- 1Health Economics and Policy Department, Division of Health Research Graduate College, Lancaster University, Lancaster, United Kingdom
- 2Economics Department, Lancaster University, Lancaster, United Kingdom
Objectives: The aim of this scoping review was to identify and provide an overview of the impact of sexual and reproductive health (SRH) interventions on reproductive health outcomes among young people in sub-Saharan Africa.
Methods: Searches were carried out in five data bases. The databases were searched using variations and combinations of the following keywords: contraception, family planning, birth control, young people and adolescents. The Cochrane risk-of-bias 2 and Risk of Bias in Non-Randomized Studies-of-Interventions tools were used to assess risk of bias for articles included.
Results: Community-based programs, mHealth, SRH education, counselling, community health workers, youth friendly health services, economic support and mass media interventions generally had a positive effect on childbirth spacing, modern contraceptive knowledge, modern contraceptive use/uptake, adolescent sexual abstinence, pregnancy and myths and misperceptions about modern contraception.
Conclusion: Sexual and reproductive health interventions have a positive impact on sexual and reproductive health outcomes. With the increasing popularity of mHealth coupled with the effectiveness of youth friendly health services, future youth SRH interventions could integrate both strategies to improve SRH services access and utilization.
1 Introduction
Sexual and reproductive health (SRH) challenges are currently recognised through Sustainable Development Goal (SDG) number 3 (1, 2). SRH problems have been shown to account for about one-fifth of the disease burden worldwide (3) and the burden is much higher among young women in the reproductive age group (4). Sexual activity and experimentation are normative parts of adolescent development that may, at the same time, be associated with adverse SRH outcomes, including the acquisition of sexually transmitted illnesses (STIs), unplanned pregnancies and abortions (5, 6). Moreover, many young women are at high risk of lack of access to, and inconsistent or incorrect use of contraception leading to unintended pregnancies (7, 8). Unintended pregnancies result in disruptions in young women's education, professional opportunities and, essentially, reproductive sovereignty. Inequalities such as these have implications on a central pillar of the SDGs: to leave no one behind. While overall, significant progress has been made on the SDGs in years gone by, some discrepancies have continued, including those between rural and urban communities as well as those caused by socioeconomic status, gender, age and other demographic factors (9).
Young people especially in sub-Saharan African have been reported to have limited access to SRH services (10, 11). Access to SRH services is affected by a myriad of factors related to young people's SRH knowledge and awareness of availability of services, and access and usage of these services. Several cultural, socioeconomic and political factors further act as barriers to the delivery of SRH information and services to young people. Additionally, failure to provide youth friendly SRH services, unwelcoming behaviour and negative attitude by healthcare workers often act as barriers to young people's access and usage of SRH services (12, 13). These scenarios puts pressure on sub-Saharan Africa policy makers and practitioners to find ways of mitigating SRH challenges (14). Therefore, health care providers have an important role to play in ensuring that young people have access to high quality and non-judgmental SRH services in youth-friendly settings that recognize the unique bio-psychosocial needs of young people (6).
Several countries in sub-Saharan Africa including Zimbabwe, Malawi, Kenya, Rwanda, Ethiopia and South Africa have implemented successful SRH programs targeting young people (15, 16). Thus, African countries have acknowledged the importance of SRH among young people, and as a result, have been implementing related strategies both at community and facility levels. These strategies have included comprehensive sexuality education (CSE), referred to as sexuality and relationship education curricula that are age-appropriate and culturally relevant (17, 18). They have also encompassed peer education, mass media campaigns, cash transfers and youth-friendly centres—which are spaces created for young people to access SRH health information and services (19–21), and youth-friendly services—which are accessible and appropriate services that appeal to youths in a manner that promotes equity and interactions between users and providers (22).
2 Objective
The aim of this scoping review was to identify SRH interventions and provide an overview of the impact these interventions on reproductive health outcomes among young people in sub-Saharan Africa.
3 Methods
Preferred Reporting Items for Systematic reviews and Meta-Analysis extension for Scoping reviews (PRISMA-ScR) guidelines were used to search and select the articles included in this scoping review (23). To make sure that all relevant information was included in the analysis, the PRISMA-ScR checklist (Table 1) was utilised. Data extraction was also guided by the PROGRESS-Plus framework, which was suggested by the Campbell and Cochrane Equity Methods Group (24). The population, intervention, comparison, outcome and context (PICOC) model for review questions was applied in the designing of the research question (25).
3.1 Search strategy
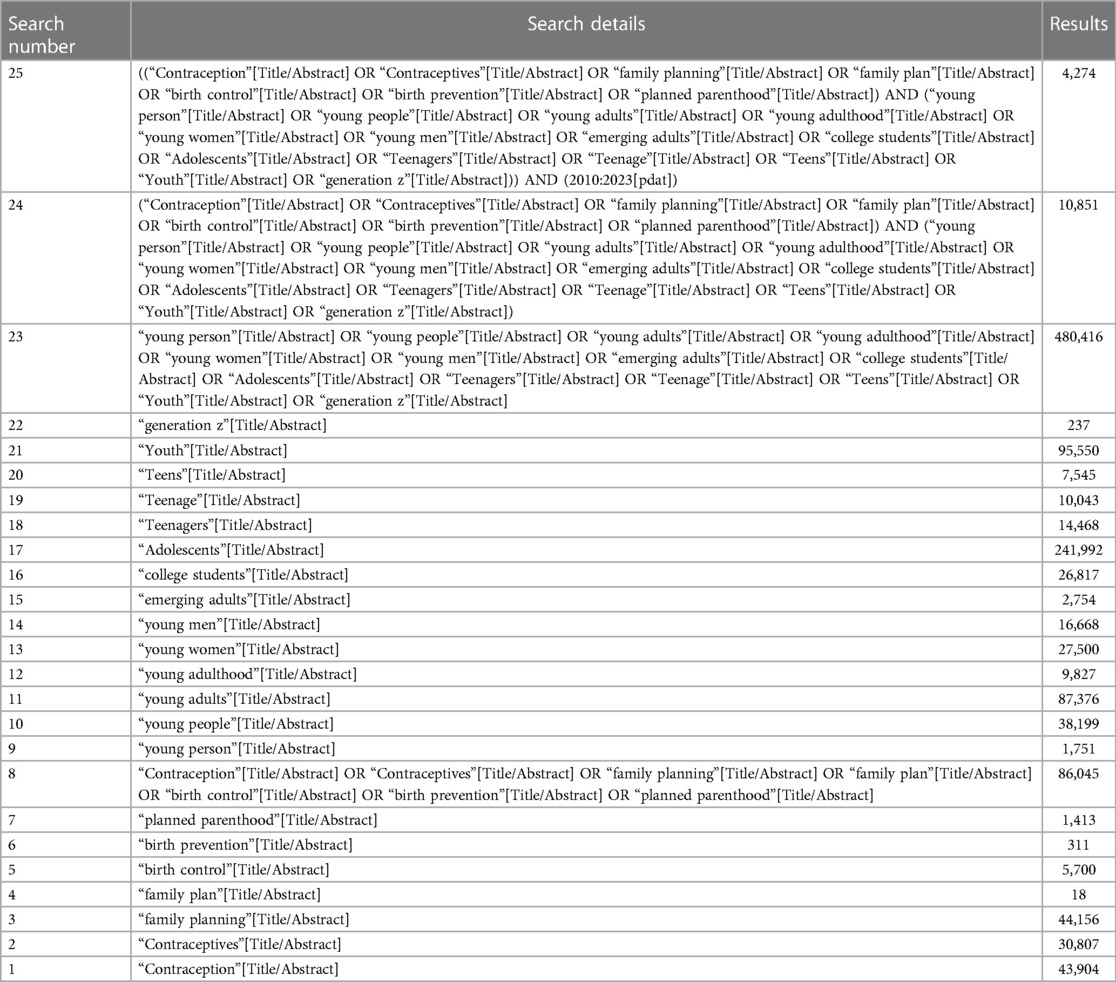
Five databases were searched: PubMed, Scopus, Psychological Information Database (PsycINFO), Cumulative Index to Nursing and Allied Health Literature (CINAHL), and the Cochrane Central Register of Controlled Trials. Predefined keywords, such as “contraceptives” and “young adults,” together with their synonyms, were used to search the databases. It was decided to create each concept's variations based on similar reviews. The initial search was conducted in August 2021 and updated in August 2023. Table 1 illustrates the search strategy for PubMed including Boolean operators, which was adapted for the other databases. Relevant articles were also searched using the PubMed “similar articles” function. To maximise the findings’ applicability to current policy, a literature search was conducted from January 2010 to August 2023.
