- 1School of Nursing, College of Health Science and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
- 2Jimma Town Health Office, Jimma, Ethiopia
- 3School of Nursing, College of Medicine and Health Science, Wachemo University, Hossana, Ethiopia
- 4School of Public Health, College of Health Science and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
- 5Department of Statistics, College of Natural and Computational Science, Ambo University, Ambo, Ethiopia
Background: Antenatal care primarily focuses on health care checkups, the provision of advice on healthy behaviors, and the delivery of psychological, social, and emotional support for women with pregnancy. The national target set by the Ethiopian government is to achieve 95% of at least four ANC visits. Nevertheless, 43.11% of women had four or more checkups, according to the 2019 Ethiopian Demographic and Health Survey. Despite this achievement, antenatal care visits differ significantly between Ethiopian regions. Consequently, the purpose of this study was to assess regional disparities in pregnant women's utilization of antenatal care and its determinants in Ethiopia.
Methods: We have used 2019 intermediate Ethiopian Demographic and Health Survey data for analysis. The analysis comprised a total of 3,917 weighted women age 15–49 who had a live birth in the 5 years preceding the survey. Poisson regression analysis was done using SAS software version 9.4. To show the strength and direction of the association, an incidence rate ratio with a 95% confidence interval was used. Variables with a p-value <0.05 were declared as significant factors associated with the number of ANC visits.
Results: In Ethiopia, the number of ANC visits differs between regions. With a mean of 4.74 (95% CI: 4.49, 4.99), Addis Ababa reported the highest percentage of ANC visits (82.7%), while the Somali Region reported the lowest percentage (11.3%) with a mean of 0.73 (95% CI: 0.57, 0.88). Maternal age, educational level, religion, household wealth index, place of delivery, and household size show significant associations with the number of antenatal care visits.
Conclusions: In Ethiopia, there is the highest regional disparity in the number of ANC visits. The number of ANC visits was influenced by the mother's age, education, religion, household wealth index, place of delivery, and household size. Regarding the ANC visits, there should be initiatives that address the demands of pastoralist and agro-pastoralist communities to increase ANC utilization. As with many other health outcomes, education and low socio-economic status were associated with low ANC visit but these are tied to the overall social development of a country and are not immediately amenable to public health interventions
Introduction
Background
Antenatal care (ANC) utilization is defined as the receipt of care by pregnant women from skilled health care provider initiated within 12 weeks of gestation and frequent visits (at least four ANC visits) for care related to pregnancy (1). ANC is one of the best opportunities for pregnant mothers to prevent maternal and child mortality and morbidity by increasing women's access to basic obstetric care (2). It's considered a starting point for prenatal, postpartum, and pediatric vaccination services by creating a connection between the clinic and the healthcare practitioner for future actions (3, 4). ANC majorly focuses on health care checkups, the provision of advice on healthy behaviors, and the delivery of psychological, social, and emotional support for women with pregnancy (5). Also, it has paramount importance in reducing complications related to pregnancy (6). Moreover, antenatal care offers services such as tetanus immunization, hypertension management to prevent eclampsia, vitamin supplements, and other services (7). The care is primarily delivered by trained and skilled health care professionals, such as doctors, nurses, midwives, and other accredited health care professionals (5).
Global maternal deaths decreased from 451,000 to 295,000 between 2000 and 2017 (8). Even though maternal mortality is showing progress in reduction, it still becomes a major health problem in some parts of the world (5), with a majority (94%) occurring in developing countries and Sub-Saharan Africa sharing approximately two-thirds of maternal deaths (9, 10). In Ethiopia, the MMR was predicted to be 401 deaths per 100,000 live births in 2017, according to UN estimations (10).
The global community has given due emphasis to reducing maternal deaths. For instance, MDG Goal 5 focused on reducing the death rate by 75% at the end of 2015, but the overall achievement was only 44%. Lowering maternal mortality was one of the Sustainable Development Goals (SDGs), which were adopted in the wake of the Millennium Development Goals. By 2030, SDG3.1 targets global maternal death rates of less than 70 per 100,000 live births by the year 2030 (11). Also, in an effort to reduce maternal mortality, WHO revised the recommended ANC visit from 4 to 8 or more contacts, with the first ANC contact in the first 12 weeks of gestation and subsequent contacts at 20, 26, 30, 34, 38, and 40 weeks of gestation to improve the effectiveness, timing, and quality of care (11, 12).
