- 1School of Hygiene and Preventive Medicine (Department of Biomedical and Neuromotor Sciences), University of Bologna, Bologna, Italy
- 2Botswana Sexual and Reproductive Health Initiative, Botswana Harvard AIDS Institute Partnership, Gaborone, Botswana
- 3Department of Epidemiology and Evaluation, London School of Hygiene & Tropical Medicine, London, United Kingdom
- 4Institute of Global Health and Infectious Diseases, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 5Clinical Research Department, Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, United Kingdom
- 6MRC Centre for Reproductive Health, University of Edinburgh, Edinburgh, United Kingdom
During the COVID-19 pandemic, family planning services over the world have been disrupted. There are still uncertainties about the impact on access to contraception, particularly among marginalised populations. This study aimed to assess the effect of COVID-19 on women's access to contraception, focusing on those experiencing loss of income and self-isolation. The International Sexual Health and Reproductive Health (I-SHARE) survey collected data from 5,216 women in 30 countries. Multivariable logistic regression was conducted to assess the association between loss of income during the pandemic, self-isolation and reduced access to contraception. Women experiencing loss of income and those who had self-isolated had reduced access to contraception (respectively aOR 2.3 and 1.7, for both p < 0.001). Most women reported inaccessibility of health centres, fear of COVID-19, and stockouts as reasons for reduced access. This study highlights how socio-demographic differences may have impacted access to contraception during the pandemic. People experiencing income loss and self-isolation might have faced increased barriers to family planning during the pandemic. Contraception should be prioritised in times of crisis: when planning services, financial support, telehealth and other measures should be implemented in order to increase access and reduce inequalities.
1 Introduction
Access to contraception is central to reducing poverty, empowering women and achieving sustainable development. The COVID-19 pandemic limited people's timely access to contraception (1, 2). Both COVID-19 itself and the public health measures implemented have weakened economies and destabilised health systems; health disparities have increased (3). According to the World Economic Forum, one in two people lost income during COVID-19 (4). Family planning services have been disrupted because many health facilities closed and healthcare professionals focused on COVID-19. In addition, people were unable to access health services because of travel restrictions, unaffordability and fear of COVID-19 (5). Telehealth and related adaptations have been variably implemented.
More research is needed on the pandemic's impact on already underserved populations, and on the mechanisms that led to reduced access (1). This analysis aimed to assess women's access to contraception during the pandemic at a multi-country level, focusing on those experiencing loss of income and self-isolation.
2 Methods
We used data from the International Sexual Health And REproductive health (I-SHARE) survey, a cross-sectional online survey conducted between 2020 and 2021 in 30 countries. There were 23,067 respondents to the survey. Sampling methods varied between countries and included convenience sampling, population-representative samples, and online panels (23, 2 and 6 countries respectively; one country used two methods). Details on the survey methods have been published (6) and the survey instrument, the countries included, their sample size and sampling strategy are attached in the Supplementary Materials.
For this paper, we restricted the analyses to participants who were assigned female sex at birth, younger than 50 years old. Participants were asked about their pregnancy intentions: we included only those who selected the option “Not currently pregnant and don't wish to be in the near future”. We excluded participants who reported having reached menopause, those with fertility issues, and those who were not sexually active. We also excluded participants who reported that they hadn't needed to seek or obtain contraceptives during the pandemic, and those with missing data on the outcome of access to contraception. The final population for this analysis included 5,216 participants (flowchart of participant inclusion in Supplementary Materials). Included participants were mainly from Europe (55.1%) and Latin America and the Caribbean (34.6%).
Reduced access to contraception was defined as a positive answer to the question “Have the COVID-19 social distancing measures stopped or hindered you from seeking or obtaining contraception?”. The two main exposure variables investigated were personal loss of income and self-isolation due to COVID-19.
We used multivariable logistic regression to explore the association between the exposures of interest and the outcome. Country of residence was included a priori in the regression models as a fixed-effect; to adjust for confounding for socio-demographic variables, we used a forward causal modelling strategy with a change-in-estimate approach. We introduced one by one in the model the variables that were associated with both exposure and outcome in the bivariable analysis, and then kept in the model the confounder that changed the OR more. We repeated this process until the OR for the exposure didn't change any more. Missing data was treated by pairwise deletion (available-case analysis).
3 Results
The analysed population was predominantly young, heterosexual, cisgender and highly educated; more than half were in a relationship (Table 1). Overall, around a third of the participants reported losing income during the pandemic. One in four had isolated due to COVID-19.
