
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Glob. Womens Health, 17 June 2024
Sec. Maternal Health
Volume 5 - 2024 | https://doi.org/10.3389/fgwh.2024.1342687
This article is part of the Research TopicInfluence of Intimate Partner Violence and Male Partner Involvement in Maternity Care in Low-and-Middle Income CountriesView all 8 articles
Background: Husbands are the primary decision-makers about the place of childbirth. Lack of husbands' support for maternal health care is associated with low maternal waiting home utilization and less is known about the husbands' intention to support their wife's use of maternal waiting homes (MWHs) and underlying beliefs in Ethiopia. This community-based cross-sectional survey aimed to study husbands' intention to support during pregnancy through the use of maternity waiting homes in Jimma Zone, Southwest Ethiopia.
Method: A cross-sectional study was conducted among 396 randomly selected husbands whose wives were pregnant. Interviewer-administered, a structured questionnaire developed based on the Theory of Planned Behavior (TPB) was used to collect the data. Multivariable logistic regression analyses were used to examine the association between behavioral intention and constructs of the theory of planned behavior.
Results: Of the 396 husbands who took part in the study, 42.7% intend to support their partner's use of a maternity waiting home. Intention to support a wife to use a maternity waiting home was associated with subjective norm [AOR = 1.303, 95% CI (1.054, 1.611)] and perceived behavioral control [AOR = 1.446, 95% CI (1.234, 1.695)]. Among the control beliefs, “having childcare”; “having a person who stays with a wife at a maternity waiting home”; and “availability of quality service provided to a wife in the maternity waiting home” significantly separated intenders and non-intenders.
Conclusion: The findings suggest that husbands who perceived more social pressure and felt in control of barriers were more likely to intend to support their partner in using a maternity waiting home. Intervention should focus on underlying normative and control beliefs to improve the husband's intention.
Ethiopia has adopted a variety of policies, including maternal waiting homes (MWH), to minimize maternal mortality (1). In MWH, community-based shelters housed by the health center or hospital, pregnant women remain until birth in the last trimester. It is an integral component of a holistic package aimed at overcoming the second delay (2). In recent years, the government of Ethiopia has established a range of health facilities to increase access to health care for people living in rural areas (3). While there is a difference between countries, more than half of the health facilities have MWH (4).
MWHs play an important role in reducing preventable maternal mortality and negative pregnancy outcomes (5, 6). Studies in Ethiopia also found MWH use accounted for 92% (0.04–0.19) reduction in maternal mortality, 83% (0.05–0.58) (9.90–11.4) reduction of stillbirth, and was associated with a lower rate of direct obstetric complications (5, 6). Despite its effectiveness in minimizing maternal mortality and adverse pregnancy effects, the use of MWH in Ethiopia is very limited. In a recent survey, it was found that only 7% of women used MWH (7). Studies also recorded that the shortage of service and transport infrastructure had a negative effect on MWH use (8–12). Many studies have identified individual and community-related influences; such as lack of awareness and limited husband supports in MWH (13, 14).
In a patriarchal society, the position of the husband goes beyond offering financial assistance to the family; they are the ones who determine where to give birth and seek care (15–17). Husbands' involvement in helping women in reproductive health care has been linked with improved maternal health benefits and better birth outcomes (18–20). The participation of husbands in maternal and infant health care has been advocated as a method to increase the use of maternal health services (21). However, studies in Ethiopia (22, 23) and other sub-Saharan African countries such as Ghana (24) Nigeria (17) and Uganda (25) have shown that husbands participate in maternal health care by assisting their wives in the use of maternal health facilities such as facility-based childbirth, but this participation remains limited.
Studies of factors that affect the engagement of husbands in MWHs have identified various factors that range from context to context. For example, studies in Liberia recorded a lack of food and respectful treatment among MWHs (9, 10). On the other hand, a study in Northern Sierra Leone showed that social and cultural traditions, lack of interest, engagement in other events, distance, and the nature of health facilities are obstacles to the participation of men (8).
Similarly, qualitative research with husbands in Zambia recorded that poor MWH conditions (e.g., lack of room, bedding, water, and sanitation facilities) and the lack of anyone to look after children at home were affected by husbands' decisions to let their wives use MWHs (26). The most prominent quotes from this study are as follows: “Empowering mothers, men, and families to recognize maternal health threats during pregnancy and to take responsibility for designing and enforcing effective responses to them” is a key measure implemented by the Ethiopian Federal Ministry of Health to reduce maternal deaths (27).