Pregnant women without complications are advised by the World Health Organization (WHO) to have four ANC checkups throughout their pregnancy (10). Only three out of five women attended at least four antenatal care visits, according to the global 2017 survey. Only 52% of women in sub-Saharan Africa, where maternal mortality is high, had at least four ANC visits (2). In Ethiopia, 43.11 percent of women had four or more checkups, according to the 2019 Ethiopian Demographic and Health Survey (EDHS) (13), which is much lower than the target set by the Ethiopian Government to achieve 95% of at least four ANC visits (12).
Well-timed ANC utilization reduces direct and indirect causes of maternal death, but there are different factors that determine the utilization, such as maternal age (3, 14), women's education (3, 8, 13, 14), pregnancy status (3), the husband's occupation (3, 13, 14), socioeconomic status (13), the wealth index (3, 8, 14), accessing radio (3, 14), the number of children (3, 8, 15), the place of residence (3, 8, 13, 14), understaffed health facilities (13), and distant to health facilities (8, 13–15).
According to the 2019 Ethiopian DHS report, just 43% of pregnant women had the recommended four visits, and 48% had given birth to their most recent children in health facilities, even though 74% of pregnant women had at least one ANC visit with a qualified provider (10). Despite the observed benefits of appropriate ANC utilization, its use remains low in Ethiopia, with significant variations across regions. Consequently, the purpose of this study was to assess regional disparities in pregnant women's utilization of antenatal care and its determinants in Ethiopia.
Methods
Data source
The Demographic and Health Survey (DHS), which was carried out in Ethiopia, served as the study's data source. Along with the Central Statistics Agency, the Ethiopian Public Health Institute (EPHI) carried out the study (16). From March 21, 2019, to June 28, 2019, estimates at the national, regional, and local levels, as well as for urban and rural areas, were used to conduct the survey on women of reproductive age (ages 15–49) (13). Data were accessed from their URL: www.dhsprogram.com, with a reasonable request. Specifically, women's files (IR) were extracted and used for this study.
Sampling procedure
The sample for the 2019 Ethiopia Mini-DHS was stratified and chosen in two stages. After dividing Ethiopia's nine regions and two administrative cities into urban and rural areas, there are 21 sampling strata. In two stages, samples of enumeration areas (EAs) were chosen individually in each stratum. 200 EAs from eight regions and 105 EAs from three regions (Oromia, SNNPR, and Amhara) were chosen for the first stage, for a total of 305 EAs (93 in urban areas and 212 in rural areas) based on the probability proportional to EA size and with independent selection in each sampling stratum. For the second stage's sampling frame, a list of every household in the chosen EAs was used. The second stage involved the proportionate selection of households from each EA using systematic sampling. The study's source population consisted of women of reproductive age who had given birth in the five years preceding the survey. Eligible interviewees were women of childbearing age, whether they were permanent residents or visitors who had stayed in the household the previous night. In households where multiple eligible women resided, only one woman was selected through a random lottery method to ensure the selection process was random. The weighted frequency was used for the analysis by calculated using Women's individual sample weight (6 decimals).
Study variables
The number of antenatal visits made during the pregnancy served as the study's outcome variable (count data). Women's age, religions, present marital status, location, level of education, wealth index of the household, region, and number of children are considered as independent variables.
Data processing and analysis
To ensure consistency with the EMDHS 2019 descriptive report, and data cleaning was done. SAS statistical software version 9.4 was used for recoding, variable formation, labeling, and data analysis. The dependent variable, ANC utilization, is count data, which is a non-negative integer. Therefore, we used the Poisson regression model for analysis. The Poisson distribution assumes that its “mean” and “variance” are equal. But this study violated this assumption since the mean and variance were 2.89 and 5.33, respectively, which suggest the presence of over dispersion. We adjusted the over dispersion and excess zeros in the data by using scale Pearson chi-square.
Ethics statement
Ethics approval was not required as the data were freely available to the public.
