
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Glob. Womens Health, 10 July 2024
Sec. Infectious Diseases in Women
Volume 5 - 2024 | https://doi.org/10.3389/fgwh.2024.1243280
 Sisay Melese Bittew1
Sisay Melese Bittew1 Seteamlak Adane Masresha2
Seteamlak Adane Masresha2 Getahun Fentaw Mulaw2
Getahun Fentaw Mulaw2 Mohammed Ahmed Yimam2
Mohammed Ahmed Yimam2 Abiot Alebel Zimamu1
Abiot Alebel Zimamu1 Atnaf Alem Abriham3
Atnaf Alem Abriham3 Atitegeb Abera Kidie2*
Atitegeb Abera Kidie2*
Background: The cells of the cervical epithelial wall are the source of the malignant tumor caused by the human papilloma virus (HPV) known as cervical cancer. In 2018, Ethiopia implemented the HPV vaccine specifically targeting girls aged 9–14 years. This vaccination initiative serves as an effective preventive measure against cervical cancer, provided that parents express a positive inclination to have their daughters vaccinated as part of the program.
Objective: The aim of the study was to assess parental willingness to vaccinate their daughters against human papillomavirus and its associated factors in Woldia town, Northeast Ethiopia.
Methods: A community-based cross-sectional study was conducted among 414 parents of daughters aged 9–14 years between 10 and 25 January 2023. Respondents were selected by a systematic sampling method and a face-to-face interview was conducted to collect data. Data were entered into Epi Data version 4.6 and exported to SPSS version 25 for analysis. Multivariable analyses were used to examine the association between dependent and independent variables. The adjusted odds ratio (AOR), 95% confidence interval (CI), and p-value <0.05 were used to determine statistical significance.
Results: A total of 410 study participants with a response rate of 99% were included in the study, and approximately 72.9% (95% CI: 68.3–77.2) of them were willing to vaccinate their daughters. This study found that parents with a family history of cervical cancer screening (AOR = 3.27, 95%; CI = 1.38–7.74), secondary and above educational status (AOR = 2.72, 95% CI = 1.29–5.73), good knowledge of the human papilloma virus vaccination (AOR = 3.00, 95% CI = 1.70–5.28), and favorable attitude toward the human papilloma virus vaccine (AOR = 4.40, 95% CI = 2.45–7.88) were significantly associated with parental willingness to vaccinate their daughters against human papilloma virus.
Recommendation: In this study, most parents were willing to vaccinate their daughters against human papilloma virus. The significant determinants of parental willingness to their daughter's human papilloma virus vaccination were family history of cervical cancer screening, level of education, and knowledge and attitude toward the human papilloma virus vaccine. Therefore, health information regarding the human papillomavirus vaccination with an emphasis on raising community awareness should be designed.
The cells of the cervical epithelial lining are responsible for the malignant tumors also known as cervical cancer (CC). Cervical cancer is known to be caused by the sexually transmitted disease (STD) human papilloma virus (HPV), particularly the HPV 16, 18, and 31 serotypes (1). Cervical cancer is a malignant disease of the cervix that occurs at a mean age of 54 years; with a pre-malignant stage that usually occurs in younger women below the age of 40 years (2). More than 80% of women who are sexually active have been infected with HPV at least once in their lifetime (3).
Cervical cancer is the fourth most common type of diagnosed and lethal cancer in the world (4). Global estimates for 2020 showed there were 604,000 new cases and 342,000 fatalities each year (5). More than 80% of the cases are found in developing countries (6). The highest rates of death and incidence are found in sub-Saharan Africa, accounting for more than 70% of the cervical cancer burden in the world (5, 7). In Eastern Africa in 2018, there were 52,633 cases of cervical cancer (8). It is now the second most common cancer-related cause of mortality in Ethiopian women, accounting for more than 7,600 new cases and more than 6,000 fatalities each year (9).
Strategies for the prevention and control of cervical cancer include vaccination programs, screening, and treatment with standard of care (10). In many high-income countries (HICs), several primary and secondary preventive measures are available to anticipate the majority of fatal cancer developments (11). Low- and middle-income countries (LMICs) lack the resources for screening, early detection, and successful treatment of precancerous cervical lesions, which is an indicator as to why the provision of vaccinations is fundamental, especially in these regions (12). High-grade precancerous lesions, aggressive malignancy, and HPV infections can all be avoided with HPV vaccines (13). Comprehensive strategies and guidelines are created by the World Health Organization (WHO), including the HPV vaccination as the primary prevention for approximately 90% of CCs (14, 15). The WHO, the Centers for Disease Control and Prevention (CDC), the European Centers for Disease Prevention and Control (ECDC), and the American Academy of Pediatrics (AAP) recommend HPV vaccination for girls aged 11–12 years and a catch-up vaccination for girls aged 13–18 years, regardless of sexual activity (16). Global coverage of the HPV vaccination was 39.7%, including high-income countries (68%), middle-income countries (28%), low- to middle-income countries (2.7%), and Ethiopia (<2%) (17). The Global Alliance for Vaccine and Immunization (GAVI) has provided Ethiopia with access to the HPV vaccine since 2018. It is delivered via a method centered on schools (18). In Ethiopia, misconceptions about the cause and vaccination of cervical cancer are common because of a lack of awareness and health-seeking behavior (18). Nevertheless, research revealed that unfounded allegations regarding the vaccine’s adverse effects had a negative influence on public trust and caused the HPV vaccine program to be suspended (19, 20). As a result of the national scale-up of the CC prevention program, assessing barriers for parental willingness and using the service through appropriate community studies is critical. Since the HPV vaccine targeted young adolescent girls, the success of the HPV vaccination depends on parental decisions and their willingness to vaccinate their daughters (21). There are numerous types of literature on the Ethiopian context that explore the prevalence of cervical cancer and its risk factors (22); however, parental willingness to give their daughters the HPV vaccination is not well assessed in many LMICs, which is worse in Ethiopia (12).