Husbands are the main decision-makers in a maternity place, with or without the presence of a mother. The wife hardly gives birth at health facilities without the assistance of her husband (15, 28, 29). Help for maternal health care by the husband may take various forms, such as enabling or promoting the use of resources, providing financial and emotional support, accompanying facilities, and joint decision-making on the place of delivery (30). The lack of support or consent for a husband was a cause for home delivery in recent studies in Ethiopia (16, 28, 29). These results underscored the need to examine the reasons behind the husbands' behavioral intention to plan intervention. However, in Ethiopia, no studies have investigated the intention of spouses, predictors of intent, and attitudes relevant to endorsing the use of MWHs, a portal to facility-based childbirth (22, 23).
Understanding the behavioral intention and the underlying causes will inform action aimed at increasing maternal healthcare use through the involvement of the husband (31). According to the Theory of Planned Behavior (TPB), intent (readiness to execute a given behavior) is the key determinant of behavior. Whereas the intention is the role of the behavioral attitude, the subjective norm, and the perceived behavioral influence. Thus, the desire to conduct a safe action is based on a constructive appraisal of the action, a belief that the referents approve of the action, and a sense of the power of the obstacles and the facilitators of the action (31, 32).
TPB assumes that attitude, subjective norm, and perceived behavioral control are determined by silent beliefs. Attitude is determined by behavioral belief and evaluation of outcome. Normative belief and motivation to comply with referents' expectations determine the subjective norm. Similarly, perceived behavioral control determines control beliefs (beliefs about factors that facilitate or hinder action) and the power of these factors to facilitate or impede acting. The theory proposes that these beliefs influence intention through their corresponding construct (32).
TPB enables the identification of predictors of behavioral intention and underlying beliefs that inform interventions to change or modify behavior. Thus, we undertook this study using the theory of planned behavior as a framework to explore predictors of husbands' intention to support wives' use of MWH and to identify underlying beliefs. TPB allows the recognition of behavioral goal predictors and core values that inform action to alter or improve behavior. We have therefore conducted this analysis using the TPB as a basis for examining the predictors of the husband's role in increasing the intention and the uptake of MWHs among pregnant women.
A community-based cross-sectional study was undertaken in three randomly selected districts of the Jimma zone (Manna, Kersa, and Seka Chekorsa). The Jimma Zone is located in the western part of Ethiopia. The zone had 121 public health centers, 5 public hospitals, and 512 public health posts at the time of the study. We conducted the study from February 20 through 30, 2019.
The study populations were husbands whose wives were pregnant and living in the selected districts during the study period.
The sample size of 429 was calculated by Epi Info™ 7.1.5.2 based on the size of the population of husbands who have a pregnant wife (800), a 95% confidence level, the proportion of husbands who intend to support their wives using MWH (50%), a 0.05% margin of error, a design effect of 1.5 to account for the heterogeneity between clusters, and 10% non-response.
Three districts were selected randomly from the districts with MWH coverage of 50% and above, i.e., the percentage of health centers accompanied by MWH as contingent maternity care provision centers. During the study period, out of 21 districts in the zone, 10 had 50% or higher coverage. We obtained a list of husbands with pregnant wives from the catchment areas with functional MWHs in the chosen districts through the assistance of health extension workers. The sample size for each area was determined based on the proportion of the eligible husband population within that specific location. Utilizing this compiled list as a sampling frame, the study participants were selected using a simple random sampling technique to ensure a fair representation of the population in the study.
We developed the instrument based on the TPB manual's suggestion (31): we conducted a qualitative elicitation study in the Gomma district among 20 husbands who had a pregnant wife to explore beliefs salient to support MWH service utilization. Open-ended questions were used to identify behavioral, normative, and control beliefs held by participants about supporting their partner to use MWH for their current pregnancy. The assessment produced eight, six, and seven major behavioral beliefs, normative, and control beliefs, respectively. Subsequently, the beliefs were used to develop belief-based indicators of intention. Finally, behavioral, normative, and control beliefs were weighted by corresponding values of evaluation of beliefs, motivation to comply, and power of the controls. The direct measure assessed four constructs of TPB: intention assessed through five items [Cronbach's alpha (α) = 0.88]; attitude measured with four items [Cronbach's alpha (α) = 0.89]; subjective norms measured with four items [Cronbach's alpha (α) = 0.83]; perceived behavioral control measured with four items [Cronbach's alpha (α) = 0.72]. All direct measures were finally assessed using five-point bipolar adjectives.