3.2 Data collection and analysis
3.2.1 Selection of studies
Two reviewers independently examined the titles and abstracts, excluding articles that were irrelevant. The articles that were identified were transferred to Mendeley Desktop, where any duplicated articles were eliminated. Afterwards, the reviewers assessed the eligibility of the remaining articles.
3.2.2 Data extraction
Two reviewers independently gathered information from each article that was included in the comprehensive review by utilizing a predetermined excel spreadsheet form for data extraction. The excel spreadsheet form was developed by the reviewers. In case of any discrepancies, a third reviewer was involved to achieve a resolution. The following information was extracted from each article:
(1) Bibliographic information
(2) Study aims or questions.
(3) Study characteristics (design, sample size, number of arms)
(4) Intervention and control (type and characteristics of interventions and controls)
(5) Study setting (country)
(6) PROGRESS-Plus factors
(7) Outcome measures (type of outcome, definition of outcome)
3.2.3 Criteria for considering studies for this review
Studies that met the following criteria were included:
Population: Studies that focused on youths aged 15–24 years in Sub-Saharan Africa. However, for the purpose and context of the scoping review the word youths was used interchangeably with young people.
Intervention: This review focused on articles that reported on the effectiveness of SRH interventions on pregnancy and contraceptive use. The review also focused on papers that report effectiveness of SRH interventions on secondary outcomes such as increased knowledge of contraceptives, positive attitude/change towards contraceptives and dispelling myths and misconceptions.
Comparison: Studies with comparison groups that included older people (25 and above), no intervention, standard care group and another intervention.
Study designs: Randomised controlled trials (RCTs), interrupted time series, prospective or retrospective cohort studies and controlled before and after designs that meet the inclusion criteria were considered for the study.
Outcomes:
Primary outcomes included studies with at least one of the following metrics:
• Using contraception; using a new technique; continuing or improving the usage of an existing method.
• Becoming pregnant (at least six months after the intervention started).
Secondary outcomes include the following:
• Attitude about contraception or a particular type of contraception.
• Knowledge of the effectiveness of contraceptives or the usage of effective methods.
• Adolescent sexual abstinence.
Context: sub-Saharan Africa.
Studies were excluded if:
• Full text and abstract were both unavailable or only the abstract was available but did not convey the needed data.
• Conference abstract
• Narrative or systematic reviews
• Published before January 2010
3.3 Assessment of study quality
The Cochrane Risk-of-Bias tool for randomised trials (RoB 2), version 2, was employed by the reviewers for randomised controlled trials (RCTs). Five categories were used to evaluate bias, with each aspect receiving a judgement (high, low, unclear), namely selection, performance, attrition, reporting, and other (26). Reviewers employed the Risk of Bias in Non-Randomized Studies—of Interventions (ROBINS-I) tool to evaluate the risk of bias in non-randomized controlled trials. Studies were categorised as having a low, moderate, significant, or critical risk of bias (27).
3.4 Data synthesis
Due to the heterogeneity in the design of the studies that were included, along with the diversity in outcomes and interventions, it was deemed unsuitable to conduct a meta-analysis. To enable the exploration of descriptive themes derived from the research, a thematic synthesis approach was employed for data synthesis. A narrative summary was utilized to provide an interpretation of the results and elucidate their connection to the objectives and inquiries of the review (28).
3.5 Patient and public involvement statement
Since the data for the review article was extracted from published articles, without direct patient involvement, ethical approval was not required.
4 Results
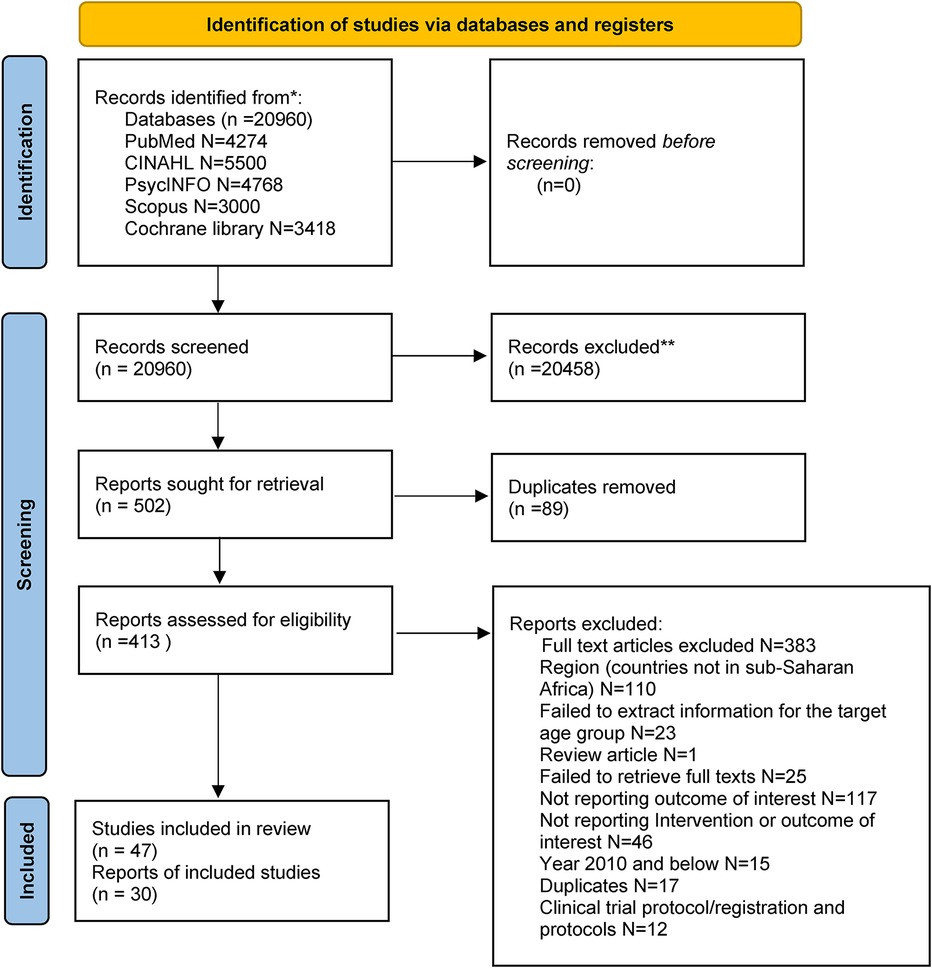
4.1 Identification of potential studies
Electronic searches of 5 databases identified 20,960 potential articles (Pubmed: 4,274, CINAHL: 5,500, Cochrane: 3,418, PsycINFO: 4,768, Scopus: 3,000). After 20,458 were excluded through screening the titles and abstracts, followed by removal of 89 duplicates, a total of 413 full text articles were screened for eligibility. Full text screening led to a total of 30 full text articles and 46 studies that were included in the scoping review. Figure 1 shows the flow chart of the studies identification and selection process.
