- 1School of Midwifery, College of Health Sciences, Woldia University, Woldia, Ethiopia
- 2Department of Nursing, Bule Hora University Teaching Hospital, Bule Hora, Ethiopia
- 3Department of Public Health, Institute of Health, Bule Hora University, Bule Hora, Ethiopia
- 4School of Public Health, College of Health Sciences, Woldia University, Woldia, Ethiopia
- 5Department of Midwifery, Institute of Health, Bule Hora University, Bule Hora, Ethiopia
Background: Contraception use remains low in Ethiopia, particularly within the first year after childbirth. While some women might have medical conditions that limit their contraceptive options, the primary obstacle to wider family planning adoption is not a specific health problem. Instead, it is the lack of equitable access to high-quality family planning services. This barrier significantly hinders women's ability to make informed decisions about their reproductive health. This study examines postpartum family planning utilization and its associated factors among postpartum mothers in the Bule Hora District.
Methods: We conducted a community-based cross-sectional study. A multistage sampling technique was employed to recruit a total of 630 women who had given birth. To collect the data, structured, standardized, and pretested questionnaires were used, and the collected data were coded and entered into Epi-data version 4.6. The data were analyzed using SPSS version 25. Both bivariable and multivariable logistic regressions were used to identify factors associated with postpartum family planning utilization.
Results: The study found that 71.3% of women utilized postpartum family planning. Significant associations were found between postpartum family planning utilization and various factors, including counseling on family planning during pregnancy [adjusted odds ratio (AOR) = 1.79, 95% confidence interval (CI) 1.61–2.82], delivery (AOR = 2.62, 95% CI 1.56–4.38), and the postpartum period (AOR = 2.71, 95% CI 1.75–4.21). Women who resumed sexual activity after birth (AOR = 1.92, 95% CI 1.25–2.96), and who had at least four antenatal care visits (AOR = 3.09, 95% CI 1.61–5.92) were also more likely to use postpartum family planning. Women with grand multiparity were 69% less likely to use family planning methods than primiparous women (AOR = 0.31, 95% CI 0.13–0.73).
Conclusion: Postpartum family planning use in this study was higher than the national average. Factors such as parity; counseling during the pregnancy, delivery, and postpartum periods; and early resumption of sexual activity were linked to increased contraceptive use. These findings suggest that enhanced counseling during antenatal, delivery, and postnatal care could significantly increase contraceptive use.
Introduction
Postpartum family planning (PPFP) services are offered to women and couples within the first year after childbirth. These services include counseling and providing contraceptive options. The goal of postpartum family planning is to address the needs of individuals who want to space their children and those who have reached their desired family size (1).
Family planning (FP) helps women, and their partners control the number of children they have and the timing between births. PPFP specifically allows families to prevent unplanned pregnancies in the 12 months following childbirth. It is recommended that after giving birth, a woman should wait at least 2 years before becoming pregnant again to reduce risks to her health, as well as to the health of her baby and pregnancy (2, 3).
Family planning has been one of the most effective development initiatives in the last 50 years. It offers a wide array of benefits, including economic growth, better maternal and child health, advancements in education, and increased empowerment for women. Research indicates that when governments implement high-quality voluntary family planning programs, they can lower fertility rates and achieve significant improvements in health, wealth, human rights, and education (4).
Identifying the various barriers to effective postpartum family planning is crucial. These barriers may include low socioeconomic status, low literacy levels among both partners, young maternal age, non-satisfaction with family planning methods, myths about family planning methods, the need for spousal permission, fears of health issues related to contraception, and negative past experiences with contraceptive methods (5). It is our responsibility to address these challenges through proper counseling and interventions during the antenatal, natal, and postnatal periods, as well as during immunization sessions.
While there are many barriers, there are also significant opportunities to promote family planning. These include access to prior family planning information; the guidance received during health facility visits; antenatal care (ANC); institutional deliveries; skilled birth attendance; counseling on family planning during antenatal, delivery, and postnatal care (PNC); and having a positive attitude (6–8).
Short pregnancy intervals are associated with adverse maternal outcomes, infant mortality, preterm birth, low birth weight, malnutrition, and stunting of children under 5 years, and the majority of these complications require multiple clinic visits and numerous medications and procedures for relief or cure, at a high cost to the healthcare system (9). Providing contraceptive services during the first 12-month period is one of the most cost-effective ways of minimizing avoidable deaths and suffering in women (10).
The World Health Organization recommends a minimum delay of 24 months following a live birth before attempting the next pregnancy to reduce the risk of unfavorable maternal, perinatal, and infant outcomes (3). Birth-to-pregnancy intervals of approximately 18 months or less are linked to increased risks of infant, neonatal, and perinatal mortality, low birth weight, small size for gestational age, and preterm delivery (11).