Data were collected using a structured questionnaire administered by an interviewer. The questionnaire was first developed in English. The English version of the questionnaire was translated into Afan Oromo and back-translated into English by an expert who is fluent in both languages to ensure consistency between the two versions. Pretesting of the Afan Oromo version of the tool was done among 21 eligible respondents in another district who share common characteristics with study participants. The questionnaire underwent significant changes to the subjective norm and perceived behavioral control items following the pretesting results. The wording was adjusted for clarity, and the questionnaire was then administered in Afan Oromo after modifying some words.
SPSS (version 20.0) was used to conduct statistical analysis. Descriptive statistics such as frequency, mean, standard deviation, and percentage were used to express categorical variables. The independent variables were age, educational status, occupation, past experience, religion, residence, direct attitude, subjective norm, and perception of control. For categorical variables, we conducted bivariate and multivariate logistic regression analyses to look at the association between independent variables and behavioral intention. A P-value of less than 0.05 was considered statistically significant. For continuous variables, we conducted bivariate correlations between direct and indirect measures of TPB using Spearman correlations with P < 01 and P < 05.
Sociodemographic data for our participants are summarized in Table 1. A total of 429 husbands had been assessed for eligibility, out of which 396 participated in this study, for a response rate of 92%. The mean age of the study participants is 33.07 (±4.76 SD), and approximately two-thirds (68.5%) of the participants are aged 20 to 39 years. The majority of the participants are Muslims (94.2%). Those who had a formal education are 4.5%. It is revealed that most of the respondents involved in the study are farmers (94.2%). Besides, 85.1% of respondents showed their wife had been pregnant before the current pregnancy, and 46% of them reported health facility delivery.
Almost all (99%) of the respondents heard of maternity waiting homes. Regarding the source of information, family members (66.2%) were the most mentioned source, followed by the media and friends. When asked about the right time to visit MWH for childbirth, only 35.9% reported 14 days before the expected delivery date. More than half (51.3%) of respondents identified seven days before the expected delivery date as the right time to visit MWH. The mean score for knowledge was 1.80 as listed in Table 2.
In the sampled population, 85.1% reported that their partner or wife had ever given birth, while 14.9% revealed that their partner got pregnant for the first time. In response to questions related to the place where their partner gave birth during the previous pregnancy, 45.4% reported delivery in a health facility, and 54.6% reported home delivery. Sixty-seven percent of participants stated that the distance between their home and MWH is over five kilometres.
Direct attitude, subjective norm, and perceived behavioral control had a mean score of 16.53 (SD ± 2.12), 14.13 (SD ± 2.23), and 14.23 (SD ± 3.39), respectively. The mean score of intention was 11.76 (SD ± 3.60). Intention is categorized based on the mean score as intended (scored above the mean score) and non-intenders (scored below the median score). Among all respondents, nearly forty-three percent (42.7%) of them intend to provide support (Table 3).
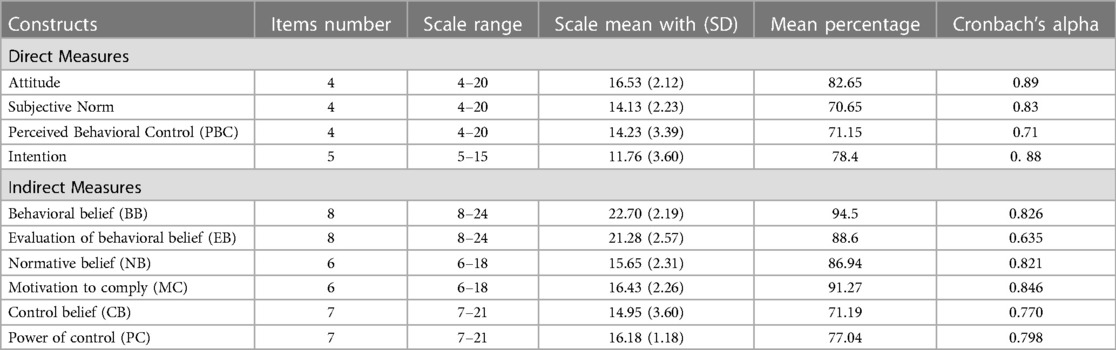
Table 3 Descriptive statistics of responses for the indirect and direct measures of TPB, jimma, Ethiopia (n = 396), 2019.
