- 1Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Department of Internal Medicine, College of Medicine and Health Sciences, Madda Walabu University, Goba, Oromia, Ethiopia
- 3Department of Environmental and Occupational Health and Safety, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 4Department of Human Anatomy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: The majority of maternal deaths were associated with a lack of access to skilled birth attendance. Because childbirth accounts for most maternal deaths, skilled birth attendance is crucial for reducing maternal mortality. The use of skilled birth attendance in Ethiopia is low, and it is crucial to identify factors that determine the use of skilled birth attendance. Hence, this study aimed to assess the spatial distribution, wealth-related inequality, and determinants for skilled birth attendance in Ethiopia.
Methods: Secondary data analysis was done with a total weighted sample of 5,251 reproductive-aged women using the 2019 mini EDHS. The concentration index and graph were used to assess wealth-related inequalities. Spatial analysis was done to identify the spatial distribution and multilevel logistic regression analysis was used to identify predictors of skilled birth attendance in Ethiopia. Analysis was done using STATA version 14, ArcGIS, and SaTscan software.
Results: The prevalence of skilled birth attendance was 50.04% (95% CI: 48.69%, 51.40%) in Ethiopia. Old age, being married, being educated, having television and radio, having ANC visits, being multiparous, having large household sizes, having a rich wealth index, living in rural residence, and living in a high level of community poverty and women's education were significant predictors of skilled birth attendance. Skilled birth attendance was disproportionately concentrated in rich households [C = 0.482; 95% CI: 0.436, 0.528]. High prevalence of unskilled birth attendance was found in Somalia, SNNP, Afar, and southern parts of the Amhara regions. Primary clusters of unskilled birth attendance Somalia and some parts of Oromia region of Ethiopia.
Conclusion: Half of the women in Ethiopia did not utilize skilled birth attendants with significant spatial clustering. Age, marital status, educational status, ANC Visit, having television and radio, parity, household size, wealth index, residence, community level poverty, and community level of women's education were significant predictors of skilled birth attendance. Skilled birth attendance was unevenly concentrated in rich households. The regions of Somalia, SNNP, Afar, and southern Amhara were identified as having a high prevalence of using unskilled birth attendance. Public health interventions should target those women at high risk of using unskilled birth attendants.
Introduction
Maternal mortality remains a major challenge for global health systems particularly in developing countries (1). One of the primary causes of high maternal and neonatal mortality rates worldwide is a lack of access to healthcare services during pregnancy and delivery (2–4). The majority of maternal deaths are caused by obstetric complications, particularly in low-income countries (5). The majority of maternal deaths occur in Sub-Saharan Africa, with the majority of these deaths being associated with a lack of access to antenatal care and skilled birth attendance (6).
Skilled birth attendance (SBA) is defined as the process by which a skilled health professional such as a doctor, nurse, or midwife provides adequate care to a woman during labor, delivery, and the early postpartum period (7). Because the majority of maternal deaths and obstetric complications occur during delivery, SBA remains the most important intervention in reducing maternal mortality and complications (8). Skilled birth attendant-assisted delivery care has been identified as a protective mechanism for saving maternal and newborn lives (9–11). According to studies, skilled birth attendance can considerably reduce obstetric complications such as stillbirths (12, 13).
Skilled birth attendance is a well-known method of reducing maternal and perinatal mortality and morbidity (14–17). A skilled delivery service provides a safe environment for both mothers and newborns, lowering the likelihood of complications (18). As a result, skilled birth attendance is critical and the best strategy for reducing maternal and perinatal deaths (19–21). Variables such as educational status (22–25), wealth index (23, 26–28), residence (28–30), ANC visit (22, 31–35), media exposure (28, 32, 36) were identified as significant predictors of skilled birth attendance.
Studies indicated that maternal mortality is typically low when a greater proportion of deliveries are attended by skilled birth attendants (37–39). Even though the Ethiopian government implemented several interventions, such as training skilled health providers and making most maternal health services free of charge, skilled birth attendance remains a major challenge in Ethiopia. Therefore, this study aimed to assess the spatial distribution; wealth-related inequality, and determinants for skilled birth attendance among reproductive-age women in Ethiopia using nationally representative data. The study's findings will support policymakers in the implementation of measures that will enhance the utilization of skilled delivery care in Ethiopia.
Methods
Study design, study period, and study setting
A community-based cross-sectional study was conducted in Ethiopia using the 2019 mini-EDHS data conducted from March 21, 2019, to June 28, 2019. The study was conducted in Ethiopia is located in the horn of Africa (3o–14o N and 33o–48°E). Ethiopia is the second-most populous country in Africa with nine regional states and two city administrations (Addis Ababa and Dire Dawa). Administratively, regions are divided into zones, zones into woredas, and woredas into the lowest administrative unit known as kebeles.
Data source
The data for this study were retrieved from EDHS data of 2019, which was the second EMDHS and the fifth DHS implemented in Ethiopia. Data were obtained from the DHS website: www.dhsprogram.com by justifying the reason for requesting the data and after obtaining an approval letter from the DHS. For this study, we used the individual record data set.
Sampling procedures and populations
The source population was all women of reproductive age who gave birth in Ethiopia within five years before the survey, while the sample population was all women of reproductive age who gave birth in the selected enumeration areas (EAs) within five years before the survey. Samples were selected using a stratified, two-stage cluster design, using EAs as primary sampling units and households as secondary sampling units.
Each region was divided into urban and rural areas, resulting in 21 different sampling strata. Firstly, a total of 305 EAs (93 in urban, 212 in rural) were chosen independently with a probability proportional to each EA. Second, from the newly formed household listing, a fixed number of 30 households/clusters were selected with an equal probability of systematic selection. The detailed sampling procedures are available on the measure DHS website in the 2019 EMDHS report (https://www.dhsprogram.com). A total weighted sample of 5,251 reproductive-age women who gave birth within five years of the survey was included.
Variables of the study
The outcome of this study was delivery by a skilled birth attendant. Skilled birth attendance refers to births delivered with the assistance of doctors, nurses/midwives, health officers, and health extension workers (40). If the woman received the assistance of skilled personnel (i.e., doctor, midwives/nurse, public health officer, and health extension) during my most recent childbirth” they coded as “yes”, otherwise “no”.
Individual and community-level independent variables were considered in this study. Maternal age, marital status, maternal educational level, household size, household head, television, radio, ANC visit, household wealth, and parity were some of the individual-level factors included in this study.
Community-level factors residence, community-level poverty, community level of women's education, and region were included. In this study region was categorized into three categories; larger central [Tigray, Amhara, Oromia, and Sothern Nations Nationalities and Peoples Region], small peripherals [Afar, Somali, Benishangul Gumuz, and Gambela], and metropolis [Harari, Dire Dawa, and Addis Ababa] based on their geopolitical features, which is consistent with a prior Ethiopian study (41–43).
Community-level poverty was the proportion of women in the community who live in the lower (poor) and higher (rich) quintiles of the wealth index are classified as high (proportion of women greater than the median national value) or low (proportion of women less than the median national value) (44). The community level of women's education was the proportion of women in the community with at least a primary level of education, categorized as high (proportion of women greater than median national value) whereas low (proportion of women below-median national value) (44).
Data management and analysis
The data was cleaned to ensure consistency with the EMDHS 2019 report. Data were weighted before statistical analysis using sampling weight (v005), primary sampling unit (v021), and strata (v023) to restore the survey's representativeness and obtain valid statistical estimates. Descriptive and summary statistics were done using STATA version 14 software.
Spatial analysis
Spatial distribution and autocorrelation
The global spatial autocorrelation (Global Moran's I) was used to determine whether skilled birth attendance patterns were dispersed, clustered, or randomly distributed in the study area (45). Moran's I value close to −1 indicate the spatial distribution of unskilled birth attendance is dispersed, whereas Moran's I value close to +1 indicate unskilled birth attendance is clustered (46). The Moran I value close to 0 means the spatial distribution of unskilled birth attendance is random. A statistically significant Moran's I (p < 0.05) indicates the spatial clustering of unskilled birth attendance.