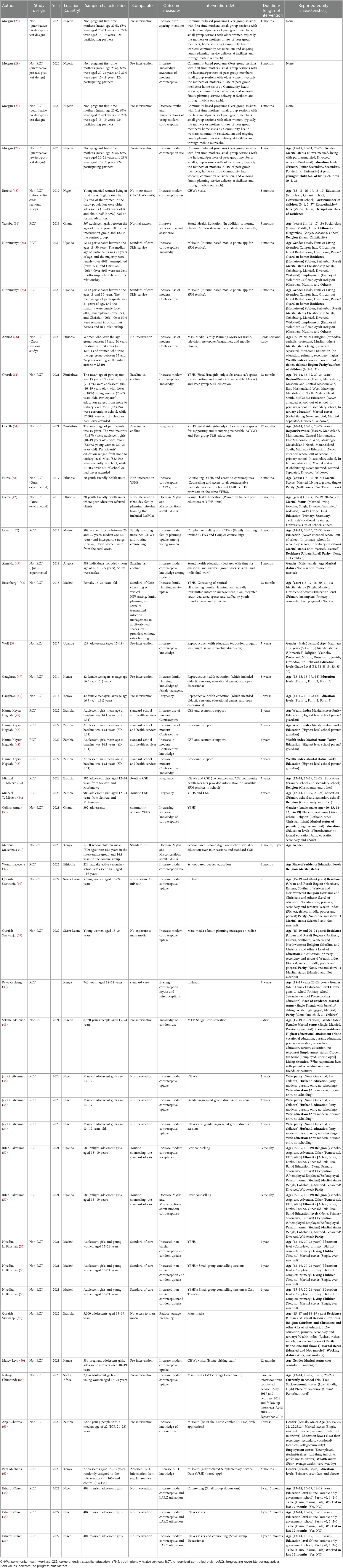
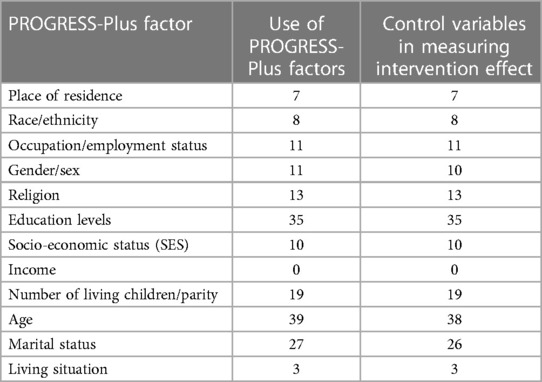
4.2 Usage of PROGRESS-Plus factors
All 30 articles and 43 individual studies reported at least 2 PROGRESS-Plus factors (Tables 2, 3). Age distribution was the most reported PROGRESS-Plus factor (reported in 39 studies) followed by education levels, marital status, and parity which were reported in 35, 27 and 19 studies respectively. Religion was reported in 13 studies, and gender, occupation and socio-economic status were reported in 11 studies each. Place of residence and race/ethnicity were reported in 7 and 8 studies respectively. Living situation was the least reported PROGRESS-Plus factor, being reported in 3 studies. Most studies (n = 43) considered PROGRESS-Plus factors as control variables when measuring the effect of the intervention for example in logistic regression. Among these, age, education levels and marital status were the most controlled for. Three studies in an article by Morgan and colleagues (29) and one study in an article by Levy and colleagues (30) identified PROGRESS-Plus factors, but failed to include them in their final analyses.
4.3 Risk of bias in included RCT studies
The risk of bias results for RCT studies (n = 20) are summarised in Figures 2, 3. Reporting on the overall risk of bias domain, six studies had low risk bias, one study each from articles by Yakubu and colleagues, Wondimagege and colleagues and Gichangi and colleagues (31–33), and three studies from an article by Silverman and colleagues (34). Most of the studies 45% (n = 9) had some concerns in the overall risk of bias domain. Lastly, five studies, two studies each from articles by Nuwamanya and colleagues (35) and Erdhardt-Ohren colleagues (36) and one study from an article by Lemani and colleagues (37) had high risk of bias.
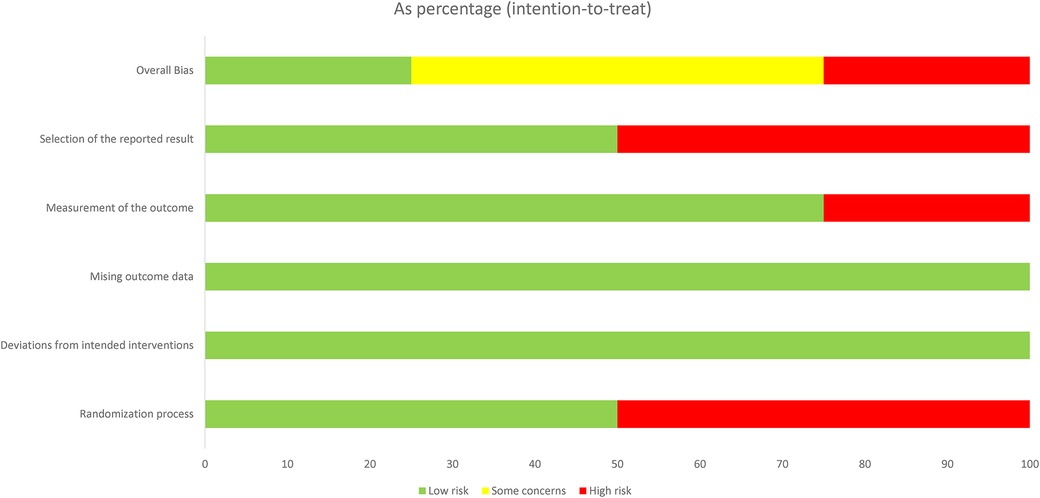
Figure 3. Risk of bias graph of each domain presented as percentages across all RCT included in the review.
4.4 Risk of bias of non-randomised control studies included in the scoping review
The risk of bias assessment results using the ROBINS-I tool for the non-RCTs studies (n = 26) is shown in Figure 4. Based on the ROBINS-I tool none of the studies included in the review had an overall low risk of bias. As expected with non-RCTs, most studies 76.9% (n = 20) included were labelled as moderate risk studies across all domains. Five studies were labelled as serious risk studies across all domains (30, 38–41) and one study by Fikree and colleagues (42) was judged to be critical risk of bias study.
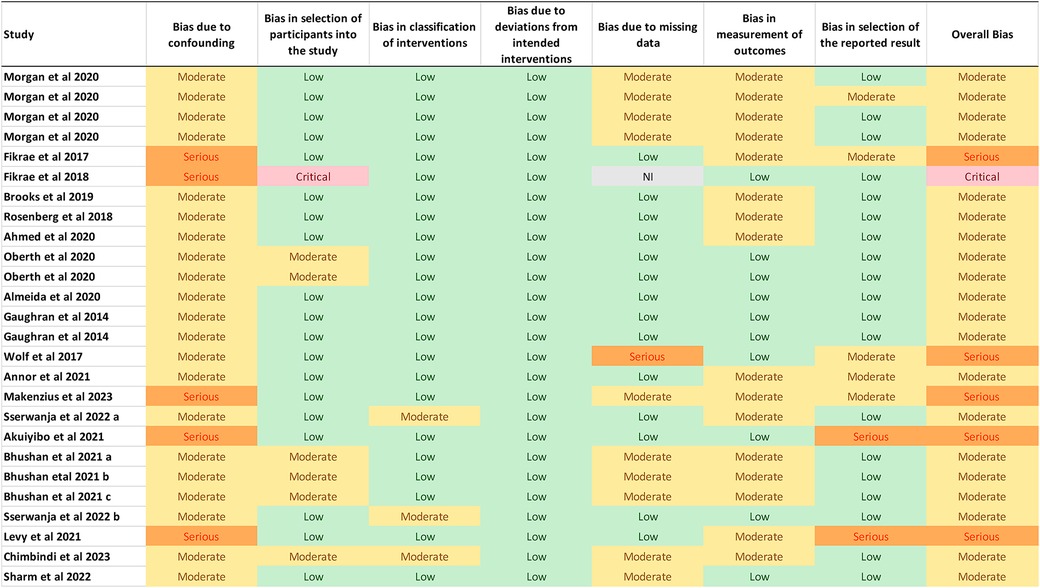
Figure 4. Quality assessment of quantitative non-randomised controlled studies included in the systematic review.