Based on the correlation analysis, all indirect measures positively correlated with their corresponding direct measures, which confirms the validity of the indirect measures. Indirect attitude correlated with direct attitude (r = 0.187, P < 0.001), a moderate correlation was observed between indirect subjective norm and direct subjective norm (r = 0.432, P < 0.001), and indirect PBC correlated with direct PBC (r = 0.350, P < 0.001) (Table 4).
In the multiple regression analysis, perceived behavioral control (PBC) and subjective norm were positively associated with the husband's intention to support. For each unit increase in perception of control, participants had a 44.6% higher likelihood of intention to support their wives by using maternity waiting homes [AOR = 1.446, 95% CI (1.234, 1.695)]. Likewise, a unit increase in the subjective norm increases the likelihood of intending to support a wife to use a maternity waiting home [AOR = 1.303, 95% CI (1.054, 1.611)] (Table 5).
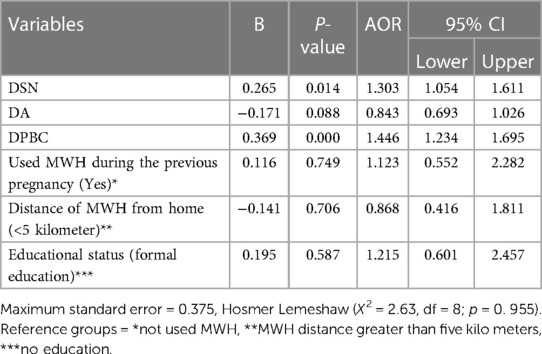
Table 5 Multivariable logistic regression model predicting husband intention to support wife to sue MWH, jimma zone, Ethiopia. (N = 396), 2019.
We have conducted further analysis to identify beliefs that had the greatest influence on intentions. We did not conduct research on beliefs underlying attitude because attitude was not significantly associated with intention in multiple logistic regression. All normative beliefs were significantly correlated with intention, their correlations varying from only 0.16 to 0.31. Similarly, three control beliefs significantly correlated with intention: presence or absence of a person who looks after children at home (r = 0.37, P < 0.01); presence or absence of a person who cares for a wife at MWH (r = 0.36, P < 0.001); and quality of services provided in the MWH (r = 0.11, P < 0.01) (Table 6).
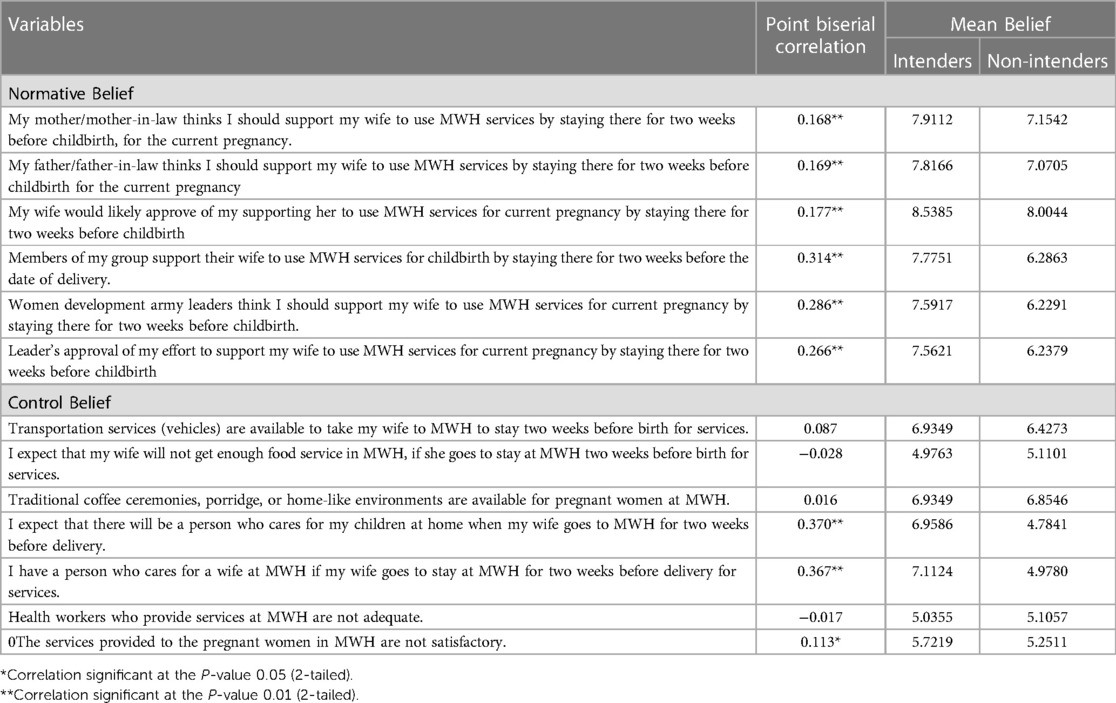
Table 6 Normative and control beliefs correlation with intention, jimma zone, southwest Ethiopia, 2019.