Many families may disregard contraception after childbirth due to misunderstandings about pregnancy risk, difficulties in accessing services, and cultural concerns (12). PPFP aims to prevent unwanted pregnancies and pregnancies that are too close together following childbirth (13).
In Ethiopia, the utilization rate of postpartum PPFP varies significantly, ranging from 12.9% to 45.8% (8, 14–16). To address this issue and improve family planning services, Ethiopia has launched the Family Planning Costed Implementation Plan for 2023–2030, aiming for a 54% contraceptive prevalence rate by 2030 (17).
The primary goal of the current study is to investigate the utilization of PPFP and identify the associated factors among women who have given birth in the past year. By providing essential data on the prevalence and various factors influencing PPFP use, this study aims to inform and motivate stakeholders including healthcare professionals, administrators, policymakers, and community health promoters to enhance PPFP utilization. The findings are intended to support efforts to increase awareness and accessibility of postpartum family planning services, ultimately contributing to the objectives outlined in the Family Planning Costed Implementation Plan (FP-CIP).
Methods and materials
Study design and population
This cross-sectional study was conducted in the Bule Hora District, West Guji Zone, Oromia Region, Ethiopia, from 1 May to 30 June 2021, focusing on women of childbearing age. The zone has nine districts. Of these, only three districts (Suro Barguda, Melka Soda, and Dugda Dawa) are pastoralist areas. The study area has a population of 287,904, including 63,627 women of childbearing age, with approximately 9,990 births in the past year. All women who gave birth in the Bule Hora District within the past year (1 May 2020 to 30 April 2021) were the source population for the study, whereas women who gave birth within the same time frame from the selected kebeles were the study population. Women were included if they had lived in the study area for at least 6 months, while those who were critically ill or unable to communicate during the data collection period were excluded from the study.
Sample size determination
The sample size was calculated using a single population proportion formula based on the following assumptions: the utilization of postpartum family planning in Ethiopia (45.8%) (18); Zα/2 = the critical value for normal distribution at the 95% confidence level, which is equal to 1.96 (Z-value of alpha = 0.05); and a 5% margin of error. The final sample size was 630 after factoring in a 10% non-response rate and 1.5 design effects.
Sampling procedures and techniques
A multistage sampling technique was used to select the study participants. First, a total of 41 kebeles in the Bule Hora District were identified, with a total of 59,980 households. Then, 12 kebeles were selected via the lottery method. The number of mothers who gave birth in the last 12 months was obtained from the District Health Bureau. On the basis of the information obtained, a proportional size allocation was made for each individual selected according to their population.
In the second sampling stage, a household with a woman who gave birth in the last 12 months was selected by a simple random sampling technique using the prepared list of households as a sample frame and computer-generated numbers. Finally, mothers who gave birth in the extended postpartum period (1 May 2020 to 30 April 2021) were interviewed. Those mothers who were not available on the first visit were revisited three times.
Study variables
The dependent variable was the utilization of postpartum family planning, whereas age, marital status, educational status of women, educational status of partners, occupation, number of live children, and asset variables, ANC, FP counseling during pregnancy, place of delivery, PNC visit, FP counseling at delivery, counseling during PNC, and birth assistance were all independent variables.
Measurement
Modern contraceptives include sterilization (male and female), subdermal implants, oral contraceptives, condoms (male and female), injectable emergency contraceptive pills, patches, diaphragms and cervical caps, and spermicidal agents (19).
Utilization of PPFP: When a woman who has recently given birth states that she is using any contemporary birth control methods (such as the pill, intrauterine device, injection, male or female condoms, male or female sterilization, or implants) within the first 12 months following her last childbirth (20).
Menstrual resumption: women who resumed menstruation after giving birth.
Sexual resumption: women who have resumed sexual relationships after giving birth.
Wealth is defined as all natural, physical, and financial assets owned by a household and reduced by its liabilities (21).
Wealth index: A principal component analysis (PCA) was used to create a wealth index score for each household based on the selected indicators, which is calculated by combining the standardized indicators. Households were categorized into wealthy quintiles or categories with each quintile representing 20% of the population. The categories included poorest, poor, middle, rich, and richest.
Data collection quality and quality control
The data were collected by 12 health extension workers, via structured and pretested questionnaires (22). Four midwives with BSc supervised the overall data collection process. The principal investigators provided 2 days of training for the data collectors before the actual data collection, with a focus on the relevance of the study, the content of the tool, maintaining confidentiality, and data collection procedures.
The questionnaire was first prepared in English, translated into Afan Oromo, and then retranslated back into English to ensure accuracy by language experts. The questionnaires were pretested on 5% of the sample size of the study area (Burka Arbicho Kebele), which has characteristics like those of the study population, to ensure the clarity of the questionnaire. The data included sociodemographic and economic factors, items related to the benefits of using modern contraceptive methods, maternal health service utilization, and the obstetric characteristics of the study subjects. The collected data were checked for completeness and consistency by supervisors and the principal investigator at the end of each day.