Results
Characteristics of the respondents
In this study, 3,962 (weighted 3,917) women who had given birth in the five years preceding the survey were included. The majority, (76.3%) of the respondents were from rural areas. The mean (±SD) age of women was 28.7 ± 6.7. About, 51.3% of women did not attend formal education. Forty-two percent of women were reported to have a poor wealth index. Regarding the place of delivery 49.3% of the total births occurred in public health institutions. The mean (±SD) number of children ever born to women was 3.7 ± 2.5 (Table 1).

Table 1. Socio-demographic characteristics of women age 15–49 who had a live birth in the 5 years preceding the survey in Ethiopia 2019.
Regional disparity in ANC utilization
Utilization of antenatal care services varies among Ethiopian regions. With a mean of 4.74 ANC visits, Addis Ababa reported the highest ANC utilization, while the Somali Region recorded the lowest, with a mean of 0.73 ANC visits. Similar to this, Addis Ababa (82.7%) and Somali (11.3%) had the greatest and lowest respective percentages of pregnant women who had four or more ANC visits. Somalia had the largest percentage of women who had no ANC visits (70.8%), and Addis Ababa had the lowest percentage (3.2%) (Table 2).
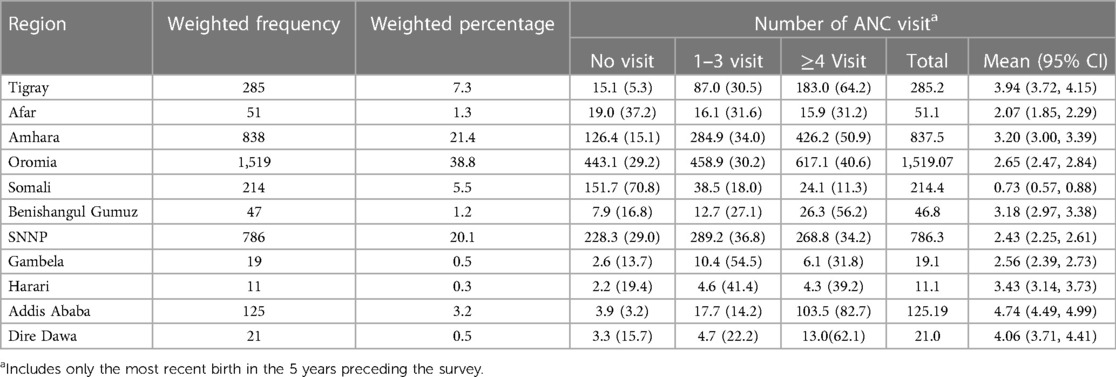
Table 2. Regional disparity in the number of antenatal care visit among women age 15–49 who had a live birth in the 5 years preceding the survey in Ethiopia 2019.
Determinant of antenatal care visit among pregnant women in Ethiopia
Maternal age, educational level, religion, household wealth index, place of delivery, and household size show significant associations with the number of antenatal care visits whereas place of residence and parity were not significantly associated with the number of antenatal care visits.
The number of ANC visits was 1.23 (IRR = 1.23, 95% CI: 1.11, 1.38), 1.33 (IRR = 1.33, 95% CI: 1.18, 1.50), 1.30 (IRR = 1.30, 95% CI: 1.15, 1.48), and 1.27 (IRR = 1.27, 95% CI: 1.09, 1.48), times higher among 25–29 years, 30–34 years, 35–39 years, and 40–44 years old women than among 15–19 years old women, respectively. Compared to pregnant women with no educational level, women who attended primary school had 1.19 (IRR = 1.19, 95% CI: 1.12, 1.26), secondary school had 1.29 (IRR = 1.29, 95% CI: 1.19, 1.40), and higher education had 1.28 (IRR = 1.28, 95% CI: 1.16, 1.40) times more ANC visits. The number of ANC visits was 16% (IRR = 0.84, 95% CI: 0.79, 0.89), and 20% (IRR = 0.80, 95% CI: 0.76, 0.84) 61% (IRR = 0.39, 95% CI: 0.26, 0.82) and 50% (IRR = 0.50, 95% CI: 0.31, 0.82) lower among Protestants, Muslims, Traditionalists, and Others compared to Orthodox religion followers, respectively. There is a high rate of ANC visits among women with a middle (1.20 times higher; IRR = 1.20; 95% CI: 1.11, 1.28); or rich household wealth index (1.22 times higher; (IRR = 1.22, 95% CI: 1.14, 1.30)) compared to women with a poor house hold index. Women who live in households with more than 10 members had a 16% (IRR = 0.84, 95% CI: 0.74, 0.94) lower number of ANC visits compared to households with fewer than 5 members. Women who delivered in a public health institution had an IRR of 1.94 (95% CI: 1.83, 2.06), a private health institution had an IRR of 2.27 (95% CI: 2.02, 2.56), and NGO health facilities had an IRR of 1.45 (95% CI: 1.25, 1.68) more ANC visits than those who gave birth at home. Women from urban area had an IRR of 1.02 (95% CI: 0.99, 1.11), times higher number of visit than women from rural area. As parity increase the number of ANC visit decreases. The number of ANC visits was 3% (IRR = (0.97, 95% CI: 0.90, 1.03) and 7% (IRR = (0.93, 95% CI: 0.85, 1.01) lower among women with 3–4, and 5 and above compared to women with parity 1–2 respectively (Table 3).