The maximum peak distance where unskilled birth attendance clustering is more pronounced was determined using incremental spatial autocorrelation. The maximum peak distance is the distance at which the spatial autocorrelation is maximum, and it was used as a distance band for hot-spot analysis. A total of ten distance bands were identified, with a beginning distance of 155,205 m, the first peak at 299,451.07 m, and peak clustering at 299,451.07 m.
Hot spot and cold spot analysis (Getis-Ord Gi* statistics)
Gettis-Ord Gi* statistics were computed for each area to determine how spatial autocorrelation varies across the study location. Z-score was calculated to ensure the statistical significance of clustering, A positive z-score >1.96 with significant p-values indicates a hotspot, whereas a negative z-score >1.96 with significant p-values indicates a cold spot (47, 48). The hot spot areas indicated areas with a high proportion of unskilled birth attendance and the cold spot ones indicated that there was a low proportion of unskilled birth attendance.
Spatial interpolation
In this study, we used a geostatistical ordinary Kriging spatial interpolation technique to predict values for areas where data points were not taken. Interpolation is based on the assumption that spatially distributed objects are spatially correlated; in other words, things that are close together tend to have similar characteristics (49, 50). Based on sampled clusters, the spatial interpolation technique is used to predict unskilled birth attendance for unsampled areas.
Spatial scan statistical analysis
Using Kuldorff's SaTScan version 9.6 statistical software, a Bernoulli-based model was used to identify statistically significant spatial clusters of unskilled birth attendance. To fit the Bernoulli model, women who had unskilled birth attendance were considered cases, while those who had skilled birth attendance were considered controls. The default maximum spatial cluster size of <50% of the population was used as an upper limit, allowing for the detection of both small and large clusters while ignoring clusters that contained more than the maximum limit. A likelihood ratio test statistic and the p-value were used for each potential cluster to determine whether the number of observed unskilled birth attendants within the potential cluster was significantly higher than expected.
Parameter estimation method
The random effects are measures of variation in skilled birth attendance across communities or clusters, were expressed in terms of the Intra-Class Correlation (ICC), the median odds ratio (MOR), and the proportional change in variance (PCV) (51–53). MOR is defined as the central value of the odds ratio between the greatest and lowest risk regions when two clusters are selected at random. The PCV explains the variability in skilled birth attendance among reproductive-aged women. The ICC shows the differences between clusters in skilled birth attendance among reproductive-aged women (54, 55).
Multilevel analysis
We used a multilevel logistic regression analysis to account for the heterogeneity between clusters in the EDHS data. Variables with p-value <0.2 in the bi-variable analysis for both individual and community-level factors were fitted in the multivariable model. Adjusted Odds Ratio (AOR) with a 95% Confidence Interval (CI) in the multivariable model was used to declare statistically significant associations with our outcome variable. Multi-collinearity was checked using the variance inflation factor (VIF) by conducting a pseudo-linear regression analysis, with a cut-off value of <5.
Model building
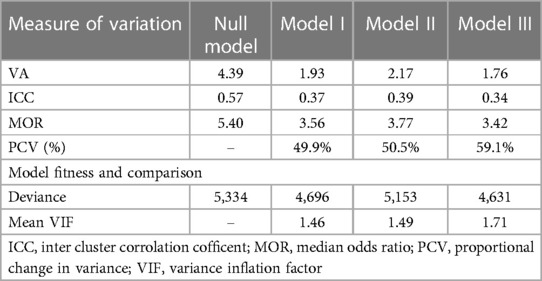
Four models have fitted: the null model (models without independent variables), model I (models with individual-level variables), model II (models include community-level variables), and model III (models with both individual and community-level variables). Deviance was used to assess model fitness since these models were nested. The variance inflation factor (VIF) was used to detect multicollinearity.
Concentration index and curve
The concentration index measures the magnitude and direction of socioeconomic inequality in a health variable. A negative sign indicates that the poor have a higher concentration of skilled birth attendance; whereas a positive sign indicates that the wealthy have a higher concentration of skilled birth attendance.
Ethical consideration
All methods were carried out following relevant guidelines of the Demographic and Health Surveys (DHS) program. Informed consent was waived from the International Review Board of Demographic and Health Surveys (DHS) program data archivists after the consent paper was submitted to the DHS Program, a letter of permission to download the dataset for this study. The dataset was not shared or passed on to other bodies and has maintained its confidentiality.
Results
A total weighted sample of 5,251 women was included in the study. The prevalence of skilled birth attendance among women was 50.04% (95% CI: 48.69%, 51.40%) in Ethiopia. More than half, 2,829 (53.88%) were between the ages of 25 and 34 years. More than half of the participants 2,801 (53.36%) of the women had no formal education. Women who had secondary and higher education were more likely to have skilled birth attendance 512(86.74%) than those who had no formal education 993(35.43%). Women with a rich wealth index of 1,414 (74.99%) were more likely to have skilled birth attendance than those who had a poor wealth index 745 (31.49%). Around three fourth of the participants 3,932 (74.89%) lived in a rural area. Women who live in rural areas were less likely to have skilled birth attendance, 1,679 (42.72%) than those who live in urban areas 948 (71.93%) (Table 1).

Table 1. Characteristics of the study population with skilled birth attendance among reproductive-age women, 2019 mini EDHS.
Random effect and model comparison
In the null model, the ICC indicated that 57% of the total variability for skilled birth attendance was due to differences between clusters while the remaining unexplained 43% of the total variability of skilled birth attendance was attributable to individual differences. Furthermore, the PCV value in the final model indicates that about 59.1% of the variations in skilled birth attendance among study subjects were attributed to both individual and community-level factors. Model comparison and fitness was used. The model with the lowest deviance was the best-fitted model, which was model three (4,631). Multi-collinearity was not found since all variables had a VIF of less than five (Table 2).
Wealth-related inequality of skilled birth attendance
Concentration index and curve
The value of a negative sign in the concentration index indicates a more concentration of skilled birth attendance among the poor, whereas a positive value indicates concentration among the rich. In this study, the overall wag staff normalized concentration index (C) analyses of the wealth-related inequality of skilled birth attendance showed the pro-rich distribution of skilled birth attendance with [C = 0.482; 95% CI: 0.436, 0.528]. This shows that skilled delivery care utilization among women was disproportionately concentrated among the richer groups (pro-rich). Similarly, the concentration curve in the figures showed that the concentration graph of skilled birth attendance was below the line of equality which indicated that the distribution of skilled birth attendance was concentrated in rich households (pro-rich distribution) (Figure 1).
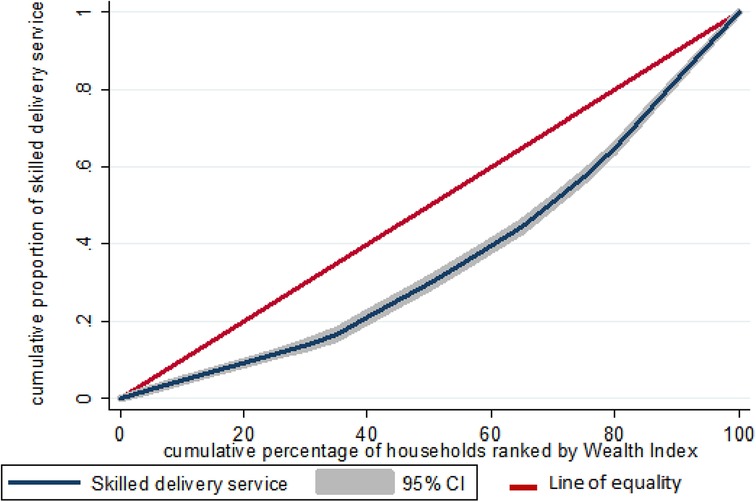
Figure 1. Wealth-related inequality of skilled birth attendance among reproductive-age women in Ethiopia, 2019 mini EDHS.