Data processing and analysis
The data accuracy, consistency, and completeness were examined. The data were subsequently entered into Epi-data version 4.6. The data were cleaned and analyzed via SPSS version 25. To describe the characteristics of the study participants, descriptive statistics such as the means, frequencies, and percentages were used. To examine the associations between the dependent and independent variables, a logistic regression was performed. Bivariable analysis was used to select candidate variables for the multivariable model. Variables with a p-value of ≤0.25 that were associated with postpartum family planning utilization were entered into the multivariable logistic regression model. The crude and adjusted odds ratios (AOR), as well as 95% confidence intervals (CI), were used to determine the strength of the associations. Before the last multivariable analysis, the logistic regression assumption was verified via the variance inflation factor and was not detected. Model goodness of fit was checked via the Hosmer–Lemeshow test and its value was insignificant (0.35). The statistical significance of the findings of this study was indicated by a p-value <0.05. The results are presented in text, tables, and graphs depending on the type of data. The asset variables were calculated via the PCA.
Results
Sociodemographic characteristics
This study included 627 women from a total of 630 postpartum mothers in the selected kebeles, with a response rate of 99.5%. The mean age of the respondents was 28.6 (SD ± 5.1) years, with ages ranging from 18 to 47 years. Among the participants, 593 (94.6%) were married women, and 270 (43.1%) were housewives. A total of 451 (71.9%) had no formal education, whereas 13 (2.1%) had a higher level of education (Table 1).
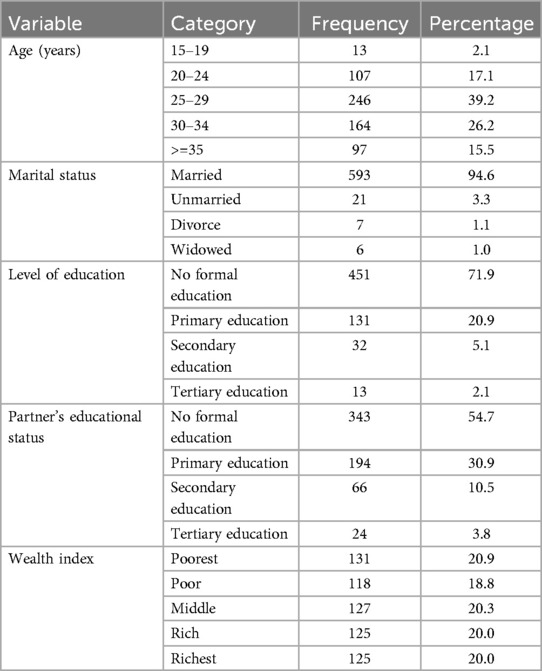
Table 1. Sociodemographic and socioeconomic characteristics of mothers in the Bule Hora Woreda, southern Ethiopia, in 2021 (n = 627).
Reproductive and maternal health service-related characteristics
The research involved a majority of women who had given birth multiple times (50.6%), with the highest percentage of participants (45.1%) having received two to three antenatal care visits. A significant proportion (69.7%) received family planning counseling before delivery. A majority (74.6%) experienced unplanned pregnancies, and 69.7% and 66.5% received PPFP information before and after delivery, respectively. While 82.3% received postnatal care, only 66.5% received PPFP counseling during this period. Most users of PPFP (71.3%) received contraceptives from government institutions. The majority of deliveries (71.3%) took place in health institutions, and 72.9% of these deliveries were attended by trained health professionals. The study participants’ reproductive preferences were categorized into five groups. The most common preference was to have another child after 2 years (57.7%, 362). A substantial number also expressed a desire to have another child soon (11.8%, 74). Conversely, 77 (12.3%) reported that they did not want any more children. A smaller proportion (7.5%, 47) were open to having another child at some unspecified point in the future, while 67 (10.7%) remained undecided about their future reproductive plans (Table 2).
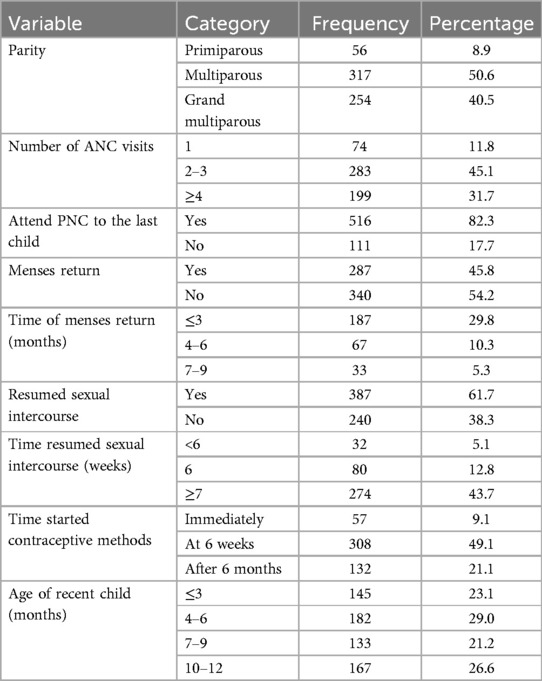
Table 2. Reproductive and maternal health service-related characteristics in the Bule Hora District, southern Ethiopia (n = 627).