Empirical evidence about parents' willingness to vaccinate their daughter against HPV is necessary as it is affected by different factors, such as poor knowledge of the HPV vaccination, lack of information sources, low household monthly income, negative rumors about the vaccine’s side effects, and illiteracy (16, 23, 24). As a result, it can cause vaccine refusal by parents for their daughters (25). Therefore, this study intended to assess parental willingness to vaccinate their daughters against HPV and its associated factors in Woldia town, Northeast Ethiopia.
The study was conducted among parents of daughters who resided in Woldia town, which is located in the North Wollo Administrative Zone of Amhara regional State, Ethiopia.
A community-based cross-sectional study was carried out between 10 and 25 January 2023. Parents who had daughters aged 9–14 years in the selected kebeles of the town were the study population. Parents who had daughters aged 9–14 years and permanently residing in the study area (for ≥6 months) at the time of data collection were included. Parents whose daughters had previous or current marital history, had been pregnant previously, and/or were found to be pregnant at the time of data collection were excluded. A total of 414 respondents were selected using a multi-stage sampling technique.
Initially, kebeles were stratified as urban and rural, of which 50% of the total kebeles (three urban and two rural) were selected using the lottery method. Based on the data obtained from Woldia administrative town health department, the total number of households with eligible daughters in the town and selected Kebeles was 7,067 and 3,484, respectively. A proportional-to-sample size allocation (PSA) was then employed to determine the study participants from the selected kebeles. Next, 414 households were selected using a systematic sampling technique. One parent per household was interviewed. If both parents were present in the selected households, one was randomly chosen as a study participant. A structured face-to-face interviewer-administered questionnaire was used for data collection, which was developed after a thorough literature review of previously conducted studies. The questions for assessing knowledge and attitude were from previously validated tools of studies conducted in Ethiopia (18, 22, 24, 26).
The reliability of these questions was again assessed in this study and the reliability coefficient for each scale of the data collection tool revealed Cronbach alpha values of 0.95 and 0.74 for attitude and knowledge questioners, respectively.
The dependent variable of this study was parental willingness to their daughters’ HPV vaccination, which was categorized as yes/no. The independent variables of the study were sex, age, residence, religion, marital status, educational status, partner’s educational status, occupation, partner’s occupation, household monthly income, number of children, number of daughters (aged 9–14 years), family history of cervical cancer, family history of cervical cancer screening, family history of sexually transmitted infections (STIs), parental fear of STIs, daughters’ HPV vaccination history, source of information about HPV, trusted source of information, knowledge of the HPV vaccination, and attitude toward the HPV vaccine.
The terms used in this study were operationalized as follows:
Attitude: Attitude toward HPV vaccination was assessed by using a 12-item attitude questions with five Likert scales ranging from strongly disagree to strongly agree with a maximum score of 12 * 5 = 60. Those respondents who scored greater than the mean value were categorized as having a favorable attitude, or otherwise categorized as an unfavorable attitude (22).
Knowledge: Knowledge about the HPV vaccination was assessed using 15-item knowledge assessing questions with three responses: 1. Yes, 2. No, and 3. I do not know. Each correct and incorrect response scored 1 (yes = 1) and zero (no and I do not know = 0) points, respectively. The scores for each item were summed, and then those respondents who scored greater than the mean value were categorized as having good knowledge, otherwise poor knowledge (22).
The collected data were entered into Epi Data version 4.6 and then exported to the SPSS version 25 for analysis. The findings were summarized and presented by tables, graphs, and other summary measures. Binary logistic regression was employed for final analysis. In the bi-variable logistic regression analysis, all independent variables with a p-value <0.25 were candidates for multivariable logistic regression model. An explanatory variable with a p-value <0.05 in the multivariable logistic regression analysis was considered significantly associated with the outcome variable. The model goodness of fit was assessed using the Hosmer and Lemeshow test and the model was well-fitted (p-value = 0.57). The presence of multi-collinearity between independent variables was checked by examining the standard error of regression coefficients for each independent variable. The strength of association was measured by adjusted odds ratio (AOR) with corresponding 95% confidence interval (CI) and those variables with a p-value <0.05 were considered statistically significant factors for the outcome variable.
Out of 414 participants, 410 responded completely to the interview and yielded a response rate of 99%. More than three-quarters [3,140 (76.6%)] of the respondents were women. More than one-third [161 (39.3%)] of respondents were aged over 40 years, with a mean age of 38.6 ± 12.7 years. The majority [302 (73.6%)] of the respondents were married, 215 (52.4%) resided in urban areas, 273 (66.6%) had five or fewer children, and 360 (87.8%) had a daughter aged 9–14 years. Almost half [197 (48%)] of the study participants had a primary education and almost one-third [128 (31.2%)] of the respondents were housewives. Of the study respondents, more than half [226 (55%)] of them had a monthly income of less than 3,200 ETB (Table 1).
