- 1Department of Microbiology, Faculty of Medical Laboratory Sciences, University of El Imam El Mahdi, Kosti, Sudan
- 2Department of Medical Laboratory Sciences, Faculty of Medicine and Health Sciences, Jamhuriya University of Science and Technology, Mogadishu, Somalia
- 3Department of Nursing and Midwifery, Faculty of Medicine and Health Sciences, Jamhuriya University of Science and Technology, Mogadishu, Somalia
Background: Hepatitis B virus (HBV) remains a leading cause of chronic hepatitis, maternal complications, and neonatal deaths in sub-Saharan Africa. Mother-to-child transmission is a major route of HBV transmission in endemic areas. This study aimed to determine the prevalence of hepatitis B infection and its associated factors among pregnant women attending Antenatal Care clinics at SOS Hospital in Mogadishu, Somalia.
Methods: The research followed a cross-sectional design, and the participants were chosen through systematic random sampling, including every fifth outpatient. Each participant provided a blood sample for standard testing, and their consent was obtained before conducting Hepatitis B screening using the ELISA method.
Results: In our study of 384 pregnant women, 43 individuals (11.2%) tested positive for HBsAg. The frequency of HBsAg seropositivity was significantly higher in subjects with no education when compared to those with primary education (AOR = 0.1, 95% CI: 0.01–0.96, p = 0.046). Caesarian Section (AOR = 0.02, 95% CI: 0.004–0.0103, p = 0.001), blood transfusion (AOR = 11.6, 95% CI: 3.44–38.08, p = 0.001), previous dental procedures (AOR = 0.1, 95% CI: 0.04–0.38, p = 0.001), and unsafe injections in the past (AOR = 0.3, 95% CI: 0.09–0.91, p = 0.035) were identified as significant risk factors for hepatitis positivity.
Conclusions: The study found a higher prevalence of hepatitis B compared to previous studies. Factors such as blood transfusion, dental procedures, Caesarian Section, and unsafe injections were associated with hepatitis B infection. It is essential to raise awareness, promote preventive measures, and implement routine screening for pregnant women so as to stop the transmission of hepatitis B to their children.
Background
Hepatitis B Virus is an emerging global health problem (1). Approximately 65 million women of reproductive age groups worldwide are infected with hepatitis B virus and 9 in every 10 mothers with hepatitis B infection transmit the diseases to their child's at the time of birth (2). Hepatitis B is widespread in Africa, affecting 7%–26% of people (3). The regions with the highest prevalence are mainly in Sub-Saharan Africa (4). As a part of Sub-Saharan region, Somalia is classified among the countries as having a high hepatitis B surface antigen (HBsAg) endemicity of more than 8% (5, 6). This indicates HBV infection among pregnant women becomes public health problem in the country. Previous studies have found different factors associated with of HBV infection in pregnant women, these include having multiple sexual partners, dental procedure history, admission history to health facilities, genital mutilation, abortion history, history of giving birth by traditional birth attendants, and blood transfusion (7, 8). The Hepatitis B virus (HBV) can be transmitted through vertical transmission from mother to child (9), and various interventions have shown efficacy in reducing this transmission. These interventions include the use of antiviral drugs during the last trimester if the viral load exceeds 10 million copies per milliliter, as well as administering both immunoglobulin and antigen to the newborn within 24 h of birth, which has demonstrated positive outcomes (10). Despite the absence of published data over the past two decades, this research provides essential insights into the prevalence and risk factors of Hepatitis B among pregnant women in Somalia, aiming to inform targeted public health strategies and ultimately reduce the burden of the disease in this vulnerable population. Therefore, this study aimed to determine the prevalence of HBV infection and associated risk factors among pregnant women attending SOS Hospital in Mogadishu, Somalia.
Methods
This is a cross-sectional study conducted at SOS Hospital in Mogadishu, Somalia from March 25, 2022, to June 5, 2022. The study focused on pregnant women receiving antenatal care (ANC) at the hospital.