4.5 SRH interventions identified from the review
The narrative synthesis of the results used in this scoping review was done in line with the recommendations set out in the PRISMA-ScR guidelines. Based on the research objectives, studies were classified into one of the following eight research domains: community-based program interventions, community health workers interventions, SRH education interventions, Youth friendly health services (YFHS) interventions, counselling interventions, mobile phone-based interventions, economic support, and mass media.
4.5.1 Community-based program intervention
Four studies in an article by Morgan and colleagues 2020, used a community-based program with multiple interventions to improve SRH among young people. The program included home visits by community health workers, community sensitization, and continuing family planning service delivery at facilities and through mobile outreach. It also included peer group sessions with first-time mothers, small group sessions with the husbands or partners of peer group members, and small group sessions with older women, usually the mothers or mothers-in-law of peer group members (29).
4.5.2 Community health workers interventions
Community health workers (CHWs) or lay health worker are defined as healthcare workers who perform functions related to health care delivery and are trained in some way in the context of an intervention, but who has not received a formal professional or para-professional certificate or tertiary education degree (7, 43). CHWs are an effective means to reach clients when access is limited especially in poor resourced remote rural areas (44). In the current review, 7 studies assessed the impact of CHWs interventions on SRH outcomes among adolescents and young adults. Brooks and colleagues, 2019 and Silverman and colleagues, 2023, reported that CHWs improved modern contraceptive uptake among adolescent girls (single, pregnant, married or pregnant) (34, 45). Mbizvo and colleagues, 2023, reported that CHWs coupled with comprehensive sexuality education (CSE) or YFHS improve pregnancy outcomes among adolescent girls. Lastly, Erhardt and colleagues, 2023, and Lemani and colleagues, 2017, reported that CHWs coupled with counselling improve modern family planning uptake among young women (36).
4.5.3 SRH education
Comprehensive SRH education has been reported to be an effective strategy for improving young people's SRH outcomes (46). In the current review, 12 studies reported use of SRH education interventions as a strategy to improve SRH outcomes. Firstly, Yakubu and colleagues, 2019, and Guaghran and colleagues, 2014, reported that sexual health education improved sexual abstinence and pregnancy outcomes among adolescents girls (31, 47). Secondly, Fikree and colleagues, 2018, and Makenzius and colleagues, 2023, reported that SRH education provided by trained peer educators at YHFs and stigma-reduction sexuality education decreased myths and misconceptions about LARCs utilization (40, 42). One study from an article by Hegdahl and colleagues, 2022, reported that comprehensive sexuality education (CSE) combined with economic support improved modern contraceptives uptake among adolescent girls (48). Lastly, 5 studies reported that SRH education improved knowledge of modern contraceptive methods among young people (39, 41, 47–49). Details of the reproductive health education strategies utilized by each study are shown in Table 2.
4.5.4 Youth friendly health services (YFHS) interventions
There is evidence that YFHS improve access to, and utilisation of SRH services by young people (19, 50). In the current review, 9 studies reported the use of YFHS interventions among young people. Four articles reported that YFHS interventions improved modern contraceptives knowledge and uptake by young people (38, 51–53). Oberth and colleagues, 2021, and Mbizvo and colleagues, 2023, reported that YFHS combined with peer group education and CSE, respectively, improved pregnancy outcomes among adolescent girls (51, 54). Three studies from an article by Bhushan and colleagues, 2021, reported that YFHS interventions improved non-barrier contraceptives and condoms uptake among young women (55) (see Table 2 for details of the interventions).
4.5.5 Counselling interventions
Counselling, as an intervention, has been shown to improve SRH services utilisation among young people. Counselling can be delivered directly in person, online, or via the telephone, either by medical or nursing staff, or peers, in individual or group settings. The counselling interventions may consist of a single component or multiple components delivered in a single session, or in multiple sessions at various time points (56). In the present review, 10 studies utilized counselling interventions as strategies for improving modern family services uptake and decreasing myths and misconceptions about modern contraceptives. Among these studies, 2 from an article by Bakesiima and colleagues, 2021, reported that peer counselling improved modern contraceptives acceptance and dispelled myths and misconceptions about modern contraceptives among adolescent girls aged 15–19 years (57). Furthermore, 8 studies from 5 articles reported that groups or couples counselling only, and counselling combined with different SRH interventions (including CHWs, economic support and YFHS) increased modern family planning services uptake and utilization among young women (34, 36–38, 55) (see Table 2 for details of the counselling multicomponent interventions).
4.5.6 Mobile phone-based interventions (mHealth)
Expansion of mobile phone technology and use in recent years provides an important tool to reach underserved populations in low to middle income countries. Populations with restricted access can be reached despite location and need (58–60). With the increasing popularity of mobile based interventions with young people, they promise to improve SRH services utilisation young people. In the present review, four studies utilised mHealth interventions to improve SRH outcomes (33, 35, 61, 62). Nuwamanya and colleagues, 2020, used an internet based mobile phone application to improve the use of modern contraceptive methods (35). Gichangi and colleague, 2022, reported that there was a statistically significant drop in the average absolute number of contraceptives myths and misconceptions believed by the mHealth intervention arm between baseline and endline (33). Sharma and colleagues 2022, reported that at the endline, an mHealth intervention resulted in higher level of knowledge related to condoms and on wearing condoms correctly (61). According to Macharia and colleagues, (2023), there was a statistically significant difference in the total knowledge scores in the mHealth intervention group compared with the control group. Young people reported gaining knowledge on abstinence and condom use from an mHealth application (62).
4.5.7 Economic support
Gender inequality and economic constrains are central factors limiting young women's urgency regarding their own SRH, and ability to use their preferred contraceptive methods (48, 63). Economic support including cash transfers have been theorised to reduce young women's economic vulnerability and engagement in unsafe or asymmetric transactional sex (48, 64). Moreover, free access to a broad contraceptive method mix could increase contraceptive uptake, reduce unmet need, and increase agency in contraceptive decision-making among young women in resource-limited settings (63). In the present review, Hegdahl and colleagues, (2022), reported that there was no evidence of the effects of economic support on contraceptive use among those ever sexually active. However, the addition of CSE improved modern contraceptive use and knowledge of modern contraceptives compared to economic support alone among those recently sexually active (48). Likewise, Bhushan and colleagues, 2021, reported that cash transfers combined with YFHS and small group counselling increased non-barrier contraception and condom uptake (55). In conclusion, economic support coupled with other SRH interventions improves reproduction health outcomes among young women.