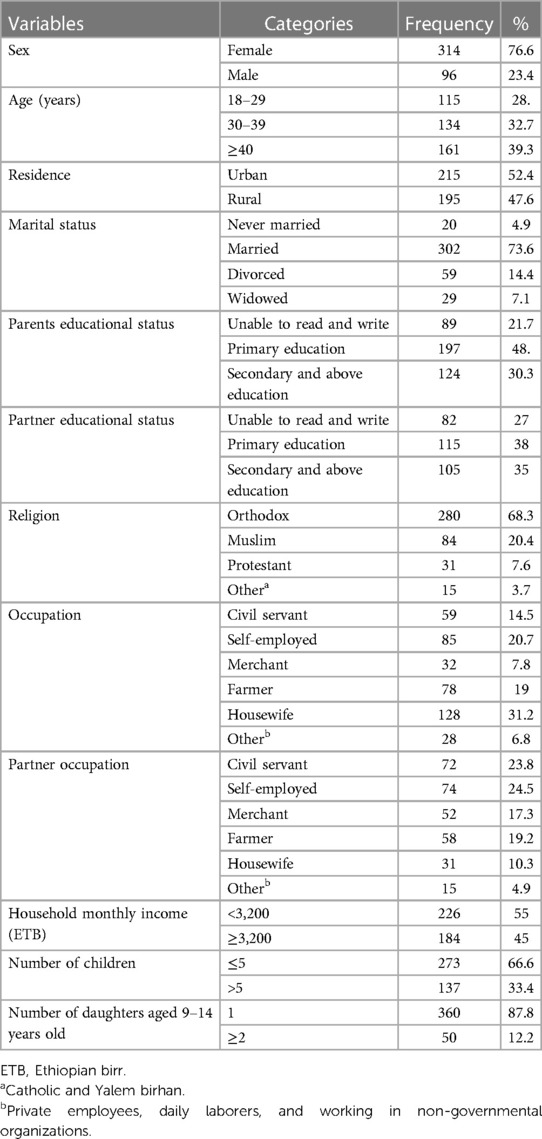
Table 1 Sociodemographic and economic characteristics of parental willingness to their daughters’ HPV vaccination in Woldia town, Northeast Ethiopia.
Most [377 (92%)] of the study participants had no family history of cervical cancer, 340 (82.9%) participants had no family history of cervical cancer screening, 243 (59.3%) did not fear STIs, 234 (57.1%) had a family history of STIs, and half of the study participants’ daughters had no history of HPV vaccination (Table 2).

Table 2 Reproductive health characteristics of parental willingness to their daughters’ HPV vaccination in Woldia town, Northeast Ethiopia.
The majority [237 (57.8%)] of study participants had heard about the HPV vaccination. Regarding source of information, 97 (40.9%) participants heard from television and/or radio and 51 (21.5%) heard from health extension workers. Of the participants who had information about the HPV vaccination, television and radio were the trusted sources for more than half [138 (58.2%)] of the respondents followed by health providers [49 (20.7%)]. The majority [286 (69.8%)] of the study participants had poor knowledge of the HPV vaccination and 302 (73.7%) had a favorable attitude toward the HPV vaccination (Table 3).
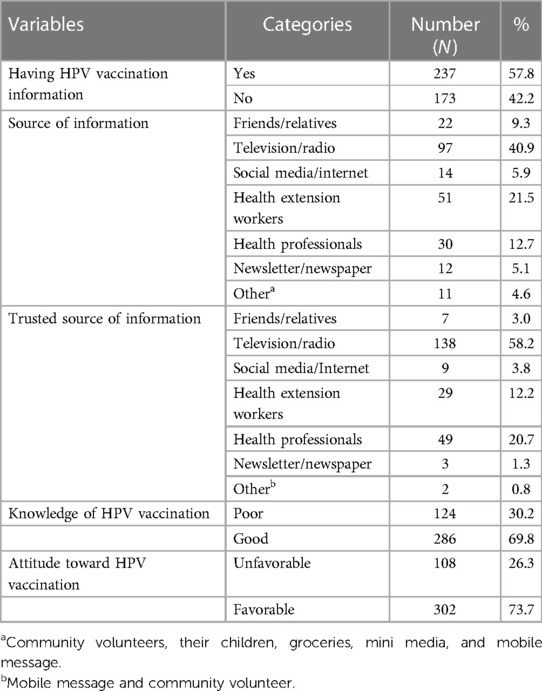
Table 3 Source of information, attitude, and knowledge about HPV vaccination among parents of daughters in Woldia town, Northeast Ethiopia.
Out of 410 interviewed parents, 299 (72.9%, 95% CI: 68.3–77.2) were willing to vaccinate their daughters against HPV infection. The major reasons for not willing to vaccinate their daughters were considering the HPV vaccine as not being widely accepted (negative rumors about the vaccine) (37%), being worried about safety (feared side effects and perceived injection pain) (27%), low personal perception of risk for cervical cancer (13.5%), and considering the vaccine not protective (12.6%) (Figure 1).
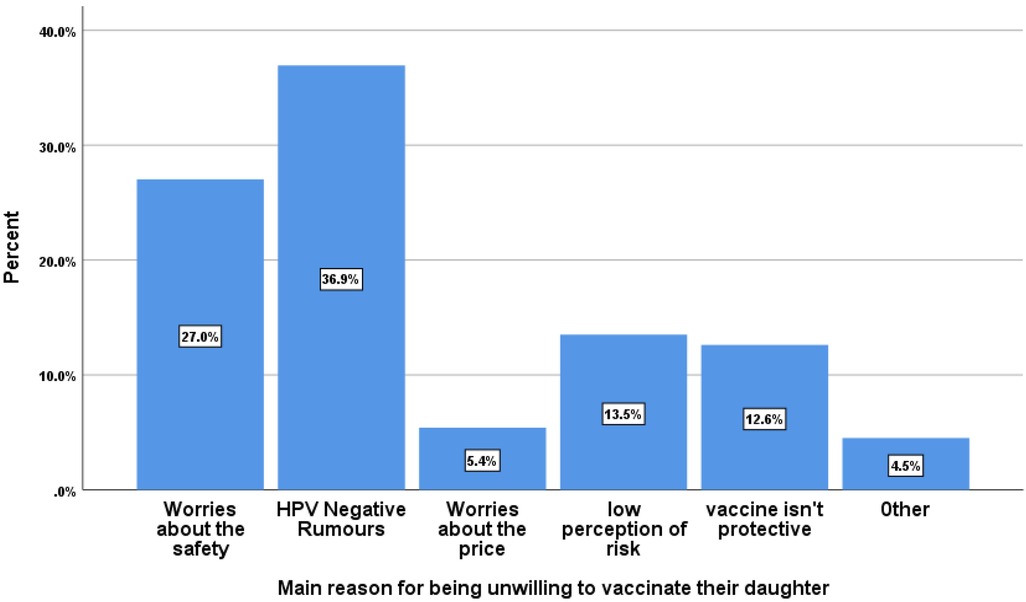
Figure 1 Main reasons for parental unwillingness toward the HPV vaccination in Woldia town, Northeast Ethiopia. Other = due to medical reasons or cultural and religious beliefs.