Postpartum family planning method utilization by type
In total, 447 (71.3%; 95% CI 67.6–74.8) respondents had used postpartum contraceptives within the previous year. In this study, injectable contraception was the most commonly used method (47.4%), followed by implants (15.8%). The main reason given by the study participants for not utilizing family planning was spousal disapproval (112, 17.9%) (Figure 1).
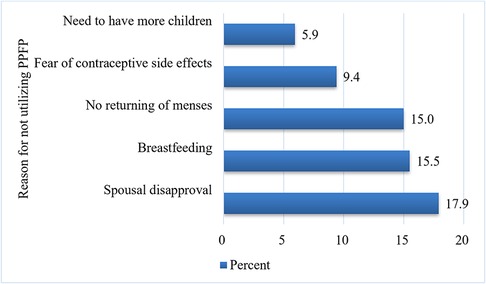
Figure 1. Reason for not utilizing postpartum family planning among women in the Bule Hora District, southern Ethiopia. PPFP, postpartum family planning.
Factors associated with postpartum family planning utilization
In the multivariable logistic regression, receiving counseling about family planning while pregnant, at the time of delivery, and during PNC; resuming sexual activity after birth; planning the last delivery; and the number of ANC visits were significantly associated with postpartum family planning utilization.
Grand multiparous women were 69% less likely to use family planning compared to primiparous women (AOR = 0.31, 95% CI 0.13–0.73).
Women who received family planning counseling during pregnancy were 1.79 times more likely to use family planning than those who did not receive counseling (AOR = 1.79, 95% CI = 1.61–2.82). Women who received family planning counseling at the time of delivery were 2.62 times more likely to use family planning than those who did not receive counseling (AOR = 2.62, 95% CI = 1.57–4.38). Women who received family planning counseling during postnatal care were 2.7 times more likely to use family planning in the postpartum period compared to those who did not receive counseling (AOR = 2.71, 95% CI = 1.75–4.21).
Women who had resumed sexual activity had nearly twice the odds of taking a modern contraceptive as those who had not resumed sexual activity since birth (AOR = 1.92, 95% CI = 1.25–2.96). Mothers who had four or more antenatal care visits were three times more likely to utilize postpartum family planning than those who had fewer visits (AOR = 3.09, 95% CI = 1.61–5.92) (Table 3).
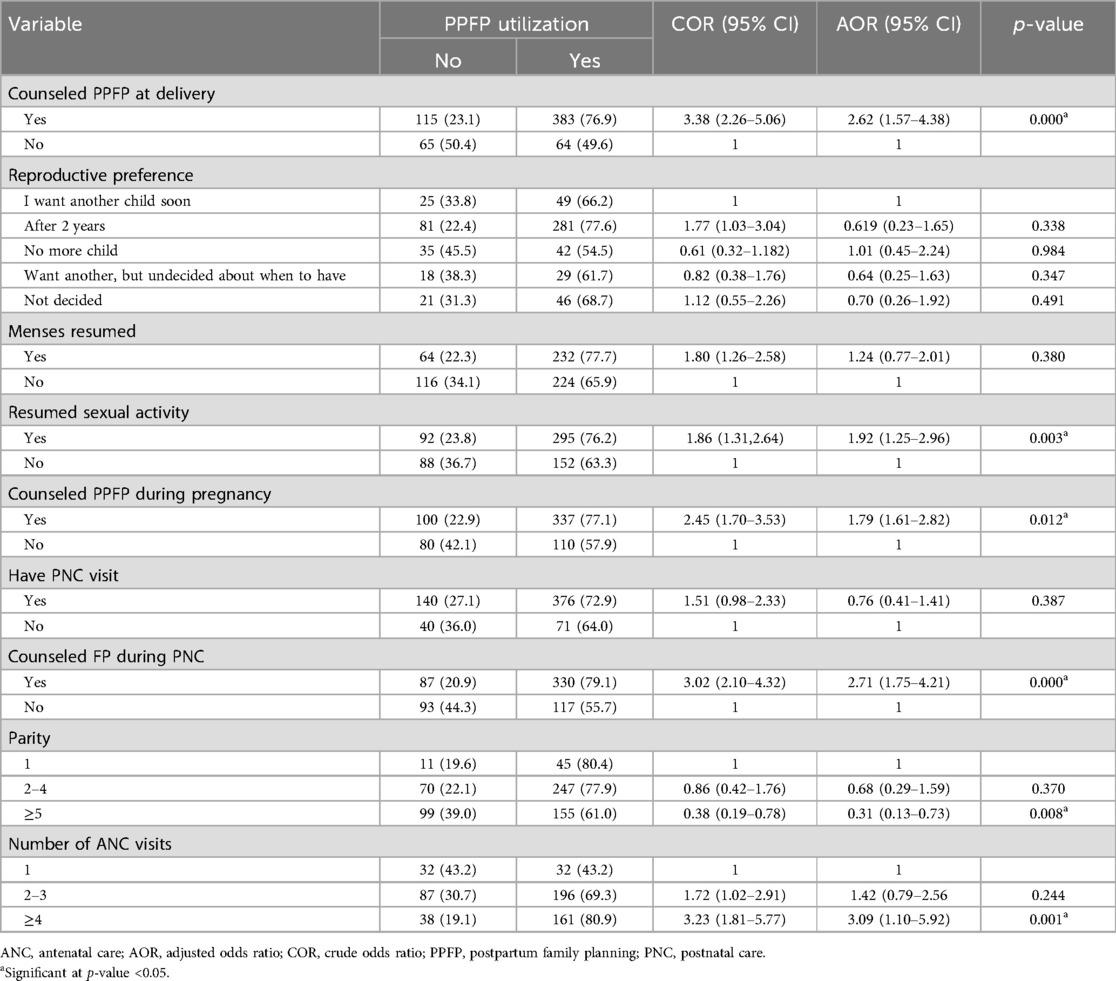
Table 3. Bivariable and multivariable logistic regression analyses of factors associated with the utilization of PPFP in the Bule Hora District, southern Ethiopia.
Discussion
The total prevalence of postpartum family planning utilization was 71.3%, with a 95% confidence interval of 67.6%–74.8%. The number of antenatal care visits; counseling during pregnancy, delivery, and postnatal care; resuming sexual activity; and anticipated last delivery were significantly associated with postpartum family planning utilization.
The prevalence of PPFP utilization in this study, at 71.3%, aligns with findings from a study in Hossana Town (72.9%) (23), suggesting a consistent trend in certain regions of Ethiopia. However, this rate is lower than that observed in Addis Ababa (80.3%) (12), potentially due to differences in access to healthcare services and sociodemographic factors. The study population in Addis Ababa may have had a higher proportion of women with better educational attainment and residing in urban areas, contributing to higher PPFP utilization.