TPB can be utilized to change the husband's behavior and increase support for the utilization of MWHs. The TPB posits that behavioral intentions are influenced by three key factors: attitude toward the behavior, subjective norms, and perceived behavioral control. In this case, changing the husband's behavior to support the utilization of MWH would involve evaluating attitude toward this behavior, the influence of subjective norms, and perceived control over engaging in this supportive behavior.
This study examined psychological factors influencing the intention to support the wife in using MWH among husbands. The findings revealed that subjective norms and perceived behavior control were significantly associated with the intention to support the wife in using MWH. Forty-two percent of respondents reported that they intend to support their wives using MWH for their current pregnancy. In this study, we did not measure behavior, but the intention is assumed to be the immediate predictor of behavior (32, 33); thus, the low involvement of the husband in maternal health care reported in previous studies (22, 23) could be explained by low motivation. Given the high preventable maternal and child mortality in the country, improving husbands' intentions is crucial to reducing maternal mortality by increasing access to and utilization of maternal health services (19, 20).
In line with previous studies (7, 9), the respondents listed “medical attention” and “institutional delivery” when asked about the benefits of MWH. With regards to the time to visit the MWH, 12.8% of respondents did not know the right time. To avoid delays in utilizing MWHs, healthcare professionals must focus on raising awareness about the appropriate time to visit MWHs. This is crucial because an insufficient understanding of the ideal timing for seeking care can result in missed opportunities for receiving MWH services.
The bivariate analyses revealed that attitude towards supporting a partner to use maternal waiting services showed statistically significant associations with intention. However, when controlled for other variables, the association becomes non-significant. The essence of the behavior and study participants may be explained as follows: Traditional gender roles delineate pregnancy and childbirth-related issues for women (17, 34, 35). The tie of target behavior with social values and the collectivist nature of participants' culture may subdue personal feelings (36, 37).
In our study, subjective norms were positively associated with the intention to support the use of MWH by women. This has demonstrated that supporting the wife to use MWH was influenced by perceptions about what the others do and referents' approval of supporting the wife to use MWH. Previous studies also showed that social pressure is one factor that influences male involvement (35, 38). This finding highlights the importance of targeting social norms to improve husbands' intentions and practices related to supporting wives to use MWH. An intervention needs to address beliefs about the approval and practice of referents with factors in a broader social context to change social norms and increase intentions and related behavior (39).
Perception of control was another predictor of intention to support a wife using MWH among husbands. In an analysis aimed at identifying the beliefs that discriminate between intenders and non-intenders, only three control beliefs were found to have significant influence or discriminate between two groups: having someone who takes care of children at home, having a person who cares for a wife in MWH, and quality service at MWH.
Husbands are income earners in the family (35) and they may be busy with activities to support the family economically (25). This could lead them to perceive the absence or presence of a person who looks after children at home and a wife in MWH as a barrier or facilitator. Moreover, belief about the quality of services provided at MWH was mentioned as one factor. This finding is consistent with previous studies that reported a lack of space for men, the absence of health workers, and the lack of amenities as barriers (9, 11).
MWHs have become an important intervention in Ethiopia to improve maternal health outcomes. In addition to the expansion of MWHs, there are ongoing community-level promotions to create demand and engage the community. However, those who have used the services reported several limitations (7). This suggests the government and stakeholders need to improve the quality of services provided in the MWHs, as poor quality of service negatively affects maternal health service utilization (40, 41).