In the bi-variable analysis, variables such as age, number of children, number of daughters aged 9–14 years, family history of cervical cancer, family history of cervical cancer screening, family history of STIs, parents’ fear of STIs, daughter's HPV vaccination history, parents’ information about HPV, parents’ educational status, parents’ attitude and knowledge status about the HPV vaccination were eligible for a multivariable analysis at a p-value <0.25.
In the multivariable logistic regression analysis, parents with a family history of cervical cancer screening, secondary and higher education, good knowledge of and favorable attitude toward the HPV vaccination were significant factors for parental willingness for their daughter’s HPV vaccination at a p-value <0.05 (Table 4).
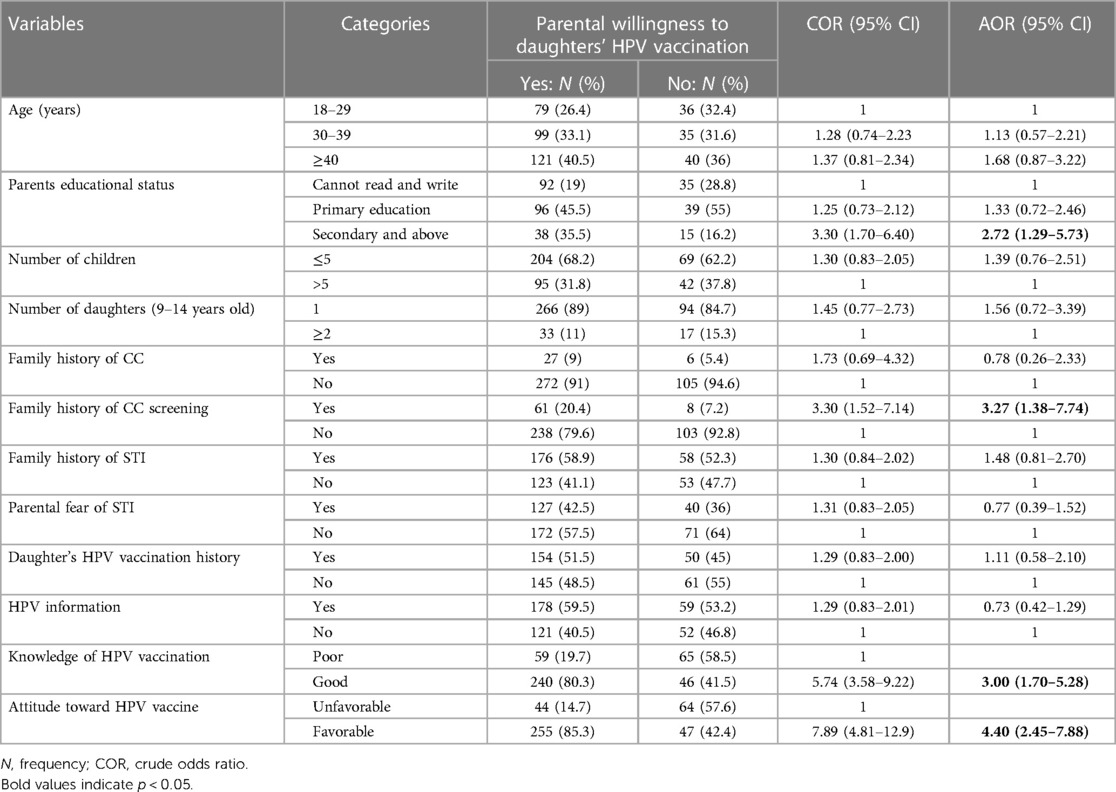
Table 4 Factors associated with parental willingness to their daughters’ HPV vaccination in Woldia town, Northeast Ethiopia.
In this study, respondents who had a family history of cervical cancer screening were three times more likely to be willing to vaccinate their daughters compared to parents who had no family history of cervical cancer screening (AOR = 3.27, 95% CI = 1.38–7.74). Those parents with a secondary and higher education were three times more likely to be willing to vaccinate their daughter against HPV compared to those parents who were unable to read and write (AOR = 2.72, 95% CI = 1.29–5.73).
Parents who had good knowledge of the HPV vaccination were three times more likely to be willing to vaccinate their daughters compared to those with poor knowledge (AOR = 3.00, 95% CI = 1.70–5.28). Parents who had a favorable attitude toward the HPV vaccination were four times more likely to be willing to vaccinate their daughter than those who had an unfavorable attitude (AOR = 4.40, 95% CI = 2.45–7.88) (Table 4).