The prevalence of PPFP utilization observed in this study (71.3%) is also significantly higher than that reported in previous studies conducted in Gondor (45.8%) (24) and Debre Birhan, Ethiopia (33.1%) (25). The difference could be due to differences in the reproductive and maternal health service use-related characteristics of the study participants.
Women who had received family planning counseling during postnatal care follow-ups were more likely to use postpartum contraceptives than those who did not. This finding was supported by studies undertaken in northern Ethiopia (12), the Aroressa District (26), Kebribeyah Town, Ethiopia (27), and the Kailali district in Nepal (28). PNC counseling plays a crucial role in promoting PPFP utilization. By introducing the concept of family planning during PNC visits, healthcare providers create an opportunity for women to reflect on their future family planning needs. This early engagement allows women to address concerns, understand the benefits of spacing pregnancies, and explore their options. Comprehensive PNC counseling also increases women's awareness of different contraceptive methods, their effectiveness, and access points. This knowledge empowers them to make informed choices about family planning. Furthermore, a supportive and respectful PNC environment fosters trust between women and healthcare providers. This trust is essential for open conversations about family planning, encouraging women to feel comfortable discussing their needs and seeking PPFP counseling.
Women who were counseled about postpartum contraception at the time of birth had a statistically significant association with postpartum family planning utilization. This finding is in line with a study conducted in Sidama, southern Ethiopia (29), and Pawe, Benishangul Gumuz, Ethiopia (30). Counseling during childbirth provides a critical opportunity to introduce PPFP, increasing awareness and acceptance of family planning. This early engagement builds trust and empowers women to discuss their future family planning needs, leading to higher PPFP utilization rates. This highlights the importance of integrating PPFP counseling into childbirth care as a standard practice. Policymakers should prioritize training healthcare providers to effectively deliver this counseling and ensure access to a variety of contraceptive methods in all birth settings.
This study suggests a strong link between resuming sexual activity and PPFP utilization, consistent with findings in Ghana (31) and Nigeria (32). Women who have resumed sexual activity are more likely to seek family planning to prevent unplanned pregnancies. Clinicians should tailor counseling strategies to address the needs of women who have resumed sexual activity, while policymakers should strengthen programs to ensure access to culturally appropriate family planning services in all regions. This includes promoting awareness, improving contraceptive access, and training healthcare providers. These efforts empower women to make informed choices about their reproductive health.