Inclusion and exclusion criteria
The inclusion criteria for this study included any pregnant woman attending SOS hospital during the study period who had not been vaccinated against hepatitis B and did not know her hepatitis B status. Conversely, the exclusion criteria encompassed any pregnant woman attending SOS hospital who had been vaccinated against the hepatitis B virus or had previously tested positive for any hepatitis B seromarkers.
Sample size determination
The sample size (N) was determined through manual calculation. The estimated proportion of exposure was 0.5 (p) for both exposed and unexposed groups. A 95% confidence interval was used with a confidence estimate of 1.96 (Z) and a precision of 0.05 (d). A design effect of 1 was applied. The sample size was obtained using the formula mentioned below (11)
Tools and techniques used to collect the Data.
The data were collected using a structured questionnaire that included details about sociodemographic characteristics, health-related factors, practices, and behavioral variables related to health. Data collectors and supervisors underwent training before data collection, and the collected data were checked daily for completeness by the supervisor and principal investigator.
The detection of HBsAg using the enzyme-linked immunosorbent assay (ELISA) followed by Sandwich principle
5 ml of blood was collected from each participant, and the serum was separated from the blood by centrifugation at 3,000 rpm for 5 min. The manufacturer's instructions were followed to examine the serum samples for the presence of hepatitis B surface antigen using an ELISA kit (LumiQuick, USA) using MR 96A ELISA reader (Mindray, China).
Data analysis
The data were analyzed using SPSS statistical software (Version 20). For descriptive statistics percentages and frequency were used. Association between prevalence and related categorical variables such as age, gender, education, occupation was analyzed using Chi-square test, with P value < 0.05 was considered significant. Binary logistic regression model was used to determine the factors significantly associated with the prevalence of HBV; the results were considered statistically significant at 95% confidence interval (p < 0.05). Crude and adjusted odds ratios with 95% CI were used to see the strength of association. Predictor variables with a p-value <0.05 in the bivariate analysis were candidates for the multivariable logistic regression model. A p-value of less than .05 in multivariable logistic regression was considered statistically significance.
Results
Demographic profile of study participants
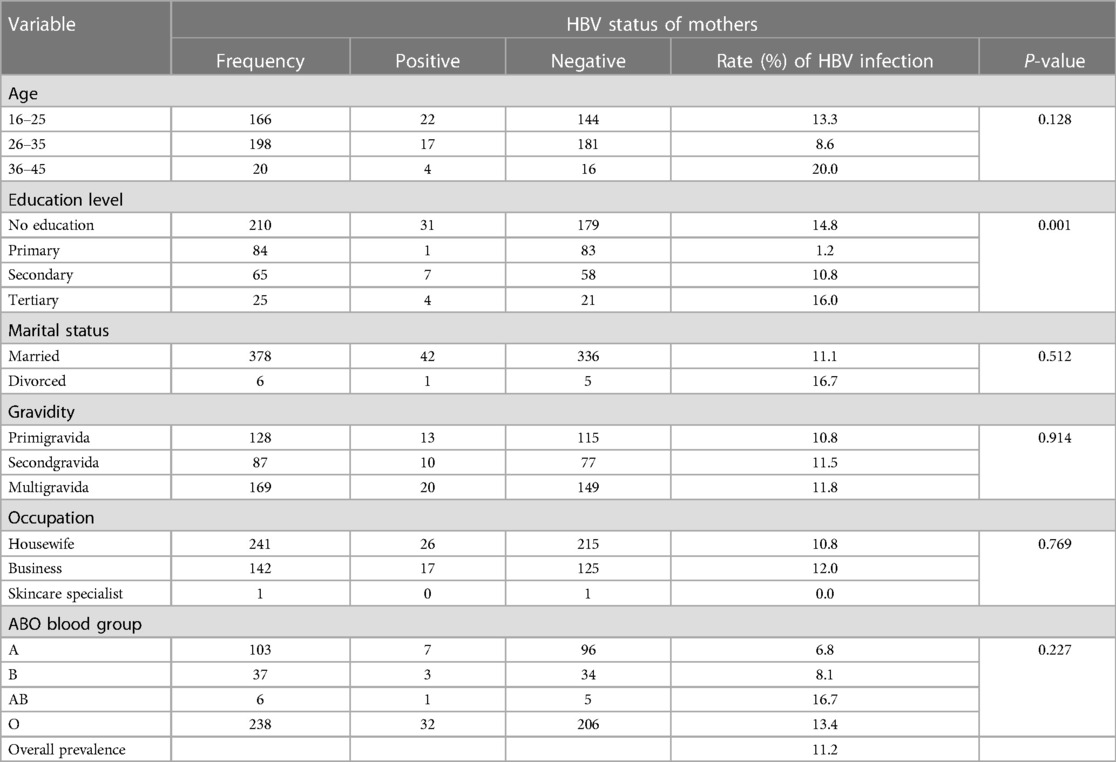
A total of 384 pregnant woman participated in this study with a response rate of 100%. Respondents age ranged between 16 to 45 years. The majority of respondents, comprising 378 (82.9%), were married, while 6 (1.3%) were divorced. In terms of educational level, 210 (46.1%) had no formal education, 84 (18.4%) had primary education, 65 (14.3%) had secondary education, and 25 (5.5%) of pregnant woman had tertiary education, as shown in Table 1.