Spatial analysis results
Spatial and incremental autocorrelation analysis
Based on the 2019 mini-EDHS, the spatial patterns of unskilled birth attendance in Ethiopia revealed a significant spatial heterogeneity across the country over regions, which was found to be non-random with Global Moran's I value of 0.65 with (p < 0.00001) (Figure 2). The incremental autocorrelation result revealed statistically significant z-scores at a peak distance of 299.451 km 4.273 (distances; Z-score) for skilled birth attendance.
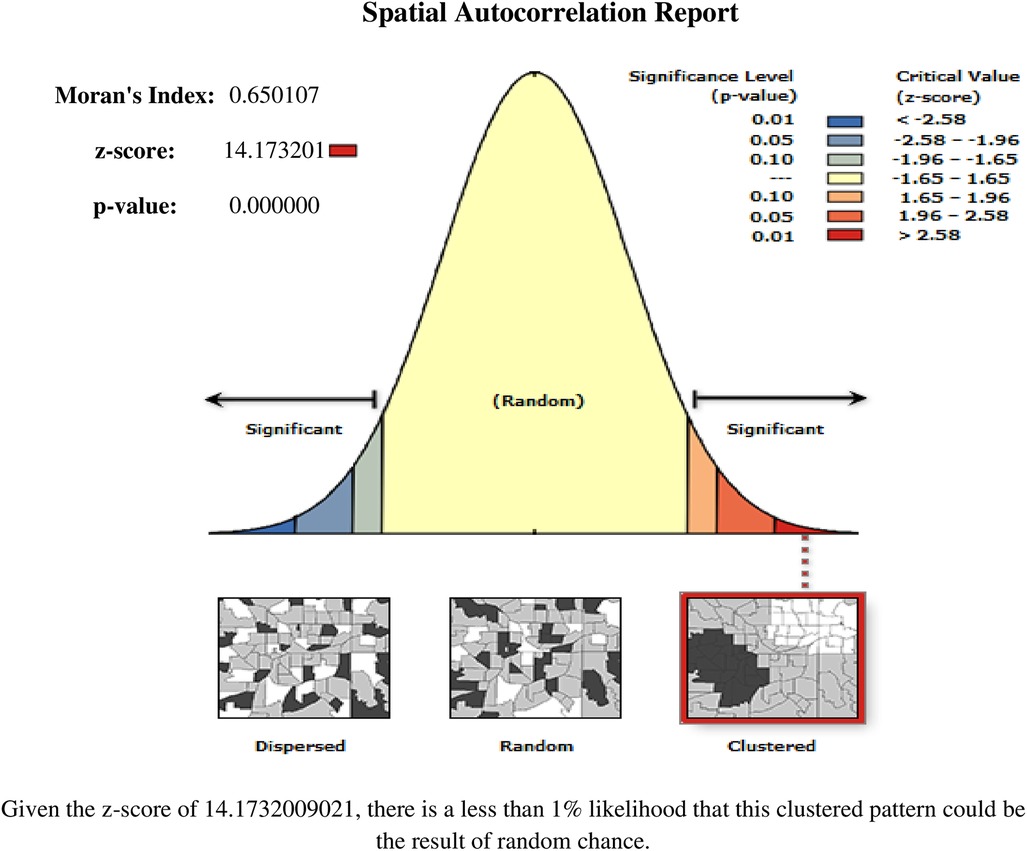
Figure 2. Spatial autocorrelation analysis of non-skilled birth attendance among reproductive-age women in Ethiopia, 2019 mini EDHS.
Spatial distribution of skilled birth attendance
For the spatial analysis of skilled birth attendance, a total of 305 clusters were considered. Each point on the map represents one enumeration area with a proportion of unskilled birth attendance in each cluster. The red color represents areas with a high proportion of unskilled birth attendance, while the blue color represents EAs with a lower proportion of skilled birth attendance (Figure 3).
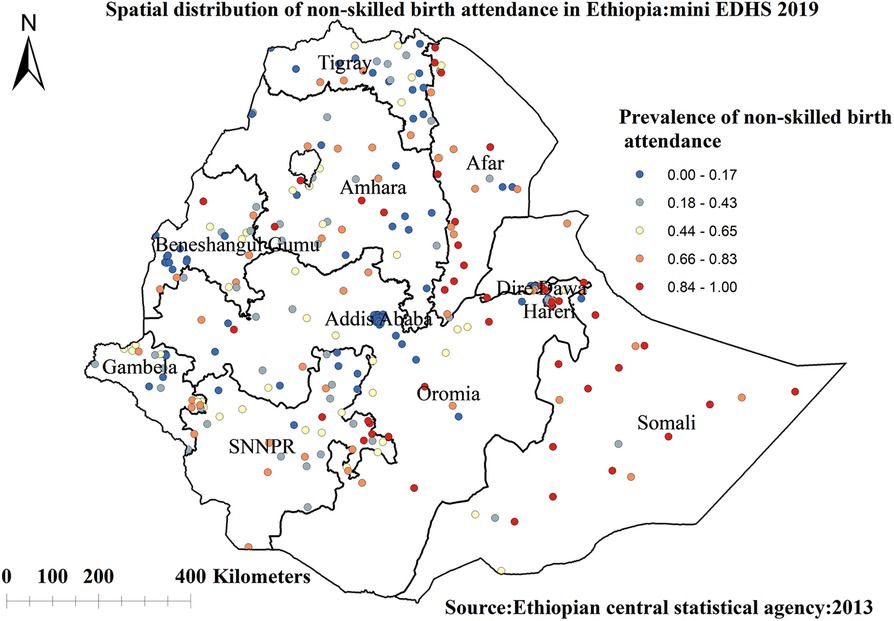
Figure 3. Spatial distribution of non-skilled birth attendance among reproductive-age women in Ethiopia, 2019 mini EDHS.
Hotspot and cold spot analysis
The red color indicates regions with significant hotspot areas (areas with high rates of unskilled birth attendance), which were found in Somalia, SNNP, Afar, and southern parts of the Amhara regions. The blue color indicates areas/regions with significantly lower rates of unskilled birth attendance (cold spot areas), which were found in Addis Ababa, Dire Dawa, Harari, and western Benishangul Gumuz regions (Figure 4).
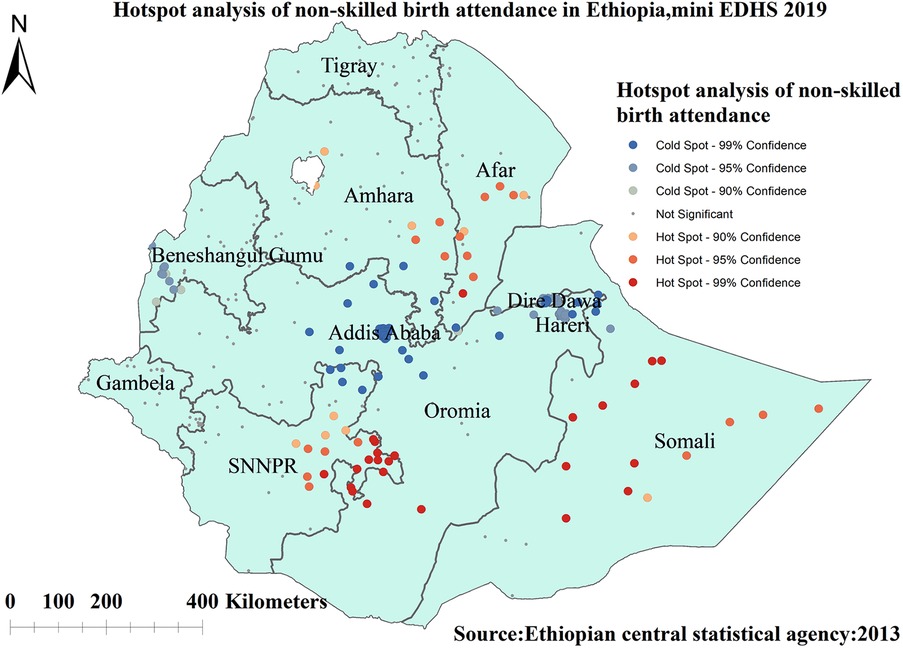
Figure 4. Hot spot analysis of non-skilled birth attendance among reproductive-age women in Ethiopia, 2019 mini EDHS.