This study found that women who completed four or more ANC visits during pregnancy were more likely to utilize PPFP. This finding aligns with research conducted in Kebribeyah Town, Somalia, Eastern Tigray, and Western Ethiopia (27, 33, 34), suggesting a consistent association between increased ANC engagement and PPFP uptake. The likely reason behind this association is that frequent ANC visits provide opportunities for women to receive comprehensive health information, including counseling on family planning and the benefits of spacing pregnancies. Women who attend more ANC visits are more likely to be aware of the risks of closely spaced pregnancies for mothers and newborns, making them more receptive to PPFP.
This finding underscores the importance of integrating family planning counseling into routine ANC visits. Clinicians should leverage these visits to discuss family planning options, address concerns, and provide comprehensive information about spacing pregnancies and their benefits. This proactive approach can significantly improve PPFP utilization.
In this research, it was observed that the adoption of postpartum family planning was lower among women with five or more children compared to those with four or fewer children. Aligning with existing literature, the study revealed that women with four or more children tended to use contraception at notably lower levels than women with one to three children. In addition, married women with four or more births exhibited lower rates of modern contraceptive usage (27.1%) in contrast to women with zero to one child (41.6%) or two to three children (43.6%) (35, 36). This might be due to access barriers and cultural and societal norms, and multiparous women may believe that they have a lower chance of unplanned pregnancies due to natural declining fertility with advanced age.
Strengths and limitations of the study
The large sample size enhances the study's statistical power and the reliability of the findings. The study examined various factors that positively influence PPFP utilization, providing valuable insights into the determinants of PPFP uptake. Because of the cross-sectional nature of the study, it is not possible to establish a causal relationship between the factors that were identified and the use of postpartum family planning.
Conclusion
In this study, the prevalence of postpartum family planning utilization was relatively high compared with that reported in previous national studies. Counseling family planning during the pregnancy, delivery, and postnatal periods; resuming sexual activity after birth; multiparity; and the number of antenatal care visits were significantly associated with postpartum family planning utilization.
Implications for policies and practice
According to the study's findings, policymakers should prioritize training healthcare providers in effective family planning, ensure that all women have access to these services, and emphasize the significance of comprehensive family planning counseling from the beginning of pregnancy to postnatal care.
It is highly recommended that the many misconceptions of PPFP are addressed and the advantages of family planning and its integration with ANC services are highlighted. During the pregnancy, delivery, and postpartum periods, proactive implementation of comprehensive and inclusive counseling is required. A key component is empowering all women to make knowledgeable decisions regarding their reproductive health.
To be able to gain an understanding of the factors driving PPFP utilization and investigate the experiences and viewpoints of women with various parities, future research incorporating qualitative investigations is advised.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval for the study was obtained from the institutional review board of Bule Hora University, and the study received ethical approval on 20/04/2021. number BHU/RPD/256/21. Written informed consent was obtained from each participant to explain the purpose and nature of the study. The study was entirely voluntary, and participants were informed of their right to withdraw or refuse participation at any time during their trial. Furthermore, confidentiality was ensured using an anonymous questionnaire.
Author contributions
NS: Conceptualization, Data curation, Formal Analysis, Investigation, Software, Methodology, Project administration, Writing – original draft. ZD: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Writing – original draft, Resources, Supervision, Writing – review & editing. WW: Conceptualization, Data curation, Writing – review & editing, Formal Analysis, Investigation, Software. AYi: Data curation, Investigation, Project administration, Software, Supervision, Writing – review & editing. FB: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Writing – review & editing. SF: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing. AYe: Data curation, Investigation, Project administration, Software, Supervision, Writing – review & editing. BB: Investigation, Project administration, Software, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank the Blue Hora University data collectors and supervisors for their support during this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ANC, antenatal care; FP, family planning; PNC, postnatal care; PPFP, postpartum family planning.
References
1. Barkataki S. Postpartum family planning in Bangladesh a situation analysis and way forward (2018).
2. Seifu B, Yilma D, Daba W. Knowledge, utilization and associated factors of postpartum family planning among women who had delivered a baby in the past year in Oromia Regional State, Ethiopia. Open Access J Contracept. (2020) 11:167–76. doi: 10.2147/OAJC.S268561
4. Bongaarts J, Cleland JC, Townsend J, Bertrand JT, Das Gupta M. Family planning programs for the 21st century fam: rational and design [Internet] (2012). p. 1–94. Available online at: https://knowledgecommons.popcouncil.org/cgi/viewcontent.cgi?article=2002&context=departments_sbsr-rh.