This study was carried out to determine parental willingness to vaccinate their daughters against HPV and its associated factors in Woldia town, Northeast Ethiopia. The study showed that nearly three-quarters (72.9%); [95% CI (68.3%, 77.2%)] of parents were willing to vaccinate their daughters for HPV infection. This study is in line with research conducted in the United Arab Emirates (76.6%) (27); Argentina (74%) (28); a study about parental acceptance of HPV in Lagos, Nigeria (72%) (29); and Gondar, Northwest Ethiopia (69.3%) (30). However, the results of this study are lower than those in studies carried out in South Africa (80%) (27); Poland (85.1%) (16); Tanzania (93%) (31); Lagos, Nigeria (81.8%) (32); Gondar, Northwest Ethiopia (81.3%) (22), and Addis Ababa, Ethiopia (94.3%) (33). As a result of the recent implementation of the HPV vaccination program in Ethiopia, the observed difference in vaccination rates could be attributed to concerns and negative rumors surrounding the potential side effects of the vaccine, as well as a lack of awareness regarding the personal risk of developing cervical cancer in the specific area under study. These findings are consistent with previous research that has identified similar factors as barriers to vaccination. This is supported by previous studies that reported similar reasons (24).
In addition, some of the above studies were carried out after the provision of HPV vaccines to daughters, which may improve parental willingness (27, 31, 32). The variation in the willingness rate from the study conducted in Addis Ababa could be due to the difference in the sociodemographic characteristics of the participants. Those living in Addis Ababa have greater access to health-based information, as expected, with a high level of health literacy compared to this study area, and there was a school-based HPV vaccination campaign in the city. Therefore, the parents might have heard and made their decision about the vaccination (33).
Conversely, the results of this study showed that there was a high level of parental willingness to vaccinate their daughters compared to those in previous studies conducted in Debre Tabor, Ethiopia (48.67%) (24) and Nigeria (67.4%) (34). The high vaccination acceptance rate may be attributable to the ongoing regional campaigns to raise awareness of cervical cancer and promote screening. The other reason in the present study, compared to the above studies, might be due to the current region-based cervical cancer awareness creation and screening campaign.
During the process of gathering data for this study, a campaign was launched in the town to raise awareness of the prevention of cervical cancer at the community level and cervical cancer screening service was being given in the town at the health facility level. The participants in the study may already possess knowledge about the HPV vaccination, which further increased their willingness (21). The high rate of willingness in this study area compared to Nigeria may be attributed to variations in the sociodemographic characteristics of the study participants (16). It might also be due to the introduction of the routine free HPV vaccination program at schools in this study area compared to Nigeria where vaccination is paid for out of pocket (18). The difference in the study period could contribute to the fact that earlier studies might represent periods when less information regarding the benefit of vaccines and the challenges posed by the disease was available (24, 34).
In this study, parents with secondary and higher educational status were more likely to be willing to vaccinate their daughters compared to participants who were unable to read and write. This finding of this study is similar to that in other studies conducted in the United States (USA) (35); China (36); Lagos, Nigeria (32); Alabama (37); Bench-Sheko zone, southwest Ethiopia (20); and Debre Tabor, Ethiopia (24). Parents that are better educated might have better access to information from schools, mass media, newspapers, and the Internet (24). Parents with higher levels of education might know about a specific disease and fear about their susceptibility to the disease, which creates health-seeking behavior that leads to an intention to understand the prevention of HPV infection. Thus, the educational level of parents significantly influences their willingness to vaccinate their daughters (19). However, apart from parental educational status, there was no significant association between other sociodemographic characteristics of respondents. This is supported by previous studies that reported similar findings (20, 37).
Parents with a family history of cervical cancer screening were more likely to be willing to vaccinate their daughters compared to parents who had no family history of cervical cancer screening. Parents who had a health facility visit for cervical cancer screening might have been exposes to cervical cancer counseling and important information on cervical cancer and HPV vaccinations. Therefore, this might create awareness, a favorable attitude toward the HPV vaccination, and the intention to understand the prevention of HPV infection, finally leading to willingness to vaccinate their daughters as well (38).
Parents with a good knowledge of the HPV vaccination were more likely to be willing to vaccinate their daughters against HPV than those with poor knowledge. This study finding is in line with those in previous studies conducted in Canada (39); Asia (40), Kilimanjaro Region, Tanzania (31); Gondar, Ethiopia (22); Bench-Sheko zone, southwest Ethiopia (20); Debre Tabor, Ethiopia (24); and Hadiya Zone, southern Ethiopia (41). This highlights that parental willingness to vaccinate their daughters against HPV is affected by their overall knowledge of HPV vaccination. This shows that knowledge of HPV and its vaccination triggers the participants to read and understand more about the route of transmission, consequence of infection, and complications of cervical cancer that may lead to behavioral change, which leads them to accept the HPV vaccination for their daughters (24, 42).
Parents who held a positive attitude toward HPV vaccination demonstrated a greater willingness to vaccinate their daughters against HPV infection compared to those who held a negative attitude. This is supported by study findings in South India (43); Iran (44); Gondar, Ethiopia (22); Bench-Sheko zone, Ethiopia (20); and Addis Ababa, Ethiopia (33). The reason for this could be attributed to the parents’ acceptance of the HPV vaccine, which is significantly influenced by their attitudes and beliefs regarding the vaccine's effectiveness, safety, and accessibility (14). Furthermore, the overall beliefs concerning the potential harm or benefits associated with the HPV vaccine can play a crucial role in determining a parent's decision to utilize the vaccine (23).