4.5.8 Mass media
Mass media campaigns have the potential to effectively convey SRH messages to a wide population. Due to their ability to reach the masses, these campaigns can specifically target a significant number of and young individuals at a relatively minimal expense. Mass media campaigns typically utilize various platforms such as newspapers, television, radio, magazines, social media, and billboards within sub-Saharan Africa. Additionally, they can also be executed through cinema or emerging digital media channels, which encompass websites, pop-up and banner advertisements, codes, and viral marketing (65). Despite previous research highlighting that mass media campaigns can influence SRH (41, 66–68), there have been few attempts to synthesise evidence across young people's reproduction SRH outcomes. Similar to the review by Stead and colleagues, 2019, this study reported mixed evidence of the effect of mass media campaigns on SRH outcomes (65). After adjusting for covariates, Sserwanja and colleagues, 2022, reported that hearing family planning messages on radio and reading texts on mobile phones were statistically associated with increased modern contraceptives uptake among young people in Sierra Leone (69). They further reported that young women who had exposure to family planning messages on radio and mobile phones were more likely to use modern contraceptives when compared to their counterparts without the same mass media exposure. In a different study conducted in Zambia, Sserwanja (67), reported that adolescent girls who had daily access to magazines or newspapers, or internet were less likely to be pregnant or to have had a pregnancy compared with those without the same mass media exposure. After adjusting for HIV-prevention, intervention-exposure, age, education, socioeconomic status, Ahmed and colleagues, 2020, reported that MTVShuga-DS exposure was associated with increased modern contraceptives uptake and consistent condom use among young Ethiopians (66). However, Ahmed and colleagues, 2020, reported that there was no statistically significant association between young women exposed to mass media family planning messages and modern contraceptives uptake in rural areas.
5 Discussion
According to the review, a variety of comprehensive interventions aimed at promoting and providing consistent birth control methods, sexual health education, counselling, and other related services may be able to prevent and control the negative effects associated with risky sexual behaviour among young people in sub-Saharan Africa. It has been demonstrated that raising awareness of SRH and the use of contraceptives lowers the number of unintended births among people. Our findings align with previous assessments that assess the efficacy of different treatments in enhancing teenage self-reported health, and integrate several interventions under a more comprehensive framework to assess their combined effectiveness. A combination of educational and contraceptive interventions may help reduce the rate of unintended pregnancies among adolescents, according to a Cochrane review on primary prevention interventions (school-based, community or home-based, clinic-based, and faith-based). On the other hand, the data from that study showed conflicting results for secondary outcomes, such as the onset of sexual activity, the use of birth control, abortion, childbirth, and STIs (70). Group-based comprehensive risk reduction intervention was found to be an effective technique to lower adolescent pregnancy, HIV, and STIs (71).
Thus, it is essential to raise knowledge of the advantages of contraceptive services and empower young people to make their own decisions about taking contraceptives (72). Combining educational programs in communities and schools with YFHS, health centre outreach initiatives, and media campaigns are examples of interventions with supporting data (73). Reproductive health services are more likely to be accessed when initiatives to increase service quality are combined with community outreach to encourage young people SRH (19). Regarding services, a number of program evaluations have detailed challenges that many teenagers encounter, including judgmental provider attitudes, a lack of anonymity, a dearth of alternatives for contraception, and a lack of rules and procedures to safeguard teenagers’ rights to information and services (21). Approximately one out of every five nations in the world has official rules that restrict access to contraceptive services: Among the most prevalent limitations, parental consent requirements are in place in 9% of the 186 countries for which data is available; limits based on a minimum age or marital status are in place in 5% of nations (74). Nevertheless, teenagers continue to experience provider prejudice in a variety of ways even in nations without official limits. Because of erroneous concerns that hormone treatments might interfere with a young person's ability to conceive, physicians might not advise hormonal treatments to them, or they might discriminate against single youth because they think they shouldn't engage in sexual activity (75). Recent guidelines for self-care treatments, such over-the-counter oral contraceptive tablets and self-administered injectables, may be able to assist young people in overcoming some of these fundamental obstacles (76).
5.1 Limitations and recommendations
Despite providing a broad overview of the impact of SRH interventions on reproductive health outcomes among young people in sub-Saharan Africa, the focus on a scoping review limited our ability to examine the impacts of interventions in detail and statistically. Statistical synthesis was not possible due to considerable heterogeneity across the large numerous articles and studies included in the review, and the SRH outcomes and interventions reported. To perform a meta-analysis, we recommend that future reviews should focus on one SRH outcome and one intervention.
Practice of medicine and public health interventions supported by mobile devices are effective strategies for improving reproductive health outcomes among young people as they promote SRH services utilization (33, 35, 61, 62). This is partly due to their popularity among young people, privacy, and ability to reach populations with restricted access to direct SRH services (58–60). Mass media campaigns can be utilized to communicate SRH information in mass populations and results from this review highlights that they can improve reproductive health outcomes. Since they are delivered at population level, mass media campaigns can target numerous numbers of young people at relatively low costs (65, 77, 78). Harnessing the advantages of both mHealth and mass media intervention could result in development of low cost, easily accessible, convenient, and age-appropriate strategies for widespread dissemination of SRH information (79). Therefore, it is highly recommended to integrate both mHealth and mass media campaigns in future SRH interventions targeting young people with access to mobile devices.
Despite different PROGRESS-Plus factors being reported to influence the effect of SRH interventions, studies in the review did not include all PROGRESS-Plus factors in their analysis which might have resulted in over estimation or underestimation of the impact of the interventions. Therefore, we recommend future studies with rigorous designs and longer-term follow-up to use all PROGRESS-Plus factors as control variables to measure the impact of SRH interventions and maximize applicability of results.
5.2 Contribution of the findings to the field of study
Young people make up a big proportion of the population in Africa's developing economies, with approximately 20% of the population aged 15–24 years. Despite increased attention to family planning, young people in this region continue to face numerous SRH challenges. The review findings could guide future strategies to improve SRH services’ access and utilization among young people in sub-Saharan Africa thereby protecting them from unintended pregnancies and unsafe abortions. The review suggests that community-based programs, mHealth, SRH education, counselling, community health workers’ visits and youth friendly health service interventions generally had a positive effect on child spacing, modern contraceptive knowledge, modern contraceptive use, adolescent sexual abstinence, pregnancy and myths and misperceptions of modern contraception. Evidence from the review has shown that bringing awareness of the benefits of modern contraceptives and enabling young people to make their own decisions regarding contraceptive services is vital. Several studies reported that mHealth is effective in promoting SRH services utilization. Therefore, future SRH strategies could utilise mHealth to improve knowledge, access and uptake of SRH services. Due to their ability to ensure privacy and reach underserved populations, incorporating mobile devices into SRH interventions among young people and utilizing mass media campaigns to reach a wider audience are recommended strategies. Combining these two components in future national SRH interventions has the potential to improve outcomes, positively impacting reproductive health on a larger scale, at relatively lower costs.
6 Conclusion
Community-based programs, mHealth, SRH education, counselling, CHWs, YFHS, economic support and mass media interventions generally had a positive effect on childbirth spacing, modern contraceptive knowledge, modern contraceptive use, adolescent sexual abstinence, pregnancy and myths and misperceptions of modern contraception. This scoping review could inform administrators, managers, and policymakers on the different SRH interventions to implement in different settings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
IC: Conceptualization, Data curation, Formal Analysis, Methodology, Resources, Writing – original draft, Writing – review & editing. SS: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. BH: Conceptualization, Data curation, Formal Analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1344135/full#supplementary-material.
References
1. Mwale M, Muula AS. Systematic review: a review of adolescent behavior change interventions [BCI] and their effectiveness in HIV and AIDS prevention in sub-saharan Africa. BMC Public Health. (2017) 17(1):1–9. doi: 10.1186/S12889-017-4729-2/PEER-REVIEW
2. United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. Sustainable Development Knowledge Platform. (n.d.). Available online at: https://sustainabledevelopment.un.org/post2015/transformingourworld/publication (Accessed October 26, 2023).