5. Abbasi Y, Shaikh SR, Memon KN. Barriers and missed opportunities towards immediate and early post-partum family planning methods in Pakistan. Prof Med J. (2020) 27(7):1448–53. doi: 10.29309/TPMJ/2020.27.07.4273
6. Tafa L, Worku Y. Family planning utilization and associated factors among postpartum women in Addis Ababa, Ethiopia, 2018. PLoS One. (2021) 16:e0245123. doi: 10.1371/journal.pone.0245123
7. Tilahun T, Bekuma TT, Getachew M, Oljira R, Seme A. Barriers and determinants of postpartum family planning uptake among postpartum women in western Ethiopia: a facility-based cross-sectional study. Arch Public Heal. (2022) 80(1):1–11. doi: 10.1186/s13690-021-00755-5
8. Silesh M, Demisse TL, Taye BT, Moltot T, Chekole MS, Wogie G, et al. Immediate postpartum family planning utilization and its associated factors among postpartum women in Ethiopia: a systematic review and meta-analysis. Front Glob Womens Health. (2023) 4:1095804. doi: 10.3389/fgwh.2023.1095804
9. Sitrin D, Jima GH, Pfitzer A, Wondimu C, Belete TW, Pleah T, et al. Effect of integrating postpartum family planning into the health extension program in Ethiopia on postpartum adoption of modern contraception. J Glob Heal Reports. (2020) 4:e2020058. doi: 10.29392/001c.13511
11. Jima GH, Garbaba WB. Postpartum family planning utilization and associated factors among women who gave birth in the last 12 months prior to the study in Lode Hetosa District, south east Ethiopia. J Womens Heal Care. (2020) 9(3):1–11. doi: 10.35248/2167-0420.20.9.488
12. Gebremedhin AY, Kebede Y, Gelagay AA, Habitu YA. Family planning use and its associated factors among women in the extended postpartum period in Addis Ababa, Ethiopia. Contracept Reprod Med. (2018) 3(1):1–8. doi: 10.1186/s40834-017-0054-5
13. Royal College of Obstetricians and Gynaecologists. Best practice in postpartum family planning. (2015).
14. Mehare T, Mekuriaw B, Belayneh Z, Sharew Y. Postpartum contraceptive use and its determinants in Ethiopia: a systematic review and meta-analysis. Int J Reprod Med. (2020) 2020:5174656. doi: 10.1155/2020/5174656
15. Gezume A, Wabeto E, Alemayehu H. Level of immediate postpartum family planning utilization and the associated factors among postpartum mothers, Bole Sub-City, Addis Ababa, Ethiopia: institution based cross- sectional study. BMC Womens Health. (2024) 24:237. doi: 10.1186/s12905-024-03038-7
16. Wassihun B, Wosen K, Getie A, Belay K, Tesfaye R, Tadesse T, et al. Prevalence of postpartum family planning utilization and associated factors among postpartum mothers in Arba Minch town, south Ethiopia. Contracept Reprod Med. (2021) 6(1):4–11. doi: 10.1186/s40834-021-00150-z
18. Wakuma B, Mosisa G, Etafa W, Mulisa D, Tolossa T, Fetensa G, et al. Postpartum modern contraception utilization and its determinants in Ethiopia: a systematic review and meta-analysis. PLoS One. (2020) 15:e0243776. doi: 10.1371/journal.pone.0243776
19. Central Statistical Agency/CSA/Ethiopia and ICF. Ethiopia Demographic Health Survey 2016. Addis Ababa and Rockville, MD: CSA and ICf (2016).
20. Abraha TH, Gebrezgiabher BB, Aregawi BG, Belay DS, Tikue LT, Welay GM. Predictors of postpartum contraceptive use in rural Tigray region, northern Ethiopia: a multilevel analysis. BMC Public Health. (2018) 18(1):1–10. doi: 10.1186/s12889-018-5941-4
21. Hjelm L, Mathiassen A, Darryl Miller AW. WFP, creation of a wealth index; VAM-guidance paper. WFP. (2017); p. 1–26.
22. Getachew M. Assessment of postpartum contraceptive adoption and associated factors in Butajira health and demographic surveillance site (HDSS), in southern investigator - Mahilet Getachew (BSc) advisor - Abiy Seifu (MPH). (2015).