This study has the strength to note: (1) This study is the first to analyze the role of husbands in increasing MWH uptake; (2) the qualitative salient beliefs were explored and integrated into the beliefs dimensions for the quantitative study; and (3) a standard pretested structured questionnaire was used. However, this study has some potential shortcomings that should be noted: (1) First, only husbands whose wives were pregnant were included in the study. Thus, the results may not be inferred from the general population of male partners; (2) this study used data obtained from self-report that might be subjected to social desirability bias. We tried to minimize these issues by recruiting experienced interviewers, providing a brief overview of the study, and ensuring that their responses were not linked to them in any way. (3) The associations reported in this study were so correlational that we cannot make a causal link. Finally, we did not measure actual behavior and incorporated variables that predict intention, such as past behavior. Therefore, future research may extend this by measuring actual behavior.
The present research used TPB to determine psychological factors impacting the intention of husbands to support their wives in the utilization of MWH. The findings of the study indicated that the subjective norm and perceived behavioral control were associated with the intention to support MWH utilization.
In a study aimed at defining particular beliefs, all the normative beliefs and three control beliefs, such as having a person who looks after children in the home and a wife at MWH, and the quality of services provided at MWH, were separated between intenders and non-intenders. Ajzen suggests interventions aim to promote change in practice through intention and the need to target underlying beliefs (31, 32). Therefore, to increase the utilization of MWHs, interventions should focus on targeting both normative and control beliefs, particularly through the support of husbands. By addressing societal norms surrounding maternity care that may prevent women from utilizing the services, interventions have a higher likelihood of success in promoting MWH utilization. By involving husbands in the decision-making process and support, women may feel more empowered to access MWHs and ultimately improve their maternal health outcomes.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Ethical Review Board of Jimma University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
MA: Conceptualization, Data curation, Investigation, Methodology, Supervision, Validation, Writing – review & editing. AB: Methodology, Supervision, Validation, Visualization, Writing – review & editing. FA: Conceptualization, Funding acquisition, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. YL: Formal Analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AG: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Supervision, Validation, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors would like to thank Jimma University for financial support. The authors highly appreciate respondents for their contribution to the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, adjusted odd ratio; MWH, maternity waiting homes; TPB, theory of planned behavior; SD, standard deviation.
1. Gaym A, Pearson L, Soe KW. Maternity waiting homes in Ethiopia–three decades experience. Ethiop Med J. (2012) 50(3):209–19.23409404
2. World Health Organization. Maternity Waiting Homes: A Review of Experiences. Geneva: World Health Organization (1996).
4. Tiruneh GT, Getu YN, Abdukie MA, Eba GG, Keyes E, Bailey PE. Distribution of maternity waiting homes and their correlation with perinatal mortality and direct obstetric complication rates in Ethiopia. BMC Pregnancy Childbirth. (2019 Dec) 19(1):214. doi: 10.1186/s12884-019-2356-x
5. Dadi TL, Bekele BB, Kasaye HK, Nigussie T. Role of maternity waiting homes in the reduction of maternal death and stillbirth in developing countries and its contribution for maternal death reduction in Ethiopia: a systematic review and meta-analysis. BMC Health Serv Res. (2018) 18(1):748. doi: 10.1186/s12913-018-3559-y
6. Bekele BB, Dadi TL, Tesfaye T. The significant association between maternity waiting homes utilization and perinatal mortality in Africa: systematic review and meta-analysis. BMC Res Notes. (2019) 12(1):13. doi: 10.1186/s13104-019-4056-z
7. Kurji J, Gebretsadik LA, Wordofa MA, Sudhakar M, Asefa Y, Kiros G, et al. Factors associated with maternity waiting home use among women in jimma zone, Ethiopia: a multilevel cross-sectional analysis. BMJ Open. (2019) 9(8):e028210. doi: 10.1136/bmjopen-2018-028210