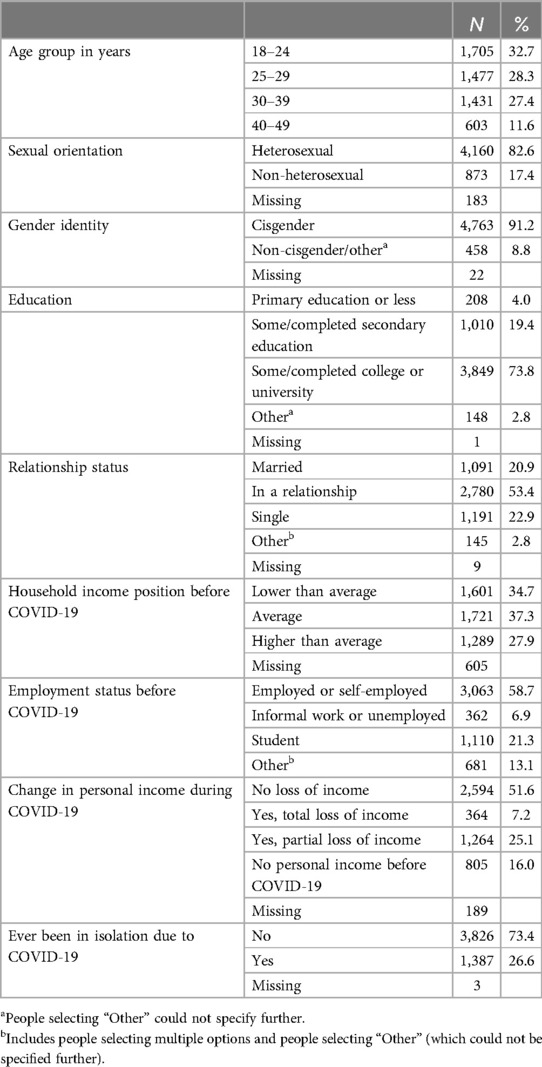
Table 1. Socio-demographic characteristics of the participants included in this analysis (N = 5,216). The percentages only apply to non-missing data out of the total study population. I-SHARE online survey 2020/21.
Overall, 9.1% of the respondents (476/5,216) reported being stopped from seeking or accessing contraception due to COVID-19. Most reported inaccessibility of health centres, fear of COVID-19 and stockouts as reasons for reduced access.
After adjusting for country, age and household income position before COVID-19, those who had experienced a total loss of income had twice the odds of reporting reduced access to contraception compared to those who had no loss of income (aOR 2.3, 95% CI: 1.7–3.3, p < 0.001). Those experiencing a partial loss of income also had higher odds of reduced access to contraception (aOR 1.3, 95% CI: 1.0–1.7, p = 0.04) (Table 2).
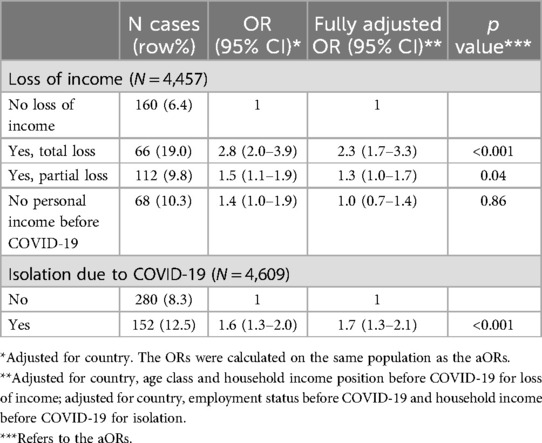
Table 2. Association between the two main exposures and reduced access to contraception. I-SHARE online survey 2020/21.
After adjusting for country, employment and household income before the pandemic, those that had been isolated had 1.7 times the odds of reporting reduced access to contraception compared to those who had not isolated (95% CI: 1.3–2.1, p < 0.001) (Table 2).