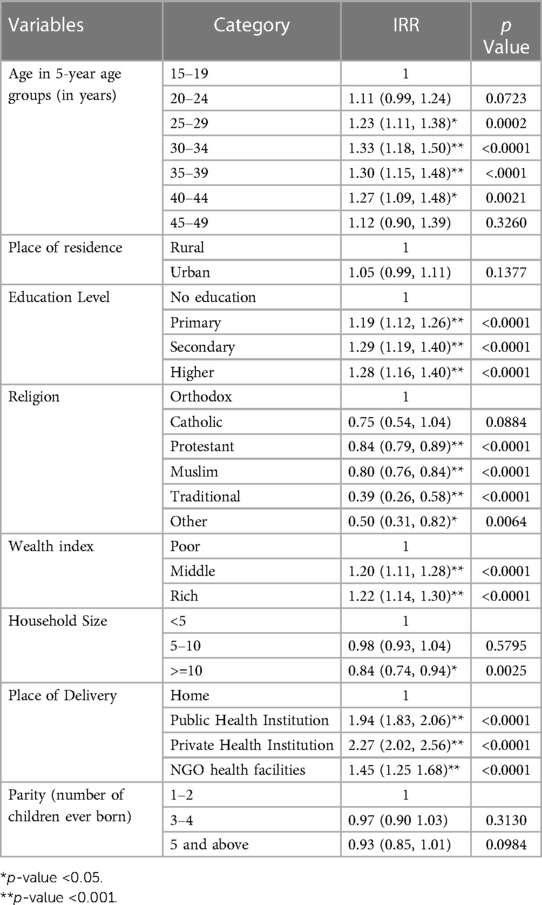
Table 3. Multivariable poisson regression result for factors associated with the number of antenatal care visit among women age 15–49 who had a live birth in the 5 years preceding the survey in Ethiopia 2019.
Discussion
The result of this study indicates there is a highest regional disparity in the number of ANC visits. The highest ANC visit was reported in Addis Ababa with mean numbers of 4.74 (95% CI: 4.49, 4.99), while the lowest was reported in the Somali Region with mean numbers of 0.73 (95% CI: 0.57, 0.88). The number of ANC visits was influenced by the mother's age, education, religion, household wealth index, place of delivery, and household size.
In descending order of frequency, Addis Ababa, Tigray, Dire Dawa, Benishangul Gumuz, Amhara, Oromia, Harari, SNNPR, Gambela, Afar, and Somalia have the highest regional disparity in the number of ANC visits. In Ethiopia, more women had four or more ANC visits in 2019 compared to the previous three DHS (16, 17).
The number of ANC visits is lowest in pastoral regions in Ethiopia. Pastoralists and agro-pastoralists are found in low-land areas of Somalia, Afar, Oromia, and SNNPR (18). Since pastoralists and agro-pastoralists spend the majority of their time searching for water and grazing for their animals during the changing seasons, the static health care service strategy of Ethiopia's health care system does not match their health care demands (19). They have problems accessing health care services due to low population density, spatial mobility, dispersion, distance from health care services, and cultural factors (20). The low number of ANC visits in the Somali region is attributed to a number of factors, including a lack of funding for transportation and accommodation, a lack of awareness about ANC, a lack of husband support, and the absence of full ANC service packages because most health facilities lack the necessary staff and supplies (21, 22).