8. Kyokan M, Whitney-Long M, Kuteh M, Raven J. Community-based birth waiting homes in northern Sierra Leone: factors influencing women’s use. Midwifery. (2016) 39:49–56. doi: 10.1016/j.midw.2016.04.013
9. Lori JR, Wadsworth AC, Munro ML, Rominski S. Promoting access: the use of maternity waiting homes to achieve safe motherhood. Midwifery. (2013) 29(10):1095–102. doi: 10.1016/j.midw.2013.07.020
10. Lori JR, Munro ML, Rominski S, Williams G, Dahn BT, Boyd CJ, et al. Maternity waiting homes and traditional midwives in rural Liberia. Int J Gynaecol Obstet. (2013) 123(2):114–8. doi: 10.1016/j.ijgo.2013.05.024
11. Chibuye PS, Bazant ES, Wallon M, Rao N, Fruhauf T. Experiences with and expectations of maternity waiting homes in Luapula Province, Zambia: a mixed-methods, cross-sectional study with women, community groups and stakeholders. BMC Pregnancy Childbirth. (2018) 18(1):42. doi: 10.1186/s12884-017-1649-1
12. Scott NA, Vian T, Kaiser JL, Ngoma T, Mataka K, Henry EG, et al. Listening to the community: using formative research to strengthen maternity waiting homes in Zambia. PLoS One. (2018) 13(3):e0194535. doi: 10.1371/journal.pone.0194535
13. Mramba L, Nassir FA, Ondieki C, Kimanga D. Reasons for low utilization of a maternity waiting home in rural Kenya. Int J Gynaecol Obstet. (2010) 108(2):152. doi: 10.1016/j.ijgo.2009.08.029
14. Ruiz MJ, van Dijk MG, Berdichevsky K, Munguía A, Burks C, García SG. Barriers to the use of maternity waiting homes in indigenous regions of Guatemala: a study of users’ and community members’ perceptions. Cult Health Sex. (2013) 15(2):205–18. doi: 10.1080/13691058.2012.751128
15. Jalu MT, Ahmed A, Hashi A, Tekilu A. Exploring barriers to reproductive, maternal, child, and neonatal (RMNCH) health-seeking behaviors in the Somali region, Ethiopia. PLoS One. (2019) 14(3):e0212227. doi: 10.1371/journal.pone.0212227
16. Roro MA, Hassen EM, Lemma AM, Gebreyesus SH, Afework MF. Why do women not deliver in health facilities: a qualitative study of the community perspectives in south-central Ethiopia? BMC Res Notes. (2014) 7(1):556. doi: 10.1186/1756-0500-7-556
17. Sharma V, Leight J, Giroux N, AbdulAziz F, Nyqvist MB. “That’s a woman’s problem”: a qualitative analysis to understand male involvement in maternal and newborn health in Jigawa state, northern Nigeria. Reprod Health. (2019) 16(1):1–1. doi: 10.1186/s12978-018-0662-9
18. Daniele MA, Ganaba R, Sarrassat S, Cousens S, Rossier C, Drabo S, et al. Involving male partners in maternity care in Burkina Faso: a randomized controlled trial. Bull W H O. (2018) 96(7):450. doi: 10.2471/BLT.17.206466
19. Tokhi M, Comrie-Thomson L, Davis J, Portela A, Chersich M, Luchters S. Involving men to improve maternal and newborn health: a systematic review of the effectiveness of interventions. PLoS One. (2018) 13(1):e0191620. doi: 10.1371/journal.pone.0191620
20. Mullany BC, Becker S, Hindin MJ. The impact of including husbands in antenatal health education services on maternal health practices in urban Nepal: results from a randomized controlled trial. Health Educ Res. (2006) 22(2):166–76. doi: 10.1093/her/cyl060
21. World Health Organization. WHO recommendations on Health Promotion Interventions for Maternal and Newborn Health 2015. Geneva: World Health Organization (2015).
22. Baraki Z, Wendem F, Gerensea H, Teklay H. Husbands involvement in birth preparedness and complication readiness in Axum town, Tigray region, Ethiopia, 2017. BMC Pregnancy Childbirth. (2019) 19(1):180. doi: 10.1186/s12884-019-2338-z
23. Mersha AG. Male involvement in the maternal health care system: implication towards decreasing the high burden of maternal mortality. BMC Pregnancy Childbirth. (2018) 18(1):493. doi: 10.1186/s12884-018-2139-9
24. Saah FI, Tarkang EE, Komesuor J, Osei E, Acquah E, Amu H. Involvement of male partners in skilled birth care in the North Dayi district, Ghana. Int J Reprod Med. (2019) 2019:1–12. doi: 10.1155/2019/2852861
25. Muheirwe F, Nuhu S. Men’s participation in maternal and child health care in Western Uganda: perspectives from the community. BMC Public Health. (2019) 19(1):1–0. doi: 10.1186/s12889-019-7371-3
26. Sialubanje C, Massar K, Kirch EM, van der Pijl MS, Hamer DH, Ruiter RA. Husbands’ experiences and perceptions regarding the use of maternity waiting homes in rural Zambia. Int J Gynaecol Obstet. (2016) 133(1):108–11. doi: 10.1016/j.ijgo.2015.08.023
27. FMOH. The Federal Democratic Republic of Ethiopia Ministry of Health, National Reproductive Health Strategy 2006–2015. Addis Ababa: Ministry of Health (2006).