3. Singh S, Darroch JE, Vlassoff M, Nadeau J. Adding it up: The Benefits of Investing in Sexual and Reproductive Health Care. Report. New York: The Alan Guttmacher Institute (2003).
4. Ezeh A, Bankole A, Cleland J, García-Moreno C, Temmerman M, Ziraba AK. Burden of reproductive ill health. Disease Control Priorities, Third Edition (Volume 2): Reproductive, Maternal, Newborn, and Child Health. Washington, DC: The International Bank for Reconstruction and Development/The World Bank (2016). p. 25–50. doi: 10.1596/978-1-4648-0348-2_CH2
5. Johnson N. Comprehensive sexual health assessments for adolescents. Paediatr Child Health. (2020) 25(8):551–551. doi: 10.1093/PCH/PXAA122
6. Todd N, Black A. Contraception for adolescents. J Clin Res Pediatr Endocrinol. (2020) 12(Suppl 1):28. doi: 10.4274/JCRPE.GALENOS.2019.2019.S0003
7. Burkman RT, Dardano KL. Use of oral contraceptives for contraception. Prin Gender-Spec Med. (2004) 2:889–98. doi: 10.1016/B978-012440905-7/50354-6
8. Polis C, Bradley SEK, Bankole A, Onda T, Croft TN, Singh S. Contraceptive Failure Rates in the Developing World: An Analysis of Demographic and Health Survey Data in 43 Countries. New York: GUTTMACHER INSTITUTE (2016). Available online at: https://www.guttmacher.org/report/contraceptive-failure-rates-in-developing-world
9. Starrs AM, Ezeh AC, Barker G, Basu A, Bertrand JT, Blum R, et al. Accelerate progress—sexual and reproductive health and rights for all: report of the guttmacher–lancet commission. Lancet. (2018) 391(10140):2642–92. doi: 10.1016/S0140-6736(18)30293-9/ATTACHMENT/311D9C15-73F7-485F-A89D-907A407ADDE8/MMC1.PDF
10. Melesse DY, Mutua MK, Choudhury A, Wado YD, Faye CM, Neal S, et al. Adolescent sexual and reproductive health in sub-Saharan Africa: who is left behind? BMJ Global Health. (2020) 5(1):e002231. doi: 10.1136/BMJGH-2019-002231
11. Ninsiima LR, Chiumia IK, Ndejjo R. Factors influencing access to and utilisation of youth-friendly sexual and reproductive health services in sub-Saharan Africa: a systematic review. Reprod Health. (2021) 18(1):135. doi: 10.1186/S12978-021-01183-Y/TABLES/1
12. Morris JL, Rushwan H. Adolescent sexual and reproductive health: the global challenges. Int J Gynaecol Obstet. (2015) 131(Suppl 1):S40–42. doi: 10.1016/J.IJGO.2015.02.006
13. Mchome Z, Richards E, Nnko S, Dusabe J, Mapella E, Obasi A. A ‘mystery client’ evaluation of adolescent sexual and reproductive health services in health facilities from two regions in Tanzania. PLoS One. (2015) 10(3):e0120822. doi: 10.1371/JOURNAL.PONE.0120822
14. Sully EA, Biddlecom A, Darroch JE, Riley T, Ashford LS, Lince-Deroche N, et al. Adding it up: investing in sexual and reproductive health 2019. Report. New York: Guttmarcher Institute (2020) Available online at: https://www.guttmacher.org/report/adding-it-up-investing-in-sexual-reproductive-health-2019 (Accessed March 3, 2022).
15. World Health Organization. Reproductive Health and Research, and World Health Organization. Medical Eligibility Criteria for Contraceptive Use. Geneva: WHO Press, World Health Organization (n.d.) 268.
16. Tsui AO, Brown W, Li Q. Contraceptive practice in sub-Saharan Africa. Popul Dev Rev. (2017) 43(Suppl Suppl 1):166. doi: 10.1111/PADR.12051
17. Haberland N, Rogow D. Sexuality education: emerging trends in evidence and practice. J Adolesc Health. (2015) 56(1):S15–21. doi: 10.1016/J.JADOHEALTH.2014.08.013
18. Haberland NA. The case for addressing gender and power in sexuality and HIV education: a comprehensive review of evaluation studies. Int Perspect Sex Reprod Health. (2015) 41(1):31–42. doi: 10.1363/4103115
19. Denno DM, Hoopes AJ, Chandra-Mouli V. Effective strategies to provide adolescent sexual and reproductive health services and to increase demand and community support. J Adolesc Health. (2015) 56(1 Suppl):S22–41. doi: 10.1016/J.JADOHEALTH.2014.09.012
21. Chandra-Mouli V, Lane C, Wong S. What does not work in adolescent sexual and reproductive health: a review of evidence on interventions commonly accepted as best practices. Glob Health Sci Pract. (2015) 3(3):333–40. doi: 10.9745/GHSP-D-15-00126
22. Thomée S, Malm D, Christianson M, Hurtig AK, Wiklund M, Waenerlund AK, et al. Challenges and strategies for sustaining youth-friendly health services — a qualitative study from the perspective of professionals at youth clinics in Northern Sweden. Reprod Health. (2016) 13(1):1–13. doi: 10.1186/S12978-016-0261-6
23. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. (2018) 169(7):467–73. doi: 10.7326/M18-0850
24. O’Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol. (2014) 67(1):56–64. doi: 10.1016/J.JCLINEPI.2013.08.005
25. Petticrew M, Roberts H. Systematic reviews in the social sciences: a practical guide. Syst Rev Soc Sci: A Prac Guide. (2008) 1:1–336. doi: 10.1002/9780470754887
26. RoB 2: A Revised Cochrane Risk-of-Bias Tool for Randomized Trials | Cochrane Bias. (n.d.). Available online at: https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials (Accessed July 27, 2021).
27. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Br Med J. (2016) 355:i4919. doi: 10.1136/BMJ.I4919
28. Edelman A, Taylor J, Ovseiko PV, Topp SM. The role of academic health centres in building equitable health systems: a systematic review protocol. BMJ Open. (2017) 7(5):e015435. doi: 10.1136/BMJOPEN-2016-015435
29. Morgan G, Kanesathasan A, Akiode A. Effects of a community-based program on voluntary modern contraceptive uptake among young first-time parents in Cross River State, Nigeria. Glob Health Sci Pract. (2020) 8(4):783–98. doi: 10.9745/GHSP-D-20-00111
30. Levy M, Duffy M, Pearson J, Akuno J, Oduong S, Yemaneberhan A, et al. Health and social outcomes of HIV-vulnerable and HIV-positive pregnant and post-partum adolescents and infants enrolled in a home visiting team programme in Kenya. Trop Med Int Health. (2021) 26(6):640–48. doi: 10.1111/TMI.13568
31. Yakubu I, Garmaroudi G, Sadeghi R, Tol A, Yekaninejad MS, Yidana A. Assessing the impact of an educational intervention program on sexual abstinence based on the health belief model amongst adolescent girls in Northern Ghana, a cluster randomised control trial. Reprod Health. (2019) 16(1):124. doi: 10.1186/S12978-019-0784-8
32. Wondimagegene YA, Debelew GT, Koricha ZB. Effectiveness of peer-led education intervention on contraceptive use, unmet need and demand among secondary school adolescents in Gedeo Zone, South Ethiopia. A study protocol for cluster randomized controlled trial. Clin Epidemiol Glob Health. (2023) 21:101289. doi: 10.1016/J.CEGH.2023.101289
33. Gichangi P, Gonsalves L, Mwaisaka J, Thiongo M, Habib N, Waithaka M, et al. Busting contraception myths and misconceptions among youth in Kwale County, Kenya: results of a digital health randomised control trial. BMJ Open. (2022) 12(1). doi: 10.1136/BMJOPEN-2020-047426
34. Silverman JG, Brooks MI, Aliou S, Johns NE, Challa S, Nouhou AM, et al. Effects of the reaching married adolescents program on modern contraceptive use and intimate partner violence: results of a cluster randomized controlled trial among married adolescent girls and their husbands in Dosso, Niger. Contracept Reprod Med. (2023) 20(1). doi: 10.1186/S12978-023-01609-9
35. Nuwamanya E, Nalwanga R, Nuwasiima A, Babigumira JU, Asiimwe FT, Babigumira JB, et al. Effectiveness of a mobile phone application to increase access to sexual and reproductive health information, goods, and services among university students in Uganda: a randomized controlled trial. Contraception and Reproductive Medicine. (2020) 5(1). doi: 10.1186/S40834-020-00134-5
36. Erhardt-Ohren B, Brooks M, Aliou S, Osseni AA, Oumarou A, Challa S, et al. Sustained impact of community-based interventions on contraceptive use among married adolescent girls in Rural Niger: results from a cluster randomized controlled trial. Int J Gynaecol Obstet. (2023) 160(2):468–75. doi: 10.1002/IJGO.14378
37. Lemani C, Tang JH, Kopp D, Phiri B, Kumvula C, Chikosi L, et al. Contraceptive uptake after training community health workers in couples counseling: a cluster randomized trial. PLoS One. (2017) 12(4):e0175879. doi: 10.1371/JOURNAL.PONE.0175879
38. Fikree FF, Abshiro WK, Mai MM, Hagos KL, Asnake M. Strengthening youth friendly health services through expanding method choice to include long-acting reversible contraceptives for Ethiopian youth. Afr J Reprod Health. (2017) 21(3):37–48. doi: 10.29063/AJRH2017/V21I3.3
39. Wolf HT, Teich HG, Halpern-Felsher BL, Murphy RJ, Anandaraja N, Stone J, et al. The effectiveness of an adolescent reproductive health education intervention in Uganda. Int J Adolesc Med Health. (2017) 29(2). doi: 10.1515/IJAMH-2015-0032
40. Makenzius M, Loi UR, Otieno B, Oguttu M. A stigma-reduction intervention targeting abortion and contraceptive use among adolescents in Kisumu County, Kenya: a quasi-experimental study. Sex Reprod Health Matters. (2023) 31(1):1–18. doi: 10.1080/26410397.2021.1881208
41. Akuiyibo S, Anyanti J, Idogho O, Piot S, Amoo B, Nwankwo N, et al. Impact of peer education on sexual health knowledge among adolescents and young persons in two North Western States of Nigeria. Reprod Health. (2021) 18(1). doi: 10.1186/S12978-021-01251-3
42. Fikree FF, Abshiro WK, Mai MM, Hagos KL, Asnake M. The effect of peer education in dispelling myths and misconceptions about long-acting reversible contraception among Ethiopian youth. Afr J Reprod Health. (2018) 22(3):90–9. doi: 10.29063/AJRH2018/V22I3.10
43. WHO Health Organization. Using lay health workers to improve access to key maternal and newborn health interventions [Internet]. Technical Report. Geneva: WHO Press (2013). Available online at: https://www.who.int/publications/i/item/WHO-RHR-13.09 (Accessed April 10, 2024).
44. Malkin M, Mickler AK, Ajibade TO, Coppola A, Demise E, Derera E, et al. Adapting high impact practices in family planning during the COVID-19 pandemic: experiences from Kenya, Nigeria, and Zimbabwe. Glob Health Sci Pract. (2022) 10(4):e2200064. doi: 10.9745/GHSP-D-22-00064
45. Brooks MI, Johns NE, Quinn AK, Boyce SC, Fatouma IA, Oumarou AO, et al. Can community health workers increase modern contraceptive use among young married women? A cross-sectional study in Rural Niger. Reprod Health. (2019) 16:38. doi: 10.1186/S12978-019-0701-1
46. Scull T, Malik C, Morrison A, Keefe E. Promoting sexual health in high school: a feasibility study of A web-based media literacy education program. J Health Commun. (2021) 26(3):147–60. doi: 10.1080/10810730.2021.1893868
47. Gaughran M, Asgary R. On-Site comprehensive curriculum to teach reproductive health to female adolescents in Kenya. J Womens Health (Larchmt). (2014) 23(4):358–64. doi: 10.1089/JWH.2013.4523
48. Hegdahl HK, Musonda P, Svanemyr J, Zulu JM, Grønvik T, Jacobs C, et al. Effects of economic support, comprehensive sexuality education and community dialogue on sexual behaviour: findings from a cluster-RCT among adolescent girls in Rural Zambia. Soc Sci Med. (2022) 306:115–25. doi: 10.1016/J.SOCSCIMED.2022.115125
49. Almeida N, Teixeira A, Garcia J, Martins N, Ramalho C. Effects of an educational intervention on Angolan adolescents’ knowledge of human reproduction: a quasi-experimental study. Int J Environ Res Public Health. (2019) 16(24):5155. doi: 10.3390/IJERPH16245155
50. Munea AM, Alene GD, Debelew GT. Does youth-friendly service intervention reduce risky sexual behavior in unmarried adolescents? A comparative study in West Gojjam Zone, Northwest Ethiopia. Risk Manag Healthc Policy. (2020) 13:941–54. doi: 10.2147/RMHP.S254685
51. Oberth G, Chinhengo T, Katsande T, Mhonde R, Hanisch D, Kasere P, et al. Effectiveness of the Sista2Sista programme in improving HIV and other sexual and reproductive health outcomes among vulnerable adolescent girls and young women in Zimbabwe. J Adolesc Heal. (2021) 20(2):158–64. doi: 10.2989/16085906.2021.1918733
52. Rosenberg NE, Bhushan NL, Vansia D, Phanga T, Maseko B, Nthani T, et al. Comparing youth-friendly health services to the standard of care through ‘girl power-Malawi’: a quasi-experimental cohort study. J Acquir Immune Defic Syndr. (2018) 79(4):458–66. doi: 10.1097/QAI.0000000000001830
53. Annor C, Alatinga KA, Abiiro GA. Reproductive health services reproductive health corner knowledge of reproductive health services use of reproductive health services adolescents Ghana. Sex Reprod Healthc. (2021) 27. doi: 10.1016/j.srhc.2020.100583
54. Mbizvo MT, Kasonda K, Muntalima NC, Rosen JG, Inambwae S, Namukonda ES, et al. Comprehensive sexuality education linked to sexual and reproductive health services reduces early and unintended pregnancies among in-school adolescent girls in Zambia. BMC Public Health. (2023) 23(1). doi: 10.1186/S12889-023-15023-0
55. Bhushan NL, Fisher EB, Gottfredson NC, Maman S, Speizer IS, Phanga T, et al. The mediating role of partner communication on contraceptive use among adolescent girls and young women participating in a small-group intervention in Malawi: a longitudinal analysis. Glob Public Health. (2021) 17(7):1392–405. doi: 10.1080/17441692.2021.1924823
56. Mack N, Crawford TJ, Guise J, Chen M, Grey TW, Feldblum PJ, et al. Strategies to improve adherence and continuation of shorter-term hormonal methods of contraception. Cochrane Database Syst Rev. (2019) 2019(4). doi: 10.1002/14651858.CD004317.PUB5
57. Bakesiima R, Beyeza-Kashesya J, Tumwine JK, Chalo RN, Gemzell-Danielsson K, Cleeve A, et al. Effect of peer counselling on acceptance of modern contraceptives among female refugee adolescents in northern Uganda: a randomised controlled trial. Cochrane Database Syst Rev. (2021) 16(9):e0256479. doi: 10.1371/JOURNAL.PONE.0256479
58. Palmer MJ, Henschke N, Bergman H, Villanueva G, Maayan N, Tamrat T, et al. Targeted client communication via mobile devices for improving maternal, neonatal, and child health. Cochrane Database Syst Rev. (2020) 2020(8). doi: 10.1002/14651858.CD013679
59. Pattnaik A, Mohan D, Chipokosa S, Wachepa S, Katengeza H, Misomali A, et al. Testing the validity and feasibility of using a mobile phone-based method to assess the strength of implementation of family planning programs in Malawi. BMC Health Serv Res. (2020) 20(1):1–9. doi: 10.1186/S12913-020-5066-1
60. Smith C, Gold J, Ngo TD, Sumpter C, Free C. Mobile phone-based interventions for improving contraception use. Cochrane Database Syst Rev. (2015) 2017:CD011159. doi: 10.1002/14651858.CD011159.PUB2
61. Sharma A, Mwamba C, Ng’andu M, Kamanga V, Mendamenda MZ, Azgad Y, et al. Pilot implementation of a user-driven, web-based application designed to improve sexual health knowledge and communication among young Zambians: mixed methods study. J Med Internet Res. (2022) 24(7):e37600. doi: 10.2196/37600
62. Macharia P, Pérez-Navarro A, Sambai B, Inwani I, Kinuthia J, Nduati R, et al. An unstructured supplementary service data-based MHealth app providing on-demand sexual reproductive health information for adolescents in Kibra, Kenya: randomized controlled trial. JMIR Mhealth Uhealth. (2022) 10(4). doi: 10.2196/31233
63. Chang W. Decision-Making Power for Women and Girls: Evaluating Interventions in Sexual and Reproductive Health in Sub-Saharan AFRICA (Thesis/dissertation, North Carolina). Dissertation/thesis number: 27997606. Chapel Hill: The University of North Carolina (2020).