The national target of four or more ANC visits set for 2025 by the Health Sector Transformation Plan II (HSTP II) is 81% (23). The program is left with only two years but among the regions of Ethiopia according to EDHS 2019 data only Addis Ababa achieved the target while other regions have made less progress compared to Addis Ababa.
In this study, there was a strong association between education level and the number of ANC visits. Women who attended primary, secondary, or higher education have a higher rate of ANC visits compared to women with no education. This study is consistent with nationally representative data collected in 2020 in Ethiopia (24), a systematic review, and meta-analysis conducted in Ethiopia (25) and in East Africa (14, 26). Also, the Demographic and Health Survey (DHS) data from Mauritania (8), Cameron (27), Gahan (28), and Sub-Saharan Africa (29) are in agreement with the finding of this study. With more education, women would become more informed when making healthcare decisions and would be more conscious of the usage of ANC services and their effects. Also, as women's educational levels increase, their knowledge of obstetric complications increases, which encourages them to use ANC services (30). Education provides the skill and knowledge required for accessing information and initiates women to receive health-related messages; on top of that, it facilitates communication with health care providers (31).
The number of ANC visits increases with maternal age. In comparison to women in the 15–19 year age group, more ANC visits were made by women in the 20–24 year, 25–29 year, 30–34 year, 35–39 year, and 40–44 year age groups. Nationally representative data collected in Ethiopia in 2020 support this (24), a systematic review and meta-analysis carried out in Cameroon (27), the DHS of Sub-Saharan Africa (29), and East African countries (26). This might be a result of the fact that women are more likely to use healthcare services as their experience and knowledge of them grows (32, 33).
Religion is significantly associated with the number of ANC visits. Women who were protestant, Muslim, traditional, or practiced another religion had fewer ANC visits than Orthodox believers. This is supported by findings from Nigeria (34) and Ghana (35). This needs additional evidence and a more qualitative approach to explore the effect of religion on the utilization of ANC.
ANC visits were higher for households in the middle or rich household wealth index than for those in the lower wealth index. This study is similar to systematic reviews and meta-analyses conducted in East African countries (26), the DHS of Mauritania (8), Cameron (27), Gahan (28). and Sub-Saharan Africa (29). Health-seeking behavior depends largely on economic factors. Income is important for purchasing health care. This affects women's ability to seek ANC services (36). Lack of income limits ANC visits, and most of them visit the service late in pregnancy (37). Even though in Ethiopia antenatal services are offered without charge, indirect costs like transportation costs to and from health facilities limit service utilization among women with low wealth index. Women in high wealth indexes also get the service from private health institutions with direct payments (38).
Women who delivered their last birth in a public health institution, a private health institution, or an NGO health facility had a higher number of ANC visits compared to those who delivered at home. This is supported by a study from Bangladesh (39) and a systematic review conducted in Sub-Saharan Africa (37).
Women are less likely to seek ANC services as household sizes increase. Compared to households with less than five members, women who live in households with more than ten people experienced fewer ANC visits. This study is in line with studies from Rwanda (40) and North West Ethiopia (41). This could be because as families become larger, financial difficulties arise, preventing the women from accessing ANC. Also, when families get larger, women take on more household duties and spend more time caring for their children, which have an impact on health care seeking behavior (42).
Since we have used the national data, which is collected from both urban and rural areas in nine regions and two city administrations in Ethiopia, the study was thought to be more representative than other studies. But the study might have faced the following limitations. There might be recall bias since the data was collected from women based on their last birth history. Due to the nature of the data, we might have missed important variables such as those related to the husband, previous exposure variables, and paternal variables.