Seroprevalence of HBV among pregnant women
Out of the 384 pregnant women included in the study, 43 tested positive for HBsAg, resulting in an overall prevalence of 11.2%. The age group between 36–45 had the highest prevalence of Hepatitis B virus (20.0%), while mothers with no education showed the highest occurrence rate of HBV infection (14.8%), compared to those with primary education as shown in Table 1.
Risk factors of hepatitis B virus infection
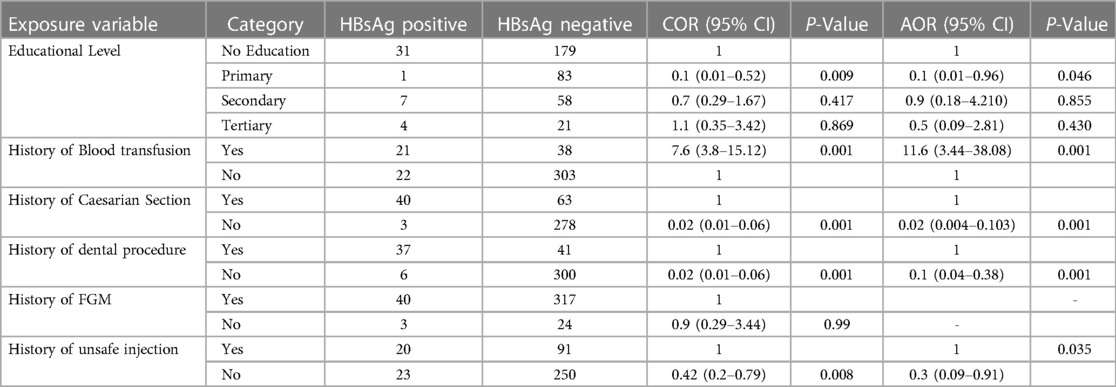
The findings suggest that primary education may be associated with a decreased odds of HBV infection compared to no education (AOR = 0.1, 95% CI: 0.01–0.96, p-value = 0.046). Women with history of blood transfusion was found to have 11.6 times more likely to test positive for HBsAg compared to those without a history of blood transfusion (AOR = 11.6 (95% CI: 3.44–38.08 with p-value = 0.001). Pregnant women who did not have a caesarian section were 98% less likely to be positive for HBsAg than those who did have a caesarian section (AOR = 0.02 (95% CI: 0.004–0.103 with p-value = 0.001). Pregnant women with no history of dental procedures were 88% less likely to test positive for HBsAg compared to those with a history of dental procedures (AOR = 0.1 (95% CI: 0.04–0.38 with p-value = 0.001). On the other hand, the study found that women who had a history of unsafe injection were 80% less likely to test positive for HBsAg compared to those who had no history of unsafe injection (AOR = 0.3, 95% CI: 0.09–0.91, p-value = 0.035), as shown in Table 2.