The major reasons why parents were not willing to vaccinate their daughters were considering the HPV vaccine not being widely accepted (negative rumors about the vaccine) (37%), being worried about safety (feared adverse effects and perceived injection pain) (27%) and having a low personal perception of risk for cervical cancer (13.5%). This is similar to other studies conducted in China, which indicated that approximately 43% of parents were worried about the safety and side effects of the HPV vaccine (45), in Nigeria, where 48.1% of parents were worried about adverse effects and 25.9% complained of poor availability of the vaccine (32), and in Debre Tabor, Ethiopia, where scarcity/cost of the HPV vaccine (57.4%), poor information about HPV vaccine (15.2%), undesirable impact on fertility (14.2%), and feared side effects (7.6%) were the reasons of parents for unwilling to vaccinate their daughters (24). A possible reason might be due to differences in sociodemographic characteristics, level of information, attitude, and knowledge status toward the HPV vaccination (29, 40).
The strength of the study lies in its community-based study design, which used a representative sample of participants who were residents in both the urban and rural areas of Woldia town.
However, the study has some limitations. First, the study could not address “how” and “why” questions. In addition, it might be affected by desirability and recall bias since the data were collected from the participants’ self-report.
This study revealed that most parents were willing to vaccinate their daughters against HPV and it was significantly associated with family history of cervical cancer screening, parents’ level of education, parents’ knowledge of HPV vaccination, and parents’ attitude toward the HPV vaccination. Therefore, efforts should be made to increase awareness in the community of cervical cancer and its prevention to ensure sustainable parental willingness to the HPV vaccination. Specifically, educational campaigns should be conducted to disseminate information about cervical cancer, its causes, risk factors, and the importance of HPV vaccination. Collaboration with local healthcare providers would also be helpful to disseminate information about the prevention of cervical cancer and the HPV vaccination. Mixed studies are better for further investigations as they would provide a comprehensive understanding of why individuals may be unwilling to vaccinate their daughters. This approach can provide valuable insights into the “how and why” behind vaccine hesitancy among individuals, families, and communities, ultimately informing targeted strategies to address this important public health issue.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Woldia University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their verbal informed consent to participate in this study.
SA, SM, AK, AZ, MY and AA wrote the proposal, participated in the data collection and entry processes, analyzed the data, and drafted the manuscript. GM was Involved in the interpretation of the results and reviewed the manuscript. All authors contributed substantially to the article and approved the final version of the submitted manuscript.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
We express our deepest gratitude to Woldia University College of Health Science, School of Public Health for its wide-ranging support in creating an arrangement for an appropriate platform for this study. Our special thanks and sincere appreciation also go to Woldia administrative town health department staff for the provision of the necessary information that was an important input for the study. Finally, we would like to extend our thanks to all study participants, data collectors, and other individuals or organizations that have participated directly or indirectly in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, adjusted odds ratio; CC, cervical cancer; COR, crude odds ratio; GAVI, Global Alliance for Vaccine and Immunization; HPV, human papilloma virus; STI, sexually transmitted infection.
1. Lin W, Wang Y, Liu Z, Chen B, Yuan S, Wu B, et al. Awareness and attitude towards human papillomavirus and its vaccine among females with and without daughter(s) who participated in cervical cancer screening in Shenzhen, China. Trop Med Int Health. (2019) 24(9):1054–63. doi: 10.1111/tmi.13283
2. Akinleye HW, Kanma-Okafor OJ, Okafor IP, Odeyemi KA. Parental willingness to vaccinate adolescent daughters against human papilloma virus for cervical cancer prevention in Western Nigeria. Pan Afr Med J. (2020) 36(1). doi: 10.11604/pamj.2020.36.112.19007
3. Midaksa M, Destaw A, Addissie A, Kantelhardt EJ, Gizaw M. Women’s sexual autonomy as a determinant of cervical cancer screening uptake in Addis Ababa, Ethiopia: a case–control study. BMC Women’s Health. (2022) 22(1):1–8. doi: 10.1186/s12905-022-01829-4
4. Wollancho W, Amdissa D, Bamboro S, Wasihun Y, Tareke KG, Gizaw AT. Determining behavioral intention and its predictors towards cervical cancer screening among women in Gomma district, Jimma, Ethiopia: application of the theory of planned behavior. PLoS One. (2020) 15(11):e0238472. doi: 10.1371/journal.pone.0238472
5. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71(3):209–49. doi: 10.3322/caac.21660
6. Bruni L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, et al. “ICO/IARC information centre on HPV and cancer (HPV information centre). Human papillomavirus and related diseases in the world. Summary Report 17 June 2019.” (2019). Available online at: https://hpvcentre.net/statistics/reports/ETH.pdf (Accessed March 10, 2023).