Kriging interpolation analysis
Figure 5 indicated kriging interpolation methods of predicting the skilled birth attendance among reproductive-age women in Ethiopia. The predicted highest prevalence of unskilled birth attendance was detected in Somalia, Oromia, and some parts of the Afar regions of Ethiopia. In contrast, areas with the lowest prevalence of unskilled birth attendance were detected in Addis Ababa, Dire Dawa, Harari, and western Benishangul Gumuz regions of Ethiopia (Figure 5).
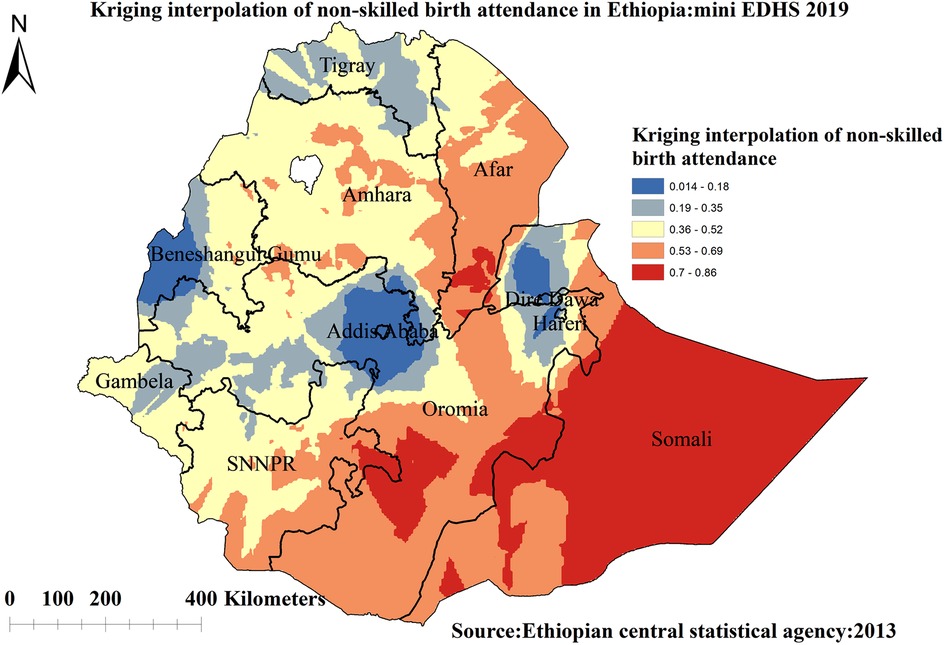
Figure 5. Kriging interpolation of non-skilled birth attendance among reproductive-age women in Ethiopia, 2019 mini EDHS.
Spatial scan statistical analysis
A spatial scan statistical analysis identified a total of 71 significant clusters, of which 27 were most likely (primary) clusters, and 44 were secondary clusters. The primary clusters were located in Somalia and some parts of Oromia region centered at 6.639662 N, 44.465855 E with a 390.28 km radius, a Relative Risk (RR) of 1.88 and Log-Likelihood Ratio (LLR) of 183.09, at p < 0.001. It showed that women inside the spatial window had a 1.88 times higher likelihood of using skilled birth attendance than women outside the spatial window (Figure 6).
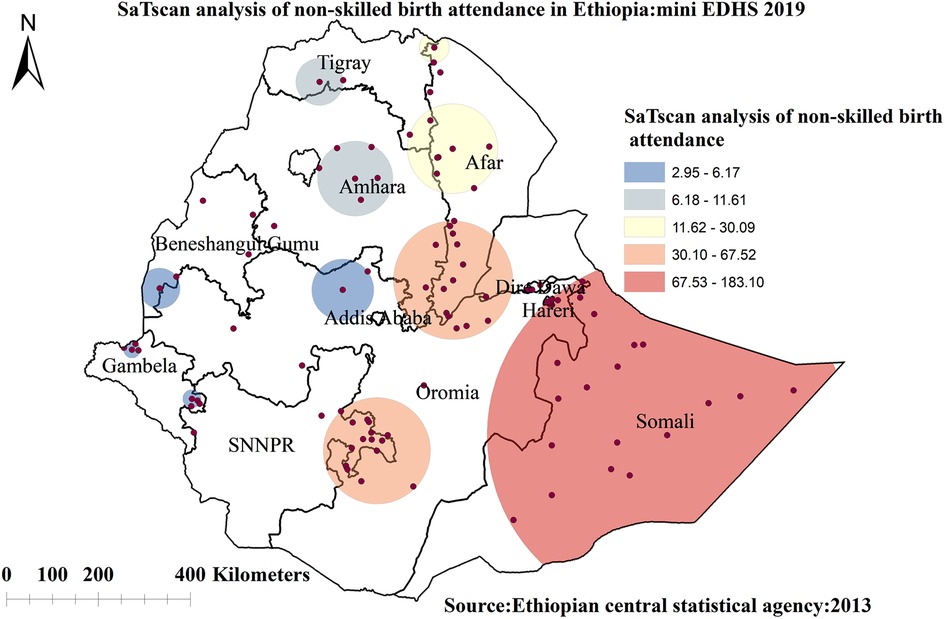
Figure 6. Spatial scan statistics analysis of non-skilled birth attendance among reproductive-age women in Ethiopia, 2019 mini EDHS.
The fixed effect analysis result
In the multivariable mixed-effect logistic regression model; age, educational ANC Visit, having radio and television, parity, household size, wealth index, residence, community level poverty, and community level of women’s education were significantly associated with skilled birth attendance.
Women aged 35–49 were 49% more likely to use skilled birth attendance (AOR = 1.49, 95% CI; 1.11–2.00) as compared to women age group 15–24. The odds of skilled birth attendance among women who were married were increased by 54% (AOR = 1.54, 95% CI; 1.09–2.17) as compared to unmarried women. The odds of using skilled birth attendance among women who had primary education were increased by 84% (AOR = 1.84, 95% CI; 1.52–2.22) as compared to those women with no formal education. Similarly, women who had secondary education had 2.87 (AOR = 2.87, 95% CI; 2.00–4.11) times higher odds of skilled birth attendance than women with no formal education.
The odds of using skilled birth attendance among women with rich were increased by 83% (AOR = 1.83, 95% CI; 1.43–2.33) as compared to poor wealth status. The odds of skilled birth attendance among women who had television were 2.15 (AOR = 2.15, 95% CI = 1.45, 3.18) times higher as compared to women who had no television. The odds of using skilled birth attendance among women who had a radio were 22% (AOR = 1.22, 95% CI = 1.00, 1.49) higher as compared to women who had no radio.
Women who had ANC visits were 4.31 times (AOR = 4.31, 95% CI; 3.38–5.50) more likely to use skilled birth attendance than those who had no ANC visit. Multiparous women are 70% (AOR = 0.30, 95% CI; 0.23–0.40) lower odds of utilizing skilled birth attendance than primiparious women. Women having a household size of greater than six have 20% (AOR = 0.80, 95% CI = 0.66, 0.96) lower odds of having skilled birth attendance than women having a household size of 1–5.