Discussion
In this study, we assessed the prevalence of hepatitis B virus and associated factors among pregnant women receiving antenatal care in SOS hospital in Mogadishu, Somalia. The prevalence of HBsAg in pregnant women in the current study was 11.2%, surpassing the WHO cut-off level of endemicity at 8%, indicating a highly endemic region. Lack of the history of blood transfusion, dental procedures, Caesarian Section, and unsafe injections have found statistically significant associations with lower hepatitis B virus seropositivity. This finding is higher than with previous studies from Somalia and Ethiopia, that revealed the prevalence of hepatitis B virus of 5.7% and 9.2% respectively (5, 12). But it was lower than studies conducted in Uganda and Ethiopia with prevalence of 11.8%, 11.3% respectively. The difference between studies may result from variations in the study's design, sample size, study populations' geographic locations, and sociocultural variables. On the other hand, similar studies in similar sample populations, across the world found greater seroprevalence of HBV. Our study revealed that the levels of education were found to be associated with HBV infection among mothers, which is consistent with previous studies (2, 13–14). History of blood transfusion emerged as a significant risk factor for HBV infection among pregnant women, this is consistent with findings from Mogadishu, Somalia (15). This could be attributed to the lack of standardization in blood collection and storage practices, which potentially lead to the use of infected blood in transfusions. Similarly, mothers who had undergone cesarean sections or dental procedures were more likely to test positive for HBsAg, aligning with previous research conducted in Ethiopia (7). Lastly, a history of unsafe injection was significantly associated with HBV infection among pregnant women, which is consistent with studies conducted in Ethiopia and Gambia (9, 10).
Limitations
The study was conducted in a single health facility, which means that the findings may not accurately represent all pregnant women in the Mogadishu area. HBV markers such as HBeAg and HBV-DNA were not detected in this study due to a lack of laboratory setup.
Conclusion
The prevalence of hepatitis B in this study is higher compared to some previous studies. The factors associated with hepatitis B infection include blood transfusion, history of dental procedures, Caesarian Section, and history of unsafe injection. To reduce the high prevalence found in this study, it's important to regularly test for HBV during pregnancy checkups. Using clean needles and ensuring sterilized equipment are also crucial. These steps can help lower the risk of spreading hepatitis B. It's also essential to raise awareness about these measures to protect against hepatitis B effectively.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
This study was approved by the Research Board of the Faculty of Medical Laboratory Sciences, University of El Imam El Mahdi, Sudan, and permission was obtained from the authorities of SOS Hospital, Mogadishu, Somalia. The study was conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
SA: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. YA: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. BSA: Data curation, Formal Analysis, Methodology, Supervision, Writing – review & editing. YH: Conceptualization, Data curation, Formal Analysis, Software, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kebede KM, Abateneh DD, Belay AS. Hepatitis B virus infection among pregnant women in Ethiopia: a systematic review and meta-analysis of prevalence studies. BMC Infect Dis. (2018) 18(1):1–9. doi: 10.1186/s12879-018-3234-2
2. Wakjira M, Darega J, Oljira H, Tura MR. Prevalence of hepatitis B virus and its associated factors among pregnant women attending antenatal care in Ambo town, central Ethiopia: a cross-sectional study. Clin Epidemiol Glob Health. (2022) 15:101054. doi: 10.1016/j.cegh.2022.101054