23. Gejo NG, Anshebo AA, Dinsa LH. Postpartum modern contraceptive use and associated factors in Hossana town. PLoS One. (2019) 14(5):1–10. doi: 10.1371/journal.pone.0217167
24. Berta M, Feleke A, Abate T, Worku T, Gebrecherkos T. Utilization and associated factors of modern contraceptives during extended postpartum period among women who gave birth in the last 12 months in Gondar town, northwest Ethiopia. Ethiop J Health Sci. (2018) 28(2):207–16. doi: 10.4314/ejhs.v28i2.12
25. Demie TG, Demissew T, Huluka TK, Workineh D, Libanos HG. Postpartum family planning utilization among postpartum women in public health institutions of Debre Berhan town, Ethiopia. J Womens Heal Care. (2018) 7(2):1–9. doi: 10.4172/2167-0420.1000426
26. Dona A, Abera M, Alemu T, Hawaria D. Timely initiation of postpartum contraceptive utilization and associated factors among women of child bearing age in Aroressa district, southern Ethiopia: a community based cross-sectional study. BMC Public Health. (2018) 18(1):1–9. doi: 10.1186/s12889-018-5981-9
27. Roble AK, Ibrahim AM, Osman MO, Wedajo GT, Absiye AU, Hudle RO. Postnatal care service utilization and associated factor among reproductive age women who live in Dolo Addo district, Somali region, southeast Ethiopia. Eur J Prev Med. (2020) 8(3):24. doi: 10.11648/j.ejpm.20200803.11
28. Joshi AK, Tiwari DP, Poudyal A, Shrestha N, Acharya U, Dhungana GP. Utilization of family planning methods among postpartum mothers in Kailali district, Nepal. Int J Womens Health. (2020) 12:487–94. doi: 10.2147/IJWH.S249044
29. Tefera L, Abera M, Fikru C, Tesfaye D. Utilization of immediate post-partum intra uterine contraceptive device and associated factors: a facility based cross sectional study among mothers delivered at public health facilities of Sidama zone, south Ethiopia. J Preg Child Heal. (2017) 4(3):16–24. doi: 10.4172/2376-127X.1000326
30. Jaleta DN, Yeshita HY, Tamirat KS. Timely initiation of postpartum contraceptive and associated factors among women of extended postpartum period in Pawe district, northwest Ethiopia, 2019. (2019); p. 1–21.
31. Coomson JI, Manu A. Determinants of modern contraceptive use among postpartum women in two health facilities in urban Ghana: a cross-sectional study. Contracept Reprod Med. (2019) 4(1):1–11. doi: 10.1186/s40834-018-0082-9
32. Adedokun B, Abdus-Salam R, Babawarun T, Morhason-Bello I, Ojengbede O. Resumption of sexual intercourse and family planning use among postpartum women attending infant welfare clinics in Ibadan, southwest Nigeria-a cross-sectional study. Niger J Clin Pract. (2020) 23(12):1648–55. doi: 10.4103/njcp.njcp_76_20
33. Gebremariam A, Gebremariam H. Contraceptive use among lactating women in Ganta Afeshum district, eastern Tigray. Int Breastfeed J. (2016) 11:1–8. doi: 10.1186/s12884-017-1613-0
34. Teka TT, Feyissa TR, Melka AS, Bobo FT. Role of antenatal and postnatal care in contraceptive use during postpartum period in western Ethiopia: a cross sectional study. BMC Res Notes. (2018) 11(1):1–6. doi: 10.1186/s13104-018-3698-6
35. Zimmerman LA, Yi Y, Yihdego M, Abrha S, Shiferaw S, Seme A, et al. Effect of integrating maternal health services and family planning services on postpartum family planning behavior in Ethiopia: results from a longitudinal survey. BMC Public Health. (2019) 19(1):1–9. doi: 10.1186/s12889-019-7703-3
36. Monitoring P. Accountability 2020 (PMA2020). PMA2015/DRC-Round4: Family Planning Key Indicator Brief. Baltimore, MD: Kinshasa School of Public Health, Tulane School of Public Health and Tropical Medicine, and Bill and Melinda Gates Institute for Population and Reproductive Health, Johns Hopkins Bloomberg school of Public Health (2016).
Keywords: utilization, postpartum, family planning, contraceptive methods, postpartum family planning utilization
Citation: Sirage N, Desalegn Z, Wako WG, Yimer A, Bizuneh FK, Feleke SF, Yesuf A and Beyene BN (2024) Family planning utilization among postpartum women in the Bule Hora District, southern Ethiopia. Front. Glob. Womens Health 5:1323024. doi: 10.3389/fgwh.2024.1323024
Received: 17 October 2023; Accepted: 19 November 2024;
Published: 9 December 2024.
Edited by:
Merlin Willcox, University of Southampton, United KingdomReviewed by:
Clare Goodhart, British Medical Association, United KingdomMeless Gebrie Bore, University of Technology Sydney, Australia
Copyright: © 2024 Sirage, Desalegn, Wako, Yimer, Bizuneh, Feleke, Yesuf and Beyene. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nurye Sirage, c2lyYWdlbnVyeWVAZ21haWwuY29t
 Nurye Sirage
Nurye Sirage Zewuditu Desalegn2
Zewuditu Desalegn2 Wako Golicha Wako
Wako Golicha Wako Ali Yimer
Ali Yimer Fassikaw Kebede Bizuneh
Fassikaw Kebede Bizuneh Belda Negesa Beyene
Belda Negesa Beyene