Conclusion
In Ethiopia, there is the highest regional disparity in the number of ANC visits. The number of ANC visits was influenced by the mother's age, education, religion, household wealth index, place of delivery, and household size. The government of Ethiopia should focus in increasing an access to health care service in areas with the fewest ANC visits in order to reduce inequities between regions in Ethiopia. Regarding the ANC visits, there should be initiatives that address the demands of pastoralist and agro-pastoralist communities to increase ANC utilization. As with many other health outcomes, education and low socio-economic status were associated with low ANC visit but these are tied to the overall social development of a country and are not immediately amenable to public health interventions.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
SK: initiated the research concept, NA, SA, EG, LK, SK: analyze and interpreted the data, wrote the manuscript; all authors: critically revise, read and approved the final manuscript. All authors have equal participation. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to acknowledge Demographic and Health Survey for providing authorization letter to access EDHS-2019 dataset to conduct this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mouhoumed HM, Mehmet N. Utilization pattern of antenatal care and determining factors among reproductive-age women in Borama, Somaliland. J Prev Med Hyg. (2021) 62(2):E439–46. doi: 10.15167/2421-4248/jpmh2021.62.2.1882
2. Belay AT, Fenta SM, Birhan Biresaw H, Abebaw Moyehodie Y, Melkam Yelam M, Mekie M. The magnitude of optimal antenatal care utilization and its associated factors among pregnant women in South Gondar Zone, Northwest Ethiopia: a cross-sectional study. Int J Reprod Med. (2022) 2022:1415247. doi: 10.1155/2022/1415247
3. Arefaynie M, Kefale B, Yalew M, Adane B, Dewau R, Damtie Y. Number of antenatal care utilization and associated factors among pregnant women in Ethiopia: zero-inflated poisson regression of 2019 intermediate Ethiopian demography health survey. Reprod Health. (2022) 19(1):36. doi: 10.1186/s12978-022-01347-4
4. Mengist B, Endalew B, Diress G, Abajobir A. Late antenatal care utilization in Ethiopia: the effect of socio-economic inequities and regional disparities. PLOS Glob Public Health. (2022) 2(11):e0000584. doi: 10.1371/journal.pgph.0000584
5. Birhanu F, Mideksa G, Yitbarek K. Are Ethiopian women getting the recommended maternal health services? The analysis of Ethiopian mini demographic and health survey 2019. Health Sci Rep. (2022) 5(6):e879. doi: 10.1002/hsr2.879
6. Aboma D, Egata G, Ayalew D. Level of antenatal care services utilization and associated factors among mothers who have given birth in the past twelve months in Gelemso Town, West Hararghe Zone, Oromia National Regional State, East Ethiopia. J Woman’s Reprod Health. (2020) 2:11. doi: 10.14302/issn.2381-862X.jwrh-20-3444
7. UNICEF. Antenatal care (2017). Available online at: https://data.unicef.org/topic/maternal-health/antenatal-care/ (accessed March 7, 2023).
8. Shibre G, Zegeye B, Ahinkorah BO, Idriss-Wheeler D, Keetile M, Yaya S. Sub-regional disparities in the use of antenatal care service in Mauritania: findings from nationally representative demographic and health surveys (2011–2015). BMC Public Health. (2021) 21(1):1818. doi: 10.1186/s12889-021-11836-z
9. Fan Q, Roque M, Nuzhath T, Hossain MM, Jin X, Aggad R, et al. Changes in levels and determinants of maternal health service utilization in Ethiopia: comparative analysis of two rounds Ethiopian demographic and health surveys. Matern Child Health J. (2021) 25(10):1595–606. doi: 10.1007/s10995-021-03182-8
10. Gurara MK, Draulans V, Van Geertruyden JP, Jacquemyn Y. Determinants of maternal healthcare utilisation among pregnant women in southern Ethiopia: a multi-level analysis. BMC Pregnancy Childbirth. (2023) 23(1):96. doi: 10.1186/s12884-023-05414-x
11. Ahinkorah BO, Ameyaw EK, Seidu AA, Odusina EK, Keetile M, Yaya S. Examining barriers to healthcare access and utilization of antenatal care services: evidence from demographic health surveys in sub-Saharan Africa. BMC Health Serv Res. (2021) 21(1):125. doi: 10.1186/s12913-021-06129-5
12. Hailemariam T, Atnafu A, Gezie LD, Tilahun B. Utilization of optimal antenatal care, institutional delivery, and associated factors in northwest Ethiopia. Sci Rep. (2023) 13(1):1071. doi: 10.1038/s41598-023-28044-x
13. Ethiopian Public Health Institute—EPHI, Federal Ministry of Health—FMoH, ICF. Ethiopia Mini Demographic and Health Survey 2019. Addis Ababa, Ethiopia: EPHI/FMoH/ICF (2021).