28. Mehretie Adinew Y, Abera Assefa N, Mehretie Adinew Y. Why do some Ethiopian women give birth at home after receiving antenatal care? Phenomenological study. BioMed Res Int. (2018) 2018:1–8. doi: 10.1155/2018/3249786
29. Yaya S, Bishwajit G, Uthman OA, Amouzou A. Why some women fail to give birth at health facilities: a comparative study between Ethiopia and Nigeria. PLoS One. (2018) 13(5):e0196896. doi: 10.1371/journal.pone.0196896
30. Yargawa J, Leonardi-Bee J. Male involvement and maternal health outcomes: systematic review and meta-analysis. J Epidemiol Community Health. (2015) 69(6):604–12. doi: 10.1136/jech-2014-204784
31. Francis J, Eccles MP, Johnston M, Walker AE, Grimshaw JM, Foy R, et al. Constructing Questionnaires Based on the Theory of Planned Behaviour: A Manual for Health Services Researchers. United Kingdom: City Research Online (2004).
32. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. (1991) 50(2):179–211. doi: 10.1016/0749-5978(91)90020-T
33. Rogers RW. Cognitive and psychological processes in fear appeals and attitude change: a revised theory of protection motivation. In: Cacioppo J, Petty R, editors. Social Psychophysiology: A Sourcebook. United States: Journal of Experimental Social Psychology (1983). p. 153–76.
34. Morgan R, Tetui M, Muhumuza Kananura R, Ekirapa-Kiracho E, George AS. Gender dynamics affecting maternal health and health care access and use in Uganda. Health Policy Plan. (2017) 32(suppl_5):v13–21. doi: 10.1093/heapol/czx011
35. Maluka SO, Peneza AK. Perceptions on male involvement in pregnancy and childbirth in Masasi District, Tanzania: a qualitative study. Reprod Health. (2018) 15(1):68. doi: 10.1186/s12978-018-0512-9
36. Zou X, Tam KP, Morris MW, Lee SL, Lau IY, Chiu CY. Culture as common sense: perceived consensus versus personal beliefs as mechanisms of cultural influence. J Pers Soc Psychol. (2009) 97(4):579. doi: 10.1037/a0016399
37. Tarhini A, Hone K, Liu X, Tarhini T. Examining the moderating effect of individual-level cultural values on users’ acceptance of E-learning in developing countries: a structural equation modeling of an extended technology acceptance model. Interact Learn Environ. (2017) 25(3):306–28. doi: 10.1080/10494820.2015.1122635
38. Aborigo RA, Reidpath DD, Oduro AR, Allotey P. Male involvement in maternal health: perspectives of opinion leaders. BMC Pregnancy Childbirth. (2018) 18(1):3. doi: 10.1186/s12884-017-1641-9
39. Cislaghi B, Heise L. Using social norms theory for health promotion in low-income countries. Health Promot Int. (2019) 34(3):616–23. doi: 10.1093/heapro/day017
40. Campbell J, DPhil WJ, Langer A, Calvert C, Campbell OM, Feigl AB, et al. Quality maternity care for every woman, everywhere: a call to action. Lancet. (2016) 388:2307–20. doi: 10.1016/S0140-6736(16)31333-2
Keywords: husband, maternity waiting home, supporting pregnant women, MWH, husband intention
Citation: Aman M, Bekele A, Abamecha F, Lemu YK and Gizaw AT (2024) Husband's intention to support during pregnancy for the use of maternity waiting home in Jimma Zone, Southwest, Ethiopia: a community-based cross-sectional study. Front. Glob. Womens Health 5:1342687. doi: 10.3389/fgwh.2024.1342687
Received: 29 November 2023; Accepted: 29 May 2024;
Published: 17 June 2024.
Edited by:
Daudet Tshiswaka, University of West Florida, United StatesReviewed by:
Adi Chereni, London Metropolitan University, United Kingdom© 2024 Aman, Bekele, Abamecha, Lemu and Gizaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abraham Tamirat Gizaw, YWJyaXNobnRhbWlyYXRAZ21haWwuY29t; YWJyYWhhbS50YW1pcmF0QGp1LmVkdS5ldA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.