Women living in high-community women's education had 77% (AOR = 1.77, 95% CI = 1.10,2.87) higher odds of using skilled birth attendance than women living in low-level community women's education. Women living in high community-level poverty were 64% (AOR = 0.36, 95% CI = 0.21, 0.60) lower odds of utilizing skilled birth attendance than women living in low-level community poverty. Women living in rural areas were 59% (AOR = 0.41, 95% CI; 0.21–0.80) less likely to use skilled birth attendance, compared to their counterparts in urban areas (Table 3).
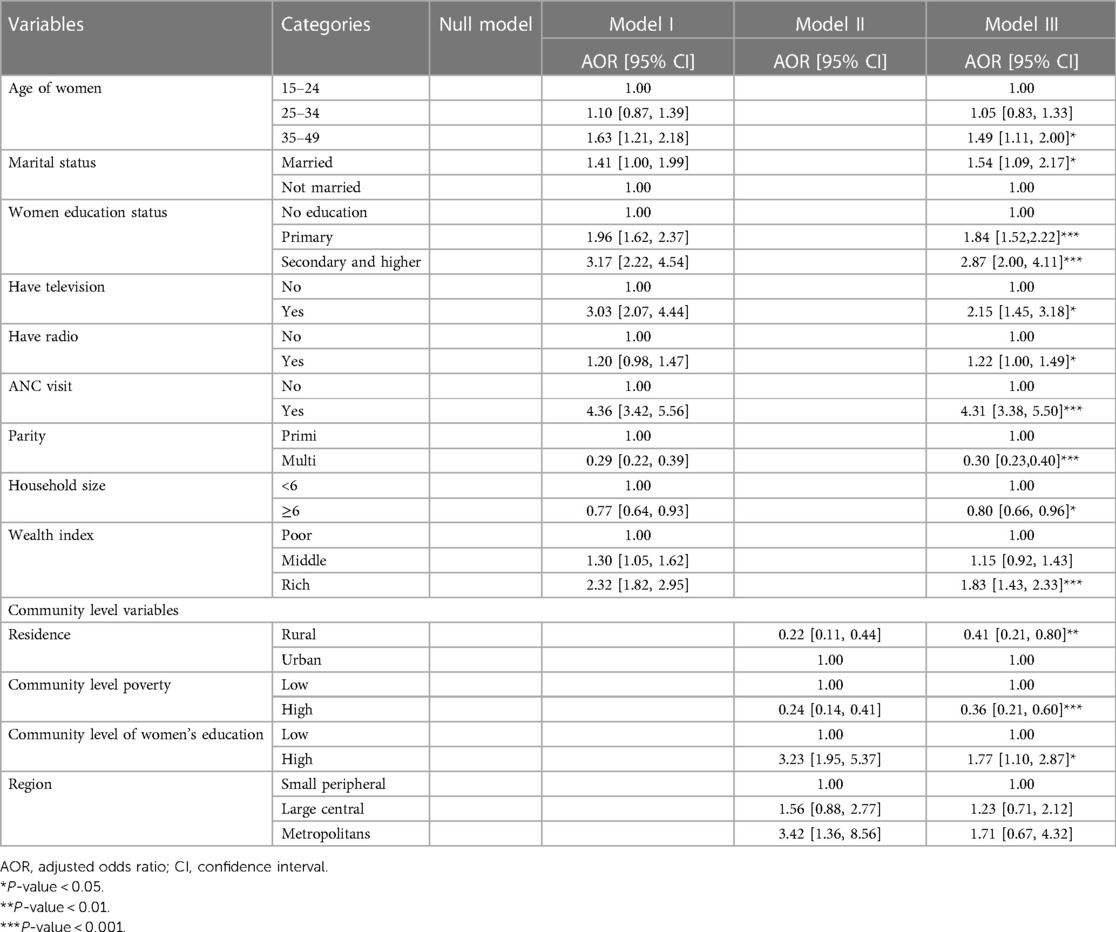
Table 3. Multilevel multivariable analysis of factors associated with skilled birth attendance among reproductive-age women, 2019 mini EDHS.
Discussion
Only half of reproductive-age women in Ethiopia attend their delivery with skilled birth attendants. The finding is similar to previous studies done in Nigeria (56) and higher than in a previous study done in Ethiopia (57), and Kenya (58), and lower than a study done in Bangladesh (59), and Cameron (36). The possible reason for the variation might be that many interventions were implemented at different locations and times, potentially increasing access to a health facility and skilled birth delivery services. The Ethiopian health sector transformation plan of 2016–2020 set a nationwide skilled birth attendance delivery target of 90% of deliveries, which has not been reached yet as per the 2019 EMDHS (60). The possible reason for these discrepancies might be due to the high proportion of women of reproductive age in Ethiopia faced impediments to healthcare access (61).
The spatial analysis revealed that the spatial distribution of unskilled birth attendance varied across the country. The regions with high rates of unskilled birth attendance were found in the Somalia, SNNP, Afar, and southern parts of the Amhara regions. The possible reason for the large proportion of unskilled birth attendance in these regions could be due to barriers to healthcare access and limited access to mass media, resulting in a lower utilization of skilled birth attendance (62, 63). A low rate of unskilled birth attendance was observed in Addis Ababa, Diredawa, Harari, and western Benishangul Gumuz regions. The difference could be due to women living in metropolis regions might have a better socioeconomic status and better access to health services, allowing them to use of skilled birth attendance (40). The statistically significant primary clusters with a high prevalence of unskilled birth attendance Somalia and some parts of Oromia regions of Ethiopia. The finding is supported by previous studies done in Ethiopia (40).
Women aged 35–49 were more likely to use skilled birth attendance as compared to women aged 15–24. The finding is similar to a study done in Nigeria and Malawi (64), Nepal (24), and East Africa (32). This could be because older women have more autonomy and may have enough money which leads them to have an access to skilled delivery services (64). Furthermore, the risks of childbirth associated with advanced age may initiate older women to use skilled birth attendance (64).
Married women were more likely to utilize skilled birth attendance than unmarried women. The finding is similar to a study done in Nigeria and Malawi (64). One possible explanation is that married women might have more financial resources and support, allowing them to pay the fees for skilled maternal health care (25).
Women with primary and secondary education were more likely to use skilled birth attendance during delivery than women with no formal education. Also living in a community with a high level of women's education are more likely to utilize skilled birth attendance. The finding is similar to a study done in Ghana (65, 66), and Kenya (8). Furthermore, by promoting health awareness, education may influence women's healthcare-seeking behavior (67).
The study's findings also revealed that women in the rich wealth index were more likely to use skilled birth attendance than women in the poor wealth index. The finding is similar to a study done in Kenya (8), Ghana (65), Bangladesh (28), Cameroon (36), and a systematic review done in African countries (68). In many low- and middle-income countries, the cost of delivery may be a significant barrier to the use of skilled birth attendants (67). Additional costs for women seeking delivery care include transportation costs as well as opportunity costs such as travel time, waiting time, and lost productive activities (69, 70). Studies also indicated that the lack of cost to travel to health facilities is the main barrier to using skilled birth attendance in Ethiopia, although the majority of maternal health services in Ethiopia are provided free of charge (71).
Women having large households are less likely to use skilled delivery care than women's having fewer household sizes (72). The possible justification could be a lack of resources and time constraints due to family care and household responsibilities among women having large household sizes.
Women who had television and radio had higher utilization of skilled birth attendance than women who did not have television or radio. The finding is consistent with a study done in Sierra Leone, Niger, and Mali (35), East Africa (32), Bangladesh (28), and Cameroon (36). Furthermore, a study conducted in Guinea found that women who watched television at least once a week were more likely to use skilled birth attendance (6). Studies also indicated that the use of mass media had a positive influence on the utilization of health services (73). One possible explanation is that information shared through the media raises community awareness and fosters a positive attitude toward healthcare utilization, which encourages women to use skilled birth attendance.