14. Raru TB, Ayana GM, Zakaria HF, Merga BT. Association of higher educational attainment on antenatal care utilization among pregnant women in east Africa using demographic and health surveys (DHS) from 2010 to 2018: a multilevel analysis. Int J Womens Health. (2022) 14:67–77. doi: 10.2147/IJWH.S350510
15. Muhwava LS, Morojele N, London L. Psychosocial factors associated with early initiation and frequency of antenatal care (ANC) visits in a rural and urban setting in South Africa: a cross-sectional survey. BMC Pregnancy Childbirth. (2016) 16:18. doi: 10.1186/s12884-016-0807-1
16. Csa I: Central statistical agency (CSA)[Ethiopia] and ICF. Ethiopia demographic and health survey, Addis Ababa, Ethiopia and Calverton, Maryland, USA (2016). p. 1.
17. Macro O. Ethiopia Demographic and Health Survey 2005. Addis Ababa: Central Statistical Agency (2006).
18. Mohamed AA. Pastoralism and development policy in Ethiopia: a review study. Budapest Int Res Critics Inst J. (2019) 2(4):01–11. doi: 10.33258/birci.v2i4.562
19. Biza N, Mohammed H. Pastoralism and antenatal care service utilization in Dubti district, Afar, Ethiopia, 2015: a cross-sectional study. Pastoralism. (2016) 6:1–7. doi: 10.1186/s13570-016-0062-0
20. Dubale T, Mariam DH. Determinants of conventional health service utilization among pastoralists in Northeast Ethiopia. Ethiop J Health Dev. (2007) 21(2):142–7. doi: 10.4314/ejhd.v21i2.10042
21. Mohammed A, Teklu A, Beyene S, Hashi A, Abebe Z, Gezahegn W, et al. Barriers of antenatal care service utilization in Somali regional state using socio ecological model framework, eastern Ethiopia, Ethiopia: a qualitative study. Res Sq. (2019). [preprint]. doi: 10.21203/rs.2.13486/v1
22. Umer A, Zinsstag J, Schelling E, Tschopp R, Hattendof J, Osman K, et al. Antenatal care and skilled delivery service utilisation in Somali pastoral communities of eastern Ethiopia. Trop Med Int Health. (2020) 25(3):328–37. doi: 10.1111/tmi.13346
23. Health EMo. Health Sector Transformation Plan II (HSTP II): 2020/21-2024/25 (2013 EFY-2017 EFY). MOH (2021).
24. Shiferaw K, Mengistie B, Gobena T, Dheresa M, Seme A. Extent of received antenatal care components in Ethiopia: a community-based panel study. Int J Womens Health. (2021) 13:803–13. doi: 10.2147/IJWH.S327750
25. Tekelab T, Chojenta C, Smith R, Loxton D. Factors affecting utilization of antenatal care in Ethiopia: a systematic review and meta-analysis. PLoS One. (2019) 14(4):e0214848. doi: 10.1371/journal.pone.0214848
26. Tessema ZT, Minyihun A. Utilization and determinants of antenatal care visits in East African countries: a multicountry analysis of demographic and health surveys. Adv Public Health. (2021) 2021:6623009. doi: 10.1155/2021/6623009
27. Ahinkorah BO, Seidu AA, Budu E, Mohammed A, Adu C, Agbaglo E, et al. Factors associated with the number and timing of antenatal care visits among married women in Cameroon: evidence from the 2018 Cameroon demographic and health survey. J Biosoc Sci. (2022) 54(2):322–32. doi: 10.1017/S0021932021000079
28. Duodu PA, Bayuo J, Mensah JA, Aduse-Poku L, Arthur-Holmes F, Dzomeku VM, et al. Trends in antenatal care visits and associated factors in Ghana from 2006 to 2018. BMC Pregnancy Childbirth. (2022) 22(1):59. doi: 10.1186/s12884-022-04404-9
29. Gebeyehu FG, Geremew BM, Belew AK, Zemene MA. Number of antenatal care visits and associated factors among reproductive age women in sub-Saharan Africa using recent demographic and health survey data from 2008 to 2019: a multilevel negative binomial regression model. PLOS Glob Public Health. (2022) 2(12):e0001180. doi: 10.1371/journal.pgph.0001180