7. Ayenew AA, Zewdu BF, Nigussie AA. Uptake of cervical cancer screening service and associated factors among age-eligible women in Ethiopia: systematic review and meta-analysis. Infect Agents Cancer. (2020) 15(1):1–17. doi: 10.1186/s13027-020-00334-3
8. Ruddies F, Gizaw M, Teka B, Thies S, Wienke A, Kaufmann AM, et al. Cervical cancer screening in rural Ethiopia: a cross-sectional knowledge, attitude and practice study. BMC Cancer. (2020) 20(1):1–10. doi: 10.1186/s12885-020-07060-4
9. Kasim J, Kalu A, Kamara B, Alema HB. Cervical cancer screening service utilization and associated factors among women in the Shabadino district, Southern Ethiopia. J Cancer Epidemiol. (2020) 2020(1):6398394. doi: 10.1155/2020/6398394
10. Endarti D, Kristina SA, Farida MA, Rahmawanti Y, Andriani T. Knowledge, perception, and acceptance of HPV vaccination and screening for cervical cancer among women in Yogyakarta province, Indonesia. Asian Pac J Cancer Prev. (2018) 19(4):1105. doi: 10.22034/APJCP.2018.19.4.1105
11. Paz-Zulueta M, Álvarez-Paredes L, Rodríguez Díaz JC, Parás-Bravo P, Andrada Becerra M, Rodríguez Ingelmo JM, et al. Prevalence of high-risk HPV genotypes, categorised by their quadrivalent and nine-valent HPV vaccination coverage, and the genotype association with high-grade lesions. BMC Cancer. (2018) 18(1):1–9. doi: 10.1186/s12885-018-4033-2
12. Lack A, Hiligsmann M, Bloem P, Tünneßen M, Hutubessy R. Parent, provider and vaccine preferences for HPV vaccination: a systematic review of discrete choice experiments. Vaccine. (2020) 38(46):7226–38. doi: 10.1016/j.vaccine.2020.08.078
13. Alaamri AM, Alghithi AM, Salih S, Omer HM, Alaamri AM, Alghithi A, et al. Acceptance and associated risk factors of human papillomavirus vaccine among parents of daughters in intermediate schools in Tabuk city, Saudi Arabia. Cureus. (2023) 15(8). doi: 10.7759/cureus.43483
14. Kristina SA, Permitasari NPAL. Knowledge, attitudes and barriers towards human papillomavirus (HPV) vaccination in developing economies countries of South-East Asia region: a systematic review. Sys Rev Pharm. (2019) 10(1):81–6. doi: 10.5530/srp.2019.1.13
15. Kamolratanakul S, Pitisuttithum P. Human papillomavirus vaccine efficacy and effectiveness against cancer. Vaccines. (2021) 9(12):1413. doi: 10.3390/vaccines9121413
16. Ganczak M, Owsianka B, Korzeń M. Factors that predict parental willingness to have their children vaccinated against HPV in a country with low HPV vaccination coverage. Int J Environ Res Public Health. (2018) 15(4):645. doi: 10.3390/ijerph15040645
17. Bruni L, Diaz M, Barrionuevo-Rosas L, Herrero R, Bray F, Bosch FX, et al. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob Health. (2016) 4(7):e453–63. doi: 10.1016/S2214-109X(16)30099-7
18. Tesfaye ZT, Gebreyohannes EA, Bhagavathula AS, Getaneh MM, Tegegn HG. Awareness and knowledge of human papillomavirus and cervical cancer among female medical and health science students at university of Gondar. J Glob Oncol. (2017) 3(2). doi: 10.1200/JGO.2017.009688
19. Kassa HN, Bilchut AH, Mekuria AD, Lewetie EM. Practice and associated factors of human papillomavirus vaccination among primary school students in Minjar-Shenkora District, North Shoa Zone, Amhara Regional State, Ethiopia, 2020. Cancer Manag Res. (2021) 13:6999–7008. doi: 10.2147/CMAR.S324078
20. Destaw A, Yosef T, Bogale B. Parents willingness to vaccinate their daughter against human papilloma virus and its associated factors in Bench-Sheko zone, Southwest Ethiopia. Heliyon. (2021) 7(5):e07051. doi: 10.1016/j.heliyon.2021.e07051
21. Chan CK, Aimagambetova G, Ukybassova T, Kongrtay K, Azizan A. Human papillomavirus infection and cervical cancer: epidemiology, screening, and vaccination—review of current perspectives. J Oncol. (2019) 2019(1):3257939. doi: 10.1155/2019/3257939
22. Alene T, Atnafu A, Mekonnen ZA, Minyihun A. Acceptance of human papillomavirus vaccination and associated factors among parents of daughters in Gondar town, Northwest Ethiopia. Cancer Manag Res. (2020) 12:8519. doi: 10.2147/CMAR.S275038
23. Netfa F, Tashani M, Booy R, King C, Rashid H, Skinner SR. Knowledge, attitudes and perceptions of immigrant parents towards human papillomavirus (HPV) vaccination: a systematic review. Trop Med Infect Dis. (2020) 5(2):58. doi: 10.3390/tropicalmed5020058
24. Mihretie GN, Liyeh TM, Ayele AD, Belay HG, Yimer TS, Miskr AD. Knowledge and willingness of parents towards child girl HPV vaccination in Debre Tabor town, Ethiopia: a community-based cross-sectional study. Reprod Health. (2022) 19(1):1–12. doi: 10.1186/s12978-022-01444-4
25. Roy S, Dubey A, Saini D, Khanna M, Kamal VK, Yau C, et al. Knowledge, attitude and practice regarding HPV vaccine among parents and caregivers of female child attending pediatric OPD: intervention for primary prevention. Ind J Soc Prev Rehab Oncol. (2017) 1(2):34–40.