Our findings show that women who received antenatal care are more likely to receive skilled birth attendance than women who did not receive antenatal care. The result is consistent with studies done in Ethiopia (22), Kenya (8), Uganda (31), East Africa (32), Zambia (33), Bangladesh (34), Sierra Leone, Niger, and Mali (35), and India (74). The ANC visit is a critical pillar for safe motherhood since it provides access to the continuum of maternity care, skilled delivery care, and a variety of essential services that promote the mother's and newborn's health (75). One essential part of ANC is sharing information and counseling women about birth preparation, as well as encouraging the value of skilled birth attendance.
The findings from this study indicated that as parity increases the likelihood of using skilled birth attendance at birth decreases. The finding is similar to a study done in Ethiopia (16, 30), East Africa (32), and Uganda (31). The possible explanation is that multiparous women perceive delivery as a usual process and choose unskilled support during delivery that will have the confidence to give birth at home (8, 69). Furthermore, a lack of prior negative experience with skilled birth attendant-assisted delivery among the primiparious may lead them to have more skilled birth attendance than multiparous women (76).
Also, we found lower utilization of skilled birth attendance among women in rural areas as compared to women living in urban areas. The result is consistent with studies done in Ethiopia (29, 30), South Sudan (27), Bangladesh (28), and Cameroon (36). A possible justification could be a lack of good road infrastructure and transportation facilities in rural communities, which could hinder the utilization of skilled birth attendance.
The main strength of the study was that it used nationally representative data with large sample size and a suitable statistical approach to accommodate the data's hierarchical nature. However, this study had limitations in that the cross-sectional nature of the data makes it impossible to infer causality between the independent and dependent variables. Since this survey relies on respondents’ self-report, there may be the possibility of recall bias because respondents were questioned to remember events from the past. Furthermore, because it was a mini report, the EMDHS data did not include information about some predictor variables of skilled birth attendance.
Conclusion
Half of the women in Ethiopia did not utilize skilled birth attendance. Significant spatial clustering of unskilled birth attendance was observed in Ethiopia. Age, marital status, educational status, ANC Visit, having television and radio, parity, household size, wealth index, residence, community level poverty, and community level of women's education were significant predictors of skilled birth attendance. Skilled birth attendance was significantly and disproportionately concentrated in rich households (Pro-rich distribution). The regions of Somalia, SNNP, Afar, and southern Amhara were identified as having a high prevalence of using unskilled birth attendance. Public health interventions should target those women at high risk of using unskilled birth attendance and hotspot areas to improve use of skilled birth attendant uptake and improve maternal health. Policymakers should concentrate on enhancing health system coordination with multisectoral agents to improve skilled attendance at delivery.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: www.dhsprogram.com.
Author contributions
FMA, GA, AHT, and DGB wrote the main manuscript text. All authors reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to acknowledge the MEASURE DHS program for providing us data set.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ANC, antenatal care; AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; DHS, demographic and health survey; EAs, enumeration areas; EMDHS, Ethiopian mini demographic and health survey; ICC, intra class correlation; LLR, log-likelihood ratio; MOR, median Odd ratio; PCV, proportional change in variance; SBA, skilled birth attendance; SNNP, Southern nation nationalities of people; VIF, variance inflation factor; WHO, World Health Organization.
References
1. Mwebesa E, Kagaayi J, Ssebagereka A, Nakafeero M, Ssenkusu JM, Guwatudde D, et al. Effect of four or more antenatal care visits on facility delivery and early postnatal care services utilization in Uganda: a propensity score matched analysis. BMC Pregnancy Childbirth. (2022) 22:1–9. doi: 10.1186/s12884-021-04354-8
2. Alvarez JL, Gil R, Hernández V, Gil A. Factors associated with maternal mortality in Sub-Saharan Africa: an ecological study. BMC Public Health. (2009) 9(1):1–8. doi: 10.1186/1471-2458-9-462
3. Birmeta K, Dibaba Y, Woldeyohannes D. Determinants of maternal health care utilization in holeta town, central Ethiopia. BMC Health Serv Res. (2013) 13(1):1–10. doi: 10.1186/1472-6963-13-256
4. Adogu P, Egenti B, Ubajaka C, Onwasigwe C, Nnebue CC. Utilization of maternal health services in urban and rural communities of Anambra State, Nigeria. Niger J Med. (2014) 23(1):61–9.24946457
5. UNICEF. The State of the World’s Children 2009: Maternal and Newborn Health. New York, NY: Unicef (2008).
6. Ahinkorah BO, Seidu A-A, Agbaglo E, Adu C, Budu E, Hagan JE, et al. Determinants of antenatal care and skilled birth attendance services utilization among childbearing women in Guinea: evidence from the 2018 Guinea demographic and health survey data. BMC Pregnancy Childbirth. (2021) 21(1):1–11. doi: 10.1186/s12884-020-03489-4
7. Islam M, Yoshida S. MDG 5: how close are we to success? BJOG. (2009) 116:2–5. doi: 10.1111/j.1471-0528.2009.02335.x
8. Lawn J, Kerber K. Opportunities for Africa’s newborns: practical data, policy and programmatic support for newborn care in Africa. Part Mat, Newborn Child Health, Cape Town. (2006) 32.
9. Bongaarts J. WHO, UNICEF, UNFPA, World Bank Group, and United Nations Population Division Trends in Maternal Mortality: 1990 to 2015 Geneva: World Health Organization, 2015. Geneva: Wiley Online Library (2016).
10. Organization WH. Neonatal and Perinatal Mortality: Country, Regional and Global Estimates. Geneva: World Health Organization (2006).
11. Yakoob MY, Ali MA, Ali MU, Imdad A, Lawn JE, Van Den Broek N, et al. The effect of providing skilled birth attendance and emergency obstetric care in preventing stillbirths. BMC Public Health. (2011) 11(3):1–8. doi: 10.1186/1471-2458-11-S3-S7
12. Alkema L, Chou D, Hogan D, Zhang S, Moller A-B, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN maternal mortality estimation inter-agency group. Lancet. (2016) 387(10017):462–74. doi: 10.1016/S0140-6736(15)00838-7
13. Blencowe H, Cousens S, Jassir FB, Say L, Chou D, Mathers C, et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. (2016) 4(2):e98–e108. doi: 10.1016/S2214-109X(15)00275-2
14. Berhan Y, Berhan A. Skilled health personnel attended delivery as a proxy indicator for maternal and perinatal mortality: a systematic review. Ethiop J Health Sci. (2014) 24:69–80. doi: 10.4314/ejhs.v24i0.7S
15. Mannah MT, Warren C, Kuria S, Adegoke AA. Opportunities and challenges in implementing community based skilled birth attendance strategy in Kenya. BMC Pregnancy Childbirth. (2014) 14(1):1–12. doi: 10.1186/1471-2393-14-279
16. Tsegay Y, Gebrehiwot T, Goicolea I, Edin K, Lemma H, Sebastian MS. Determinants of antenatal and delivery care utilization in Tigray Region, Ethiopia: a cross-sectional study. Int J Equity Health. (2013) 12(1):1–10. doi: 10.1186/1475-9276-12-30
17. Esena RK, Sappor M-M. Factors associated with the utilization of skilled delivery services in the Ga East municipality of Ghana. Part 1: demographic characteristics. Int J Sci Technol Res. (2013) 2(8):184–94.
18. WHO. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF. UNFPA, World Bank Group and the United Nations Population Division. Geneva: WHO (2019).
19. Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comandé D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. (2016) 388(10056):2176–92. doi: 10.1016/S0140-6736(16)31472-6
20. Campbell OM, Calvert C, Testa A, Strehlow M, Benova L, Keyes E, et al. The scale, scope, coverage, and capability of childbirth care. Lancet. (2016) 388(10056):2193–208. doi: 10.1016/S0140-6736(16)31528-8
21. Campbell OM, Graham WJ. Strategies for reducing maternal mortality: getting on with what works. Lancet. (2006) 368(9543):1284–99. doi: 10.1016/S0140-6736(06)69381-1
22. Ayele GS, Melku AT, Belda SS. Utilization of skilled birth attendant at birth and associated factors among women who gave birth in the last 24 months preceding the survey in Gura Dhamole Woreda, Bale Zone, Southeast Ethiopia. BMC Public Health. (2019) 19(1):1–14. doi: 10.1186/s12889-019-7818-6
23. Do MJ. Utilization of skilled birth attendants in public and private sectors in Vietnam. J Biosoc Sci. (2009) 41(3):289–308. doi: 10.1017/S0021932009003320
24. Dhakal S, Van Teijlingen E, Raja EA, Dhakal KB. Skilled care at birth among rural women in Nepal: practice and challenges. J Health Popul Nutr. (2011) 29(4):371. doi: 10.3329/jhpn.v29i4.8453
25. Adewemimo AW, Msuya SE, Olaniyan CT, Adegoke AA. Utilisation of skilled birth attendance in Northern Nigeria: a cross-sectional survey. Midwifery. (2014) 30(1):e7–e13. doi: 10.1016/j.midw.2013.09.005
26. Mati K, Adegoke KK, Michael-Asalu A, Salihu HM. Health insurance coverage and access to skilled birth attendance in Togo. Int J Gynaecol Obstet. (2018) 141(2):181–8. doi: 10.1002/ijgo.12449
27. Mugo NS, Agho KE, Dibley MJ. Risk factors for non-use of skilled birth attendants: analysis of South Sudan household survey, 2010. Matern Child Health J. (2016) 20(6):1266–79. doi: 10.1007/s10995-016-1928-x
28. Kibria GMA, Ghosh S, Hossen S, Barsha RAA, Sharmeen A, Uddin SI, et al. Factors affecting deliveries attended by skilled birth attendants in Bangladesh. Matern Health Neonatol Perinatol. (2017) 3(1):1–9. doi: 10.1186/s40748-017-0046-0
29. Fekadu M, Regassa N. Skilled delivery care service utilization in Ethiopia: analysis of rural-urban differentials based on national demographic and health survey (DHS) data. Afr Health Sci. (2014) 14(4):974–84. doi: 10.4314/ahs.v14i4.29
30. Wilunda C, Quaglio G, Putoto G, Takahashi R, Calia F, Abebe D, et al. Determinants of utilisation of antenatal care and skilled birth attendant at delivery in South West Shoa Zone, Ethiopia: a cross sectional study. Reprod Health. (2015) 12(1):1–12. doi: 10.1186/s12978-015-0067-y
31. Kwagala B, Nankinga O, Wandera SO, Ndugga P, Kabagenyi A. Empowerment, intimate partner violence and skilled birth attendance among women in Rural Uganda. Reprod Health. (2016) 13(1):1–9. doi: 10.1186/s12978-016-0167-3
32. Tessema ZT, Tesema GA. Pooled prevalence and determinants of skilled birth attendant delivery in East Africa countries: a multilevel analysis of demographic and health surveys. Ital J Pediatr. (2020) 46(1):1–11. doi: 10.1186/s13052-020-00943-z
33. Jacobs C, Moshabela M, Maswenyeho S, Lambo N, Michelo C. Predictors of antenatal care, skilled birth attendance, and postnatal care utilization among the remote and poorest rural communities of Zambia: a multilevel analysis. Front Public Health. (2017) 5:11. doi: 10.3389/fpubh.2017.00011
34. Bhowmik J, Biswas R, Woldegiorgis M. Antenatal care and skilled birth attendance in Bangladesh are influenced by female education and family affordability: BDHS 2014. Public Health (Elsevier). (2019) 170:113–21. doi: 10.1016/j.puhe.2019.02.027
35. Ameyaw EK, Dickson KS. Skilled birth attendance in Sierra Leone, Niger, and Mali: analysis of demographic and health surveys. BMC Public Health. (2020) 20(1):1–10. doi: 10.1186/s12889-020-8258-z
36. Yaya S, Zegeye B, Ahinkorah BO, Seidu A-A, Ameyaw EK, Adjei NK, et al. Predictors of skilled birth attendance among married women in Cameroon: further analysis of 2018 Cameroon demographic and health survey. Reprod Health. (2021) 18(1):1–12. doi: 10.1186/s12978-021-01124-9
37. Chandrasekhar S, Gebreselassie T, Jayaraman A. Maternal health care seeking behavior in a post-conflict HIPC: the case of Rwanda. Popul Res Policy Rev. (2011) 30(1):25–41. doi: 10.1007/s11113-010-9175-0
38. Abera M, Belachew T. Predictors of safe delivery service utilization in arsi zone, south-east Ethiopia. Ethiop J Health Sci. (2011) 21(3):95–106.24776809
39. Teferra AS, Alemu FM, Woldeyohannes SM. Institutional delivery service utilization and associated factors among mothers who gave birth in the last 12 months in Sekela District, North West of Ethiopia: a community-based cross sectional study. BMC Pregnancy Childbirth. (2012) 12(1):1–11. doi: 10.1186/1471-2393-12-74
40. Teshale AB, Alem AZ, Yeshaw Y, Kebede SA, Liyew AM, Tesema GA, et al. Exploring spatial variations and factors associated with skilled birth attendant delivery in Ethiopia: geographically weighted regression and multilevel analysis. BMC Public Health. (2020) 20(1):1–19. doi: 10.1186/s12889-020-09550-3
41. Ahmed KY, Page A, Arora A, Ogbo FA. Trends and determinants of early initiation of breastfeeding and exclusive breastfeeding in Ethiopia from 2000 to 2016. Int Breastfeed J. (2019) 14(1):1–14. doi: 10.1186/s13006-019-0234-9
42. Teshale AB, Tesema GA. Prevalence and associated factors of delayed first antenatal care booking among reproductive age women in Ethiopia; a multilevel analysis of EDHS 2016 data. PLoS One. (2020) 15(7):e0235538. doi: 10.1371/journal.pone.0235538
43. Liyew AM, Kebede SA, Agegnehu CD, Teshale AB, Alem AZ, Yeshaw Y, et al. Spatiotemporal patterns of anemia among lactating mothers in Ethiopia using data from Ethiopian demographic and health surveys (2005, 2011 and 2016). PLoS One. (2020) 15(8):e0237147. doi: 10.1371/journal.pone.0237147
44. Sisay D, Ewune HA, Muche T, Molla W. Spatial distribution and associated factors of institutional delivery among reproductive-age women in Ethiopia: the case of Ethiopia demographic and health survey. Obstet Gynecol Int. (2022) 2022:1–12. doi: 10.1155/2022/4480568
45. Waldhör T. The spatial autocorrelation coefficient moran’s I under heteroscedasticity. Stat Med. (1996) 15(7-9):887–92. doi: 10.1002/(SICI)1097-0258(19960415)15:7/9%3C887:AID-SIM257%3E3.0.CO;2-E
46. McMillen DP. Geographically Weighted Regression: The Analysis of Spatially Varying Relationships. New York, NY: Oxford University Press (2004).
47. Wulder M, Boots B. Local spatial autocorrelation characteristics of remotely sensed imagery assessed with the getis statistic. Int J Remote Sens. (1998) 19(11):2223–31. doi: 10.1080/014311698214983
48. De Valck J, Broekx S, Liekens I, De Nocker L, Van Orshoven J, Vranken LJL, et al. Contrasting collective preferences for outdoor recreation and substitutability of nature areas using hot spot mapping. Landsc Urban Plan. (2016) 151:64–78. doi: 10.1016/j.landurbplan.2016.03.008
49. Franklin J. Mapping species Distributions: Spatial Inference and Prediction. Cambridge: Cambridge University Press (2010).