64. Gichane MW, Wamoyi J, Atkins K, Balvanz P, Maman S, Majani E, et al. The influence of cash transfers on engagement in transactional sex and partner choice among adolescent girls and young women in Northwest Tanzania. Contracept Reprod Med. (2020) 24(1):1–15. doi: 10.1080/13691058.2020.1811890
65. Stead M, Angus K, Langley T, Katikireddi V, Hinds K, Hilton S, et al. Mass media to communicate public health messages in six health topic areas: a systematic review and other reviews of the evidence. (Public Health Research, No. 7.8.) Scientific summary. Southampton (UK): NIHR Journals Library (2019). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK540700/
66. Ahmed M, Seid A. Association between exposure to mass media family planning messages and utilization of modern contraceptive among urban and rural youth women in Ethiopia. International Journal of Women’s Health. (2020) 12:719–29. doi: 10.2147/IJWH.S266755
67. Sserwanja Q, Sepenu AS, Mwamba D, Mukunya D. Access to mass media and teenage pregnancy among adolescents in Zambia: a national cross-sectional survey. BMJ Open. (2022) 12:52684. doi: 10.1136/bmjopen-2021-052684
68. Chimbindi N, Mthiyane N, Chidumwa G, Zuma T, Dreyer J, Birdthistle I, et al. Evaluating use of mass-media communication intervention ‘MTV-shuga’ on increased awareness and demand for HIV and sexual health services by adolescent girls and young women in South Africa: an observational study. BMJ Open. (2023) 13(5):e062804. doi: 10.1136/BMJOPEN-2022-062804
69. Sserwanja Q, Turimumahoro P, Nuwabaine L, Kamara K, Musaba MW. Association between exposure to family planning messages on different mass media channels and the utilization of modern contraceptives among young women in Sierra Leone: insights from the 2019 Sierra Leone demographic health survey. BMC Womens Health. (2022) 22(1). doi: 10.1186/s12905-022-01974-w
70. Oringanje C, Meremikwu MM, Eko H, Esu E, Meremikwu A, Ehiri JE. Interventions for preventing unintended pregnancies among adolescents. Cochrane Database Syst Rev. (2016) 2016:2. doi: 10.1002/14651858.CD005215.PUB3/MEDIA/CDSR/CD005215/IMAGE_T/TCD005215-CMP-005-04.XXX
71. Chin HB, Sipe TA, Elder R, Mercer SL, Chattopadhyay SK, Jacob V, et al. The effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections: two systematic reviews for the guide to community preventive services. Am J Prev Med. (2012) 42(3):272–94. doi: 10.1016/J.AMEPRE.2011.11.006
72. Chandra-Mouli V, McCarraher DR, Phillips SJ, Williamson NE, Hainsworth G. Contraception for adolescents in low and middle income countries: needs, barriers, and access. Reprod Health. (2014) 11(1):1–8. doi: 10.1186/1742-4755-11-1/TABLES/2
73. Kesterton AJ, De Mello MC. Generating demand and community support for sexual and reproductive health services for young people: a review of the literature and programs. Reprod Health. (2010) 7(1):1–12. doi: 10.1186/1742-4755-7-25
74. Reproductive Health Policies 2017: Data Booklet | Population Division. (n.d.). Available online at: https://www.un.org/development/desa/pd/content/reproductive-health-policies-2017-data-booklet (Accessed January 18, 2024).
75. Solo J, Festin M. Provider bias in family planning services: a review of its meaning and manifestations. Glob Health Sci Pract. (2019) 7(3):371–85. doi: 10.9745/GHSP-D-19-00130
76. WHO Consolidated Guideline on Self-Care Interventions for Health. WHO Consolidated Guideline on Self-Care Interventions for Health: Sexual and Reproductive Health and Rights (2019). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK544164/
77. Aboagye RG, Ahinkorah BO, Seidu AA, Adu C, Hagan JE, Amu H, et al. Mass media exposure and safer sex negotiation among women in sexual unions in sub-Saharan Africa: analysis of demographic and health survey data. Behav Sci (Basel). (2021) 11(5):63. doi: 10.3390/BS11050063
78. Silva M, Loll D, Ezouatchi R, Kassegne S, Hugues Y R, Nagbe LB, et al. Evaluating a youth-designed sexual and reproductive health mass and social media campaign in côte d’Ivoire: triangulation of three independent evaluations. Sex Reprod Health Matters. (2023) 31(1). doi: 10.1080/26410397.2023.2248748
Keywords: sexual and reproductive health, young people, adolescents, contraception, family planning, sub-Saharan Africa
Citation: Chipako I, Singhal S and Hollingsworth B (2024) Impact of sexual and reproductive health interventions among young people in sub-Saharan Africa: a scoping review. Front. Glob. Womens Health 5:1344135. doi: 10.3389/fgwh.2024.1344135
Received: 25 November 2023; Accepted: 29 March 2024;
Published: 18 April 2024.
Edited by:
Negussie Boti Sidamo, Arba Minch University, EthiopiaReviewed by:
Bilcha Oumer, Arba Minch University, EthiopiaTadele Dana Darebo, Wolaita Sodo University, Ethiopia
© 2024 Chipako, Singhal and Hollingsworth. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Isaac Chipako aS5jaGlwYWtvQGxhbmNhc3Rlci5hYy51aw==; aWNoaXBha0B5YWhvby5jby51aw==
 Isaac Chipako
Isaac Chipako Saurabh Singhal2
Saurabh Singhal2