30. Furuta M, Salway S. Women’s position within the household as a determinant of maternal health care use in Nepal. Int Fam Plan Perspect. (2006) 32(1):17–27. doi: 10.1363/3201706
31. Vanden Broeck J, Feijen-de Jong E, Klomp T, Putman K, Beeckman K. Antenatal care use in urban areas in two European countries: predisposing, enabling and pregnancy-related determinants in Belgium and The Netherlands. BMC Health Serv Res. (2016) 16(a):337. doi: 10.1186/s12913-016-1478-3
32. Chilot D, Belay DG, Ferede TA, Shitu K, Asratie MH, Ambachew S, et al. Pooled prevalence and determinants of antenatal care visits in countries with high maternal mortality: a multi-country analysis. Front Public Health. (2023) 11:1035759. doi: 10.3389/fpubh.2023.1035759
33. Suleman Hassen S, Mulatu Teshale B, Abate Adulo L. Identifying factors associated with barriers in the number of antenatal care service visits among pregnant women in rural parts of Ethiopia. Sci World J. (2021) 2021:7146452. doi: 10.1155/2021/7146452
34. Umar AS. The use of maternal health services in Nigeria: does ethnicity and religious beliefs matter. MOJ Public Health. (2017) 6:00190. doi: 10.15406/mojph.2017.06.00190
35. Ganle JK, Parker M, Fitzpatrick R, Otupiri E. Inequities in accessibility to and utilisation of maternal health services in Ghana after user-fee exemption: a descriptive study. Int J Equity Health. (2014) 13:89. doi: 10.1186/s12939-014-0089-z
36. Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Rahman MH. Poverty and access to health care in developing countries. Ann N Y Acad Sci. (2008) 1136:161–71. doi: 10.1196/annals.1425.011
37. Okedo-Alex IN, Akamike IC, Ezeanosike OB, Uneke CJ. Determinants of antenatal care utilisation in sub-Saharan Africa: a systematic review. BMJ Open. (2019) 9(10):e031890. doi: 10.1136/bmjopen-2019-031890
38. Tegegne TK, Chojenta C, Getachew T, Smith R, Loxton D. Antenatal care use in Ethiopia: a spatial and multilevel analysis. BMC Pregnancy Childbirth. (2019) 19(1):399. doi: 10.1186/s12884-019-2550-x
39. Islam MM, Masud MS. Determinants of frequency and contents of antenatal care visits in Bangladesh: assessing the extent of compliance with the WHO recommendations. PLoS One. (2018) 13(9):e0204752. doi: 10.1371/journal.pone.0204752
40. Manzi A, Munyaneza F, Mujawase F, Banamwana L, Sayinzoga F, Thomson DR, et al. Assessing predictors of delayed antenatal care visits in Rwanda: a secondary analysis of Rwanda demographic and health survey 2010. BMC Pregnancy Childbirth. (2014) 14:290. doi: 10.1186/1471-2393-14-290
41. Ambaye E, Regasa ZW, Hailiye G. Early initiation of antenatal care and its associated factors among pregnant women attending antenatal care at public health centres in Bahir Dar Zuria zone, Northwest Ethiopia, 2021: a cross-sectional study. BMJ Open. (2023) 13(1):e065169. doi: 10.1136/bmjopen-2022-065169
Keywords: antenatal care, number of visits, poisson regression, DHS, Ethiopia
Citation: Awoke N, Ababulgu SA, Hanfore LK, Gebeyehu EG and Wake SK (2024) Regional disparities in antenatal care utilization among pregnant women and its determinants in Ethiopia. Front. Glob. Womens Health 5:1230975. doi: 10.3389/fgwh.2024.1230975
Received: 29 May 2023; Accepted: 1 February 2024;
Published: 9 February 2024.
Edited by:
Mona Pathak, University of North Texas Health Science Center, United States© 2024 Awoke, Ababulgu, Hanfore, Gebeyehu and Wake. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nefsu Awoke bmVmc2VhQGdtYWlsLmNvbQ==
 Nefsu Awoke
Nefsu Awoke Sabit Abazinab Ababulgu2
Sabit Abazinab Ababulgu2