4 Discussion
This study highlights how people experiencing income loss and self-isolation may have faced increased barriers to family planning during the pandemic. Personal loss of income and financial insecurity have been linked to reduced access to contraception in other online surveys conducted in the USA (1, 7). Income loss has also been associated with increased odds of not using a preferred contraceptive method (8), which in itself could lead to an increased risk of contraception discontinuation and unintended pregnancy. Loss of income might lead to reduced contraception access due to unaffordability. Direct costs such as the visit or the contraceptive itself could be prohibitive. Indirect costs such as travel and opportunity loss due to missed time at work can also act as barriers. According to a study conducted in Brazil, ethnicity, low education and unemployment also contributed to difficulties with contraceptive methods (9). The link between self-isolation and reduced contraception access has been also described by Kavanaugh and colleagues, who illustrated how those who had tested positive for COVID-19 had 80% higher odds of experiencing healthcare delays (10). These delays, combined with economic insecurity, increase the barriers to contraception, disproportionately affecting already vulnerable groups. To improve access to contraception for these communities, it would be beneficial to have an intersectional approach (11), that considers the overlapping social, economic and cultural factors that contribute to these disparities, including violence, gender-based discrimination, and cultural norms. Violence, including intimate partner violence, could further restrict access to contraception by limiting individuals' ability to seek healthcare or make autonomous reproductive decisions (12). Future research should explore how these factors intersect and compound barriers to contraception access.
This study explores access to contraception during COVID-19 at a multi-country level and includes a relatively large sample size. The study is limited by the data collection method—an online survey—and the sampling method, which was convenience sampling for the majority of the countries involved; only two countries used population-representative sampling. The survey's distribution within sexual health networks likely resulted in respondents being more aware of contraception needs and access, potentially overestimating barriers. Since I-SHARE was an open online survey, the sampling frame is unknown; we cannot determine how many people received the survey link or how many began the survey. This reduces the generalizability of the results, particularly in low-resource settings or among populations with limited internet access (13). Missing data might also represent a source of bias in the study: 18% of the population did not respond to the question on access to contraception, and there were significant differences between those who did and those who did not answer (i.e., they were older, more frequently non-heterosexual and non-cisgender). This may indicate that certain demographic groups were underrepresented, which could affect the robustness of our results. Finally, the association between the exposures of interest may vary significantly according to country; however, it was not possible to calculate measures of association at the country level due to the low number of participants in some countries. Future research should explore these differences in more depth at the country or regional level.
COVID-19 likely exacerbated pre-existing problems and inequalities in contraception access, but it has also highlighted innovative ways to provide contraception and opened new opportunities for more diverse and inclusive services in the future, such as telehealth (14). When planning contraceptive services that may be resilient to epidemics and other health crises, financial support for people who have lost income (15), telehealth and other measures, such as self-administered contraception and postal prescriptions, should therefore be implemented to preserve contraception access and reduce inequalities. More research is needed on the mechanisms that led to reduced access, and on the consequences of reduced contraception access, like increased contraceptive discontinuation: UNFPA has estimated 1.4 million unintended pregnancies in 2020 (16), but there is currently no evidence on the longer-term consequences (17). Finally, future research could explore the role of financial support for those who have lost income during public health crises, and how such support may help mitigate barriers to contraception access.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to Joe Tucker,amR0dWNrZXJAbWVkLnVuYy5lZHU=.
Ethics statement
The studies involving humans were approved by University of Ghent Ethics Committee; University of North Carolina IRB. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their informed consent online to participate in this study.
Author contributions
SC: Conceptualization, Methodology, Formal Analysis, Writing – original draft. RR: Data curation. AM: Data curation. JH: Methodology, Supervision. JT: Conceptualization, Data curation, Writing – review & editing. CM: Conceptualization, Data curation, Supervision, Writing – review & editing.
Acknowledgments
We would like to thank the members of the ISHARE research consortium (a list can be found at https://docs.google.com/spreadsheets/d/1tHIXp0sM92CrpNDASdN_3hGIH7rj2x9FWY4Gmze6lgs/edit#gid=0).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1235475/full#supplementary-material
References
1. Mukherjee TI, Khan AG, Dasgupta A, Samari G. Reproductive justice in the time of COVID-19: a systematic review of the indirect impacts of COVID-19 on sexual and reproductive health. Reprod Health. (2021) 18:252. doi: 10.1186/s12978-021-01286-6
2. Tam MW, Davis VH, Ahluwalia M, Lee RS, Ross LE. Impact of COVID-19 on access to and delivery of sexual and reproductive healthcare services in countries with universal healthcare systems: a systematic review. PLoS One. (2024) 19(2):e0294744. doi: 10.1371/journal.pone.0294744
3. Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. (2020) 74(11):964–8. doi: 10.1136/jech-2020-214401
4. World Economic Forum. One in two people globally lost income due to the pandemic. Available online at: https://www.weforum.org/agenda/2021/05/how-many-people-experienced-a-lower-income-due-to-covid-19/ (Cited August 19, 2022).
5. Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. (2021) 11(3):e045343. doi: 10.1136/bmjopen-2020-045343
6. Michielsen K, Larrson EC, Kågesten A, Erausquin JT, Griffin S, de Velde SV, et al. International sexual health and REproductive health (I-SHARE) survey during COVID-19: study protocol for online national surveys and global comparative analyses. Sex Transm Infect. (2021) 97(2):88–92. doi: 10.1136/sextrans-2020-054664
7. Manze M, Romero D, Johnson G, Pickering S. Factors related to delays in obtaining contraception among pregnancy-capable adults in New York state during the COVID-19 pandemic: the CAP study. Sex Reprod Healthc. (2022) 31:100697. doi: 10.1016/j.srhc.2022.100697
8. Diamond-Smith N, Logan R, Marshall C, Corbetta-Rastelli C, Gutierrez S, Adler A, et al. COVID-19’s impact on contraception experiences: exacerbation of structural inequities in women’s health. Contraception. (2021) 104(6):600–5. doi: 10.1016/j.contraception.2021.08.011
9. Marcelino AC, da Cunha Pereira P, ‘Poca CM, Bahamondes L. A particular epidemiological profile: disparities in access to contraceptive methods in Brazil during the SARS-CoV-2 (COVID-19) pandemic. Sci Rep. (2024) 14(1):14982. doi: 10.1038/s41598-024-65946-w
10. Kavanaugh ML, Pleasure ZH, Pliskin E, Zolna M, MacFarlane K. Financial instability and delays in access to sexual and reproductive health care due to COVID-19. J Womens Health. (2022) 31(4):469–79. doi: 10.1089/jwh.2021.0493
11. Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev. (1991) 43(6):1241–99. doi: 10.2307/1229039
12. Maxwell L, Devries K, Zionts D, Alhusen JL, Campbell J. Estimating the effect of intimate partner violence on women’s use of contraception: a systematic review and meta-analysis. PLoS One. (2015) 10(2):e0118234. doi: 10.1371/journal.pone.0118234
13. Andrade C. The limitations of online surveys. Indian J Psychol Med. (2020) 42(6):575–6. doi: 10.1177/0253717620957496
14. Rao L, Comfort AB, Dojiri SS, Goodman S, Yarger J, Shah N, et al. Telehealth for contraceptive services during the COVID-19 pandemic: provider perspectives. Women’s Health Issues. (2022)32(5):477–83. doi: 10.1016/j.whi.2022.05.001
15. Khan ME, Hazra A, Kant A, Ali M. Conditional and unconditional cash transfers to improve use of contraception in low and middle income countries: a systematic review. Stud Fam Plann. (2016) 47(4):371–83. doi: 10.1111/sifp.12004
16. UNFPA. Impact of COVID-19 on Family Planning: What we know one year into the pandemic. Available online at: https://www.unfpa.org/resources/impact-covid-19-family-planning-what-we-know-one-year-pandemic] (Cited November 11, 2024).
Keywords: contraception, family planning, COVID-19, disparities, access, income loss
Citation: Cavagnis S, Ryan R, Mussa A, Hargreaves JR, Tucker JD and Morroni C (2024) Disparities in adult women's access to contraception during COVID-19: a multi-country cross-sectional survey. Front. Glob. Womens Health 5:1235475. doi: 10.3389/fgwh.2024.1235475
Received: 6 June 2023; Accepted: 2 December 2024;
Published: 24 December 2024.
Edited by:
Ahmet Fatih Durmusoglu, Istanbul Medipol University, TürkiyeReviewed by:
Theresa Hoke, Family Health International 360, United StatesSandeep Poddar, Lincoln University College, Malaysia
Copyright: © 2024 Cavagnis, Ryan, Mussa, Hargreaves, Tucker and Morroni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sara Cavagnis, c2FyYS5jYXZhZ25pc0BzdHVkaW8udW5pYm8uaXQ=
 Sara Cavagnis
Sara Cavagnis Rebecca Ryan
Rebecca Ryan Aamirah Mussa2
Aamirah Mussa2 Joseph D. Tucker
Joseph D. Tucker Chelsea Morroni
Chelsea Morroni