26. Tarekegn AA, Yismaw AE. Health professionals’ willingness to pay and associated factors for human papilloma virus vaccination to prevent cervical cancer at College of Medicine and Health Sciences University of Gondar, Northwest Ethiopia. BMC Res Notes. (2019) 12(1):1–6. doi: 10.1186/s13104-019-4085-7
27. Hoque ME. Acceptability of human papillomavirus vaccination among academics at the university of KwaZulu-Natal, South Africa. S Afr Fam Pract. (2015) 57(5):318–21. doi: 10.1080/20786190.2015.1078157
28. Arrossi S, Maceira V, Paolino M, Sankaranarayanan R. Acceptability and uptake of HPV vaccine in Argentina before its inclusion in the immunization program: a population-based survey. Vaccine. (2012) 30(14):2467–74. doi: 10.1016/j.vaccine.2012.01.032
29. Rabiu KA, Alausa TG, Akinlusi FM, Davies NO, Shittu KA, Akinola OI. Parental acceptance of human papillomavirus vaccination for adolescent girls in Lagos, Nigeria. J Family Med Prim Care. (2020) 9(6):2950. doi: 10.4103/jfmpc.jfmpc_102_20
30. Geneti HB, Hailu DA, Muleta G. Assessment of the knowledge, attitude and acceptability towards human papillomavirus and its vaccine among undergraduate female medical students. Gynecol Obstet (Sunnyvale). (2016) 6(11):1–9. doi: 10.4172/2161-0932.1000410
31. Cunningham MS, Skrastins E, Fitzpatrick R, Jindal P, Oneko O, Yeates K, et al. Cervical cancer screening and HPV vaccine acceptability among rural and urban women in Kilimanjaro region, Tanzania. BMJ Open. (2015) 5(3):e005828. doi: 10.1136/bmjopen-2014-005828
32. Okunade KS, Sunmonu O, Osanyin GE, Oluwole AA. Knowledge and acceptability of human papillomavirus vaccination among women attending the gynaecological outpatient clinics of a university teaching hospital in Lagos, Nigeria. J Trop Med. (2017) 2017(1):8586459. doi: 10.1155/2017/8586459
33. Dereje N, Ashenafi A, Abera A, Melaku E, Yirgashewa K, Yitna M, et al. Knowledge and acceptance of HPV vaccination and its associated factors among parents of daughters in Addis Ababa, Ethiopia: a community-based cross-sectional study. Infect Agents Cancer. (2021) 16(1):1–7. doi: 10.1186/s13027-021-00399-8
34. Makwe CC, Anorlu RI. Knowledge of and attitude toward human papillomavirus infection and vaccines among female nurses at a tertiary hospital in Nigeria. Int J Womens Health. (2011) 3:313–7. doi: 10.2147/IJWH.S22792
35. Mohammed KA, Vivian E, Loux TM, Arnold LD. Factors associated with parents’ intent to vaccinate adolescents for human papillomavirus: findings from the 2014 national immunization survey–teen. Prev Chronic Dis. (2017) 14:E45. doi: 10.5888/pcd14.160314
36. Baumann A, Andersen B, Østergaard L, Larsen MB. Sense & sensibility: decision-making and sources of information in mothers who decline HPV vaccination of their adolescent daughters. Vaccine X. (2019) 2:100020. doi: 10.1016/j.jvacx.2019.100020
37. Litton AG, Desmond RA, Gilliland J, Huh WK, Franklin FA. Factors associated with intention to vaccinate a daughter against HPV: a statewide survey in Alabama. J Pediatr Adolesc Gynecol. (2011) 24(3):166–71. doi: 10.1016/j.jpag.2011.01.004
38. Suzuki Y, Sukegawa A, Ueda Y, Sekine M, Enomoto T, Melamed A, et al. The effect of a web-based cervical cancer survivor’s story on parents’ behavior and willingness to consider human papillomavirus vaccination for daughters: randomized controlled trial. JMIR Public Health Surveill. (2022) 8(5):e34715. doi: 10.2196/34715
39. Fernandes R, Potter BK, Little J. Attitudes of undergraduate university women towards HPV vaccination: a cross-sectional study in Ottawa, Canada. BMC Women’s Health. (2018) 18(1):1–9. doi: 10.1186/s12905-018-0622-0
40. Farsi NJ, Al Sharif S, Al Qathmi M, Merdad M, Marzouki H, Merdad L. Knowledge of human papillomavirus (HPV) and oropharyngeal cancer and acceptability of the HPV vaccine among dental students. Asian Pac J Cancer Prev. (2020) 21(12):3595. doi: 10.31557/APJCP.2020.21.12.3595
41. Larebo YM, Elilo LT, Abame DE, Akiso DE, Bawore SG, Anshebo AA, et al. “Awareness, acceptance and associated factors of human papillomavirus vaccine among parents of daughters in Hadiya zone, Southern Ethiopia: a cross-sectional study.” medRxiv (2022).
42. Kolek CO, Opanga SA, Okalebo F, Birichi A, Kurdi A, Godman B, et al. Impact of parental knowledge and beliefs on HPV vaccine hesitancy in Kenya—findings and implications. Vaccines. (2022) 10(8):1185. doi: 10.3390/vaccines10081185
43. Shetty S, Prabhu S, Shetty V, Shetty AK. Knowledge, attitudes and factors associated with acceptability of human papillomavirus vaccination among undergraduate medical, dental and nursing students in South India. Hum Vaccin Immunother. (2019) 15(7-8):1656–65. doi: 10.1080/21645515.2019.1565260
44. Taebi M, Riazi H, Keshavarz Z, Afrakhteh M. Knowledge and attitude toward human papillomavirus and HPV vaccination in Iranian population: a systematic review. Asian Pac J Cancer Prev. (2019) 20(7):1945. doi: 10.31557/APJCP.2019.20.7.1945
Keywords: HPV, daughters, Northeast Ethiopia, parental willingness, North Wollo Zone
Citation: Bittew SM, Masresha SA, Mulaw GF, Yimam MA, Zimamu AA, Abriham AA and Kidie AA (2024) Parental willingness to vaccinate their daughters against human papilloma virus and its associated factors in Woldia town, Northeast Ethiopia. Front. Glob. Womens Health 5:1243280. doi: 10.3389/fgwh.2024.1243280
Received: 20 June 2023; Accepted: 31 May 2024;
Published: 10 July 2024.
Edited by:
Rebecca F. Grais, Epicentre, FranceReviewed by:
Linda Dong-Ling Wang, Yangzhou University, China© 2024 Bittew, Masresha, Mulaw, Yimam, Zimamu, Abriham and Kidie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Atitegeb Abera Kidie, YXRpdGVnZWJhYmVyYUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.