50. Le ND, Zidek JV. Interpolation with uncertain spatial covariances: a Bayesian alternative to kriging. J Multivar Anal. (1992) 43(2):351–74. doi: 10.1016/0047-259X(92)90040-M
51. Austin PC, Merlo J. Intermediate and advanced topics in multilevel logistic regression analysis. Stat Med. (2017) 36(20):3257–77. doi: 10.1002/sim.7336
52. Sommet N, Morselli D. Keep calm and learn multilevel logistic modeling: a simplified three-step procedure using stata, R, mplus, and SPSS. Int Rev Soc Psychol. (2017) 30:203–18. doi: 10.5334/irsp.90
53. Weinmayr G, Dreyhaupt J, Jaensch A, Forastiere F, Strachan DP. Multilevel regression modelling to investigate variation in disease prevalence across locations. Int J Epidemiol. (2017) 46(1):336–47. doi: 10.1093/ije/dyw274
54. Liyew AM, Teshale AB. Individual and community level factors associated with anemia among lactating mothers in Ethiopia using data from Ethiopian demographic and health survey, 2016; a multilevel analysis. BMC Public Health. (2020) 20:1–11. doi: 10.1186/s12889-020-08934-9
55. Merlo J, Chaix B, Yang M, Lynch J, Råstam L. A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health. (2005) 59(6):443–9. doi: 10.1136/jech.2004.023473
56. Imo CK, Ugwu NH, Ukoji UV, Isiugo-Abanihe UC. Intimate partner violence and its association with skilled birth attendance among women in Nigeria: evidence from the Nigeria demographic and health surveys. BMC Pregnancy Childbirth. (2022) 22(1):1–11. doi: 10.1186/s12884-021-04335-x
57. Tolossa T, Bekele D. Multilevel analysis of skilled birth attendance and associated factors among reproductive age women in Ethiopia: data from EDHS 2016. Int J Afr Nurs Sci. (2020) 13:100268. doi: 10.1016/j.ijans.2020.100268
58. Ibrahim HA, Ajuwon AJ, Oladokun A. Predictors of utilization of skilled birth attendants among women of reproductive age in Mandera East sub county, Mandera county, Kenya. Sci J Public Health. (2017) 5(3):230–9. doi: 10.11648/j.sjph.20170503.21
59. Nahar MT, Anik SFI, Islam MA, Islam SMS. Individual and community-level factors associated with skilled birth attendants during delivery in Bangladesh: a multilevel analysis of demographic and health surveys. PLoS One. (2022) 17(6):e0267660. doi: 10.1371/journal.pone.0267660
60. Anteneh HA. Inequality in Skilled Birth Attendance Service Utilization in Ethiopia across Geographic, Residential Differences and Level of Women’s Education. (2023).
61. Tamirat KS, Tessema ZT, Kebede FB. Factors associated with the perceived barriers of health care access among reproductive-age women in Ethiopia: a secondary data analysis of 2016 Ethiopian demographic and health survey. BMC Health Serv Res. (2020) 20:1–8. doi: 10.1186/s12913-020-05485-y
62. Okwaraji YB, Webb EL, Edmond KM. Barriers in physical access to maternal health services in Rural Ethiopia. BMC Health Serv Res. (2015) 15(1):1–8. doi: 10.1186/s12913-015-1161-0
63. Alamneh TS, Teshale AB, Yeshaw Y, Alem AZ, Ayalew HG, Liyew AM, et al. Barriers for health care access affects maternal continuum of care utilization in Ethiopia; spatial analysis and generalized estimating equation. PLoS One. (2022) 17(4):e0266490. doi: 10.1371/journal.pone.0266490
64. Atuoye KN, Amoyaw JA, Kuuire VZ, Kangmennaang J, Boamah SA, Vercillo S, et al. Utilisation of skilled birth attendants over time in Nigeria and Malawi. Glob Public Health. (2017) 12(6):728–43. doi: 10.1080/17441692.2017.1315441
65. Amoakoh-Coleman M, Ansah EK, Agyepong IA, Grobbee DE, Kayode GA, Klipstein-Grobusch K. Predictors of skilled attendance at delivery among antenatal clinic attendants in Ghana: a cross-sectional study of population data. BMJ Open. (2015) 5(5):e007810. doi: 10.1136/bmjopen-2015-007810
66. Gudu W, Addo B. Factors associated with utilization of skilled service delivery among women in rural northern Ghana: a cross sectional study. BMC Pregnancy Childbirth. (2017) 17(1):1–10. doi: 10.1186/s12884-016-1183-6
67. Yaya S, Bishwajit G, Shah V. Wealth, education and urban–rural inequality and maternal healthcare service usage in Malawi. BMJ Glob Health. (2016) 1(2):e000085. doi: 10.1136/bmjgh-2016-000085
68. Chukwuma A, Wosu AC, Mbachu C, Weze K. Quality of antenatal care predicts retention in skilled birth attendance: a multilevel analysis of 28 African countries. BMC Pregnancy Childbirth. (2017) 17(1):1–10. doi: 10.1186/s12884-016-1183-6
69. Gabrysch S, Campbell OMR. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. (2009) 9(1):1–18. doi: 10.1186/1471-2393-9-34
70. McIntyre D, Thiede M, Dahlgren G, Whitehead M. What are the economic consequences for households of illness and of paying for health care in low-and middle-income country contexts? Soc Sci Med. (2006) 62(4):858–65. doi: 10.1016/j.socscimed.2005.07.001
71. Kanini CM, Kimani H, Mwaniki P. Utilisation of skilled birth attendants among women of reproductive age in Central district, Kitui county, Kenya. Afr J Midwif Women’s Health. (2013) 7(2):80–6. doi: 10.12968/ajmw.2013.7.2.80
72. Ugboaja JO, Oguejiofor CB, Oranu EO, Igwegbe AO. Factors associated with the use of traditional birth attendants in Nigeria: a secondary analysis of 2013 Nigeria national demography and health survey. Nig J Gen Prac. (2018) 16(2):45. doi: 10.4103/NJGP.NJGP_27_17
73. Zamawe CO, Banda M, Dube AN. The impact of a community driven mass media campaign on the utilisation of maternal health care services in Rural Malawi. BMC Pregnancy Childbirth. (2016) 16(1):1–8. doi: 10.1186/s12884-016-0816-0
74. Nair M, Ariana P, Webster P. What influences the decision to undergo institutional delivery by skilled birth attendants? A cohort study in Rural Andhra Pradesh, India. Rural Remote Health. (2012) 12(4):1–11.22624570
75. AbouZahr C, Wardlaw T. Antenatal Care in Developing Countries: Promises, Achievements and Missed Opportunities-an Analysis of Trends, Levels and Differentials, 1990-2001. Geneva: World Health Organization (2003). p. 32.
Keywords: skilled birth attendance, women, spatial variation, multilevel analysis, Ethiopia
Citation: Aragaw FM, Atlie G, Tesfaye AH and Belay DG (2024) Spatial variation of skilled birth attendance and associated factors among reproductive age women in Ethiopia, 2019; a spatial and multilevel analysis. Front. Glob. Womens Health 5:1082670. doi: 10.3389/fgwh.2024.1082670
Received: 28 October 2022; Accepted: 16 July 2024;
Published: 12 August 2024.
Edited by:
Mrutyunjaya Bellad, Jawaharlal Nehru Medical College, IndiaReviewed by:
Bilal Ahmed Usmani, Aga Khan University, PakistanAnke van der Kwaak, Royal Tropical Institute (KIT), Netherlands
© 2024 Aragaw, Atlie, Tesfaye and Belay. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fantu Mamo Aragaw, ZmFudHVtYTNAZ21haWwuY29t
 Fantu Mamo Aragaw
Fantu Mamo Aragaw Gela Atlie2
Gela Atlie2 Amensisa Hailu Tesfaye
Amensisa Hailu Tesfaye Daniel Gashaneh Belay
Daniel Gashaneh Belay