3. Tadesse M, Tafesse G, Hajare ST, Chauhan NM. Assessment of prevalence of hepatitis B virus and its associated factors among pregnant women from Wolaita Sodo, Ethiopia. J Clin Virol Plus. (2022) 2(2):100069. doi: 10.1016/j.jcvp.2022.100069
4. Amponsah-Dacosta E. Hepatitis B virus infection and hepatocellular carcinoma in sub-Saharan Africa: implications for elimination of viral hepatitis by 2030? World J Gastroenterol. (2021) 27(36):6025–38. doi: 10.3748/wjg.v27.i36.6025
5. Hassan-Kadle MA, Osman MS, Ogurtsov PP. Epidemiology of viral hepatitis in Somalia: systematic review and meta-analysis study. World J Gastroenterol. (2018) 24(34):3927–57. doi: 10.3748/wjg.v24.i34.3927
6. Hassan YSA, Hassan SA, Ahmed NR. Uptake of hepatitis B vaccination and associated factors among health sciences students, Mogadishu, Somalia. Front Public Health. (2023) 11(September):1–6. doi: 10.3389/fpubh.2023.1203519
7. Kassaw B, Abera N, Legesse T, Workineh A, Ambaw G. Sero-prevalence and associated factors of hepatitis B virus among pregnant women in Hawassa city public hospitals, Southern Ethiopia: cross-sectional study design. SAGE Open Med. (2022) 10. doi: 10.1177/20503121221140778
8. Kafeero HM, Ndagire D, Ocama P, Walusansa A, Sendagire H. Sero-prevalence of human immunodeficiency virus–hepatitis B virus (HIV–HBV) co-infection among pregnant women attending antenatal care (ANC) in sub-Saharan Africa (SSA) and the associated risk factors: a systematic review and meta-analysis. Virol J. (2020) 17(1):1–19. doi: 10.1186/s12985-020-01443-6
9. Gedefaw G, Waltengus F, Akililu A, Gelaye K. Risk factors associated with hepatitis B virus infection among pregnant women attending antenatal clinic at Felegehiwot referral hospital, Northwest Ethiopia, 2018: an institution based cross sectional study. BMC Res Notes. (2019) 12(1):1–7. doi: 10.1186/s13104-019-4561-0
10. Bittaye M, Idoko P, Ekele BA, Obed SA, Nyan O. Hepatitis_B_virus_sero-prevalence_amongst_pregnant. BMC Infect Dis. (2019):1–8.
11. Fisher AA, Laing J, Stoeckel JE, Townsend JW. Handbok for family planning, operations research designthe population council. Soc. Sci. Med. (1991) 39:381–90.
12. Tadiwos MB, Kanno GG, Areba AS, Kabthymer RH, Abate ZG, Aregu MB. Sero-prevalence of hepatitis B virus infection and associated factors among pregnant women attending antenatal care services in Gedeo zone, southern Ethiopia. J Prim Care Community Health. (2021) 12. doi: 10.1177/2150132721993628
13. Oladeinde BH, Olaniyan MF, Muhibi MA, Uwaifo F, Richard O, Omabe NO, et al. Association between ABO and RH blood groups and hepatitis B virus infection among young Nigerian adults. J Prev Med Hyg. (2022) 63(1):E109–14. doi: 10.15167/2421-4248/jpmh2022.63.1.1967
14. Malungu Ngaira JA, Kimotho J, Mirigi I, Osman S, Ng’ang’a Z, Lwembe R, et al. Prevalence, awareness and risk factors associated with hepatitis b infection among pregnant women attending the antenatal clinic at Mbagathi district hospital in Nairobi, Kenya. Pan Afr Med J. (2016) 24:1–7. doi: 10.11604/pamj.2016.24.315.9255
Keywords: hepatitis B virus, hepatitis B surface antigen, pregnancy, associated factors, Mogadishu city
Citation: Hassan SA, Ahmed YMA, Almugadam BS and Hassan YSA (2024) Prevalence and associated factors for hepatitis B infection among pregnant women attending antenatal clinic at SOS Hospital in Mogadishu, Somalia. Front. Glob. Womens Health 5:1279088. doi: 10.3389/fgwh.2024.1279088
Received: 8 September 2023; Accepted: 9 April 2024;
Published: 21 May 2024.
Edited by:
Rebecca F. Grais, Epicentre, FranceReviewed by:
Oluwadamilola Osasona, Redeemer's University, NigeriaPhilip Apraku Tawiah, Kwame Nkrumah University of Science and Technology, Ghana
Hussein Mukasa Kafeero, Islamic University in Uganda, Uganda
© 2024 Hassan, Ahmed, Almugadam and Hassan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yousif Mousa Alobaid Ahmed, YWJ1d2FkZGFoMjAxNkBnbWFpbC5jb20=
 Shafie Abdulkadir Hassan
Shafie Abdulkadir Hassan Yousif Mousa Alobaid Ahmed
Yousif Mousa Alobaid Ahmed Babiker Saad Almugadam1
Babiker Saad Almugadam1 Yahye Sheikh Abdulle Hassan
Yahye Sheikh Abdulle Hassan