic medications and oral contraceptives. Expert Opin Drug Metab Toxicol. (2022) 18(6):395–411. doi: 10.1080/17425255.2022.2106214
22. Bunney PE, Zink AN, Holm AA, Billington CJ, Kotz CM. Orexin activation counteracts decreases in nonexercise activity thermogenesis (NEAT) caused by high-fat diet. Physiol Behav. (2017) 176(8):139–48. doi: 10.1016/j.physbeh.2017.03.040
23. Tilahun T, Coene G, Luchters S, Kassahun W, Leye E, Temmerman M, et al. Family planning knowledge, attitude and practice among married couples in Jimma zone, Ethiopia. PLoS One. (2013) 8(4):1–8. doi: 10.1371/journal.pone.0061335
24. Kimuna SR, Adamchak DJ. Gender relations: husband-wife fertility and family planning decisions in Kenya. J Biosoc Sci. (2001) 33(1):13–23. doi: 10.1017/S002193200100013X
25. Duze MC, Mohammed IZ. Male knowledge, attitudes, and family planning practices in Northern Nigeria. Afr J Reprod Heal. (2006) 10. Available online at: https://pubmed.ncbi.nlm.nih.gov/17518131/
Keywords: family planning, women, mental illness, epilepsy, psychiatric disorders
Citation: Mukangabire P, Umuziga MP, Umubyeyi B, Mukamana D, Gishoma D, Baziga V, Uwimana P, Sebera F, Bazirete O and Kanazayire C (2024) Family planning knowledge, use, and associated factors among women with mental illness and epilepsy in Rwanda: a cross-sectional study. Front. Glob. Womens Health 5:1373051. doi: 10.3389/fgwh.2024.1373051
Received: 5 March 2024; Accepted: 18 September 2024;
Published: 25 October 2024.
Edited by:
Saranraj Loganathan, Mepco Schlenk Engineering College, IndiaReviewed by:
Abraham Gyamfi, Akenten Appiah-Menka University of Skills Training and Entrepreneurial Development, GhanaSankar Malayandi, Mepco Schlenk Engineering College, India
Copyright: © 2024 Mukangabire, Umuziga, Umubyeyi, Mukamana, Gishoma, Baziga, Uwimana, Sebera, Bazirete and Kanazayire. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pacifique Mukangabire, cGFjaW5nYWJpcmVAeWFob28uZnI=
 Pacifique Mukangabire
Pacifique Mukangabire M. Providence Umuziga1
M. Providence Umuziga1 Benoite Umubyeyi
Benoite Umubyeyi Philomene Uwimana
Philomene Uwimana